
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Nutr. , 11 April 2022
Sec. Clinical Nutrition
Volume 9 - 2022 | https://doi.org/10.3389/fnut.2022.864024
Objective: The Global Leader Initiative on Malnutrition (GLIM) criteria have been recommended for malnutrition diagnosis recently, for which the first step is malnutrition risk screening with any validated tool. This study aims to investigate the incidence of malnutrition risk in gastrointestinal stromal tumor (GIST) inpatients and compare the suitability of Nutritional Risk Screening 2002 (NRS2002) and Malnutrition Universal Screening Tool (MUST) as the first-step screening tool for GLIM criteria.
Methods: We retrospectively analyzed the clinical data of GIST inpatients in our hospital from January 2015 to December 2019. NRS2002 and MUST were used to screen malnutrition risk at the time of admission. The diagnostic consistency of these two tools with GLIM criteria for malnutrition was analyzed, and the predictive performance of both tools for the length of hospital stay and the occurrence of complications was also evaluated in surgical and non-surgical inpatients.
Results: A total of 269 GIST inpatients were included in this study, of which 45.7 and 40.9% were at malnutrition risk determined by NRS2002 and MUST, respectively. In non-surgical inpatients, NRS2002 and MUST had similar diagnostic consistency with GLIM criteria in sensitivity (93.0 vs. 97.7%), specificity (81.1 vs. 81.1%), and Kappa value (K = 0.75 vs. 0.80), and high nutritional risk classified by NRS2002 and malnutrition identified by GLIM criteria were found to be associated with the length of hospital stay. In surgical inpatients, MUST had better diagnostic consistency with GLIM criteria in sensitivity (86.1 vs. 53.5%) and Kappa value (K = 0.61 vs. 0.30) than NRS2002, but no factors were found associated with the length of postoperative hospital stay or the occurrence of complications.
Conclusion: The malnutrition risk is common in GIST inpatients. NRS2002 is more suitable than MUST for the first-step risk screening of the GLIM scheme in non-surgical inpatients, considering its better performance in screening malnutrition risk and predicting clinical outcomes. MUST was found to have good diagnostic consistency with GLIM criteria for malnutrition in both non-surgical and surgical GIST inpatients, and further studies need to be conducted to investigate its predictive performance on clinical outcomes.
Gastrointestinal stromal tumor (GIST) is the most common mesenchymal neoplasm in the digestive tract (1), which can rapidly turn from a potentially malignant tumor to cancer (2). As we know, patients with gastrointestinal tumors are usually accompanied by unbalanced nutritional status, such as protein deficiency and energy imbalance, and the incidence of malnutrition even reached from 40 to 80% (3). In general, malnutrition in patients with gastrointestinal tumors was correlated with shorter survival time, poorer tolerance to chemotherapy, and worse quality of life (4–6). If malnutrition, especially undernutrition, has not been identified and corrected in time, it could lead to reduced immune function, increased infectious complications, prolonged hospitalization, increased mortality rates of patients, and more associated medical expenditure (7–9). Therefore, it is of great significance to make an accurate assessment of the nutritional status in time, and then draw up an individualized plan for the nutritional treatment, thereby improving or even reversing the clinical outcomes of patients with gastrointestinal tumors (10).
Although the diagnosis of malnutrition is the basis of clinical nutrition intervention, there were no recognized definitions and uniform diagnostic criteria for malnutrition for quite a long time around the world. Recently, the global (nutrition) leaders launched the criteria for the diagnosis of malnutrition, referred to as Global Leader Initiative on Malnutrition (GLIM) criteria. According to GLIM criteria, malnutrition can be diagnosed by conforming to at least one phenotypic criterion (involuntary weight loss, low body mass index, and muscle loss) and one etiologic criterion (reduced food intake or assimilation and inflammation or disease burden) (11).
A consensus scheme for malnutrition diagnosis in adults was also proposed by GLIM, of which the first step is malnutrition risk screening with any validated tool, and the second step is assessment for diagnosis and severity grading of malnutrition (11). Over the past decades, several screening tools have been introduced and evaluated. Among them, two tools commonly used in clinical practice are Nutritional Risk Screening 2002 (NRS2002) and Malnutrition Universal Screening Tool (MUST) (12, 13). NRS2002 is the tool proposed by the European Society for Clinical Nutrition and Metabolism (ESPEN) and mainly applied to inpatients for screening the indications for nutritional support (14). MUST was developed by the British Association for Parenteral and Enteral Nutrition (BAPEN) to detect the malnutrition risk for all adult patients in different medical institutions (15). Compared with MUST, the NRS2002 scoring system contains the nutritional components of MUST, and in addition, grading of severity of disease as a reflection of increased nutritional requirements, and the age assessment (14).
At present, the management of GIST inpatients has been mainly focused on surgery and medication, and the nutritional status of GIST inpatients has been less explored. Therefore, this study aims to investigate the incidence of malnutrition risk by the use of NRS2002 and MUST, as well as to compare the suitability of these two tools as the first-step screening tool for GLIM criteria in GIST inpatients.
This study retrospectively analyzed the clinical data of GIST inpatients in our hospital from January 2015 to December 2019. Participants were patients with GIST admitted to the department of gastrointestinal surgery in the First Affiliated Hospital of Chongqing Medical University during that period. This study was performed in accordance with the World Medical Association Declaration of Helsinki and approved by the Medical Ethical Committee of the First Affiliated Hospital of Chongqing Medical University. All the patients included in this study provided informed consent.
