- 1Centre for Quality Management of Medicines, Faculty of Pharmacy, Universiti Kebangsaan Malaysia, Kuala Lumpur, Malaysia
- 2Centre for Community Health Studies, Faculty of Health Sciences, Universiti Kebangsaan Malaysia, Kuala Lumpur, Malaysia
Purpose: To estimate the vitamin D status of participants residing in Malaysia.
Methods: PubMed, Scopus, Web of Science, and MyJurnal were searched up to June 2022 without language restrictions. Studies that reported the 25-hydroxyvitamin D [25(OH)D] concentrations and defined their cut-off for deficiency or insufficiency from healthy participants residing in Malaysia were included. The random effects model was used to pool vitamin D status using established cut-offs of <30, <50, and <75 nmol/L according to age group.
Results: From 299 studies screened, 32 studies were included in the meta-analysis. The pooled proportion for <30 nmol/L was 21% (95% CI 9–36, n = 2,438 from 10 studies), while the pooled proportion <50 nmol/L was 64% (95% CI 56–72, n = 13,977 from 30 studies), and <75 nmol/L was 85% (95% CI 61–100, n = 1,376 from five studies). Heterogeneity was high (I2 ranged from 98–99%). Higher proportions of vitamin D insufficiency (defined as <50 nmol/L) were found in participants living in the urban areas (compared to rural areas), in females (compared to males), and in Malays and Malaysian Indians (compared to Malaysian Chinese) ethnicities.
Conclusion: More than half of Malaysians have insufficient vitamin D levels, despite being a country that is close to the equator. We strongly urge prompt public health measures to improve the vitamin D status in Malaysia.
Systematic review registration: [https://www.crd.york.ac.uk/prospero/], identifier [CRD42021260259].
Introduction
Vitamin D is well-recognized as a hormone that plays an essential role in maintaining adequate serum calcium and phosphate concentrations and bone health. The importance of vitamin D in maintaining a sound immune system has also been well-discussed (1). Following the coronavirus disease-2019 (COVID-19) pandemic, there has been a renewed interest in understanding the role of vitamin D in managing COVID-19 infection (2). Several systematic reviews have demonstrated that vitamin D levels are associated with the severity of COVID-19 conditions (3–11). This is echoed by several clinical trials showing positive outcomes of supplementing vitamin D in COVID-19 infection, especially in deficient patients (8, 12–15). Although the exact benefit of vitamin D in COVID-19 management remains debatable (16–19), the importance of maintaining adequate vitamin D levels for general health is not disputed.
There is no consensus on the optimal vitamin D concentration in the body [measured as 25-hydroxyvitamin D; 25(OH)D]. It is generally agreed that concentrations <30 nmol/L (or 12 ng/ml) should be avoided in all age groups (20), but the definition of deficiency and insufficiency varies between guidelines. The Endocrine Society Clinical Practice Guidelines 2011 defines vitamin D deficiency as 25(OH)D concentrations <50 nmol/L (or <20 ng/ml), while 50–75 nmol/L (or 20–30 ng/ml) is defined as insufficient (21). The Endocrine Society further recommends levels above 75 nmol/L to reduce the risk of infectious diseases and to obtain other non-calcemic benefits of vitamin D. On the other hand, the Institute of Medicine (IOM) defines vitamin D deficiency as <30 nmol/L, while 30–50 nmol/L is insufficient (22). The IOM have used bone health as the main basis for their recommendations. Misra et al. (23), define vitamin D deficiency as ≤37.5 nmol/L and insufficiency as 37.5–50 nmol/L (23). Although there is no consensus on the terminology, a cut-off of <50 nmol/L is commonly used between guidelines. At this concentration, there are compensatory mechanisms activated to maintain calcium homeostasis, which will affect bone and muscle health (24).
Malaysia is a Southeast Asian country close to the equator, with latitudes ranging from 1.2°N to 6.8°N. Malaysia consists of two regions: Peninsular Malaysia, which houses approximately 80% of the Malaysian population, and Malaysian Borneo. It has an equatorial climate with relatively stable temperatures all year that are hot, sunny, and humid with an average daily temperature that ranges between 21 and 32°C. Seasonal climate variability is closely tied to the drier Southwest Monsoon, which occurs from April to September, and the wetter Northeast Monsoon, from October to March (25). In theory, during periods of heavy rainfall, more of the population may be confined indoors, limiting their sun exposure during the day. However, in a recent study, Aris et al. (26) reported that while there was a significant decrease in vitamin D concentrations during the monsoon season for some subgroup of individuals, there was no significant difference in the vitamin D status between monsoon and non-monsoon season (26). Approximately 69.8% of the 29.9 million Malaysian population is Malay and Bumiputera, 22.4% is Chinese (i.e., Malaysian Chinese), 6.8% is Indian (i.e., Malaysian Indian), and the remainder is other ethnicities (27). Malaysian Chinese generally have fair skin tone, whereas, Malays’ skin tone may vary from light to tanned, and most Malaysian-Indians have darker skin tone (28). As vitamin D is synthesized in the skin following sunlight exposure and is highly correlated with skin color, the Malay and Malaysian Indian populations are at higher risk of lower vitamin D status.
A recent review article has highlighted several studies have investigated the vitamin D status of subpopulations in Malaysia (29). Most of the results have indicated that vitamin D status is low in Malaysia. However, the prevalence of vitamin D status has not been pooled across studies. Therefore, the primary aim of this research is to combine the data from studies that have been conducted on the vitamin D status in populations living in Malaysia.
Methods
This systematic review was conducted following the PRISMA guidelines (37) and was registered in PROSPERO (CRD42021260259).
Identifying published studies
We searched through PubMed, Scopus, Web of Science, and MyJurnal (a Malaysian Journal database) from the inception of each database until June 2022. A systematic search was conducted to identify all studies that reported vitamin D status in Malaysian residents. The search terms included (Vitamin D OR its synonyms) AND (Malaysia OR its synonyms). The full record of the search strategy is presented in Supplementary material 1. We did not use any language or other search limits. Key review publications were also identified and searched for further relevant studies. In addition, the reference lists from the identified studies were also examined for potentially relevant studies.
Inclusion and exclusion criteria
For a study to be included in the systematic review, there were two inclusion criteria: (i) the study measured serum 25(OH)D levels in healthy Malaysians, and (ii) it was non-interventional study and conducted either as a cross-sectional, case-control, or longitudinal study design. For longitudinal studies, baseline vitamin D levels must be provided. Studies were excluded if they were: (i) case reports or case series, or (ii) meeting abstracts or unpublished materials, (iii) articles that were not written in English, (iv) review articles and meta-analyses.
The meta-analysis considered only data from healthy population subgroups for case-control studies. We excluded studies where the lifestyle differed significantly from Malaysia’s general population from the meta-analysis. If a subsequent research included data from a previous cohort of individuals, the study with the larger sample size would be included in the meta-analysis.
Three investigators (NAJ, SMS, NAMT) developed the search strategy. Then, SMS and NAMT performed the database search and independently screened the retrieved articles based on the titles and abstracts. All four authors assessed the full-text articles and selected studies based on the inclusion and exclusion criteria. Any disagreements in the study selection were resolved by consensus. All data were extracted from the selected studies using a standardized extraction form, including information on the study location, data collection period, population demographics (ethnicity, sex, age), assay method, vitamin D status (including cut-off definitions), and vitamin D concentrations.
Critical appraisal of studies included
After considering various quality assessment tools for prevalence studies (38), the Joanna Briggs Institute Prevalence Critical Appraisal Tool, 2014 (39, 40) was used for quality assessment. Three investigators (EMH, NAJ, and SMS) critically appraised and rated the studies included in the meta-analysis using the tool. The tool consists of nine questions with four standard answer options (yes/no/unclear/not applicable). Each rater rated independently; however, discussions were carried out to ensure that discrepancies were discussed and agreed upon through consensus.
Statistical analysis
For the overall data, we performed a meta-analysis using three predetermined vitamin D cut-off values (<30, <50, and <75 nmol/L) sub-grouped by age category and a meta-analysis of mean 25(OH)D levels. The random-effects model was used to pool the proportion and mean values given an a priori assumption of heterogeneity between prevalence studies (41). If the mean and standard deviation were not provided, they were estimated from the median, interquartile range, range, and sample size, assuming that the data were not significantly skewed (42). For all meta-analyses of specific subgroup proportions (e.g., gender, ethnicity), a cut-off of <50 nmol/L was used, in view that this cut-off is present in almost all of the studies. We examined the presence of heterogeneity using the Q statistic with P < 0.05 indicating significant heterogeneity exists. The heterogeneity between studies was then quantified using the I2 statistics with values of <25, <50, and <75% indicating low, moderate, and high, and the χ2 test with P < 0.05 to denote significance (43). All analyses were performed using MetaXL, version 5.3 (EpiGear International, Sunrise Beach, QLD, Australia). A sensitivity analysis is, by default, reported by MetaXL by excluding one study at a time and recalculating the pooled effect sizes and the associated heterogeneity statistics. The funnel plot was not used as it is inaccurate to assess publication bias for prevalence studies (44). The overall mean vitamin D levels and the proportion of vitamin D deficiency/insufficiency were also summarized by study location.
