
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Nutr., 25 January 2022
Sec. Nutritional Epidemiology
Volume 9 - 2022 | https://doi.org/10.3389/fnut.2022.815578
This article is part of the Research TopicInsights in Nutritional EpidemiologyView all 17 articles
 Hongpeng Liu1
Hongpeng Liu1 Jing Jiao1*†
Jing Jiao1*† Minglei Zhu2
Minglei Zhu2 Xianxiu Wen3
Xianxiu Wen3 Jingfen Jin4
Jingfen Jin4 Hui Wang5
Hui Wang5 Dongmei Lv6
Dongmei Lv6 Shengxiu Zhao7
Shengxiu Zhao7 Xiang Sun1
Xiang Sun1 Xinjuan Wu1*†
Xinjuan Wu1*† Tao Xu8*†
Tao Xu8*†Background: Studies are scarce in China that explore the association of nutritional status, measured using the Short-Form Mini Nutritional Assessment (MNA-SF) and biochemical data, on adverse clinical outcomes among older inpatients. In this study, we aimed to determine the prevalence of malnutrition in tertiary hospitals of China and the associations between malnutrition and adverse clinical outcomes.
Methods: This prospective study involved 5,516 older inpatients (mean age 72.47 ± 5.77 years) hospitalized in tertiary hospitals between October 2018 and February 2019. The tertiary hospitals refer to the hospital with more than 500 beds and can provide complex medical care services. The MNA-SF was used to assess nutritional status. Multiple logistic regression and negative binomial regression were used to analyze the relationship between nutritional parameters and risk of hospital length of stay (LoS), mortality, and rehospitalization.
Results: We found that 46.19% of hospitalized patients had malnutrition or malnutrition risk, according to the MNA-SF. Death occurred in 3.45% of patients. MNA-SF scores 0–7 (odds ratio [OR] 5.738, 95% confidence interval [CI] 3.473 to 9.48) were associated with a six-fold higher likelihood of death, and scores 8–11 (OR 3.283, 95% CI 2.126–5.069) with a three-fold higher likelihood of death, compared with MNA-SF scores 12–14 in the logistic regression model, after adjusting for potential confounders. A low MNA-SF score of 0–7 (regression coefficient 0.2807, 95% CI 0.0294–0.5320; P < 0.05) and a score of 8–11 (0.2574, 95% CI 0.0863–0.4285; P < 0.01) was associated with a significantly higher (28.07 and 25.74%, respectively) likelihood of increased LoS, compared with MNA-SF score 12–14. MNA-SF scores 0–7 (OR 1.393, 95% CI 1.052–1.843) and 8–11 (OR 1.356, 95% CI 1.124–1.636) were associated with a nearly 1.5-fold higher likelihood of 90-day readmission compared with MNA-SF scores 12–14 in the logistic regression model. Moreover, hemoglobin level, female sex, education level, former smoking, BMI 24–27.9 kg/m2, age 75 years and above, and current alcohol consumption were the main factors influencing clinical outcomes in this population.
Conclusions: Malnutrition increases the risk of hospital LoS, mortality, and 90-day readmission. The use of nutritional assessment tools in all hospitalized patients in China is needed. The MNA-SF combined with hemoglobin level may be used to identify older inpatients with a high risk of adverse clinical outcomes. These findings may have important implications for the planning of hospital services.
With the rapid development of health science and the global economy, the life span of the world's population is increasing (1–3). By 2050, it is estimated that 16% of the world's population would be aged 65 years and older (4), with 80% of those living in low- and middle-income countries (5). China, as the world's second-largest economy, has the world's largest population of 1.44 billion (19% of the world's population) and is rapidly becoming an aging nation (6–8).
Older adults are likely to have poor nutritional status and decreased quality of life (8–10). Nutritional deficits in the elderly can be caused by insufficient nutrient and energy intake (11). A few age-related pathophysiological, psychosocial, and pharmacological factors determine changes in dietary habits, as well as intake and use of nutrients, leading to specific deficits (12). The adverse effects of malnutrition or malnutrition risk on health substantially affect the quality of life by increasing the risk of physical frailty, disability, mortality, and deterioration during hospitalization (15, 19).
The prevalence of hospital malnutrition or the risk of malnutrition in elderly patients is considerable (30–50%) (11, 13, 14). This is primarily due to challenges in identifying and appropriately managing at-risk patients (15). As the European Society for Parenteral and Enteral Nutrition (ESPEN) recommends (16), Nutrition Risk Screening (NRS 2002) should be used to screen undernutrition in all inpatients. Several nutritional measures have been developed to determine nutritional status among inpatients in China, including the NRS 2002 and Short-Form Mini Nutritional Assessment (MNA-SF) (14, 17). However, appropriate nutritional risk screening is not performed in many Chinese hospitals, only in some large-scale nationwide, provincial, and municipal tertiary hospitals with more than 500 beds (18), where nutritional risk screening is mandatory.
Previous reports have suggested that malnutrition is associated with increased mortality among older residents of nursing homes (19). Other studies have used various nutritional screening tools, including the NRS 2002 and Malnutrition Universal Screening Tool, to estimate nutritional status and adverse clinical outcomes in the general hospitalized population (17, 20, 21) and in surgical patients (10, 22, 23), or these have used hospital data only or a smaller sample size (10, 24–27).
The European Society for Parenteral and Enteral Nutrition (ESPEN) suggests the use of NRS 2002 and Malnutrition Universal Screening Tool, whereas for older populations ESPEN recommends the use of the Mini Nutritional Assessment (MNA) either in its full or short form (MNA-SF) (28). Previous studies also indicated that the MNA-SF is a valid instrument with good specificity and sensitivity for the diagnosis of malnutrition, and this tool is specific for the older population (28–30). Nevertheless, few studies have reported on the prevalence of malnutrition in Asia hospitals (31), and studies are scarce in China that explore the associations between nutritional status, measured using the MNA-SF and biochemical data, on adverse clinical outcomes among older inpatients. To address this issue, we used data from a cohort study to examine the implementation of nutritional risk screening. We also assessed the prevalence, determinants, and associations between nutritional status and hospital length of stay (LoS), mortality, and readmission.
