- Food Science and Human Nutrition Department, University of Florida, Gainesville, FL, United States
Vitamin D deficiency is a global issue that may be attributed to various factors such as dietary habits, sun exposure, age, race and chronic conditions. The purpose of this study was to determine the relationship between vitamin D intake from food/supplements and factors that may be associated with self-reported vitamin D deficiency among US adults. A cross-sectional online study was conducted among 1,637 adults using a 38-item questionnaire. Frequency counts and percentages were tabulated and a multiple linear regression was performed. Statistical significance was determined at p < 0.05. Participants (n = 554, 33.8%) were considered vitamin D deficient and consumed an average of 347.05 ± 307.8 IUs of vitamin D through foods/beverages. The multivariate linear regression showed no statistically significant difference with vitamin D intake from foods/beverages on vitamin D deficiency status. Significant positive correlations were seen with vitamin D deficiency status and certain chronic conditions such as chronic kidney disease (p = 0.04), depression (p < 0.001), diabetes (p = 0.02), and vitamin D supplement use (p < 0.001). Significant negative correlations were observed with vitamin D deficiency status and age (p = 0.01) and sun exposure (p < 0.001). Future focus should be on educating individuals about factors associated with vitamin D to reduce the prevalence of vitamin D deficiency.
Introduction
Vitamin D, a fat-soluble vitamin, regulates serum calcium and phosphate to aid with bone mineralization, reduce inflammation and modulate immune function (1). Vitamin D can be obtained naturally through few food sources such as fatty fish, egg yolks and red meat, fortified foods such as cereals and fortified beverages such as milk, and through sun exposure (2). When vitamin D is obtained through food or sunlight, it undergoes two hydroxylations in the liver and kidney prior to activation. In the liver, vitamin D is converted to calcifediol [25(OH)D] and in the kidney, 25(OH)D-1α-hydroxylase, creates the active form, 1,25(OH)2D (3, 4). A study had illustrated that 5.9% of the US population were considered vitamin D deficient (serum vitamin D concentrations of <30 nmol or 12 ng/mL) and 24% of the US population were considered vitamin D insufficient (serum vitamin D concentrations of <50 nmol or <20 ng/mL) (5). Individuals at highest risk for vitamin D insufficiency/deficiency are those of advanced age, geographical location, race, sunscreen use, and significant time spent indoors (6–9). Furthermore, cross-sectional studies have illustrated that individuals who have certain chronic diseases such as kidney and obesity are at a higher risk for vitamin D deficiency (6, 10).
In the United States, 51.8% of adults have been diagnosed with at least one chronic disease (11) with the most prominent being heart disease, diabetes and kidney disease (12–14). Multiple factors contribute to chronic diseases such as age, sex, lifestyle behaviors such as limited physical activity (<150 min/week) (15) and dietary habits such as high intake of sodium, total fats and low intake of fruits, vegetables, and fiber (14, 16–19). Dietary habits that reduce intake of fruits, vegetables and other nutritious foods and beverages contributes to underconsumption of vitamin D (14, 20). The recommended daily allowances (RDA) of vitamin D for adults, aged 19–69 years, is 600 IUs or 15 mcgs daily and for adults >70 years old is 800 IUs or 20 mcgs daily with a tolerable upper limit of 4,000 IUs (21). Based on the results from the 2015–2016 NHANES dataset, men and women consumed, on average, 201.4 and 168 IU of vitamin D, respectively (22). Even though cross-sectional studies have shown the intake of vitamin D through supplements and dietary intake among American adults, they report this information based on 24-h recalls. Twenty-four-hour recalls can provide more accurate estimations of intake but tend to be labor-intensive and contribute to over or underreporting of information. Additionally, these only give a small insight to the dietary habits of an individual (23, 24). On the other hand, food frequency questionnaires (FFQs) are used for epidemiological studies as they are practical, easy to use and can provide an estimation of nutrients consumed based on the frequency, types and quantities of foods/beverages consumed (25, 26). Various FFQs have been validated to determine vitamin D intake in adults of various age ranges (e.g., young adults, college-aged athletes, post-menopausal females) (7, 27–30). However, one validated FFQ not only assesses vitamin D intake from food, but also sunlight exposure, sunscreen use, and supplement intake (7).
Strategies to improve vitamin D status, dependent on chronic disease or illness, has been to prescribe supplements in various quantities (e.g., 200–540,000 IU), frequencies (e.g., once to monthly) and forms (e.g., vitamin D2 or D3) (31–33). For healthy adults who are vitamin D deficient, 800 IUs daily of vitamin D supplements is recommended to achieve a sufficient serum 25(OH)D level of >20 ng/mL (34). Based on results from a 2015–2016 study, 49% of men and 59% of women aged 60 years and older took a vitamin D supplement, regardless if they were vitamin D deficient (22). Therefore, the purpose of this study was to explore the relationship between frequency and type of vitamin D intake from foods/beverages and risk factors associated with self-reported vitamin D deficiency among US adults.