Results
Literature search results and characteristics of the eligible studies
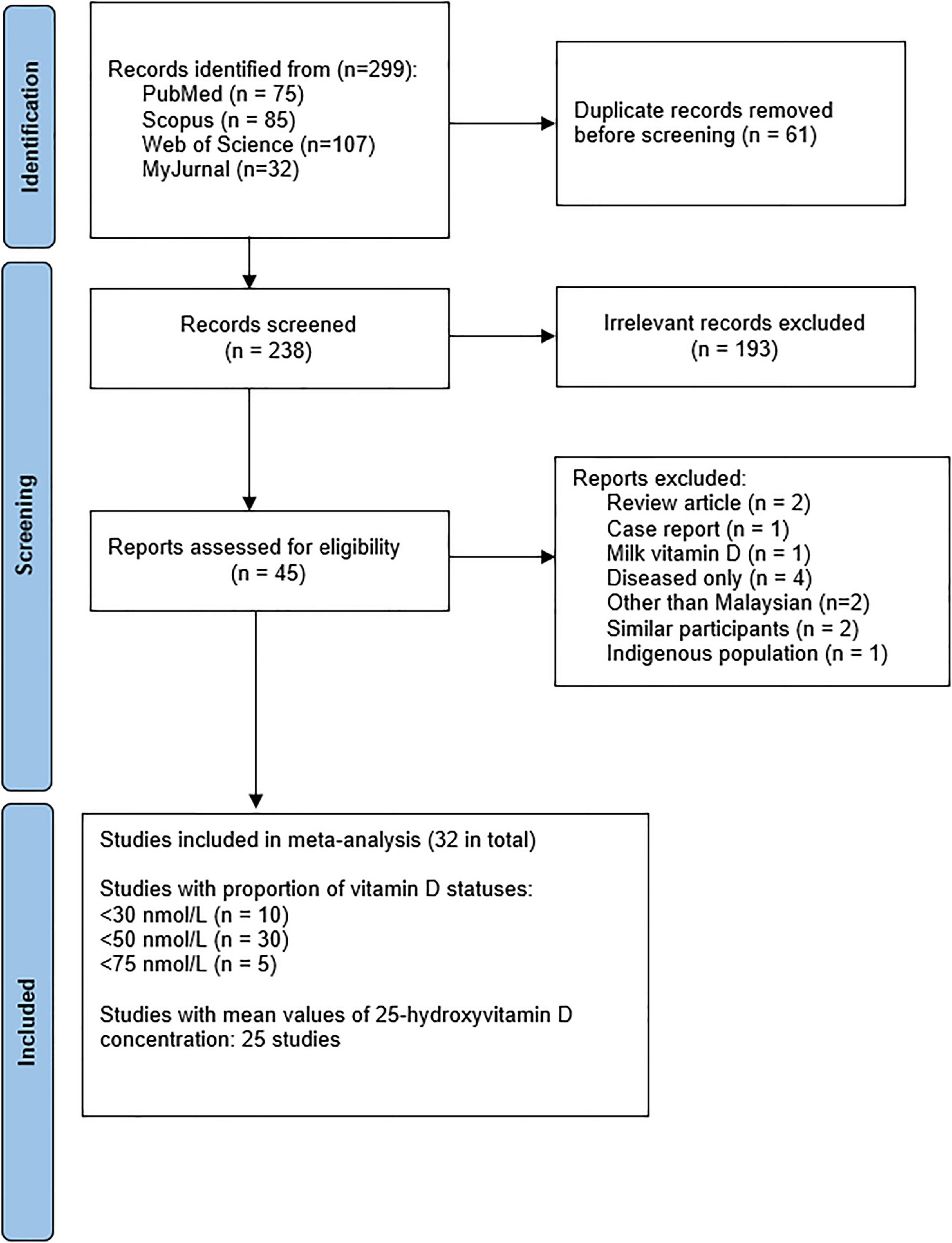
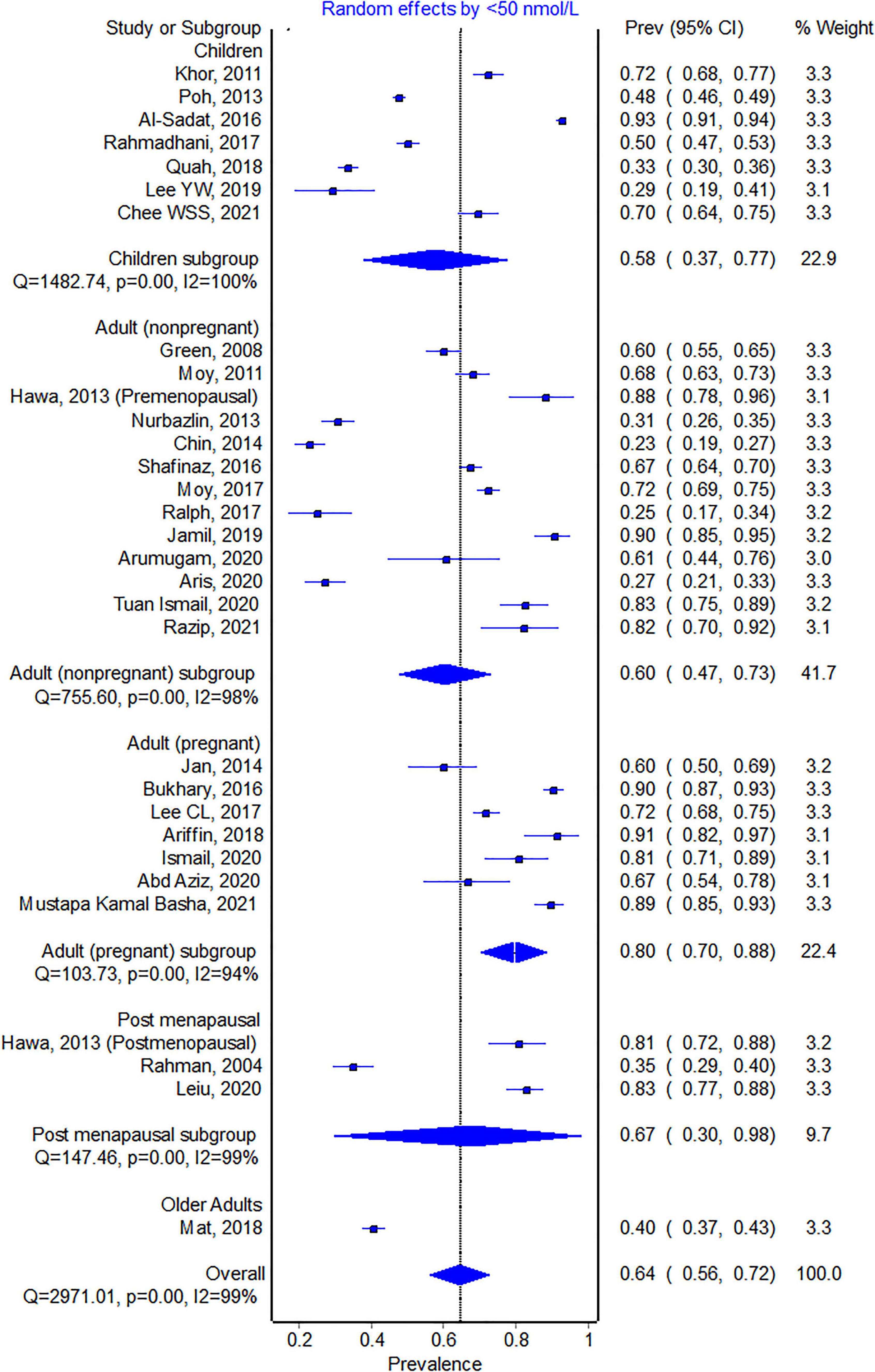
From the 299 articles identified, 45 full-text articles were assessed, and 32 studies were included in the systematic review and meta-analysis (see Figure 1). Table 1 shows the characteristics of the studies included in the systematic review. Two studies were published before 2010 (45, 46). Twenty-five studies were mainly from participants in Malaysia’s capital city (Kuala Lumpur and its surrounding areas). Four studies were excluded as they only presented data on specific patients (47–50) and did not include healthy controls. One study on indigenous people (51) was excluded because their lifestyles differed significantly from the rest of the population. Two studies were excluded from the meta-analysis because it has part of the same individuals from a previous research (52, 53). The summary the of study quality assessment is presented in Supplementary material 2. The included studies measured 25(OH)D levels using immunoassays, except for four studies that used chromatographic methods (54–57).
