
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Nutr., 08 July 2022
Sec. Nutrition and Metabolism
Volume 9 - 2022 | https://doi.org/10.3389/fnut.2022.900422
This article is part of the Research TopicWomen in Nutrition and MetabolismView all 6 articles
 Rouzha Pancheva1*
Rouzha Pancheva1* Lyubomir Dimitrov2
Lyubomir Dimitrov2 Michal Gillon-Keren3
Michal Gillon-Keren3 Kaloyan Tsochev4
Kaloyan Tsochev4 Tatyana Chalakova5
Tatyana Chalakova5 Natalya Usheva6
Natalya Usheva6 Silviya Nikolova6
Silviya Nikolova6 Yoto Yotov5
Yoto Yotov5 Violeta Iotova4
Violeta Iotova4Introduction: Nutrition education attempts to maintain and enhance good eating habits to achieve optimal metabolic control in people with type 1 diabetes (T1D). Recommendations for patients with T1D are comparable to those of the general population.
This Study Aimed: To investigate dietary habits and adherence to nutritional recommendations of patients with T1D as compared with age, gender, and BMI matched people in Bulgaria.
Methods: A case-control study included 124 patients with T1D with long disease duration (mean duration 25.3 ± 8.2 years) followed up at a diabetes clinic in Varna, Bulgaria for 2 years (2017–2019) and 59 controls matched for gender, age and BMI. A 24-h dietary recall method was used to assess the nutrition of both groups. A standardized questionnaire was applied to assess the frequency of food consumption (Feel4Diabtes). Height and weight were standardly measured, and BMI was calculated. Findings were compared with Bulgarian recommendations and reference values for energy and nutrient intake for healthy adults. The data were analyzed with the statistical package SPSSv21.0 and Jamovi v.22.5.
Results: The nutritional characteristics of T1D men and women differ. Men with T1D had a higher intake of total carbohydrates (CHO) (p = 0.009), a lower intake of total fats (p = 0.007), and monounsaturated fatty acids (p = 0.029) as a percentage of total daily energy compared with the controls. Women with T1D had a different distribution of energy intake per meal compared to controls: they consumed more energy (p = 0.001) and a corresponding share of CHO for lunch, less for dinner (p = 0.015) and had a higher overall healthy diet score when compared to controls (p = 0.02). Adherence to dietary recommendations (e.g., CHO, total fats, saturated fat, fibers) was low in both genders, but lower in the general population compared to people with T1D.
Conclusion: Our data demonstrate that people with T1D consume a healthier diet than the general population, which could be attributed to healthier diet awareness, still far from the recommendations. Introduction of annual consultations with a dietitian may improve long-term outcomes.
Nutrition is fundamental in the management of type 1 diabetes (T1D). Dietary counseling and guidance are integral parts of the treatment and self-management of diabetes aiming to maintain or improve nutritional and physiological health and to achieve optimal metabolic control (1, 2). Nutrition helps to prevent acute and long-term complications of diabetes and associated comorbid conditions (3, 4).
According to the International Society for Pediatric and Adolescent Diabetes (ISPAD) clinical consensus guidelines, dietary recommendations are based on healthy eating principles suitable for all children and families (5). Avoiding low-carbohydrate diet and taking 45–55 percent of total energy in the form of carbohydrates, 15–20 percent of total energy in the form of protein (more precisely 0.8–0.9 g/kg in those above 10 years), and 30–35 percent of total energy in the form of fat are some of these recommendations. ISPAD and the American Diabetes Association (ADA) are both referring to the 2015–2020 Dietary Guidelines for Americans (6) that advocate limiting of saturated fat to <10% of the total energy intake in patients with diabetes. Furthermore, the American Heart Association (AHA) (7) and the American Association of Clinical Endocrinologists (AACE) (8) both recommend limiting saturated fat to <7% of the total calories, trans-fats <1% and cholesterol <200 mg/day. Protein intake should be reduced to 0.8 g/kg in people with renal disease to avoid nephropathy deterioration (9, 10). Because establishing good glycaemic control (HbA1c 7%) is a key ADA (11) objective for patients with type 1 diabetes, balancing adequate carbohydrate intake with avoiding postprandial hyperglycemia is critical. It can potentially be handled by carbohydrate counting and insulin adjustment, as well as avoiding high fat and/or high protein meals, which may contribute to delayed hyperglycemia and the need for additional insulin dose adjustments (11).
There are no specific recommendations for patients with T1D who have a longstanding disease, and may have a double burden of disease due to the basic chronic condition and to the non-communicable disease risk that rises with age (12). Nutrition advise should be individualized, regularly evaluated, and reinforced in an intensive manner (13), and should incorporate self-management education (14). A nutritionist or dietitian should be part of the diabetes multidisciplinary team and involved in the delivery of care wherever possible (4). Many factors influence nutritional choices, which might alter over time. As a result, it is critical to gather data on the nutritional intake at regular intervals and to adapt education policies to the current demands and specific guidance for type 1 diabetes patients.
