- 1Department of Decision Neuroscience and Nutrition, German Institute of Human Nutrition (DIfE), Potsdam-Rehbrücke, Germany
- 2Neuroscience Research Center, Charité - Universitätsmedizin Berlin, Corporate Member of Freie Universität Berlin, Humboldt-Universität zu Berlin and Berlin Institute of Health, Berlin, Germany
- 3Deutsches Zentrum für Diabetes, Neuherberg, Germany
The COVID-19 pandemic has increased the occurrence of conspiracy theories. It has been suggested that a greater endorsement of these theories may be associated with psychotic-like experiences (PLEs), as well as with social isolation. In this preregistered study, we investigated whether both PLEs and measures of social isolation (e.g., loneliness) can predict conspiratorial beliefs and, if so, which of these variables can mediate the association with conspiratorial beliefs. Furthermore, based on previous studies on schizophrenia, we explored whether the diet is associated with PLEs and conspiratorial beliefs. Participants (N = 142) completed online questionnaires measuring PLEs, social isolation, mental well-being, and conspiratorial beliefs. They also submitted their daily food intake for a week using a smartphone app. We found that loneliness predicted the endorsement of conspiracy theories during the COVID-19 lockdown. Strikingly, the proneness to experience subclinical psychotic symptoms played an underlying mediating role. In addition, these subclinical symptoms were associated with lower fruit, carbohydrate, and iron intakes, as well as with higher fat intake. Our results add insights into how conspiratorial beliefs can affect individuals’ mental health and relationships. Moreover, these results open the avenue for potential novel intervention strategies to optimize food intake in individuals with PLEs.
Introduction
The COVID-19 pandemic has affected almost all aspects of human societal daily life. A typical psychological reaction to a highly uncertain situation such as a pandemic is the increased occurrence of conspiracy theories (1, 2). These theories are alternative explanations of important events as the results of malevolent actions (or patterns of secret causal connections) involving small powerful groups, when other explanations are more plausible (3).
During the COVID-19 pandemic, the overload of COVID-19 related information, the lack of knowledge about the disease, and the more general climate of uncertainty have given rise to conspiracy theories (4). Believing in such theories may have several detrimental effects. For example, conspiracy theories linking the 5G cellular network with COVID-19 have led to episodes of violence against telecom workers in the U.K. (5). Further, conspiratorial beliefs increase vaccine refusals (6) and decrease compliance with preventive measures such as social distancing (5). Given their impact on individuals’ health and safety, it is essential to identify the factors associated with beliefs in conspiracy theories.
In view of these detrimental consequences, recent studies have found that a greater endorsement of conspiracy theories is associated with psychotic-like experiences (PLEs) (7, 8). More in detail, PLEs refer to subclinical psychotic events (e.g., subthreshold forms of paranoid delusions) experienced by healthy individuals in the general population in the absence of a clear psychotic disorder (9, 10). Studies on the general adult population have found that approximately 8% of individuals who reported PLEs will become clinically psychotic after 2 years (11), suggesting that PLEs may represent a risk factor for developing psychotic disorders.
Interestingly, paranoia and conspiracy theories seem to have in common an intuitive thinking style and the so called “jumping to conclusion” bias, which is the tendency to make quick decisions based mostly on a few pieces of evidence (8). Thus, PLEs may be an indicator of the latent liability for conspiratorial beliefs. Moreover, several studies have found links between psychotic disorders and environmental factors such as a poorer diet quality (e.g., lower intake of fruit and vegetable). Some evidence has particularly identified iron deficiency as one of the most important dietary risk factor for psychosis (12, 13). Indeed, iron deficiency due to a reduced iron intake may alter prefrontal dopaminergic transmission in the brain leading to negative symptoms in schizophrenia (12, 14). Since food is a modifiable risk factor, it may be possible that nutritional interventions may prevent the occurrence also of PLEs and consequently reduce the susceptibility to believe in conspiratorial theories. However, empirical evidence is lacking.
Besides PLEs, another factor that has been linked to conspiratorial beliefs is social isolation (7). In particular, contention measures during the COVID-19 pandemic such as lockdowns and social distancing have influenced the quantity and quality of social interactions and enormously increased feelings of loneliness (15). Loneliness refers to perceived social isolation and is associated with poorer mental health including stress (16) and PLEs (17). Interestingly, some studies showed that loneliness could continue even when the lockdowns ended (15) and that the development of mental health problems can further strengthen the magnitude of loneliness (18). Previous research on ostracism, a form of social exclusion, has suggested that one of its most important consequences is indeed conspiratorial thinking (19, 20). Thus, the social exclusion experienced during the COVID-19 lockdown could have led people to endorse conspiracy theories.