Meta-analyses
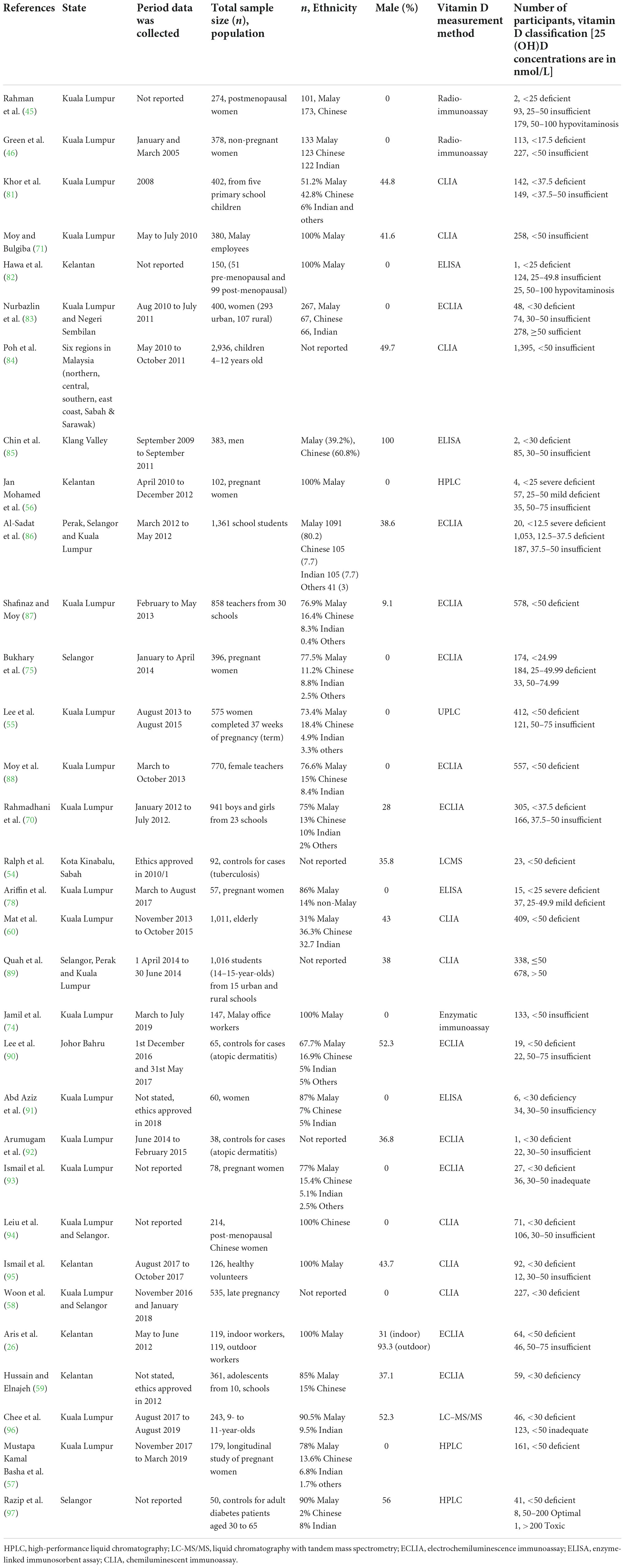
For the <30 nmol/L cut-off, ten studies with a total of 2,438 participants were included. The pooled proportion for this cut-off was 21% (95% CI 9–36%, see Figure 2). Pregnant women had a higher proportion of participants with 25(OH)D levels <30 nmol/L (n = 613, 40%).
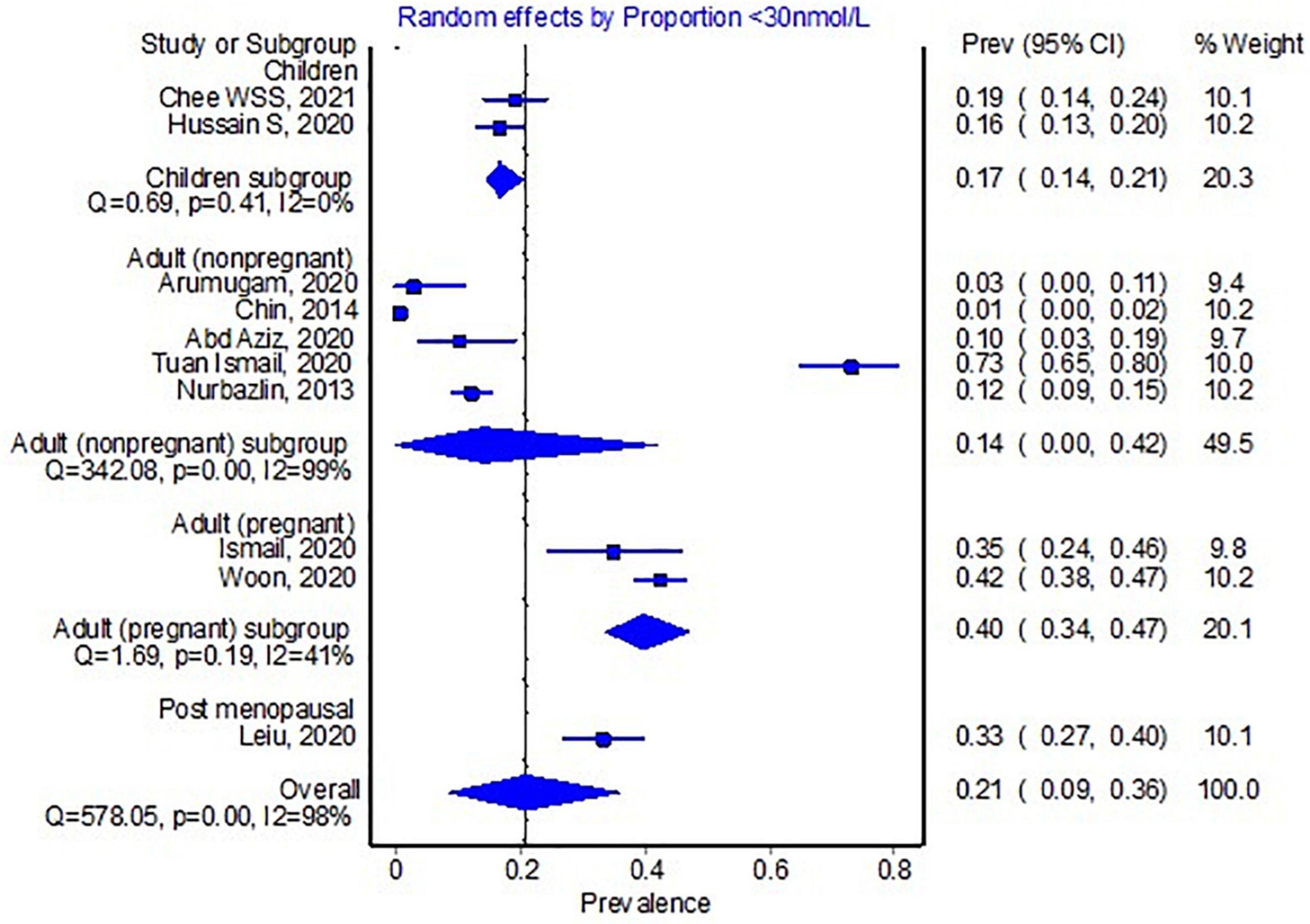
All studies eligible for the meta-analysis, except for two studies (58, 59), had a <50 nmol/L cut-off. The pooled proportion for <50 nmol/L from three studies with data from 13,977 individuals was 64.5% (95% CI 56.1–72.5, see Figure 3). Again, pregnant women represent the highest proportion with vitamin D levels of <50 nmol/L. The pooled proportion for each subgroup of participants was above 50% except for one study (60). Mat et al. (60) conducted a study on adults above 55 years old, and 203 out of the 1,011 participants were taking vitamin D supplements, which could explain the lower proportion of individuals with levels <50 nmol/L.
