- 1School of Kinesiology, Shanghai University of Sport, Shanghai, China
- 2Department of Nursing, Xinhua Hospital Affiliated to Shanghai Jiaotong University School of Medicine, Shanghai, China
- 3Department of Health Professions, Faculty of Art, Health and Design, Swinburne University of Technology, Melbourne, VIC, Australia
- 4Department of Surgery, School of Medicine, University of Melbourne, Melbourne, VIC, Australia
- 5Research Institute for Sport and Exercise, University of Canberra, Canberra, ACT, Australia
- 6College of Rehabilitation Sciences, Shanghai University of Medicine and Health Sciences, Shanghai, China
- 7Department of Cardiology, Xinhua Hospital Affiliated to Shanghai Jiaotong University School of Medicine, Shanghai, China
Mediterranean Diet management for people with cardiovascular disease (CVD) or CVD risk is supported by evidence. However, there is no valid Chinese language instrument for the measurement of adherence to this diet. The objective of this study was to generate a Chinese version of the Mediterranean Diet Scale (MDS-Chinese) and to validate a self-administered version with Chinese participants with CVD or CVD risk. The MDS-Chinese was created by translation and cultural adaptation and tested for psychometric properties. A panel of 10 experts in the field, who evaluated the MDS-Chinese content, showed that the content validity index ranged from 0.88 to 1.00. Sixteen native Chinese speakers with CVD or CVD risk evaluated the clarity of the MDS-Chinese, and the resulting instruction and items clarity scores ranged from 9.2 to 10.0. A total of 326 participants completed the MDS-Chinese and a Chinese version of the Coronary Artery Disease Education Questionnaire–Short Version (CADE-Q SV). Analysis indicated that the MDS-Chinese has 4 factors, and the Pearson's correlation between the MDS-Chinese and CADE-Q SV was 0.73. Fifty randomly selected participants completed the MDS-Chinese again with a 1-week interval to assess reliability. Internal consistency was acceptable (Cronbach's α was 0.62) and the inter-class correlation reliability coefficients (ICC) for each item ranged from 0.73 to 0.88. This study showed that the MDS-Chinese has acceptable reliability and validity for use among those in the Chinese population with CVD or CVD risk. Given that diet is one of the key secondary prevention strategies for management in cardiac rehabilitation, the MDS-Chinese instrument may be a useful and convenient tool for use with those in the Chinese population with CVD or with high risk of CVD, to monitor the level of Mediterranean diet (MD) adherence, information which is important for clinical practice. In addition, the establishment of the MDS-Chinese gives a fundamental tool for diet-related CVD research in the Chinese population. Moreover, employment of the MDS-Chinese in the Chinese community may improve awareness of the importance of a healthy diet in CVD prevention and management.
Clinical Trial Registration: http://www.chictr.org.cn/enIndex.aspx, identifier: ChiCTR2000032810.
Introduction
Due to its high morbidity and mortality, cardiovascular disease (CVD) has been one of the leading health burdens worldwide, and it has affected 303 million people in China (1, 2). Research has shown that a range of factors, such as smoking, exercise, and diet, may contribute to CVD risk (3). Diet has been shown to play a fundamental role in preventing CVD (4–6). Healthy diets for the general population include the Mediterranean diet (MD), Dietary Approaches to Stop Hypertension (DASH), and Nordic and Paleolithic diets. Research has shown beneficial effects with these diet patterns in preventing CVD and reducing CVD risk (7–9). Of all these healthy diets, MD has undergone the most comprehensive and international assessment in relation to cardiovascular effect (10). A meta-analysis demonstrated that MD is associated with a 38% lower risk of CVD, and MD also has advantages in reducing CVD risk and mortality (11–13). The concept of MD was studied by Keys and Grande, who observed the inhabitants of the Mediterranean basin and then developed a questionnaire to reflect the typical dietary habits in a series of conference papers titled Public Health Implications of Traditional Diets during the early 1960s (14, 15). Different countries have slightly different recommendations for MD (16). The MD pattern in China is the habitual diet adhered to in Mediterranean countries (17, 18), which is mainly characterized by high consumption of plant-based food (with more than 200 g vegetables in every meal, 30–400 g fruits in every meal, 25–50 g cereals in every meal, and more than 200 g legumes every week) and low consumption of animal-based food (with <120 g red meat) (15, 19, 20).