The inclusion criteria were as follows: (1) pathologically confirmed GIST; (2) aged 18–90 years; (3) hospitalized for more than 24 h; (4) no emergency surgery within 24 h after admission; and (5) willing to accept malnutrition risk screening and assessment. Patients were excluded if it was difficult to obtain their accurate height and weight, perform body composition measurements on them, or they could not complete malnutrition risk screening and assessment.
The collected data mainly included the following aspects: patient general information, anthropometric measurement, implementation of malnutrition screening and malnutrition assessment.
Patient general information were obtained from medical records, which included age, sex, medical treatment history, laboratory examination and combined symptoms at admission, primary tumor site, tumor risk stratification, length of hospital stay, or complications, during hospitalization.
Anthropometric measurements included body weight, height, body mass index (BMI), and muscle mass, which were carried out by a trained nurse or dietician. The weight and height of the patients were measured by using uniform calibrated instruments on the morning within 24 h after admission. After overnight fasting, emptying of bowels, and urinating in the morning, the patients wearing hospital gowns were weighed before breakfast without shoes. Meanwhile, barefoot heights were measured. BMI was calculated using the standard formula as weight (kg) divided by the square of height (m2). Muscle mass was determined by fat free mass (FFM), which was obtained through bioelectrical impedance measured by InBodyS10. Fat free mass index (FFMI) was calculated as FFM divided by the square of height (m2).
Malnutrition risk of GIST inpatients was screened with NRS2002 and MUST, which was performed by a trained nutritional support pharmacist within 48 h of admission. The NRS2002 scoring system consists of three parts according to ESPEN guidelines (14). The first part of NRS2002 assesses the nutritional status of the patient, which is based on the changes in weight in the recent 3 months, dietary intake one-week before hospitalization, and the BMI. The second part of the NRS2002 assesses the severity of the disease, which could be scored by its impact on the increased nutritional requirements of patients. The scores for the first two parts of the NRS2002 vary from 0 to 3. The last part of the NRS2002 is the age assessment. If the patient is 70 years or older, add 1 score. Therefore, the final score of NRS2002 can range from 0 to 7. Patients with a total NRS2002 score of ≥ 3 indicate a high nutritional risk. The MUST was also used to screen malnutrition risk in this study, which includes three components, such as BMI (in kg/m2), unplanned weight loss in past 3–6 months, and absence or inadequacy of dietary intake for > 5 d due to the presence of acute disease (15). The score for each component varies from 0 to 2. Overall risk of malnutrition according to MUST is rated as low (score = 0), medium (score = 1), or high (score ≥ 2).
According to GLIM criteria (11), malnutrition can be diagnosed for patients by conforming to at least one phenotypic criterion and one etiologic criterion based on the first step of malnutrition risk screening (Figure 1). To assess the diagnostic consistency between the two risk-screening tools and GLIM criteria for malnutrition in this study, malnutrition was directly diagnosed according to GLIM criteria without the first step of malnutrition risk screening. Phenotype criteria include: (1) involuntary weight loss: > 5% within 6 months or > 10% beyond 6 months; (2) low BMI for Asian: < 18.5 kg/m2 if < 70 years or < 20 kg/m2 if > 70 years; and (3) reduced muscle mass: a low FFMI (< 15 kg/m2 for women, < 17 kg/m2 for men). Etiological criteria include: (1) < 50% of energy requirements > 1 week, or any reduction for at least 2 weeks, or any chronic gastrointestinal symptoms that lead to inadequate or impaired absorption and assimilation in patients; (2) inflammation associated with acute disease/injury or chronic disease. As GLIM consensus mentioned that most chronic organ diseases, such as cancer, are associated with chronic or recurrent inflammation of a mild to a moderate degree, patients diagnosed with GIST in this study were all thought to meet the etiologic criterion.
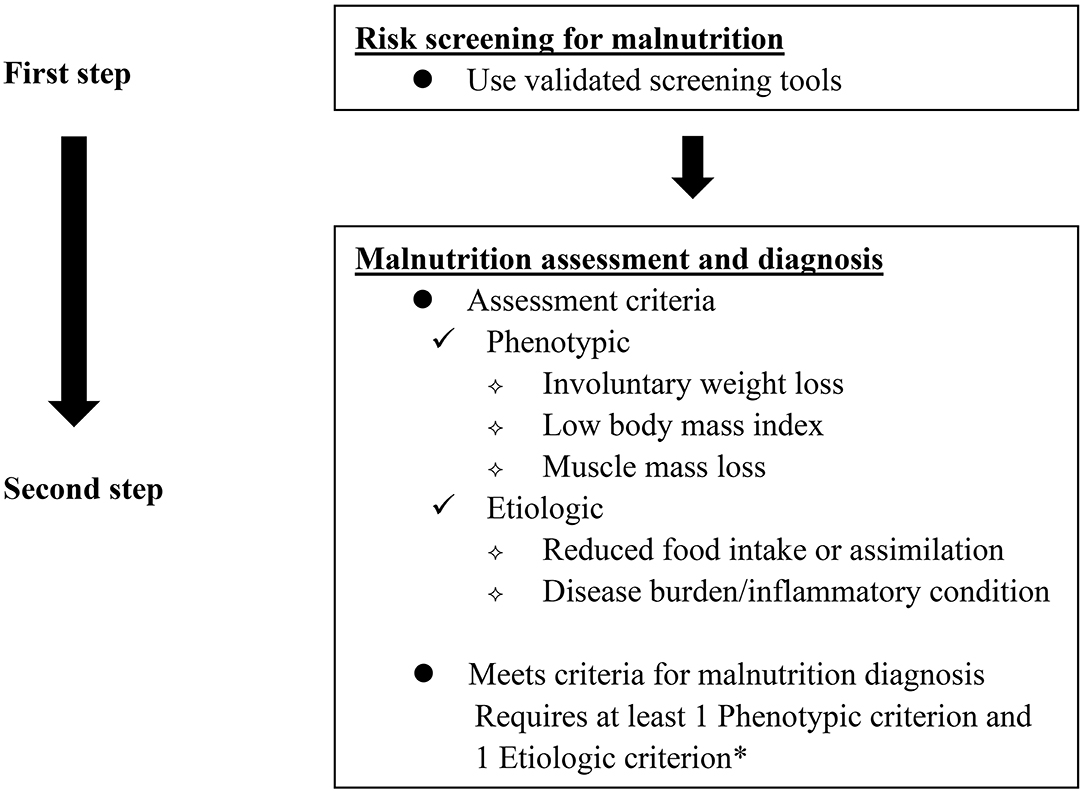
Figure 1. GLIM diagnostic scheme for screening, assessment, and diagnosis of malnutrition. *In this study, patients diagnosed with GIST were all thought to meet the etiologic criterion as GLIM consensus mentioned that most chronic organ diseases, such as cancer, are associated with chronic or recurrent inflammation of a mild to moderate degree.