Methods
Study Design and Participants
A cross-sectional study was conducted online through QualtricsXM, an online survey platform, during July–September 2021. Recruitment was voluntary and anonymous and occurred through e-blasts, social media platforms and ResearchMatch. ResearchMatch is a national health volunteer registry created by several academic institutions and supported by the National Institutes of Health as part of the Clinical Translational Science Award (CTSA) program (35). Inclusion criterion was adults being over the age of 18 years. Individuals who were not 18 years of age were excluded from the study. Initially a total of 1,837 adults consented to the study with 1,637 participants having complete data. All aspects of the study were approved exempt by the Institutional Review Board at the University of Florida (IRB202100807).
Questionnaire
Participants responded to a 38-item validated vitamin D questionnaire (7) that included demographics (10 items), sunlight exposure (4 items), supplement use (5 items), and foods/beverages consumed (24 items). Demographic questions included age range, sex, race/ethnicity, state of residence for the past 11 months, vitamin D insufficient/deficient, and chronic diseases/conditions. The vitamin D insufficient/deficient question had participants select yes/no or unsure, if participants selected yes, another question appeared with when they were diagnosed. Multiple selections were provided for the chronic diseases/conditions, if participants selected chronic kidney/renal disease, three additional prompt questions appeared that focused on when they were diagnosed, the stage they are currently in and stage they were in when initially diagnosed.
For questions surrounding sunlight exposure, participants selected the length of time they generally spent in the sun. Based on state of residence, participants were categorized as either receiving low, medium, or high sun exposure based on the National Environmental Public Health tracking network (36). Participants also identified the use of sunscreen as never/rarely, sometimes, usually or always. If they responded sometimes, usually or always, they received an additional question about the sunscreen SPF they used. For supplement use, if participants selected anything else but never, a prompt appeared for them to provide a free text response about the dosage.
The frequency of consuming foods/beverages that contained vitamin D either naturally or fortified were slightly modified from the original questionnaire to include additional sources of vitamin D foods (e.g., cheeses) and removal of sub-way sandwich (see Supplementary Table 1). The modified questionnaire included a total of 24 food/beverage items that provided portion sizes and categorized based on food group. Participants selected the frequency of consuming these foods/beverages over a 30-day period from never, rarely, 1–2 portions/week, 3–5 portions/week, one portion/day, 2–3 portions/day, and 4 or more portions/day. Adhering to the methodology by Larson-Meyer et al. (7), the intake of vitamin D from foods and beverages was estimated by multiplying the frequency midpoint by the average content of vitamin D and subsequently expressed as International Units (IU) daily over the 30-day period.
Statistical Analysis
Frequency counts and percentages were tabulated for demographic variables, average vitamin D intake, frequency of vitamin D supplement intake, and exposure to sun. Multiple linear regression was conducted to examine the relationships between self-reported vitamin D status and vitamin D intake from foods/beverages, supplements, sun exposure, and demographics (sex, race, age, chronic conditions/diseases, and state of residence). This analysis examined the key study co-variates (vitamin D intake from foods/beverages, supplements, and chronic conditions/diseases) and confounding variables (sex, race, age, state of residence, sun exposure) and isolated the relationship of interest—vitamin D status. Statistical significance was determined at p < 0.05 using JMP SAS v16 (SAS institute Inc, Cary, NC).
