
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Nutr., 08 December 2022
Sec. Nutrition and Microbes
Volume 9 - 2022 | https://doi.org/10.3389/fnut.2022.1073576
A correction has been applied to this article in:
Corrigendum: The effects of three weight management methods on body composition and serum lipids of overweight and obese people
Introduction: Obesity has become a major health problem worldwide. Diet management is an important means of weight loss. The aim of this study was to explore the improvement effect of a calorie-restricted diet (CRD), 5 + 2 intermittent fasting (5 + 2 IF), and high protein diet (HPD) on weight composition and serum lipid level of overweight and obese people in a short period (3 months).
Methods: Fifty-three participants aged 18–60 years and with body mass index (BMI) ranging from 24 to 35 kg/m2 were screened for inclusion and exclusion criteria and were randomly divided into three groups, i.e., CRD, 5 + 2 IF, and HPD. Basic information, body composition, and venous blood samples were collected at baseline and after 3 months of intervention. Body composition was measured using a body composition analyzer (SK-V9), and serum lipids were assayed using the Roche Cobas e702 automatic biochemistry analysis system. The generalized estimating equation (GEE) was used to analyze and compare the repeated measurements of body composition and levels of serum lipids.
Results: The results showed that total weight, BMI, body fat mass, muscle mass, visceral fat index, and waist and hip circumferences had significantly decreased in all three groups after 3 months of intervention, and the average weight loss was 3.3 ± 1.14, 4.12 ± 0.05, and 2.62 ± 0.13 kg in CRD, 5 + 2 IF, and HPD groups, respectively. The results of the GEE model indicated that compared with the CRD group, the 5 + 2 IF group showed a more significant decrease in weight (β = −0.272, P < 0.001), BMI (β = −0.091, P < 0.001), body fat mass (β = −0.172, P < 0.001), muscle (β = −0.043, P < 0.001), and visceral fat index (β = −0.019, P < 0.001), however, HPD has more advantages in visceral fat index loss (β = −0.011, P < 0.001) and lean body mass preserve (β = 0.229, P < 0.001).
Conclusion: Our findings showed that the 5 + 2 IF may be more effective in reducing total weight and body fat, and HPD may be more helpful in preventing lean body mass loss during a short-term weight loss intervention.
Obesity is defined as “abnormal or excessive fat accumulation that may impair health,” which has become a major health problem worldwide and ranked as the sixth most common leading cause of death and disability in 2019 (1, 2). China has the highest number of overweight and obese people in the world; according to the Chinese criteria, about half of the adults are overweight or obese (3). Being overweight and obese are risk factors for many non-communicable diseases (NCDs), such as type 2 diabetes mellitus, cardiovascular disease, neurodegenerative diseases, and certain cancers (4). However, some studies have considered that the distribution of adipose tissue rather than the amount has shown a strong adverse association with the development of NCDs (5).
Comprehensive lifestyle interventions (CLIs) have been the foundation of the management of weight loss continuously, including the following three critical components: behavioral, dietary, physical activity change, and to produce a negative energy balance (6). Calorie-restricted diet (CRD) has recommended a daily caloric deficit of approximately 500 kcal (women: 1,200–1,500 kcal/day; men: 1,500–1,800 kcal/day) (7). Intermittent fasting (IF) is a more flexible calorie restriction strategy, which requests individuals to alternate between fasting and usual intake based on time, in which “fasting” days of 500–800 kcal intake (8). The efficiency of metabolic regulation and weight loss can be affected by circadian rhythms as energy homeostasis is maintained by the interaction of peripheral signals with the central nervous system (9). Besides, a high protein diet (HPD) might be a novel strategy for the weight loss of overweight and obesity. HPD adjusts the proportion of dietary protein in the energy supply of the macronutrients, which could promote satiety, and energy expenditure and in changing body composition in favor of lean mass (10). Changes in the macronutrient composition affect hormones, metabolic pathways, gene expression, and the composition and function of the gut microbiome which might impact fat storage (9). Although the above three weight management methods have significant weight loss effects, which can effectively lose weight in a short period and improve metabolic indicators, this needs to be confirmed by further research.