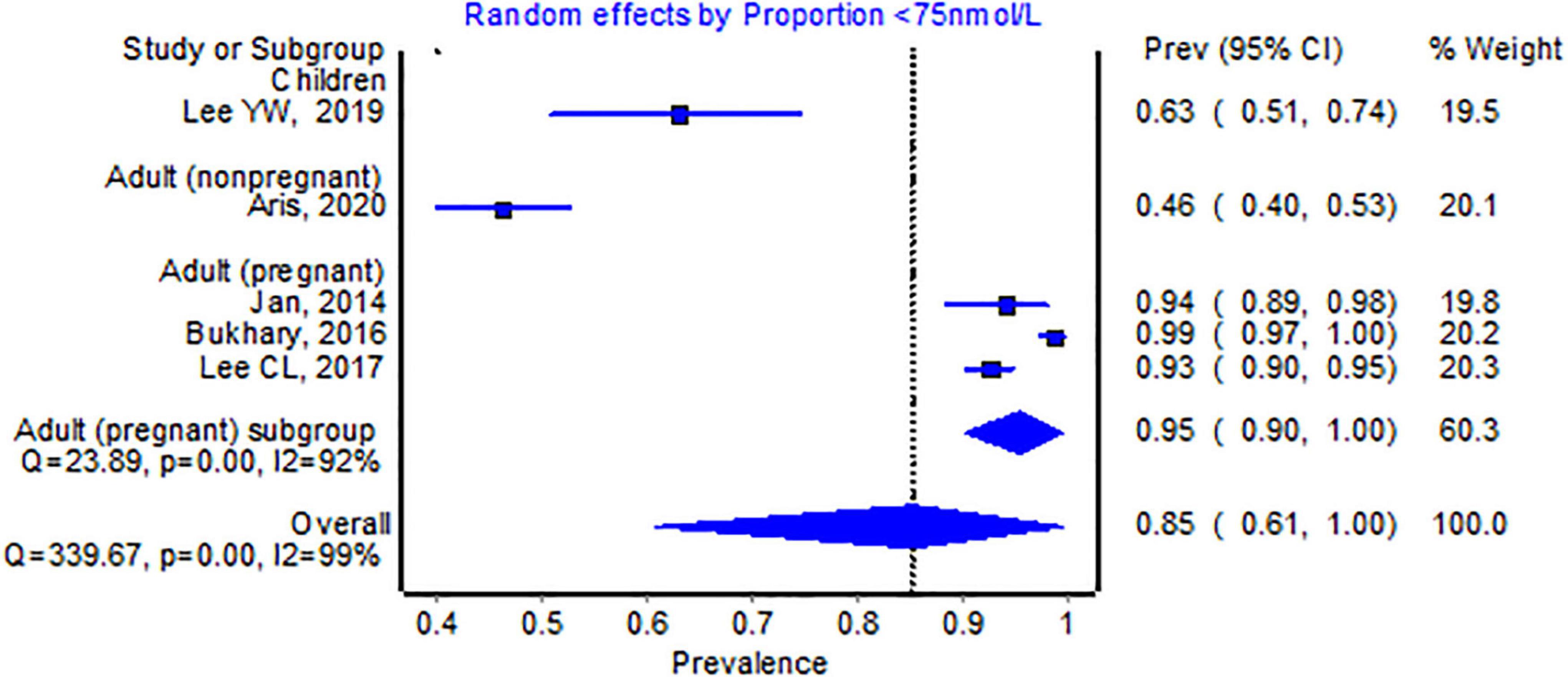
Only five studies with 1,376 participants reported a cut-off of <75 nmol/L, and the pooled proportion was 85% (95% CI 61–100, see Figure 4). All pooled proportions, including most subgroups, were considered high, indicating substantial heterogeneity (>99%).
The pooled mean (95% CI) according to the location of the study is reported in Figure 5. Not surprisingly, the urban population had a higher proportion of vitamin D insufficiency (66.8%, 95% CI 57.8–75.3, n = 10,893) compared to the rural population (45.6%, 95% CI 21–71.1, n = 3,487), respectively (see Supplementary materials 3, 4). Chua et al. (51) conducted a study on the indigenous population, considered a significant outlier and thus excluded from the meta-analysis. However, Chua et al. reported that only 1.4% (out of 555 indigenous people) had 25(OH)D levels <50 nmol/L, and 26.3% had levels <75 nmol/L.
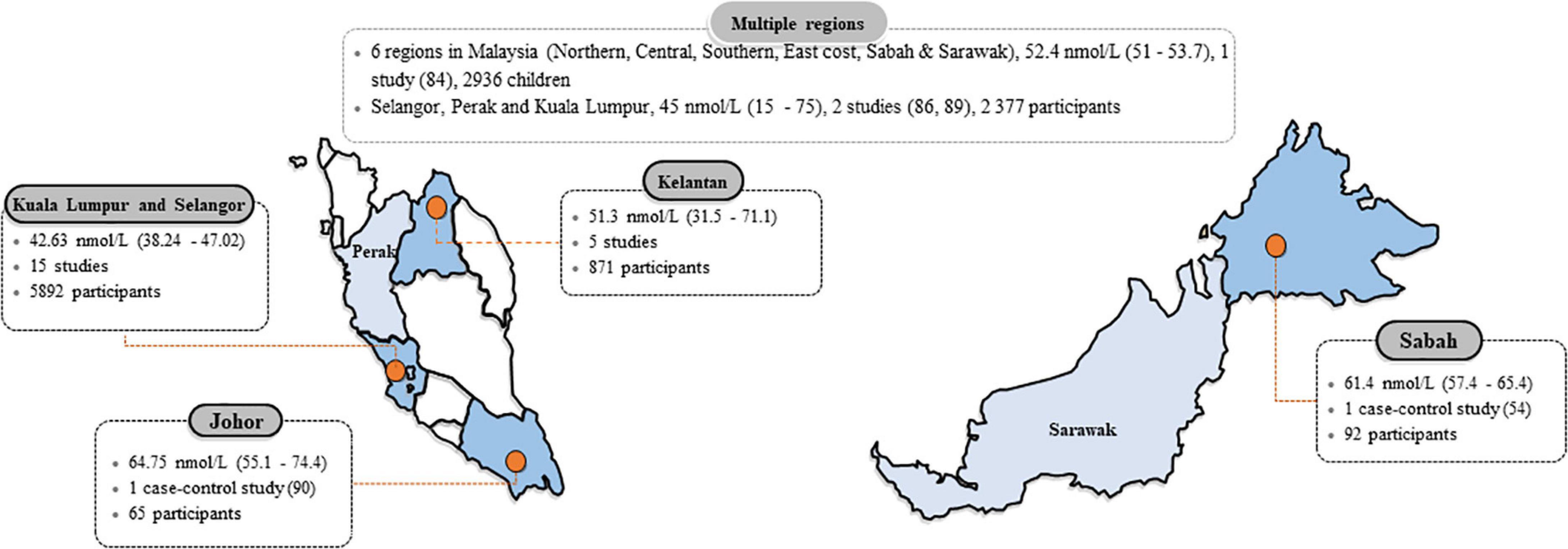
Figure 5. Mean 25-hydroxyvitamin D [25(OH)D] concentrations in Malaysia according to states. Data are the mean (95% confidence interval) of 25(OH)D concentrations reported in studies done in each state. The 25(OH)D mean values were pooled if there were more than one study from a form and were computed only from studies that stated the mean (SD), or median and interquartile range or range.
Vitamin D insufficiency is also more common in females (76%, 95% CI 65–86, n = 6,264, see Supplementary material 5) compared to males (46%, 95% CI 25.6–67%, n = 3,664, see Supplementary material 6). In terms of ethnicity, Malays (77%, 95% CI 65–87; n = 4,928, see Supplementary material 7) and Indians (77%, 95% CI 57–92; n = 768, see Supplementary material 8) had higher proportions of vitamin D insufficiency than the Chinese population (34.5%, 95%CI 17–54; n = 1,353, Supplementary material 9). One study examined the relationship between monsoon seasonality and vitamin D status and found no significant association (26).
Discussion
This study found that vitamin D deficiency and insufficiency, as defined by three cut-offs, is common in Malaysia. Precisely, over half of the population is estimated to have 25(OH)D levels <50 nmol/L (see Figure 3). Only two studies (45, 46) were conducted prior to 2010, and the majority were studies within the past 5 years, indicating that the data would reflect the current situation. However, all of the studies reported data collected before the COVID-19 pandemic. COVID-19 pandemic-related confinement has been shown to worsen vitamin D status in several studies outside of Malaysia (61, 62), however it is unclear if the same impact will be observed in Malaysia. We found that individuals living in the urban areas have higher prevalence of vitamin D insufficiency compared to rural areas. This is not surprising considering individuals living in rural areas tend to spend more time outdoor and hence receive higher doses of UVB radiation compared to individuals living in urban areas. Vitamin D deficiency was still detected in the indigenous population, whose lifestyle would involve more outdoor activities and sun exposure. However, the proportion is much lower than the general Malaysian population (51). It should be noted that there was substantial heterogeneity between the studies, which could partly be explained by age group, living in urban areas, gender, and ethnicity. Pregnant women had a much higher risk of vitamin D deficiency than all other age groups for all cut-offs. A longitudinal study followed 179 pregnant women from early pregnancy to birth found that at early pregnancy, 89% had levels <50 nmol/L, and this rose to 96.1% at birth (57). Although 11.1% took vitamin D supplements, none of the women had sufficient vitamin D status at birth.
Our study indicates that vitamin D deficiency/insufficiency in Malaysia can be considered very high compared to other regions worldwide. Table 2 is adapted and updated from a commentary on reviews or systematic reviews of vitamin D status for a country or continent by Bouillon (24). Vitamin D levels < 30 nmol/L in Malaysia are approximately equal to the African continent, but the proportion of levels <50 nmol/L is much higher. However, the prevalence for both cut-offs is comparable to estimates from Mainland China (36). It is also interesting to note that Malaysian Chinese have a much lower proportion of vitamin D insufficiency (35%, <50 nmol/L) compared to Chinese from Mainland China. We are unaware of any studies exploring the difference between Chinese in different international geographical regions and their vitamin D status.
