
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Nutr. , 28 October 2022
Sec. Clinical Nutrition
Volume 9 - 2022 | https://doi.org/10.3389/fnut.2022.946378
This article is part of the Research Topic Diet Behavior and Heart Health View all 21 articles
 Simone Radavelli-Bagatini1*
Simone Radavelli-Bagatini1* Abadi K. Gebre1
Abadi K. Gebre1 Mary A. Kennedy1
Mary A. Kennedy1 Marc Sim1,2
Marc Sim1,2 Lauren C. Blekkenhorst1,2
Lauren C. Blekkenhorst1,2 Catherine P. Bondonno1,2
Catherine P. Bondonno1,2 Ben Jackson3,4
Ben Jackson3,4 James Dimmock5
James Dimmock5 Markus P. Schlaich6,7,8
Markus P. Schlaich6,7,8 Jonathan M. Hodgson1,2
Jonathan M. Hodgson1,2 Joshua R. Lewis1,2,9
Joshua R. Lewis1,2,9Background: Although a healthy diet and physical activity have been shown to prevent or delay cardiovascular disease (CVD) hospitalizations and deaths, most adults do not meet current guidelines. Provision of coronary artery calcification (CAC) and carotid ultrasound (CUS) imaging results may motivate beneficial lifestyle changes. We scoped the existing literature for studies providing non-invasive vascular imaging results and reporting diet, physical activity, and/or anthropometric measures to identify knowledge gaps and opportunities for further research.
Methods: A systematic search was performed across three electronic databases, in line with PRISMA ScR guidelines and Arksey and O'Malley's scoping review framework.
Results: Twenty studies (thirteen observational and seven randomized controlled trials) examining the impact of provision of CAC/CUS imaging results on diet and/or physical activity behaviors were included. Nearly half the studies did not clearly state whether participants received dietary and physical activity advice along with vascular imaging results, and these were secondary outcomes in most studies, with data assessment and reporting being inconsistent.
Conclusion: Well-designed clinical trials with consistent and clear messaging based on detailed subjective and objective measures of diet and physical activity are needed to determine whether this approach may stimulate long-term dietary and physical activity change.
Cardiovascular disease (CVD) accounts for almost 1 in 3 deaths globally, with the majority (85%) attributable to either ischemic heart disease or cerebrovascular disease (1). Most survivors have substantially impaired quality of life due to ongoing functional deficits (2, 3). Suboptimal lifestyle behaviors are the leading causes of CVD globally (4), and most CVD-related events could be prevented or substantially delayed by improving diet, increasing physical activity, and ceasing smoking (1). Even modest sustained lifestyle changes can reduce CVD risk (5). Despite evidence showing that high consumption of fruit and vegetables (FV) can lead to an estimated 20% lower risk of CVD, compared to low FV intake (a 5% lower risk for each additional serving) (6), only 51 and 8% of Australians meet the minimum recommended 2 serves of fruit (≥300 g/d) and 5 serves of vegetables (≥375 g/d) daily (7, 8), respectively. Moreover, only 15% of adults age 18–64 years meet the recommended amount of physical activity (9) each week. Clearly, currently policies and strategies to increase FV intake to recommended amounts have not been successful. New strategies are warranted to further encourage a healthier diet and lifestyle, aiming at improving heart health, and provision of vascular health may further encourage these changes. High quality evidence from large randomized controlled trials (RCTs) and meta-analyses has shown that provision of vascular imaging can increase behavior change resulting in improved medication adherence in the long term (10–12), highlighting its potential utility as a promising approach to elicit diet and physical activity change. This is because people are more likely to make healthy changes if they perceive they are at risk of developing a disease and that the condition can lead to serious consequences (13).
Vascular health is commonly assessed in the coronary arteries (coronary artery calcification [CAC]) or in the carotid arteries (carotid ultrasound [CUS]). CAC testing has been increasingly used in clinical practice to screen asymptomatic patients for advanced atherosclerosis (14, 15) and to identify asymptomatic individuals at higher risk of future cardiovascular events (16). CUS is used to assess common carotid artery intimal medial thickness (cIMT) and focal carotid atherosclerotic plaques, as measures of carotid atherosclerosis (17). Detection of CAC using computed tomography (CT) and ultrasound, has been shown to strongly predict future cardiovascular events (16) among asymptomatic individuals. It has been proposed that such imaging techniques could provide superior insight as a marker of CVD risk, beyond conventional risk factors (18).
Although the impact of provision of vascular health imaging on medication adherence is well-known, the effects on diet and physical activity behaviors are less certain due to the lack of well-designed clinical trials with a focus on those outcomes. A systematic review and meta-analysis including six studies with a total of 11,256 participants on the impact of provision of CAC results on medication initiation and continuation, as well as on preventive lifestyle changes, observed improvements in the use of aspirin (OR [95%CI]: 2.6 [1.8–3.8], lipid-lowering medication: 2.9 [1.9–4.4], hypertension medication: 1.9 [1.6–2.3] and continuation of lipid-lowering medication: 2.3 [1.6–3.3]) (19). In addition, participants with abnormal CAC scans significantly improved their diet and exercise (OR [95%CI]: 1.9 [1.5–2.5] and 1.8 [1.4–2.4], respectively), compared to those with absence of CAC (19). However, no studies have mapped the literature to understand key features of these studies and highlight the areas of focus for improving diet and physical activity as part of provision of vascular health imaging.
The aim of this scoping review was to map the literature to understand the evidence to date and identify opportunities to implement diet and physical activity interventions to support changes in these areas. We sought to summarize the literature to identify the nature of study participants, understand how messages were conveyed to participants and which recommendations were provided, as well as to highlight which tools were used to measure the outcomes of interest, and the duration of follow-up period. The outcomes of this study may allow us to identify gaps in the literature to guide the design of high-quality RCTs.
Our study was guided by Arksey and O'Malley (20) scoping review framework and included five stages: (1) the research question was identified; (2) relevant studies were flagged; (3) suitable studies were selected; (4) data was charted and; (5) relevant information was collated, summarized and described. The PRISMA Extension for Scoping Reviews (PRISMA-ScR) checklist was also used to guide this review (21).
A scoping review question was established with the view of broadly scoping the evidence in the literature that suggests provision of non-invasive carotid or coronary vascular imaging can promote healthy diet and physical activity change, with best practices being not clear:
By scoping the literature to identify studies in asymptomatic adults that provided non-invasive carotid or coronary vascular imaging and measured diet and/or physical activity, can we determine which approaches may lead to healthy long-term changes in diet and physical activity, in whom and why?