Participants were inpatients aged 65 years and older from an ongoing, prospective, large-scale cohort study of elder patients hospitalized in tertiary hospitals in China (Eastern: Zhejiang Province; South-Central: Hubei Province; southwest: Sichuan Province; Northeast: Heilongjiang Province; Northern: Beijing municipality/city; Northwest: Qinghai Province). Details can be found elsewhere (14, 32). Eligible study subjects are recruited from neurology, surgical, orthopedics departments, intensive care unit (ICU), as well as internal medicine of selected hospitals, are consecutively enrolled. The surveys are managed by trained nurses using a structured Case Report Form (CRF). Our research team developed manuals for the project survey and operation process. To ensure data quality, the nurses received training and test before they apply the assessment to the patients. All CRF results were reviewed by the head nurse. The research team also developed a quality control team, and a communication platform based on the WeChat App to guarantee timely feedback. If the participant is unable to answer questions on his or her own, proxy interviewees (usually spouses or other legal guardians) are interviewed.
The current study was based on baseline survey data collected from October 2018 to February 2019. During this period, there were 9,996 hospitalizations; of these, 8,326 patients had complete data at 90-day follow-up, and 5,516 had an LoS of at least 2 days or had initial biochemical data during hospitalization. Thus, the study subjects included a total of 5,516 patients aged 65 years and older.
Nutritional status was assessed using the MNA-SF, a six-item instrument with scores ranging from 0 to 14 points (19). The MNA-SF has been validated and shows good specificity and sensitivity for the diagnosis of malnutrition, mainly in older adults (10, 29). For the purpose of our study, participants were categorized into a group with normal nutritional status (12–14 points), the patient at risk of malnutrition (8–11 points), or malnourished patients (0–7 points) (33). The MNA-SF has been verified in the Chinese elderly and has extraordinary test characteristics (14, 34).
Participants' height (cm) was measured to the nearest 1 mm using a stadiometer, while weight (kg) was measured to the nearest 0.1 kg using a digital electronic chair scale. Patients were weighed while wearing light clothing and without shoes. Considering most of the ICU patients were immobility, the body weight and height were recorded when they were first admitted to the general ward, and this data can be synchronized to the ICU nursing information system. Therefore, our research team record their body weight and height according to the information system. Body mass index (BMI) was calculated as body weight divided by height (in meters) squared (kg/m2) (35) and was used to classify patients of underweight (<18.5 kg/m2), normal (18.5–23.9 kg/m2), overweight (24–27.9) kg/m2), and obese greater or equal to 28 kg/m2) (36, 37).
The following parameters were also analyzed: age, alcohol consumption, smoking (former smokers refer to at least 6 months without smoking), sex, education level, ethnicity, and marital status. All biochemical parameters included in the analysis (such as hemoglobin, serum albumin, blood urea nitrogen, and creatinine) were the first determinations during patients' respective hospitalizations (21).
The following outcomes were measured: death (record all-cause mortality within 90 days, which consists of in-hospital deaths), LoS (duration of hospitalization) (38), and nonelective readmission (second and subsequent hospitalizations during the period analyzed) during the 90 days following discharge.
This study was ethically approved by the review board of Peking Union Medical College Hospital (S-K540). All patients participating in this study provided written informed consent. If patients had cognitive decline, the investigator interviewed their proxy respondents and obtained their consent for the patient to participate in this study. Patients were excluded if they were persistently unconscious, or if their proxy respondents were unable to provide effective information.
Statistical analysis using SAS 9.4 software (SAS Institute Inc., Cary, NC, USA). Continuous variables are summarized as mean and standard deviation (SD). Categorical variables were summarized as counts and percentages. Bivariate analyses were performed using the χ2 test or Fisher's exact test for qualitative variables and the Student t-test, analysis of variance, or Kruskal–Wallis test for quantitative variables. We ran separate models for each parameter of nutritional status in all analyses, owing to the collinearity between them. Both logistic and negative binomial regression analyses were conducted. The strength of the associations was estimated as odds ratios (ORs) for the logistic models, and as the regression coefficient for negative binomial regression, with 95% confidence intervals (95% CIs). A P-value of <0.05 was considered statistically significant.
In Table 1, the mean age of the included patients was 72.47 ± 5.77 years at baseline, and 59.77% of participants (3,297/5,516) were men. Approximately 54% of patients had a middle school education and above, and 90.1% were married. A major proportion of respondents were of Han nationality (94.65%). More than half of the participants were non-smokers (65.07%) and non-drinkers (74.85%). The average BMI was 23.56 ± 3.52 kg/m2, and approximately half (49.02%) had a BMI between 18.5 and 23.9 kg/m2. 40.08% of patients were from medicine departments and only 5.73% of patients were from ICU. According to the MNA-SF, 46.19% (2,548/5,516) of hospitalized individuals were at risk of malnutrition or malnourishment (Table 2). Patients who were malnourished were with higher mortality and 90-day readmission, and longer LoS. 11.89% (656/5,516) of malnourished patients had low serum albumin [cut-off 35 g/L for serum albumin levels (19)] compared with the well-nourished patients or patients at risk of malnutrition. The remaining data for hospitalizations analyzed according to MNA-SF values for malnutrition, malnutrition risk, or normal, are presented in Tables 1, 2.