The present study reviewed the metabolic indicators of body weight, body composition, and serum lipids before and after 3 months of weight loss management in the participants who have participated in the CRD, 5 + 2 IF, and HPD in the weight management clinic, and we would like to explore the safety and effective weight loss management in the short term.
All participants gave written informed consent to this study, and this study obtained a favorable opinion from the Human Ethics Committee of the Peking Union Medical College Hospital (2020PHD007-001). The participants were overweight or obese staff volunteers who participated in weight loss intervention at the nutrition and weight loss Clinic of Peking University People’s Hospital from August to September 2020. Inclusion criteria were 18–60 years of age and body mass index (BMI) ranged from 24 to 35 kg/m2. The exclusion criteria were (1) secondary obesity caused by endocrine or genetic, such as hypothalamic obesity, pituitary obesity, hypothyroidism obesity, obesity caused by Cushing’s syndrome, and hypogonadism obesity; (2) unable to consume test protein intake due to intolerances/dietary preferences/severe liver and kidney diseases; (3) those who are dieting or trying to lose weight recently; (4) pregnant or planning to become pregnant (within 3 months) or currently breastfeeding; and (5) metabolic health disturbance, malignancy, or other severe illnesses, such as diabetes, cancer, coronary heart disease, stroke, severe gastrointestinal diseases, or treatment that may interfere with study variable.
Fifty-three participants underwent a 3-month intervention with three different weight management methods, and the sample size of this study is combined with the research demand. A computer-generated random number was used to randomly divide the patients into three groups, i.e., 18 people were on a CRD, 18 people were on a 5 + 2 intermittent fasting (5 + 2 IF), and 17 people were on an HPD. CRD is a dietary pattern that limits energy intake while ensuring basic nutritional needs. The energy supply ratio of macronutrients meets the requirements of a balanced diet. Based on satisfying the five nutrients of proteins, vitamins, minerals, dietary fibers, and water, moderately reduce the intake of fat and carbohydrates, and reduce the energy of normal diet by 30–50% of the low-energy dietary pattern; 5 + 2 IF, in which participants fasted for 2 days per week (either consecutively or non-consecutively) with total caloric intake 1/4 of the usual energy (approximately 500 kcal for women and 600 kcal for men) and 5 days of ad libitum eating; HPD recommended participants daily intake for protein at 1.5 g/(kg body weight daily), or 20∼30% of the total daily energy intake. In this study, participants in the HPD group consumed protein with 20∼25% of the total daily energy intake.
Researchers were professional nutritionists and dietitians. Participants were asked to follow up with the weight loss clinic once a week to strengthen the personalized diet plan, and nutrition education will be carried out online every 2 weeks. A group management approach to quality control of subjects’ implementation of weight management methods was through WeChat.
Researchers have collected basic information on participants at baseline and after 3 months of intervention, including gender, age, waist and hip circumferences, systolic pressure (SBP), and diastolic pressure (DBP). Body composition including height, weight, BMI (BMI was calculated as weight kg/height m2), body fat mass, muscle mass, and visceral fat index (visceral fat index = visceral fat area cm2/10 cm2) was measured and calculated using a body composition analyzer (SK-V9).
Notably, 6 ml of venous blood samples for biochemical parameters were obtained in the morning after overnight fasting (more than 10 h) for analysis. Whole blood and plasma were collected in vacutainer tubes with anticoagulant Ethylenediaminetetraacetic acid (EDTA), and the relevant indicators were tested in a timely manner. Serum levels of total cholesterol (TC), triglyceride (TG), low-density lipoprotein cholesterol (LDL-C), and high-density lipoprotein cholesterol (HDL-C) were assayed using the Roche Cobas e702 automatic biochemistry analysis system. Serum levels of alanine transaminase (ALT), aspartate transaminase (AST), total bilirubin (TBIL), direct bilirubin (DBIL), urea, creatinine (CRE), and uric acid (UA) were assayed using the BECKMAN COULTER AU5800 automatic biochemistry analysis system, and Roche and BECKMAN kit for auto-analyzer were used.
