- 1Department of Medicine, University of Udine, Udine, Italy
- 2School of Sport Sciences, University of Udine, Udine, Italy
- 3Experimental Laboratory for Auxo-Endocrinological Research, Istituto Auxologico Italiano, Scientific Institute for Hospitalization and Care (IRCCS), Piancavallo, Italy
- 4Division of Auxology, Istituto Auxologico Italiano, Scientific Institute for Hospitalization and Care (IRCCS), Piancavallo, Italy
Background: The aim of the present study was to examine the short-term changes in body composition and physical capabilities in subjects with obesity during a multidisciplinary inpatient body weight reduction program (BWRP).
Methods: One hundred thirty-nine adolescents (56 boys and 83 girls; BMI: 37.1 ± 6.5 kg/m2; Fat Mass, FM: 45.3 ± 7.2%) and 71 adults (27 males and 44 females; BMI: 44 ± 4.7 kg/m2; FM: 51.4 ± 4.7%) followed a 3-week inpatient BWRP consisting of regular physical activity, moderate energy restriction, nutritional education and psychological counseling. Before (T0) and after the end of the BWRP (T21), body composition was assessed with an impedancemeter, lower limb muscle power with Margaria Stair Climbing Test (SCT), lower limb functionality with Short Physical Performance Battery (SPPB), and the capacity of performing activity of daily living (ADL) with Physical Performance Test (PPT).
Results: At T21, obese adolescents showed a 4% reduction in body mass (BM) (p < 0.001), associated with a FM reduction in boys (−10%) and girls (−6%) (p < 0.001) and with a 3% reduction in fat-free mass (FFM) recorded only in boys (p = 0.013). Obese adults showed a 5% BM reduction (p < 0.001), associated with a 2% FFM and 9% FM reduction (p < 0.001) in males, and 7% FM reduction in females (p < 0.001). Regarding physical capabilities, at T21 in obese adolescents, PPT score increased by 4% (p < 0.001), SCT decreased by −5% (boys) and −7% (girls) (p < 0.001), while SPPB score did not change significantly. In obese adults at T21, PPT score increased by 9% (p < 0.001), SCT decreased by −16% (p < 0.001) only in females, and SPPB score increased by 7% (males) and 10% (females) (p < 0.01).
Conclusion: In conclusion, moderate energy restriction and regular physical activity determine a 4-5% BM reduction during a 3-week inpatient BWRP, improve physical capabilities and induce beneficial changes in body composition in adolescents and adults with obesity.
Trial registration: This study was approved by the Ethical Committee of the Istituto Auxologico Italiano (Milan, Italy; research code: 01C124; acronym: PRORIPONATFIS). Registered 11 November 2020 - Retrospectively registered.
Introduction
Over the past two decades, obesity has tripled in both children and adults in industrialized countries (1, 2), mainly due to the excess food-intake combined with an increase in time spent in sedentary activities, leading to a decrease in physical activity level (3–5). Excessive levels of body fat is associated with major health consequences associated with obesity, including hypertension (6–8), type 2 diabetes, and cardiovascular disease (9). In addition, reduced physical activity levels in adolescents and adults with obesity is reported to lead to a lower aerobic and anaerobic capacities, and lower limb muscle power output than their normal-weight counterparts (10–12). Consequently, obese subjects with high values of fat mass and poor physical abilities, usually suffer from lower limb functionality, higher perceived difficulty in performing physical exercise and activities of daily living (ADL) (13–16). Nevertheless, in obese subjects, short-term multidisciplinary inpatient body weight-reduction programs (BWRP) entailing moderate-intensity physical training, energy-restricted diets, and changes in food and behavioral habits have been reported to promote weight loss, reduce fat mass (FM) (17–19) and improve physical capacities. The improvements in body composition and physical capacities is reported to exert a positive effects on metabolic and cardiovascular risk profiles (20, 21), as well on both lower limb muscle power and functionality (17–19) and on performing ADL (13). However, the presence of a lower limb function and ability to perform ADL is often overlooked in adolescents and adults with obesity (22), even if their poor physical abilities actually worsen their quality of life, as it happens elderly obese (22).
Therefore, the aim of the present study was to determine whether a short-term (3-week) multidisciplinary BWRP entailing physical activity, moderate energy restriction, nutrition education, and psychological counseling, can positively affect body composition, lower limb muscle power and functionality, capacity of performing ADL in adolescents and adults with obesity.
Materials and Methods
Subjects
One hundred thirty-nine adolescents (56 boys and 83 girls; age range: 13–17 years) and 71 adults (27 males and 44 females; age range: 35–68 years) with obesity, participated in this study. Among adolescents, BMIs for gender and chronological age were above the 99th percentile (23), while for adults the BMIs were above 35 kg/m2. Subjects were recruited as inpatients from the Division of Auxology (subjects aged <18 year) and from the Division of Metabolic Diseases (subjects aged >18 years), Istituto Auxologico Italiano, IRCCS, Piancavallo (VB), Italy. Before admission to the hospital for BWRP, none of the subjects had engaged in structured physical activity (i.e., regular activity of more than 60 min/week) evaluated with the validated International Physical Activity Questionnaire Short Form (IPAQ-SF) (24). All subjects had a complete medical history and physical examination. None of the adolescents or adults with obesity had signs or symptoms indicative of serious cardiovascular, respiratory, or orthopedic disease that could significantly interfere with the functional test used in the study.
Study Protocol
The study was approved by the Ethical Committee of the Istituto Auxologico Italiano (Milan, Italy; research code: 01C124; acronym: PRORIPONATFIS) and was in accordance with the Declaration of Helsinki 1975, as revised in 2008. For adolescents, the protocol was explained to parents and written informed consent was obtained from parents or legal representatives. Patients aged ≥18 gave written informed consent to participate in the study. Patients were hospitalized for a period of 3 weeks in the Division of Auxology (patients <18 years) or in the Division of Metabolic Diseases (patients >18 years), Istituto Auxologico Italiano, IRCCS, Piancavallo (VB). They followed a 3-week personalized BWRP consisting of moderate energy restriction, physical activity, nutrition education, and psychological counseling. Full testing sessions were conducted at the beginning (T0) and at completion of the 3-week BWRP (T21). Testing session included assessment of anthropometric characteristics, body composition, blood pressure (BP), lower limb muscle power, lower limb functionality, and ability to perform ADL (see below for detailed description).
Physical Activity
The physical activity program consisted of five training days per week, under the supervision of a physical trainer. Each training session included: (i) 45–60 min per day of aerobic activities (walking on a treadmill or cycling on an ergometer) under heart rate monitoring (HR) and medical supervision and (ii) 5–7 min of stretching before and after training. The intensity of aerobic activities was set at heart rate (HR) corresponding to 60 and 80% of the individual maximal HR estimated as 220-age (year). The research assistant and the physical trainers verified that each subject participated in each training session, performed the exercises correctly, and completed at least 95% of the exercise session and program. In addition, subjects had 1 h/day of aerobic leisure activities at the institution on Saturday and Sunday.