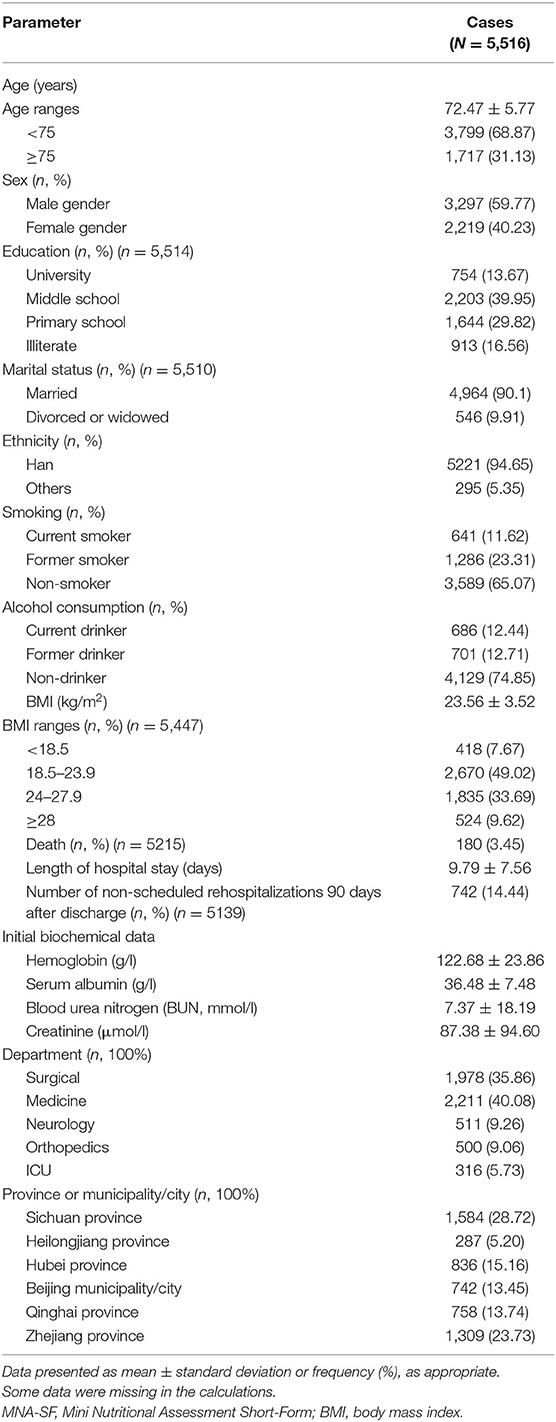
Table 1. Demographic and clinical characteristics of patients in relation to MNA-SF score on admission.
Table 1 displays mortality among the study participants. Overall, death occurred in 3.45% of study participants. In Table 2, the number of patients who died who were malnourished, at risk of malnutrition, and normal was 61 (10.29%), 84 (4.72%), and 35 (1.23%), respectively (P < 0.001). MNA-SF scores 0–7 (OR 5.738, 95% CI 3.473 to 9.48; P < 0.001) were associated with a six-fold higher likelihood of death and scores 8–11 (OR 3.283, 95% CI 2.126–5.069) with a three-fold higher likelihood of death, compared with MNA-SF scores 12–14 in the logistic regression model, after adjusting for potential confounders (Table 3). However, hemoglobin (OR 0.992, 95% CI 0.985–0.998; P < 0.05) and serum albumin (OR 0.927, 95% CI 0.902–0.951; P < 0.001) had a lower likelihood of increased mortality. Additionally, female patients had a lower likelihood of death than male patients (OR 0.646, 95% CI 0.433–0.962; P < 0.05). A higher level of education (OR 0.484, 95% CI 0.247–0.947; P < 0.05) was statistically associated with a decline in the risk of death, in comparison with illiterate patients.
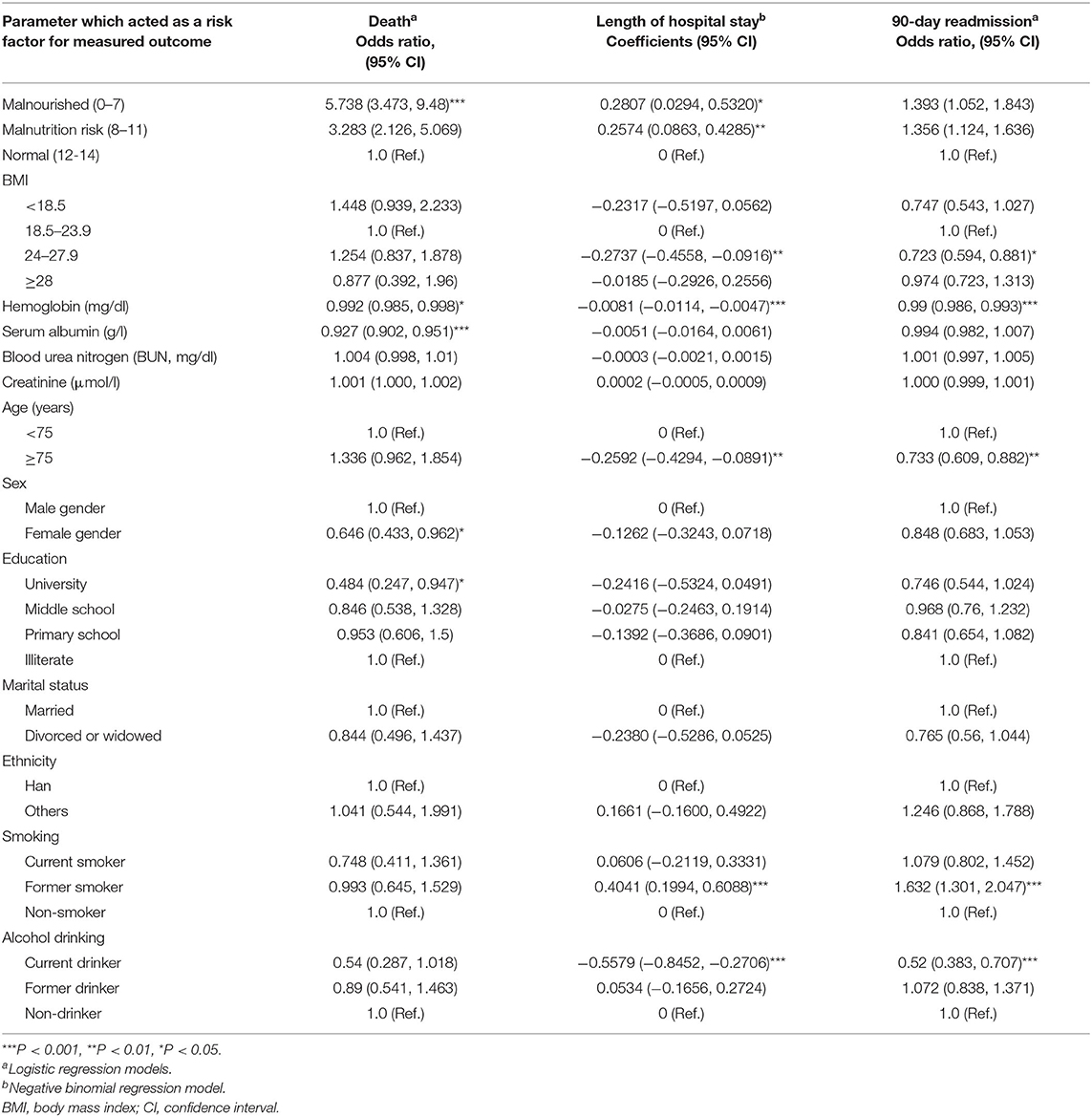
Table 3. Prevalence of measured outcomes in relation to nutritional status and clinical parameters analyzed.