The search for studies focused on the effects of knowledge of vascular health across the adult lifespan on changes in diet and physical activity, and anthropometric measures (as a result of changes in diet and physical activity). Full text original articles available in English with no restriction on year of publication were included. The inclusion criteria for studies were: (1) adult men and women without prior diagnosis of CVD; (2) carotid or coronary vascular imagining results provided to participants; (3) studies with information on changes in diet and/or physical activity and/or anthropometric measures after provision of vascular imaging results. We used these inclusion criteria to reflect an approach to primary prevention using vascular imaging results.
A comprehensive online literature search of scientific papers listed on Medline, Embase, and CINAHL was undertaken from database inception until January 24th, 2022. A hand search of references and gray literature sources were also performed (e.g., Google Scholar), to ensure that all relevant articles were included. Table 1 shows the search terms included in this review. Although the term “behavior change” is broad and may include behaviors not related to diet and physical activity (psychological behavior changes, for example), this was included in our search to identify any publications that may have included any of our outcomes of interest and avoid missing relevant studies. To ensure that variations of all keywords were retrieved, keywords and combinations of keywords were used, as well as the wildcard symbol (*). No limits or filters were used for year of publication. Only articles published in English and including adults (age ≥18 years) were considered. Only data related to pre-established outcomes of interest were extracted.
A total of 821 publications were retrieved using the search terms, and 4 other articles were retrieved by hand search. Figure 1 shows the PRISMA flow diagram. All references were imported into EndNote software and screened for duplicates (n = 188). Screening of the remaining 637 studies was conducted in the following order: (i) article title; (ii) abstract; and (iii) full text. Two authors (SRB and AKG) screened all articles for specific outcomes of interest. The following words were used to identify the outcomes of interest for this review: diet, exercise, physical activity, exercise, nutrition, weight, BMI, body mass index, body mass, body composition, waist circumference. Discrepancies between the screening authors were resolved through discussions with a senior author (JRL) until consensus was reached. A total of 20 studies were eligible and therefore included in this scoping review (Figure 1).
Data from each of the selected records were presented in a narrative format and sorted into tables in chronological order (oldest to newest publications). Pertinent data were retrieved from eligible articles including authorship, publication year, and country; population details (sample size, age, sex); methods and intervention details; outcomes of interest (for RCTs); follow-up period; and significant findings for the outcomes of interest, for both observational (Table 2) and RCT (Table 3) studies. The outcomes of interest found in the records included: overall diet composition, vegetable intake, fiber intake, fat intake, salt intake, consumption of processed foods, exercise/physical activity and anthropometric measures which included body weight and/or body mass index (BMI), and waist circumference.
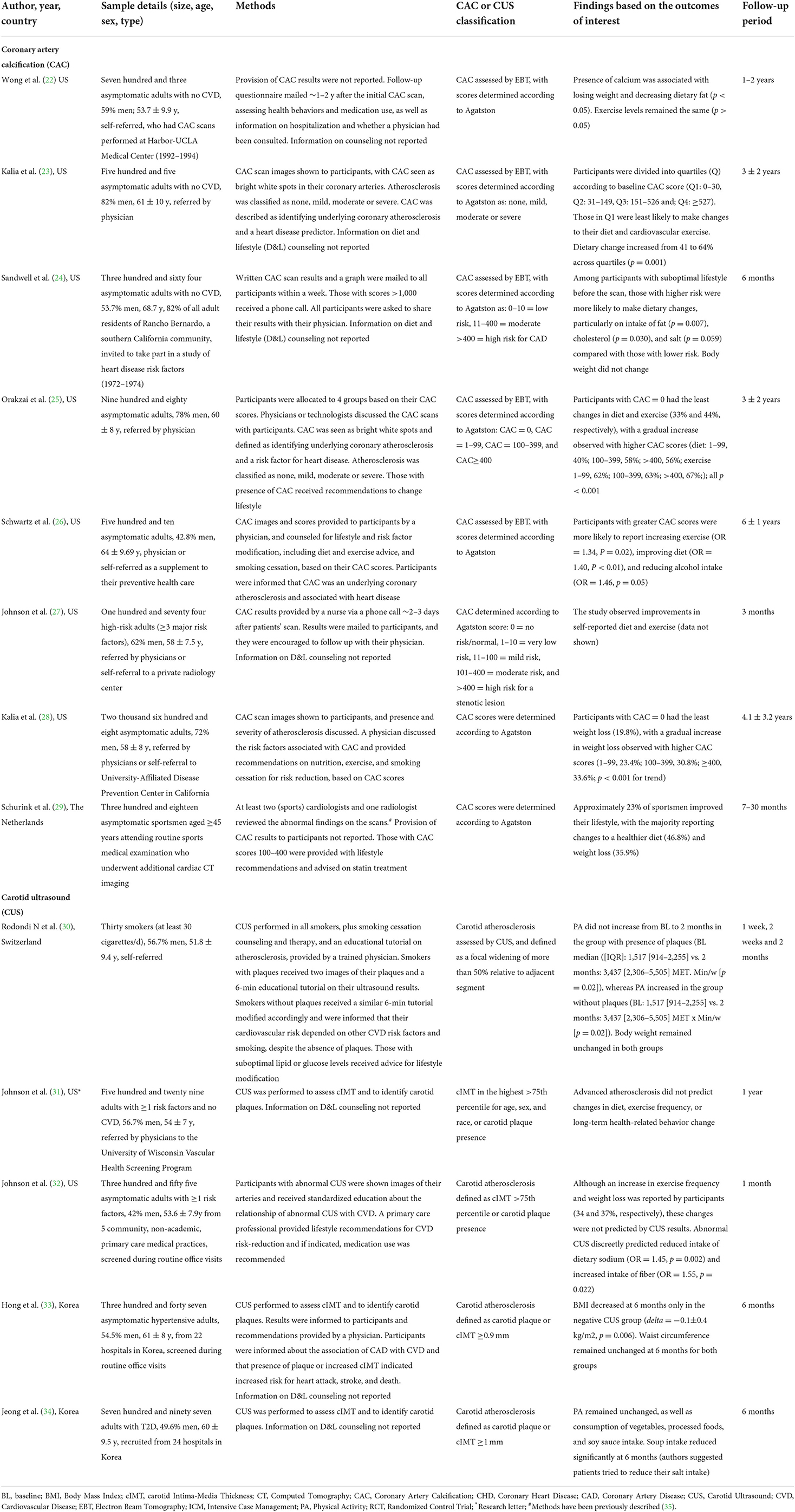
Table 2. Summary of observational studies on provision of CAC and CUS results and changes in diet, physical activity and anthropometric measures.