Ghisi et al. developed the Mediterranean Diet Scale (MDS) and psychometrically validated it in Canadians with CVD or CVD risk. The MDS is a low cost and quick application tool, which has widespread application and reduces clinician time (21). The MDS includes four factors (Factor 1 reflects items related to meats and processed foods, Factor 2—olive oil and sauce items, Factor 3—fruits, vegetable, nuts, and legumes, and Factor 4—fish and seafood) with a total of 13 questions with “yes” or “no” responses. Notably, the dietary indices are investigator-driven and based on dietary guidelines (22). Recently, the MDS has been translated into Brazilian Portuguese (23). To date, there is no specific tool available for screening the pattern of MD adherence for those in the Chinese population with CVD or CVD risk. Accordingly, the aim of this study was to translate and culturally adapt the Canadian version of the MDS into an MDS-Chinese version, and to validate it in Chinese participants with CVD or at risk of CVD.
Materials and Methods
Design and Procedure
Permission was obtained to conduct this Chinese translation and validation study from the first author of the Canadian version of the MDS, in September 2020. This study was approved by the Ethics Committee for Research with Human Subjects at Xinhua Hospital, affiliated to Shanghai Jiao Tong University school of Medicine (Ethics number: XHEC-C-2020-078), and was registered in the Chinese Clinical Registration Center (clinical trial registry number: No. Chi CTR2000032810; clinical trial website: http://www.chictr.org.cn/enIndex.aspx). All the participants signed the informed consent forms before commencement of data collection.
The study consisted of two phases. First, translation, cultural adaptation, and clarity test were done which involved the following steps (24): (1) The forward translation process was independently completed by two physical therapists who were proficient in both the English and Chinese languages. After obtaining two Chinese versions, an expert panel composed of one professor of cardiology and one professor of physiotherapy checked the translation and synthesized them into one version. (2) The backward translation was completed by an English professor. In order to ensure the quality of this step, the English professor did not know that backward translation work was being done and was not familiar with the MDS. A detailed review by the expert panel followed to focus on the comparison between the backward translation version and the original English version and to ensure that the semantic consistency rate reached 90%. (3) The cultural adaptation process was performed by an expert team including two professors of dietetics, one professor of cardiology, two senior cardiologists, three professors of physiotherapy, one professor of nursing, and one chief nurse in cardiology. Collectively they reviewed the Chinese version and the experts' opinions, and made suggestions that were collated and analyzed to improve the accuracy and clarity of each item. (4) A preliminary test was conducted in at least 10 Chinese participants with CVD or at CVD risk (such as hypertension, diabetes, and dyslipidemia) to evaluate the clarity of the MDS-Chinese form. In the final step of this phase, feedback was analyzed to further revise the scale.
In the second phase, the psychometric properties of the MDS-Chinese were evaluated by a cross-sectional survey. This included content validity, construct validity, criterion validity, internal consistency, and test–retest reliability.
For content validity, the expert team, who were involved in the cultural adaptation process, evaluated item content. Experts were asked to rate each item on a 4-point Likert scale (ranging from 1 = completely uncorrelated to 4 = strongly correlated) based on the content applicability and the clarity of the phrasing (25, 26).
For construct validity, the study recruited 326 participants for validity testing so as to safely exceed the recommendation of a sample size of 10 participants per item (27). All the participants answered a total of 13 questions in the MDS-Chinese. Participants were asked to answer each question with a “yes” or “no” response, where an answer of “yes” equated to one point. The higher the score, the higher was the adherence to the MD pattern.
For criterion validity, the 326 participants also completed the Chinese form of the Coronary Artery Disease Education Questionnaire–Short Version (CADE-Q SV), which is a tool to assess patients' knowledge about CVD (28), as it has been shown that participants with good knowledge about CVD and nutrition have a higher level of adherence to the MD pattern (29–31). The score for the CADE-Q SV and the diet dimension score of CADE-Q SV were thus obtained together with the MDS-Chinese score.
For internal consistency and test-retest reliability, 50 participants were randomly selected to complete the MDS-Chinese instrument again after a 1-week interval, based on the recommendation for test-retest analysis (32).