Table 2 also indicates the LoS among the patients, with an average LoS in the group with MNA-SF scores 0–7 of 12.58 ± 9.25 days, 11.52 ± 8.54 days in the group with MNA-SF scores 8–11, and 9.87 ± 7.49 in the group with MNA-SF scores 12–14. In Table 3, after adjusting for potential confounders in the negative binomial regression model, a low MNA-SF score of 0–7 (regression coefficient 0.2807, 95% CI 0.0294–0.5320; P < 0.05) and a score of 8–11 (0.2574, 95% CI 0.0863–0.4285; P < 0.01) was associated with a significantly (28.07 and 25.74%, respectively) higher likelihood of increased LoS compared with an MNA-SF score 12–14. Additionally, compared with nonsmokers, former smokers had a 40.41% (0.4041, 95% CI 0.1994–0.6088; P < 0.001) higher likelihood of increased LoS, whereas there was no significance among current smokers. However, BMI 24–27.9 kg/m2 (−0.2737, 95% CI −0.4558 to −0.0916; P < 0.01) and hemoglobin (−0.0081, 95% CI −0.0114 to −0.0047; P < 0.001) had a lower likelihood of increased LoS. Age 75 years and above (−0.2592, 95% CI −0.4294 to −0.0891; P < 0.01) and current alcohol consumption (−0.5579, 95% CI −0.8452 to −0.2706; P < 0.001) were also protective factors.
Table 1 also shows that 742 participants (14.44%) had unscheduled rehospitalization 90 days after discharge. In Table 2, the number of patients with malnutrition, malnutrition risk, and normal nutritional status who had 90-day readmission was 106 (18.76%), 295 (16.92%), and 341 (12.05%), respectively (P < 0.001). In Table 3, MNA-SF scores 0–7 (OR 1.393, 95% CI 1.052–1.843) and 8–11 (OR 1.356, 95% CI 1.124–1.636) were associated with a nearly 1.5-fold higher likelihood of 90-day readmission, compared with MNA-SF scores 12–14 scores in the logistic regression model, after adjusting for potential confounders. Additionally, former smokers (OR 1.632, 95% CI 1.301–2.047; P < 0.001) had a higher risk of 90-day readmission than nonsmokers. However, BMI 24–27.9 kg/m2 (OR 0.723, 95% CI 0.594–0.881; P < 0.05), hemoglobin (OR 0.99, 95% CI 0.986–0.993; P < 0.001), age 75 years and above (OR 0.733, 95% CI 0.609–0.882; P < 0.01), and current drinking (OR 0.52, 95% CI 0.383–0.707; P < 0.001) were significantly associated with a lower risk of 90-day readmission in the multivariate model.
This study is among the first to examine the association between nutritional status and LoS, mortality, and readmission in a nationally representative sample of Chinese elder inpatients of tertiary hospitals. We found malnutrition (MNA-SF score 0–7) in 11.89% of all older hospitalized patients, and low MNA-SF scores were associated with increased average LoS, a greater likelihood of death, and 90-day readmission.
Studies are scarce in China that explore the associations between nutritional status and health outcomes among older inpatients. Adigüzel et al. (39) indicated that nutritional parameters and sociodemographic features could affect health-related quality of life and functional ability among home care patients in Turkey. A study conducted in Germany also suggested that malnutrition could increase the risk of morbidity, mortality, hospital LoS, and costs among surgical patients (22). Additionally, Valmorbida et al. (19) suggested that malnutrition is associated with an increased risk of hospital admission and death among the 144 Italian older adults. Therefore, these studies are in accordance with our results and emphasize the urgent need for physicians, nurses, and clinical institutions to be aware of the high prevalence of malnutrition in the elderly, periodic nutritional screening of geriatric inpatients is critical.
Malnutrition is a crucial condition among older inpatients, both as a cause and consequence of disease (14, 40). The prevalence of malnutrition is 46.19% in tertiary hospitals of China, which is higher than the results of a cross-sectional study conducted in nursing homes of Spain reporting that 40.1% of older residents had malnutrition or risk of malnutrition, as measured using the Mini Nutritional Assessment (MNA®) (41). Previous research has indicated that 38.2% of nursing home residents in Italy are malnourished or at risk of malnutrition according to the MNA-SF (19), and the prevalence of malnutrition and malnutrition risk among older patients with hip fracture in Israel ranges from 55.81% using the MNA-SF (10) to 56.59% (medium risk and nutritionally at risk, measured using the NRS-2002) in Hyogo, Japan (42). These differences are likely owing to a variety of factors, including differences in the nutritional assessment tools used, study participants, study design, study periods, and local factors, such as the health systems in different countries and the standards of medical treatment received (10, 15, 19, 21, 43).
In comparison with well-nourished patients, malnourished older patients in our study had higher mortality (OR 5.738, 95% CI 3.473–9.48; 10.29% vs. 1.23%), longer LoS (0.2807, 95% CI 0.0294–0.5320; P < 0.05; 12.58 ± 9.25 vs. 9.87 ± 7.49) and were more likely to be readmitted within 90 days (OR 1.393, 95% CI 1.052–1.843; 18.76% vs. 12.05%). In line with our results, Lim et al. (31) suggested that approximately 29% of malnourished Singaporean patients had a longer hospital stay (6.9 ± 7.3 days vs. 4.6 ± 5.6 days, P < 0.001) and were more likely to be readmitted within 15 days (adjusted relative risk = 1.9, 95% CI 1.1–3.2, P=0.025) than well-nourished patients (31). Agarwal et al. (44) suggested that the 90-day in-hospital mortality in malnourished patients was around 1.09–3.34 times that of well-nourished patients, readmission rates and mean LoS among the malnourished patients were 36% and 15 days, respectively. These differences might result from the demographic characteristics of study participants and different follow-up periods after discharge. These findings confirm that early and compulsory nutritional assessment to identify malnutrition or malnutrition risk in elder inpatients is critical and may help in targeting interventions to tackle malnutrition (16).