Results
Study Population
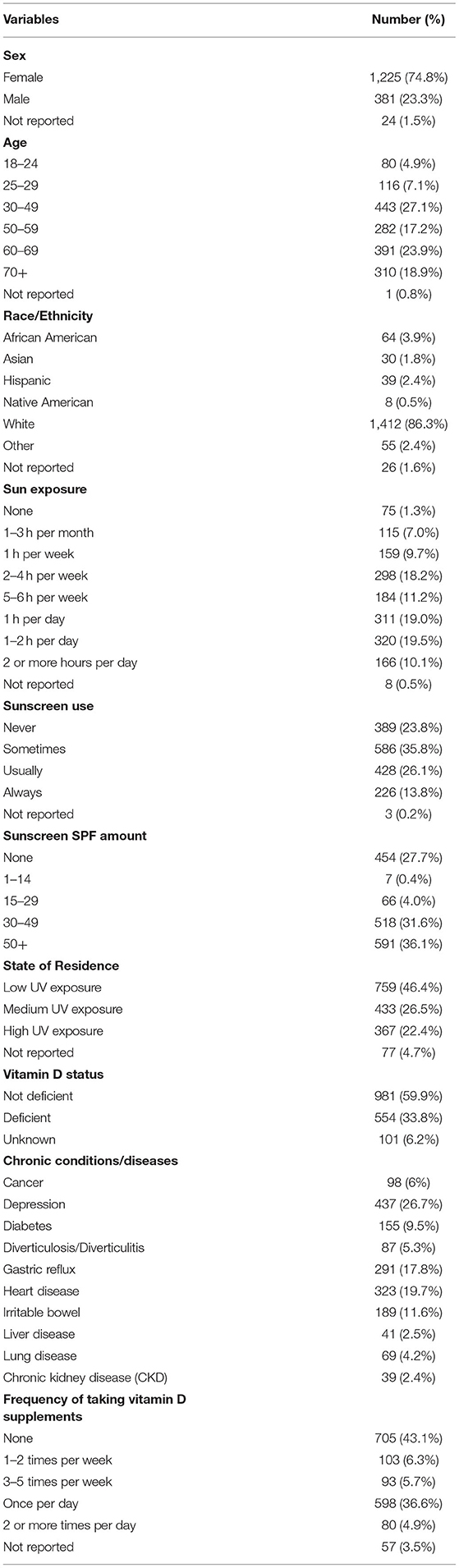
A total of 1,637 adults with a total completed survey were included in the analysis. A majority of participants were female (74.8%), between the ages of 30–49 years (27.1%), who identified as white/ non-Hispanic (86.3%), were never informed they were vitamin D deficient (60.0%), regardless of vitamin D status, 36.6% took a vitamin D supplement at least once daily, and a majority lived in a state that was considered low UV exposure (46.4%). Few participants indicated that they had a chronic disease/condition. Participants spent between 0.5–1 and 1–2 h in the sun daily from 10 a.m. to 3 p.m. (19.0 and 19.5%, respectively), and sometimes wore sunscreen (35.8%) and if they wore sunscreen chose an SPF of 50+ (36.1%) (see Table 1).
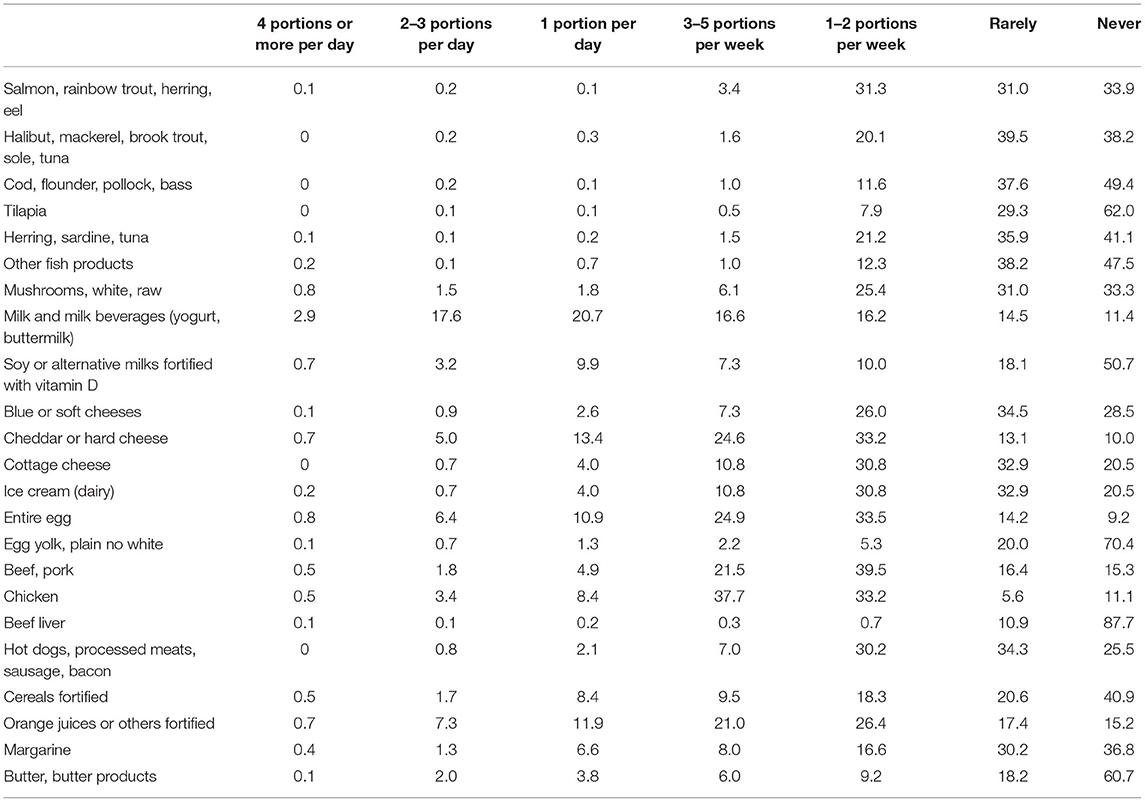
Vitamin D Intake From Foods and Beverages
On average, participants consumed 347.05 ± 307.8 IUs of vitamin D from foods/beverages. Foods/beverages that contained vitamin D were never or rarely consumed except for milk and milk products that were consumed once daily (20.7%), chicken that was consumed 3–5 times per week (37.7%), and orange juice or other juices fortified with vitamin D (26.4%), cheddar or hard cheeses (33.2%), entire egg (33.5%), and beef/pork (39.5%) consumed 1–2 times per week (see Table 2).