Participants
Participants included all patients with CVD or at CVD risk in the Department of Cardiology from Xinhua Hospital between September 2020 and July 2021. Inclusion criteria included: ① Clinically diagnosed CVD or multiple CVD risk factors (such as hypertension, diabetes, and dyslipidemia); ② Mini Mental State Examination (MMSE) ≥24 (33); ③ native language is Chinese; ④ age ≥18 years. The exclusion criteria were: ① Unable to complete the questionnaire independently for any reason (such as being illiterate or having visual dysfunction); ② inability to eat by mouth or food restrictions or diets that do not include meat and fish (i.e., food allergies to legumes, nuts, olive oil, fish, or seafood, or being vegetarian or vegan); ③ individuals living in a retirement home (set menus are provided by the institutions); ④ having experienced or undergoing cardiac rehabilitation (CR).
Statistical Analysis
SPSS Version 25.0 (Armonk, NY: IBM Corp.) was used for data analysis. Descriptive statistics was applied to the demographic data, and knowledge scores and the difference scores were analyzed by Multi-Factor Variance Analysis. Continuous variables were presented as mean values and standard deviation (), while categorical/nominal variables were presented as frequencies and percentages.
Content validity was evaluated by the expert team, and was assessed by the content validity index (CVI) (25, 26). CVI of each item (I-CVI) was calculated by using the number of the score≥3 divided by the total number of the experts. A value of CVI >0.70 was regarded as acceptable (34). The CVI of the whole questionnaire was estimated by calculating the average CVI of all the items (35). Construct validity was assessed using exploratory factor analysis (EFA) to explore the factorial structure of the MDS-Chinese, and confirmatory factor analysis (CFA) was used to examine the factorial structure. SPSS AMOS 26.0 was used for CFA. If EFA showed Kaiser-Meyer-Olkin index (KMO) >0.6, p < 0.05 for the Bartlett's Sphericity tests, and the factor loadings greater than 0.30 on only one factor, then CFA was conducted (36). CFA provides information including chi square by χ2/df, goodness-of-fit index (GFI), comparative fit index (CFI), root mean square error of approximation (RMSEA), and standardized root mean square residual (SRMR). Values of 1 ≤ χ2/df ≤ 3, GFI > 0.90, CFI > 0.90, RMSEA ≤ 0.08, and SRMR < 0.08 were considered to be acceptable (36–38). Criterion validity was analyzed by Pearson's correlation, with values higher than 0.70 considered acceptable (39).
For reliability, internal consistency was assessed by Cronbach's alpha, where a value >0.60 was considered acceptable (39). Test-retest reliability was assessed via the inter-class correlation coefficient (ICC) with values > 0.70 considered acceptable (39).
Results
Translation, Backward Translation, and Cultural Adaptation
After review by the expert panel, semantic equivalence between the backward translation version and the original version was achieved. For cultural adaptation, the expert panel suggested that the unit reference to “ounce” be modified to “gram” to align with more commonly-used units of measurement in the Chinese language (Supplementary File) (40).
Clarity Test
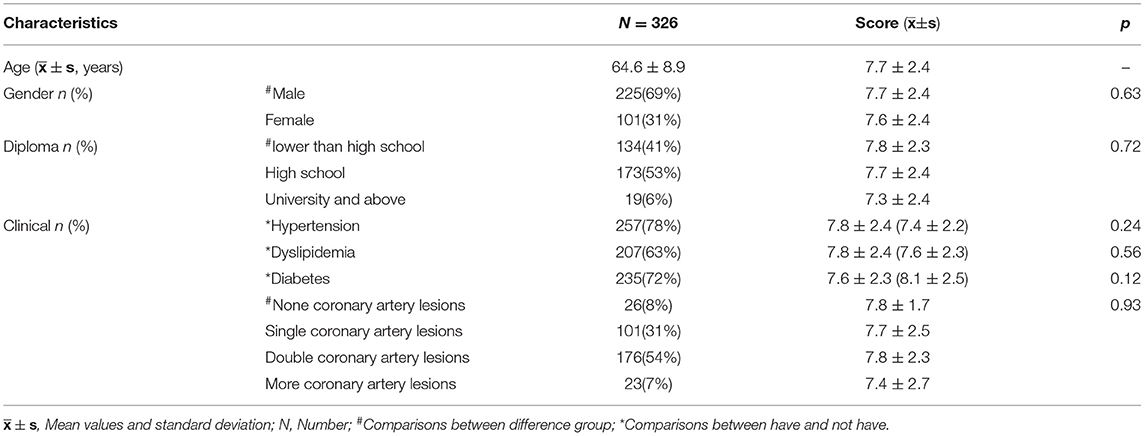
Sixteen participants with CVD or CVD risk participated in the pilot test, and evaluated its clarity. There were no unclear or ambiguous sentences in the instructions provided or the items within the MDS-Chinese version. The clarity scores ranged from 9.2 to 10.0 (Table 1).
