
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Nutr. , 28 February 2022
Sec. Nutrition and Microbes
Volume 9 - 2022 | https://doi.org/10.3389/fnut.2022.823288
This article is part of the Research Topic Next-Generation Prebiotics and Probiotics: Current Status and Future Development View all 7 articles
 Jing Feng1,2†
Jing Feng1,2† Min Gao1†
Min Gao1† Chengcheng Zhao3
Chengcheng Zhao3 Jian Yang1
Jian Yang1 Haiyan Gao1
Haiyan Gao1 Xin Lu1
Xin Lu1 Rong Ju4
Rong Ju4 Xiuwei Zhang1*
Xiuwei Zhang1* Yunlei Zhang1,2,3*
Yunlei Zhang1,2,3*Background: Chemotherapy generally causes serious diarrhea and oral mucositis in cancer patients, and subsequently affects treatment. Oral administration of probiotics provides a therapeutic choice to address these limitations. This study aims to conduct a systematic review and meta-analysis on the efficacy of oral probiotic use in the management of the chemotherapy-induced adverse reactions, and to summarize the mechanisms underlying the action.
Methods: We searched PubMed, Embase, ClinicalTrials.gov, and Web of Science from the start of the study to its completion on Dec. 31, 2021. Risk of bias was assessed using Cochrane Collaboration's Tool. Statistical analysis of the acquired data was performed via the RevMan and the Stata Statistical Software. The protocol was registered in the International Prospective Register of Systematic Reviews (PROSPERO registration number: CRD42020220650).
Results: Twelve randomized controlled trials including 1,013 patients were recruited and analyzed via the standard procedure of meta-analysis. In contrast to the control group, orally taking probiotics significantly decreased the risk of chemotherapy-induced diarrhea (≥ 1 grade) (RR = 0.70; 95% Cl: 0.56, 0.88; P = 0.002) and oral mucositis (≥ 1 grade) (RR: 0.84; 95% Cl: 0.78, 0.91; P < 0.00001) at all grades. Further analysis found that severe diarrhea (≥ 2 grades) (RR: 0.50; 95% Cl: 0.32, 0.78; P = 0.002) and severe oral mucositis also significantly declined (≥ 3 grades) (RR: 0.66; 95% Cl: 0.55, 0.79; P < 0.00001) after oral probiotic use. Interestingly, the beneficial effects of probiotics displayed statistically significant only in Asian patients. Importantly, the more species of bacteria they took, the lower the incidences of the adverse reactions occurred. We used Egger's test P value to confirm that there is no publication bias.
Conclusions: This meta-analysis demonstrated that orally administrated probiotics has a potential to decrease chemotherapy-induced diarrhea and oral mucositis incidences. However, the efficacy of oral probiotic use against the adverse reactions needs to be further verified through more clinical trials, and the species and number of probiotics have to be optimized and standardized prior to clinical applications.
Systematic Review Registration: https://www.crd.york.ac.uk, identifier: 220650.
Diarrhea and oral mucositis elicited by chemotherapy lead to interruptions or changes to the therapeutic regime and subsequently affect patient prognosis and overall survival. Current clinical practice guidelines for treating chemotherapy-induced diarrhea mainly rely on diet modification and heteropathy treatment using drugs (including loperamide, octreotide, and opium tinctures) (1). However, the treatments are often accompanied by additional gastrointestinal symptoms, including stomach pain, diarrhea, and vomiting (2, 3). Also, chemotherapy-induced oral mucositis does not have any evidence-based clinical management regimes, although some clinical strategies have been recommended by the Multinational Association of Supportive Care in Cancer and International Society of Oral Oncology (MASCC/ISOO) (4). Therefore, it is crucial to develop novel drugs or treatment strategies to decrease diarrhea and oral mucositis as a result of chemotherapy.
Increasing evidences demonstrate the key role of probiotics in the management of patients with inflammatory bowel disease, allergy, autoimmune disease, and cancer (5), presenting a new avenue to address these limitations. The bacteria can stimulate the proliferation of beneficial bacteria of intestinal microbiota, thus maintaining a healthy intestinal environment or improving diseased one (6, 7). Actually, daily probiotic use succeeded in reducing the adverse reactions of chemotherapy in several clinical trials (8–10). For example, cervical and colorectal cancer patients who took probiotic capsules exhibited a lower incidence of diarrhea during chemotherapy than those who used the placebos (11, 12). Orally administrated probiotics obviously decreased grade III and IV oral mucositis in chemotherapy-treated patients with head and neck squamous cell carcinoma and nasopharyngeal carcinoma (13). In addition, postoperative complications due to infection were significantly reduced in cancer patients because of oral probiotic use (14). The mechanisms underlying the beneficial effects mainly include immunoregulation, metabolite production (organic acids, antimicrobial compounds, and enzymes), resident microbiota interactions, interfacing with the host, and improved gut barrier integrity (15–18). Also, the effect could be due to the regulation of blood levels of certain pro-inflammatory cytokines such as TNF-α and IL-6 (9).
Until now, several studies have already been conducted via meta-analysis of the efficacy of orally taking probiotics on the incidence reduction of diarrhea and oral mucositis in cancer patients with chemotherapy, radiotherapy, and chemoradiotherapy (14, 19, 20). However, the treatment methods for cancer patients in these studies concerned a variety of techniques, and subsequently resulted in a large heterogeneity (14, 19). Simultaneously, the data from one of the meta-analysis reports was extracted from the retrospective studies to evaluate the efficacy of probiotics on the remission of diarrhea in cancer patients with chemotherapy (20). Further, the former reports did not consider the ethnic differences that could affect the results of daily probiotic use for disease therapy. More important, several new clinical trials regarding the use of probiotics in the management of adverse reactions during chemotherapy have been published recently (9, 12, 21), which we have seriously considered in the meta-analysis. The statistical analysis demonstrated that orally administered probiotics greatly reduced the incidence of diarrhea and oral mucositis at all grades in the cancer patients with chemotherapy, but this effect was only found in Asian populations (China, India, Japan, Thailand, and Malaysia), indicating the efficacy may change in different countries because of ethnic difference. This phenomenon could be explained by the fact that the widely use of probiotics in daily healthcare, and some foods, such as cheese and yogurt, containing a great deal of probiotics are taken daily by people in Europe and America for a long history while the Asian people that begin to take probiotics as daily foods only occurs in recent decades (22). Notably, the treatment schemes including multiple species of probiotics exhibited better effects than the single bacterium in the cancer adjuvant therapy. Additionally, contrary to the former reports that the cancer patients were treated by multiple therapy methods (13, 16, 17), this meta-analysis is further confined to the adjuvant therapy of chemotherapy-induced adverse reactions in cancer patients. We fully expect that an updating meta-analysis of oral probiotic use in disease management could provide a new clinical idea for reducing the incidence of chemotherapy-induced adverse reactions.
The systematic review and meta-analysis strictly followed the Cochrane Handbook requirements, and it had been registered in PROSPERO (CRD42020220650). We performed a preliminary search and result screening prior to registration. A systematic search and result screening has been conducted again to include all the eligible publications after registration.
This study was performed following the Population, Intervention, Comparator, Outcomes and Study design (PICOS)-model, which is in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) (23). The population was confined to the cancer patients with chemotherapy, in which the patients in the intervention group took the probiotic preparation by orally administration, and they had to be controlled (placebo or control group), but could be open-label or blinded. During the treatment, the incidences of diarrhea and oral mucositis in the cancer patients were carefully observed and recorded [Diarrhea and oral mucositis severity was graded, respectively, according to The National Cancer Institute Common Terminology Criteria for Adverse Events (CTCAE) (24) and Radiation Therapy Oncology Group (RTOG)] (25). Also, the clinical studies must be performed following the principle of randomized controlled trials. We sought to determine whether oral probiotic use could reduce the incidences of chemotherapy-induced diarrhea and oral mucositis.