Relationship Between Vitamin D Intake, Risk Factors on Self-Reported Vitamin D Deficiency
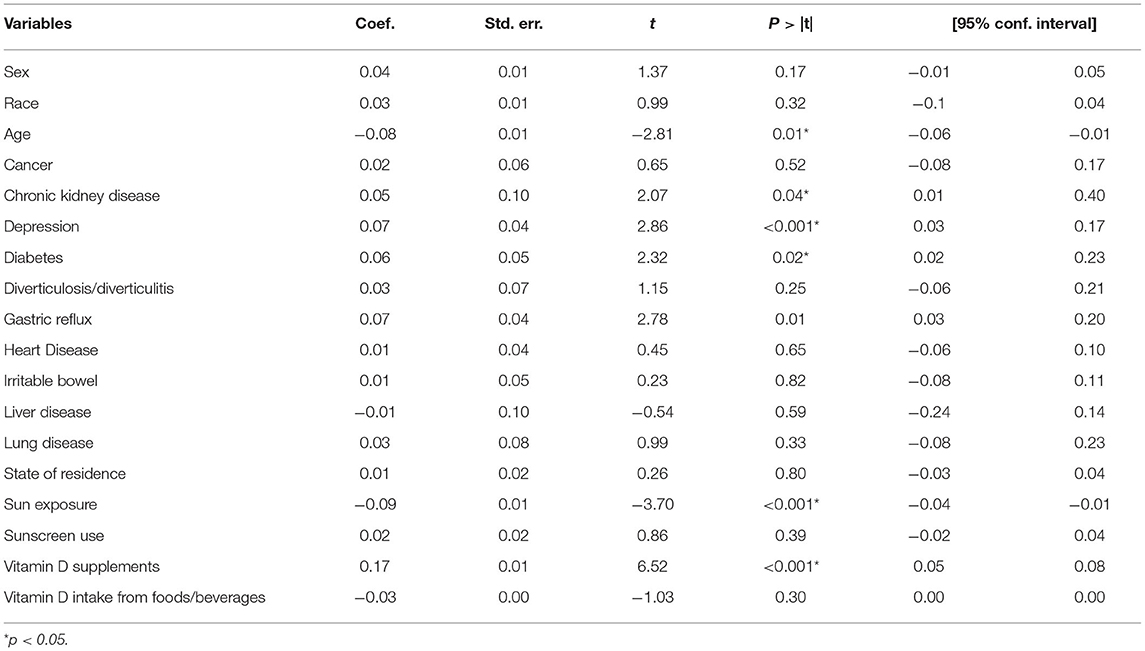
The multivariate linear regression showed significant positive correlations for chronic kidney disease (0.05, CI 95% 0.01–0.40; p = 0.04), depression (0.07, CI 95% 0.03–0.17; p < 0.001), diabetes (0.06, CI 95% 0.02–0.23; p = 0.02), and vitamin D supplement use (0.17, CI 95% 0.05–0.08; p < 0.001) on vitamin D status. Significant negative correlations were discovered with age (−0.08, CI 95% −0.06 to −0.01; p = 0.01) and sun exposure (−0.09, CI 95% −0.04−0.01; p < 0.001) on vitamin D status (see Table 3).
Discussion
Vitamin D deficiency is prevalent within the United States. Findings from this study demonstrated that 38.8% of participants had indicated they were vitamin D deficient and that associations were observed regarding vitamin D status with age, sun exposure, vitamin D supplement intake, and conditions.