Continuous variables are presented as mean ± SD or median (interquartile range), and categorical variables are presented as frequencies (percentages). One-way analysis of variance (ANOVA) or Kruskal–Wallis rank sum test for continuous variables and the chi-square test or Fisher exact test for categorical variables were run to determine whether there were differences between groups at baseline. The generalized estimating equation (GEE) was used to analyze and compare the repeated measurements of weight, BMI, body fat mass, muscle mass, visceral fat index, and serum lipids among the three groups at baseline and after 3 months of intervention. All the studies were collected by questionnaire and analyzed using SPSS (version 24.0), and GraphPad Prism 8.0 software was used to draw statistical figures. P < 0.05 was considered statistically significant.
A summary of the characteristics of 53 participants at baseline is shown in Table 1. There were 18 people in the CRD group, 18 people in the 5 + 2 IF group, and 17 people in the HPD group. At baseline, three groups were of balanced sex, age, height, ALT, AST, TBIL, DBIL, urea, CRE, UA, SBP, and DBP.
As shown in Figure 1, there was no significant difference in weight, BMI, body fat mass, muscle mass, visceral fat index, waist circumference, and hip circumference of CRD, 5 + 2 IF, and HPD at baseline (P > 0.05). Among CRD, 5 + 2 IF, and HPD groups, after 3 months of intervention, the average weight loss was 3.3 ± 1.14, 4.12 ± 0.05, and 2.62 ± 0.13 kg, respectively; the average BMI reduction was 1.15 ± 0.194, 1.422 ± 0.19, and 1.024 ± 0.112, respectively; the body fat mass loss was 2.35 ± 0.56, 2.86 ± 0.2, and 2.23 ± 0.23 kg, respectively; the muscle mass reduction was 0.94 ± 0.52, 1.07 ± 