In Bulgaria, patients with diabetes are not offered a regular consultation with a dietitian. Dietary counseling is done by endocrinologists and trained endocrinology nurses. It is focused mainly on improving glycaemic control through carbohydrate matching with insulin and, to a limited degree, on healthy eating habits. It is unknown how this approach to diabetes care reflects dietary compliance with the national nutritional recommendations in Bulgaria (15).
Studies have investigated dietary intake and adherence to the recommendations in patients with T1D (16), generally reporting poor adherence for most macronutrients. For patients with longstanding T1D in Bulgaria, comparative studies with the general population have not previously been reported to the best of our knowledge. The current study aimed to investigate dietary habits and adherence to nutritional recommendations of patients with T1D as compared with age, gender, and BMI matched people in Bulgaria.
A case-control study was conducted over a period of 2 years (2017–2019). A sample of 124 adults (>18 years of age) with T1D with a long disease duration who were followed in the Diabetes clinic in St. Marina University hospital-Varna, Bulgaria, and 59 control subjects matched for gender, age, and body mass index (BMI) were recruited.
Inclusion criteria for patients and controls were: Patients with T1D for more than 15 years; healthy volunteers of the same gender, age, and BMI. The existence of any of the following conditions constitutes an exclusion criteria: participation in a clinical trial; significant mental impairment or other type of impediment to making an informed decision about participation; significant disability and/or immobilization; more than 3% change in body weight in the last 3 months; acute illness or condition during the study; pregnancy in women of childbearing age (in case of a delay in the regular menstrual cycle-exclusion via a pregnancy test); severe hypoglycemia or diabetes ketoacidosis in the preceding 3 months in patients with diabetes; severe confirmed microvascular diabetes complications.
Participants were interviewed using a structured questionnaire that included questions about their demographic characteristics (gender, age, and ethnicity) and socio-economic status (highest achieved educational degree, marital status, occupation, and current income). Diabetes-specific data regarding the age at diabetes onset, diabetes duration, treatment plan, control, and insulin therapy regimen was analyzed. Information on each participant's negative lifestyle behaviors, such as tobacco smoking and alcohol consumption, was collected.
A thorough clinical examination was performed together with anthropometric measurements of weight (kg), height (cm), waist circumference (cm), and the calculation of a body mass index (BMI) (kg/m2) and waist-to-height ratio for each participant.
Accelerometers used for 3 days were utilized to objectively evaluate physical activity level (PAL). A GCDC USB accelerometer (supported by Copyright 2011 Hookie Technologies Ltd) was used for objective measure of step counts, total amount, frequency, intensity and duration of physical activity, sedentary behavior in free living conditions for a period of 4 days.
Accelerometer was positioned on the waist and was warn full day except in case of bath or swimming. The data was uploaded and processed by online software Hookie Research Database version 1.10. The data was categorized into three physical activity level groups: based on Food and Agriculture Organization (FAO) classification of lifestyles in relation to the intensity of habitual physical activity (17). Energy intake adequateness was recalculated accordingly.
Measurement of glycated hemoglobin (HbA1c) in percent was performed after at least 12 h of fasting prior to venous blood collection. The levels of HbA1c were tested according to standardized methods in the Central Clinical Laboratory of the University Hospital “St. Marina”, Varna.
Data on food intake included the completion of a diet food frequency semi quantitative questionnaire—Feel4Diabetes (FFQ), and a 24-h dietary recall (24 HR).
The FFQ that we use was developed and validated with the main goal of capturing habitual dietary intake (18). The tool was applied to simplify and rate food selections, which aided in the statistical analysis. Twelve Feel4Diabetes intervention goals relating to food choices or behavior were chosen as the primary components of a Healthy diet score. Breakfast, vegetables, fruit, and berries, sugary beverages, whole-grain cereals, nuts and seeds, low-fat dairy goods, oils and fats, red meat, sweet snacks, salty snacks, and family meals were all included in these subcategories. The components were rated using the fourteen diet-related items presented in the Feel4Diabetes survey. Each component consisted of one or two questions pertaining to the frequency of intake of certain food categories or activities. These questions were used to calculate the Healthy diet score; the maximum score for each component was set based on its perceived relative importance, with a higher score indicating a better quality of diet. The overall score, which was calculated as the sum of the component scores, varied from 0 to 100, with a higher score indicating a diet of greater quality and a maximum score indicating full compliance with the Feel4Diabetes dietary objectives. This specific instrument was selected for a variety of reasons: It is composed of scored items based on food rather than nutrient intake, demonstrating dietary patterns; it is sensitive to all healthy and beneficial trends in diet; it is composed of all the relevant information available in a validated in Bulgaria questionnaire; and the Feel4Diabetes Healthy Diet Score category is significantly correlated with clinical risk factors—the blood lipoprotein profile.