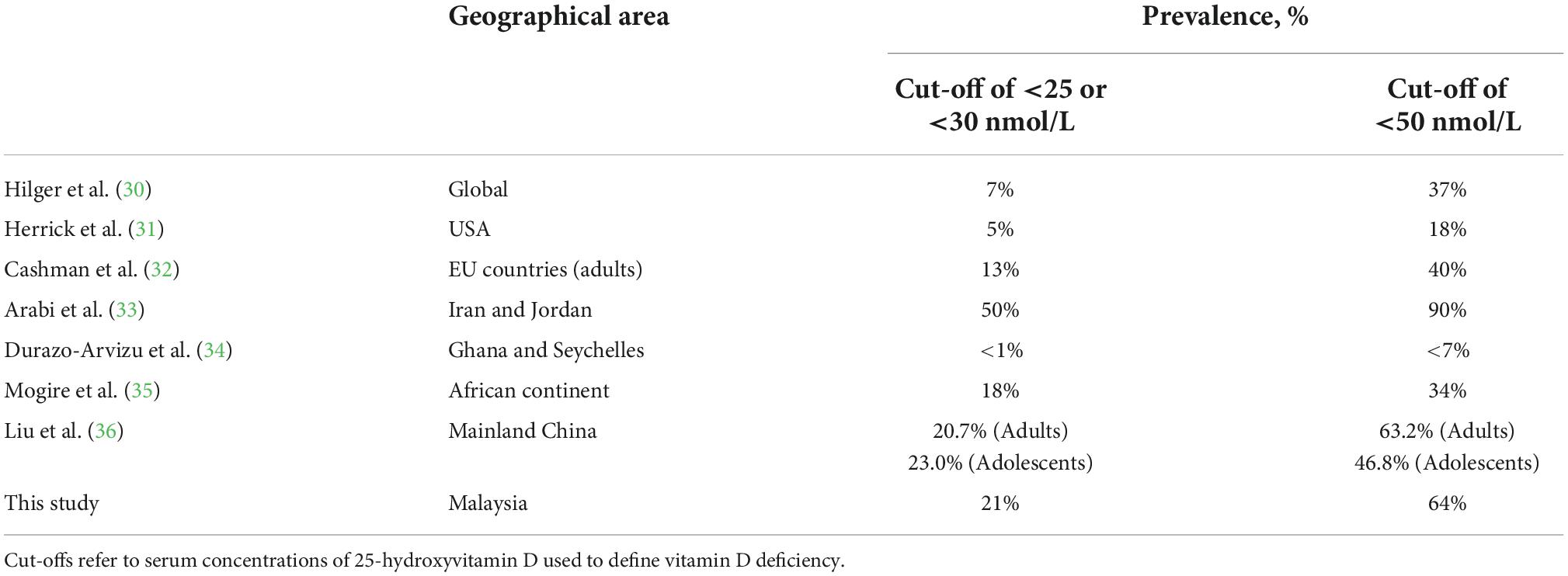
Table 2. Vitamin D deficiency by geographical area and 25-hydroxyvitamin D cut-offs, updated from Bouillon (24).
The prevalence of vitamin D deficiency could be associated to the prevalence of several non-communicable diseases in Malaysia. It has been shown that obese individuals have lower vitamin D levels compared to non-obese subjects (63) due to the reduced bioavailability of the fat-soluble vitamin D (64). According to Malaysia’s National Health and Morbidity Survey 2019, approximately half of Malaysians were above the ideal body weight, with 30.4% overweight and 19.7% obese (65). Vitamin D deficiency has also been linked to the onset of insulin resistance and diabetes mellitus (66). The prevalence of diabetes mellitus in Malaysia is increasing at an alarming rate, with the overall prevalence exceeding 18% in 2019 (67). In addition, the prevalence of raised blood glucose in individuals with unknown diabetes is even higher at 43.4% (95% CI 37.37–49.65) among people aged 65–69 years, which can be attributed to a high intake of sugary beverages (65). In mechanistic animal studies, chronic consumption of high fructose diets can reduce circulating 1,25-(OH)2D3 (68, 69). In this study, only two articles explored the association between vitamin D status and obesity in our study, but the results were conflicting (70, 71). This prompts for more studies exploring the association of vitamin D and metabolic syndrome in Malaysia.
Dietary vitamin D can be obtained by consuming food that naturally contains vitamin D, fortified food, or supplements. However, limited food choices naturally contain vitamin D in the Malaysian diet (72). Furthermore, vitamin D fortification in Malaysia is voluntary by the manufacturers, with only a few fortifying milks for children and adults (72). The Malaysian Adult Nutrition survey reported that the highest consumer of full cream milk is amongst adults aged 50–59, with only 24% reported daily consumption, while only 15% of individuals aged 18 and 19 reported daily consumption (73). In this meta-analysis, only approximately 10–20% of the participants take vitamin D supplements (57, 60, 74, 75), although the frequency and dosage of supplementation are unclear.
Without significant dietary sources, Malaysians are left to sunlight exposure to achieve adequate vitamin D levels. However, there are numerous reasons why Malaysians tend to avoid sun exposure. Some of the barriers to sun exposure identified amongst Malay women with low vitamin D status include misunderstanding about vitamin D, health concerns toward sun exposure, including effects on skin color and surface, weather (hot and rainy), and religious/cultural clothing practices (76). Additionally, there are limited studies investigating vitamin D synthesis following sun exposure in Malaysia (77). Due to the scarcity of studies, it is unclear exactly how long and how much skin surface is required to be exposed to the sun to obtain adequate vitamin D levels in Malaysia. Different ethnicities further complicate recommendations with different skin tones and different cultural/religious clothing. Hence, more research on sun exposure in Malaysia to meet adequate vitamin D levels is required to provide more explicit guidelines.
There are several notable limitations in this study. Most studies do not report vitamin D supplementation, although some include this information (78). However, vitamin D supplementation is not a common practice among the Malaysian population, and therefore it is unlikely to affect our results significantly. Secondly, 25(OH)D levels were measured using different chromatographic and immunoassays. This is a common issue when comparing studies that involve measurements of vitamin D plasma levels as there is no worldwide standardization (79, 80). Nevertheless, in Mogire’s (35) study, different vitamin D assays accounted for only 5% of the heterogeneity and had no significant impact on the overall 25(OH)D mean concentrations estimate. Thirdly, most of the studies included in the meta-analysis used convenient sampling, which is prone to bias. Finally, although we tried to be inclusive by having a broad inclusion and minimal exclusion criteria, there were limited data for many states in Malaysia.
Conclusion
Malaysia has a high prevalence of vitamin D deficiency and insufficiency, with more than half of the population estimated to have levels <50 nmol/L. Vitamin D deficiency is more prevalent in Malay and Malaysian Indian ethnic groups than in Malaysian Chinese. The female gender has lower vitamin D levels compared to the male. We strongly recommend immediate public health measures such as the refinement of nutritional guidelines, development of government policies, and awareness campaigns to improve vitamin D status in Malaysia.
Data availability statement
The requests to access the datasets analysed in this study should be directed to SM, c2hhbWluQHVrbS5lZHUubXk=.