0.17, and 0.25 ± 0.06 kg, respectively; the visceral fat index was decreased by 0.56 ± 0.27, 0.61 ± 0.16, and 0.59 ± 0.14, respectively; the waist circumference was decreased by 5.72 ± 0.47, 4.78 ± 0.18, and 4.41 ± 0.73 cm, respectively; the hip circumference was decreased by 5.16 ± 0.02, 5.56 ± 1.52, and 3.58 ± 0.57 cm, respectively.
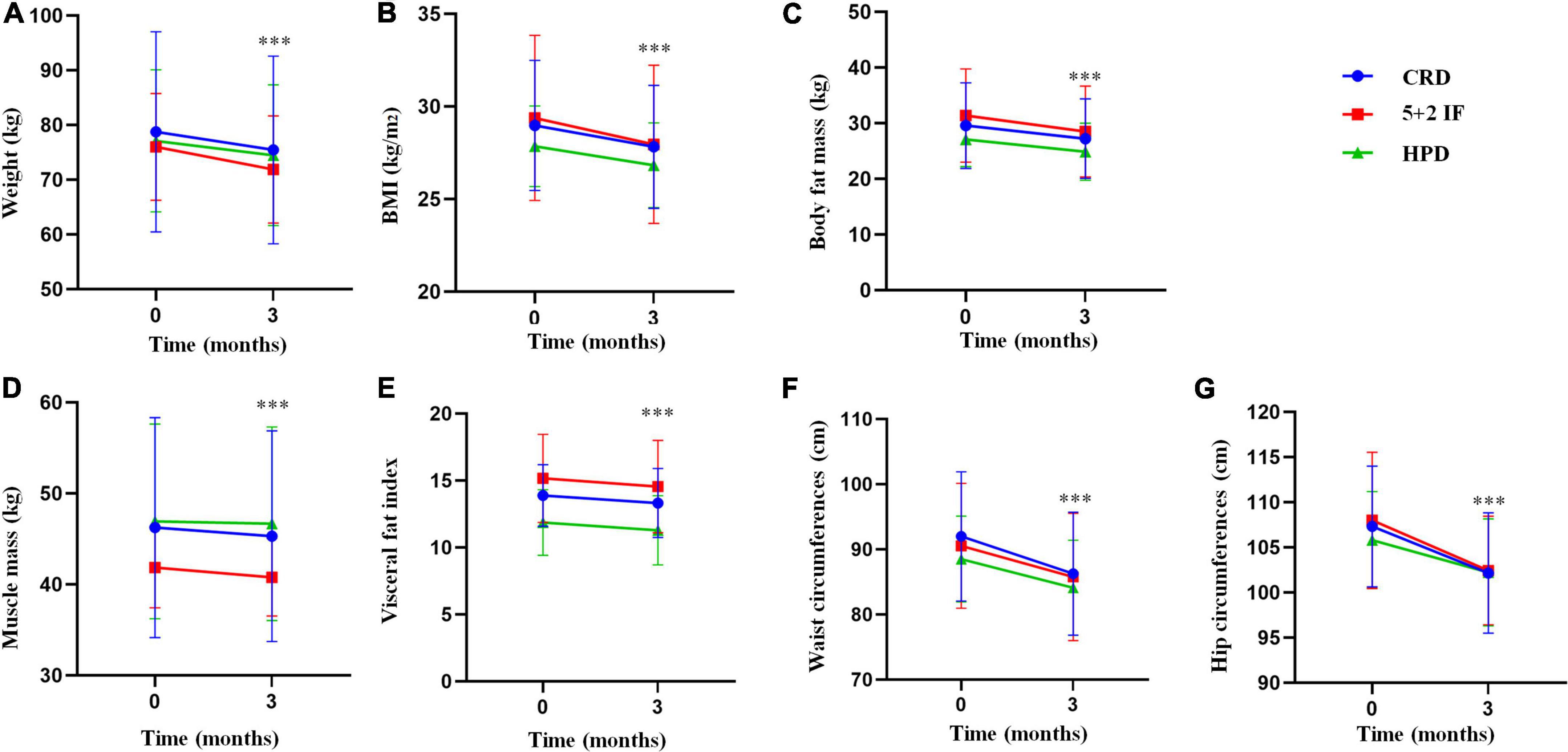
Figure 1. Results of body composition and body mass index (BMI) among the treatment and control groups. 5 + 2 IF, 5 + 2 intermittent fasting; BMI, body mass index; CRD, calorie-restricted diet; HPD, high protein diet; SE, standard error. The figure shows the level of body composition before and after three weight management methods by mean ± standard deviation [(A) weight; (B) BMI; (C) body fat mass; (D) muscle mass; (E) visceral fat index; (F) waist circumference; (G) hip circumference], ***P < 0.001.
Table 2 shows the results of the GEE model adjusting gender, age, group, time, and interaction factors of group and time. The results show that, compared with the baseline, the three weight management methods are (β = −1.1, P < 0.001), BMI (β = −0.383, P < 0.001), body fat mass (β = −0.738, P < 0.001), muscle mass (β = −0.313, P < 0.001), visceral fat index (β = −0.185, P < 0.001), waist circumference (β = −1.907, P < 0.001), and hip circumference (β = −1.722, P < 0.001). Compared with the CRD group, the 5 + 2 IF group showed a more significant decrease in weight (β = −0.272, P < 0.001), BMI (β = −0.091, P < 0.001), body fat mass (β = −0.172, P < 0.001), muscle (β = −0.043, P < 0.001), and visceral fat index (β = −0.019, P < 0.001), however, HPD has more advantages in visceral fat index loss (β = −0.011, P < 0.001) and lean body mass preserve (β = 0.229, P < 0.001).