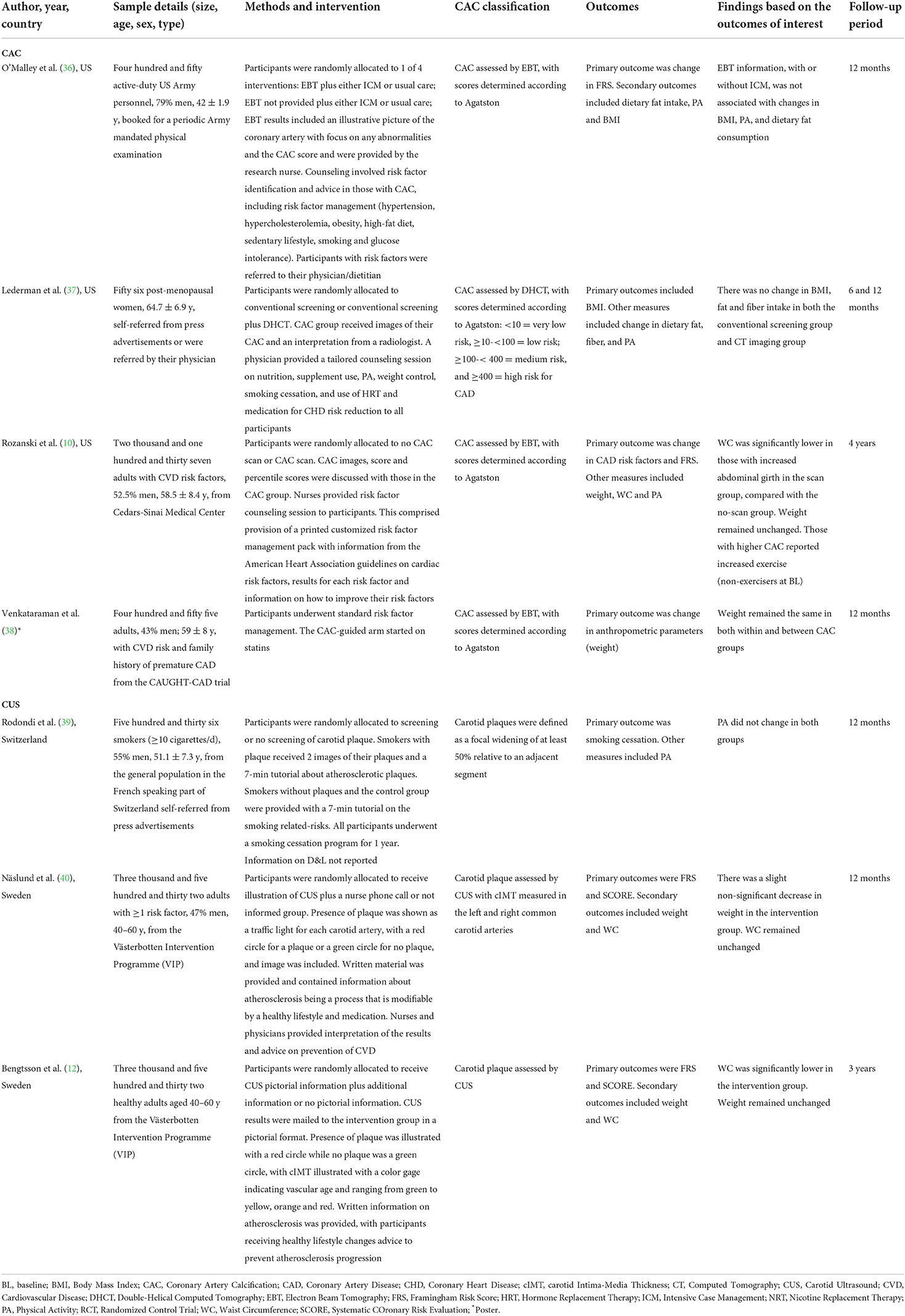
Table 3. Summary of RCTs on provision of CAC and CUS results and changes in diet, physical activity and anthropometric measures.
Twenty studies (10, 12, 22–34, 36–40) met the inclusion criteria by providing vascular images to motivate changes toward improving diet, physical activity or anthropometric measures. Of these, thirteen were observational studies (22–34) and 7 were RCTs (10, 12, 36–40). Nineteen articles were published within 2006 to 2021, while one study was published in 1996 (Tables 2, 3).
The outcomes of interest found in the eligible studies comprised: overall diet composition (23, 25–27, 29, 31, 34), vegetable intake (34), fiber intake (32, 37), fat and cholesterol intake (22, 24, 36, 37), salt intake (24, 32), consumption of processed foods (34), and amount of physical activity or exercise (10, 22, 23, 25–27, 30–32, 34, 36, 39). These components were chosen due to their role as critical modifiable lifestyle factors to prevent and/or delay the development of CVD. Studies which examined weight and/or BMI (10, 12, 22, 24, 28–30, 32, 33, 36–38, 40) and waist circumference (10, 12, 33, 40) were also included, as those measures are likely to change primarily as a result of changes in diet and/or physical activity. Results regarding the positive and neutral changes on diet, physical activity, and anthropometric measures, due to provision of vascular imaging, for the observational studies and RCTs can be found in Table 4.
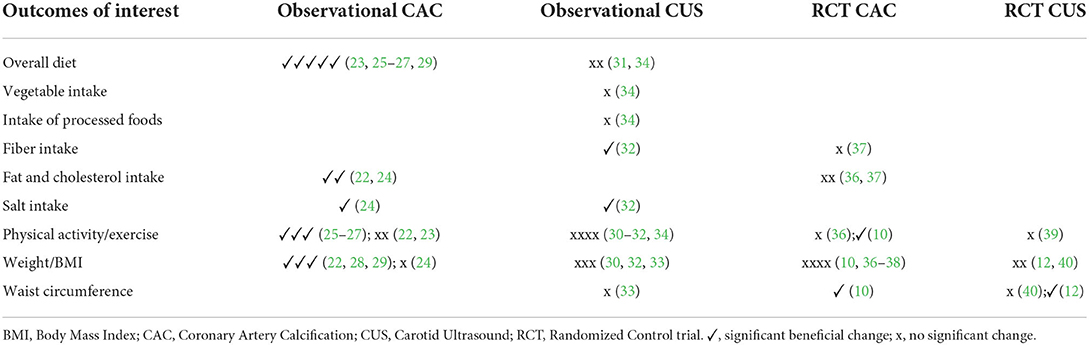
Table 4. Changes in diet, physical activity and anthropometric measures in observational studies and RCTs.