We conducted a preliminary search and result screening of PubMed, Embase, ClinicalTrials.gov, and Web of Science databases on Nov. 20, 2020 to determine whether this meta-analysis could be carried out. A systematic search and result screening were performed on Dec. 31, 2021 to identify articles associated with oral probiotic use to decrease the side effects of chemotherapy in cancer patients. Literature searching was conducted by two authors (Jing Feng and Min Gao). Disagreements were resolved by discussion with a third author (Yunlei Zhang). The following keywords were used as search terms: (“Neoplasms” [MeSH Terms] OR (“Neoplasia” [Title/Abstract] OR “Neoplasms” [Title/Abstract] OR “Tumors” [Title/Abstract] OR “Tumor” [Title/Abstract] OR “Cancer” [Title/Abstract] OR “Cancers” [Title/Abstract] OR “Malignancy” [Title/Abstract] OR “Malignancies” [Title/Abstract] OR “Malignant Neoplasms” [Title/Abstract] OR “Malignant Neoplasm” [Title/Abstract] OR “Neoplasm Malignant”[Title/Abstract] OR “Neoplasms Malignant”[Title/Abstract] OR “Benign Neoplasms” [Title/Abstract] OR “Neoplasms Benign” [Title/Abstract] OR “Benign Neoplasm” [Title/Abstract] OR “Neoplasm Benign” [Title/Abstract])) AND (“Probiotics” [MeSH Terms] OR (“Probiotic” [Title/Abstract] OR “Prebiotic” [Title/Abstract] OR “Prebiotics” [Title/Abstract] OR “Symbiotic” [Title/Abstract] OR “Lactobacillus” [Title/Abstract] OR “Lactobacilli” [Title/Abstract] OR “Bifidobacterium” [Title/Abstract] OR (“Paraprobiotics” [Title/Abstract] OR “Bacterial Lysate” [Title/Abstract] OR “Postbiotics” [Title/Abstract] OR “Tyndallized” [Title/Abstract] OR “Heat-killed” [Title/Abstract])) AND (“Drug Therapy” [MeSH Terms] OR (“Therapy Drug” [Title/Abstract] OR “Drug Therapies” [Title/Abstract] OR “Therapies Drug” [Title/Abstract] OR “Chemotherapy” [Title/Abstract] OR “Chemotherapies” [Title/Abstract] OR “Pharmacotherapy” [Title/Abstract] OR “Pharmacotherapies” [Title/Abstract])) AND (“Clinical Trial” [Publication Type] OR “Intervention Study” [Title/Abstract]).
The studies included in the meta-analysis were screened following the principle of PICOS: (1) Population: The studies that concern cancer patients treated by chemotherapy were considered; (2) Intervention: Cancer patients undergoing chemotherapy were given oral probiotics; (3) Comparison: Patients that did not take probiotics; (4) Outcomes: The number of patients with diarrhea or oral mucositis should be recorded; (5) Studies: The study followed the principle of randomized controlled trial.
Studies were excluded if any of the following reasons were involved: (1) Studies without control groups; (2) Articles published in languages other than English; (3) Ongoing or unpublished experiments; (4) Studies with <10 patients; (5) Reviews, retrospective articles, animal experiments, independent protocols, letters, books, and personal opinions.
The data were independently extracted into pre-made tables by two of the listed authors (Chengcheng Zhao and Jian Yang). Any uncertain issues were determined by a third author (Yunlei Zhang). The data were extracted from the studies by the following terms: (1) Study characteristics: first author, publication year, country; (2) Baseline patient characteristics: patient population, cancer type, sample number, chemotherapy regimen, experimental group intervention, and comparison; (3) Outcomes measured by the number of adverse events and total number of participants; (4) The elements contributing to bias (Generation of randomization sequences, allocation concealment, participants, investigators, data assessors, integrity of outcome data, and selective outcome reporting.
We analyzed the data through using RevMan Statistical Software (version 5.4) and Stata Statistical Software (version 12.0). The risk ratio (RR) and 95% confidence intervals (CI) were calculated by the proportion of patients with adverse reactions in the total patients. The presence of heterogeneity was assessed through using Cochran's Q statistics and quantified by I2 statistics. The fixed effect model was performed if I2 < 50, and the random effect model was used if I2 > 50. The α level was set at 0.05. A P value of < 0.05 indicates that the differences among the groups are significant. When there was statistical heterogeneity among the studies, sensitivity analysis would be performed to identify the source of heterogeneity. The inhibitory effects of oral probiotic use on the incidence of diarrhea and oral mucositis caused by chemotherapy were further analyzed in terms of continental region, duration of intake, and number of strains.
A total of 596 articles were acquired from the databases. Following the above inclusion and exclusion criteria, 507 articles (ongoing studies, unexpectedly terminated trials, non-cancer patients, not oral probiotic use, in vitro studies, non-chemotherapy studies, and reviews) and 38 duplicate articles were removed after carefully reading their titles and abstract, leaving only 51 articles. After reading the remaining articles, 39 additional studies were further excluded because of that 12 studies did not include cancer patients or they were not receiving chemotherapy (26–37), two did not include oral probiotic use (38, 39), 20 had no record of diarrhea or oral mucositis in patients (40–59) (18 of them did not include diarrhea or oral mucositis indicators (40–46, 49–59), and the other two studies only recorded the frequency of diarrhea or oral mucositis rather than the number of patients who had the adverse reactions (47, 48)), and five were not randomized controlled trials (60–64). Finally, 12 articles were selected for the meta-analysis. Figure 1 describes the screening procedure, and characteristics of the 12 included studies are shown in Table 1.
The clinical trials used in our meta-analysis were performed in multiple countries including Italy, India, Sweden, Japan, America, Thailand, Malaysia, and China. All patients were adults (≥ 18 years old), and they were diagnosed with cancer following the clinical guidelines for cancer diagnosis in their respective countries. All the patients in the 12 clinical trials had been treated by chemotherapy. Patients in three of the studies were treated by surgery plus chemotherapy (8, 9, 67), in five studies received radiation therapy in addition to chemotherapy (11, 13, 21, 65, 68), and in the remaining studies was treated by chemotherapy alone (10, 12, 66, 69). In addition, the included patients were diagnosed with seven types of cancers, including head and neck cancer (13, 68, 69), nasopharyngeal carcinoma (21, 65), colon cancer (8–10), esophageal cancer (65), cervical cancer (11), bladder cancer (67), and lung cancer (12). The clinical trials in the 12 studies were performed following the rule of randomized controlled trials. Detailed features of these studies have been described in Table 1.
The risk of bias was assessed using Cochrane Collaboration's tool (70). We determined the risk of bias based on the detailed description of the treatment process in the studies. The e-mail had been sent to the authors of the studies that did not elaborate on the treatment process, and the record was labeled “unclear” in Supplementary Table 1 if there was still no enough information. The risk of bias for each article was evaluated, which has been shown in Figure 2; Supplementary Table 1.
Chemotherapy-induced diarrhea is one of the main adverse reactions induced by chemotherapy, and it occurs in most cancer patients (71). Five of the 12 articles in the meta-analysis included cancer patients with diarrhea at all grades (≥ 1 grade) (diarrhea at all grades was used as an evaluation index in the clinical trials) (9, 10, 12, 66, 69). These studies were analyzed to determine whether oral administration of probiotics could decrease side effects in cancer patients receiving chemotherapy. One report demonstrated that oral probiotic use significantly reduced the incidence of diarrhea at all grades (12), and the others did not show statistically significance (9, 10, 66, 69). The forest plot revealed that the risk of diarrhea at all grades (RR = 0.70; 95% Cl: 0.56, 0.88; P = 0.002) (Figure 3) significantly decreased because of orally taking probiotics in comparison with the control group. No significant heterogeneity was found after implementing the fixed effect model (I2 = 2%; P = 0.39). Then, a subgroup analysis was conducted by continental region where the clinical trials were performed. The results demonstrated that orally taking probiotics could not reduce the incidence of diarrhea at all grade in European and American populations (RR: 0.69; 95% Cl: 0.39, 1.21; P = 0.20). However, this side effect significantly decreased in Asian populations because of oral probiotics use (RR: 0.70; 95% Cl: 0.56, 0.88; P = 0.002) (Figure 4). The Egger's test (P = 0.301) indicated that there was no significant publication bias (Supplementary Table 2).
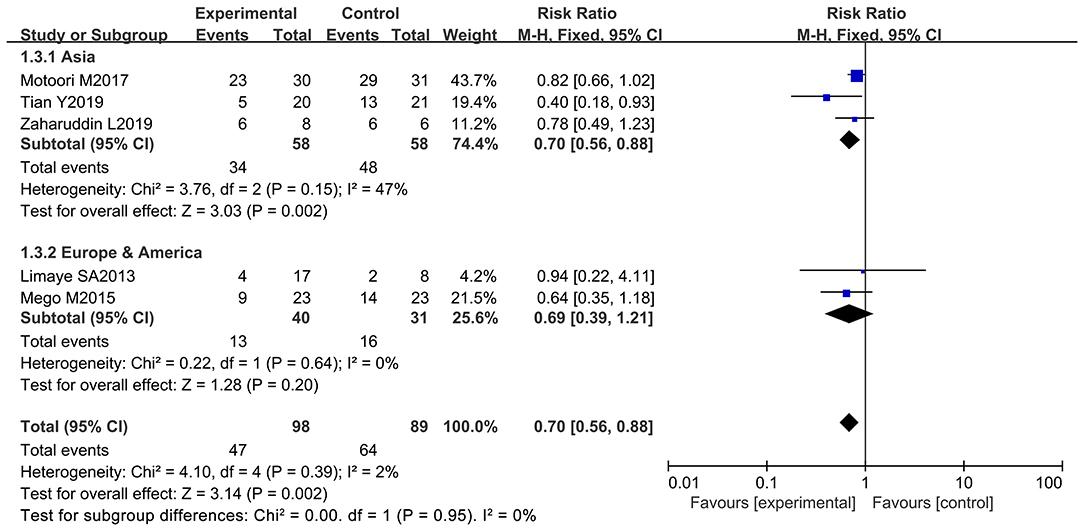
Figure 4. Subgroup analysis of the efficacy of oral probiotic use in the incidence reduction of diarrhea based on continental region in cancer patients.