The 24HR was given by a trained enumerator who gathered thorough, quantitative data on individual participants' diets by enquiring about the kind and amount of every meal and beverage consumed in the previous 24 h. The responder provided additional culinary information about each meal or beverage, such as the cooking technique and other features, as well as an estimate of the portion size ingested. The food data was matched with nutrient information from a food composition database to determine the nutrient content. The average intakes of macronutrients and micronutrients were determined. The results were compared with Bulgarian recommendations and reference values for energy and nutrient intake for healthy adults (15). According to the PAL and the corresponding reference for energy intake, participants were classified into low, adequate and high Energy intake category.
Descriptive statistics were reported as percentages for categorical data, mean ± standard deviation (SD) for normally distributed continuous data, and median (IQR) for non-normally distributed data. The paired comparisons between the case and control groups were done with Independent samples t-test for normally distributed variables and Mann-Whitney U-test for non-normally distributed variables. Additionally, Chi-square test was used to test for significant associations between patients and controls regarding different categorical and ordinal variables. Statistical data processing was performed using the IBM SPSS v.23 statistical package and Jamovi v.22.5. P-value ≤ 0.05 was considered statistically significant.
A total of 183 participants – 124 with T1D, mean duration of 25.3 years without known cardiovascular diseases (67.8%) and 59 healthy controls (32.2%) were recruited for the study (Table 1). The mean age of all participants was 43.5 ± 10.1 (range 19–67 years). Both genders were equally distributed—a total of 54.1% men with no significant difference between the groups. Controls were predominantly people with higher education compared to T1D (71 vs. 50% respectively; p = 0.16). The majority of T1D (72.6%) and controls (81.4%) were married or living in partnership, and most self-identified as Bulgarians.
Table 1 provides an overview of all additional demographic, anthropometric and lifestyle characteristics of both study populations. The T1DM and control group differed significantly only regarding PAL, weight (but not BMI) and, understandably, HbA1c.
Mean HbA1c in T1D patients was 8.4 ± 1.8% (68.5 ± 8.8 mmol/mol), 95% CI 8.11–8.73% (65.1–71.9 mmol/mol). With excellent control of diabetes (HbA1c <6%) were only 6 (4.8%), with good control (HbA1c <7%) were 14 (11.3%) of the T1D patients. There were no gender differencies in both patients and controls (Figure 1; Supplementary Figure 1). Of all patients with diabetes, 123/124 used bolus insulin and almost all −121/124 used also a basal type of insulin. The mean total insulin dose was 51.06 ± 17.33 IU, 95% CI 47.96–54.15 IU.