Author contributions
SM, NJ, and NM conducted the literature search. EH, NJ, and SM critically appraised the included studies. SM performed the data analysis and EH and NJ checked it. SM wrote the first draft of the manuscript. All authors contributed to the study’s conception and design and data extraction, commented on previous versions of the manuscript, read, and approved the final manuscript.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fnut.2022.1050745/full#supplementary-material
References
1. Prietl B, Treiber G, Pieber TR, Amrein K. Vitamin D and immune function. Nutrients. (2013) 5:2502–21. doi: 10.3390/nu5072502
2. Shah Alam M, Czajkowsky DM, Aminul Islam M, Ataur Rahman M. The role of vitamin D in reducing Sars-Cov-2 infection: an update. Int Immunopharmacol. (2021) 97:107686. doi: 10.1016/j.intimp.2021.107686
3. Petrelli F, Luciani A, Perego G, Dognini G, Colombelli PL, Ghidini A. Therapeutic and prognostic role of vitamin D for covid-19 infection: a systematic review and meta-analysis of 43 observational studies. J Steroid Biochem Mol Biol. (2021) 211:105883. doi: 10.1016/j.jsbmb.2021.105883
4. Wang Z, Joshi A, Leopold K, Jackson S, Christensen S, Nayfeh T, et al. Association of vitamin D deficiency with covid-19 infection severity: systematic review and meta-analysis. Clin Endocrinol. (2021) 96:281–7. doi: 10.1111/cen.14540
5. Teshome A, Adane A, Girma B, Mekonnen ZA. The impact of vitamin D level on covid-19 infection: systematic review and meta-analysis. Front Public Health. (2021) 9:624559. doi: 10.3389/fpubh.2021.624559
6. Shah K, Saxena D, Mavalankar D. Vitamin D supplementation, covid-19 and disease severity: a meta-analysis. QJM. (2021) 114:175–81. doi: 10.1093/qjmed/hcab009
7. Rawat D, Roy A, Maitra S, Shankar V, Khanna P, Baidya DK. Vitamin D supplementation and covid-19 treatment: a systematic review and meta-analysis. Diabetes Metab Syndr. (2021) 15:102189. doi: 10.1016/j.dsx.2021.102189
8. Pal R, Banerjee M, Bhadada SK, Shetty AJ, Singh B, Vyas A. Vitamin D supplementation and clinical outcomes in covid-19: a systematic review and meta-analysis. J Endocrinol Invest. (2021) 45:53–68. doi: 10.1007/s40618-021-01614-4
9. Jayawardena R, Jeyakumar DT, Francis TV, Misra A. Impact of the vitamin D deficiency on covid-19 infection and mortality in Asian countries. Diabetes Metab Syndr. (2021) 15:757–64. doi: 10.1016/j.dsx.2021.03.006
10. Bassatne A, Basbous M, Chakhtoura M, El Zein O, Rahme M, El-Hajj Fuleihan G. the link between covid-19 and vitamin D (Vivid): a systematic review and meta-analysis. Metabolism. (2021) 119:154753. doi: 10.1016/j.metabol.2021.154753
11. Pereira M, Dantas Damascena A, Galvão Azevedo LM, de Almeida Oliveira T, da Mota Santana J Vitamin D deficiency aggravates COVID-19: systematic review and meta-analysis. Crit Rev Food Sci Nutr. (2022) 62:1308–16. doi: 10.1080/10408398.2020.1841090
12. Annweiler G, Corvaisier M, Gautier J, Dubée V, Legrand E, Sacco G, et al. Vitamin D supplementation associated to better survival in hospitalized frail elderly covid-19 patients: the geria-covid quasi-experimental study. Nutrients. (2020) 12:3377. doi: 10.3390/nu12113377
13. Rastogi A, Bhansali A, Khare N, Suri V, Yaddanapudi N, Sachdeva N, et al. Short term, high-dose vitamin D supplementation for covid-19 disease: a randomised, placebo-controlled, study (shade study). Postgrad Med J. (2020) 98:87–90. doi: 10.1136/postgradmedj-2020-139065
14. Annweiler C, Hanotte B, Grandin de l’Eprevier C, Sabatier JM, Lafaie L, Célarier T. Vitamin D and survival in covid-19 patients: a quasi-experimental study. J Steroid Biochem Mol Biol. (2020) 204:105771. doi: 10.1016/j.jsbmb.2020.105771
15. Entrenas Castillo M, Entrenas Costa LM, Vaquero Barrios JM, Alcalá Díaz JF, López Miranda J, Bouillon R, et al. “Effect of calcifediol treatment and best available therapy versus best available therapy on intensive care unit admission and mortality among patients hospitalized for covid-19: a pilot randomized clinical study”. J Steroid Biochem Mol Biol. (2020) 203:105751. doi: 10.1016/j.jsbmb.2020.105751
16. Smolders J, van den Ouweland J, Geven C, Pickkers P, Kox M. Letter to the editor: vitamin D deficiency in covid-19: mixing up cause and consequence. Metabolism. (2021) 115:154434. doi: 10.1016/j.metabol.2020.154434
17. Murai IH, Fernandes AL, Sales LP, Pinto AJ, Goessler KF, Duran CSC, et al. Effect of a single high dose of vitamin D3 on hospital length of stay in patients with moderate to severe covid-19: a randomized clinical trial. JAMA. (2021) 325:1053–60. doi: 10.1001/jama.2020.26848
18. Leaf DE, Ginde AA. Vitamin D3 to treat covid-19: different disease, same answer. JAMA. (2021) 325:1047–8. doi: 10.1001/jama.2020.26850
19. Rubin R. Sorting out whether vitamin D deficiency raises covid-19 risk. JAMA. (2021) 325:329–30. doi: 10.1001/jama.2020.24127
20. Bouillon R. Comparative analysis of nutritional guidelines for vitamin D. Nat Rev Endocrinol. (2017) 13:466–79. doi: 10.1038/nrendo.2017.31
21. Holick MF, Binkley NC, Bischoff-Ferrari HA, Gordon CM, Hanley DA, Heaney RP, et al. Evaluation, treatment, and prevention of vitamin D deficiency: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. (2011) 96:1911–30. doi: 10.1210/jc.2011-0385
22. Institute of Medicine Committee to Review Dietary Reference Intakes for Vitamin D, Calcium. The National Academies Collection: Reports Funded by National Institutes of Health. In: Ross AC, Taylor CL, Yaktine AL, Del Valle HB editors. Dietary Reference Intakes for Calcium and Vitamin D. Washington (DC): National Academies Press (US) Copyright © 2011, National Academy of Sciences (2011).
23. Misra M, Pacaud D, Petryk A, Collett-Solberg PF, Kappy M. Vitamin D deficiency in children and its management: review of current knowledge and recommendations. Pediatrics. (2008) 122:398–417. doi: 10.1542/peds.2007-1894
24. Bouillon R. Vitamin D status in Africa is worse than in other continents. Lancet Glob Health. (2020) 8:e20–1. doi: 10.1016/s2214-109x(19)30492-9
25. Kwan MS, Tangang FT, Juneng L. Projected changes of future climate extremes in Malaysia. Sains Malaysiana. (2013) 42:1051–9.
26. Aris N, Mitra AK, Wan Mohamed WMI, Wan Muda WAM, Jan Mohamed HJ. Effects of occupational sunlight exposure and monsoon season on vitamin D concentration among outdoor and indoor workers in Malaysia. Malaysian J Nutr. (2020) 26:425–39. doi: 10.31246/mjn-2020-0038
27. Department of Statistics Malaysia Official Portal,. Demographic Statistics Second Quarter 2021. (2022). Available online at: https://www.dosm.gov.my/v1/index.php?r=column/cthemeByCat&cat=430&bul_id=eGtwdjd4amZJb1JmcFFkYXBKNHg3dz09&menu_id=L0pheU43NWJwRWVSZklWdzQ4TlhUUT09 (accessed November 9, 2022).
28. Isa ZM, Shamsuddin K, Bukhari NBI, Lin KG, Mahdy ZA, Hassan H, et al. The reliability of fitzpatrick skin type chart comparing to mexameter (Mx 18) in measuring skin color among first trimester pregnant mothers in Petaling District, Malaysia. Malaysian J Public Health Med. (2016) 3:59–65.
29. Md Isa Z, Mohd Nordin NR, Mahmud MH, Hashim S. An update on vitamin D deficiency status in malaysia. Nutrients. (2022) 14:567. doi: 10.3390/nu14030567
30. Hilger J, Friedel A, Herr R, Rausch T, Roos F, Wahl DA, et al. A systematic review of vitamin D status in populations worldwide. Br J Nutr. (2014) 111:23–45. doi: 10.1017/S0007114513001840
31. Herrick KA, Storandt RJ, Afful J, Pfeiffer CM, Schleicher RL, Gahche JJ, et al. Vitamin D status in the United States, 2011-2014. Am J Clin Nutr. (2019) 110:150–7. doi: 10.1093/ajcn/nqz037
32. Cashman KD, Dowling KG, Škrabáková Z, Gonzalez-Gross M, Valtueña J, De Henauw S, et al. Vitamin D deficiency in Europe: pandemic? Am J Clin Nutr. (2016) 103:1033–44. doi: 10.3945/ajcn.115.120873
33. Arabi A, El Rassi R, El-Hajj Fuleihan G. Hypovitaminosis D in developing countries-prevalence, risk factors and outcomes. Nat Rev Endocrinol. (2010) 6:550–61. doi: 10.1038/nrendo.2010.146
34. Durazo-Arvizu RA, Camacho P, Bovet P, Forrester T, Lambert EV, Plange-Rhule J, et al. 25-hydroxyvitamin D in African-origin populations at varying latitudes challenges the construct of a physiologic norm. Am J Clin Nutr. (2014) 100:908–14. doi: 10.3945/ajcn.113.066605
35. Mogire RM, Mutua A, Kimita W, Kamau A, Bejon P, Pettifor JM, et al. Prevalence of vitamin D deficiency in Africa: a systematic review and meta-analysis. Lancet Glob Health. (2020) 8:e134–42. doi: 10.1016/s2214-109x(19)30457-7
36. Liu W, Hu J, Fang Y, Wang P, Lu Y, Shen N. Vitamin D status in Mainland of China: a systematic review and meta-analysis. EClinicalMedicine. (2021) 38:101017. doi: 10.1016/j.eclinm.2021.101017
37. Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, et al. The prisma statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol. (2009) 62:e1–34. doi: 10.1016/j.jclinepi.2009.06.006
38. Migliavaca CB, Stein C, Colpani V, Munn Z, Falavigna M. Quality assessment of prevalence studies: a systematic review. J Clin Epidemiol. (2020) 127:59–68. doi: 10.1016/j.jclinepi.2020.06.039
39. Munn Z, Moola S, Riitano D, Lisy K. The development of a critical appraisal tool for use in systematic reviews addressing questions of prevalence. Int J Health Policy Manag. (2014) 3:123–8.