Diet and Nutrition Education
A Mediterranean diet was prescribed based on the initial basal metabolic rate test and physical activity level for each patients, and the amount of energy to be given with diet was calculated by subtracting approximately ∼25% from the estimated daily energy expenditure. In terms of macronutrients, the diet contained 21% proteins, 53% carbohydrates, and 26% lipids. The diet composition was formulated according to the Italian recommended daily allowance (25). Each patient was free to choose foods from a heterogeneous daily menu, although five daily servings of fruits and vegetables were mandatory. Foods to which the patient reported allergic reactions were eliminated from the menu. A fluid intake of at least 1.5 L/day was encouraged. In addition, the dietitian team checked that each subject had eaten every meal. On each day of the BWRP, the patients had dietetics classes consisting of lectures, demonstrations, and group discussions with and without a supervisor.
Psychological Counseling
Cognitive-behavioral therapy strategies, such as stimulus control procedures, problem-solving and stress management training, development of healthy eating habits, assertiveness and social skills training, cognitive restructuring of negative maladaptive thoughts, and relapse prevention training, were chosen for the psychological sessions, which were conducted by a clinical psychologist 2–3 times per week in individual or group sessions as previously reported (26). When possible (1 day per week), additional sessions were also conducted with parents of the obese adolescents aimed at improving motivation for lifestyle change and interpersonal communication.
Measurements
Physical Characteristics and Body Composition
Medical history was obtained and a baseline physical examination was performed. Stature and body mass (BM) were measured using a Harpenden stadiometer (Holtain Ltd., United Kingdom), and an electronic scale (Selus, Italy), respectively, with the subject wearing only light underwear. BMI (kg/m2) was calculated. The standard deviation score (SDS) of BMI-SDS was calculated using the LMS method (23) on Italian reference values for children and adolescents (27). Body composition was measured using a multifrequency tetrapolar impedancemeter (BIA, Human-IM Scan, DS-Medigroup, Milan, Italy) with a delivered current of 800 μA at a frequency of 50 kHz. To reduce measurement errors, care was taken to standardize the variables that affect the validity, reproducibility and precision of the measurement. The measurements were performed according to the method of Lukaski et al. (28) (after 20 min of rest in the supine position with arms and legs relaxed and without contact with other parts of the body) and under strictly controlled conditions according to NIH guidelines (29). Before measurements, technical accuracy has been validated by an external parallel circuit containing a high-precision resistor and capacitor. Low-impedance electrodes were used for reliable and accurate assessment of the raw bioimpedance parameters (e.g., R, Xc, and phase angle) (30). The within-day coefficient of variation for three repeated assessments of FFM in obese subjects (with repositioning of electrodes) has been previously assessed in our laboratory (2.4%).
All females were studied outside of the menstrual period in order to avoid any possible influence on fluid retention, as suggested by the NIH guidelines (29). For the adolescents, Fat-Free Mass (FFM) was calculated using the prediction equation previously developed by our group against DEXA (31):
where, ZI is the impedance index calculated as stature (cm2) divided by whole-body impedance (Z) at 50 kHz (Ω). For the adults, we used the equation developed by Gray et al. (32):
FM (kg) was derived as the difference between BM (kg) and FFM (kg).
BP measurements were taken after the participants have rested in the sitting position for at least 5 min, the average of 2 BP readings was used for analysis.
Lower Limb Muscle Power
The Stairs Climbing Test (SCT) is a well-standardized procedure for measuring maximal anaerobic power in adolescents and adults with obesity (20, 33). Prior to administering the test, 2–3 practise trials were scheduled to allow subjects to gain sufficient confidence with the technique. Briefly, subjects were asked to climb an ordinary stair at the highest possible speed, according to their abilities. The stairs consisted of 13 steps of 15.3 cm each, so that a total vertical distance of 1.99 m was covered. An experimenter measured the time taken to complete the test using a digital stopwatch. SCT repeatability in obese subjects has been previously evaluated in our laboratory and the coefficient of variation between measurements was found to be lower than 5% (20).
Short Physical Performance Battery
A Short Physical Performance Battery (SPPB) (34, 35) was administered. The SPPB consists of the following three parts: (i) tests of standing balance, included semi-tandem position, side-by-side stands and tandem position (each held for 10 s), (ii) walking a 4 m distance at normal gait speed, and (iii) rising from a chair and returning to the seated position five times. Scores for each item ranged from 0 to 4, for a maximum of 12 points. Performance categories were created for each set of performance measures to allow for analyses that included those unable to perform a task. The three tests of standing balance were considered hierarchical in difficulty by assigning a single score from 0 to 4 for standing balance (35). For 4 m walking and repeated chair stands, a score of 0 was assigned to those who could not complete the task. Those who were able to complete the task were assigned scores from 1 up to 4, corresponding to quartiles of time required for the task, with the fastest times scored as 4 (35). Higher scores were associated with better lower limb functionality (34).
Physical Performance Test
The ability to perform ADL was assessed using the Physical Performance Test (PPT) (36). The PPT test used in the present study includes 7 standardized tasks [(i) walk 15.2 m, (ii) put on and take off a coat, (iii) pick up a coin, (iv) lift a book, (v) simulate the act of eating, (vi) perform a 360° turn, and (vii) write a sentence]. The score for each item ranged from 0 to 4, with 0 corresponding to “unable to do” and 4 corresponding to “most able or quickest” (36). The maximum score was 28, and participants were classified as mildly to moderately frail if they scored between 19 and 24 (37).
Statistical Analyses
Statistical analyses were performed using Graph Pad Prism version 9.1.0-2021 software (GraphPad Software, Inc., San Diego, CA, United States) with a significance set at p < 0.05. All results were expressed as mean and standard deviation (SD). Normal distribution of the data was tested using the Kolmogorov–Smirnov test. The effects of gender, time, and the interaction between these variables on physical characteristics, body composition, lower limb muscle power, lower limb functionality and ability to perform ADL were tested using General Linear Model repeated measures. When significant differences were found, a Bonferroni post hoc test was evaluated implementing multiple comparisons. Relationships between the different factors were examined using Pearson or Spearman product–moment correlation coefficient.
Results
Effects of the 3-Week BWRP in Adolescents
Anthropometric Characteristics and Body Composition
At T0, age, BM, BMI, and BMI-SDS were not significantly different between boys and girls, whereas stature was ∼5% higher in boys than girls (p < 0.001, Table 1). At the end of BWRP (T21), BM and BMI decreased by ∼4% (p < 0.001, Table 1) in both genders, a greater reduction (∼7%, p < 0.001, Table 1) being observed in BMI-SDS in both genders.