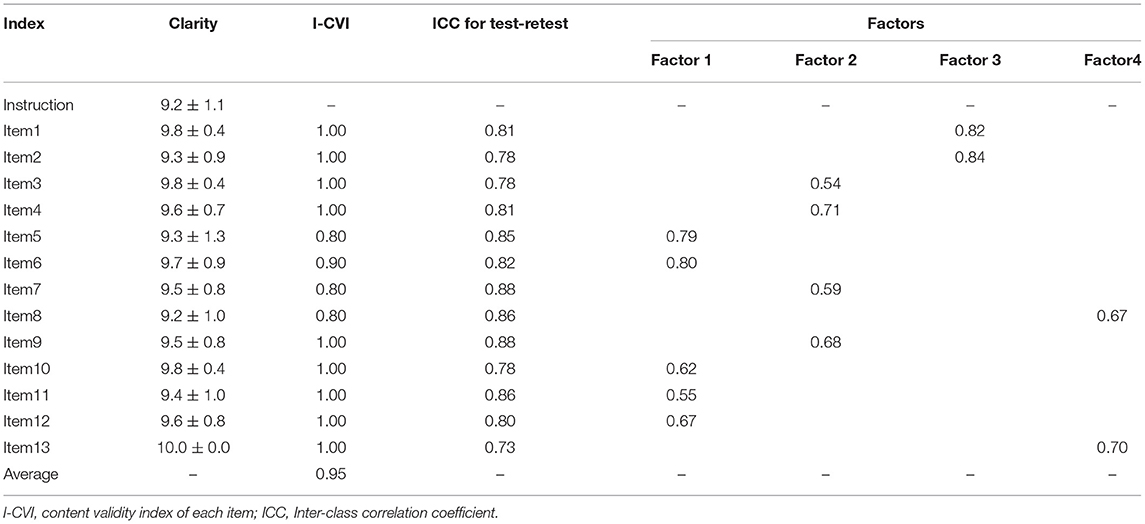
Table 1. Clarity, content validity index for each item (I-CVI), inter-class correlation coefficient (ICC), and factor loading for each item.
Psychometric Validation
The study recruited 326 participants and they all completed the questionnaires. The characteristics of the participants are presented in Table 2.
Regarding content validity, I-CVIs ranged from 0.80 to 1.00. CVI for the whole questionnaire was 0.96. The results indicated an adequate content validity of the questionnaire (Table 1).
For construct validity, the EFA factorial analysis showed that the KMO was 0.68 and Bartlett's sphericity was χ2 = 622.1, p < 0.001. The four-factor loading coefficients of the model ranged from 0.54 to 0.80, and all were within the acceptable level, indicating that the data was suitable for factor analysis. CFA was used to test the four-factor model established. The results showed that the model resulted in good data fitting (χ2/df = 1.651; RMSEA = 0.045; CFI = 0.931; GFI = 0.957; SRMR = 0.051). Therefore, the four-factor of MDS-Chinese was considered acceptable. Specifically, Factor 1 reflected items related to meats and processed foods, Factor 2—fruits, vegetables, nuts, and legumes, Factor 3—olive oil, and Factor 4—fish, seafood, and flavor (Table 1).
For criterion validity, the Pearson's correlation results showed that the scores of MDS-Chinese were significantly correlated with that of CADE-Q SV (r = 0.73, p < 0.01) and dimension of CADE-Q SV (r = 0.70, p < 0.01).
Internal consistency as assessed by Cronbach's alpha was 0.62. With regard to reproducibility, test-retest reliability evaluated through the ICC of each item showed a range from 0.73 to 0.88 (Table 1).