Based on the above-mentioned studies, conspiratorial beliefs may be associated with several interconnected factors including PLEs, social isolation, and a more general reduced mental well-being. However, not all individuals experiencing social isolation or having PLEs may believe in conspiracy theories. Yet, it is unknown which factors may interact with each other and play a role in making people more susceptible to believing in conspiracy theories.
In this preregistered study, we first investigated whether conspiratorial beliefs during a global health crisis, such as the COVID-19 pandemic, are associated with the proneness to present PLEs. We hypothesized that during times encompassing high loneliness and uncertainty (21), individuals who report PLEs are more susceptible to believe in conspiracy theories. Second, we examined how other pandemic-related factors such as social isolation and mental well-being may relate to conspiracy theories beliefs and PLEs. We hypothesized that all these variables may be associated with each other. If so, we will then perform separate mediation analyses to determine the possible mechanisms by which PLEs, social isolation or mental well-being may relate to the endorsement of conspiracy theories. Lastly, based on previous research on schizophrenia we will explore possible associations between diet, PLEs and conspiratorial beliefs. We postulate that people reporting low average iron intake are also more prone to show PLEs as well as to believe in conspiracy theories. To test these hypotheses, participants completed questionnaires assessing PLEs, social isolation (loneliness, social support, quantity, and quality of social interactions), mental health (e.g., stress), and conspiratorial beliefs. They also submitted their daily food intake for 7 days using a smartphone app (see Figure 1 and section “Materials and methods”).
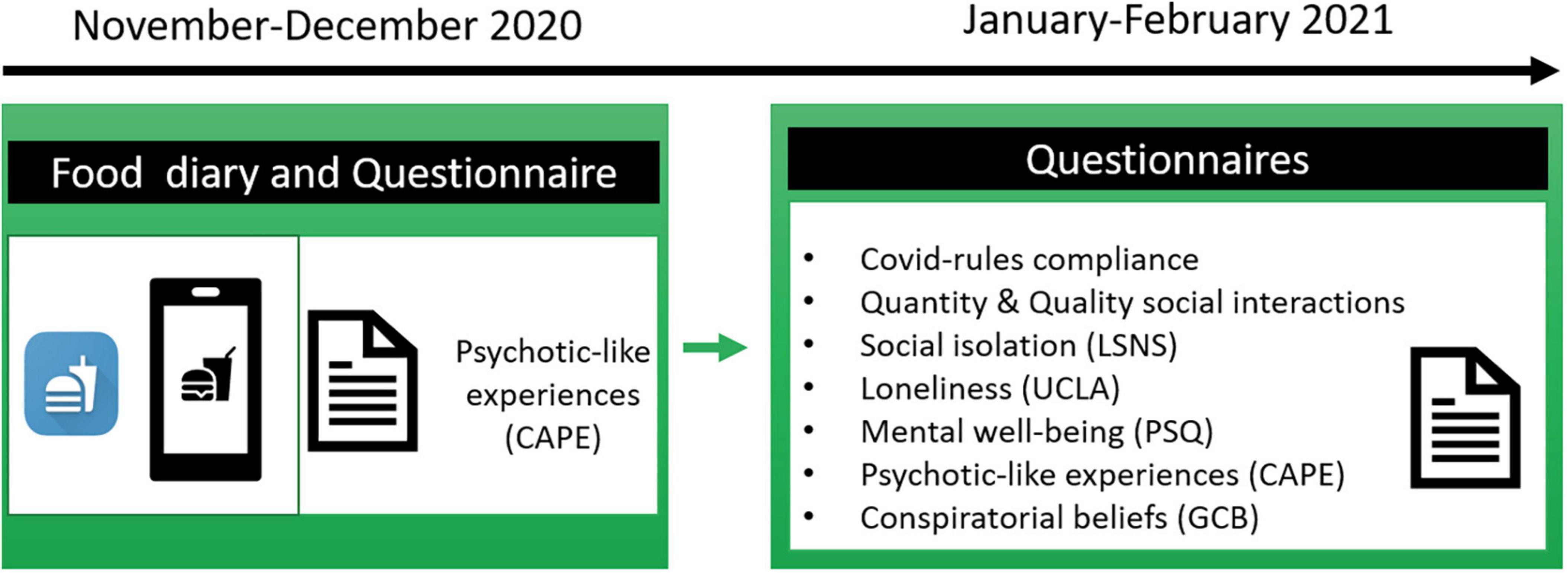
Figure 1. Study outline. Participants first answered a questionnaire assessing psychotic-like experiences (PLEs) and completed a daily food diary for 7 days via a smartphone app. Subsequently, they completed questionnaires measuring social isolation, conspiratorial beliefs, mental well-being, PLEs, demographics among others.
Materials and methods
Procedure
After providing instructions, participants were invited to complete a battery of online questionnaires assessing PLEs, social isolation (loneliness, social support, quantity, and quality of social interactions), mental health (e.g., stress), and conspiratorial beliefs see Figure 1. Written informed consent was obtained from each participant. Data were collected between 29 January and 8 February 2021) at which time there was a strict lockdown in Germany and Austria.