Despite the association between malnutrition assessed by the MNA-SF and adverse clinical outcomes, hemoglobin level was associated with the hospital LoS, mortality, and 90-day readmission, after adjusting for confounders in our sample. These results are in line with the current literature (45–47) that low hemoglobin is associated with adverse clinical outcomes among older adults. Moreover, previous research indicates that the Geriatric Nutrition Risk Index (GNRI) (42) combined with biochemical objective indicators, such as albumin, can be used to identify and diagnose malnutrition and can better predict 30-day mortality rate in older patients (48). In addition, Hong et al. (49) and Pérez-Ros et al. (50) indicated that compared with the robust, levels of hemoglobin showed lower values among the prefrail and frail group, and nutritional markers may be used for the evaluation of adverse clinical outcomes in older patients. Therefore, our study suggests that the MNA-SF may be used in combination with hemoglobin levels to predict clinical outcomes among older inpatients. Although further evaluations are needed to clarify this, we believe that such findings may have concrete, helpful implications in the clinical practice.
Serum albumin is a protective factor of death among this study population. Only 11.89% of older inpatients had low serum albumin [cut-off of 35 g/L (19)] in our sample. Besides, Bouillanne et al. suggested that serum albumin lower than 35 g/L was associated with a higher risk of death (51). Therefore, during nutritional assessment in older inpatients, we might take albumin values into consideration, which may inform prognosis and hospital services planning.
Concerning BMI <18.5 kg/m2 as an indicator of undernutrition, we did not find significant associations with LoS, mortality or readmission, which differs from reports that individuals with BMI <25 kg/m2 had a higher risk of death than those who were overweight or obese (19). Interestingly, among BMI categories, only BMI 24–27.9 kg/m2 was significantly associated with a lower LoS and risk of 90-day readmission than BMI 18.5–23.9 kg/m2. This can hypothetically indicate that older overweight inpatients have significantly higher muscle mass than their normal counterparts. Thus, characteristics related to overweight and higher muscle mass could introduce a positive association for LoS and readmission (52). However, other relevant clinical data were lacking, including muscle mass in older inpatients; therefore, prospective studies with more sophisticated assessments are needed to confirm our findings.
In addition to the nutritionally related parameters assessed, former smokers were associated with a 40.41% higher likelihood of increased LoS and 90-day readmission than nonsmokers, which further supports previous research findings (14, 53, 54). However, current alcohol consumption and age ≥75 years were protective factors for LoS and readmission. This can possibly be explained by evidence that older people who consume small to moderate amounts of alcohol [1–25 g/day (55)] are more likely to maintain functional status and mobility than nondrinkers (32, 56); limited alcohol consumption has been associated with a decreased risk of adverse clinical outcomes (57). Another possible explanation is that compared with inpatients aged 75 years and above, those younger than 75 years may be able to withstand surgical stresses, and underwent more surgical treatment, which increases the risk of medical complications and longer LoS (58, 59).
Older female inpatients had a lower likelihood of death than male inpatients, and higher education level was significantly associated with a lower mortality risk than low education levels. The clinical phenomenon that female individuals survive longer than male adults is well described (57, 60), and well-educated older people may better comprehend the importance of nutrient intake, daily exercise, and disease prevention (61, 62).
The main limitations of our study include the limited follow-up; investigations with a longer duration are needed to better clarify the present findings. A further limitation of this paper is not having assessed all nutritional parameters over time; we only used the MNA-SF with a few anthropometric measures and limited biochemical data. Moreover, the older inpatients enrolled in our study were all from tertiary hospitals and only one hospital in each province or municipality/city, patients may have more complex clinical features, which may limit the generalizability of our results to different settings. Additionally, patients are taken from multiple hospitals or wards with differing baselines, the severity of the comorbidity along with different characteristics of the patients may influence the mortality rate and length of stay. The patients enrolled in this study were relatively young, 68.87% of the patients were <75 years old, which also limited the generalizability of this study. ICU patients have a higher mortality rate compared to general wards, it is meaningful to explore the nutritional status and adverse clinical outcomes among the ICU older inpatients. We are going to conduct this study in the future. Besides, our use of a limited number of nutritional screening tools restricted the comparison of our results with those of other studies, and the nutritional status was analyzed using the original MNA-SF which was derived based on Western populations, whereas the recent studies conducted in Taiwan of China have resulted in a modified MNA-SF, we will use this modified MNA-SF for further study (63, 64). Finally, the study participants were hospitalized in multiple wards or departments; we did not analyze the medical and nursing care received by patients, nor did we analyze the reason for the hospital admission. The patients enrolled in the present study were older adults from surgical, neurology, orthopedics departments, internal medicine, and ICU of selected hospitals, thus there would be great differences in nutritional status among these participants who have these health conditions, have chronic diseases, or undergoing surgery could be associated with poor nutritional status among hospitalized older people. To be meaningful, we will learn from previous research and results will be analyzed according to the like-kind of patients only (65, 66). Chronic diseases including cancer, diabetes, and cardiovascular diseases could be associated with poor nutritional status among elder patients, whereas we did not analyze the impact of chronic diseases in this study. There is a lack of other relevant clinical data, including albumin data, comorbidities, clinical severity of disease, comprehensive geriatric assessment, sarcopenia, the fat fold, upper arm circumference, and thigh circumference, because these features were not recorded in the first place, which is an inherent drawback of retrospective analysis of a prospectively collected database. Prospective studies with more sophisticated assessments are needed in the future.
The findings of this study suggested that malnutrition increases the risk of hospital LoS, mortality, and 90-day readmission among inpatients, in comparison with well-nourished inpatients. Use of nutritional assessment tools in all hospitalized Chinese patients is needed. The MNA-SF in combination with hemoglobin level may be used to identify a high risk of adverse clinical outcomes among older inpatients and may be a good predictor of patient outcomes. These findings could have major importance for the planning of hospital services, discharge planning, and post-discharge care.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by Peking Union Medical College Hospital (S-K540). The patients/participants provided their written informed consent to participate in this study.
XWu: study concept and design. HL, JJia, and TX: analysis and interpretation of data. HL: editing of the manuscript and drafting of tables. XWu and HL: critical review of the manuscript for important intellectual content. MZ, XWe, JJin, HW, DL, XS, and SZ: patient recruitment, data collection, and manuscript editing. All authors critically reviewed and approved the manuscript before it was submitted.
The Special Research Fund for Central Universities, Peking Union Medical College [Grant Number 2018PT33001] supported this study but had no role in study design or data collection, analysis, and interpretation, or manuscript conception and writing.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The authors are grateful to all the persons who participated in the collection of the data. We thank Analisa Avila, ELS, of Liwen Bianji, for editing the English text of a draft of this paper.