The mean age of participants across studies ranged from 45 to 69 years, and the sample sizes varied from 30 to 2,608. The changes in diet, physical activity or anthropometric measures were investigated over a period of 1 month to 6 years following provision of results. For clarity, the characteristics and findings of the studies are presented separately for observational studies and RCTs, due to the particular characteristics of each type of study.
In the observational studies, participants were asymptomatic (Table 2) and included healthy individuals (22–26, 28, 29), smokers (30), adults with at least one CVD risk factor (27, 31, 32), individuals with hypertension (33) and individuals with type 2 diabetes (34). Participants were recruited by contacting the study investigators directly (22, 30), or referred by physicians (23, 25, 31), or a combination of the above (26–28), and were enrolled at routine clinic visits (29, 32, 33), or at hospitals (34). In one study, investigators recruited a subsample of most residents (82%) from a southern California community (24) (Table 2).
In the observational studies, CAC and CUS results were provided to participants either as images only (23, 25, 28, 32), a combination of images/graphs and/or scores/text (24, 26), pictures followed by an educational tutorial (30), or via a phone call followed by mailed written information (27). Five studies did not report or specify this information (22, 29, 31, 33, 34). The results were provided to participants by physicians (25, 26, 28), a primary care provider (27, 32), mailed to participants (24) or were not reported / not specified (22–24, 29–31, 33, 34). Two observational studies (26, 28) clearly stated that participants were provided with diet and physical activity recommendations, with all other studies mentioning general lifestyle modifications or not reporting on providing any information. Only 38% (n = 5) of the studies provided participants with specific recommendations for lifestyle change (25, 26, 28, 30, 32), with one proving specific lifestyle advice to a subgroup with abnormal lipid or glucose levels (30).
In the observational studies, diet and physical activity changes made by participants were followed up via mail (22, 24, 26, 27, 32), electronically (29) and face-to-face during clinic visits (28, 30, 34). In two studies, follow-up data were obtained via surveys/interviews (25, 31), but the authors did not specify whether surveys were mailed to participants, or whether interviews took place face-to-face or via phone.
Results relating to the impact of provision of vascular imaging results on diet, physical activity and anthropometric measures were charted (Table 2). Observational studies exploring the associations between provision of coronary artery and carotid calcification and changes in diet yielded mixed results. Five studies (out of seven studies) observed a positive change in overall diet measures (23, 25–27, 29). Improvements in dietary fiber (32), fat (22, 24) and salt (24, 32) were observed. However, no changes were observed for consumption of vegetables (34) or processed foods (34). Positive changes in weight and/or BMI were observed in three studies (out of seven studies) (22, 28, 29). However, waist circumference remained similar (33). Three studies (25–27) reported an increase in physical activity levels after provision of vascular imaging results (Table 2).
In the RCTs (Table 3), participant were either smokers (39), post-menopausal women (37), adults with CVD risk factors (10, 38, 40), and otherwise healthy individuals (12, 36). Sample sizes varied from 56 to 3,532 and the mean/median age of participants ranged from 42 to 65 years. The duration of interventions in the RCTs ranged from 6 months to 4 years. Across RCTs, participants were recruited from previous trials (12, 38, 40), a medical center (10), self-referral (39), both self-referral or referral from physicians (37), or a mandatory periodic physical examination (36) (Table 3).
In the RCTs, CAC and CUS results were mainly provided as images (36), or a combination of images with written information (12, 37, 40), including scores (10), as well as a video (39). In one of the studies this information was not reported (38). Except for two RCTs that reported that the results were delivered to participants by a research nurse (10, 36) and via mail (12), this information in all others studies was not specifically stated (37–40). Only two RCTs (36, 37) clearly specified that counseling on diet and physical activity was provided to participants. All other RCTs (n = 5) provided counseling with focus on risk factor management and lifestyle without explicitly mentioning diet and physical activity (10, 12, 38–40). Further details have been reported in Table 3.
RCT study participants were followed-up at clinic visits after 6 months to 4 years following provision of results (10, 12, 36–40).
The RCTs focused on changing Framingham Risk Score (FRS) (10, 12, 36, 40), Systematic Coronary Risk Evaluation (SCORE) (12, 40), smoking cessation (39), and improving risk factors such as blood pressure and lipids, rather than diet, physical activity and anthropometric measures. Therefore, these trials were not specifically designed to examine whether provision of CAC and CUS could lead to healthy changes in diet, physical activity and anthropometric measures. Only two RCTs (37, 38) included BMI and body weight within their primary outcomes. In all other RCTs, diet, physical activity and anthropometric measures were considered secondary or non-specified outcomes (Table 3).
Findings from seven RCTs included in this scoping review (Table 5) showed that provision of scan results did not lead to changes in the intake of dietary fiber and fat a year later, compared to the no scan group (37). Similarly, BMI remained unchanged in both the scan and no scan groups (37). In the EISNER (Early Identification of Subclinical Atherosclerosis by non-invasive Imaging Research) study (10), when comparing the CAC scan group with the non-CAC scan group, investigators observed a significant decrease in waist circumference at 4 years in a subgroup with increased waist circumference (M>40, W>35) at baseline (Table 5), whereas body weight remained unchanged (10). Provision of vascular imaging did not lead to changes in physical activity levels in the scan group, compared to no scan group over 1 year (39) and 4 years (10).