We also previously collected (10 November–23 December 2020) from the same participants, as a part of a larger study (preregistered under),1 a daily diary of their food consumption. In particular, participants were asked to install a food-diary app provided by us on their smartphone, and submit their daily intake of food items and beverages in the app, from which we extracted the total calories, and the macro- and micronutrients per meal per day (22) (see Figure 1).
Participants
An initial sample of 147 participants took part in the study. Participants recruitment was completely online via Prolific,2 including invitations and data collection. Inclusion criteria were: (1) residing in Germany or Austria, (2) being fluent in German, and (3) no personal history of psychiatric illness.
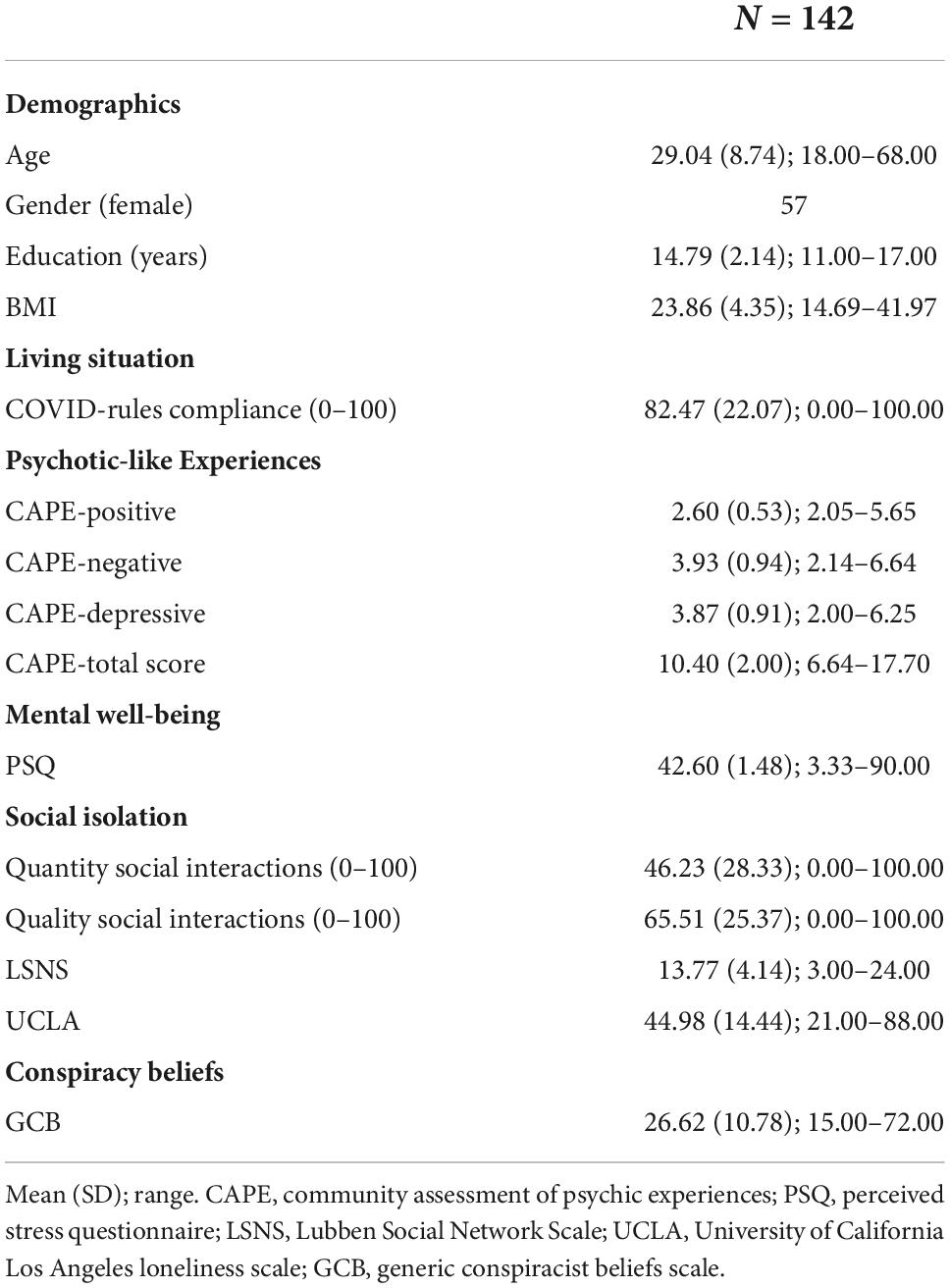
Five participants were excluded from the analyses, as they were not residing in Germany or Austria. Thus, the final sample included 142 participants (see Table 1 for demographics). All subjects were paid £3.50 for their participation. The Humbold Ethics Committee approved the study, which was conducted in accordance with the Declaration of Helsinki.