Statistical evaluations of the two risk-screening tools (i.e., MUST and NRS2002) compared with the GLIM criteria for malnutrition diagnosis were performed in both total sample and subgroups (with surgery or not suitable for surgery because of metastatic or advanced GIST). Continuous variables were expressed as mean values ± SD (mean ± SD), while categorical variables were presented as absolute values and percentages. Differences between variables were tested with the use of the Mann–Whitney U-test or the chi-square test depending on data characteristics. Multivariable logistic regressions were used to identify the factors associated with the length of hospital stay or the occurrence of complications.
Cohen's Kappa statistic was calculated to determine the diagnostic consistency between the screening tools (i.e., MUST and NRS2002) and GLIM criteria for the identification of malnutrition according to some studies (12, 16, 17). The kappa value can be interpreted as follows: 0–0.20 as no agreement, 0.21–0.39 as minimal, 0.40–0.59 as weak, 0.60–0.79 as moderate, 0.80–0.90 as strong, and above 0.9 as almost perfect agreement (18). The sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), positive (LR+), and negative (LR-) likelihood ratio of the two tools were also evaluated referred to the GLIM criteria. Meanwhile, the receiver operating characteristic (ROC) curve of the two tools was also used to determine the ability to accurately distinguish patients with malnutrition from well nutrition according to some studies (12, 16, 17). Accuracy is considered low when the area under the ROC curve varies from 0.50 to 0.69, moderate from 0.70 to 0.90, and high if more than 0.9 (17).
Statistical analysis was performed by SPSS for Windows (version 22.0, IBM Corp., Armonk, NY, USA), and P <0.05 were considered statistically significant (two-tailed).
At the time of data analysis, a total of 301 GIST inpatients from January 2015 to December 2019 were alive, of which 7 inpatients were excluded because of emergency surgery on the day of admission and 25 inpatients were excluded because they refused to accept risk screening and assessment for malnutrition. Finally, 269 inpatients were included. The median age was 57 years (range: 29–90), with a sex ratio of 1.07:1 (51.7% were women). The characteristics of the total, surgical, and non-surgical participants were shown in Table 1.
In this study, we found that malnourished patients had a significantly lower BMI in total, non-surgical, and surgical GIST inpatients (P <0.001), a significantly lower level of serum albumin in total and non-surgical GIST inpatients (P <0.001), and a significantly longer length of hospital stay in non-surgical GIST inpatients (P <0.001) as compared with well-nourished patients. In addition, GIST patients with targeted therapy had a higher incidence of malnutrition compared to the patients with no targeted therapy (P <0.001 for total patients and P = 0.001 for non-surgical patients). With the number of combined symptoms at admission increasing, the incidence of malnutrition increased significantly (P <0.001 for total patients and P = 0.023 for non-surgical patients).
Table 2 showed the details of the classifications for malnutrition risk determined by NRS2002 and MUST. The incidence of moderate/high risk of malnutrition determined by NRS2002 and MUST was 45.7 and 40.9% for total inpatients, 58.8 and 61.3% for non-surgical inpatients, and 40.2 and 32.3% for surgical in patients.
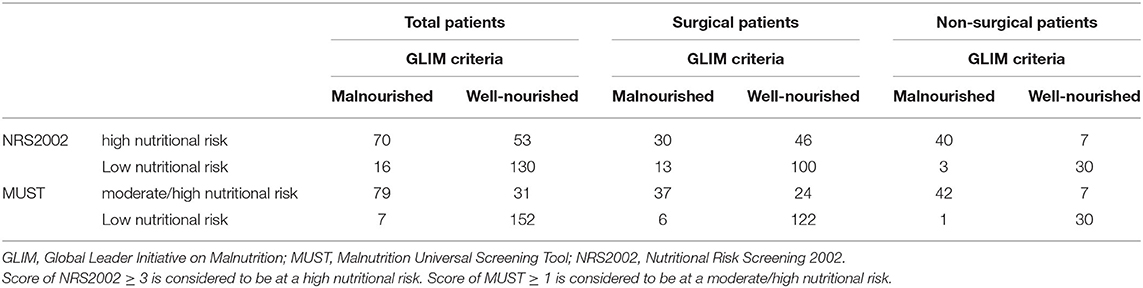
Table 2. Cross-tabulation results of the malnutrition identified by GLIM criteria and the malnutrition risk classified by NRS2002 and MUST.