Further analysis was performed to observe whether oral administration of probiotics could reduce the incidence of severe diarrhea (≥ 2 grade). Patients who developed severe diarrhea during chemotherapy were recorded by five of the 12 studies (only severe diarrhea (≥ 2 grade) was used as an evaluation index in the clinical trials) (10–12, 66, 67). However, only one study clarified that oral probiotic use significantly reduced the incidence of severe diarrhea (11), and the other studies did not exhibit statistically significance (10, 12, 66, 67). Statistical analysis demonstrated that the use of probiotics decreased the severe diarrhea incidence in the cancer patients compared to the control groups (RR: 0.50; 95% Cl: 0.32, 0.78; P = 0.002) (Figure 5). No significant heterogeneity was found among the studies after implementing the fixed effect model (I2 = 22%; P = 0.28). Furthermore, the five studies were categorized and sorted into Asia (11, 12, 66, 67) and western countries (European and American) (10). Severe diarrhea incidence was clearly reduced in Asian cancer patients after oral probiotic use (RR: 0.47; 95% Cl: 0.29, 0.77; P = 0.003). There was no significant difference between the control groups and the experimental groups in European and America populations (RR: 0.67; 95% Cl: 0.22, 2.05; P = 0.48) (Figure 6). Importantly, no significant publication bias among the studies was found after conducting the Egger's test (P = 0.838) (Supplementary Table 3).
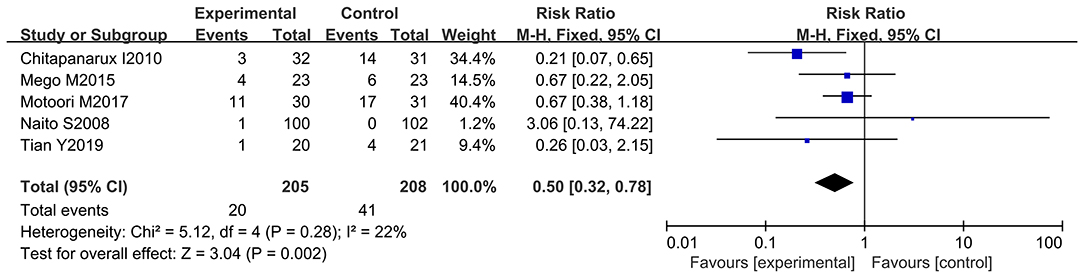
Figure 5. Forest plot of orally administrated probiotics for reducing severe diarrhea in cancer patients.
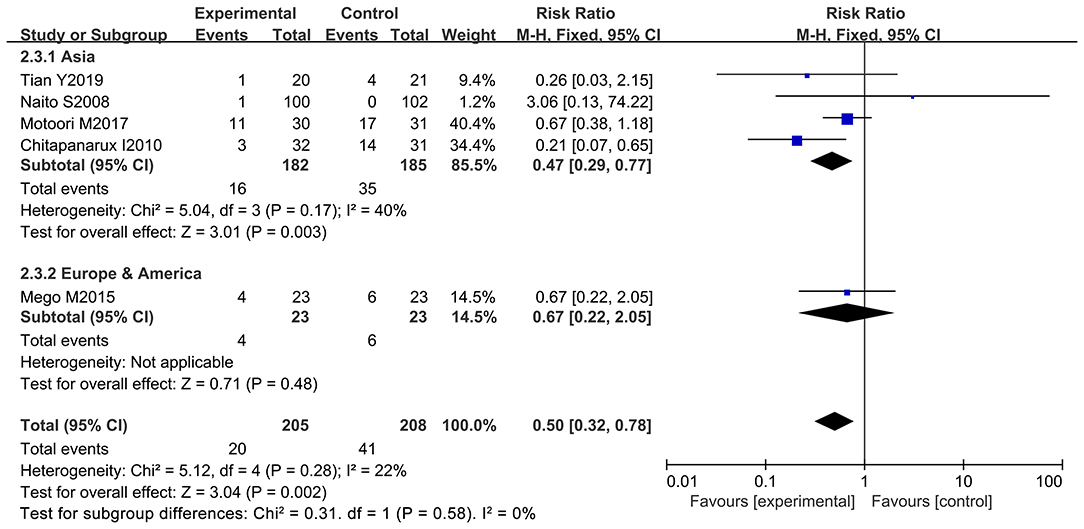
Figure 6. Subgroup analysis of orally administrated probiotics for reducing severe diarrhea in cancer patients based on continental region.
Many studies reported oral mucositis as a significant adverse reaction of chemotherapy (72). Oral mucositis may lead to serious oral pain, which impairs nutritional intake, quality of life, and treatment regimens (73). Four of the 12 articles documented patients with all grades of oral mucositis (oral mucositis at all grades was used as an evaluation index in the clinical trials) due to chemotherapy (13, 21, 65, 66). Of note, three studies demonstrated that oral probiotic use significantly reduced the incidence of oral mucositis at all grades (13, 21, 65), and one did not have statistically significance (66). The forest plot indicated that oral administration of probiotics was closely associated with a lower incidence of oral mucositis in cancer patients undergoing chemotherapy (RR: 0.84; 95% Cl: 0.78, 0.91; P < 0.00001) (Figure 7). No significant heterogeneity was found among the studies (I2 = 28.0%; P = 0.24). Due to the low number of samples, the subgroup analysis by the continental region and duration of intake was not performed for the oral mucositis incidence at all grades. Besides, we did not find significant publication bias after evaluating our results with the Egger's test (P = 0.839) (Supplementary Table 4).
Patient data taken from seven studies were used to analyze patients with severe oral mucositis (≥ 3 grade) (only severe oral mucositis was used as an evaluation index in the clinical trials) (8, 13, 21, 66–69). Notably, two of the seven studies support the beneficial effects of oral probiotic use on the incidence reduction of severe oral mucositis (13, 65), and the other five studies did not have statistically significance (8, 21, 66, 68, 69). The forest plot signified that no significant heterogeneity occurred among the studies (I2 = 13%; P = 0.33). Statistical analysis showed that few patients undergoing chemotherapy developed severe oral mucositis (≥ 3 grade) because of oral probiotic use in comparison with the control group (RR: 0.66; 95% Cl: 0.55, 0.79; P < 0.00001) (Figure 8). The subgroup analysis further demonstrated that taking probiotics lowered the incidence of severe oral mucositis in Asian populations (RR: 0.59; 95% Cl: 0.48, 0.73; P < 0.00001), but not in European and American populations (RR: 0.84; 95% Cl: 0.60, 1.18; P = 0.32) (Figure 9). The Egger's Test (P = 0.450) did not find a significant publication bias among the studies (Supplementary Table 5).
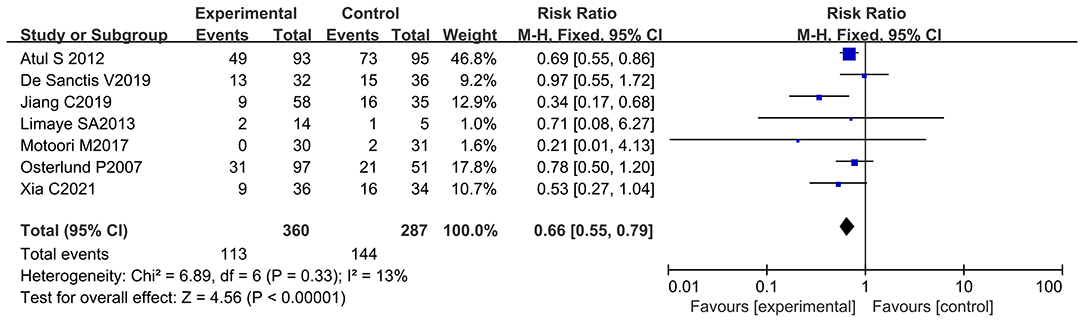
Figure 8. Forest plot of orally administrated probiotics for reducing severe oral mucositis in cancer patients.