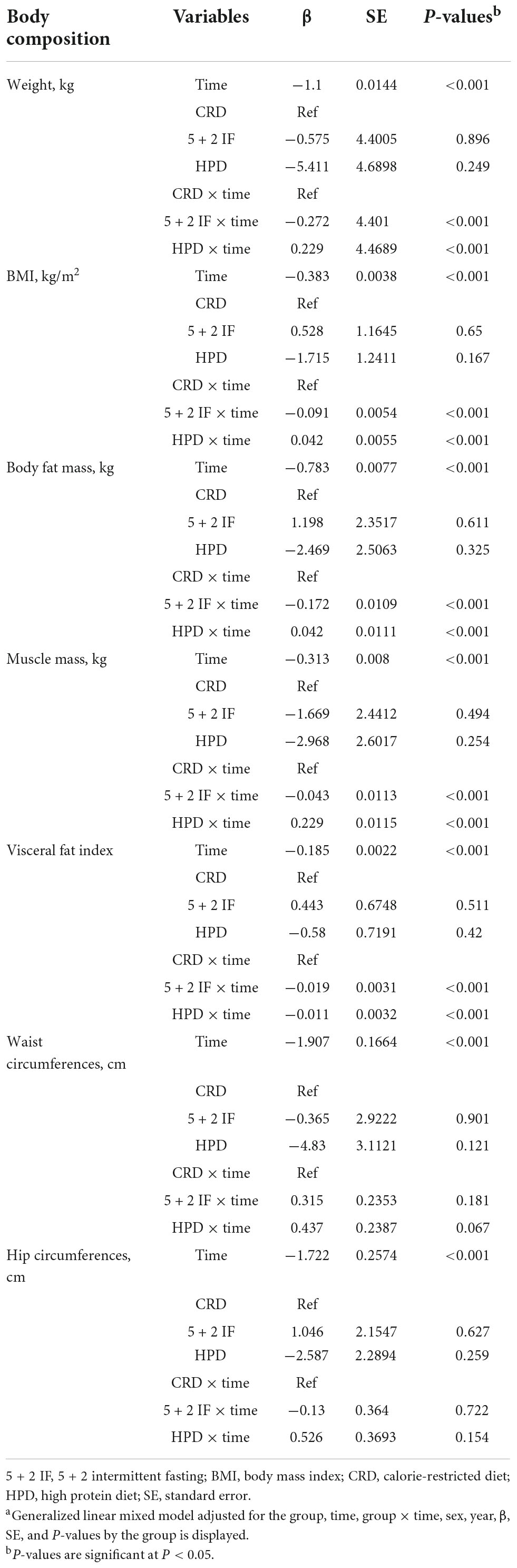
Table 2. Adjusted model for body composition and body mass index (BMI) results at baseline and 3 months among three groups in a randomized, placebo-controlled trial.a
The results of the model have an adjustment for gender, age, group, time, and interaction factors of the group, and time showed that TC, TG, HDL-C, LDL-C, and LDL-C/HDL-C did not differ among the three groups, and the specific results are shown in Table 3.
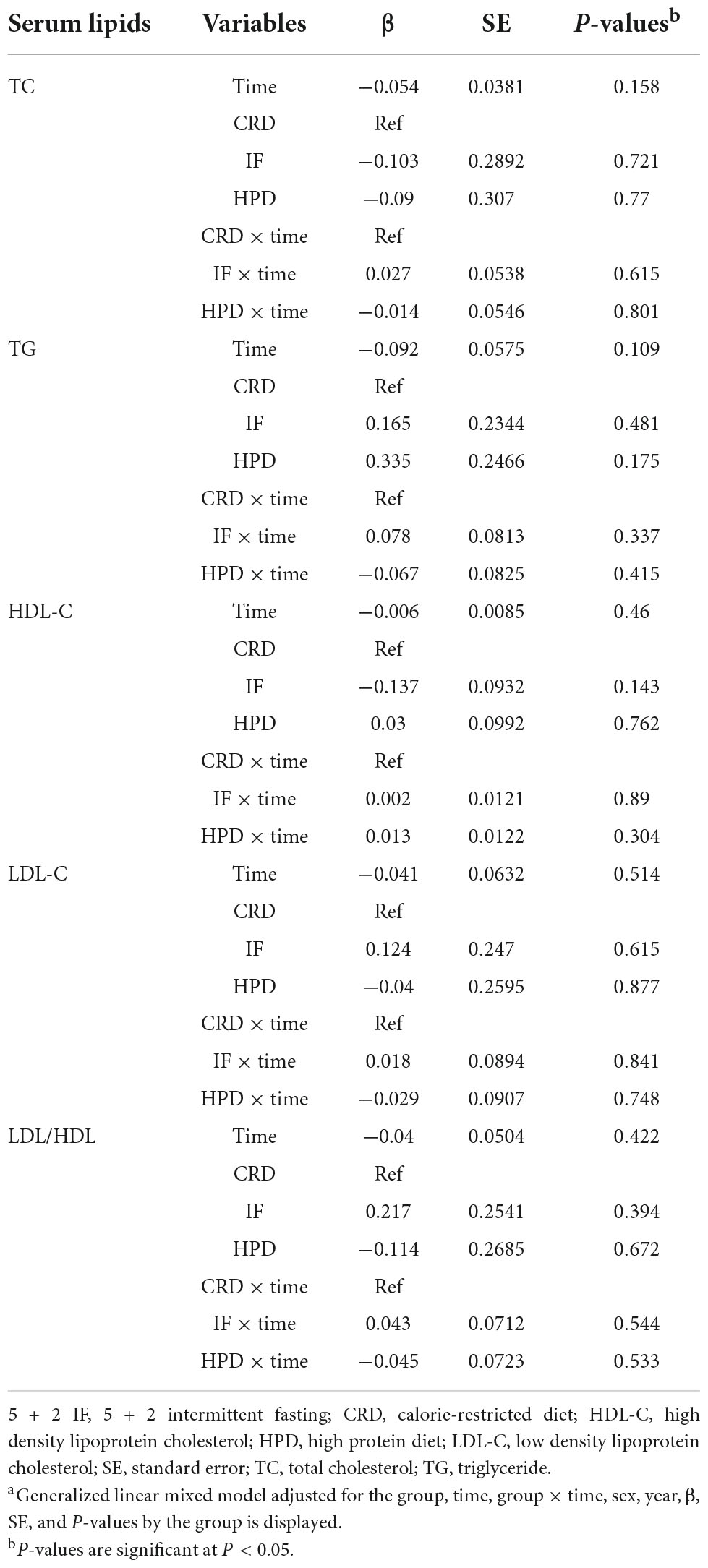
Table 3. Adjusted model for serum lipid results at baseline and 3 months among three groups in a randomized, placebo-controlled trial.a
Our findings found that all three weight management diets had significant effects on weight loss, BMI, total fat, visceral fat index, and waist and hip circumferences. Compared with the other two weight loss diets, 5 + 2 IF is more effective in reducing weight, BMI, total fat content, and visceral fat; an HPD is more helpful in preventing muscle mass loss while reducing weight.
Meta-analysis suggests that IF is associated with statistically significant weight loss of more than 5% in adults with overweight or obese, and participants were found to be significantly decreased by 1.67 kg (95% CI, −2.79 to −0.55) following 3 months of the 5 + 2 diet (11–13). A study on overweight and obese women (n = 115) aged 20–69 years with a family history of breast cancer found that the IF diet is superior to the CRD diet with respect to the improvements in insulin sensitivity and the loss of body fat (14). Michelle et al.’s study on 107 patients with overweight and obese found that the average weight loss of the 3-month CRD diet group was 4.1 kg, and the average weight loss of the IF was 3.0 kg (15). In this research, the average weight loss of the 5 + 2 IF group was 4.12 kg after 3 months, accounting for 5.3% of the baseline weight, which was consistent with the research before. In addition, our study shows that the 5 + 2 IF group is superior to the CRD group and the HPD group in reducing BMI, body fat mass, visceral fat index, and waist and hip circumferences. A meta-analysis suggested that IF diets were associated with higher weight loss and fat mass decrease compared with a continuous energy restriction (CER) regimen (16), which shows that the 5 + 2 IF has greater advantages in short-term (3 months) weight loss.