Discussion
The MD is supported by evidence as being the healthiest diet worldwide to reduce the risk of CVD (41, 42). The self-administered version of the MDS is a practical and useful screening tool, and it has been widely used internationally (21, 23). This study aimed to translate and assess the validity of a newly created MDS-Chinese version with those in the general population with CVD or with risk of CVD.
The mean total score for the MDS-Chinese was 7.7 ± 2.4, which was lower than that for Canadians with CVD or risk of CVD (10.2 ± 1.9) (21), but the mean total score for the MDS-Chinese with diabetes mellitus (DM) (7.6 ± 2.3) was slightly higher than that found in Brazilian adults with DM (6.9 ± 2.0) (23). It may be because of the sampling difference, since the Canadian adult post CR may have improved adherence to healthy diet behaviors (43).
The cross-cultural adaptation conducted here was completed in concordance with prior guidelines (44). Only some minor changes were made, specifically for the metric unit utilized to quantify the amount of food eaten. Preliminary pilot testing demonstrated that the instructions and all item descriptions were clear and easy to understand. The clarity of the MDS-Chinese was excellent with scores ranging from 9.2 to 10.0, a finding which supports it as a self-administered scale.
Psychometric analysis demonstrated that the test-retest reliability and internal consistency of the MDS-Chinese was acceptable, and this result is similar to findings reported for the original version (21). Content, criterion, and construct validity were acceptable for Chinese participants with CVD or CVD risk. Construct validity analysis through EFA and CFA demonstrated that in comparison to the original MDS, there were also four-factors in MDS-Chinese (Table 1). However, item 13 (“Do you flavor foods with a combination of tomato, garlic, onions, or leeks two times or more per week?”) was assigned in different factor groups. This is presumably because different dietary opinions related to cooking habits exist between the Chinese and the western general population (40). In China, olive oil is not used with tomato, garlic, and onion (45, 46). Tomato, garlic, and onion are usually used when cooking fish, especially in coastal regions (40, 45). Thus, item 13 belongs to Factor 4 instead of Factor 3 in the MDS-Chinese (Table 1). Criterion validity was assessed through the scores of MDS-Chinese being related to the score of CADE-Q SV and the diet dimension score of CADE-Q SV, as it is known that nutrition knowledge determines diet habits. This study has also shown that the CADE-Q SV score is strongly correlated with the MDS-Chinese score, a finding similar to that in other studies (29–31). For test-retest reliability and internal consistency of the MDS-Chinese, our results were in the acceptable range and were similar to the findings reported in the original version (21).
Limitations
There are some limitations in this study. For validation, the MDS-Chinese was evaluated with regard to content validity, construct validity, and criterion validity. However, the dietary assessment validation will be done in future studies as it was out-of-scope in the present work. In addition, given that the MDS is a self-administered instrument, there might be some participants who did not understand the questions correctly.
Conclusions
The self-administered version MDS was translated and culturally adapted to create a Chinese version, and validated in a cohort of the Chinese population with CVD or CVD risk. The MDS-Chinese version is shown to be reliable and valid for assessing the level of MD adherence in native Chinese language users. Given that diet is one of the key secondary prevention strategies for the management of CR, the MDS-Chinese could be an important tool for use with those with cardiovascular problems.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Ethics Statement
The studies involving human participants were reviewed and approved by Xinhua Hospital, Affiliated to Shanghai Jiao Tong University school of Medical. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
JL, JH, and SM designed the study and had primary responsibility for this work. JL, HD, and ZW were responsible for the execution of the trial and data collection. JL and HD analyzed the data and discussed with JH and SM. JL wrote the first draft, which was improved by SM and JH. DE-A and RA critically reviewed and improved the manuscript. All authors read and approved the final manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
The authors thank Gabriela Lima de Melo Ghisi, who is the first author of the Canadian version of a self-administered version MDS, for permission to conduct the translation and validation study. The authors express their gratitude to all the volunteers who took part.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fnut.2022.831109/full#supplementary-material
MDS-Chinese please refer to Supplementary File.