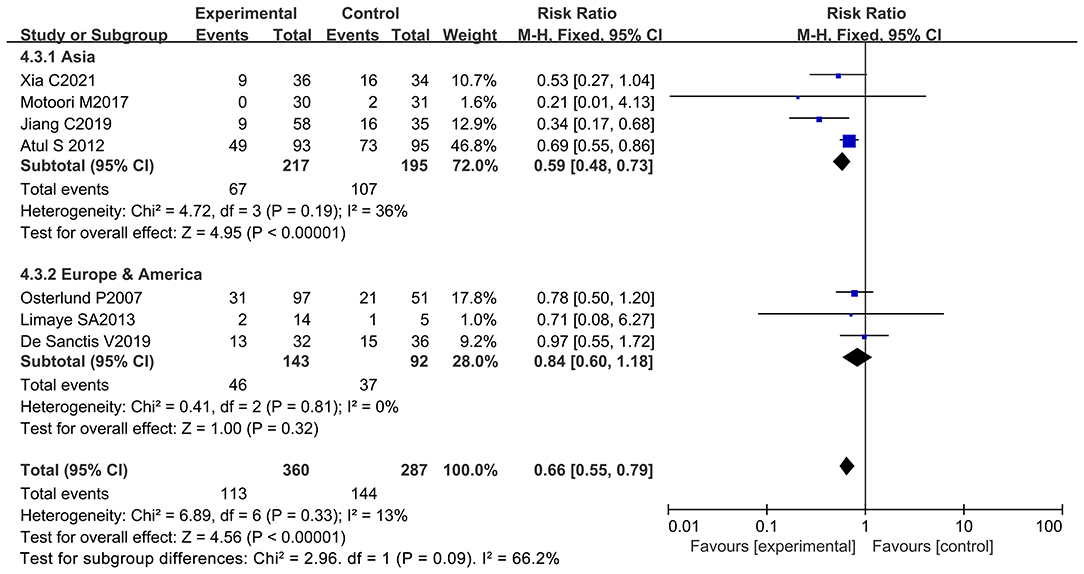
Figure 9. Subgroup analysis of the efficacy of oral probiotic use against severe oral mucositis in cancer patients based on continental region.
Despite the beneficial effects of oral probiotic use on the reduction of diarrhea and oral mucositis during chemotherapy, the probiotics used in the 12 studies are very different in bacterial species and number. Six of the 12 studies used only one species of bacterium as active ingredient (8, 12, 13, 67–69) while other studies employed a mixture of multiple strains (9–11, 21, 65, 66) The results revealed that the treatment scheme of multiple strains significantly reduced diarrhea at all grades (RR: 0.76; 95% Cl: 0.62, 0.95; P = 0.01) and severe diarrhea (RR: 0.49; 95% Cl: 0.31, 0.78; P = 0.003). However, the single strain did not exhibit any significant effects on the incidence reduction of diarrhea at all grades (RR: 0.50; 95% Cl: 0.24, 1.02; P = 0.06) or severe diarrhea (RR: 0.58; 95% Cl: 0.13, 2.60; P = 0.47) (Figures 10, 11). Also, the treatment strategy containing multiple species of bacteria significantly decreased the incidence of oral mucositis at all grades (RR: 0.90; 95% Cl: 0.83, 0.97; P = 0.007) and severe oral mucositis (RR: 0.41; 95% Cl: 0.26, 0.66; P = 0.0003). Simultaneously, the use of single strain could also significantly lower the incidence of oral mucositis at all grades (RR: 0.78; 95% Cl: 0.68, 0.89; P = 0.0004) and severe oral mucositis (RR: 0.74; 95% Cl: 0.61, 0.90; P = 0.002) (Figures 12, 13). Collectively, oral administration of multiple strains was better than the single bacterium in the management of diarrhea and oral mucositis during chemotherapy. This could be probably due to the synergistic effects of a great number of metabolites produced by various different probiotics, the advantages of which in health management have been claimed by many studies (74, 75). The number of probiotics, strain name, drug appearance, dosage, frequency intake per day, and duration of intake are summarized in Table 2.
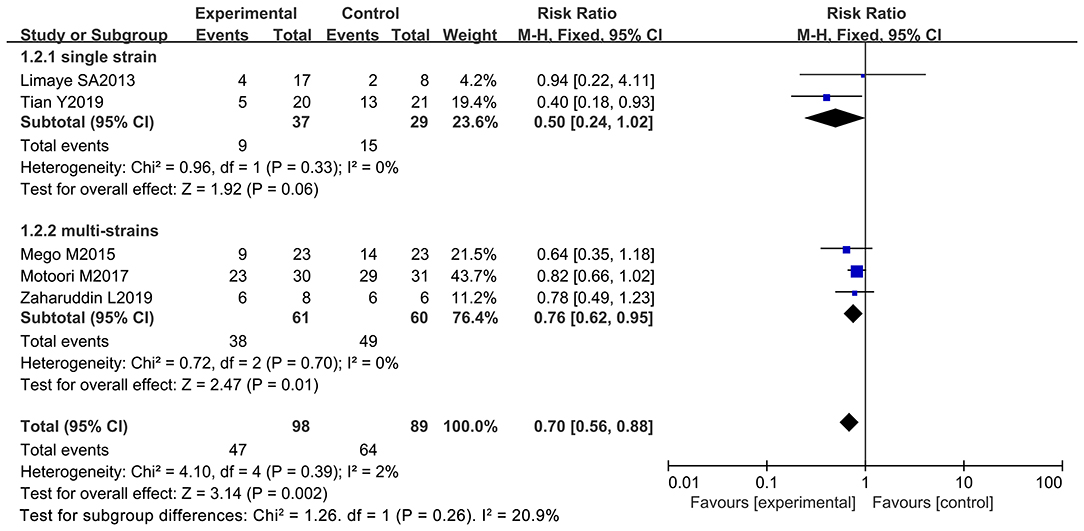
Figure 10. Subgroup analysis of the effect of the bacterial number on the incidence reduction of diarrhea in cancer patients.
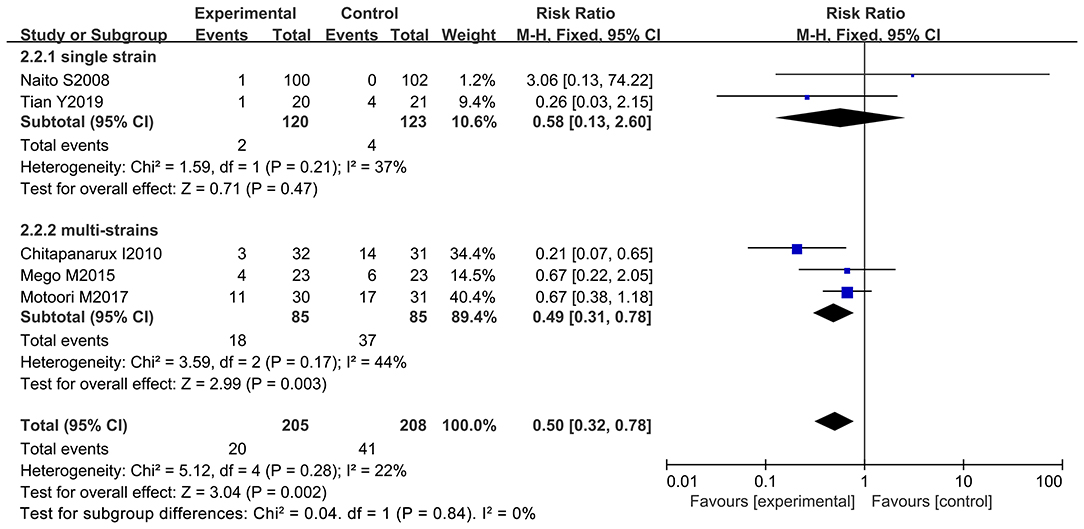
Figure 11. Subgroup analysis of the efficacy of bacterial number on the incidence of severe diarrhea in cancer patients.
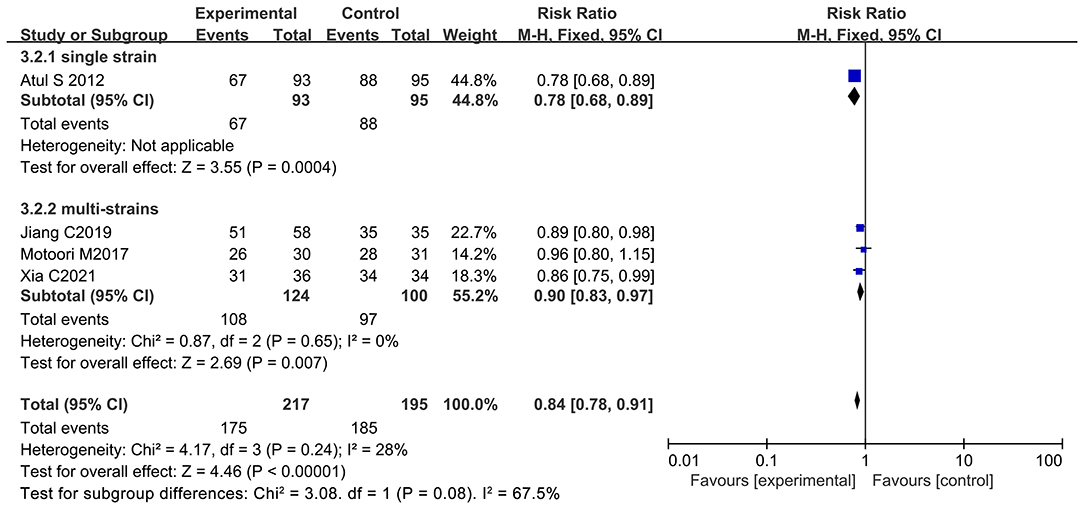
Figure 12. Subgroup analysis of the inhibitory effect of bacterial number on the incidence of oral mucositis in cancer patients.