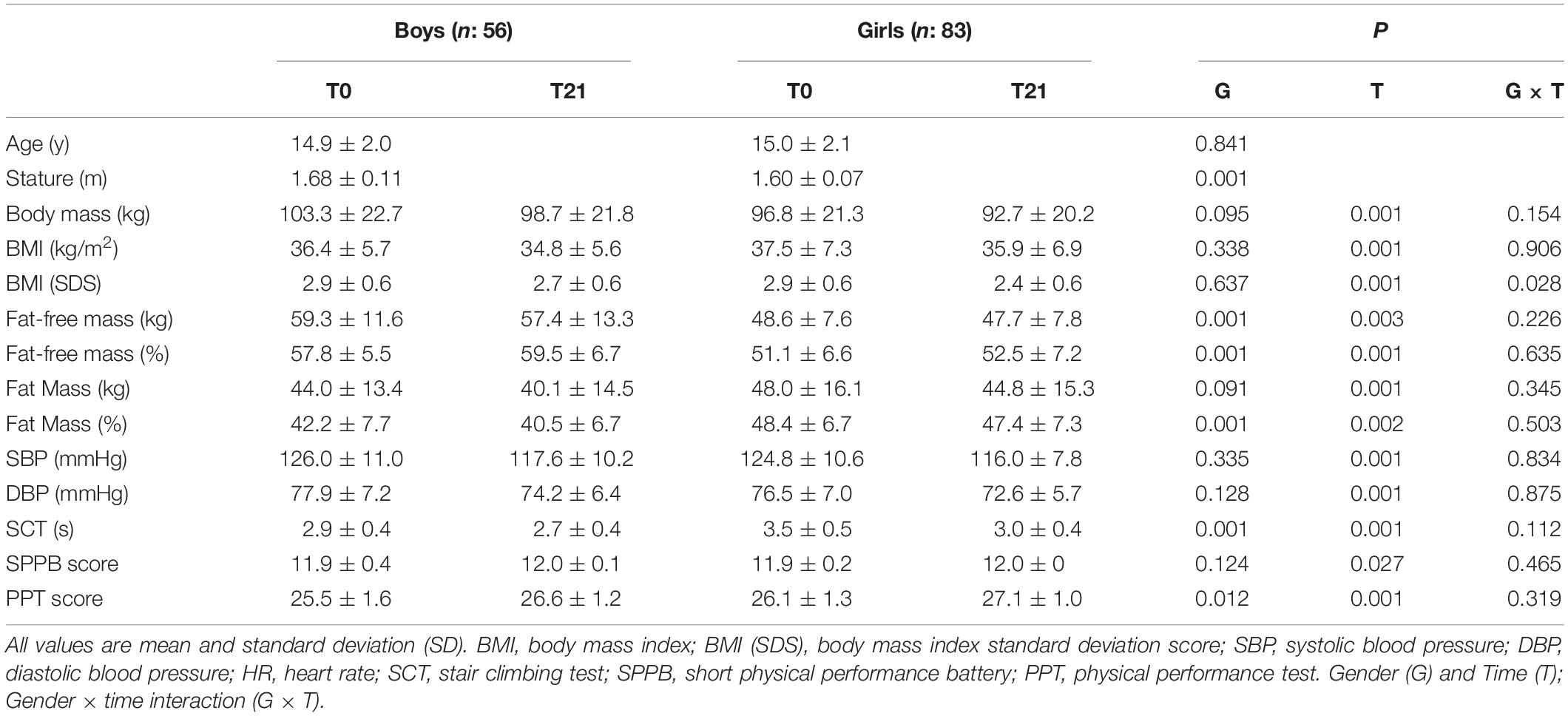
Table 1. Physical characteristics of adolescents with obesity before (T0) and after (T21) the 3-week BWRP.
At T0, FFM (kg) and FFM (%) were 22 and 13% higher in boys than in girls, respectively (p < 0.001, Table 1 and Figure 1A). Regarding FM (kg), no difference was found between boys and girls (Table 1 and Figure 1C), while FM expressed as a percentage was ∼15% (p < 0.001, Table 1) lower in boys than in girls. At T21, FFM (kg) decreased by 3% (p = 0.013, Table 1) in boys only (Figure 1B), while FFM (%) increased by ∼3 and ∼2% (p < 0.005, Table 1) in boys and girls, respectively. In contrast, FM (kg) decreased by ∼9 and ∼7% in boys and girls, respectively (p < 0.001, Table 1 and Figure 1D), with a smaller decrease when FM was expressed as a percentage (∼3 and ∼2% in boys and girls, respectively, p = 0.017, Table 1).
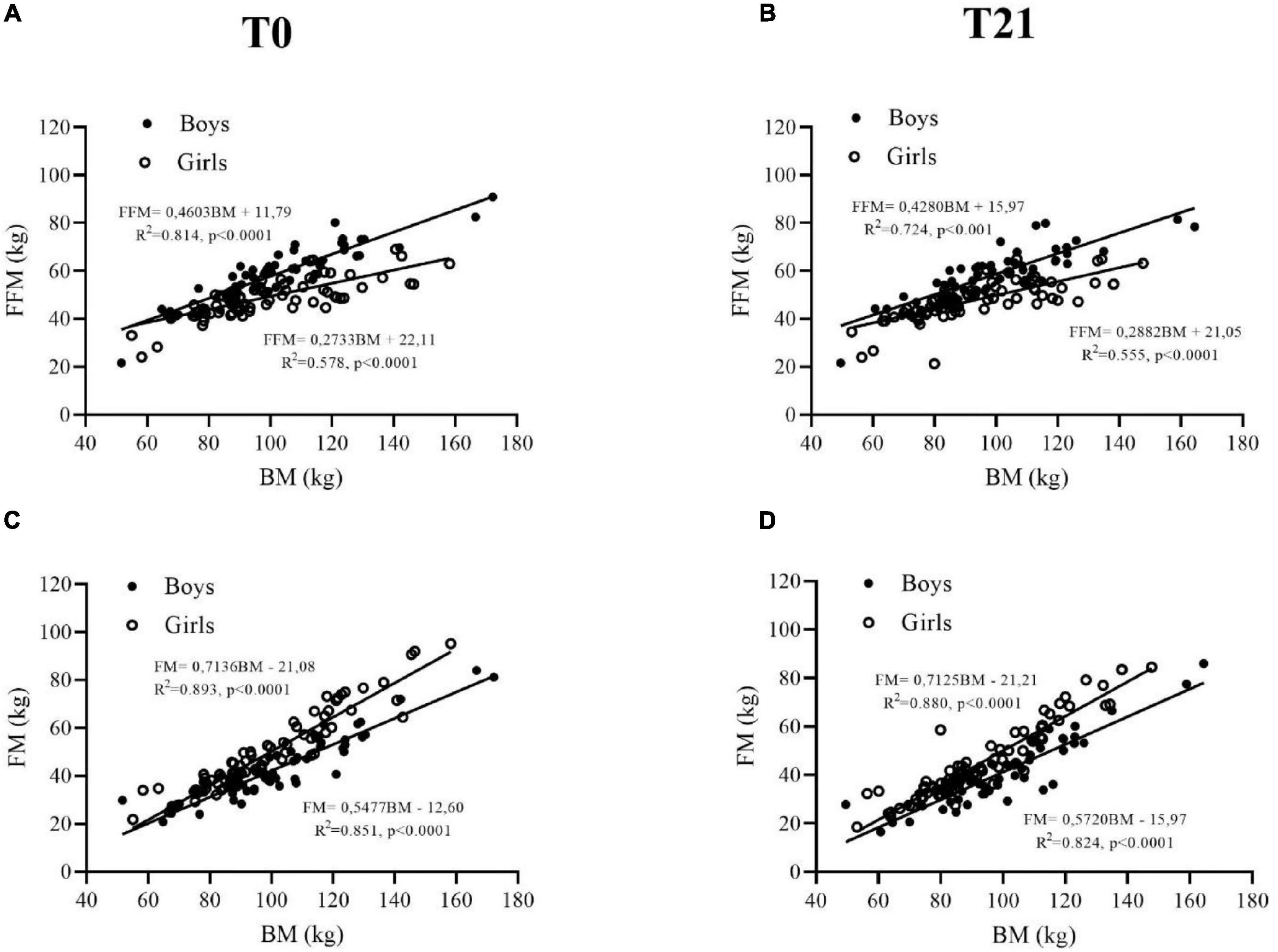
Figure 1. Fat-free mass (FFM) (A,B) and fat mass (FM) (C,D) are plotted as a function of body mass in adolescent obese boys (closed symbols) and girls (open symbols) before (T0) and after (T21) the 3-week BWRP.