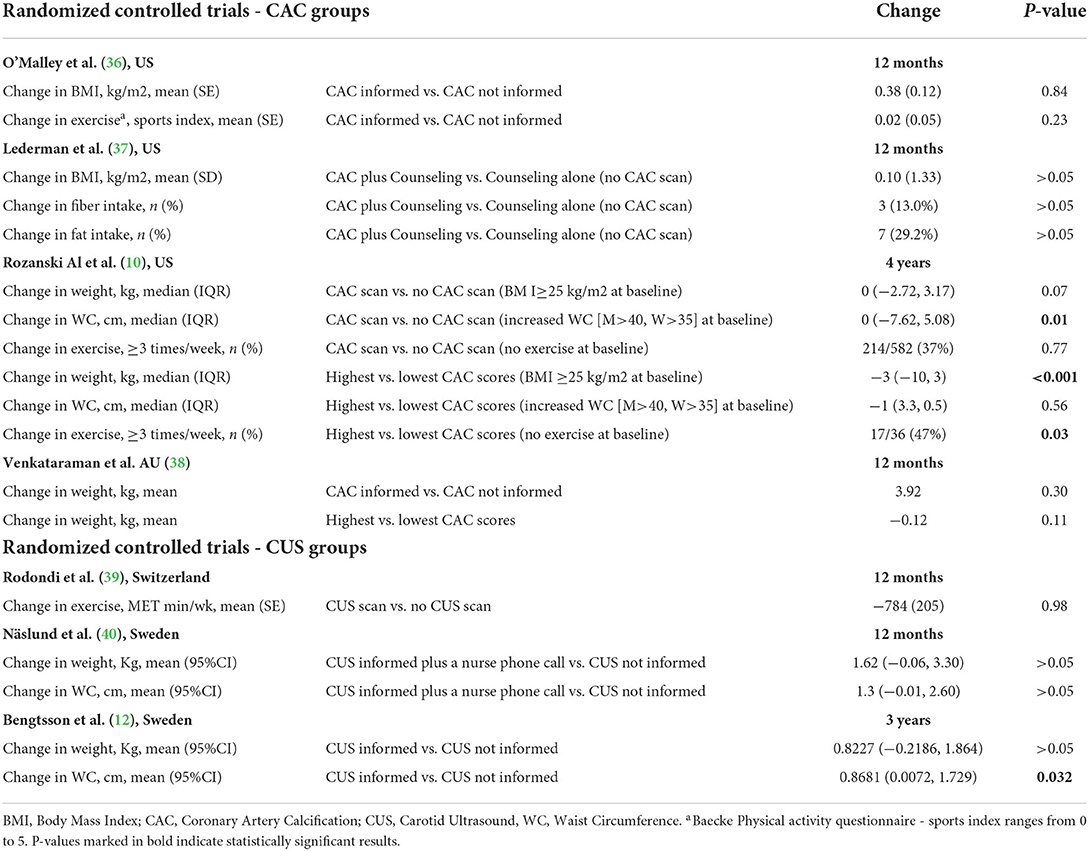
Table 5. Changes in diet, physical activity and anthropometric measures according to CAC and CUS scores in RCTs.
Compared to participants who were not informed of their scan results, provision of vascular imaging did not lead to reductions in body weight (12, 38, 40) or BMI (36). Waist circumference did not change after 1 year in one study (40), but provision of CUS led to significant reductions in another study (12) after 3 years of provision of results, compared to the group not informed (Table 5). No changes in physical activity were observed in participants after a year of being informed of their vascular results, compared to those who were not informed (36).
When examining the changes within groups according to CAC/CUS scores in the EISNER study (10), participants who were overweight and had a CAC score >100 had a greater weight loss after 4 years (Table 5). However, no significant changes in body weight were observed within groups in the Venkataraman trial (38). Participants with higher CAC scores in the EISNER study (10), who were non-exercisers at baseline, reported an increase in exercise levels after 4 years.
A range of instruments were used to assess diet and physical activity in the eligible studies, with many being self-reported or single-item questions (Supplementary Tables S1, S2, for observational and RCT studies, respectively). The results were also reported in several different ways (i.e., mean ± SE, mean (SE), median and interquartile range, mean and 95% confidence interval) and given in dissimilar unit measures (i.e., MET, min/week, percentages), which makes comparability of results difficult.
In this scoping review, we identified many gaps and opportunities to inform the design of future high quality RCTs providing vascular imagining results to elicit positive changes to diet and physical activity. We revealed three key messages. First, the results of observational studies gathered in this scoping review suggest that providing CAC and CUS imaging could lead to healthy changes to diet, physical activity, and anthropometric measures (weight, BMI and waist circumference). However, well-designed clinical trials with particular focus on improving diet and physical activity and reducing anthropometric measures (rather than focused on CVD risk factor management) are needed to strengthen quality of evidence regarding the impact of CAC and CUS imaging results on these particular lifestyle behaviors. Secondly, the outcomes of interest in the present review were mainly secondary or non-specified outcomes for the studies included. These studies were largely designed to answer a broader question, focusing mainly on estimated cardiovascular risk or smoking cessation. Finally, the methodologies used varied significantly. For instance, few studies included counseling sessions or other well-recognized behavior change techniques, such as methods for self-monitoring (41). Studies using provision of vascular health imagining eliciting changes on CVD risk have demonstrated mixed results. There is need for interventions to be tested in large clinical trials before implementing in clinical practice (15).
Twenty studies examining the impact of provision of CAC/CUS imaging results on diet and/or physical activity were reviewed. Of these, twelve studies focused on CAC (four RCTs and eight observational) and eight studies focused on CUS (three RCTs and five observational). Half of the participants were free of CVD and the other half were at high risk for CVD (at least 1 CVD risk factor, i.e., smokers, hypertensive). Most studies reported providing written/verbal/imaging results but only some studies clearly stated they provided dietary and physical activity advice when providing vascular imaging results. None of the RCTs had dietary or physical activity as a primary outcomes and assessment and reporting of the outcomes were suboptimal and inconsistent among studies. The considerations discussed below can potentially help with the design of future studies where participants receive appropriate guidance and support after provision of vascular imaging, which can be translated into significant changes to their diet and physical activity.
We observed that the primary outcomes of most of the studies included in this scoping review focused on managing blood pressure and smoking cessation, rather than changing diet, physical activity and anthropometric measures. Hence, the recommendations for behavior changes were focused on medication and other therapies specific to manage those outcomes. Although some RCTs provided information on risk factor management (10, 36, 38, 39), specific recommendations to promote a healthy diet and lifestyle, beyond risk factor management, was a missed opportunity. Evidence shows that providing this information grounded in theory can produce change, helping people to make healthier choices. Such changes have the potential to translate to a more successful change in diet, physical activity and body weight as well as risk factor management.
In general, the methodologies of the studies included in this review varied greatly, making it difficult to determine which study design would have been potentially more promising at leading to positive changes in diet and physical activity. These included: disparities in randomization methods (i.e., CAC informed group vs. not informed, or CAC performed vs. not performed), instruments used to assess diet and physical activity (e.g., no reference to questionnaires being validated), how the messages were conveyed (including a lack of clarity in how this was performed), which recommendations for lifestyle change were provided (i.e., recommendations from national/international guidelines), and by whom (i.e., clinician, counselor, researcher, etc.). Some observational studies reported physicians had delivered the results to participants, although in most of the observational studies, this was not specified. Only one RCT clearly stated that a physician provided the participants with their results; in all others, this information was not reported or not specified. Previous studies have shown that interventions are more likely to be unsuccessful if not delivered by a clinician (36). In addition, individuals are unlikely to make changes to their diet and lifestyle if no guidance is provided on how to achieve specific goals to improve risk factors (36).
Overall, behavior change has been shown to be possible but needs to be deliberately included and designed, taking advantage of the “teachable moment” (42). These are brief moments during life when people are more receptive to behavior change messages, and these moments can be used to encourage individuals to change unhealthy behaviors (43). The findings of this study indicate that future well-designed interventions should not only focus on providing recommendations on diet and physical activity change, but equally important, follow up, motivate, and support individuals, to enhance the likelihood of achieving significant beneficial changes.