40. Munn Z, Moola S, Lisy K, Riitano D, Tufanaru C. Methodological guidance for systematic reviews of observational epidemiological studies reporting prevalence and cumulative incidence data. Int J Evid Based Healthc. (2015) 13:147–53.
41. Barendregt JJ, Doi SA, Lee YY, Norman RE, Vos T. Meta-analysis of prevalence. J Epidemiol Commun Health. (2013) 67:974–8. doi: 10.1136/jech-2013-203104
42. Wan X, Wang W, Liu J, Tong T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol. (2014) 14:135. doi: 10.1186/1471-2288-14-135
43. Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. (2003) 327:557–60. doi: 10.1136/bmj.327.7414.557
44. Hunter JP, Saratzis A, Sutton AJ, Boucher RH, Sayers RD, Bown MJ. In meta-analyses of proportion studies, funnel plots were found to be an inaccurate method of assessing publication bias. J Clin Epidemiol. (2014) 67:897–903. doi: 10.1016/j.jclinepi.2014.03.003
45. Rahman SA, Chee WS, Yassin Z, Chan SP. Vitamin D status among postmenopausal Malaysian women. Asia Pac J Clin Nutr. (2004) 13:255–60.
46. Green TJ, Skeaff CM, Rockell JE, Venn BJ, Lambert A, Todd J, et al. Vitamin D status and its association with parathyroid hormone concentrations in women of child-bearing age living in Jakarta and Kuala Lumpur. Eur J Clin Nutr. (2008) 62:373–8. doi: 10.1038/sj.ejcn.1602696
47. Fong CY, Kong AN, Poh BK, Mohamed AR, Khoo TB, Ng RL, et al. Vitamin D deficiency and its risk factors in malaysian children with epilepsy. Epilepsia. (2016) 57:1271–9. doi: 10.1111/epi.13443
48. Kong AN, Fong CY, Ng CC, Mohamed AR, Khoo TB, Ng RL, et al. Association of common genetic variants with vitamin D status in Malaysian children with epilepsy. Seizure. (2020) 79:103–11. doi: 10.1016/j.seizure.2020.05.009
49. Lee WS, Jalaludin MY, Wong SY, Ong SY, Foo HW, Ng RT. Vitamin D non-sufficiency is prevalent in children with chronic liver disease in a tropical country. Pediatr Neonatol. (2019) 60:12–8. doi: 10.1016/j.pedneo.2018.03.011
50. Fong CY, Ong FN, Ong LC, Khoo TB, Lee ML. Vitamin D deficiency and insufficiency in malaysian children with spina bifida. Spinal Cord. (2020) 58:1030–6. doi: 10.1038/s41393-020-0441-7
51. Chua EY, Mohd Shariff Z, Sulaiman N, Appannah G, Yong HY. Associations of serum 25-hydroxyvitamin D with adiposity and at-risk lipid profile differ for indigenous (orang asli) male and female adults of Peninsular Malaysia. Int J Environ Res Public Health. (2020) 17:2855. doi: 10.3390/ijerph17082855
52. Moy FM. Vitamin D status and its associated factors of free living malay adults in a tropical country, Malaysia. J Photochem Photobiol B. (2011) 104:444–8. doi: 10.1016/j.jphotobiol.2011.05.002
53. Poh BK, Rojroongwasinkul N, Nguyen BK, Sandjaja, Ruzita AT, Yamborisut U, et al. 25-hydroxy-vitamin d demography and the risk of vitamin D insufficiency in the South East Asian nutrition surveys (seanuts). Asia Pac J Clin Nutr. (2016) 25:538–48. doi: 10.6133/apjcn.092015.02
54. Ralph AP, Rashid Ali MRS, William T, Piera K, Parameswaran U, Bird E, et al. Vitamin D and activated vitamin D in tuberculosis in equatorial Malaysia: a prospective clinical study. BMC Infect Dis. (2017) 17:312. doi: 10.1186/s12879-017-2314-z
55. Lee CL, Ng BK, Wu LL, Cheah FC, Othman H, Ismail NAM. Vitamin D deficiency in pregnancy at term: risk factors and pregnancy outcomes. Horm Mol Biol Clin Investig. (2017) 31:1–8. doi: 10.1515/hmbci-2017-0005
56. Jan Mohamed HJ, Rowan A, Fong B, Loy SL. Maternal serum and breast milk vitamin D levels: findings from the universiti sains malaysia pregnancy cohort study. PLoS One. (2014) 9:e100705. doi: 10.1371/journal.pone.0100705
57. Mustapa Kamal Basha MA, Abdul Majid H, Razali N, Abd Rashed A, Muhammad H, Yahya A. Longitudinal vitamin D deficiency among malaysian pregnant women and its correlation with neonatal serum 25-hydroxyvitamin D levels. Front Public Health. (2021) 9:654292. doi: 10.3389/fpubh.2021.654292
58. Woon FC, Chin YS, Ismail IH, Abdul Latiff AH, Batterham M, Chan YM, et al. Maternal vitamin D levels during late pregnancy and risk of allergic diseases and sensitization during the first year of life-a birth cohort study. Nutrients. (2020) 12:2418. doi: 10.3390/nu12082418
59. Hussain S, Elnajeh M. Prevalence and risk factors for hypovitaminosis D among healthy adolescents in Kota Bharu, Kelantan. J ASEAN Fed Endocr Soc. (2020) 35:176–80. doi: 10.15605/jafes.035.02.05
60. Mat S, Jaafar MH, Sockalingam S, Raja J, Kamaruzzaman SB, Chin AV, et al. Vitamin D deficiency is associated with ethnicity and knee pain in a multi-ethnic South-East Asian nation: results from malaysian elders longitudinal research (Melor). Int J Rheum Dis. (2018) 21:930–6. doi: 10.1111/1756-185x.13279
61. Yu L, Ke HJ, Che D, Luo SL, Guo Y, Wu JL. Effect of pandemic-related confinement on vitamin D status among children aged 0-6 years in Guangzhou, China: a cross-sectional study. Risk Manag Healthc Policy. (2020) 13:2669–75. doi: 10.2147/RMHP.S282495
62. Dhatt SS, Kumar V, Neradi D, Sodavarapu P, Meetei TT, Goni V. Need for testing and supplementation of vitamin D3 after release of covid-19 lockdown in patients with increased musculoskeletal pain. Indian J Orthop. (2021) 55:1046–9. doi: 10.1007/s43465-021-00376-8
63. Pereira-Santos M, Costa PR, Assis AM, Santos CA, Santos DB. Obesity and vitamin D deficiency: a systematic review and meta-analysis. Obes Rev. (2015) 16:341–9. doi: 10.1111/obr.12239
64. Wortsman J, Matsuoka LY, Chen TC, Lu Z, Holick MF. Decreased bioavailability of vitamin D in obesity. Am J Clin Nutr. (2000) 72:690–3. doi: 10.1093/ajcn/72.3.690
65. Institute for Public Health (IPH), National Institutes of Health, Ministry of Health Malaysia. National Health & Morbidity Survey (NHMS 2019) Technical Report 2019 Volume I: NCDs – Non-Communicable Diseases: Risk Factors and Other Health Problems. (2020). Available online at: https://iku.moh.gov.my/images/IKU/Document/REPORT/NHMS2019/Report_NHMS2019-NCD_v2.pdf (accessed November 9, 2022).
66. Berridge MJ. Vitamin D deficiency and diabetes. Biochem J. (2017) 474:1321–32. doi: 10.1042/bcj20170042
67. Ministry of Health Malaysia. National Diabetes Registry Report 2013 – 2019. Putrajaya: Ministryof Health Malaysia (2020).
68. Douard V, Patel C, Lee J, Tharabenjasin P, Williams E, Fritton JC, et al. Chronic high fructose intake reduces serum 1,25 (oh)2d3 levels in calcium-sufficient rodents. PLoS One. (2014) 9:e93611. doi: 10.1371/journal.pone.0093611
69. Douard V, Sabbagh Y, Lee J, Patel C, Kemp FW, Bogden JD, et al. Excessive fructose intake causes 1,25-(oh)d-dependent inhibition of intestinal and renal calcium transport in growing rats. Am J Physiol Endocrinol Metab. (2013) 304:E1303–13. doi: 10.1152/ajpendo.00582.2012
70. Rahmadhani R, Zaharan NL, Mohamed Z, Moy FM, Jalaludin MY. The associations between Vdr Bsmi polymorphisms and risk of vitamin D deficiency, obesity and insulin resistance in adolescents residing in a tropical country. PLoS One. (2017) 12:e0178695. doi: 10.1371/journal.pone.0178695
71. Moy F-M, Bulgiba A. High prevalence of vitamin D insufficiency and its association with obesity and metabolic syndrome among malay adults in Kuala Lumpur, Malaysia. BMC Public Health. (2011) 11:735. doi: 10.1186/1471-2458-11-735
72. National Coordinating Committee on Food and Nutrition Ministry of Health Malaysia. Recommended Nutrient Intakes for Malaysia 2017, a Report of the Technical Working Group onNutritional Guidelines. Putrajaya: National Coordinating Committee on Food and Nutrition Ministryof Health Malaysia (2017).