At T0, systolic BP and diastolic BP were not significantly different between boys and girls (Table 1). At T21, systolic BP and diastolic BP decreased by ∼7% in both genders (p < 0.001, Table 1).
Physical Capabilities
At T0, SCT and PPT scores were ∼11 and ∼3% lower in boys than in girls, respectively (p < 0.05, Table 1), while SPPB did not differ significantly between boys and girls (Table 1). At T21, SCT decreased by ∼5 and ∼7% (p < 0.001) in boys and girls, respectively. While PPT score increased by ∼4% (p < 0.001, Table 1) in both boys and girls. The SPPB score did not change significantly in both genders (Table 1).
Changes in FM (ΔFM) (kg) were not related to changes in SCT (ΔSCT), SPPB (ΔSPPB), PPT (ΔPPT, score), systolic BP (ΔSBP), and diastolic BP (ΔDBP) in both boys and girls (Table 2).
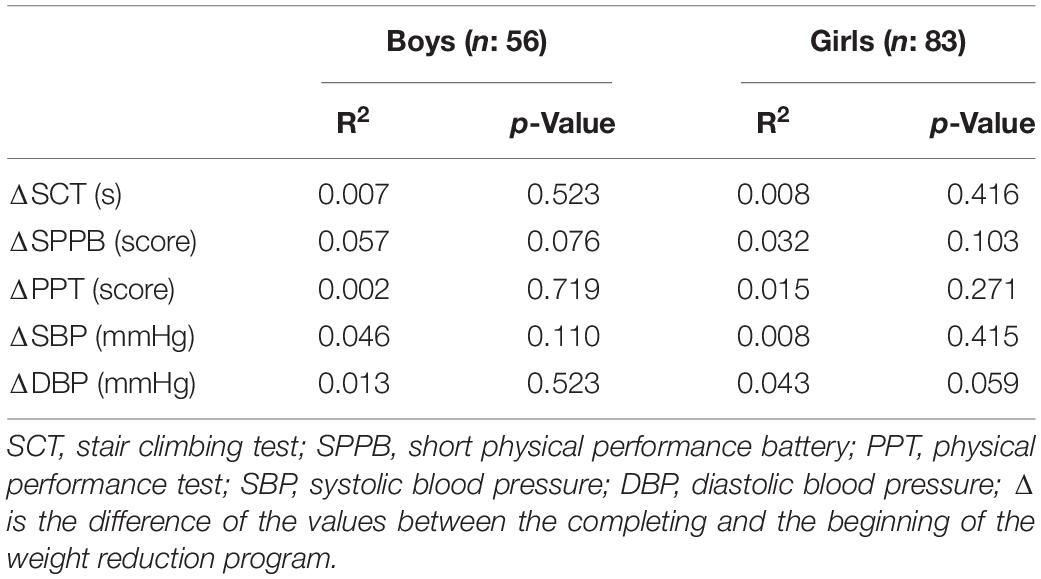
Table 2. Linear regression between changes in Fat Mass (ΔFM) (kg) in adolescents with obesity and possible predictors.
Effects of the 3-Week BWRP on Adults
Anthropometric Characteristics and Body Composition
At T0, mean age and BMI did not differ significantly between males and females (Table 3), whereas stature and BM were significantly higher in males than females by ∼7 and ∼10%, respectively (p < 0.005, Table 3). At T21, BM and BMI decreased by ∼5 and ∼4% (p < 0.001, Table 3) in males and females, respectively.
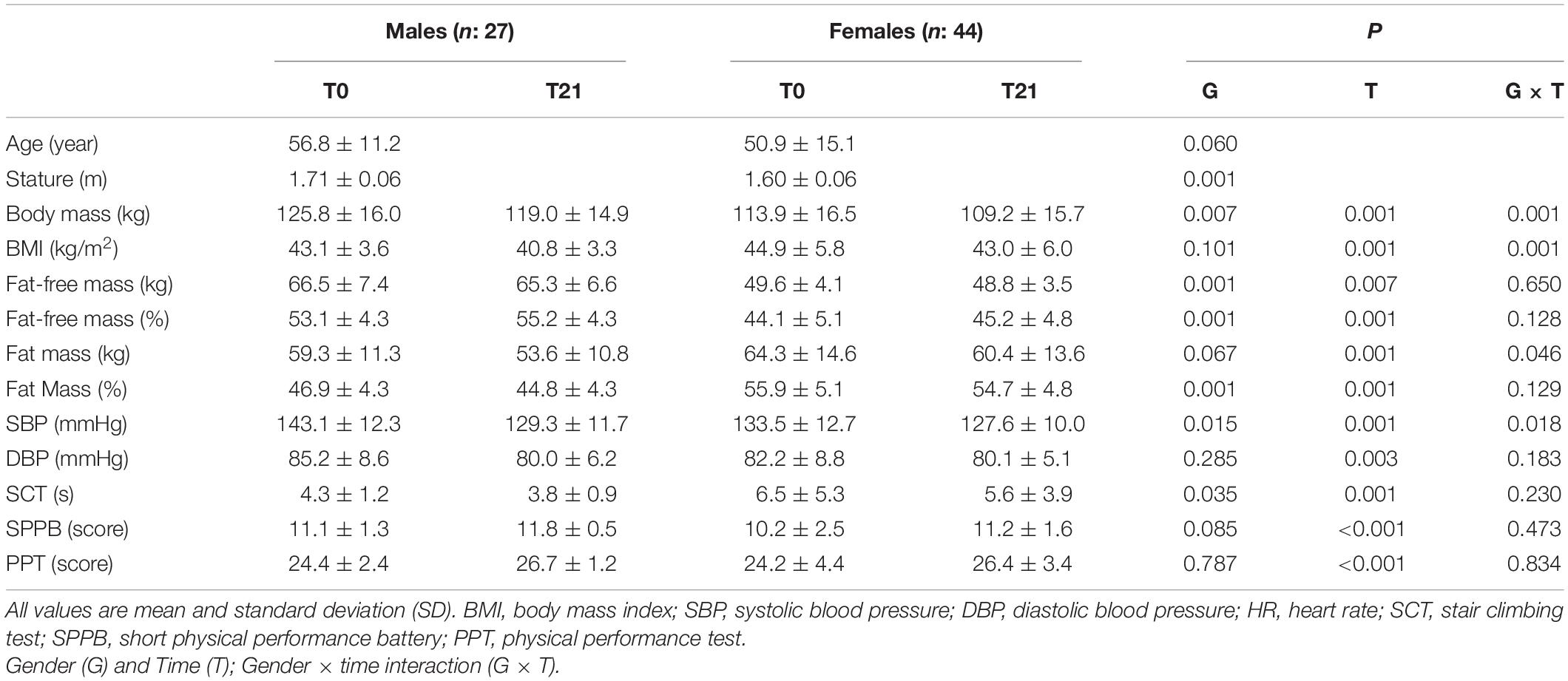
Table 3. Physical characteristics of adults with obesity before (T0) and after (T21) the 3-week BWRP.