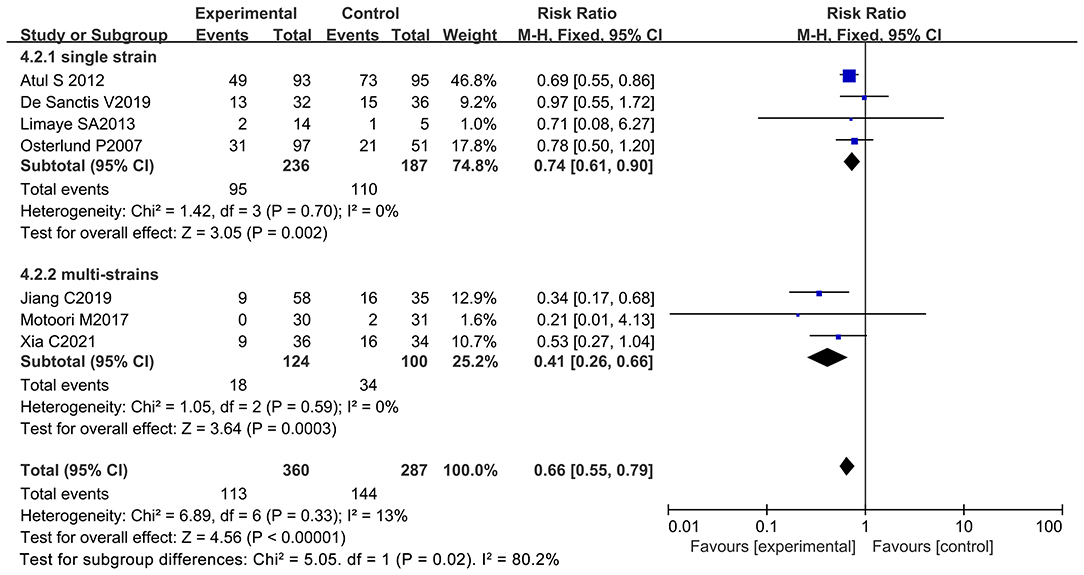
Figure 13. Subgroup analysis of the effect of bacterial number on the incidence reduction of severe oral mucositis in cancer patients.
A total of twelve articles including 1,013 patients were recruited for the meta-analysis after conducting standard search and selection criteria. No significant heterogeneity or publication bias was found among the articles. Oral administration of probiotics could significantly decrease diarrhea and oral mucositis incidence in cancer patients undergoing chemotherapy compared with the control group. No death or adverse effects due to oral probiotic supplementation were recorded. In detail, seven studies reported that patients could safely ingest probiotics (8–10, 12, 13, 65, 69), and two studies demonstrated the high tolerance of patients to them (8, 69). Interestingly, six of the 12 studies used only one bacterium as active ingredient (8, 12, 13, 67–69) while other studies employed a mixture of multiple strains (9–11, 21, 65, 66) (Table 2). It should be noted that most strains used in the clinical studies, including Lactobacillus brevis CD2, VSL#3, and Lactobacillus rhamnosus GG, have already been well-studied for treating acute gastroenteritis (76), irritable bowel syndrome (77, 78), and ulcerative colitis (79). This indicates that most probiotics used to regulate intestinal microecology have potential to reduce the adverse effects in cancer therapy. Notably, the decrease of chemotherapy-induced side effects associated with probiotic use only occurred in Asian populations, not in European or American populations. This could be possibly ascribed to the ethnic difference that the people in the western countries used to daily taking probiotics that contained in the various fermented foods, resulting in the immunologic tolerance to the probiotics (22). Therefore, additional clinical studies should be conducted to thoroughly evaluate the inhibitory effects of oral probiotic use on the adverse effects caused by chemotherapy.
Moreover, it would be interesting to understand the mechanisms underlying chemotherapy-induced side effects to assist in the search of new drugs to treat cancer patients. A series of in vitro and in vivo experiments revealed that chemotherapeutic drugs induce crypt cell apoptosis as well as histopathological changes in the small intestine and colon, resulting in the alteration of intestinal absorption and subsequent diarrhea (80, 81). Chemotherapeutic drugs change the intestinal flora, destroy the dynamic balance of the intestinal tract, and lead to diarrhea (82). Also, chemotherapeutic drugs target basal epithelial cells to produce reactive oxygen species. Subsequently, mucus cells release inflammatory cytokines and induce cell apoptosis (83). Conversely, probiotics are particularly advantageous in resisting pathogenic bacteria and maintaining the intestinal microecological balance (84, 85). Specific probiotics, such as lactobacillus, may alter the gene expression that involved in inflammation and cell apoptosis and reverse the adverse events (86). These beneficial effects of probiotics possibly contribute to the incidence reduction of adverse reactions caused by chemotherapy in some cancer patients of the included studies.
However, small samples (1,013 patients) in the meta-analysis are not sufficient to fully assess the beneficial effects of oral probiotic use on the incidence reduction of adverse reactions in cancer patients during chemotherapy. Additionally, not all patients in the meta-analysis strictly adhered to a single treatment by chemotherapy. Some patients were treated with two clinical methods, such as chemoradiotherapy or surgery plus chemotherapy. Simultaneously, eight of the included 12 studies used placebo as the control (9–13, 21, 65, 69), and the remaining studies just used other bacteria or non-treatment as the control (8, 66–68). More important, despite the statistical results of data extracted from the 12 studies revealed the inhibitory effects of oral probiotic use on the incidence of diarrhea and oral mucositis during chemotherapy, only two studies demonstrated the relieve of diarrhea while three studies indicated the incidence reduction of oral mucositis in the cancer patients. Simultaneously, the species and number of strains used in the clinical trials of the meta-analysis were totally different, indicating the imperative requirement to further explore the valuable probiotics and the preparation of multi-strain combination in the management of these chemotherapy-induced side effects. Of note, considering the negative result caused by ethnic difference in the meta-analysis, probiotic species should be also seriously considered when use them to assist cancer treatment in different ethnicities. Thus, more clinical trials and basic researches are needed to fully address these limitations prior to clinical application of the probiotics.
Collectively, this meta-analysis presented the efficacy of orally administered probiotics in the incidence reduction of diarrhea and oral mucositis in cancer patients during chemotherapy based on multiple clinical trials, and the mechanism underlying the action was also discussed. Considering the crucial role of chemotherapy in cancer treatment, the conclusion of the meta-analysis could provide some suggestions for people to control chemotherapy-induced adverse effects. Future studies should further evaluate the efficacy of probiotics in the management of adverse reactions in cancer patients during chemotherapy through conducting more clinical trials, and also determine the most effective probiotic species, the doses of each strain, and the dosing schedule for probiotic use in alleviating the side effects.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding authors.
YZ, JF, and MG conceived and designed the research. YZ had primary responsibility for final content, established eligibility criteria and search strategy. JF and MG conducted the database search and screened. JY and CZ worked on literature selection, data extraction and quality assessment. JF, HG, XL, and XZ performed statistical analysis. MG, RJ, and CZ prepared the figures and tables. All authors read the manuscript and approved the final draft.