A total of 8 weeks of randomized clinical trials (RCTs) suggested that HPD appeared to be more beneficial than a low glycemic index (GI) diet, as indicated by the greater fat mass loss and preservation of muscle mass (17). Our study suggests that the average weight loss of the HPD group was 2.62 kg, accounting for 3.4% of the baseline weight. The HPD group was slightly inferior to the CRD group and the 5 + 2 IF group in terms of total weight loss, BMI, and body fat loss, but better than the CRD group in terms of visceral fat index reduction. In addition, the HPD group had the least reduction in muscle mass, which was more conducive to reducing the loss of lean weight than the CRD and the 5 + 2 IF group. A recent meta-analysis suggested that supplying whey protein to overweight and obese individuals decreased body fat mass, preserved lean body mass, and improved metabolic waist circumference (10, 18, 19). This may indicate that protein plays a key role in preventing muscle loss during weight management.
An umbrella review of 11 meta-analyses of RCTs indicated that modified alternate-day fasting (MADF) was also found to be associated with the improvement of several cardiometabolic risk factors including LDL-C, TC, TG, and blood pressure (11), and this indicates that MADF may have the effect of improving serum lipids, although our study has not found the improvement effect of 5 + 2 IF on blood lipid. An RCT found that compared with obese patients who added maltodextrin to their diet, obese patients who added whey protein-lipid profiles in plasma have improved (20), and this shows that whey protein may play a role in improving serum lipids. Our research has not found that HPD can reduce blood lipids. We speculate that it might have normal blood lipids and blood pressure at baseline, and it was not surprising that most metabolic risk indicators were unchanged.