Questionnaires
Psychotic-like experiences
The Community Assessment of Psychic Experience (CAPE) is a 42-item questionnaire that measures self-reported subclinical psychotic symptoms in the general population based on three dimensions: positive symptoms, negative symptoms, and depression (23, 24). Several studies have shown that the CAPE can be a screening tool to identify people who might be at risk for psychosis (9, 10, 25).
Conspiratorial beliefs
The Generic Conspiracist Beliefs Scale (GCB) (26) includes 15 questions relating to different conspiracy theories and asks respondent how much they agree with each given statement on a five-point scale. This scale has a total score ranging from 15 to 75, with higher scores reflecting higher levels of conspiracy beliefs. The GCB is one of the most largely used measure of beliefs in conspiracy theories (27) and comprises distinct but related factors such as Government Malfeasance, Extraterrestrial Cover-up, Malevolent Global Conspiracies, Personal Wellbeing, and Control of Information (27, 28).
Mental well-being
The Perceived Stress Questionnaire (PSQ-20) is a psychological instrument measuring subjective experiences of perceived stress (29, 30), which has been considered as a predictor of health and well-being (31).
Social isolation
We used two different questions assessing participants’ quantity and quality of social interactions. The first question was: “How many social interactions, on average, did you have in the past week?.” Social interactions could be face-to-face, via telephone or online. The second question was: “On average, how satisfied are you with the social interactions of the past week?.” For both questions participants were asked to report a number from 1 (not at all) to 100 (very). Further, we used the Lubben Social Network Scale (LSNS-6) (32), a six-item self-report questionnaire assessing perceived social support received by friends and family. Lastly, the 20-item UCLA scale was employed to measure participants’ feeling of loneliness (33).
Food diary via FoodApp
Participants could input using a smartphone FoodApp when they had a meal (date and time), the type of meal (e.g., lunch, dinner snack), food item, and quantity (in grams or milliliters). They were asked to complete the daily food diary for 7 consecutive days (34). The output allowed us to compute two main variables: caloric content and information on micro- and macronutrients of the consumed food using the German Federal Food Key data table (Bundeslebensmittelschlüssel; Dehne et al. (35)). We calculated energy intake adjusted values (g/1,000 kcal/day) to account for an individuals’ total energy intake (36). Furthermore, we extracted daily energy derived from each macronutrient. In particular, the daily intake of carbohydrates (g/day) was multiplied by 4 kcal, while fat intake by 9 kcal (22). Lastly, tyrosine and tryptophan to large neutral amino acids (LNAA) ratios were calculated by dividing the quantity of tyrosine and of tryptophan by the sum of the other LNAAs (22, 37, 38).
Statistical analyses
The analysis plan was preregistered on the public data repository Open Science Framework.3 The data was analyzed using R statistical software (R Core Team). Mediation analyses were performed using JASP (version 0.14.1.0). The Shapiro–Wilk test was undertaken to demonstrate that data were normally distributed.
Spearman correlations were performed to test possible associations between each of the variables among social isolation (UCLA, Lubben Scale, self-report measures of quantity, and quality of social interactions), PLEs (CAPE), mental well-being (PSQ-20), and beliefs in conspiracy theories (GCB). Correlations were corrected for multiple comparisons separately for each results section using the Bonferroni method. A mediation analysis was performed to assess if the variable social isolation was mediating the relationship between PLEs and the dependent variable beliefs in conspiracy beliefs. A further mediation analysis was performed using PLEs as a mediator in the relationship between social isolation and conspiracy beliefs. Bootstrapping (1,000 samples) was performed as implemented in the “lavaan” package (39) in JASP.
A Wilcoxon signed-rank test was performed to examine within-group differences in CAPE scores between two different time-points (10 November–23 December 2020 vs. 29 January–8 February 2021). Spearman correlations were performed to test associations between participants’ CAPE scores and GCB scores with their daily food intake ratings.
Results
An initial sample of 147 participants signed up via Prolific. Five participants were excluded from the analyses, as they were not residing in Germany or Austria (see the section “Materials and methods”). Thus, analyses on questionnaire data were performed on the resulting 142 participants (see Table 1 for descriptive statistics). Of those participants, a total of 126 completed their food intake for at least 3 days using the food-diary app. Hence, analysis including food measures was conducted on these 126 participants.