The median daily energy intake was lower in female and identical for male T1D patients as compared to controls, but with no statistical significance was found (Table 2). The proportion of patients with T1D achieving adequate Energy intake category was 25.2 and 23.7%, respectively (data not shown), but a high proportion of both patients and controls with a high BMI (>25 kg/m2) reported low Energy category – 54.8 vs. 66.7%, respectively (p = 0.70).
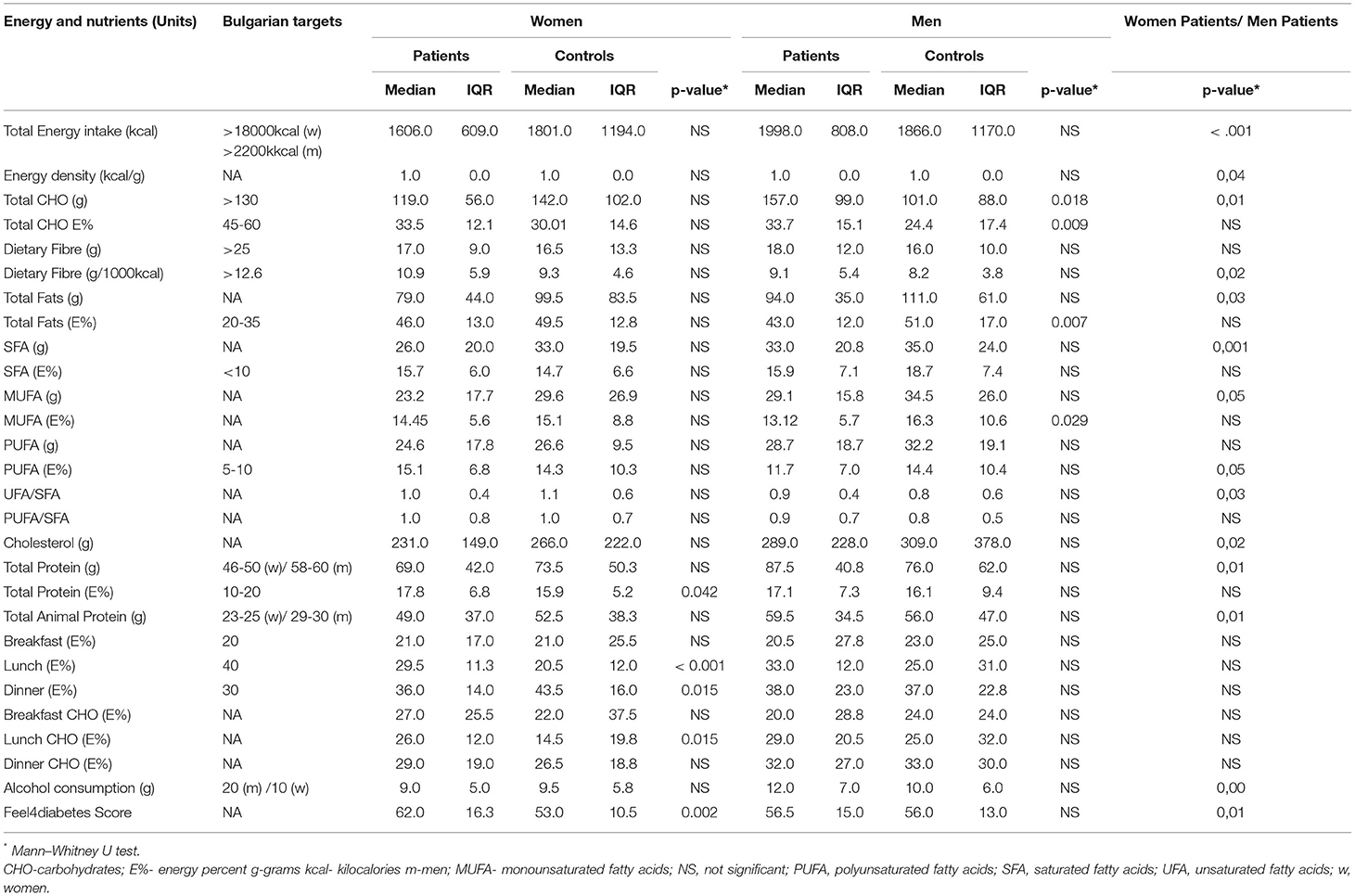
Table 2. Intake of energy and nutrients per day in T1D patients with long disease duration compared to healthy age and gender matched controls.
The median intake of carbohydrates was lower than the range of 45–60 E%, and closest to the adequate in male patients (33.7 E%; 157.5 g>130 g). Although higher for T1D, the median for dietary fiber did not reach the recommended intake of 25 g/day, and was lowest again in male controls (16 g/day). Adjusted for total energy, fibers intake was highest in female T1D patients compared to controls (~11 g/1,000 kcal). All groups had adequate to the recommended intake of proteins (~17 E% in patients with diabetes vs. ~16 E% in the control group), while the absolute amount of protein (in g) was higher than the recommendation, and the type of protein was mainly animal protein (>50% of total protein). All groups ingested higher than the reference level of total fat (>20–35 E%) and saturated fatty acids (SFA) >10 E%, the highest values reported by male controls—total fat 51 E% and SFA 18.7 E% (p = 0.007). Compared with the Bulgarian recommendation for polyunsaturated fatty acids (PUFA) intake of 5–10 E%, the adherence of all groups was acceptable, but lowest for male controls.
Both genders of T1D patients had higher adherence to Energy intake distribution per meal with closer to the recommended amount for Lunch (recommended ~40 E%) and Dinner (recommended ~30 E%) with the least fluctuations of carbohydrates (CHO) E% consumption in women patients. The median alcohol intake for the participants was within the recommendations in male T1D participants demonstrating a 17% lower intake as compared to controls (10 vs. 12 g).
In a subgroup comparison of female and male patients, it was determined that women had significantly superior eating habits, particularly with the consumption of saturated (26 vs. 33 g, p = 0.001), unsaturated fats, fiber, and animal protein, as well as alcohol consumption (Table 2).
Applying the Feel4diabetes scoring system, most of the food groups scored higher in patients (Figure 2), except for snacks and fats. Statistical significance was reached only for the regular presence of breakfasts—on week days (median 7 vs. 4 points, p = 0.001) and weekends (median 3 vs. 2 points, p = 0.002), T1D subjects vs. controls. The clear trend for female patients to have a higher FFQ than male patients was once again evident (62.0 vs. 56.5, p = 0.01).
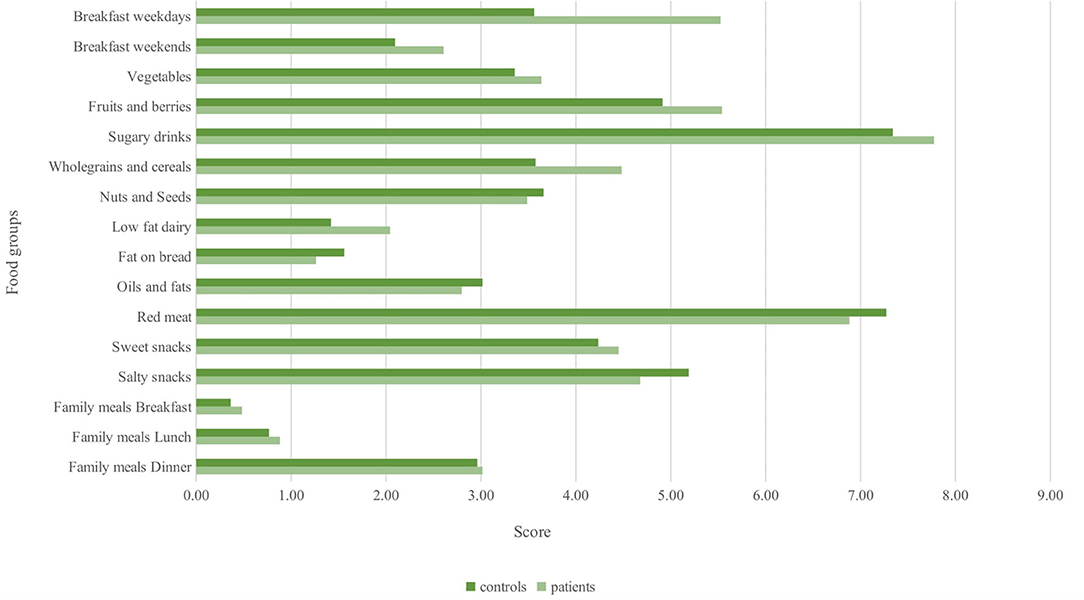
Figure 2. Comparison between T1D patients and controls of items included in Feel4Diabetes healthy score.