This research was supported by the National Natural Science Foundation of China (grant number: 81971726).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Thanks to all the authors and patients of previous research for providing the data in the study.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fnut.2022.823288/full#supplementary-material
1. Andreyev J, Ross P, Donnellan C, Lennan E, Leonard P, Waters C, et al. Guidance on the management of diarrhoea during cancer chemotherapy. Lancet Oncol. (2014) 15:e447–e60. doi: 10.1016/S1470-2045(14)70006-3
2. Prieto-Callejero B, Rivera F, Fagundo-Rivera J, Romero A, Romero-Martin M, Gomez-Salgado J, et al. Relationship between chemotherapy-induced adverse reactions and health-related quality of life in patients with breast cancer. Medicine (Baltimore). (2020) 99:1–10. doi: 10.1097/MD.0000000000021695
3. Qin N, Jiang G, Zhang X, Sun D, Liu M. The effect of nutrition intervention with oral nutritional supplements on ovarian cancer patients undergoing chemotherapy. Front Nutr. (2021) 8:685967. doi: 10.3389/fnut.2021.685967
4. Elad S, Cheng KKF, Lalla RV, Yarom N, Hong C, Logan RM, et al. MASCC/ISOO clinical practice guidelines for the management of mucositis secondary to cancer therapy. Cancer. (2020) 126:4423–31. doi: 10.1002/cncr.33100
5. Wu X, Xia Y, He F, Zhu C, Ren W. Intestinal mycobiota in health and diseases: from a disrupted equilibrium to clinical opportunities. Microbiome. (2021) 9:60–77. doi: 10.1186/s40168-021-01024-x
6. Sommer F, Anderson JM, Bharti R, Raes J, Rosenstiel P. The resilience of the intestinal microbiota influences health and disease. Nat Rev Microbiol. (2017) 15:630–8. doi: 10.1038/nrmicro.2017.58
7. Nathan NN, Philpott DJ, Girardin SE. The intestinal microbiota: from health to disease, and back. Microbes Infect. (2021) 23:104849. doi: 10.1016/j.micinf.2021.104849
8. Osterlund P, Ruotsalainen T, Korpela R, Saxelin M, Ollus A, Valta P, et al. Lactobacillus supplementation for diarrhoea related to chemotherapy of colorectal cancer: a randomised study. Br J Cancer. (2007) 97:1028–34. doi: 10.1038/sj.bjc.6603990
9. Zaharuddin L, Mokhtar NM, Muhammad Nawawi KN, Raja Ali RA. A randomized double-blind placebo-controlled trial of probiotics in post-surgical colorectal cancer. BMC Gastroenterol. (2019) 19:131–8. doi: 10.1186/s12876-019-1047-4
10. Mego M, Chovanec J, Vochyanova-Andrezalova I, Konkolovsky P, Mikulova M, Reckova M, et al. Prevention of irinotecan induced diarrhea by probiotics: a randomized double blind, placebo controlled pilot study. Complement Ther Med. (2015) 23:356–62. doi: 10.1016/j.ctim.2015.03.008
11. Chitapanarux I, Chitapanarux T, Traisathit P, Kudumpee S, Tharavichitkul E, Lorvidhaya V. Randomized controlled trial of live lactobacillus acidophilus plus Bifidobacterium bifidum in prophylaxis of diarrhea during radiotherapy in cervical cancer patients. Radiat Oncol. (2010) 5:31–6. doi: 10.1186/1748-717X-5-31
12. Tian Y, Li M, Song W, Jiang R, Li YQ. Effects of probiotics on chemotherapy in patients with lung cancer. Oncol Lett. (2019) 17:2836–48. doi: 10.3892/ol.2019.9906
13. Atul S, Rath GK, Chaudhary SP, Thakar A, Mohanti BK, Bahadur S. Lactobacillus brevis CD2 lozenges reduce radiation-and chemotherapy-induced mucositis in patients with head and neck cancer: a randomized double-blind placebo-controlled study. Eur J Cancer. (2012) 48:875–81. doi: 10.1016/j.ejca.2011.06.010
14. Wei D, Heus P, van de Wetering FT, van Tienhoven G, Verleye L, Scholten RJ. Probiotics for the prevention or treatment of chemotherapy or radiotherapy-related diarrhoea in people with cancer. Cochrane Database Syst Rev. (2018) 8:1–71. doi: 10.1002/14651858.CD008831.pub3
15. Sanders ME, Merenstein DJ, Reid G, Gibson GR, Rastall RA. Probiotics and prebiotics in intestinal health and disease: from biology to the clinic. Nat Rev Gastroenterol Hepatol. (2019) 16:605–16. doi: 10.1038/s41575-019-0173-3
16. Baarlen PV, Troost F, Meer CV, Hooiveld G, Boekschoten M, Brummer RJ, et al. Human mucosal in vivo transcriptome responses to three lactobacilli indicate how probiotics may modulate human cellular pathways. Proc Natl Acad Sci U S A. (2011) 108(Suppl. 1):4562–9. doi: 10.1073/pnas.1000079107
17. Rodríguez GI, Gaspar P, Sánchez B, Gueimonde M, Margolles A, Neves AR. Catabolism of glucose and lactose in Bifidobacterium animalis subsp. lactis, studied by 13C nuclear magnetic resonance. Appl Environ Microbiol. (2013) 79:7628–38. doi: 10.1128/AEM.02529-13
18. Sanders ME, Benson A, Lebeer S, Merenstein DJ, Klaenhammer TR. Shared mechanisms among probiotic taxa: implications for general probiotic claims. Curr Opin Biotechnol. (2018) 49:207–16. doi: 10.1016/j.copbio.2017.09.007
19. Shu Z, Li P, Yu B, Huang S, Chen Y. The effectiveness of probiotics in prevention and treatment of cancer therapy-induced oral mucositis: a systematic review and meta-analysis. Oral Oncol. (2020) 102:1–11. doi: 10.1016/j.oraloncology.2019.104559
20. Lu D, Yan J, Liu F, Ding P, Chen B, Lu Y, et al. Probiotics in preventing and treating chemotherapyinduced diarrhea: a meta-analysis. Asia Pac J Clin Nutr. (2019) 28:701–10. doi: 10.6133/apjcn.201912_28(4).0005
21. Xia C, Jiang C, Li W, Wei J, Hong H, Li J, et al. A phase II randomized clinical trial and mechanistic studies using improved probiotics to prevent oral mucositis induced by concurrent radiotherapy and chemotherapy in nasopharyngeal carcinoma. Front Immunol. (2021) 12:618150. doi: 10.3389/fimmu.2021.618150
22. Ozen M, Dinleyici EC. The history of probiotics: the untold story. Benef Microbes. (2015) 6:159–65. doi: 10.3920/BM2014.0103
23. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. (2021) 29:372–81. doi: 10.1136/bmj.n71
24. Freites-Martinez A, Santana N, Arias-Santiago S., Viera A. Using the common terminology criteria for adverse events (CTCAE-Version 50) to evaluate the severity of adverse events of anticancer therapies. Actas Dermosifiliogr (Engl Ed). (2021) 112:90–2. doi: 10.1016/j.adengl.2019.05.021
25. Klopp AH, Yeung AR, Deshmukh S, Gil KM, Wenzel L, Westin SN, et al. Patient-reported toxicity during pelvic intensity-modulated radiation therapy: NRG Oncology-RTOG 1203. J Clin Oncol. (2018) 36:2538–44. doi: 10.1200/JCO.2017.77.4273
26. Agosta C, Atlante M, Benvenuti C. Randomized controlled study on clinical efficacy of isoflavones plus Lactobacillus sporogenes, associated or not with a natural anxiolytic agent in menopause. Minerva Ginecol. (2011) 63:11–7.