Average total IUs of vitamin D intake daily from this study was 347.05 ± 307.8, which was similar to the intake reported by another study (7). Larson-Meyer et al. (7) demonstrated that participants' average consumption of vitamin D from foods and beverages was between 341 ± 228 IUs (n = 86) and 584 ± 589 IUs (n = 49), dependent on the season; fall, winter or spring. Although, the findings from this study showed that reported average vitamin D consumption was higher from foods and beverages compared to other studies that had reported vitamin D consumption between 68 IUs (37) and 178 IUs (30). This discrepancy may exist due to the different instruments used to obtain vitamin D intake. In this study, a modified validated food frequency questionnaire was used to determine the frequency participants consumed foods that contained vitamin D over a 30-day period. In the other studies (30, 37), 24-h recalls were used to determine amount of vitamin D consumed. Other studies demonstrated a discrepancy in vitamin D intake averages from food frequency questionnaires and 24-h recalls from 3.2% (38)−84% (30) likely due to over/under estimation of reporting or inability to recall frequency of consuming foods/beverages over certain time (39, 40). Overall, though, participants, on average, did not meet the vitamin D RDAs for healthy people. This is mainly related to participants rarely or never consuming foods high in vitamin D such as fish and dairy products. On the other hand, regardless of vitamin D status, 53% of participants took a vitamin D supplement at least once per week with the majority (36.6%) taking a vitamin D supplement at least once daily. An attempt was to gather the IUs/mcgs that participants took of vitamin D supplements, but many did not complete this section nor completed this correctly (e.g., provided the amount without indication of the units or provided amounts that were not commonly found in vitamin D supplements−600 mgs), thus no further analysis was able to be performed with how the supplement amount accounted for the total vitamin D intake.
Participants who completed this study may have been considered healthy as few indicated they had been diagnosed with the chronic conditions/diseases that have been associated with vitamin D deficiency. Although, positive associations were found with vitamin D status and chronic condition/disease in which those who had indicated they were depressed, diagnosed with diabetes, GI conditions such as gastric reflux, and chronic kidney disease had identified they were vitamin D deficient. This corresponds to other studies that showed associations between lower serum 25(OH)D levels (e.g., <20 ng/mL or 50 nmol/L) and the above conditions (41–44).
Furthermore, participants who had indicated sun exposure of 30 min or more daily had indicated no vitamin D deficiency. On the other hand, there were no associations between place of residence (low, middle or high UV exposure) and vitamin D status. This is in opposition to studies that have suggested that individuals who live in areas where there is low UV exposure, they are at a higher risk for vitamin D deficiency (6, 10, 45, 46). There was a negative association between age and vitamin D status, in which younger individuals had identified they were vitamin D deficient. Marzban et al. (47) observed that participants (n = 1,806) who were between the ages of 30–39 had lower serum vitamin D levels compared to participants who were 80 years and older. This was further confirmed by analyses of NHANES data (n = 25,010) that showed 42.4% of individuals between the ages of 18–39 years old were vitamin D deficient compared to 21.0% of individuals aged 60 years and older (48). Younger individuals may be at a higher risk for vitamin D deficiency due to low consumption of foods and beverages naturally high in vitamin D or limited sun exposure (49, 50). As this study was conducted over the summer for most of the United States, it is unknown if participants obtain the same sun exposure during colder months. Moreover, few, 13.7% of participants, met the RDAs for vitamin D, which could explain the number of participants who were <60 years of age indicating they were vitamin D deficient. Another explanation could be that participants who were older were taking a vitamin D supplement compared to the younger participants. There were no associations between sunscreen use and vitamin D deficiency, which is similar to findings from other studies (51, 52).
Limitations of this study included self-reporting of dietary intake and vitamin D status level. Further studies should focus on obtaining vitamin D serum samples and collecting them in different seasons. Even though participants from across the United States participated in this study, limited generalization of the results can occur from this study due to the limited variability of the demographics. As this study was conducted online, individuals who were without internet or were limited in their technological capability may have been excluded from participating (53, 54). Furthermore, this study was conducted while COVID-19 was occurring, thus ability to purchase seafood or other high vitamin D foods due to various reasons may have been limited, so conducting a follow-up study would be necessary for identifying shifts in consumption patterns.
Conclusion
In conclusion, this study showed that through self-reporting, the prevalence of vitamin D deficiency was nearly 39%. Foods that are naturally rich in vitamin D were rarely/never consumed. Although, intake of vitamin D supplements occurred frequently. Associations were seen with certain chronic conditions/diseases and vitamin D deficiency. Therefore, attempts should be made among the educational and scientific community to develop nutrition education programs to educate individuals about consuming and preparing foods naturally high in vitamin D to reduce the prevalence of vitamin D deficiency.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Ethics Statement
The studies involving human participants were reviewed and approved by University of Florida Institutional Review Board. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
JA: conceptualization of this study. JA, PG, and SS: methodology, formal analysis, investigation, and writing—review and editing. JA: data curation, writing—original draft preparation, supervision, and project administration. All authors have read and agreed to the published version of the manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We thank the assistance of statistical consultants to ensure accurate data analysis. Also, we could not have completed this research without the assistance of our participants.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fnut.2022.899300/full#supplementary-material
References
1. Ross AC, Taylor CL, Yaktine AL, Del Valle HB. DRI: Dietary Reference Intakes - Calcium Vitamin D. Institute of Medicine of the National Academies. Washington, DC: National Academies Press (2011).