Psychotic-like experiences and conspiratorial beliefs
We first preregistered to test whether PLEs are associated with conspiratorial beliefs. To do so, we performed a Spearman correlation between the CAPE-total score and the GCB score. Results showed a significant positive correlation between the two questionnaires (rho = 0.28; p < 0.001). Thus, the more participants presented PLEs the more they tended to believe in conspiracy theories (see Figure 2A). Further, we assessed which of the three CAPE subscales (positive, negative, and depressive) was correlating with GCB scores. We found that both CAPE-positive (rho = 0.45; p < 0.001) and negative (rho = 0.25; p = 0.008) subscales positively correlated with GCB scores, while CAPE-depressive did not (rho = 0.15; p = 0.231). P-values are Bonferroni corrected. These results support a relationship between PLEs (and their positive and negative dimensions) and conspiratorial beliefs.
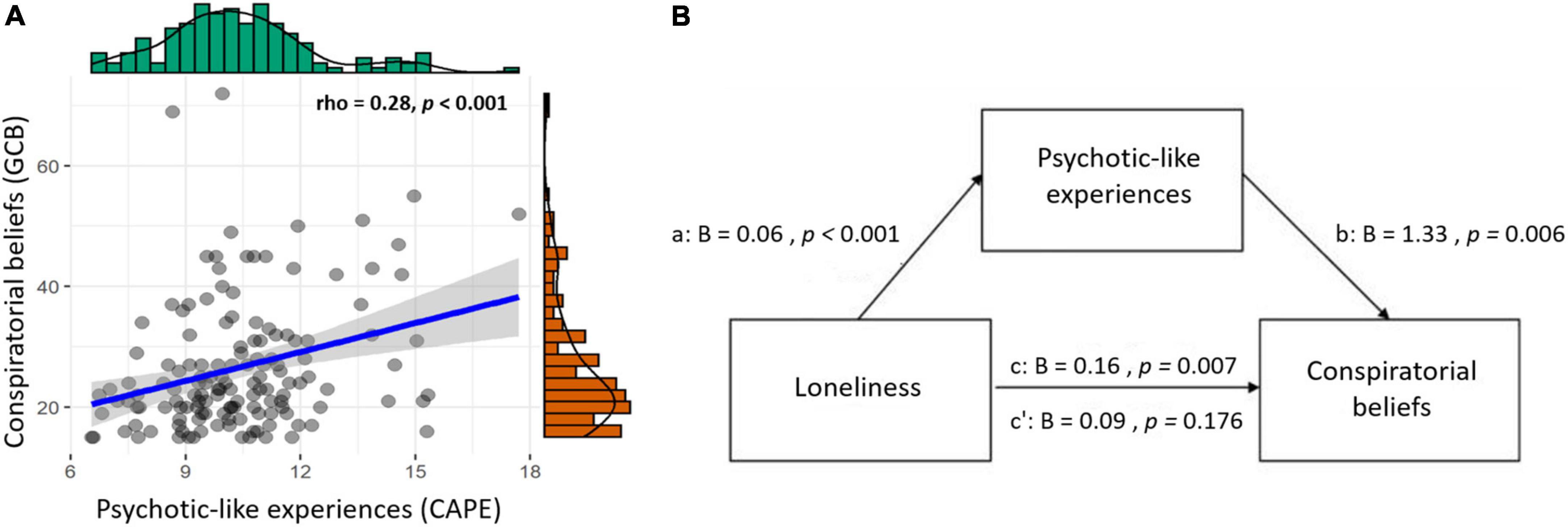
Figure 2. Associations between loneliness, psychotic-like experiences (PLEs) and conspiratorial beliefs. (A) Significant positive correlation between conspiratorial beliefs and PLEs (rho = 0.28, p < 0.001); (B) Mediation model with loneliness as predictor and PLEs as mediator predicting conspiratorial beliefs. Betas are unstandardized, total effect (c), direct path (c’).
Loneliness, psychotic-like experiences, and their influence on conspiratorial beliefs
So far, we showed that PLEs are associated with conspiratorial beliefs. Next, we aimed to investigate whether perceived social isolation in a period of social restrictions is associated with conspiratorial beliefs and PLEs.
Hence, we performed different Spearman correlations between the total scores of questionnaires assessing loneliness (UCLA), social support (LSNS), and self-report measures of quantity and quality of social interactions with GCB scores. Results showed a significant positive correlation only between UCLA and GCB (rho = 0.28; p = 0.004). No other significant correlations emerged (all p’s > 0.38) see Supplementary Table 1. Similarly, UCLA was the only measure of social isolation among others also correlating with CAPE-total scores (rho = 0.37; p < 0.001) (all p’s > 0.69) see Supplementary Table 1.