The current study revealed that both T1D patients and controls are not following the Bulgarian dietary guidelines (15) for energy and macronutrient consumption. Nevertheless, patients had some beneficial trends when compared to controls. Total fats, particularly SFA and cholesterol, were high in T1D patients but even higher in controls, with only total fats in men- T1D vs. controls, reaching significance. These findings demonstrate an even worse trend than that observed in the 2014 Bulgarian representative survey (19). Similar findings were observed in previous studies on the diets of patients with T1D since adolescence, where total fat and saturated fat intake surpassed recommendations, even when energy intake was low (2, 20–22). Historically, dietary approaches have focused on lowering saturated fatty acids (SFA) and dietary cholesterol. Diets that have <7% SFA and <200 g of dietary cholesterol a day have been shown to improve lipids and other cardiovascular disease (CVD) risk factors when compared to diets with more SFA and less cholesterol. In recent years, however several studies have revealed that for CVD risk reduction, the quality of fat (the kind of fatty acids) is more important than the quantity of fat.
Interestingly, CHO consumption was low in all participants, both as a percentage of daily energy and as an absolute intake in grams, and reached a significant difference in men with T1D compared to controls. Previous research also discovered a lack of compliance with the dietary advice for CHO (2, 16, 20) with a tendency to consume less CHO. While dietary recommendations are evidence-based and the existing data does not support a low-CHO diet, female patients and male controls tended to have a low-CHO diet, less than the recommended minimum of 130 g/day. Contrary to the popular belief, a low-carbohydrate diet can interact with the hyperglycaemic consequences of fat and protein consumption (23). There is evidence that such diets may potentially be harmful to the patient's health. They can cause acute hypo- or hyperglycemia, worsen the predictability of the diet on glycemia, increase the likelihood of ketosis, and deplete systemic glycogen reserves. Although the long-term effects of a low-carbohydrate diet are unknown, potential concerns include changes in lipid profiles, nutritional deficiency, CVD problems, and nephrolithiasis (23).
On the other hand, fiber intake is also lower than recommended in our study (4). Neither patients nor controls met the Bulgarian requirement of 25 g fiber per day as well as fiber density (12.6 g of fiber per 1,000 kcal), which is consistent with previous observational research (22, 24). Perhaps the recommended dietary fiber consumption is impossible for the majority of people, given the country's traditional diet, which continues to vary seasonally and the availability of fiber-rich foods during the winter, as well as the diet's westernization during the last 30 years. There is widespread agreement among nutritional societies that increasing fiber intake, particularly from whole grain cereals, is associated with a reduction in CVD-specific and all-cause mortality in T1D patients and also improves glycemic control, with a significant reduction in HbA1c following fiber intake increases (4). Long-term compliance with such high fiber intakes, on the other hand, may be difficult in daily practice (21).
The participants' median protein intake stayed within the recommended range as a percentage of energy, but was significantly higher as an absolute intake in grams. Proteins have been shown to defend against the onset of hypoglycemia (5). Although the participants stayed within the recommended protein consumption range (10–20% E) for people with diabetes who do not have abnormal albuminuria, there was a definite tendency toward increased animal protein and decreased plant protein, respectively. This could have been driven in part by patients' focus on insulin-CHO ratio and desire to reduce CHO, which resulted in an increase in animal protein intake together with total and saturated fat in their diets, as these dietary components are abundant and co-present in animal foods. The current findings corroborate those of several earlier observational studies (25, 26). The within-recommended intake of protein is important, as increased protein consumption impairs the synthesis of anti-insulin hormones such as glucagon, resulting in a postprandial rise in blood glucose levels, as well as cortisol secretion, resulting in insulin resistance and elevated postprandial blood glucose levels (27).