27. Sari FN, Dizdar EA, Oguz S, Erdeve O, Uras N, Dilmen U. Oral probiotics: Lactobacillus sporogenes for prevention of necrotizing enterocolitis in very low-birth weight infants: a randomized, controlled trial. Eur J Clin Nutr. (2011) 65:434–9. doi: 10.1038/ejcn.2010.278
28. Bellikci-Koyu E, Sarer-Yurekli BP, Akyon Y, Aydin-Kose F, Karagozlu C, Ozgen AG, et al. Effects of regular kefir consumption on gut microbiota in patients with metabolic syndrome: a parallel-group, randomized, controlled study. Nutrients. (2019) 11:2089–111. doi: 10.3390/nu11092089
29. Wang Y, Dilidaxi D, Wu Y, Sailike J, Sun X, Nabi XH. Composite probiotics alleviate type 2 diabetes by regulating intestinal microbiota and inducing GLP-1 secretion in db/db mice. Biomed Pharmacother. (2020) 125:1–11. doi: 10.1016/j.biopha.2020.109914
30. Elsharkawy I, Noureldin E, Mohamed E, Mohamed A, Abdeldayem H, Mansour SAM. Continuous versus interrupted use of vaginal probiotics plus vaginal clindamycin cream for bacterial vaginosis: a randomized controlled study. J Matern Fetal Neonatal Med. (2021) 34:58–65. doi: 10.1080/14767058.2019.1588246
31. Ciernikova S, Mego M, Drgona L, Semanova M, Wachsmannova L, Adamcikova Z, et al. An informative study about probiotic use between slovak cancer patients. J Clin Gastroenterol. (2016) 50:S215–6. doi: 10.1177/1534735416643828
32. Demers M, Dagnault A, Desjardins J. A randomized double-blind controlled trial: impact of probiotics on diarrhea in patients treated with pelvic radiation. Clin Nutr. (2014) 33:761–7. doi: 10.1016/j.clnu.2013.10.015
33. Linn YH, Thu KK, Win NHH. Effect of probiotics for the prevention of acute radiation-induced diarrhoea among cervical cancer patients: a randomized double-blind placebo-controlled study. Probiotics Antimicrob Proteins. (2018) 11:638–47. doi: 10.1007/s12602-018-9408-9
34. Dizman N, Hsu J, Bergerot PG, Gillece JD, Folkerts M, Reining L, et al. Randomized trial assessing impact of probiotic supplementation on gut microbiome and clinical outcome from targeted therapy in metastatic renal cell carcinoma. Cancer Med. (2020) 10:79–86. doi: 10.1002/cam4.3569
35. Okawa T, Niibe H, Arai T, Sekiba K, Noda K, Takeuchi S, et al. Effect of LC9018 combined with radiation therapy on carcinoma of the uterine cervix. A phase III, multicenter, randomized, controlled study. Cancer. (1993) 72:1949–54. doi: 10.1002/1097-0142(19930915)72:6<1949::AID-CNCR2820720626>3.0.CO;2-W
36. Butov DA, Efremenko YV, Prihoda ND, Zaitzeva SI, Yurchenko LV, Sokolenko NI, et al. Randomized, placebo-controlled phase II trial of heat-killed Mycobacterium vaccae (Immodulon batch) formulated as an oral pill (V7). Immunotherapy. (2013) 5:1047–54. doi: 10.2217/imt.13.110
37. DeMaria PJ, Bilusic M, Park DM, Heery CR, Donahue RN, Madan RA, et al. Randomized, double-blind, placebo-controlled phase II study of Yeast-Brachyury vaccine (GI-6301) in combination with standard-of-care radiotherapy in locally advanced, unresectable chordoma. Oncologist. (2021) 26:e847–e58. doi: 10.1002/onco.13720
38. Holma R, Korpela R, Sairanen U, Blom M, Rautio M, Poussa T, et al. Colonic methane production modifies gastrointestinal toxicity associated with adjuvant 5-fluorouracil chemotherapy for colorectal cancer. J Clin Gastroenterol. (2013) 47:45–51. doi: 10.1097/MCG.0b013e3182680201
39. Assersohn L, Souberbielle BE, O'Brien ME, Archer CD, Mendes R, Bass R, et al. A randomized pilot study of SRL172 (Mycobacterium vaccae) in patients with small cell lung cancer (SCLC) treated with chemotherapy. Clin Oncol (R Coll Radiol). (2002) 14:23–7. doi: 10.1053/clon.2001.0030
40. Bajramagic S, Hodzic E, Mulabdic A, Holjan S, Smajlovic SV, Rovcanin A. Usage of probiotics and its clinical significance at surgically treated patients sufferig from colorectal carcinoma. Med Arch. (2019) 73:316–20. doi: 10.5455/medarh.2019.73.316-320
41. Liu J, Huang XE. Efficacy of Bifidobacterium tetragenous viable bacteria tablets for cancer patients with functional constipation. Asian Pac J Cancer Prev. (2014) 15:10241–4. doi: 10.7314/APJCP.2014.15.23.10241
42. Bergerot P, Philip EJ, Bergerot CD, Dizman N, Salgia M, Salgia N, et al. Pilot study to evaluate the biologic effect of the probiotic CBM588 in combination with nivolumab/ ipilimumab for patients with mRCC. Kidney cancer. (2020) 4:45–6. doi: 10.3233/KCA-200001
43. Donders G, Neven P, Moegele M, Lintermans A, Bellen G, Prasauskas V, et al. Ultra-low-dose estriol and Lactobacillus acidophilus vaginal tablets (Gynoflor((R))) for vaginal atrophy in postmenopausal breast cancer patients on aromatase inhibitors: pharmacokinetic, safety, and efficacy phase I clinical study. Breast Cancer Res Treat. (2014) 145:371–9. doi: 10.1007/s10549-014-2930-x
44. Farshi Radvar F, Mohammad-Zadeh M, Mahdavi R, Andersen V, Nasirimotlagh B, Faramarzi E, et al. Effect of synbiotic supplementation on matrix metalloproteinase enzymes, quality of life and dietary intake and weight changes in rectal cancer patients undergoing neoadjuvant chemoradiotherapy. Med J Nutrition Metab. (2020) 13:225–35. doi: 10.3233/MNM-200413
45. Mego M, Ebringer L, Drgona L, Mardiak J, Trupl J, Greksak R, et al. Prevention of febrile neutropenia in cancer patients by probiotic strain Enterococcus faecium M-74. Pilot study phase I. Neoplasma. (2005) 52:159–64. doi: 10.1007/s00520-005-0891-7
46. Riechelmann R, Camandaroba M, Mello C., Souza e, Silva V, Felismino T, Jesus V, et al. P-54 BISQUIT: a randomized phase II study of the administration of prebiotics and probiotics during definitive treatment with chemotherapy-radiotherapy for patients with squamous cell carcinoma of the anal canal. Ann Oncol. (2020) 31:107–8. doi: 10.1016/j.annonc.2020.04.136
47. Wada M, Nagata S, Saito M, Shimizu T, Yamashiro Y, Matsuki T, et al. Effects of the enteral administration of Bifidobacterium breve on patients undergoing chemotherapy for pediatric malignancies. Support Care Cancer. (2010) 18:751–9. doi: 10.1007/s00520-009-0711-6
48. Golkhalkhali B, Rajandram R, Paliany AS, Ho GF, Wan Ishak WZ, Johari CS, et al. Strain-specific probiotic (microbial cell preparation) and omega-3 fatty acid in modulating quality of life and inflammatory markers in colorectal cancer patients: a randomized controlled trial. Asia Pac J Clin Oncol. (2017) 14:179–91. doi: 10.1111/ajco.12758
49. Ali RAR, Zaharuddin L, Chan SN, Wong Z, Ngiu CS, Mokhtar NM. The clinical and circulating inflammatory cytokines effects of probiotic containing lactobacillus and bifidobacterium strains in patients with colorectal cancer: a randomized double blind controlled trial. Gastroenterology. (2018) 154:414–5. doi: 10.1016/S0016-5085(18)31661-5
50. Marschalek J, Farr A, Marschalek M, Domig KJ, Kneifel W, Singer CF, et al. Influence of orally administered probiotic lactobacillus strains on vaginal microbiota in women with breast cancer during chemotherapy: a randomized placebo-controlled double-blinded pilot study. Breast Care (Basel). (2017) 12:335–9. doi: 10.1159/000478994
51. De Loera Rodríguez LH, Ortiz GG, Rivero Moragrega P, Velázquez Brizuela IE, Santoscoy Gutiérrez JF, Rincón Sánchez AR, et al. Effect of symbiotic supplementation on fecal calprotectin levels and lactic acid bacteria, Bifidobacteria, Escherichia coli and Salmonella DNA in patients with cervical cancer. Nutr Hosp. (2018) 35:1394–400. doi: 10.20960/nh.1762
52. O'Brien ME, Saini A, Smith IE, Webb A, Gregory K, Mendes R, et al. A randomized phase II study of SRL172 (Mycobacterium vaccae) combined with chemotherapy in patients with advanced inoperable non-small-cell lung cancer and mesothelioma. Br J Cancer. (2000) 83:853–7. doi: 10.1054/bjoc.2000.1401
53. Stanford JL, Stanford CA, O'Brien ME, Grange JM. Successful immunotherapy with Mycobacterium vaccae in the treatment of adenocarcinoma of the lung. Eur J Cancer. (2008) 44:224–7. doi: 10.1016/j.ejca.2007.08.021
54. Cananzi FC, Mudan S, Dunne M, Belonwu N, Dalgleish AG. Long-term survival and outcome of patients originally given Mycobacterium vaccae for metastatic malignant melanoma. Hum Vaccin Immunother. (2013) 9:2427–33. doi: 10.4161/hv.25618
55. Bilusic M, Heery CR, Arlen PM, Rauckhorst M, Apelian D, Tsang KY, et al. Phase I trial of a recombinant yeast-CEA vaccine (GI-6207) in adults with metastatic CEA-expressing carcinoma. Cancer Immunol Immunother. (2014) 63:225–34. doi: 10.1007/s00262-013-1505-8