Overall, these results suggest positive associations between loneliness (regardless of the amount of social interaction and/or social support the participants received), PLEs, and conspiratorial beliefs. These results persisted even when controlling for demographics such as gender and the level of education. More in details, GCB and CAPE total score are still significantly positively associated (rho = 0.272; p = 0.002), as well as UCLA and GCB (rho = 0.255; p < 0.003), and UCLA and CAPE total score (rho = 0.341; p < 0.001). To better understand how loneliness and PLEs relate to conspiratorial beliefs, we preregistered to explore different mediation analyses (see the section “Materials and methods”). More in detail, we first tested whether UCLA could mediate (mediating variable) the relationship between CAPE (predictor variable) and GCB (dependent variable). Results from this analysis showed that UCLA did not mediate the effect of CAPE on GCB [bootstrapped indirect effect (a*b) B = 0.26, SE = 0.20, Z = 1.31, p = 0.189]. The result of this mediation model persisted even when controlling for demographic variables such as gender and level of education [bootstrapped indirect effect (a*b) B = 0.24, SE = 0.20, Z = 1.21, p = 0.23]. Next, a second mediation analysis was performed using CAPE as a mediator in the relationship between UCLA (predictor variable) and GCB (dependent variable). Results showed that CAPE fully mediated the effect of UCLA on GCB [bootstrapped indirect effect (a*b) B = 0.08, SE = 0.03, Z = 2.57, p = 0.012; see Figure 2B], meaning that the more participants felt lonely, the more they believed in conspiracy theories, but this was dependent on their propensity to have PLEs. This mediation model persisted when controlling for demographics such as gender and level of education [bootstrapped indirect effect (a*b) B = 0.08, SE = 0.03, Z = 2.58, p = 0.010].
Perceived stress is not related to conspiratorial beliefs
Next, we examined if also another factor related to health and well-being such as perceived-stress (PSQ-20) is associated with different levels of conspiratorial beliefs. Correlations were performed using both PSQ-20 total scores and PSQ-20 subscales scores (worries, joy, tension, and demands). A Spearman correlation between PSQ-20 and GCB scores did not reveal a significant result (rho = 0.15; p = 0.380). No significant results emerged also between PSQ-20 subscales and GCB (all p’s > 0.22) see Supplementary Table 2. These results suggest that conspiratorial beliefs are specifically associated with PLEs and loneliness but not with a more general subjective well-being or distress.
Exploratory analyses
Since a large body of literature has shown an association between dietary intake and the severity of psychotic symptoms in patients with schizophrenia (40), we preregistered to explore whether diet also relates to PLEs in healthy individuals. In particular, we focus on large amino acids such as tyrosine, tryptophan, as well as on iron intake levels since they all have been reported to be involved in the dopaminergic and serotoninergic transmission in the brain and in the pathophysiology of psychosis (12, 37, 40). Based on previous studies on schizophrenia (40), we also examined whether food intake indexed by certain nutrient compositions (e.g., carbs, fat, fruit, and vegetables) is associated with CAPE. More in details, high total intake of fruit and vegetables has been associated with better mental health (22, 41, 42). In line with this evidence, several studies reported a negative association between dietary intake of fruits and vegetables and the presence of psychosis (40, 41, 43–45). Furthermore, studies on stress in animals and humans have found that stress can modify the diet by preferring high-fat and high-carb foods (46, 47). Importantly, psychological stress is often comorbid with schizophrenia (48, 49) and correlates positively with PLEs (50). Regarding the dopaminergic precursor tyrosine and the serotoninergic precursor tryptophan, studies have reported their crucial role in motivation and mood, respectively. For example, it has been shown that acute tyrosine and tryptophan depletions can reduce motivation for reward and lower mood (22, 37, 51, 52). Simultaneously, dopamine and serotonin play an important role in psychosis (53, 54). Based on these results, dietary tyrosine and tryptophan intake levels may be associated with different levels of PLEs. Spearman correlations showed that CAPE scores were not associated with estimated Tyrosine/LNAA, Phenylalanine/LNAA, and Tryptophan/LNAA intakes (all p’s > 0.73) see Supplementary Table 3. Interestingly, CAPE scores negatively correlated with fruit (rho = −0.31; p = 0.002) and carbohydrate (rho = −0.26; p = 0.013) intakes, and positively correlated with fat intake (rho = 0.22; p = 0.045) see Figure 3. No significant associations were found between CAPE scores and vegetable intake (rho = 0.00; p = 1) see Supplementary Table 4. Lastly, CAPE scores negatively correlated with iron intake (rho = −0.25; p = 0.004) (see Figure 3). Further decomposing this correlation, by performing separate correlations between the different CAPE subscales (positive, negative, and depressive) and iron intake, showed that lower CAPE-negative symptoms were associated with reduced iron intake (rho = −0.28; p = 0.005) (see Figure 3D). No significant correlations emerged with the CAPE-positive (rho = −0.17; p = 0.171) and the CAPE-depressive (rho = −0.14; p = 0.374) subscales (see Supplementary Table 5). These results suggest that the negative dimension of PLEs in healthy individuals is associated with lower iron intake. Strikingly, these results are in line with studies on patients with chronic psychotic disorders (12, 40). Lastly, no significant associations emerged between GCB and food intake (all p’s > 0.38) see Supplementary Tables 6–8.