Our findings indicated that dinner was the principal meal of the day in the Bulgarian population- the E percent from dinner meals was higher than recommended in both patients and controls, implying that supper is the primary meal of the day. This may pose a difficulty for insulin dose calculation since dinner has the worst postprandial control of all meals (28), with a glucose response lasting up to 6 h after the meal. This is of particular concern because, together with its characteristics as a protein- and fat-dense meal, it may result in an even higher increase in postprandial glucose concentrations and for long hours during the night. Thus, we can hypothesize that late postprandial glucose increases are more pronounced.
With regards to healthy eating habits according to the Feel4Diabetes score (18) we observed a significant difference in overall score between men and women with T1D, indicating a greater awareness in female patients of the importance of the frequency of consumption of various food groups. However, upon closer examination of the individual items, the difference was primarily for breakfast frequency. Breakfast inclusion and the suggestion of at least three meals per day are two of the recommendations for healthy eating in Bulgaria.
Although the Feel4Diabetes score was designed largely for the purpose to prevent type 2 diabetes, it represents both favorable (higher score) and unfavorable nutritional (lower score) trends, which are critical in the management of T1D as well. The Healthy Diet Score was found to be strongly, if moderately, linked with clinical risk variables such as HDL- and LDL-cholesterol and triglycerides, all of which are critical for long-term T1D treatment. In our study, we observed a significant difference in overall score between men and women with T1D, indicating a greater awareness in female patients of the importance of the frequency of consumption of various food groups. However, upon closer examination of the individual items, the difference was primarily for breakfast frequency. Breakfast inclusion and the suggestion of at least three meals per day are two of the recommendations for healthy eating in Bulgaria. Comparative studies on meal and snack frequency are nearly non-existent. Nonetheless, a recent study discovered that when single meal occasions were compared to corresponding HbA1c levels, both breakfast and lunch were associated with improved glycemic management (29).
Among the study's strengths is the large sample size for Bulgaria, which allowed for the collection of comprehensive data on energy, nutrient intake assessment, meal/snacking frequency, and associated carbohydrate intake. The meal pattern and energy and nutrient consumption of patients with long-term T1D are of particular interest, as the majority of nutrition research focuses on T2D and, when T1D patients are included, does not differentiate between recently diagnosed and long-term disease duration patients. For the first time, the nutrition of Bulgarian patients was investigated. Another strength was the use of a validated in the country tool to collect dietary data, as well as the assessment of potential discrepancies in eating patterns between patients and control groups, which reflected nutrition in the general community. Additional value was contributed by using two different approaches to assess nutrition: a 24-h recall and a FFQ.
Though we were unable to reassess nutrition using a second 24-h recall, we can presume that all type 1 diabetes patients for whom solely dietary data was available were assessed using an FFQ. The degree of plausibility attained in energy reporting was poor and in a high proportion of patients it did not correspond to BMI, indicating that participants may be underreporting. Nonetheless, the obvious trends outweigh the underreporting. We were unable to recruit a larger number of controls in our study, and the ratio of controls to patients was 1:2, which may have contributed to the uncertainty regarding the nutrition of controls but not so much to the eating habits of T1D patients. Lastly, the cross-sectional nature of the study design limits the generalizability of the study.
In conclusion, our study found that both patients with T1D and controls frequently do not adhere to the country's dietary recommendations. Bulgarian patients with T1D consume significantly less CHO and dietary fiber and have a higher total fat intake, which contributes to possible poor glycemic control and may increase the risk of late metabolic problems. Still, people with T1D consume a healthier diet than the general population, which could be attributed to healthier diet awareness, still far from the recommendations. These findings lend support to the notion that dietitian-assisted dietary counseling may result in an increase in patient adherence to dietary guidelines, as well as improve diabetes control and reduce CVD risk factors and other diabetic complications. Dietary education for people with T1D should place a higher emphasis on efforts to improve the overall quality of the diet and, consequently, on adherence to current dietary recommendations for diabetes management and metabolic control.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
The studies involving human participants were reviewed and approved by Ethical Committee at the Medical University of Varna. The patients/participants provided their written informed consent to participate in this study.
YY and VI conceptualized and supervised the study. TC and KT have been involved in the design of the study. RP conceived the idea. LD selected and retrieved relevant papers. RP, LD, and MG-K drafted this review. NU and SN evaluated the statistical analysis. All authors revised and approved the final manuscript.
This study was supported by a research grant N 17022/2017, from the Fund “Science”, Medical University of Varna.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The authors would like to thank Sergei Glinkov for managing the reference list, Desislava Zhelyazkova and Fatme Ahmed for their invaluable assistance in gathering data on the nutrition of project participants.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fnut.2022.900422/full#supplementary-material
24HR, 24-h dietary recall; AACE, American association of clinical endocrinologists; ADA, American diabetes association; AHA, American heart association; BMI, Body mass index; CHO, carbohydrates; CI, confidence interval; CVD, cardiovascular disease; E%, energy percent; FAO, food and agriculture organization; Feel4Diabtes, feel for diabetes diet score; FFQ, food frequency questionnaire; g, grams; HbA1c, glycated hemoglobin; IQR, interquartile range; ISPAD, international society for pediatric and adolescent diabetes; IU, international units; kcal, kilocalories; MUFA, monounsaturated fatty acids; NS, not significant; PAL, physical activity level; PUFA, polyunsaturated fatty acids; SD, standard deviation; SFA, saturated fatty acids; T1D, type 1 diabetes; UFA, unsaturated fatty acids.