73. Norimah AK Jr, Safiah M, Jamal K, Haslinda S, Zuhaida H, Rohida S, et al. Food consumption patterns: findings from the Malaysian adult nutrition survey (Mans). Malays J Nutr. (2008) 14:25–39.
74. Jamil NA, Shahudin NN, Abdul Aziz NS, Jia Qi C, Wan Aminuddin WAA, Mat Ludin AF, et al. Knowledge, attitude and practice related to vitamin D and its relationship with vitamin D status among malay female office workers. Int J Environ Res Public Health. (2019) 16:4735. doi: 10.3390/ijerph16234735
75. Bukhary NBI, Isa ZM, Shamsuddin K, Lin KG, Mahdy ZA, Hassan H, et al. Risk factors for antenatal hypovitaminosis D in an Urban District in Malaysia. BMC Pregnancy Childbirth. (2016) 16:156. doi: 10.1186/s12884-016-0939-3
76. Shahudin NN, Sameeha MJ, Mat Ludin AF, Manaf ZA, Chin KY, Jamil NA. Barriers towards sun exposure and strategies to overcome these barriers in female indoor workers with insufficient vitamin D: a qualitative approach. Nutrients. (2020) 12:2994. doi: 10.3390/nu12102994
77. Jamil NA, Yew MH, Noor Hafizah Y, Gray SR, Poh BK, Macdonald HM. Estimated vitamin D synthesis and dietary vitamin D intake among Asians in two distinct geographical locations (Kuala Lumpur, 3 Degrees N V. Aberdeen, 57 Degrees N) and climates. Public Health Nutr. (2018) 21:3118–24. doi: 10.1017/S1368980018002057
78. Ariffin MASM, Fazil FN, Yassin NM, Junaida NS, Gan PV, Rahman RA, et al. Prevalence of vitamin D deficiency and its associated risk factors during early pregnancy in a tropical country: a pilot study. J Clin Diagnos Res. (2018) 12:19–22. doi: 10.7860/jcdr/2018/36585.12104
79. Rajaretnam A, Abdalqader M, Ghazi H, Hasan DT, Fuad M. Knowledge regarding vitamin D among private university students in Malaysia. Ann Nutr Disord Ther. (2014) 1:1008.
80. Altieri B, Cavalier E, Bhattoa HP, Perez-Lopez FR, Lopez-Baena MT, Perez-Roncero GR, et al. Vitamin D testing: advantages and limits of the current assays. Eur J Clin Nutr. (2020) 74:231–47. doi: 10.1038/s41430-019-0553-3
81. Khor GL, Chee WS, Shariff ZM, Poh BK, Arumugam M, Rahman JA, et al. High prevalence of vitamin D insufficiency and its association with Bmi-for-Age among primary school children in Kuala Lumpur, Malaysia. BMC Public Health. (2011) 11:95. doi: 10.1186/1471-2458-11-95
82. Hawa M, Sakinah H, Hermizi H. Calcium and vitamin D status of kelantanese malay women from low income family: a population-based study. J Aging Res Clin Prac. (2013) 2:191–6.
83. Nurbazlin M, Chee WS, Rokiah P, Tan AT, Chew YY, Nusaibah AR, et al. Effects of sun exposure on 25(oh) vitamin D concentration in urban and rural women in Malaysia. Asia Pac J Clin Nutr. (2013) 22:391–9. doi: 10.6133/apjcn.2013.22.3.15
84. Poh BK, Ng BK, Siti Haslinda MD, Nik Shanita S, Wong JE, Budin SB, et al. Nutritional status and dietary intakes of children aged 6 months to 12 years: findings of the nutrition survey of Malaysian children (Seanuts Malaysia). Br J Nutr. (2013) 110(Suppl 3.):S21–35. doi: 10.1017/S0007114513002092
85. Chin KY, Ima-Nirwana S, Ibrahim S, Mohamed IN, Wan Ngah WZ. Vitamin D status in Malaysian men and its associated factors. Nutrients. (2014) 6:5419–33. doi: 10.3390/nu6125419
86. Al-Sadat N, Majid HA, Sim PY, Su TT, Dahlui M, Abu Bakar MF, et al. Vitamin D deficiency in Malaysian adolescents aged 13 years: findings from the Malaysian health and adolescents longitudinal research team study (Myhearts). BMJ Open. (2016) 6:e010689. doi: 10.1136/bmjopen-2015-010689
87. Shafinaz IS, Moy FM. Vitamin D level and its association with adiposity among multi-ethnic adults in Kuala Lumpur, Malaysia: a cross sectional study. BMC Public Health. (2016) 16:232. doi: 10.1186/s12889-016-2924-1
88. Moy FM, Hoe VC, Hairi NN, Vethakkan SR, Bulgiba A. Vitamin D deficiency and depression among women from an urban community in a tropical country. Public Health Nutr. (2017) 20:1844–50. doi: 10.1017/S1368980016000811
89. Quah SW, Abdul Majid H, Al-Sadat N, Yahya A, Su TT, Jalaludin MY. Risk factors of vitamin D deficiency among 15-year-old adolescents participating in the Malaysian health and adolescents longitudinal research team study (Myhearts). PLoS One. (2018) 13:e0200736. doi: 10.1371/journal.pone.0200736
90. Lee YW, Choon SE, Izham S. Serum 25-hydroxyvitamin D deficiency in Malaysian children with severe atopic dermatitis. Med J Malaysia. (2019) 74:259–65.
91. Abd Aziz NH, Yazid NA, Abd Rahman R, Abd Rashid N, Wong SK, Mohamad NV, et al. Is first trimester maternal 25-hydroxyvitamin D level related to adverse maternal and neonatal pregnancy outcomes? A prospective cohort study among Malaysian women. Int J Environ Res Public Health. (2020) 17:3291. doi: 10.3390/ijerph17093291
92. Arumugam M, Jamil A, Nor NM, Baseri M, Thevarajah S, Mustafa N. Sun exposure, dietary vitamin D and vitamin D status in adult atopic dermatitis: a case control study. Malaysian J Med Health Sci. (2020) 16:66–9.
93. Ismail NA, Mohamed Ismail NA, Bador KM. Vitamin D in gestational diabetes mellitus and its association with hyperglycaemia, insulin sensitivity and other factors. J Obstet Gynaecol. (2020) 41:899–903. doi: 10.1080/01443615.2020.1820462
94. Leiu KH, Chin YS, Mohd Shariff Z, Arumugam M, Chan YM. High body fat percentage and low consumption of dairy products were associated with vitamin D inadequacy among older women in Malaysia. PLoS One. (2020) 15:e0228803. doi: 10.1371/journal.pone.0228803
95. Ismail TST, Wong SH, Din MH, Mustapha Z, Haron J, Zun ABB. Correlation of vitamin D with bone mineral density by dual energy x-ray absorptiometry (Dxa) scan among healthy malay adult. Malaysian J Med Health Sci. (2020) 16:16–22.
96. Chee WSS, Chang CY, Arasu K, Wong SY, Ong SH, Yang WY, et al. Vitamin D status is associated with modifiable lifestyle factors in pre-adolescent children living in Urban Kuala Lumpur, Malaysia. Nutrients. (2021) 13:2175. doi: 10.3390/nu13072175
Keywords: Malaysia, vitamin D, 25-hydroxyvitamin D, prevalence, cholecalciferol
Citation: Mohd Saffian S, Jamil NA, Mohd Tahir NA and Hatah E (2022) Vitamin D insufficiency is high in Malaysia: A systematic review and meta-analysis of studies on vitamin D status in Malaysia. Front. Nutr. 9:1050745. doi: 10.3389/fnut.2022.1050745
Received: 22 September 2022; Accepted: 03 November 2022;
Published: 18 November 2022.
Edited by:
Sumantra Ray, NNEdPro Global Centre for Nutrition and Health, United KingdomReviewed by:
Laurel M. Wentz, Appalachian State University, United StatesShanshan Wang, Huazhong University of Science and Technology, China
Copyright © 2022 Mohd Saffian, Jamil, Mohd Tahir and Hatah. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Shamin Mohd Saffian, c2hhbWluQHVrbS5lZHUubXk=
 Shamin Mohd Saffian
Shamin Mohd Saffian Nor Aini Jamil
Nor Aini Jamil Nor Asyikin Mohd Tahir
Nor Asyikin Mohd Tahir Ernieda Hatah
Ernieda Hatah