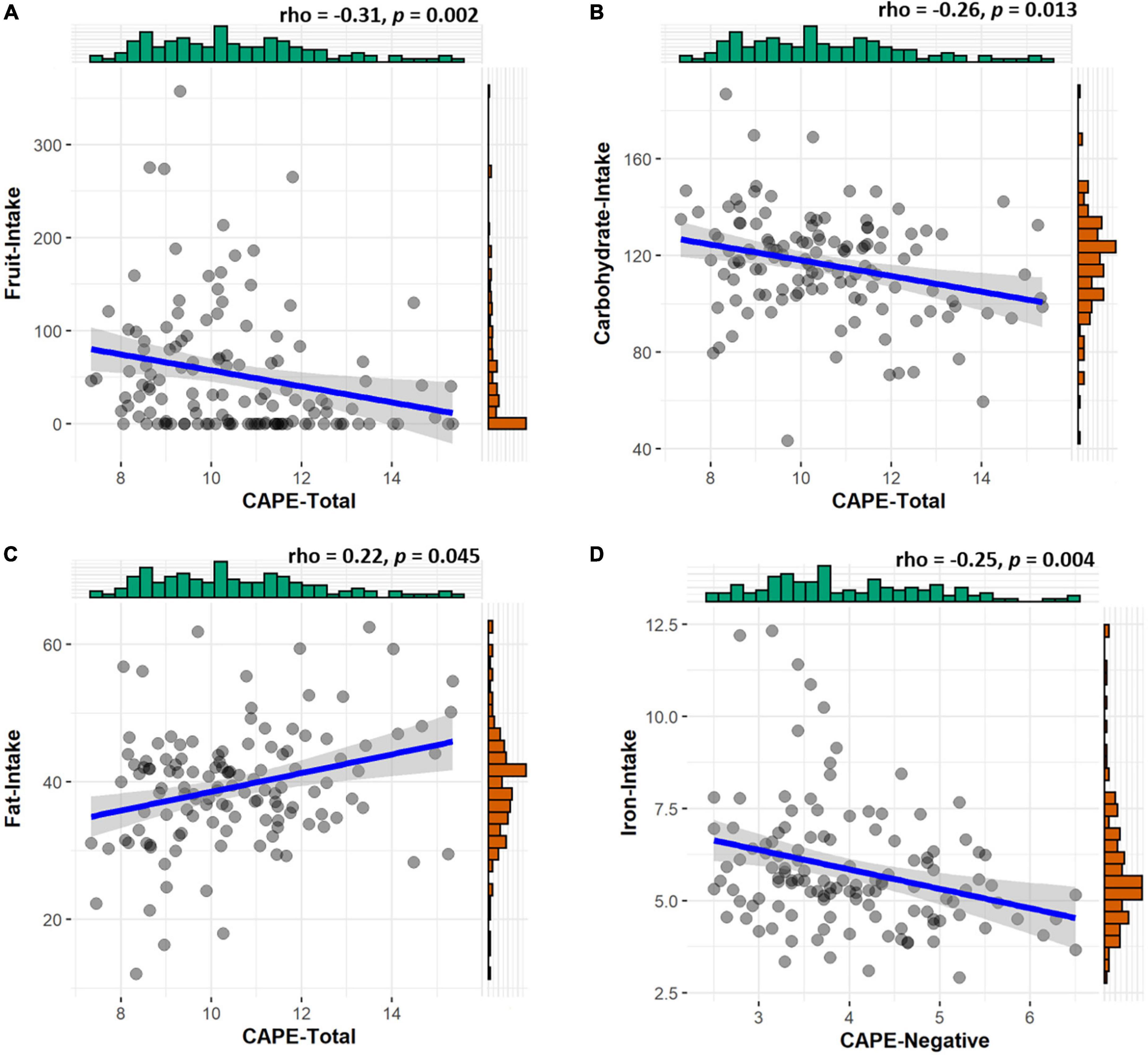
Figure 3. Associations between psychotic-like experiences (PLEs) and food intake. PLEs negatively correlate with (A) fruit (rho = −0.31, p = 0.002), (B) carbohydrate (rho = −0.26, p = 0.013), and (D) iron (rho = −0.25, p = 0.004) intakes. They also positively correlate with (C) fat intake (rho = 0.22, p = 0.045).
Note that food intake measures and CAPE scores used in these analyses were collected during time-point one (10 November–23 December 2020), while all the other questionnaire measures were collected during time-point two (29 January–8 February 2021) (see Figure 1). Since the same participants were asked to fill out the CAPE questionnaire during both time-points, a Wilcoxon signed-rank test was performed to assess whether their levels of PLEs changed over time. Results showed no differences in CAPE scores between the two time-points (time-point one M = 10.51, SD = ± 1.84; timepoint two M = 10.40, SD = ± 0.91; V Wilcoxon = 4490, p = 0.306). Since we did not exclude participants outside of the normal BMI range, we tested through correlations and mediation analyses whether this variability may (or may not) impact our results. These analyses seem to suggest that the variability of participants’ BMI did not impact our results (see Supplementary materials).