1. Nutrition Therapy for Adults With Diabetes or Prediabetes: A Consensus Report | Diabetes Care | American Diabetes Association. Available online at: https://diabetesjournals.org/care/article/42/5/731/40480/ (accessed March 7, 2022).
2. Ewers B, Trolle E, Jacobsen SS, Vististen D, Almdal TP, Vilsbøll T, et al. Dietary habits and adherence to dietary recommendations in patients with type 1 and type 2 diabetes compared with the general population in Denmark. Nutrition. (2019) 61:49–55. doi: 10.1016/j.nut.2018.10.021
3. American Diabetes Association. 5. Facilitating behavior change well-being to improve health outcomes: standards of medical care in diabetes-−2021. Diabetes Care. (2020) 44(Supple. 1):S53–72. doi: 10.2337/dc21-S005 Available online at: https://diabetesjournals.org/care/article/44/Supplement_1/S53/30778/5-Facilitating-Behavior-Change-and-Well-being-to
4. Sievenpiper JL, Chan CB, Dworatzek PD, Freeze C, Williams SL. Nutrition therapy. Can J Diabetes. (2018) 42:S64–79. doi: 10.1016/j.jcjd.2017.10.009
5. Smart CE, Annan F, Higgins LA, Jelleryd E, Lopez M, Acerini CL. ISPAD clinical practice consensus guidelines 2018: nutritional management in children and adolescents with diabetes. Pediatr Diabetes. (2018) 19:136–54. doi: 10.1111/pedi.12738
6. 2015-2020 Dietary Guidelines for Americans. Available online at: https://health.gov/sites/default/files/2019-09/2015-2020_Dietary_Guidelines.pdf (accessed March 4, 2022).
7. Krauss RM, Eckel RH, Howard B, Appel LJ, Daniels SR, Deckelbaum RJ, et al. AHA dietary guidelines: revision 2000: a statement for healthcare professionals from the nutrition committee of the American heart association. Circulation. (2000) 102:2284–99. doi: 10.1161/01.CIR.102.18.2284
8. Jellinger PS, Handelsman Y, Rosenblit PD, Bloomgarden ZT, Fonseca VA, Garber AJ, et al. American association of clinical endocrinologists and American college of endocrinology guidelines for management of dyslipidemia and prevention of cardiovascular disease. Endocrine Pract. (2017) 23:1–87. doi: 10.4158/EP171764.GL
9. Ko GJ, Obi Y, Tortorici AR, Kalantar-Zadeh K. Dietary protein intake and chronic kidney disease. Curr Opin Clin Nutr Metab Care. (2017) 20:77–85. doi: 10.1097/MCO.0000000000000342
10. Franz MJ, MacLeod J, Evert A, Brown C, Gradwell E, Handu D, et al. Academy of nutrition and dietetics nutrition practice guideline for type 1 and type 2 diabetes in adults: systematic review of evidence for medical nutrition therapy effectiveness and recommendations for integration into the nutrition care process. J Acad Nutr Diet. (2017) 117:1659–79. doi: 10.1016/j.jand.2017.03.022
11. Holt RIG, DeVries JH, Hess-Fischl A, Hirsch IB, Kirkman MS, Klupa T, et al. The management of type 1 diabetes in adults. A consensus report by the american diabetes association (ADA) and the European association for the study of diabetes (EASD). Diabetes Care. (2021) 44:2589–625. doi: 10.2337/dci21-0043
12. Leroux C, Brazeau A-S, Gingras V, Desjardins K, Strychar I, Rabasa-Lhoret R. Lifestyle and cardiometabolic risk in adults with type 1 diabetes: a review. Can J Diabetes. (2014) 38:62–9. doi: 10.1016/j.jcjd.2013.08.268
13. Settineri S, Frisone F, Merlo EM, Geraci D, Martino G. Compliance, adherence, concordance, empowerment, and self-management: five words to manifest a relational maladjustment in diabetes. J Multidiscip Healthc. (2019) 12:299–314. doi: 10.2147/JMDH.S193752
14. Type 1 Diabetes Self-Care Manual | ADA. Available online at: https://www.diabetes.org/diabetes/type-1/type-1-self-care-manual (accessed March 19, 2022).
15. Ministry of Health. Decree No.1 from January 22, 2018 on the nutritional physiological norms of the population. Available online at: https://www.mh.government.bg/media/filer_public/2018/02/13/naredba1-22-01-2018-fiziologicni-normi-hranene-naselenie.pdf (accessed March 27, 2022).