At T0, FFM (kg) and FFM (%) were higher in males than females (+25% and +17%, respectively, p < 0.001), as shown in Table 3 and Figure 2A. FM (kg) was not significantly different between males and females (p = 0.240, Table 3 and Figure 2C), whereas males showed lower FM (%) than females (-16%, p = 0.001, Table 3). At T21, FFM (kg) decreased by ∼2% in males and females with significant time interaction (p = 0.007) (Table 3 and Figure 2B), while FFM (%) increased in males (∼4%, p < 0.001) and females (∼3%, p = 0.012) (Table 3). FM (kg) decreased by ∼10 and ∼6% in males and females, respectively (p < 0.001, Table 3 and Figure 2D), although a decrease was also observed when FM was expressed as a percentage, in both males (∼5%, p = 0.002) and females (∼2%, p = 0.012) (Table 3).
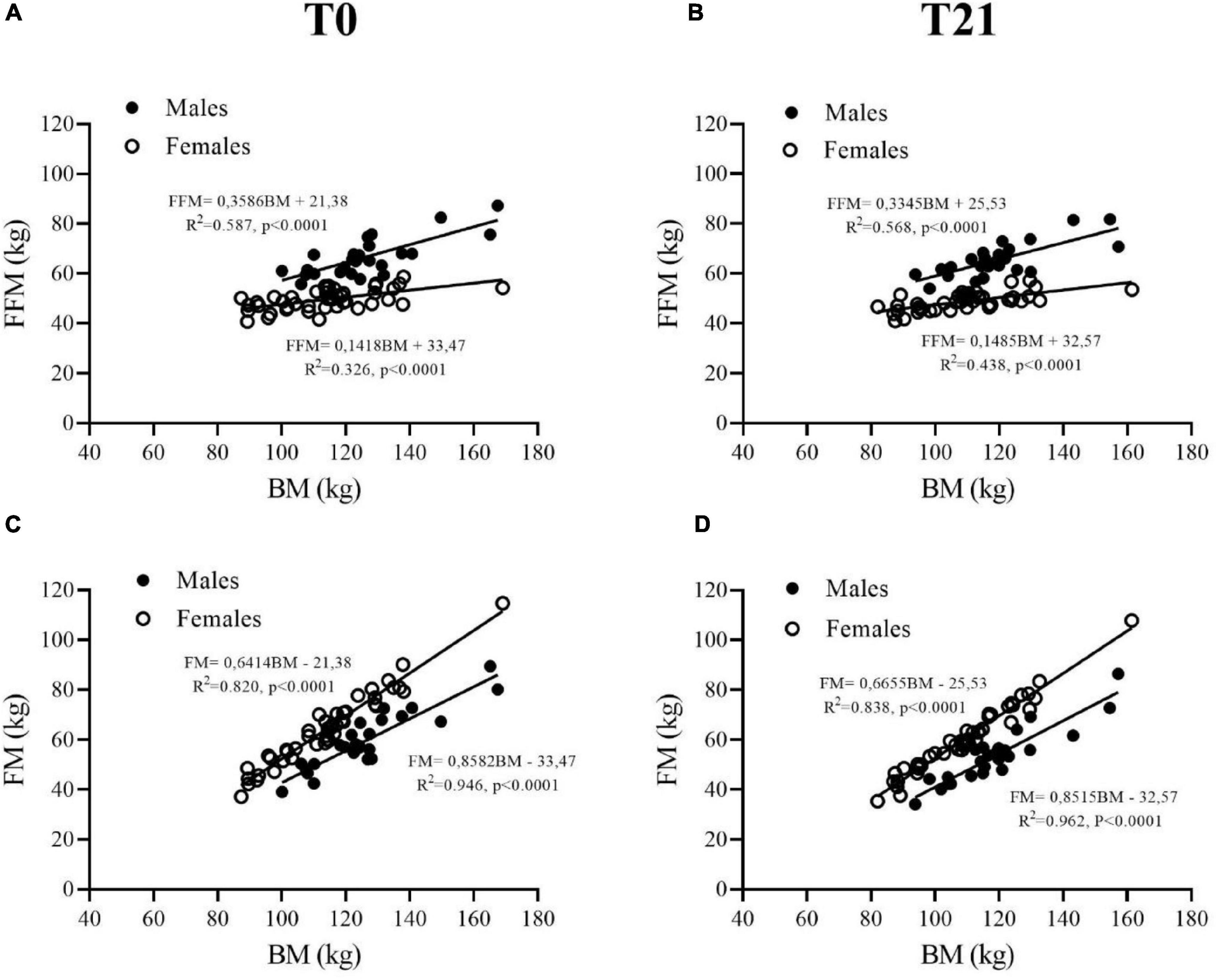
Figure 2. Fat free mass (FFM) (A,B) and fat mass (FM) (C,D) are plotted as a function of body mass (BM) in adult obese males (closed symbols) and females (open symbols) before (T0) and after (T21) of the 3-week BWRP.
At T0, systolic BP at rest was greater in males (+7%, p = 0.001, Table 3) than in females, while diastolic BP did not differ significantly between the two genders. At T21, systolic BP at rest reduced significantly in both males (∼10%, p = 0.001) and females (∼5%, p = 0.010, Table 3), while diastolic BP reduced significantly by ∼6% in males only (p = 0.012, Table 3).
Physical Capabilities
At baseline, SCT was lower in males than females by ∼5% (p = 0.042), whereas SPPB and PPT scores were not significantly different between the two genders (Table 3).
At T21, SCT decreased significantly only in females by ∼16% (p < 0.001, Table 3). SPPB score increased by ∼7 and ∼10% (p < 0.010, Table 3) in males and females, respectively. Similarly, PPT score increased by mean 9% (p < 0.001, Table 3) in the two genders.
Changes in FM (ΔFM) (kg) were inversely related to changes in both systolic BP (ΔSBP) (R2 = 0.242, p = 0.009; Table 4) and diastolic BP (ΔDBP) (R2 = 0.203, p = 0.009; Table 4) in males. In obese females, changes in FM (ΔFM) (kg) were inversely related to changes in both SPPB (ΔSPPB) (R2 = 0.345, p < 0.001; Table 4) and PPT (ΔPPT) (R2 = 0.187, p = 0.003; Table 4).
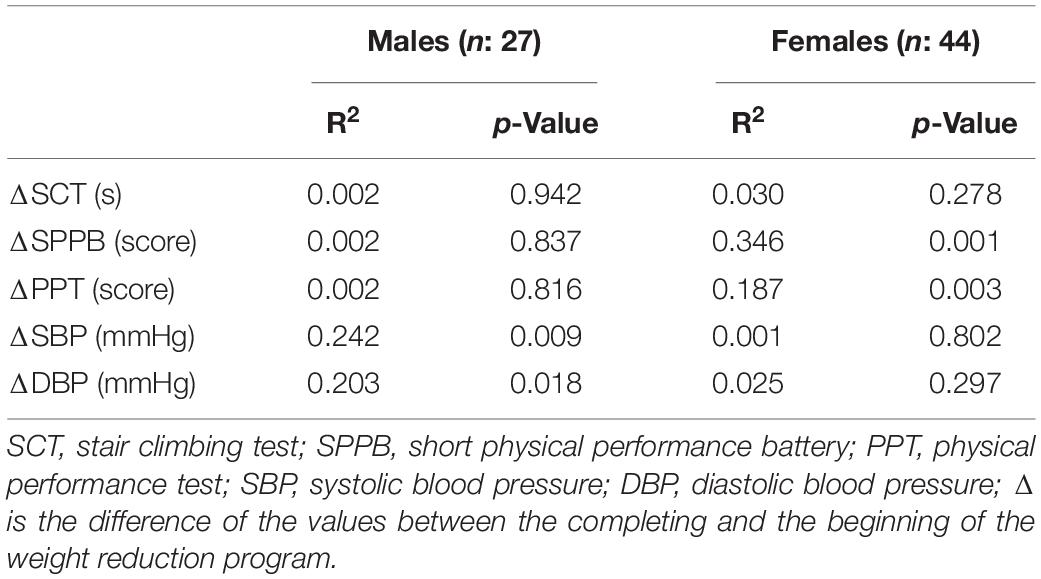
Table 4. Linear regression between changes in Fat Mass (ΔFM) (kg) in adults with obesity and possible predictors.