The use of behavior change techniques (BCTs) appears to positively impact the effectiveness of behavior change interventions. A meta-analysis investigating e-health interventions to increase fruit and vegetable intake observed that interventions using 7–8 BCTs (n = 4) were more successful compared with interventions using six or less BCTs (44). The following 5 BCTs identified as more commonly used in studies appeared to equally positively influence the study interventions (44): i. Provide directions on how to change behavior; ii. Provide feedback on performance; iii. Identification of barriers; iv. Goal Setting and v. Inform on consequences of behaviors (44). This suggests that adding BCT may improve effectiveness of interventions, by providing further support to individuals to achieve and maintain a healthy lifestyle (37).
Evidence shows that presence of CAC, rather than simply having a scan performed, leads to a greater motivation toward improving CVD risk factors (19). Moreover, participants with presence of calcification, and more importantly those with higher risk factors for CVD (14) seem to be more motivated to change their behavior (37), with interventions being more successful (14) among those with higher risk. Conversely, having a normal vascular image (no calcification) has been suggested to discourage behavior change toward risk factors (37), but the evidence for this remains limited. This highlights the importance of clarifying to individuals that changes in diet and physical activity, do not only slow the progression of CVD, but can also prevent the onset of vascular-related conditions, particularly in those with CVD risk factors.
Furthermore, vascular imaging has been shown to improve CVD management without leading to great increase in medical costs to participants (10). The need for larger clinical trials has been suggested to confirm whether these findings can be extended to more diverse populations, as well as to investigate whether provision of vascular imaging and the subsequent improvement in CVD risk factors lead to a lower rate of cardiovascular events (10).
A systematic review and meta-analysis including 21 RCTs published in 2022 (45) reported the potential of provision of medical images to encourage risk-reducing behaviors and reduce risk factors. However, they indicated the need for further satisfactorily powered trials well-controlled for risk of bias (45). The review also suggested that building further evidence for some key behavioral outcomes is warranted, as most trials focused on medication use and adherence, smoking cessation, and increase physical activity (45). A study protocol investigating whether provision of vascular imagining to individuals could significantly lead to beneficial behavior change, including diet and physical activity among other behavior change outcomes has been previously published (46) with the RCT underway. Results of this study may contribute to further understanding and potentially strengthening the current evidence that provision of imagining can encourage health behavior modification.
Overall, the data summarized in this review contributes to the literature on the topic and can serve as a reference for future clinical trials and as a guide for future research. We have identified numerous opportunities to improve interventions aiming to promote changes to diet and physical activity via the provision of vascular imaging.
A limitation was the lack of studies specifically designed to answer the question on whether visualization of non-invasive vascular imaging results could lead to beneficial changes in diet and physical activity, and as such it is difficult to evaluate specific knowledge gaps or beneficial approaches. Most of the existing studies focused on smoking cessation and improving estimated cardiovascular risks, with changes in diet and physical activity being mainly secondary outcomes. In addition, the outcomes of interest were assessed using several different instruments. Noteworthy, physical activity/exercise levels were estimated using different and non-comparable instruments (i.e., questions to estimate physical activity [yes/no questions], and the disparities in reporting the results [i.e., MET min/week, mean ± SE]) made comparison difficult. Furthermore, the terms exercise and physical activity were used interchangeably in many studies (i.e., self-reported physical activity was referred as exercise – structured exercise such as going to the gym). As physical activity and dietary intake data was mostly self-reported, these data should be interpreted with caution.
The results of this scoping review suggest the need for well-structured interventions with the objective of motivating individuals to make positive changes to their diet and physical activity. Although there is consistent evidence that provision of non-invasive vascular imaging results can encourage individuals to make positive behavior changes in relation to medication adherence and other CVD risk factors, evidence for its impact on diet and physical activity remains very weak. However, this is largely due to the lack of studies designed to address this question. Well-designed clinical trials are warranted to further clarify and strengthen the beneficial results mainly seen in observational studies. Future clinical trials should consider a consistent and clear message on how to achieve positive diet, physical activity and other lifestyle changes, preferably be delivered by a trained counselor, and include a follow up session to reinforce advice, ensure understanding, and to provide further encouragement to support positive diet and physical activity changes.
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author/s.
SR-B searched the literature and retrieved the articles. SR-B and AKG screened the papers for eligibility. SR-B, MAK, and JRL participated in the writing of the manuscript. SR-B, AKG, MAK, MS, LCB, CPB, BJ, JD, MPS, JMH, and JRL contributed to the work's conception and design, data interpretation, critical revision of the manuscript, and approved the version of the manuscript being submitted. All authors contributed to the article and approved the submitted version.
This study received no specific grant from any funding agency in the public, commercial or not-for-profit sectors. The salary of MS was supported by a Royal Perth Hospital Research Foundation Career Advancement Fellowship (ID: CAF 130/2020) and an Emerging Leader Fellowship from the Western Australian Future Health Research and Innovation Fund. The salary of LCB was supported by a National Health and Medical Research Council (NHMRC) of Australia Emerging Leadership Investigator Grant (ID: 1172987) and a National Heart Foundation of Australia Post-Doctoral Research Fellowship (ID: 102498). The salary of CPB was supported by a Royal Perth Hospital Research Foundation Lawrie Beilin Career Advancement Fellowship (ID: CAF 127/2020). The salary of JMH was supported by a National Health and Medical Research Council of Australia Senior Research Fellowship (ID: 1116973). The salary of JRL was supported by a National Heart Foundation of Australia Future Leader Fellowship (ID: 102817). None of the funding agencies had any role in the conduct and management of the study, data interpretation, preparation, review, or approval of the manuscript.
The authors would like to thank Pamela Thornton, former ECU librarian, who helped identifying the specific search terms, provided important information on how to perform a comprehensive online literature search of scientific papers, and suggested relevant search databases, to prevent missing out on any relevant articles.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fnut.2022.946378/full#supplementary-material
1. WHO. Cardiovascular diseases (CVDs). World Health Organization (2021). Available online at: https://www.who.int/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds) (accessed October 6, 2022).