Table 3 showed the evaluation of diagnostic consistency for malnutrition between the two screening tools and the GLIM criteria. In total inpatients, MUST had a higher value of sensitivity (91.9 vs. 65.1%), PPV (71.8 vs. 56.9%), NPV (95.6 vs. 89.0%), Kappa (K = 0.70 vs. 0.47), and a larger area under the ROC curve (AUC = 0.90 vs. 0.83) compared with NRS2002.
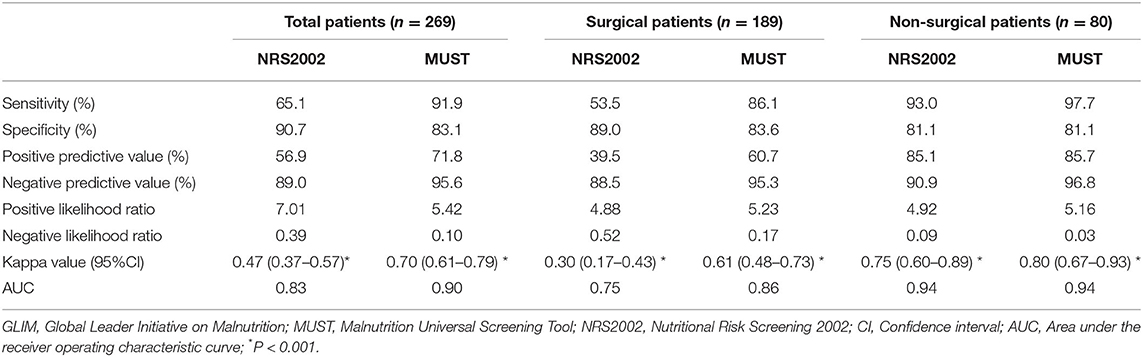
Table 3. Statistical evaluations of the two risk-screening tools compared with GLIM criteria for the diagnosis of malnutrition.
Considering that there might be some heterogeneity between non-surgical and surgical inpatients, we performed subgroup analyses to further evaluate the accuracy of NRS2002 and MUST in light of GLIM criteria for the malnutrition diagnosis (Table 3). In the non-surgical inpatients, NRS2002 and MUST had similar consistency with GLIM criteria in sensitivity (93.0 vs. 97.7%), specificity (81.1 vs. 81.1), PPV (85.1 vs. 85.7%), NPV (90.9 vs. 96.8%), Kappa value (K = 0.75 vs. 0.80), and area under the ROC curve (AUC = 0.94 vs. 0.94). In surgical inpatients, MUST had a higher value of sensitivity (86.1 vs. 53.5%), PPV (60.7 vs. 39.5%), NPV (95.3 vs. 88.5%), Kappa (K = 0.61 vs. 0.30), and a larger area under the ROC curve (AUC = 0.86 vs. 0.75) compared with NRS2002. ROC curves were presented in Figure 2.
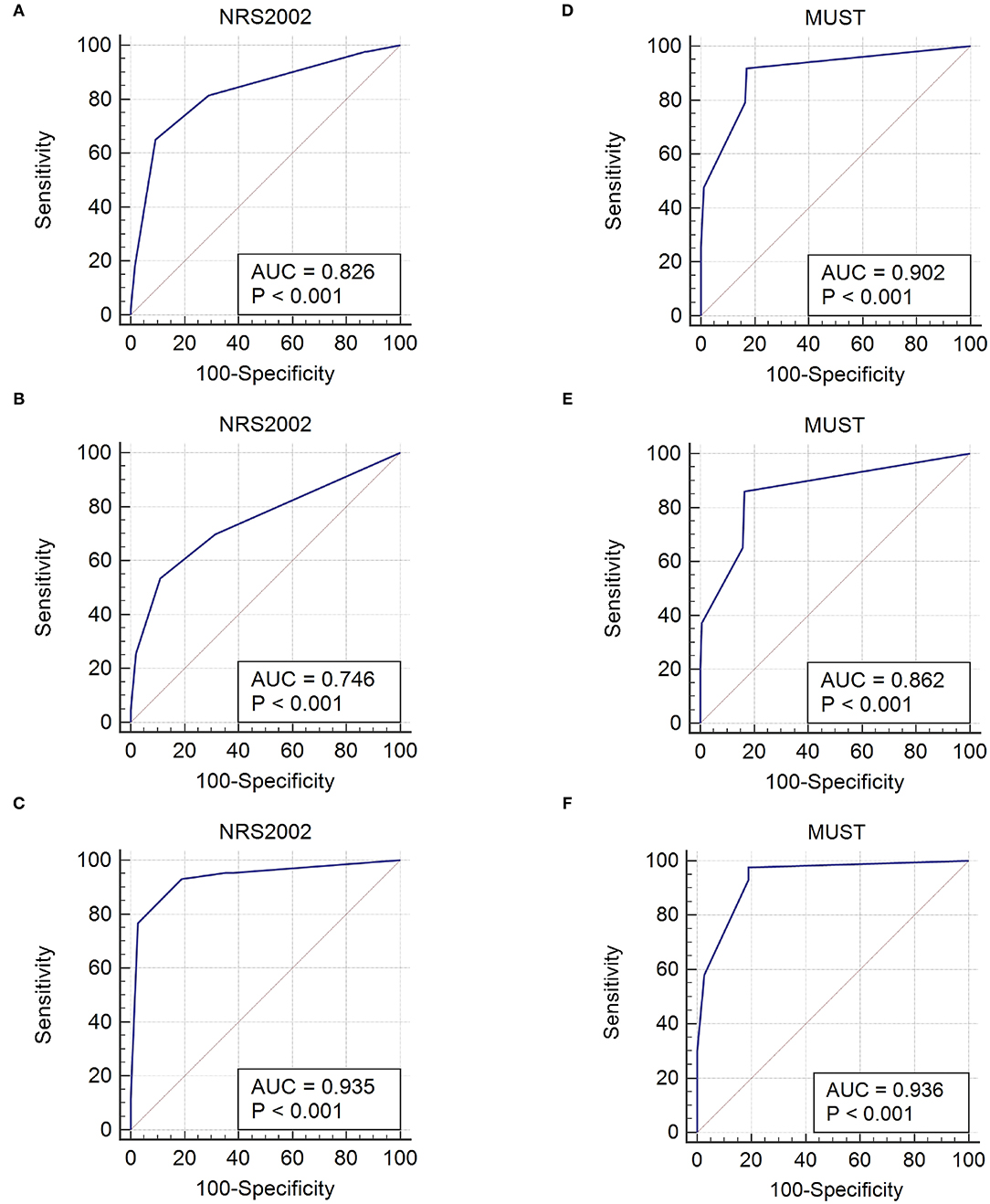
Figure 2. Diagnostic accuracy of NRS2002 compared to GLIM criteria for malnutrition in total (A), surgical (B), and non-surgical (C) GIST inpatients. Diagnostic accuracy of MUST compared to GLIM criteria for malnutrition in total (D), surgical (E), and non-surgical (F) GIST inpatients. NRS2002, Nutritional Risk Screening 2002; MUST, Malnutrition Universal Screening Tool; AUC, Area under the receiver operating characteristic curve; GLIM, Global Leadership Initiative on Malnutrition.