MNA-SF, Mini Nutritional Assessment Short-Form; BMI, body mass index; SD, standard deviation; CI, confidence interval; ICU, intensive care unit; CRF, Case Report Form.
2. Bloom DE, Luca DL: Chapter 1—the global demography of aging: facts explanations future. In: Piggott J, Woodland A, editors. Handbook of the Economics of Population Aging. vol. 1: North-Holland. (2016). p. 3–56. doi: 10.1016/bs.hespa.2016.06.00
3. Liu H, Jiao J, Zhu M, Wen X, Jin J, Wang H, et al. An early predictive model of frailty for older inpatients according to nutritional risk: protocol for a cohort study in China. BMC Geriatr. (2021) 21:465. doi: 10.1186/s12877-021-02396-3
4. Søreide K, Wijnhoven BP. Surgery for an ageing population. Br J Surg. (2016) 103:e7–9. doi: 10.1002/bjs.10071
5. The L: how to cope with an ageing population. Lancet. (2013) 382. doi: 10.1016/S0140-6736(13)62080-2
6. Lv X, Li W, Ma Y, Chen H, Zeng Y, Yu X, et al. Cognitive decline and mortality among community-dwelling Chinese older people. BMC Med. (2019) 17:63. doi: 10.1186/s12916-019-1295-8
7. Fang EF, Scheibye-Knudsen M, Jahn HJ Li J, Ling L, Guo H, Zhu X, et al. A research agenda for aging in China in the 21st century. Ageing Res Rev. (2015) 24:197–205. doi: 10.1016/j.arr.2015.08.003
8. The L: ageing and health—an agenda half completed. Lancet. (2015) 386. doi: 10.1016/S0140-6736(15)00521-8
9. Kelaiditi E, Demougeot L, Lilamand M, Guyonnet S, Vellas B, Cesari M. Nutritional status and the incidence of pneumonia in nursing home residents: results from the INCUR study. J Am Med Dir Assoc. (2014) 15:588–92. doi: 10.1016/j.jamda.2014.04.012
10. Koren-Hakim T, Weiss A, Hershkovitz A, Otzrateni I, Anbar R, Gross Nevo RF, et al. Comparing the adequacy of the MNA-SF, NRS-2002 and MUST nutritional tools in assessing malnutrition in hip fracture operated elderly patients. Clin Nutr. (2016) 35:1053–8. doi: 10.1016/j.clnu.2015.07.014
11. Martínez-Reig M, Gómez-Arnedo L, Alfonso-Silguero SA, Juncos-Martínez G, Romero L, Abizanda P. Nutritional risk, nutritional status and incident disability in older adults. FRADEA study J Nutr Health Aging. (2014) 18:270–6. doi: 10.1007/s12603-013-0388-x
12. Inzitari M, Doets E, Bartali B, Benetou V, Di Bari M, Visser M, et al. Nutrition in the age-related disablement process. J Nutr Health Aging. (2011) 15:599–604. doi: 10.1007/s12603-011-0053-1
13. Vanderwee K, Clays E, Bocquaert I, Gobert M, Folens B, Defloor T. Malnutrition and associated factors in elderly hospital patients: a Belgian cross-sectional, multi-centre study. Clin Nutr. (2010) 29:469–76. doi: 10.1016/j.clnu.2009.12.013
14. Liu H, Jiao J, Zhu C, Zhu M, Wen X, Jin J, Wang H, Lv D, Zhao S, Wu X et al. Associations between nutritional status, sociodemographic characteristics, and health-related variables and health-related quality of life among Chinese elderly patients: a multicenter prospective study. Front Nutr. (2020) 7:583161. doi: 10.3389/fnut.2020.583161
15. Khalatbari-Soltani S, Marques-Vidal P. Impact of nutritional risk screening in hospitalized patients on management, outcome and costs: a retrospective study. Clin Nutr. (2016) 35:1340–6. doi: 10.1016/j.clnu.2016.02.012
16. Kondrup J, Allison SP, Elia M, Vellas B, Plauth M. ESPEN guidelines for nutrition screening 2002. Clin Nutr. (2003) 22:415–21. doi: 10.1016/S0261-5614(03)00098-0
17. Jie B, Jiang ZM, Nolan MT, Efron DT, Zhu SN Yu K, Kondrup J. Impact of nutritional support on clinical outcome in patients at nutritional risk: a multicenter, prospective cohort study in Baltimore and Beijing teaching hospitals. Nutrition. (2010) 26:1088–93. doi: 10.1016/j.nut.2009.08.027
18. Liu H, Zhu D, Cao J, Jiao J, Song B, Jin J, et al. The effects of a standardized nursing intervention model on immobile patients with stroke: a multicenter study in China. Eur J Cardiovasc Nurs. (2019) 18:753–63. doi: 10.1177/1474515119872850
19. Valmorbida E, Trevisan C, Imoscopi A, Mazzochin M, Manzato E, Sergi G. Malnutrition is associated with increased risk of hospital admission and death in the first 18 months of institutionalization. Clin Nutr. (2020) 39:3687–94. doi: 10.1016/j.clnu.2020.03.029
20. Marques-Vidal P, Khalatbari-Soltani S, Sahli S, Coti Bertrand P, Pralong F, Waeber G. Undernutrition is associated with increased financial losses in hospitals. Clin Nutr. (2018) 37:681–6. doi: 10.1016/j.clnu.2017.02.012
21. Budzynski J, Tojek K, Czerniak B, Banaszkiewicz Z. Scores of nutritional risk and parameters of nutritional status assessment as predictors of in-hospital mortality and readmissions in the general hospital population. Clin Nutr. (2016) 35:1464–71. doi: 10.1016/j.clnu.2016.03.025
22. Thomas MN, Kufeldt J, Kisser U, Hornung HM, Hoffmann J, Andraschko M, et al. Effects of malnutrition on complication rates, length of hospital stay, and revenue in elective surgical patients in the G-DRG-system. Nutrition. (2016) 32:249–54. doi: 10.1016/j.nut.2015.08.021
23. Schiesser M, Muller S, Kirchhoff P, Breitenstein S, Schafer M, Clavien PA. Assessment of a novel screening score for nutritional risk in predicting complications in gastro-intestinal surgery. Clin Nutr. (2008) 27:565–70. doi: 10.1016/j.clnu.2008.01.010
24. Rasheed S, Woods RT. An investigation into the association between nutritional status and quality of life in older people admitted to hospital. J Human Nutr Diet. (2014) 27:142–51. doi: 10.1111/jhn.12072
25. Kostka J, Borowiak E, Kostka T. Nutritional status and quality of life in different populations of older people in Poland. Eur J Clin Nutr. (2014) 68:1210–5. doi: 10.1038/ejcn.2014.172
26. Jimenez-Redondo S, Beltran de. Miguel B, Gavidia Banegas J, Guzman Mercedes L, Gomez-Pavon J, Cuadrado Vives C: Influence of nutritional status on health-related quality of life of non-institutionalized older people. J Nutr Health Aging. (2014) 18:359–64. doi: 10.1007/s12603-013-0416-x
27. Eriksson BG, Dey DK, Hessler RM, Steen G, Steen B. Relationship between MNA and SF-36 in a free-living elderly population aged 70 to 75. J Nutr Health Aging. (2005) 9:212–20.