2. McClellan M, Brown N, Califf RM, Warner JJ. Call to action: urgent challenges in cardiovascular disease: a presidential advisory from the American heart association. Circulation. (2019) 139:e44–54. doi: 10.1161/CIR.0000000000000652
3. Levine DA, Davydow DS, Hough CL, Langa KM, Rogers MA, Iwashyna TJ. Functional disability and cognitive impairment after hospitalization for myocardial infarction and stroke. Circ Cardiovascu Qual Outcom. (2014) 7:863–71. doi: 10.1161/HCQ.0000000000000008
4. Ezzati M, Riboli E. Behavioral and dietary risk factors for noncommunicable diseases. N Eng J Med. (2013) 369:954–64. doi: 10.1056/NEJMra1203528
5. Artinian NT, Fletcher GF, Mozaffarian D, Kris-Etherton P, Van Horn L, Lichtenstein AH, et al. Interventions to promote physical activity and dietary lifestyle changes for cardiovascular risk factor reduction in adults. A scientific statement from the American heart association. Circulation. (2010) 122:406–41. doi: 10.1161/CIR.0b013e3181e8edf1
6. Wang X, Ouyang Y, Liu J, Zhu M, Zhao G, Bao W, et al. Fruit and vegetable consumption and mortality from all causes, cardiovascular disease, and cancer: systematic review and dose-response meta-analysis of prospective cohort studies. Bmj. (2014) 349:g4490. doi: 10.1136/bmj.g4490
7. Lee-Kwan SH, Moore LV, Blanck HM, Harris DM, Galuska D. Disparities in state-specific adult fruit and vegetable consumption—United States, 2015. MMWR Morbid Mortal Week Rep. (2017) 66:1241. doi: 10.15585/mmwr.mm6645a1
8. ABS. Australian Health Survey: Consumption of food groups from the Australian Dietary Guidelines, Australia 2011–12. Australian Bureau of Statistics (2016).
9. ABS. Physical activity: Contains Key Statistics And Information About Exercise and Physical Activity Trends Within Australia, Including State and Territory Specific Findings. Australian Bureau of Statistics (2018).
10. Rozanski A, Gransar H, Shaw LJ, Kim J, Miranda-Peats L, Wong ND, et al. Impact of coronary artery calcium scanning on coronary risk factors and downstream testing the EISNER (early identification of subclinical atherosclerosis by noninvasive imaging research) prospective randomized trial. J Am Coll Cardiol. (2011) 57:1622–32. doi: 10.1016/j.jacc.2011.01.019
11. Mamudu HM, Paul TK, Veeranki SP, Budoff M. The effects of coronary artery calcium screening on behavioral modification, risk perception, and medication adherence among asymptomatic adults: a systematic review. Atherosclerosis. (2014) 236:338–50. doi: 10.1016/j.atherosclerosis.2014.07.022
12. Bengtsson A, Norberg M, Ng N, Carlberg B, Grönlund C, Hultdin J, et al. The beneficial effect over 3 years by pictorial information to patients and their physician about subclinical atherosclerosis and cardiovascular risk: Results from the VIPVIZA randomized clinical trial. Am J Prevent Cardiol. (2021) 7:100199. doi: 10.1016/j.ajpc.2021.100199
13. Glanz K, Rimer BK. Theory at a glance: A guide for health promotion practice. National Cancer Institute, NIH. Public Health Service. Washington, DC: US Government Printing Office (2005).
14. Greenland P. Improving risk of coronary heart disease: can a picture make the difference? Jama. (2003) 289:2270–2. doi: 10.1001/jama.289.17.2270
15. Rodondi N, Auer R, de Bosset Sulzer V, Ghali WA, Cornuz J. Atherosclerosis screening by noninvasive imaging for cardiovascular prevention: a systematic review. J Gen Intern Med. (2012) 27:220–31. doi: 10.1007/s11606-011-1833-3
16. Joshi PH, Patel B, Blaha MJ, Berry JD, Blankstein R, Budoff MJ, et al. Coronary artery calcium predicts cardiovascular events in participants with a low lifetime risk of cardiovascular disease: the Multi-Ethnic Study of Atherosclerosis (MESA). Atherosclerosis. (2016) 246:367–73. doi: 10.1016/j.atherosclerosis.2016.01.017
17. Finn AV, Kolodgie FD, Virmani R. Correlation between carotid intimal/medial thickness and atherosclerosis: a point of view from pathology. Arterioscler Thromb Vasc Biol. (2010) 30:177–81. doi: 10.1161/ATVBAHA.108.173609
18. Yeboah J, McClelland RL, Polonsky TS, Burke GL, Sibley CT, O'Leary D, et al. Comparison of novel risk markers for improvement in cardiovascular risk assessment in intermediate-risk individuals. Jama. (2012) 308:788–95. doi: 10.1001/jama.2012.9624
19. Gupta A, Lau E, Varshney R, Hulten EA, Cheezum M, Bittencourt MS, et al. The identification of calcified coronary plaque is associated with initiation and continuation of pharmacological and lifestyle preventive therapies: a systematic review and meta-analysis. JACC: Cardiovasc Imag. (2017) 10:833–42. doi: 10.1016/j.jcmg.2017.01.030
20. Arksey H, O'Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. (2005) 8:19–32. doi: 10.1080/1364557032000119616
21. Tricco AC, Lillie E, Zarin W, O'Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. (2018) 169:467–73. doi: 10.7326/M18-0850
22. Wong ND, Detrano RC, Diamond G, Rezayat C, Mahmoudi R, Chong EC, et al. Does coronary artery screening by electron beam computed tomography motivate potentially beneficial lifestyle behaviors? Am J Cardiol. (1996) 78:1220–3. doi: 10.1016/S0002-9149(96)00599-1
23. Kalia NK, Miller LG, Nasir K, Blumenthal RS, Agrawal N, Budoff MJ. Visualizing coronary calcium is associated with improvements in adherence to statin therapy. Atherosclerosis. (2006) 185:394–9. doi: 10.1016/j.atherosclerosis.2005.06.018
24. Sandwell JC, Wingard DL, Laughlin GA, Barrett-Connor E. Electron beam computed tomography screening and heart disease risk factor modification. Prev Cardiol. (2006) 9:133–7. doi: 10.1111/j.1520-037X.2006.04862.x
25. Orakzai RH, Nasir K, Orakzai SH, Kalia N, Gopal A, Musunuru K, et al. Effect of patient visualization of coronary calcium by electron beam computed tomography on changes in beneficial lifestyle behaviors. Am J Cardiol. (2008) 101:999–1002. doi: 10.1016/j.amjcard.2007.11.059
26. Schwartz J, Allison M, Wright CM. Health behavior modification after electron beam computed tomography and physician consultation. J Behav Med. (2011) 34:148–55. doi: 10.1007/s10865-010-9294-4