In the univariate analysis of complications occurrence, gender was the only associated factor in surgical inpatients (OR = 2.96, P = 0.013), and no statistical difference was found in other factors among surgical or non-surgical inpatients.
Table 4 showed the univariate and multivariate analyses for the length of hospital stay in non-surgical inpatients and postoperative hospital stay in surgical inpatients. In non-surgical inpatients, the associated factors in the univariate analysis for the length of hospital stay were BMI, serum albumin, targeted therapy, number of combined symptoms at admission, malnutrition risk classified by NRS2002 or MUST, malnutrition identified by GLIM criteria, of which high risk of malnutrition classified by NRS2002 and malnutrition identified by GLIM criteria were found to be associated with the length of hospital stay ≥ 9 d (median hospital stay = 9 d) in the multivariate analysis. In the univariate analysis for the length of postoperative hospital stay in surgical inpatients, the associated factors were serum albumin, hemoglobin, primary tumor site, tumor risk stratification, and malnutrition risk classified by NRS2002. However, no significant associated factor was found in the multivariate analysis.
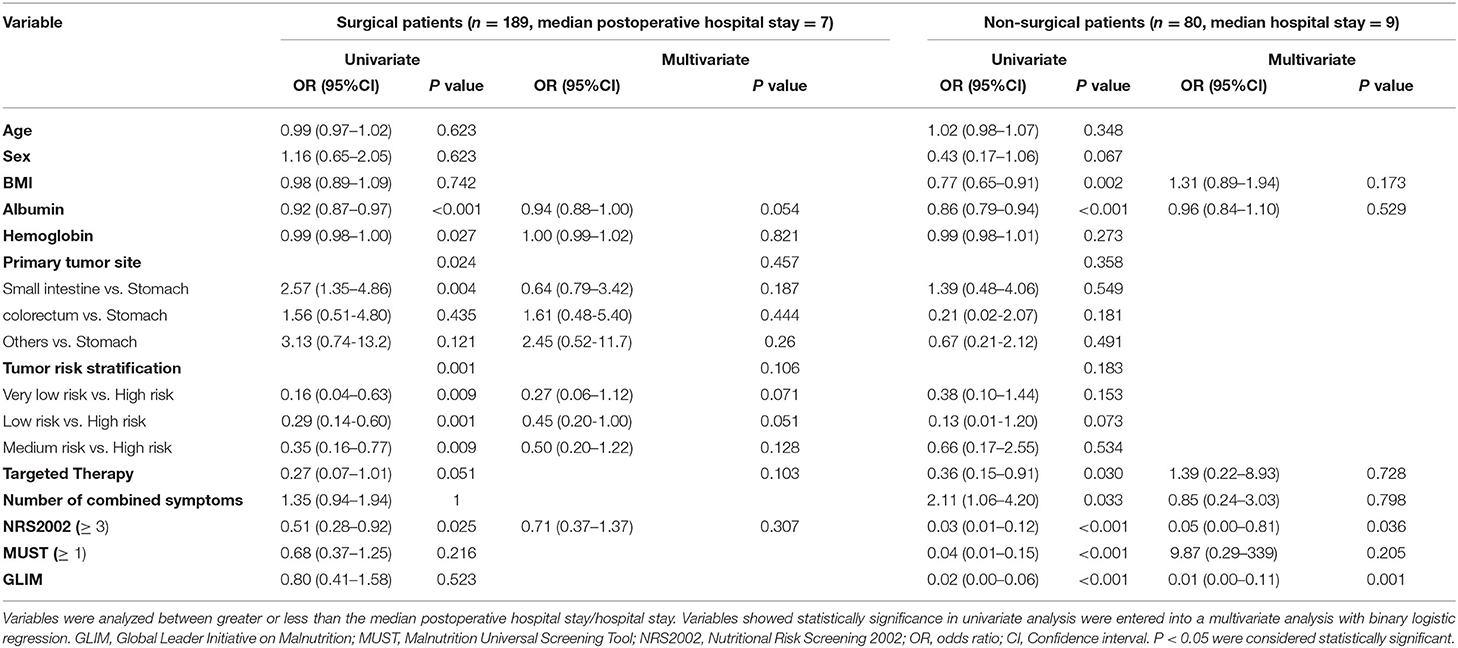
Table 4. Univariate and multivariate analyses for the length of hospital/postoperative hospital stay in non-surgical/surgical patients with GIST.