Discussion
The present study shows that a 3-week inpatient multidisciplinary BWRP, which includes physical training, moderate energy restriction, nutrition education, and psychological counseling, determines in adolescents and adults with obesity: (1) a significant reduction in BM and FM with a slight decrease in FFM, (2) improvements in SCT time, SPPB score in adults and PPT score in both groups, and (3) a positive relationship between reduction in FM and reduction in systolic BP and diastolic BP in obese male adults.
Our intervention was effective in reducing BM and FM for both adolescents and adults with obesity, in agreement with previous results reported in our laboratory after 3-week inpatient BWRP for patients aged 8–17 years (38, 39) and even for older obese male and females aged 61–75 year (40), confirming that body composition can be improved in obese individuals at any age. However, during the short-term BWRP adolescents and adults with obesity have shown a slight reduction in FFM, probably because no specific strength training was considered in this first phase of metabolic rehabilitation of patients with obesity, as previously observed (41).
After a 3-week of BWRP, SCT time was reduced after the BWRP in adolescents and in female, evaluated with the modified Margaria test (42) previously used to assess lower limb muscle power in obese subjects (43). Although there was no direct correlation between the BM reduction and the improvement in SCT time, as previously observed by our research group (17), it seems plausible to hypothesize that the reduction of BM may be associated with reduced body inertia (44) and the reduction of intramyocellular lipids may have played a role in the improvement of lower limb strength evaluated in our study by SCT (45). SPPB is a test useful for assessing lower limb functionality (static balance, 4 m walking and lower limb strength) (46). In our study, although SPPB scores were at the upper limit of normality (i.e., in the range of 11–12 points) (34), improvements of ∼0.8 and ∼1 points were found for male and female obese adults after 3-week BWRP, whereas smaller improvements, albeit statistically significant, were found in obese adolescents. In this regard, our findings are relevant because multidisciplinary 3-week BWRP appears to positively affect lower limb functionality in tasks such as walking and in those requiring getting up and down from a chair, which are typically impaired in obese patients (47–49), thus contributing to improve their quality of life. PPT is useful in assessing functional capabilities as it mimics ADL (36, 50–52). Previous studies showed that obese subjects had perceived difficulty in performing physical exercise and ADL (13–16). In the present study, the PPT score increased in both obese adolescents and adults, thus suggesting that a structured exercise program administered during a 3-week BWRP can improve the ability to perform ADL. Our findings are consistent with those recently reported by Wilson et al. (53), showing that regular physical activity and moderate energy restriction have positive effects on physical performance and quality of life. Furthermore, the improvements in SPPB and PPT scores in adult obese females were positively correlated with FM loss. At T0, mean SPPB and PPT scores in our obese females were lower than 11 and 28, respectively, and these two scores are considered signs of poor lower limb functionality (54, 55). Several factors have been considered to explain lower limb physical performance in females compared to males, such as lower muscle strength (56), higher body fat (56), lower muscle mass (57), and greater muscle fat infiltration (58) with the greatest adipose tissue thickness in the lower limbs (59).
Finally, reduction of FM was positively related to a reduction in systolic BP and diastolic BP only in obese males. Indeed, visceral adiposity is generally higher in obese male adults than in female counterparts (45), and visceral fat has been linked to the secretion of adipocytokines, that contribute to the development and progression of hypertension (60). Thus, BWRP has proven to be effective in improvement cardio metabolic profile of obese males (61). However, since we did not directly measured visceral adiposity, this missing information can be considered a limitation of the present study. Future studies involving BWRP in the hospital environment should measure visceral adiposity not only in relation to cardiovascular risk profile, but also as a marker of quality of life improvement in adolescents and adults with obesity.
Conclusion
In conclusion, our study confirms that a 3-week inpatient multidisciplinary BWRP, even if it only detects a 4–5% reduction in BM, is able to induce a significant reduction in FM, improvements in lower limb functionality and lower limb muscle power, and improvements in performing ADL, all of which are positive changes highly relevant to improve quality of life of adolescents and adults with obesity.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics Statement
The studies involving human participants were reviewed and approved by Ethical Committee of the Istituto Auxologico Italiano (Milan, Italy). Written informed consent to participate in this study was provided by the participants’ legal guardian/next of kin.
Author Contributions
AS, SL, MD’A, and FV: conceptualization. AS, MD’A, SL, FV, GT, and RD: data curation. FV and MD’A: formal analysis. AS: funding acquisition, project administration, and supervision. GT and RD: investigation. MD’A: writing original draft. AS, MD’A, SL, and FV: writing, review and editing. All authors have read and agreed to the published version of the manuscript.
Funding
Research funded by the Italian Ministry of Health.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We are grateful to adolescents (and their parents) and adults for participating in the present study, to the nursing staff at the Division of Auxology and at the Division of Metabolic Diseases, Istituto Auxologico Italiano, IRCCS, Piancavallo (VB) for their qualified assistance during the execution of the functional tests.
Abbreviations
ADL, activities of daily living; BM, body mass; BMI, body mass index; BMI (SDS), body mass index standard deviation score; BP, blood pressure; BWRP, body weight-reduction programs; DBP, diastolic blood pressure; HR, heart rate; PPT, physical performance test; SBP, systolic blood pressure; SCT, stair climbing test; SPPB, short physical performance battery.
References
1. Cancela Carral J, Ayán C, Sturzinger L, Gonzalez G. Relationship between body mass index and static and dynamic balance in active and inactive older adults. J Geriatr Phys Ther. (2018) 42:1. doi: 10.1519/JPT.0000000000000195
2. Inoue Y, Qin B, Poti J, Sokol R, Gordon-Larsen P. Epidemiology of obesity in adults: latest trends. Curr Obes Rep. (2018) 7:276–88. doi: 10.1007/s13679-018-0317-8
3. Guthold R, Stevens GA, Riley LM, Bull FC. Worldwide trends in insufficient physical activity from 2001 to 2016: a pooled analysis of 358 population-based surveys with 1•9 million participants. Lancet Glob Health. (2018) 6:e1077–86. doi: 10.1016/s2214-109x(18)30357-7
4. Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair-Rohani H, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the global burden of disease study 2010. Lancet. (2012) 380:2224–60. doi: 10.1016/s0140-6736(12)61766-8
5. Swinburn B. Commentary: physical activity as a minor player in the obesity epidemic: what are the deep implications? Int J Epidemiol. (2013) 42:1838–40. doi: 10.1093/ije/dyt162
6. Brady TM. Obesity-related hypertension in children. Front Pediatr. (2017) 5:197. doi: 10.3389/fped.2017.00197
7. Henry SL, Barzel B, Wood-Bradley RJ, Burke SL, Head GA, Armitage JA. Developmental origins of obesity-related hypertension. Clin Exp Pharm Phys. (2012) 39:799–806. doi: 10.1111/j.1440-1681.2011.05579.x
8. Kannel WB, Higgins M. Smoking and hypertension as predictors of cardiovascular risk in population studies. J Hypertens Suppl. (1990) 8:S3–8.