27. Johnson JE, Gulanick M, Penckofer S, Kouba J. Does knowledge of coronary artery calcium affect cardiovascular risk perception, likelihood of taking action, and health-promoting behavior change? J Cardiovasc Nursi. (2015) 30:15–25. doi: 10.1097/JCN.0000000000000103
28. Kalia NK, Cespedes L, Youssef G, Li D, Budoff MJ. Motivational effects of coronary artery calcium scores on statin adherence and weight loss. Coron Artery Dis. (2015) 26:225–30. doi: 10.1097/MCA.0000000000000207
29. Schurink M, Braber T, Prakken N, Doevendans P, Backx F, Grobbee D, et al. No psychological distress in sportsmen aged 45 years and older after cardiovascular screening, including cardiac CT: the Measuring Athlete's Risk of Cardiovascular events (MARC) study. Netherlands Heart Journal. (2017) 25:271–7. doi: 10.1007/s12471-017-0948-5
30. Rodondi N, Auer R, Devine PJ, O'Malley PG, Hayoz D, Cornuz J. The impact of carotid plaque screening on motivation for smoking cessation. Nicotine and tobacco research. J Soc Res Nicotine Tobacco. (2008) 10:541–6. doi: 10.1080/14622200801902011
31. Johnson HM, Einerson J, Korcarz CE, Aeschlimann SE, Stein JH. Long-term effects of carotid screening on patient outcomes and behaviors. Arch Intern Med. (2011) 171:589–91. doi: 10.1001/archinternmed.2011.90
32. Johnson HM, Turke TL, Grossklaus M, Dall T, Carimi S, Koenig LM, et al. Effects of an office-based carotid ultrasound screening intervention. J Am Soc Echocardio. (2011) 24:738–47. doi: 10.1016/j.echo.2011.02.013
33. Hong S-J, Chang H-J, Song K, Hong G-R, Park SW, Kang H-J, et al. Impact of atherosclerosis detection by carotid ultrasound on physician behavior and risk-factor management in asymptomatic hypertensive subjects. Clin Cardiol. (2014) 37:91–6. doi: 10.1002/clc.22220
34. Jeong I-K, Kim S-G, Cho DH, Kim CH, Kim CS, Lee W-Y, et al. Impact of carotid atherosclerosis detection on physician and patient behavior in the management of type 2 diabetes mellitus: a prospective, observational, multicenter study. BMC Cardiovasc Disord. (2016) 16:220. doi: 10.1186/s12872-016-0401-5
35. Braber TL, Mosterd A, Prakken NH, Rienks R, Nathoe HM, Mali WP, et al. Occult coronary artery disease in middle-aged sportsmen with a low cardiovascular risk score: the measuring athlete's risk of cardiovascular events (MARC) study. Eur J Prev Cardiol. (2016) 23:1677–84. doi: 10.1177/2047487316651825
36. O'Malley PG, Feuerstein IM, Taylor AJ. Impact of electron beam tomography, with or without case management, on motivation, behavioral change, and cardiovascular risk profile: a randomized controlled trial. JAMA. (2003) 289:2215–23. doi: 10.1001/jama.289.17.2215
37. Lederman J, Ballard J, Njike VY, Margolies L, Katz DL. Information given to postmenopausal women on coronary computed tomography may influence cardiac risk reduction efforts. J Clin Epidemiol. (2007) 60:389–96. doi: 10.1016/j.jclinepi.2006.07.010
38. Venkataraman P, Huynh Q, Marwick TH, Investigators C-C. Improving cardiovascular prevention through visualisation of CAC: insights from the CAUGHT-CAD trial. J Am Coll Cardiol. (2020) 75:2064. doi: 10.1016/S0735-1097(20)32691-7
39. Rodondi N, Collet T-H, Nanchen D, Locatelli I, Depairon M, Aujesky D, et al. Impact of carotid plaque screening on smoking cessation and other cardiovascular risk factors: a randomized controlled trial. Arch Intern Med. (2012) 172:344–52. doi: 10.1001/archinternmed.2011.1326
40. Näslund U, Ng N, Lundgren A, Fhärm E, Grönlund C, Johansson H, et al. Visualization of asymptomatic atherosclerotic disease for optimum cardiovascular prevention (VIPVIZA): a pragmatic, open-label, randomised controlled trial. Lancet. (2019) 393:133–42. doi: 10.1016/S0140-6736(18)32818-6
41. Michie S, Abraham C, Whittington C, McAteer J, Gupta S. Effective techniques in healthy eating and physical activity interventions: a meta-regression. Health psychology. (2009) 28:690. doi: 10.1037/a0016136
42. Lawson PJ, Flocke SA. Teachable moments for health behavior change: a concept analysis. Patient Educ Couns. (2009) 76:25–30. doi: 10.1016/j.pec.2008.11.002
43. Flocke SA, Clark E, Antognoli E, Mason MJ, Lawson PJ, Smith S, et al. Teachable moments for health behavior change and intermediate patient outcomes. Patient Educ Couns. (2014) 96:43–9. doi: 10.1016/j.pec.2014.03.014
44. Rodriguez Rocha NP, Kim H. eHealth interventions for fruit and vegetable intake: a meta-analysis of effectiveness. Health Edu Behav. (2019) 46:947–59. doi: 10.1177/1090198119859396
45. Hollands GJ, Usher-Smith JA, Hasan R, Alexander F, Clarke N, Griffin SJ. Visualising health risks with medical imaging for changing recipients' health behaviours and risk factors: Systematic review with meta-analysis. PLoS Med. (2022) 19:e1003920. doi: 10.1371/journal.pmed.1003920
Keywords: coronary artery calcification (CAC), carotid ultrasound (CUS), vascular imagining, cardiovascular disease (CVD), diet and physical activity change
Citation: Radavelli-Bagatini S, Gebre AK, Kennedy MA, Sim M, Blekkenhorst LC, Bondonno CP, Jackson B, Dimmock J, Schlaich MP, Hodgson JM and Lewis JR (2022) Provision of non-invasive coronary and carotid vascular imaging results on changes in diet and physical activity in asymptomatic adults: A scoping review. Front. Nutr. 9:946378. doi: 10.3389/fnut.2022.946378
Received: 17 May 2022; Accepted: 29 September 2022;
Published: 28 October 2022.
Edited by:
Hongtao Tie, The First Affiliated Hospital of Chongqing Medical University, ChinaReviewed by:
Jean-Claude Desfontis, Ecole Nationale Vétérinaire Agroalimentaire et de l'Alimentation, FranceCopyright © 2022 Radavelli-Bagatini, Gebre, Kennedy, Sim, Blekkenhorst, Bondonno, Jackson, Dimmock, Schlaich, Hodgson and Lewis. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Simone Radavelli-Bagatini, cy5yYWRhdmVsbGliYWdhdGluaUBlY3UuZWR1LmF1
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.