2. Vitamin D: Fact Sheet for Health Professionals. National Institutes of Health: Office of Dietary Supplements (2020). Available online at: https://ods.od.nih.gov/factsheets/VitaminD-HealthProfessional/ (accessed October6, 2020).
3. Ramasamy I. Vitamin D metabolism and guidelines for vitamin D supplementation. Clin Biochem Rev. (2020) 41:103–26. doi: 10.33176/AACB-20-00006
4. Bikle DD. Vitamin D metabolism, mechanism of action, and clinical applications. In: Feingold K, Anawalt B, and Boyce A, editors. Chemical Biology. South Dartmouth, MA: Endotext (2021). p. 319–29. doi: 10.1016/j.chembiol.2013.12.016
5. Schleicher RL, Sternberg MR, Looker AC, Yetley EA, Lacher DA, Sempos CT, et al. National estimates of serum total 25-hydroxyvitamin D and metabolite concentrations measured by liquid chromatography-tandem mass spectrometry in the US population during 2007-2010. J Nutr. (2016) 146:1051–61. doi: 10.3945/jn.115.227728
6. Kaur J, Ferguson SL, Freitas E, Miller R, Bemben D, Knehans A, et al. Association of vitamin d status with chronic disease risk factors and cognitive dysfunction in 50–70 year old adults. Nutrients. (2019) 11:141. doi: 10.3390/nu11010141
7. Larson-meyer DE, Douglas CS, Thomas JJ, Johnson EC, Barcal JN, Heller JE, et al. Validation of a vitamin D specific questionnaire to determine vitamin D status in athletes. Nutrients. (2019) 11:2732. doi: 10.3390/nu11112732
8. Herrick KA, Storandt RJ, Afful J, Pfeiffer CM, Schleicher RL, Gahche JJ, et al. Vitamin D status in the United States, 2011-2014. Am J Clin Nutr. (2019) 110:150–7. doi: 10.1093/ajcn/nqz037
9. Dimakopoulos I, Magriplis E, Mitsopoulou AV, Karageorgou D, Bakogianni I, Micha R, et al. Association of serum vitamin D status with dietary intake and sun exposure in adults. Clin Nutr ESPEN. (2019) 34:23–31. doi: 10.1016/j.clnesp.2019.09.008
10. Holick MF. The vitamin D deficiency pandemic: approaches for diagnosis, treatment and prevention. Rev Endocr Metab Disord. (2017) 18:153–65. doi: 10.1007/s11154-017-9424-1
11. Boersma P, Black L, Ward B. Prevalence of multiple chronic conditions among US adults, 2018. Prev Chronic Dis. (2020) 17:200130. doi: 10.5888/pcd17.200130
12. Raghupathi W, Raghupathi V. An empirical study of chronic diseases in the united states: a visual analytics approach. Int J Environ Res Public Health. (2018) 15:10–2. doi: 10.3390/ijerph15030431
13. National Center for Chronic Disease Prevention Health Promotion. Chronic Diseases in America. (2019). p. 1–3. Available online at: www.cdc.gov/chronicdisease
15. Orces CH. Association between leisure-time aerobic physical activity and vitamin D concentrations among US older adults: the NHANES 2007–2012. Aging Clin Exp Res. (2019) 31:685–93. doi: 10.1007/s40520-018-1031-9
16. Wu XV, Chi Y, Selvam UP, Devi MK, Wang W, Chan YS, et al. A clinical teaching blended learning program to enhance registered nurse preceptors' teaching competencies: pretest and posttest study. J Med Internet Res. (2020) 22:1–13. doi: 10.2196/18604
17. Mirmiran P, Yuzbashian E, Aghayan M, Mahdavi M, Asghari G, Azizi F. A prospective study of dietary meat intake and risk of incident chronic kidney disease. J Ren Nutr. (2020) 30:111–8. doi: 10.1053/j.jrn.2019.06.008
18. Haring B, Selvin E, Liang M, Coresh J, Grams ME, Petruski-Ivleva N, et al. Dietary protein sources and risk for incident chronic kidney disease: results from the atherosclerosis risk in communities (ARIC) study. J Ren Nutr. (2017) 27:233–42. doi: 10.1053/j.jrn.2016.11.004
19. Allès B, Baudry J, Méjean C, Touvier M, Péneau S, Hercberg S, et al. Comparison of sociodemographic and nutritional characteristics between self-reported vegetarians, vegans, and meat-eaters from the nutrinet-santé study. Nutrients. (2017) 9:1023. doi: 10.3390/nu9091023
20. Romagnolo DF, Selmin OI. Mediterranean diet and prevention of chronic diseases. Nutr Today. (2017) 52:208–22. doi: 10.1097/NT.0000000000000228
21. Institute of Medicine. Dietary Reference Intakes for Calcium Vitamin D. Washington, DC: National Academy Press (2011).