56. Chaft JE, Litvak A, Arcila ME, Patel P, D'Angelo SP, Krug LM, et al. Phase II study of the GI-4000 KRAS vaccine after curative therapy in patients with stage I-III lung adenocarcinoma harboring a KRAS G12C, G12D, or G12V mutation. Clin Lung Cancer. (2014) 15:405–10. doi: 10.1016/j.cllc.2014.06.002
57. Stebbing J, Dalgleish A, Gifford-Moore A, Martin A, Gleeson C, Wilson G, et al. An intra-patient placebo-controlled phase I trial to evaluate the safety and tolerability of intradermal IMM-101 in melanoma. Ann Oncol. (2012) 23:1314–9. doi: 10.1093/annonc/mdr363
58. Stanford J, Stanford C, Dlugovitzky D, Fiorenza G, Martinel-Lamas D, Selenscig D, et al. Potential for immunotherapy with heat-killed Mycobacterium vaccae in respiratory medicine. Immunotherapy. (2009) 1:933–47. doi: 10.2217/imt.09.62
59. Xia W, Hilgenbrink AR, Matteson EL, Lockwood MB, Cheng JX, Low PS, et al. functional folate receptor is induced during macrophage activation and can be used to target drugs to activated macrophages. Blood. (2009) 113:438–46. doi: 10.1182/blood-2008-04-150789
60. Chaudhary S, Sharma A, Tilak T, Bakhshi S, Raina V, Kumar L, et al. Pilot study of efficacy of lactobacillus CD2 lozenges in preventing high-dose chemotherapy induced oral mucositis in patients undergoing hematopoietic stem celltransplantation. Support Care Cancer. (2014) 22:1–238. doi: 10.1007/s00520-014-2222-3
61. Lacouture ME, Keefe DM, Sonis S, Jatoi A, Gernhardt D, Wang T, et al. A phase II study (ARCHER 1042) to evaluate prophylactic treatment of dacomitinib-induced dermatologic and gastrointestinal adverse events in advanced non-small-cell lung cancer. Ann Oncol. (2016) 27:1712–8. doi: 10.1093/annonc/mdw227
62. Guarino A, Guandalini S, Lo Vecchio A. Probiotics for prevention and treatment of diarrhea. J Clin Gastroenterol. (2015) 1:37–45. doi: 10.1097/MCG.0000000000000349
63. Zhang C, Zhang Z, Wang L, Han J, Li F, Shen C, et al. Pseudomonas aeruginosa-mannose sensitive hemagglutinin injection treated cytokine-induced killer cells combined with chemotherapy in the treatment of malignancies. Int Immunopharmacol. (2017) 51:57–65. doi: 10.1016/j.intimp.2017.08.003
64. Patel PM, Sim S, O'Donnell DO, Protheroe A, Beirne D, Stanley A, et al. An evaluation of a preparation of Mycobacterium vaccae (SRL172) as an immunotherapeutic agent in renal cancer. Eur J Cancer. (2008) 44:216–23. doi: 10.1016/j.ejca.2007.11.003
65. Jiang C, Wang H, Xia C, Dong Q, Chen E, Qiu Y, et al. A randomized, double-blind, placebo-controlled trial of probiotics to reduce the severity of oral mucositis induced by chemoradiotherapy for patients with nasopharyngeal carcinoma. Cancer. (2019) 125:1081–90. doi: 10.1002/cncr.31907
66. Motoori M, Yano M, Miyata H, Sugimura K, Saito T, Omori T, et al. Randomized study of the effect of synbiotics during neoadjuvant chemotherapy on adverse events in esophageal cancer patients. Clin Nutr. (2017) 36:93–9. doi: 10.1016/j.clnu.2015.11.008
67. Naito S, Koga H, Yamaguchi A, Fujimoto N, Hasui Y, Kuramoto H, et al. Prevention of recurrence with epirubicin and Lactobacillus casei after transurethral resection of bladder cancer. J Urol. (2008) 179:485–90. doi: 10.1016/j.juro.2007.09.031
68. De Sanctis V, Belgioia L, Cante D, La Porta MR, Caspiani O, Guarnaccia R, et al. Lactobacillus brevis CD2 for prevention of oral mucositis in patients with head and neck tumors: a multicentric randomized study. Anticancer Res. (2019) 39:1935–42. doi: 10.21873/anticanres.13303
69. Limaye SA, Haddad RI, Cilli F, Sonis ST, Colevas AD, Brennan MT, et al. Phase 1b, multicenter, single blinded, placebo-controlled, sequential dose escalation study to assess the safety and tolerability of topically applied AG013 in subjects with locally advanced head and neck cancer. Cancer. (2013) 119:4268–76. doi: 10.1002/cncr.28365
70. Higgins JP, Altman DG, Gotzsche PC, Juni P, Moher D, Oxman AD, et al. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ. (2011) 343:5928–36. doi: 10.1136/bmj.d5928
71. Deng C, Lou Y, Gao Y, Deng B, Su F, Jia L. Efficacy and safety of Shengjiang Xiexin decoction in prophylaxis of chemotherapy-related diarrhea in small cell lung cancer patients: study protocol for a multicenter randomized controlled trial. Trials. (2020) 21:370–8. doi: 10.1186/s13063-020-04275-5
72. Daugelaite G, Uzkuraityte K, Jagelaviciene E, Filipauskas A. Prevention and treatment of chemotherapy and radiotherapy induced oral mucositis. Medicina (Kaunas). (2019) 55:25–39. doi: 10.3390/medicina55020025
73. Blakaj A, Bonomi M, Gamez ME, Blakaj DM. Oral mucositis in head and neck cancer: evidence-based management and review of clinical trial data. Oral Oncol. (2019) 95:29–34. doi: 10.1016/j.oraloncology.2019.05.013
74. Azad MAK, Sarker M, Li T, Yin J. Probiotic species in the modulation of gut microbiota: an overview. Biomed Res Int. (2018) 2018:1–8. doi: 10.1155/2018/9478630
75. Lopes R, Balbino KP, Jorge MP, Ribeiro AQ, Martino HSD, Alfenas RCG. Modulation of intestinal microbiota, control of nitrogen products and inflammation by pre/probiotics in chronic kidney disease: a systematic review. Nutr Hosp. (2018) 35:722–30. doi: 10.20960/nh.1642
76. Schnadower D, Tarr PI, Casper TC, Gorelick MH, Dean JM, O'Connell KJ, et al. Lactobacillus rhamnosus GG versus placebo for acute gastroenteritis in children. N Engl J Med. (2018) 379:2002–14. doi: 10.1056/NEJMoa1802598
77. Li B, Liang L, Deng H, Guo J, Shu H, Zhang L. Efficacy and safety of probiotics in irritable bowel syndrome: a systematic review and meta-analysis. Front Pharmacol. (2020) 11:332. doi: 10.3389/fphar.2020.00332
78. Mack I, Schwille-Kiuntke J, Mazurak N, Niesler B, Zimmermann K, Mönnikes H, et al. A nonviable probiotic in irritable bowel syndrome: a randomized, double-blind, placebo-controlled, multicenter study. Clin Gastroenterol Hepatol. (2021) 21:1–9. doi: 10.1016/j.cgh.2021.06.028
79. Wang CS Li WB, Wang HY, Ma YM, Zhao XH, Yang H, et al. VSL#3 can prevent ulcerative colitis-associated carcinogenesis in mice. World J Gastroenterol. (2018) 24:4254–62. doi: 10.3748/wjg.v24.i37.4254
80. Gibson RJ, Bowen JM, Inglis MRB, Cummins AG, Keefe DMK. Irinotecan causes severe small intestinal damage, as well as colonic damage, in the rat with implanted breast cancer. J Gastroenterol Hepatol. (2003) 18:1095–100. doi: 10.1046/j.1440-1746.2003.03136.x
81. Gibson RJ, Keefe DM. Cancer chemotherapy-induced diarrhoea and constipation: mechanisms of damage and prevention strategies. Support Care Cancer. (2006) 14:890–900. doi: 10.1007/s00520-006-0040-y
82. McQuade RM, Stojanovska V, Abalo R, Bornstein JC, Nurgali K. Chemotherapy-induced constipation and diarrhea: pathophysiology, current and emerging treatments. Front Pharmacol. (2016) 7:414–27. doi: 10.3389/fphar.2016.00414
83. Scully C, Sonis S, Diz PD. Oral mucositis. Oral Dis. (2006) 12:229–41. doi: 10.1111/j.1601-0825.2006.01258.x
84. Nagpal R, Kumar A, Kumar M, Behare PV, Jain S, Yadav H. Probiotics, their health benefits and applications for developing healthier foods: a review. FEMS Microbiol Lett. (2012) 334:1–15. doi: 10.1111/j.1574-6968.2012.02593.x
85. Ribeiro FM, Petriz B, Marques G, Kamilla LH, Franco OL. Is there an exercise-intensity threshold capable of avoiding the leaky gut? Front Nutr. (2021) 8:1–12. doi: 10.3389/fnut.2021.627289
Keywords: probiotics, cancer, chemotherapy, diarrhea, oral mucositis
Citation: Feng J, Gao M, Zhao C, Yang J, Gao H, Lu X, Ju R, Zhang X and Zhang Y (2022) Oral Administration of Probiotics Reduces Chemotherapy-Induced Diarrhea and Oral Mucositis: A Systematic Review and Meta-Analysis. Front. Nutr. 9:823288. doi: 10.3389/fnut.2022.823288
Received: 27 November 2021; Accepted: 03 February 2022;
Published: 28 February 2022.
Edited by:
Satya Prakash, McGill University, CanadaReviewed by:
Reza Rastmanesh, American Physical Society, United StatesCopyright © 2022 Feng, Gao, Zhao, Yang, Gao, Lu, Ju, Zhang and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yunlei Zhang, eXVubGVpemhhbmdAbmptdS5lZHUuY24=; Xiuwei Zhang, emhhbmd4aXV3ZWl5d3lAMTI2LmNvbQ==
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.