28. Cederholm T, Barazzoni R, Austin P, Ballmer P, Biolo G, Bischoff SC, et al. ESPEN guidelines on definitions and terminology of Clin Nutr. Clin Nutr. (2017) 36:49–64. doi: 10.1016/j.clnu.2016.09.004
29. Fernández-Barrés S, García-Barco M, Basora J, Martínez T, Pedret R, Arija V. The efficacy of a nutrition education intervention to prevent risk of malnutrition for dependent elderly patients receiving Home Care: A randomized controlled trial. Int J Nurs Stud. (2017) 70:131–41. doi: 10.1016/j.ijnurstu.2017.02.020
30. Guigoz Y, Vellas B, Garry PJ. Assessing the nutritional status of the elderly: The Mini Nutritional Assessment as part of the geriatric evaluation. Nutr Rev. (1996) 54:S59–65. doi: 10.1111/j.1753-4887.1996.tb03793.x
31. Lim SL, Ong KCB, Chan YH, Loke WC, Ferguson M, Daniels L. Malnutrition and its impact on cost of hospitalization, length of stay, readmission and 3-year mortality. Clin Nutr. (2012) 31:345–50. doi: 10.1016/j.clnu.2011.11.001
32. Liu H, Jiao J, Zhu C, Zhu M, Wen X, Jin J, et al. Potential associated factors of functional disability in Chinese older inpatients: a multicenter cross-sectional study. BMC Geriatr. (2020) 20:319. doi: 10.1186/s12877-020-01738-x
33. Verlaan S, Aspray TJ, Bauer JM, Cederholm T, Hemsworth J, Hill TR, et al. Nutritional status, body composition, and quality of life in community-dwelling sarcopenic and non-sarcopenic older adults: A case-control study. Clin Nutr. (2017) 36:267–74. doi: 10.1016/j.clnu.2015.11.013
34. Lei Z, Qingyi D, Feng G, Chen W, Hock RS, Changli W. Clinical study of mini-nutritional assessment for older Chinese inpatients. J Nutr Health Aging. (2009) 13:871–5. doi: 10.1007/s12603-009-0244-1
35. Weir CB, Jan A. BMI classification percentile and cut off points. In: StatPearls. (2019). Treasure Island (FL).
36. Zhou BF. Effect of body mass index on all-cause mortality and incidence of cardiovascular diseases–report for meta-analysis of prospective studies open optimal cut-off points of body mass index in Chinese adults. Biomed Environ Sci. (2002) 15:245–52.
37. Obesity: preventing and managing the global epidemic. Report of a WHO consultation. World Health Organ Tech Rep Ser. (2000) 894:i–xii, 1–253.
38. Liu H, Song B, Jin J, Liu Y, Wen X, Cheng S, Nicholas S, Maitland E, Wu X, Zhu D. Length of stay, hospital costs and mortality associated with comorbidity according to the charlson comorbidity index in immobile patients after ischemic stroke in China: a national study. Int J Health Policy Manag. (2021) 1–8. doi: 10.34172/ijhpm.2021.79
39. Adigüzel E, Acar-Tek N. Nutrition-related parameters predict the health-related quality of life in home care patients. Exp Gerontol. (2019) 120:15–20. doi: 10.1016/j.exger.2019.02.018
40. Lorenzo-López L, Maseda A, de Labra C, Regueiro-Folgueira L, Rodríguez-Villamil JL, Millán-Calenti JC. Nutritional determinants of frailty in older adults: A systematic review. BMC Geriatr. (2017) 17:108. doi: 10.1186/s12877-017-0496-2
41. Serrano-Urrea R, Garcia-Meseguer MJ. Malnutrition in an elderly population without cognitive impairment living in nursing homes in Spain: study of prevalence using the Mini Nutritional Assessment test. Gerontology. (2013) 59:490–8. doi: 10.1159/000351763
42. Inoue T, Misu S, Tanaka T, Kakehi T, Ono R. Acute phase nutritional screening tool associated with functional outcomes of hip fracture patients: A longitudinal study to compare MNA-SF, MUST, NRS-2002 and GNRI. Clin Nutr. (2019) 38:220–6. doi: 10.1016/j.clnu.2018.01.030
43. Jeejeebhoy KN, Keller H, Gramlich L, Allard JP, Laporte M, Duerksen DR, et al. Nutritional assessment: comparison of clinical assessment and objective variables for the prediction of length of hospital stay and readmission. Am J Clin Nutr. (2015) 101:956–65. doi: 10.3945/ajcn.114.098665
44. Agarwal E, Ferguson M, Banks M, Batterham M, Bauer J, Capra S, et al. Malnutrition and poor food intake are associated with prolonged hospital stay, frequent readmissions, and greater in-hospital mortality: results from the Nutrition Care Day Survey 2010. Clin Nutr. (2013) 32:737–45. doi: 10.1016/j.clnu.2012.11.021
45. Grossman A, Beloosesky Y, Schlesinger A, Gafter-Gvili A, Koren-Morag N, Meyerovitch J, et al. The association between glycated hemoglobin levels and mortality in non-diabetic elderly subjects. Eur J Intern Med. (2016) 27:57–61. doi: 10.1016/j.ejim.2015.10.010
46. Lee G, Choi S, Kim K, Yun JM, Son JS, Jeong SM, Kim SM, Park SM. Association of hemoglobin concentration and its change with cardiovascular and all-cause mortality. J Am Heart Assoc. (2018) 7:e007723. doi: 10.1161/JAHA.117.007723
47. Zakai NA, French B, Arnold AM, Newman AB, Fried LF, Robbins J, et al. Hemoglobin decline, function, and mortality in the elderly: the cardiovascular health study. Am J Hematol. (2013) 88:5–9. doi: 10.1002/ajh.23336