22. USDA. What We Eat in American/National Health and Nutrition Examination Survey, 2015-2016. Washington, DC (2020). Available online at: https://www.fns.usda.gov/resource/healthy-eating-index-hei
23. Gibson RS, Ruth Charrondiere U, Bell W. Measurement errors in dietary assessment using self-reported 24-hour recalls in low-income countries and strategies for their prevention. Adv Nutr. (2017) 8:980–91. doi: 10.3945/an.117.016980
24. Brassard D, Laramée C, Robitaille J, Lemieux S, Lamarche B. Differences in population-based dietary intake estimates obtained from an interviewer-administered and a self-administered web-based 24-h recall. Front Nutr. (2020) 7:137. doi: 10.3389/fnut.2020.00137
25. Procter-Gray E, Olendzki B, Kane K, Churchill L, Hayes RB, Aguirre A, et al. Comparison of dietary quality assessment using food frequency questionnaire and 24-hour-recalls in older men and women. Public Health. (2017) 4:326–46. doi: 10.3934/publichealth.2017.4.326
26. Solbak NM, Robson PJ, Lo Siou G, Al Rajabi A, Paek S, Vena JE, et al. Administering a combination of online dietary assessment tools, the automated self-administered 24-hour dietary assessment tool, and diet history questionnaire II. in a cohort of adults in alberta's tomorrow project. J Acad Nutr Diet. (2021) 121:1312–26. doi: 10.1016/j.jand.2021.01.014
27. Glabska D, Guzek D, Sidor P, Wlodarek D. Vitamin D dietary intake questionnaire validation conducted among young polish women. Nutrients. (2016) 8:36. doi: 10.3390/nu8010036
28. Wu H, Gozdzik A, Barta JL, Wagner D, Cole DE, Vieth R, et al. The development and evaluation of a food frequency questionnaire used in assessing vitamin D intake in a sample of healthy young Canadian adults of diverse ancestry. Nutr Res. (2009) 29:255–61. doi: 10.1016/j.nutres.2009.03.006
29. Pritchard JM, Seechurn T, Atkinson SA. A food frequency questionnaire for the assessment of calcium, vitamin D and vitamin K: a pilot validation study. Nutrients. (2010) 2:805–19. doi: 10.3390/nu2080805
30. Hacker-Thompson A, Schloetter M, Sellmeyer DE. Validation of a dietary vitamin d questionnaire using multiple diet records and the block 98 health habits and history questionnaire in healthy postmenopausal women in Northern California. J Acad Nutr Diet. (2012) 112:419–23. doi: 10.1016/j.jada.2011.08.043
31. Nair P, Venkatesh B, Center JR. Vitamin D deficiency and supplementation in critical illness - the known knowns and known unknowns. Crit Care. (2018) 22:1–9. doi: 10.1186/s13054-018-2185-8
32. Cianferotti L, Bertoldo F, Bischoff-Ferrari HA, Bruyere O, Cooper C, Cutolo M, et al. Vitamin D supplementation in the prevention and management of major chronic diseases not related to mineral homeostasis in adults: Research for evidence and a scientific statemtn from the European society for clinical and economic aspects of osteoporosis. Endocrine. (2017) 56:245–61. doi: 10.1007/s12020-017-1290-9
33. Ikizler TA, Burrowes JD, Byham-Gray LD, Campbell KL, Carrero JJ, Chan W, et al. KDOQI clinical practice guideline for nutrition in CKD: 2020 update. Am J Kidney Dis. (2020) 76:S1–107. doi: 10.1053/j.ajkd.2020.05.006
34. Amrein K, Scherkl M, Hoffmann M, Neuwersch-Sommeregger S, Köstenberger M, Tmava Berisha A, et al. Vitamin D deficiency 2.0: an update on the current status worldwide. Eur J Clin Nutr. (2020) 74:1498–513. doi: 10.1038/s41430-020-0558-y
35. ResearchMatch. Vanderbuilt University. (2020). Available online at: https://www.researchmatch.org/
36. CDC. National Environmental Public Health Tracking Network. (2022). Available online at: https://ephtracking.cdc.gov/ (accessed August 20, 2021).