9. Faulkner JL, Belin de Chantemèle EJ. Sex differences in mechanisms of hypertension associated with obesity. Hypertension. (2018) 71:15–21. doi: 10.1161/HYPERTENSIONAHA.117.09980
10. Loftin M, Sothern M, Trosclair L, O’Hanlon A, Miller J, Udall J. Scaling VO(2) peak in obese and non-obese girls. Obes Res. (2001) 9:290–6. doi: 10.1038/oby.2001.36
11. Thivel D, Isacco L, Lazaar N, Aucouturier J, Ratel S, Doré E, et al. Effect of a 6-month school-based physical activity program on body composition and physical fitness in lean and obese schoolchildren. Eur J Pediatr. (2011) 170:1435–43. doi: 10.1007/s00431-011-1466-x
12. Török K, Szelényi Z, Pórszász J, Molnár D. Low physical performance in obese adolescent boys with metabolic syndrome. Int J Obes Relat Metab Disord. (2001) 25:966–70. doi: 10.1038/sj.ijo.0801646
13. Backholer K, Wong E, Freak-Poli R, Walls HL, Peeters A. Increasing body weight and risk of limitations in activities of daily living: a systematic review and meta-analysis. Obes Rev. (2012) 13:456–68. doi: 10.1111/j.1467-789X.2011.00970.x
14. Tareque MdI, Saito Y, Chan A, Visaria A, Ma S, Malhotra R. Years of life with and without limitation in physical function and in activities of daily living by body mass index among older adults. Int J Obes. (2019) 43:2244–53. doi: 10.1038/s41366-019-0370-8
15. Vásquez E, Batsis JA, Germain CM, Shaw BA. Impact of obesity and physical activity on functional outcomes in the elderly: data from NHANES 2005-2010. J Aging Health. (2014) 26:1032–46. doi: 10.1177/0898264314535635
16. Valerio G, Licenziati MR, Manco M, Ambruzzi AM, Bacchini D, Baraldi E, et al. [Health consequences of obesity in children and adolescents]. Minerva Pediatr. (2014) 66:381–414.
17. Rigamonti AE, Cicolini S, Caroli D, De Col A, Scacchi M, Cella SG, et al. Effects of a 3-week in-hospital body weight reduction program on cardiovascular risk factors, muscle performance, and fatigue: a retrospective study in a population of obese adults with or without metabolic syndrome. Nutrients. (2020) 12:1495. doi: 10.3390/nu12051495
18. Sartorio A, Agosti F, De Col A, Lafortuna CL. Age- and gender-related variations of leg power output and body composition in severely obese children and adolescents. J Endocrinol Invest. (2006) 29:48–54. doi: 10.1007/BF03349176
19. Scott D, Shore-Lorenti C, McMillan LB, Mesinovic J, Clark RA, Hayes A, et al. Calf muscle density is independently associated with physical function in overweight and obese older adults. J Musculoskelet Neuronal Interact. (2018) 18:9–17.
20. Sartorio A, Narici MV, Fumagalli E, Faglia G, Lafortuna CL. Aerobic and anaerobic performance before and after a short-term body mass reduction program in obese subjects. Diabetes Nutr Metab. (2001) 14:51–7.
21. Roberts CK, Lee MM, Katiraie M, Krell SL, Angadi SS, Chronley MK, et al. Strength fitness and body weight status on markers of cardiometabolic health. Med Sci Sports Exerc. (2015) 47:1211–8. doi: 10.1249/MSS.0000000000000526
22. Stephenson J, Smith CM, Kearns B, Haywood A, Bissell P. The association between obesity and quality of life: a retrospective analysis of a large-scale population-based cohort study. BMC Public Health. (2021) 21:1990. doi: 10.1186/s12889-021-12009-8
23. Cole TJ, Bellizzi MC, Flegal KM, Dietz WH. Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ. (2000) 320:1240–3. doi: 10.1136/bmj.320.7244.1240
24. Craig CL, Marshall AL, Sjöström M, Bauman AE, Booth ML, Ainsworth BE, et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. (2003) 35:1381–95. doi: 10.1249/01.MSS.0000078924.61453.FB
25. Nutrition ISo. Recommended Levels of Energy and Nutri-ents Intake for the Italian Population (LARN). New York, NY: Edra Medical Publishing and New Media M (1996).
26. Lazzer S, Bravo G, Tringali G, de Micheli R, de Col A, Sartorio A. A 3-week multidisciplinary body weight reduction program improves body composition and lower limb power output in 3,778 severely obese children and adolescents. Front Physiol. (2020) 11:548. doi: 10.3389/fphys.2020.00548
27. Cacciari E, Milani S, Balsamo A, Dammacco F, De Luca F, Chiarelli F, et al. Italian cross-sectional growth charts for height, weight and BMI (6-20 y). Eur J Clin Nutr. (2002) 56:171–80. doi: 10.1038/sj.ejcn.1601314
28. Lukaski HC, Bolonchuk WW, Hall CB, Siders WA. Validation of tetrapolar bioelectrical impedance method to assess human body composition. J Appl Physiol. (1986) 60:1327–32. doi: 10.1152/jappl.1986.60.4.1327
29. NIHT. Bioelectrical impedance analysis in body composition measurement: national institutes of health technology assessment conference statement. Am J Clin Nutr. (1996) 64:524S–32S. doi: 10.1093/ajcn/64.3.524S
30. Lukaski H, Raymond-Pope CJ. New frontiers of body composition in sport. Int J Sports Med. (2021) 42:588–601. doi: 10.1055/a-1373-5881
31. Lazzer S, Bedogni G, Agosti F, De Col A, Mornati D, Sartorio A. Comparison of dual-energy X-ray absorptiometry, air displacement plethysmography and bioelectrical impedance analysis for the assessment of body composition in severely obese Caucasian children and adolescents. Br J Nutr. (2008) 100:918–24. doi: 10.1017/S0007114508922558
32. Gray DS, Bray GA, Gemayel N, Kaplan K. Effect of obesity on bioelectrical impedance. Am J Clin Nutr. (1989) 50:255–60. doi: 10.1093/ajcn/50.2.255
33. Sartorio A, Proietti M, Marinone P, Agosti F, Adorni F, Lafortuna C. Influence of gender, age and BMI on lower limb muscular power output in a large population of obese men and women. Int J Obes Relat Metab Disord. (2004) 28:91–8. doi: 10.1038/sj.ijo.0802433
34. Ostir GV, Volpato S, Fried LP, Chaves P, Guralnik JM. Reliability and sensitivity to change assessed for a summary measure of lower body function: results from the women’s health and aging study. J Clin Epidemiol. (2002) 55:916–21. doi: 10.1016/s0895-4356(02)00436-5
35. Guralnik JM, Simonsick EM, Ferrucci L, Glynn RJ, Berkman LF, Blazer DG, et al. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. (1994) 49:M85–94. doi: 10.1093/geronj/49.2.m85
36. Reuben DB, Siu AL. An objective measure of physical function of elderly outpatients. The physical performance test. J Am Geriatr Soc. (1990) 38:1105–12. doi: 10.1111/j.1532-5415.1990.tb01373.x