References
1. Roth GA, Johnson C, Abajobir A, Abd-Allah F, Abera SF, Abyu G, et al., Global, regional, and national burden of cardiovascular diseases for 10 causes, 1990 to 2015. J Am Coll Cardiol. (2017) 70:1–25. doi: 10.1016/j.jacc.2017.04.052
2. Shengshou H. Report on Cardiovascular Health and Diseases Burden in China: an Updated Summary of 2020. Chin Circ J. (2021) 36:521–45. doi: 10.3969/j.issn.1007-5062.2021.09.001
3. Smith SC Jr, Benjamin EJ, Bonow RO, Braun LT, Creager MA, Franklin BA, et al., AHA/ACCF Secondary Prevention and Risk Reduction Therapy for Patients with Coronary and other Atherosclerotic Vascular Disease: 2011 update: a guideline from the American Heart Association and American College of Cardiology Foundation. Circulation. (2011) 124:2458–73. doi: 10.1161/CIR.0b013e318235eb4d
4. Chiavaroli L, Nishi SK, Khan TA, Braunstein CR, Glenn AJ, Mejia SB, et al., Portfolio dietary pattern and cardiovascular disease: a systematic review and meta-analysis of controlled trials. Prog Cardiovasc Dis. 61:43–53. doi: 10.1016/j.pcad.2018.05.004 (1873-1740 (Electronic)).
5. Reedy J, Krebs-Smith SM, Miller PE, Liese AD, Kahle LL, Park Y, et al. Higher diet quality is associated with decreased risk of all-cause, cardiovascular disease, and cancer mortality among older adults. J Nutr. (2014) 144:881–9. doi: 10.3945/jn.113.189407 (1541-6100 (Electronic)).
6. Schwingshackl L, Bogensberger B, Hoffmann G. Diet quality as assessed by the healthy eating index, alternate healthy eating index, dietary approaches to stop hypertension score, and health outcomes: an updated systematic review and meta-analysis of cohort studies. J Acad Nutr Diet. (2018) 118:74–100.e11. doi: 10.1016/j.jand.2017.08.024 (2212-2672 (Print)).
7. Ramezani-Jolfaie N, Mohammadi M, Salehi-Abargouei A. The effect of healthy Nordic diet on cardio-metabolic markers: a systematic review and meta-analysis of randomized controlled clinical trials. Eur J Nutr. (2019) 58:2159–74. doi: 10.1007/s00394-018-1804-0 (1436-6215 (Electronic)).
8. Sacks FM, Svetkey LP, Vollmer WM, Appel LJ, Bray GA, Harsha D, et al. Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. DASH-Sodium Collaborative Research Group. N Engl J Med. (2001) 344:3–10. doi: 10.1056/NEJM200101043440101 (0028-4793 (Print)).
9. Trichopoulou A, Costacou T, Bamia C, Trichopoulos D. Adherence to a mediterranean diet and survival in a greek population. N Engl J Med. (2003) 348:2599–608. doi: 10.1056/NEJMoa025039
10. Martínez-González MA, Gea A, Ruiz-Canela M. The Mediterranean Diet and Cardiovascular Health. (1524-4571 (Electronic)).
11. Becerra-Tomás N, Blanco Mejía S, Viguiliouk E, Khan T, Kendall CWC, Kahleova H, et al. Mediterranean diet, cardiovascular disease and mortality in diabetes: a systematic review and meta-analysis of prospective cohort studies and randomized clinical trials. Crit Rev Food Sci Nutr. (2020) 60:1207–27. doi: 10.1080/10408398.2019.1565281 (1549-7852 (Electronic)).