Our study has compared the effects of CRD, 5 + 2 IF, and HPD on weight loss, BMI, body fat mass, muscle mass, visceral fat index, waist circumference, hip circumference, and serum lipids within 3 months, and this study provides a reference for short-term weight loss and body fat mass reduction, which is innovative and practical. Weight loss can effectively improve metabolic indicators and prevent the occurrence and development of diseases related to overweight and obesity, such as diabetes and cardiovascular and cerebrovascular diseases. This study provides three methods that can effectively reduce body weight and improve lipid metabolism and distribution with certain clinical significance. However, this study also has some limitations. Due to the short-term of the study, the effect of three weight management methods on improving serum lipids has not been found, which needs to be confirmed by further longer and larger sample size studies. Besides, we lack using a tool to assess dietary intake as well; in addition, we will increase observation time points in future research and analyze inflammation, glucose metabolism, and other indicators to further explore the effects of three weight loss methods on metabolism and explore the mechanism.
Three ways of weight management have significant reduction effects on weight loss, body fat mass, visceral fat index, and waist and hip circumferences. The 5 + 2 IF has the most significant effect on total weight loss and body and visceral fat reduction, and HPD has more advantages in preserving muscle mass.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by the Human Ethics Committee of the Peking Union Medical College Hospital. The patients/participants provided their written informed consent to participate in this study.
PL conceived and designed the study. JC and WL performed the analyses and wrote the manuscript. LS and SZ collected and analyzed the data. All authors read and approved the final manuscript.
This study was supported by the Research and Development Fund of Peking University People’s Hospital (2020).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
5 + 2 IF, 5 + 2 intermittent fasting; ALT, alanine transaminase; AST, aspartate transaminase; BMI, body mass index; CRD, calorie-restricted diet; CRE, creatinine; DBIL, direct bilirubin; DBP, diastolic pressure; HDL-C, high-density lipoprotein cholesterol; HPD, high protein diet; SBP, systolic pressure; LDL-C, low-density lipoprotein cholesterol; TBIL, total bilirubin; TC, total cholesterol; TG, triglyceride; UA, uric acid.
1. Safaei M, Sundararajan EA, Driss M, Boulila W, Shapi’i A. A systematic literature review on obesity: Understanding the causes & consequences of obesity and reviewing various machine learning approaches used to predict obesity. Comput Biol Med. (2021) 136:104754. doi: 10.1016/j.compbiomed.2021.104754
2. Lin X, Li H. Obesity: epidemiology, pathophysiology, and therapeutics. Front Endocrinol (Lausanne). (2021) 12:706978. doi: 10.3389/fendo.2021.706978
3. Wang Y, Zhao L, Gao L, Pan A, Xue H. Health policy and public health implications of obesity in China. Lancet Diabetes Endocrinol. (2021) 9:446–61. doi: 10.1016/S2213-8587(21)00118-2
4. Stefan N, Birkenfeld AL, Schulze MB. Global pandemics interconnected - obesity, impaired metabolic health and COVID-19. Nat Rev Endocrinol. (2021) 17:135–49. doi: 10.1038/s41574-020-00462-1
5. Wan H, Wang Y, Xiang Q, Fang S, Chen Y, Chen C, et al. Associations between abdominal obesity indices and diabetic complications: Chinese visceral adiposity index and neck circumference. Cardiovasc Diabetol. (2020) 19:118. doi: 10.1186/s12933-020-01095-4
6. Mayer SB, Graybill S, Raffa SD, Tracy C, Gaar E, Wisbach G, et al. Synopsis of the 2020 U.S. VA/DoD clinical practice guideline for the management of adult overweight and obesity. Mil Med. (2021) 186:884–96. doi: 10.1093/milmed/usab114