37. Torna E, Smith E, Lamothe M, Langkamp-Henken B, Andrade JM. Comparison of diet quality of US adults based on primary motivation for following a vegetarian diet: a cross-sectional online study. Nutr Res. (2021) 90:13–23. doi: 10.1016/j.nutres.2021.04.001
38. Kiely M, Collins A, Lucey AJ, Andersen R, Cashman KD, Hennessy A. Development, validation and implementation of a quantitative food frequency questionnaire to assess habitual vitamin D intake. J Hum Nutr Diet. (2016) 29:495–504. doi: 10.1111/jhn.12348
39. Carroll RJ, Midthune D, Subar AF, Shumakovich M, Freedman LS, Thompson FE, et al. Taking advantage of the strengths of 2 different dietary assessment instruments to improve intake estimates for nutritional epidemiology. Am J Epidemiol. (2012) 175:340–7. doi: 10.1093/aje/kwr317
40. Shim J-S, Oh K, Kim HC. Dietary assessment methods in epidemiologic studies. Epidemiol Health. (2014) 36:e2014009. doi: 10.4178/epih/e2014009
41. Hoogendijk WJG, Lips P, Dik MG, Deeg DJH, Beekman ATF, Penninx BWJH. Depression is associated with decreased 25-hydroxyvitamin D and increased parathyroid hormone levels in older adults. Arch Gen Psychiatry. (2008) 65:508–12. doi: 10.1001/archpsyc.65.5.508
42. Jhee JH, Kim H, Park S, Yun HR, Jung SY, Kee YK, et al. Vitamin D deficiency is significantly associated with depression in patients with chronic kidney disease. PLoS ONE. (2017) 12:e0171009. doi: 10.1371/journal.pone.0171009
43. Gois PHF, Wolley M, Ranganathan D, Seguro AC. Vitamin D deficiency in chronic kidney disease: recent evidence and controversies. Int J Environ Res Public Health. (2018) 15:1–16. doi: 10.3390/ijerph15081773
44. Gao Y, Zheng T, Ran X, Ren Y, Chen T, Zhong L, et al. Vitamin D and incidence of prediabetes or type 2 diabetes: a four-year follow-up community-based study. Dis Markers. (2018) 2018:1926308. doi: 10.1155/2018/1926308
45. Plum LA, Deluca HF. Vitamin D, disease and therapeutic opportunities. Nat Rev Drug Discov. (2010) 9:941–55. doi: 10.1038/nrd3318
46. Engelsen O. The relationship between ultraviolet radiation exposure and vitamin D status. Nutrients. (2010) 2:482–95. doi: 10.3390/nu2050482
47. Marzban M, Kalantarhormozi M, Mahmudpour M, Ostovar A, Keshmiri S, Darabi AH, et al. Prevalence of vitamin D deficiency and its associated risk factors among rural population of the northern part of the Persian Gulf. BMC Endocr Disord. (2021) 21:219. doi: 10.1186/s12902-021-00877-5
48. Liu X, Baylin A, Levy P. Vitamin D deficiency and insufficiency among US adults: prevalence, predictors and clinical implications. Br J Nutr. (2018) 119:928–36. doi: 10.1017/S0007114518000491
49. Tangprich V, Pearce EN, Chen TC, Holick MF. Vitamin D insufficiency among free-living healthy young adults. Am J Med. (2002) 112:659–62. doi: 10.1016/S0002-9343(02)01091-4
50. Tønnesen R, Hovind PH, Jensen LT, Schwarz P. Determinants of vitamin D status in young adults: influence of lifestyle, sociodemographic and anthropometric factors. BMC Public Health. (2016) 16:385. doi: 10.1186/s12889-016-3042-9
51. Linos E, Keiser E, Kanzler M, Sainani KL, Lee W, Vittinghoff E, et al. Sun protective behaviors and vitamin D levels in the US population: NHANES 2003-2006. Cancer Causes Control. (2012) 23:133–40. doi: 10.1007/s10552-011-9862-0
52. Neale RE, Khan SR, Lucas RM, Waterhouse M, Whiteman DC OC. The effect of sunscreen on vitamin D: a review. Br J Dermatol. (2019) 181:907–15. doi: 10.1111/bjd.17980
Keywords: vitamin D, adults, food frequency questionnaire, chronic conditions, sun exposure
Citation: Andrade JM, Grandoff PG and Schneider ST (2022) Vitamin D Intake and Factors Associated With Self-Reported Vitamin D Deficiency Among US Adults: A 2021 Cross-Sectional Study. Front. Nutr. 9:899300. doi: 10.3389/fnut.2022.899300
Received: 18 March 2022; Accepted: 25 April 2022;
Published: 11 May 2022.
Edited by:
Lidia Montero, University of Duisburg-Essen, GermanyReviewed by:
Majid Hajifaraji, National Nutrition and Food Technology Research Institute, IranMohamed Fawzy Ramadan Hassanien, Umm Al-Qura University, Saudi Arabia
Radjassegarin Arumugam, A. V. C. College, India
Copyright © 2022 Andrade, Grandoff and Schneider. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jeanette M. Andrade, amFuZHJhZGUxQHVmbC5lZHU=
 Jeanette M. Andrade
Jeanette M. Andrade Philip G. Grandoff
Philip G. Grandoff Sydney T. Schneider
Sydney T. Schneider