16. Pancheva R, Zhelyazkova D, Ahmed F, Gillon-Keren M, Usheva N, Bocheva Y, et al. Dietary intake and adherence to the recommendations for healthy eating in patients with type 1 diabetes: a narrative review. Front Nutr. (2021) 8:782670. doi: 10.3389/fnut.2021.782670
17. Human Energy Requirements. Available online at: https://www.fao.org/3/y5686e/y5686e07.htm (accessed March 4, 2022).
18. Virtanen E, Kivelä J, Wikström K, Lambrinou C-P, De Miguel-Etayo P, Huys N, et al. Feel4Diabetes healthy diet score: development and evaluation of clinical validity. BMC Endocr Disord. (2020) 20(Suppl. 2):46. doi: 10.1186/s12902-020-0521-x
19. Duleva V, Rangelova L, Petrova St, Dimitrov P, Bozhilova D. Nutrition for people aged over 19 years in Bulgaria, 2014: energy and macronutrients intake. Bulg J Public Health. (2017) 9:34–46.
20. Snell-Bergeon JK, Chartier-Logan C, Maahs DM, Ogden LG, Hokanson JE, Kinney GL, et al. Adults with type 1 diabetes eat a high-fat atherogenic diet that is associated with coronary artery calcium. Diabetologia. (2009) 52:801–9. doi: 10.1007/s00125-009-1280-4
21. Ahola AJ, Mikkilä V, Mäkimattila S, Forsblom C, Freese R, Groop P-H, et al. Energy and nutrient intakes and adherence to dietary guidelines among Finnish adults with type 1 diabetes. Ann Med. (2012) 44:73–81. doi: 10.3109/07853890.2010.530682
22. Jaacks LM, Liu W, Ji L, Mendez MA, Du S, Crandell J, et al. Diabetes nutrition therapy and dietary intake among individuals with type 1 diabetes in China. Diabet Med. (2015) 32:399–406. doi: 10.1111/dme.12634
23. Low-Carbohydrate Diets and Glycaemic Control in Type 1 Diabetes Mellitus - European Medical Journal. Available online at: https://www.emjreviews.com/diabetes/article/low-carbohydrate-diets-and-glycaemic-control-in-type-1-diabetes-mellitus/ (accessed March 27, 2021).
24. Soedamah-Muthu SS, Chaturvedi N, Fuller JH, Toeller M. Do European people with type 1 diabetes consume a high atherogenic diet? 7-year follow-up of the EURODIAB prospective complications study. Eur J Nutr. (2013) 52:1701–10. doi: 10.1007/s00394-012-0473-7
25. Faulkner MS, Chao W-H, Kamath SK, Quinn L, Fritschi C, Maggiore JA, et al. Total homocysteine, diet, and lipid profiles in type 1 and type 2 diabetic and nondiabetic adolescents. J Cardiov Nurs. (2006) 21:47–55. doi: 10.1097/00005082-200601000-00010
26. Lodefalk M, Åman J. Food habits, energy and nutrient intake in adolescents with type 1 diabetes mellitus: original article. Diabetic Med. (2006) 23:1225–32. doi: 10.1111/j.1464-5491.2006.01971.x
27. Abdou M, Hafez MH, Anwar GM, Fahmy WA, Abd Alfattah NM, Salem RI, et al. Effect of high protein and fat diet on postprandial blood glucose levels in children and adolescents with type 1 diabetes in Cairo, Egypt. Diabetes Metab Syndr. (2021) 15:7–12. doi: 10.1016/j.dsx.2020.11.020
28. Vetrani C, Calabrese I, Cavagnuolo L, Pacella D, Napolano E, Di Rienzo S, et al. Dietary determinants of postprandial blood glucose control in adults with type 1 diabetes on a hybrid closed-loop system. Diabetologia. (2022) 65:79–87. doi: 10.1007/s00125-021-05587-0
29. Baechle C, Hoyer A, Castillo-Reinado K, Stahl-Pehe A, Kuss O, Holl R, et al. Eating frequency and carbohydrate intake in adolescents with type 1 diabetes differ from those in their peers and are associated with glycemic control. Exp Clin Endocrinol Diabetes. (2018) 126:277–86. doi: 10.1055/s-0043-115010
Keywords: type 1 diabetes, long duration, nutrition, healthy, dietary habits
Citation: Pancheva R, Dimitrov L, Gillon-Keren M, Tsochev K, Chalakova T, Usheva N, Nikolova S, Yotov Y and Iotova V (2022) Dietary Behavior and Compliance to Bulgarian National Nutrition Guidelines in Patients With Type 1 Diabetes With Longstanding Disease. Front. Nutr. 9:900422. doi: 10.3389/fnut.2022.900422
Received: 20 March 2022; Accepted: 14 June 2022;
Published: 08 July 2022.
Edited by:
Teodora Handjieva-Darlenska, Medical University, BulgariaReviewed by:
Stefan Kabisch, Charité Universitätsmedizin Berlin, GermanyCopyright © 2022 Pancheva, Dimitrov, Gillon-Keren, Tsochev, Chalakova, Usheva, Nikolova, Yotov and Iotova. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Rouzha Pancheva, cm91emhhLnBhbmNoZXZhQGdtYWlsLmNvbQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.