Recently, the GLIM criteria have been recommended for the malnutrition diagnosis, and a two-step model for risk screening and diagnostic assessment was also proposed by GLIM consensus. In this study, we investigated the incidence of malnutrition risk in GIST inpatients, and compared the suitability of NRS2002 and MUST as the first-step screening tool for GLIM criteria in GIST inpatients in view of their screening and predictive performance.
GIST is the most common mesenchymal neoplasm in the digestive tract (1). However, few people paid attention to the nutritional status of GIST patients and related studies were limited. Therefore, we investigated the incidences of malnutrition risk in GIST inpatients. As we know, malnutrition risk screening was performed only with NRS2002 in GIST patients in previous studies (19, 20). The incidence of malnutrition risk for total GIST inpatients in our study (46% with NRS2002 and 41% with MUST, respectively) was lower than 78% reported by Ding et al. (19), but higher than 34% reported by Yin et al. (20). In the study of Ding et al. (19), the average age of patients was higher than that in our study and more patients had a BMI <18.5 kg/m2, which were both important components of the NRS2002 scoring system. That might explain the difference in the incidence of malnutrition risk between the two studies. In the study of Yin et al. (20), the incidence of malnutrition risk was lower in patients with intermediate-risk of tumor stratification than that in our study. The reason for this difference might be that most patients with intermediate-risk admitted to our hospital were in serious condition, while the patients with mild illness were not admitted to the hospital for having been treated in the daily follow-up.
A consensus scheme consisting of risk screening and assessment for the malnutrition diagnosis was proposed by GLIM, and there was a strong consensus that the key first step in the evaluation of nutritional status is malnutrition risk screening to identify “at-risk” status by the use of any validated screening tool (11). As observed in this study, there was a difference between the incidences of malnutrition risk identified by NRS2002 and MUST for total, non-surgical, or surgical GIST inpatients. Considering that there might be some heterogeneity between non-surgical and surgical inpatients, the suitability of NRS2002 and MUST as the first-step screening tool for GLIM criteria in GIST was further evaluated in these two types of patients, respectively. Given the screening tool with better diagnostic consistency with GLIM criteria might indicate its better application in the GLIM scheme, we firstly compared the screening performance of NRS2002 and MUST on malnutrition in light of the GLIM criteria, which could be quantitated by measures, such as sensitivity, specificity, PPV, NPV, LR+, LR-, and area under the ROC curve (21). Besides that, we also evaluated the predictive performance of NRS2002 and MUST on the length of hospital stay and the occurrence of complications, for better prediction of meaningful health outcomes that are known to be associated with malnutrition (22).
For non-surgical inpatients included in this study, NRS2002 and MUST had similar consistency with GLIM criteria in sensitivity, specificity, PPV, NPV, Kappa value, and area under the ROC curve. However, only malnutrition risk classified by NRS2002 and malnutrition diagnosed by GLIM criteria were found to be associated with the length of hospital stay in the multivariate analysis. This result can be attributed to differences in the original design of the NRS2002 and MUST. The purpose of the NRS2002 is to screen patients who might benefit from receiving nutritional support (14), while MUST is developed for the screening of malnutrition (14, 15). In some studies (23, 24), NRS2002 had been suggested as a strong predictor of clinical outcomes, such as length of hospital stays, complications, and mortality. Thus, NRS2002 might be suitable as the first-step screening tool for GLIM criteria in non-surgical GIST inpatients considering its screening and predictive performance. In addition, it was also found that the OR values for MUST in non-surgical GIST patients differed greatly in the univariate and multivariate analyses for the length of hospital stay. This might be because of the influence of other covariates in multivariate analysis and the uneven distribution of the raw data. Therefore, further prospective studies are needed to confirm whether moderate/high nutritional risk classified by MUST is associated with the length of hospital stay or other indicators for clinical outcomes.
For surgical GIST inpatients included in this study, MUST showed better consistency with GLIM criteria manifested as a higher value of sensitivity, PPV, NPV, Kappa value, and a larger area under the ROC curve. As we mentioned in the method, patients diagnosed with GIST in this study were all thought to meet the etiologic criterion. Thus, the consistency between NRS2002/MUST and GLIM criteria mainly depends on the comparison between the components of the two screening tools and the phenotypic indicators of GLIM criteria. Since NRS2002 is designed to screen patients who may benefit from nutritional support, the disease score of NRS2002 increased by 2 points if the patient planned to undergo major abdominal surgery. As a result, the patient would be classified as high malnutrition risk even without weight loss, low BMI, or reduced muscle mass, if he or she was ≥ 70 years old, which leads to poor consistency with GLIM criteria. A similar result was observed by Xu et al. in surgical patients that more than half of patients with malnutrition risk screened by NRS2002 did not meet the GLIM criteria for malnutrition (25). In the previous studies, MUST was found to have a high sensitivity and specificity and excellent diagnostic accuracy for the identification of malnutrition in patients with geriatric gastrointestinal cancer and patients with colorectal cancer (13, 26). In this study, MUST was also found to have good consistency with GLIM criteria for malnutrition diagnosis in surgical GIST inpatients. However, malnutrition risk classified by MUST did not show a correlation with the length of postoperative hospital stay or the occurrence of complications in this study. For these reasons, the predictive value of MUST for clinical outcomes in surgical GIST inpatients needs to be further verified in combination with other meaningful health outcomes associated with malnutrition.