12. Zampelas A, Magriplis E. Dietary patterns and risk of cardiovascular diseases: a review of the evidence. Proc Nutr Soc. (2020) 79:68–75. doi: 10.1017/S0029665119000946
13. Badimon L, Chagas P, Chiva-Blanch G. Diet and cardiovascular disease: Effects of foods and nutrients in classical and emerging cardiovascular risk factors. Curr Med Chem. (2019) 26:3639–51. doi: 10.2174/0929867324666170428103206
14. Martínez-González MA, Sánchez-Villegas A. The emerging role of Mediterranean diets in cardiovascular epidemiology: monounsaturated fats, olive oil, red wine or the whole pattern? Eur J Epidemiol. (2004) 19:9–13. doi: 10.1023/b:ejep.0000013351.60227.7b
15. Willett WC, Sacks F, Trichopoulou A, Drescher G, Ferro-Luzzi A, Helsing E, et al. Mediterranean diet pyramid: a cultural model for healthy eating. Am J Clin Nutr. (1995) 61(6):1402–6. doi: 10.1093/ajcn/61.6.1402S
16. Figueroa C, Echeverría G, Villarreal G, Martínez X, Ferreccio C, Rigotti A. Introducing plant-based mediterranean diet as a lifestyle medicine approach in latin america: Opportunities within the chilean context. Front Nutr. (2021) 25:680452. doi: 10.3389/fnut.2021.680452
17. Chen GD, Dong XW, Zhu YY, Tian HY, He J, Chen YM. Adherence to the mediterranean diet is associated with a higher bmd in middle-aged and elderly chinese. Sci Rep. (2016) 9:25662. doi: 10.1038/srep25662
18. Woo J, Woo KS, Leung SS, Chook P, Liu B, Ip R, et al. The Mediterranean score of dietary habits in chinese populations in four different geographical areas. Eur J Clin Nutr. (2001) 55:215–20. doi: 10.1038/sj.ejcn.1601150
19. Bach-Faig A, Berry EM, Lairon D, Reguant J, Trichopoulou A, Dernini S, et al. Mediterranean diet foundation expert group. mediterranean diet pyramid today. science and cultural updates. Public Health Nutr. (2011) 14:2274–84. doi: 10.1017/S1368980011002515
20. Davis C, Bryan J, Hodgson J, Murphy K. Definition of the mediterranean diet: A literature review. Nutrients. (2015) 7:9139–53. doi: 10.3390/nu7115459
21. Ghisi GLM, Mahajan A, da Silva Chaves GS, Rouse V, Brum M, Ajwani F, et al. Validation of a self-administered version of the Mediterranean diet scale (MDS) for cardiac rehabilitation patients in Canada. Int J Food Sci Nutr. (2019) 70:202–11. doi: 10.1080/09637486.2018.1486392
22. Michels KB, Schulze MB. Can dietary patterns help us detect diet-disease associations? Nutr Res Rev. (2005) 18:241–248. doi: 10.1079/NRR2005107
23. Teixeira RL, Jansen AK, Pereira DA, Ghisi GLM, Silva LPD, Cisneros LL, et al. Brazilian portuguese version of the mediterranean diet scale: Translation procedures and measurement properties. Diab Metab Syndr. (2021) 15:102165. doi: 10.1016/j.dsx.2021.06.002
24. Guillemin F, Bombardier C, Beaton D. Cross-cultural adaptation of health-related quality of life measures: literature review and proposed guidelines. J Clin Epidemiol. (1993) 46:1417–32. doi: 10.1016/0895-4356(93)90142-N
25. Lynn MR. Determination and quantification of content validity. Nurs Res. (1986) 35:382–5. doi: 10.1097/00006199-198611000-00017
26. Mastaglia B, Toye C, Kristjanson LJ. Ensuring content validity in instrument development: challenges and innovative approaches. Contemp Nurse. (2003) 14:281–91. doi: 10.5172/conu.14.3.281
27. Sousa VD, Rojjanasrirat W. Translation, adaptation and validation of instruments or scales for use in cross-cultural health care research: a clear and user-friendly guideline. J Eval Clin Pract. (2011) 17:268–74. doi: 10.1111/j.1365-2753.2010.01434.x
28. Jiajia L, Zheng W, Nan C, Nan Y, Shu M, Jia H. Reliability and validity of Chinese version of coronary artery disease education questionnaire short version Academic. J Second Mil Med Univ. (2021) 42:294–300. doi: 10.16781/j.0258-879x.2021.03.0294
29. Santella ME, Hagedorn RL, Wattick RA, Barr ML, Horacek TM, Olfert MD. Olfert. Learn first, practice second approach to increase health professionals' nutrition-related knowledge, attitudes and self-efficacy. Int J Food Sci Nutr. (2020) 71:370–7. doi: 10.1080/09637486.2019.1661977