48. Yenibertiz D, Cirik MO. The comparison of GNRI and other nutritional indexes on short-term survival in geriatric patients treated for respiratory failure. Aging Clin Exp Res. (2020) 33:611–7. doi: 10.1007/s40520-020-01740-8
49. Hong X, Yan J, Xu L, Shen S, Zeng X, Chen L. Relationship between nutritional status and frailty in hospitalized older patients. Clin Interv Aging. (2019) 14:105–11. doi: 10.2147/CIA.S189040
50. Pérez-Ros P, Vila-Candel R, López-Hernández L, Martínez-Arnau FM. Nutritional status and risk factors for frailty in community-dwelling older people: a cross-sectional study. Nutrients. (2020) 12:1041. doi: 10.3390/nu12041041
51. Bouillanne O, Morineau G, Dupont C, Coulombel I, Vincent JP, Nicolis I, et al. Geriatric Nutritional Risk Index: a new index for evaluating at-risk elderly medical patients. Am J Clin Nutr. (2005) 82:777–83. doi: 10.1093/ajcn/82.4.777
52. Sousa AS, Guerra RS, Fonseca I, Pichel F, Amaral TF. Sarcopenia and length of hospital stay. Eur J Clin Nutr. (2016) 70:595–601. doi: 10.1038/ejcn.2015.207
53. Debbi EM, Rajaee SS, Spitzer AI, Paiement GD. Smoking and Total Hip Arthroplasty: Increased Inpatient Complications, Costs, and Length of Stay. J Arthroplasty. (2019) 34:1736–9. doi: 10.1016/j.arth.2019.03.059
54. Sari AA, Rezaei S, Arab M, Majdzadeh R, Matin BK, Zandian H. Effects of Smoking on Cost of Hospitalization and Length of Stay among Patients with Lung Cancer in Iran: a Hospital-Based Study. Asian Pac J Cancer Prev. (2016) 17:4421–6.
55. Miyagi S, Takamura T, Nguyen TTT, Tsujiguchi H, Hara A, Nakamura H, et al. Moderate alcohol consumption is associated with impaired insulin secretion and fasting glucose in non-obese non-diabetic men. J Diabetes Investig. (2021) 12:869–76. doi: 10.1111/jdi.13402
56. LaCroix AZ, Guralnik JM, Berkman LF, Wallace RB, Satterfield S. Maintaining mobility in late life. II Smoking, alcohol consumption, physical activity, and body mass index. Am J Epidemiol. (1993) 137:858–69. doi: 10.1093/oxfordjournals.aje.a116747
57. Stuck AE, Walthert JM, Nikolaus T, Büla CJ, Hohmann C, Beck JC. Risk factors for functional status decline in community-living elderly people: a systematic literature review. Soc Sci Med. (1999) 48:445–69. doi: 10.1016/S0277-9536(98)00370-0
58. Dworsky JQ, Russell MM. Surgical Decision Making for Older Adults. JAMA. (2019) 321:716. doi: 10.1001/jama.2019.0283
59. Kow AW. Prehabilitation and its role in geriatric surgery. Ann Acad Med Singap. (2019) 48:386–92.
60. Gordon EH, Peel NM, Samanta M, Theou O, Howlett SE, Hubbard RE. Sex differences in frailty: A systematic review and meta-analysis. Exp Gerontol. (2017) 89:30–40. doi: 10.1016/j.exger.2016.12.021
61. Snowdon DA, Ostwald SK, Kane RL. Education, survival, and independence in elderly Catholic sisters, 1936-1988. Am J Epidemiol. (1989) 130:999–1012. doi: 10.1093/oxfordjournals.aje.a115433
62. Luo Y, Zhang Z, Gu D. Education and mortality among older adults in China. Soc Sci Med. (2015) 127:134–42. doi: 10.1016/j.socscimed.2014.09.039
63. Tsai AC, Chang TL, Wang YC, Liao CY. Population-specific short-form mini nutritional assessment with body mass index or calf circumference can predict risk of malnutrition in community-living or institutionalized elderly people in taiwan. J Am Diet Assoc. (2010) 110:1328–34. doi: 10.1016/j.jada.2010.06.003
64. Tsai AC, Chang TL, Chen JT, Yang TW. Population-specific modifications of the short-form Mini Nutritional Assessment and Malnutrition Universal Screening Tool for elderly Taiwanese. Int J Nurs Stud. (2009) 46:1431–8. doi: 10.1016/j.ijnurstu.2009.05.004
65. Tsai AC, Chang MZ. Long-form but not short-form Mini-Nutritional Assessment is appropriate for grading nutritional risk of patients on hemodialysis–a cross-sectional study. Int J Nurs Stud. (2011) 48:1429–35. doi: 10.1016/j.ijnurstu.2011.05.004
Keywords: malnutrition parameters, mortality, length of stay, readmission, older inpatients, nutritional epidemiology
Citation: Liu H, Jiao J, Zhu M, Wen X, Jin J, Wang H, Lv D, Zhao S, Sun X, Wu X and Xu T (2022) Nutritional Status According to the Short-Form Mini Nutritional Assessment (MNA-SF) and Clinical Characteristics as Predictors of Length of Stay, Mortality, and Readmissions Among Older Inpatients in China: A National Study. Front. Nutr. 9:815578. doi: 10.3389/fnut.2022.815578
Received: 15 November 2021; Accepted: 03 January 2022;
Published: 25 January 2022.
Edited by:
Mauro Serafini, University of Teramo, ItalyReviewed by:
Yuan Hu, Chinese Center for Disease Control and Prevention, ChinaCopyright © 2022 Liu, Jiao, Zhu, Wen, Jin, Wang, Lv, Zhao, Sun, Wu and Xu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jing Jiao, amlhb2ppbmcuMjAwNkBhbGl5dW4uY29t; Xinjuan Wu, d3V4aW5qdWFuQHNpbmEuY29t; Tao Xu, eHV0YW9zZEAxMjYuY29t
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.