The strength of our study is that hospitalized patients with GIST were divided into surgical and non-surgical inpatients to compare the suitability of NRS2002 and MUST as the first-step screening tool for GLIM criteria in view of the screening and predictive performance of the two risk-screening tools. In our study, different results were obtained for surgical and non-surgical inpatients, and it may provide a better reference for clinical practice by considering both the screening and predictive performance of these two tools.
As the limitation of this study, the etiologic components of the GLIM criteria were determined only based on the cancer diagnosis without a clarification of disease severity and the reduction of food intake or assimilation, which may have some impacts on the results. Thus, we plan to carry out a prospective study to find a more accurate diagnostic combination in the future since different combinations of phenotypic and etiologic criteria can identify malnutrition according to GLIM criteria. In addition, we did not investigate the relationships between the malnutrition risk classified by NRS2002 or MUST and other indicators for clinical outcomes, such as survival time and mortality, in patients with GIST, which would be implemented after we collect enough data.
The malnutrition risk is common in GIST inpatients. NRS2002 is more suitable than MUST for the first-step risk screening of the GLIM scheme in non-surgical inpatients, considering its better performance in screening malnutrition risk and predicting clinical outcomes. MUST was found to have good diagnostic consistency with GLIM criteria for malnutrition in both non-surgical and surgical GIST inpatients, and further studies need to be carried out to investigate its predictive performance on clinical outcomes.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by the Medical Ethical Committee of the First Affiliated Hospital of Chongqing Medical University. The patients/participants provided their written informed consent to participate in this study.
JLi contributed to conception, design, administration, validation, writing, and editing of the manuscript. XZ contributed to writing, malnutrition risk screening, and assessment. JLiu and XW contributed to data collection and analysis. QZ contributed to body composition measurement. SR contributed to weight and height measurements. JZ contributed to the provision of patients. All authors contributed to the article and approved the submitted version.
This work was supported by the Chongqing Municipal Health Commission (grant number: 2021MSXM335).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The authors would thank all members who participated in the diagnosis and treatment of patients with gastrointestinal stromal tumor in the First Affiliated Hospital of Chongqing Medical University.
1. von Mehren M, Joensuu H. Gastrointestinal Stromal Tumors. J Clin Oncol. (2018) 36:136–43. doi: 10.1200/JCO.2017.74.9705
2. Ge XY, Lei LW, Ge F, Jiang X. Analysis of risk factors of gastrointestinal stromal tumors in different age groups based on SEER database. Scand J Gastroenterol. (2019) 54:480–4. doi: 10.1080/00365521.2019.1604798
3. Dou L, Wang X, Cao Y, Hu A, Li L. Relationship between Postoperative Recovery and Nutrition Risk Screened by NRS 2002 and Nutrition Support Status in Patients with Gastrointestinal Cancer. Nutr Cancer. (2020) 72:33–40. doi: 10.1080/01635581.2019.1612927
4. Shaw C. Management of diet in gastrointestinal cancer. Proc Nutr Soc. (2021) 80:65–72. doi: 10.1017/S0029665120007041
5. Zheng HL, Lu J, Li P, Xie JW, Wang JB, Lin JX, et al. Effects of Preoperative Malnutrition on Short- and Long-Term Outcomes of Patients with Gastric Cancer: Can We Do Better? Ann Surg Oncol. (2017) 24:3376–85. doi: 10.1245/s10434-017-5998-9
6. Maia FCP, Silva TA, Generoso SV, Correia MITD. Malnutrition is associated with poor health-related quality of life in surgical patients with gastrointestinal cancer. Nutrition. (2020) 75–6:110769. doi: 10.1016/j.nut.2020.110769
7. Arends J, Baracos V, Bertz H, Bozzetti F, Calder PC, Deutz NEP, et al. ESPEN expert group recommendations for action against cancer-related malnutrition. Clin Nutr. (2017) 36:1187–96. doi: 10.1016/j.clnu.2017.06.017
8. Garla P, Waitzberg DL, Tesser A. Nutritional Therapy in Gastrointestinal Cancers. Gastroenterol Clin North Am. (2018) 47:231–42. doi: 10.1016/j.gtc.2017.09.009
9. Mizukami T, Piao Y. Role of nutritional care and general guidance for patients with advanced or metastatic gastric cancer. Future Oncol. (2021) 17:3101-9. doi: 10.2217/fon-2021-0186
10. Lee H, Cho YS, Jung S, Kim H. Effect of nutritional risk at admission on the length of hospital stay and mortality in gastrointestinal cancer patients. Clin Nutr Res. (2013) 2:12–8. doi: 10.7762/cnr.2013.2.1.12