30. Neshatbini Tehrani A, Farhadnejad H, Salehpour A, Beyzai B, Hekmatdoost A, Rashidkhani B. The association between nutrition knowledge and adherence to a Mediterranean dietary pattern in Iranian female adolescents. Int J Adolesc Med Health. (2019) 33. doi: 10.1515/ijamh-2018-0188
31. Sahingoz SA, Sanlier N. Compliance with Mediterranean Diet Quality Index (KIDMED) and nutrition knowledge levels in adolescents A case study from Turkey. Appetite. (2011) 57:272–7. doi: 10.1016/j.appet.2011.05.307
32. Hopkins WG. Measures of reliability in sports medicine and science. Sports Med. (2000) 30:1–15. doi: 10.2165/00007256-200030010-00001
33. Li H, Jia J, Yang Z. Mini-mental state examination in elderly chinese: a population-based normative study. J Alzheimers Dis. (2016) 53:487–96. doi: 10.3233/JAD-160119
34. Grant JS, Davis LL. Selection and use of content experts for instrument development. Res Nurs Health. (1997) 20:269–74 doi: 10.1002/(sici)1098-240x(199706)20:3<269::aid-nur9>3.0.co;2-g
35. Shi J, Mo X, Sun Z. Content validity index in scale development. Zhong Nan Da Xue Xue Bao Yi Xue Ban. (2012) 37:152–5. doi: 10.3969/j.issn.1672-7347.2012.02.007
37. Steiger JH. Structural model evaluation and modification: an interval estimation approach. Multivariate Behav Res. (1990) 25:173–80. doi: 10.1207/s15327906mbr2502_4
38. Barrett P. Structural equation modelling: adjudging model fit. Pers Individ Dif. (2007) 42:815–24. doi: 10.1016/j.paid.2006.09.018
39. Terwee CB, Bot SD, de Boer MR, van der Windt DA, Knol DL, Dekker J, et al. Quality criteria were proposed for measurement properties of health status questionnaires. J Clin Epidemiol. (2007) 60:34–42. doi: 10.1016/j.jclinepi.2006.03.012
40. Wang SS, Lay S, Yu HN, Shen SR. Dietary guidelines for chinese residents (2016): comments and comparisons. J Zhejiang Univ Sci B. (2016) 17:649–56. doi: 10.1631/jzus.B1600341
41. Veronese N, Stubbs B, Noale M, Solmi M, Luchini C, Maggi S. Adherence to the Mediterranean diet is associated with better quality of life: data from the Osteoarthritis Initiative. Am J Clin Nutr. (2016) 104:1403–9. doi: 10.3945/ajcn.116.136390
42. Estruch R, Ros E, Salas-Salvadó J, Covas MI, Corella D, Arós F, et al. Primary prevention of cardiovascular disease with a Mediterranean diet. N Engl J Med. (2013) 368:1279–90. doi: 10.1056/NEJMoa1200303
43. Sharp PB, Salyer J. Self-efficacy and barriers to healthy diet in cardiac rehabilitation participants and nonparticipants. (1550-5049 (Electronic)).
44. Beaton DE, Bombardier C, Guillemin F, Ferraz MB. Guidelines for the process of cross-cultural adaptation of self-report measures. Spine (Phila Pa 1976). (2000) 25:3186–91. doi: 10.1097/00007632-200012150-00014
45. Wang J, Lin X, Bloomgarden ZT, Ning G. The Jiangnan diet, a healthy diet pattern for Chinese. J Diabetes. (2020) 12:365–71. doi: 10.1111/1753-0407.13015
Keywords: cardiovascular disease, Mediterranean diet, Mediterranean diet scale, reliability, validity, psychometric
Citation: Li J, Ding H, Wang Z, El-Ansary D, Adams R, Han J and Meng S (2022) Translation, Cultural Adaptation, Reliability, and Validity Testing of a Chinese Version of the Self-Administered Mediterranean Diet Scale. Front. Nutr. 9:831109. doi: 10.3389/fnut.2022.831109
Received: 08 December 2021; Accepted: 25 February 2022;
Published: 28 March 2022.
Edited by:
Aida Turrini, Independent Researcher, Rome, ItalyReviewed by:
Leila Itani, Beirut Arab University, LebanonJeanette Mary Andrade, University of Florida, United States
Copyright © 2022 Li, Ding, Wang, El-Ansary, Adams, Han and Meng. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jia Han, SmlhLkhhbkBjYW5iZXJyYS5lZHUuYXU=; Shu Meng, bXNkb2N0b3JAMTI2LmNvbQ==
†These authors have contributed equally to this work
 Jiajia Li
Jiajia Li Huirong Ding2†
Huirong Ding2† Zheng Wang
Zheng Wang Roger Adams
Roger Adams Jia Han
Jia Han