37. Brown M, Sinacore DR, Binder EF, Kohrt WM. Physical and performance measures for the identification of mild to moderate frailty. J Gerontol A Biol Sci Med Sci. (2000) 55:M350–5. doi: 10.1093/gerona/55.6.m350
38. Lazzer S, Lafortuna C, Busti C, Galli R, Agosti F, Sartorio A. Effects of low- and high-intensity exercise training on body composition and substrate metabolism in obese adolescents. J Endocrinol Invest. (2011) 34:45–52. doi: 10.1007/BF03346694
39. Maffiuletti NA, De Col A, Agosti F, Ottolini S, Moro D, Genchi M, et al. Effect of a 3-week body mass reduction program on body composition, muscle function and motor performance in pubertal obese boys and girls. J Endocrinol Invest. (2004) 27:813–20. doi: 10.1007/BF03346274
40. Sartorio A, Lafortuna CL, Agosti F, Proietti M, Maffiuletti NA. Elderly obese women display the greatest improvement in stair climbing performance after a 3-week body mass reduction program. Int J Obes Relat Metab Disord. (2004) 28:1097–104. doi: 10.1038/sj.ijo.0802702
41. Stiegler P, Cunliffe A. The role of diet and exercise for the maintenance of fat-free mass and resting metabolic rate during weight loss. Sports Med. (2006) 36:239–62. doi: 10.2165/00007256-200636030-00005
42. Margaria R, Aghemo P, Rovelli E. Measurement of muscular power (anaerobic) in man. J Appl Physiol. (1966) 21:1662–4. doi: 10.1152/jappl.1966.21.5.1662
43. Lafortuna CL, Fumagalli E, Vangeli V, Sartorio A. Lower limb alactic anaerobic power output assessed with different techniques in morbid obesity. J Endocrinol Invest. (2002) 25:134–41. doi: 10.1007/BF03343977
44. Thivel D, Ring-Dimitriou S, Weghuber D, Frelut ML, O’Malley G. Muscle strength and fitness in pediatric obesity: a systematic review from the european childhood obesity group. Obes Facts. (2016) 9:52–63. doi: 10.1159/000443687
45. Choi SJ, Files DC, Zhang T, Wang ZM, Messi ML, Gregory H, et al. Intramyocellular lipid and impaired myofiber contraction in normal weight and obese older adults. J Gerontol A Biol Sci Med Sci. (2016) 71:557–64. doi: 10.1093/gerona/glv169
46. Perera S, Mody SH, Woodman RC, Studenski SA. Meaningful change and responsiveness in common physical performance measures in older adults. J Am Geriatr Soc. (2006) 54:743–9. doi: 10.1111/j.1532-5415.2006.00701.x
47. Dufek JS, Currie RL, Gouws P-L, Candela L, Gutierrez AP, Mercer JA, et al. Effects of overweight and obesity on walking characteristics in adolescents. Hum Mov Sci. (2012) 31:897–906. doi: 10.1016/j.humov.2011.10.003
48. Galli M, Crivellini M, Sibella F, Montesano A, Bertocco P, Parisio C. Sit-to-stand movement analysis in obese subjects. Int J Obes. (2000) 24:1488–92. doi: 10.1038/sj.ijo.0801409
49. Kim S-H, Ju S-K. Comparison of muscle activity during sit-to-stand movement at different chair heights between obese and normal-weight subjects. J Exerc Rehabil. (2021) 17:39–44. doi: 10.12965/jer.2040800.400
50. Bittel DC, Bittel AJ, Tuttle LJ, Hastings MK, Commean PK, Mueller MJ, et al. Adipose tissue content, muscle performance and physical function in obese adults with type 2 diabetes mellitus and peripheral neuropathy. J Diabetes Complications. (2015) 29:250–7. doi: 10.1016/j.jdiacomp.2014.11.003
51. Stoever K, Heber A, Eichberg S, Brixius K. influences of resistance training on physical function in older obese men and women with sarcopenia. J Geriatr Phys. Ther. (2018) 41:20–7. doi: 10.1519/JPT.0000000000000105
52. Villareal DT, Chode S, Parimi N, Sinacore DR, Hilton T, Armamento-Villareal R, et al. Weight loss, exercise, or both and physical function in obese older adults. Obstet Gynecol Surv. (2011) 66:488–9. doi: 10.1097/OGX.0b013e3182352181
53. Wilson K. Obesity: lifestyle modification and behavior interventions. FP Essent. (2020) 492:19–24.
54. Bergland A, Strand BH. Norwegian reference values for the short physical performance battery (SPPB): the Tromsø study. BMC Geriatr. (2019) 19:216. doi: 10.1186/s12877-019-1234-8
55. Gregorio L, Brindisi J, Kleppinger A, Sullivan R, Mangano KM, Bihuniak JD, et al. Adequate dietary protein is associated with better physical performance among post-menopausal women 60-90 years. J Nutr Health Aging. (2014) 18:155–60. doi: 10.1007/s12603-013-0391-2
56. Tseng LA, Delmonico MJ, Visser M, Boudreau RM, Goodpaster BH, Schwartz AV, et al. Body composition explains sex differential in physical performance among older adults. J Gerontol A Biol Sci Med Sci. (2014) 69:93–100. doi: 10.1093/gerona/glt027
57. Sternfeld B, Ngo L, Satariano WA, Tager IB. Associations of body composition with physical performance and self-reported functional limitation in elderly men and women. Am J Epidemiol. (2002) 156:110–21. doi: 10.1093/aje/kwf023
58. Goodpaster BH, Carlson CL, Visser M, Kelley DE, Scherzinger A, Harris TB, et al. Attenuation of skeletal muscle and strength in the elderly: the health ABC study. J Appl Physiol. (2001) 90:2157–65. doi: 10.1152/jappl.2001.90.6.2157
59. Krotkiewski M, Bjorntorp P, Sjostrom L, Smith U. Impact of obesity on metabolism in men and women importance of regional adipose tissue distribution. J Clin Invest. (1983) 72:1150–62. doi: 10.1172/JCI111040
60. Carobbio S, Rodriguez-Cuenca S, Vidal-Puig A. Origins of metabolic complications in obesity: ectopic fat accumulation. The importance of the qualitative aspect of lipotoxicity. Curr Opin Clin Nutr Metab Care. (2011) 14:520–6. doi: 10.1097/MCO.0b013e32834ad966
Keywords: physical capabilities, body composition, adolescents, adults, obesity, physical activity
Citation: Lazzer S, D’Alleva M, Vaccari F, Tringali G, De Micheli R and Sartorio A (2022) Effects of a 3-Week Inpatient Multidisciplinary Body Weight Reduction Program on Body Composition and Physical Capabilities in Adolescents and Adults With Obesity. Front. Nutr. 9:840018. doi: 10.3389/fnut.2022.840018
Received: 20 December 2021; Accepted: 18 February 2022;
Published: 31 March 2022.
Edited by:
Roberto Fernandes da Costa, Federal University of Rio Grande do Norte, BrazilReviewed by:
Reza Rastmanesh, The Nutrition Society, United KingdomStephan Garcia Andrade Silva, Federal University of São Paulo, Brazil
Copyright © 2022 Lazzer, D’Alleva, Vaccari, Tringali, De Micheli and Sartorio. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mattia D’Alleva, ZGFsbGV2YS5tYXR0aWFAc3Blcy51bml1ZC5pdA==
†These authors have contributed equally to this work and share first authorship
 Stefano Lazzer
Stefano Lazzer