7. Tchang BG, Saunders KH, Igel LI. Best practices in the management of overweight and obesity. Med Clin North Am. (2021) 105:149–74. doi: 10.1016/j.mcna.2020.08.018
8. Fanti M, Mishra A, Longo VD, Brandhorst S. Time-restricted eating, intermittent fasting, and fasting-mimicking diets in weight loss. Curr Obes Rep. (2021) 10:70–80. doi: 10.1007/s13679-021-00424-2
9. Freire R. Scientific evidence of diets for weight loss: different macronutrient composition, intermittent fasting, and popular diets. Nutrition. (2020) 69:110549. doi: 10.1016/j.nut.2019.07.001
10. Simonson M, Boirie Y, Guillet C. Protein, amino acids and obesity treatment. Rev Endocr Metab Disord. (2020) 21:341–53. doi: 10.1007/s11154-020-09574-5
11. Patikorn C, Roubal K, Veettil SK, Chandran V, Pham T, Lee YY, et al. Intermittent fasting and obesity-related health outcomes: an umbrella review of meta-analyses of randomized clinical trials. JAMA Netw Open. (2021) 4:e2139558. doi: 10.1001/jamanetworkopen.2021.39558
12. Holmer M, Lindqvist C, Petersson S, Moshtaghi-Svensson J, Tillander V, Brismar TB, et al. Treatment of NAFLD with intermittent calorie restriction or low-carb high-fat diet - a randomised controlled trial. JHEP Rep. (2021) 3:100256. doi: 10.1016/j.jhepr.2021.100256
13. He S, Wang J, Zhang J, Xu J. Intermittent versus continuous energy restriction for weight loss and metabolic improvement: a meta-analysis and systematic review. Obesity (Silver Spring). (2021) 29:108–15. doi: 10.1002/oby.23023
14. Harvie M, Wright C, Pegington M, McMullan D, Mitchell E, Martin B, et al. The effect of intermittent energy and carbohydrate restriction v. daily energy restriction on weight loss and metabolic disease risk markers in overweight women. Br J Nutr. (2013) 110:1534–47. doi: 10.1017/S0007114513000792
15. Harvie MN, Pegington M, Mattson MP, Frystyk J, Dillon B, Evans G, et al. The effects of intermittent or continuous energy restriction on weight loss and metabolic disease risk markers: a randomized trial in young overweight women. Int J Obes (Lond). (2011) 35:714–27. doi: 10.1038/ijo.2010.171
16. Enriquez Guerrero A, San MMI, Garicano VE, Camina MMA. Effectiveness of an intermittent fasting diet versus continuous energy restriction on anthropometric measurements, body composition and lipid profile in overweight and obese adults: a meta-analysis. Eur J Clin Nutr. (2021) 75:1024–39. doi: 10.1038/s41430-020-00821-1
17. Walilko E, Napierala M, Bryskiewicz M, Fronczyk A, Majkowska L. High-protein or low glycemic index diet-which energy-restricted diet is better to start a weight loss program? Nutrients. (2021) 13:1086. doi: 10.3390/nu13041086
18. Badely M, Sepandi M, Samadi M, Parastouei K, Taghdir M. The effect of whey protein on the components of metabolic syndrome in overweight and obese individuals; a systematic review and meta-analysis. Diabetes Metab Syndr. (2019) 13:3121–31. doi: 10.1016/j.dsx.2019.11.001
19. Hall KD. The potential role of protein leverage in the US obesity epidemic. Obesity (Silver Spring). (2019) 27:1222–4. doi: 10.1002/oby.22520
Keywords: 5 + 2 IF, 5 + 2 intermittent fasting, body mass index (BMI), calorie-restricted diet (CRD), high protein diet (HPD), obesity, serum lipids
Citation: Cai J, Shao L, Zhao S, Liu W and Liu P (2022) The effects of three weight management methods on body composition and serum lipids of overweight and obese people. Front. Nutr. 9:1073576. doi: 10.3389/fnut.2022.1073576
Received: 19 October 2022; Accepted: 16 November 2022;
Published: 08 December 2022.
Edited by:
George Grant, University of Aberdeen, United KingdomReviewed by:
Haitham Jahrami, Arabian Gulf University, BahrainCopyright © 2022 Cai, Shao, Zhao, Liu and Liu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Wen Liu, YWFhMjAwODQxQDE2My5jb20=; Peng Liu, bGl1cGVuZ3BrdUAxNjMuY29t
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.