11. Cederholm T, Jensen GL, Correia MITD, Gonzalez MC, Fukushima R, Higashiguchi T, et al. GLIM criteria for the diagnosis of malnutrition - A consensus report from the global clinical nutrition community. Clin Nutr. (2019) 38:1–9. doi: 10.1016/j.clnu.2018.08.002
12. Poulia KA, Klek S, Doundoulakis I, Bouras E, Karayiannis D, Baschali A, et al. The two most popular malnutrition screening tools in the light of the new ESPEN consensus definition of the diagnostic criteria for malnutrition. Clin Nutr. (2017) 36:1130–5. doi: 10.1016/j.clnu.2016.07.014
13. Ye XJ, Ji YB, Ma BW, Huang DD, Chen WZ, Pan ZY, et al. Comparison of three common nutritional screening tools with the new European Society for Clinical Nutrition and Metabolism (ESPEN) criteria for malnutrition among patients with geriatric gastrointestinal cancer: a prospective study in China. BMJ Open. (2018) 8:e019750. doi: 10.1136/bmjopen-2017-019750
14. Kondrup J Allison SP Elia M Vellas B Plauth M; Educational and Clinical Practice Committee European European Society of Parenteral and Enteral Nutrition (ESPEN). ESPEN guidelines for nutrition screening 2002. Clin Nutr. (2003) 22:415–21. doi: 10.1016/S0261-5614 (03)00098-0
15. Stratton RJ, Hackston A, Longmore D, Dixon R, Price S, Stroud M, et al. Malnutrition in hospital outpatients and inpatients: prevalence, concurrent validity and ease of use of the ‘malnutrition universal screening tool' (‘MUST') for adults. Br J Nutr. (2004) 92:799-808. doi: 10.1079/BJN20041258
16. Clark AB, Reijnierse EM, Lim WK, Maier AB. Prevalence of malnutrition comparing the GLIM criteria, ESPEN definition and MST malnutrition risk in geriatric rehabilitation patients: RESORT. Clin Nutr. (2020) 39:3504–11. doi: 10.1016/j.clnu.2020.03.015
17. Zhang Z, Wan Z, Zhu Y, Zhang L, Zhang L, Wan H. Prevalence of malnutrition comparing NRS2002, MUST, and PG-SGA with the GLIM criteria in adults with cancer: a multi-center study. Nutrition. (2021) 83:111072. doi: 10.1016/j.nut.2020.111072
18. McHugh ML. Interrater reliability: the kappa statistic. Biochem Med (Zagreb). (2012) 22:276–82. doi: 10.11613/BM.2012.031
19. Ding P, Guo H, Yang P, Sun C, Tian Y, Liu Y, et al. Association Between the Nutritional Risk and the Survival Rate in Newly Diagnosed GIST Patients. Front Nutr. (2021) 8:743475. doi: 10.3389/fnut.2021.743475
20. Yin YQ, Liu CJ, Liu LR, Zhong J, Wen Y, Wu XT. Screening of nutritional risk in hospital patients with gastrointestinal stromal tumors (Article in Chinese). Parenter Enteral Nutr. (2014) 21:211–3. doi: 10.16151/j.1007-810x.2014.04.020
21. Borges LSR. Diagnostic Accuracy Measures in Cardiovascular Research. Int J Cardiovasc Sci. (2016) 29:218–22. doi: 10.5935/2359-4802.20160030
22. de van der Schueren MAE, Keller H; GLIM Consortium, Cederholm T, Barazzoni R, Compher C, et al. Global Leadership Initiative on Malnutrition (GLIM): Guidance on validation of the operational criteria for the diagnosis of protein-energy malnutrition in adults. Clin Nutr. (2020) 39:2872–80. doi: 10.1016/j.clnu.2019.12.022
23. Qiu M, Zhou YX, Jin Y, Wang ZX, Wei XL, Han HY, et al. Nutrition support can bring survival benefit to high nutrition risk gastric cancer patients who received chemotherapy. Support Care Cancer. (2015) 23:1933–9. doi: 10.1007/s00520-014-2523-6
24. Hersberger L, Bargetzi L, Bargetzi A, Tribolet P, Fehr R, Baechli V, et al. Nutritional risk screening (NRS 2002) is a strong and modifiable predictor risk score for short-term and long-term clinical outcomes: secondary analysis of a prospective randomised trial. Clin Nutr. (2020) 39:2720–9. doi: 10.1016/j.clnu.2019.11.041
25. Xu JY, Zhang XN, Jiang ZM, Jie B, Wang Y, Li W, et al. Nutritional support therapy after GLIM criteria may neglect the benefit of reducing infection complications compared with NRS2002: Reanalysis of a cohort study. Nutrition. (2020) 79–80:110802. doi: 10.1016/j.nut.2020.110802
Keywords: gastrointestinal stromal tumor (GIST), malnutrition, malnutrition risk, Global Leadership Initiative on Malnutrition (GLIM), Nutritional Risk Screening 2002 (NRS2002), Malnutrition Universal Screening Tool (MUST)
Citation: Zhou X, Liu J, Zhang Q, Rao S, Wu X, Zhang J and Li J (2022) Comparison of the Suitability Between NRS2002 and MUST as the First-Step Screening Tool for GLIM Criteria in Hospitalized Patients With GIST. Front. Nutr. 9:864024. doi: 10.3389/fnut.2022.864024
Received: 28 January 2022; Accepted: 02 March 2022;
Published: 11 April 2022.
Edited by:
Harriët Jager-Wittenaar, Hanze University of Applied Sciences, NetherlandsReviewed by:
Nicole Kiss, Deakin University, AustraliaCopyright © 2022 Zhou, Liu, Zhang, Rao, Wu, Zhang and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Juan Li, enBmaXJzdEBzaW5hLmNvbQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.