Discussion
This preregistered study investigated whether PLEs are associated with conspiratorial beliefs during the lockdown in a global health crisis. As an emerging field of research (3), only a few studies have investigated the possible relationship between conspiratorial beliefs and PLEs (7, 55, 56). We were also interested in other pandemic-related factors such as social isolation as a possible contributor to conspiratorial beliefs since social restriction measures were so prominent during lockdowns. Therefore, we assessed whether both PLEs and social isolation can predict conspiratorial beliefs and, if so, which of these variables can mediate the association with conspiratorial beliefs. Furthermore, based on previous studies on schizophrenia, we explored whether the diet is associated with PLEs and conspiratorial beliefs.
We hypothesized that PLEs are associated with conspiratorial beliefs. Similarly, we hypothesized that also other pandemic-related factors such as social isolation and mental well-being are associated with conspiratorial beliefs. Lastly, we hypothesized that PLEs, social isolation and mental well-being could all be associated with each other and predict conspiratorial beliefs. If so, we tested through different mediation analyses whether one of these variables can mediate the contribution of the other in predicting the endorsement of conspiracy beliefs.
In line with our hypothesis, results show that PLEs are positively associated with conspiratorial beliefs, meaning that the higher the participants’ levels of PLEs the more they reported to endorse conspiratorial beliefs. This result provides an extension of previous research, showing an association between a subcomponent of PLEs such as paranoia and the endorsement of conspiracy theories (2, 7). It has been argued that similar to individuals with high levels of PLEs, those supporting conspiratorial beliefs tend to collect less information to make decisions (jumping to conclusion bias). Therefore, both PLEs and conspiratorial thinking may have in common a more intuitive thinking style (2). In line with this observation, studies have found negative associations between analytic thinking and the endorsement of conspiratorial beliefs (57, 58). Interestingly, we found that not only the positive dimension of PLEs (e.g., paranoia) but also its negative dimension (e.g., avolition or lack of motivation) is associated with conspiratorial beliefs. This association was not found with the depression dimension (e.g., affective component) of PLEs. Overall, these findings suggest that not all subdimensions of PLEs are associated with conspiratorial beliefs and that both the positive (possibly through cognitive processes such as the jump to conclusion bias) and negative (reduced motivation) dimensions of PLEs may contribute to believing in conspiracy theories. In line with these findings, a study by Ståhl and colleagues (59) proposed that skepticism toward conspiratorial beliefs requires sufficient cognitive and motivational abilities, which are both altered in individuals with high levels of PLEs (9, 59, 60).
Another important result that emerged from our study is the role of loneliness in the endorsement of conspiracy theories. During the COVID-19-pandemic, social distancing restrictions led some people to experience greater social isolation and mental health illnesses (61). It is currently unknown what role social isolation plays in the dynamic between PLEs and conspiratorial beliefs in the context of the pandemic. Interestingly, loneliness positively predicted both PLEs and conspiratorial beliefs. However, this association was not found with other measures of social isolation such as social support and measures of quantity and quality of social interactions. Therefore, although studies showed that these measures of social isolation are highly correlated (62), our results suggest that only the subjective feeling of a lack of satisfactory interpersonal relationships (and not the objective amount of social support) is related to PLEs and conspiratorial beliefs during difficult times such as the COVID-19 pandemic. Similar associations between loneliness, PLEs, and conspiratorial beliefs were found in a previous study (7). The authors argued that the increased feelings of loneliness may have led people more susceptible to hear voices or perceive humanlike agency also in non-human stimuli (63), eventually influencing their association with conspiratorial beliefs (7). Our mediation analysis could confirm this hypothesis by showing that the proneness to show PLEs fully mediated the relationship between loneliness and conspiratorial beliefs. That is, the experience of loneliness during the COVID-19 pandemic enhances the proneness to experience psychotic events that increases the endorsement of conspiracy theories.
Besides social isolation and PLEs, the lockdown also resulted in diet changes (64). Research shows that a healthy diet helps to protect mental health (65). However, no studies have investigated the link between diet, PLEs and conspiratorial beliefs during challenging, and stressful times. We explored whether food intake, and in particular iron intake levels, may be associated with PLEs and conspiratorial beliefs. We found that food intake was not associated with conspiratorial beliefs. However, in line with studies on patients with schizophrenia, we found a significant association between food intake and PLEs levels. More in detail, PLEs were negatively associated with fruit, carbohydrate, and iron intakes, and positively with fat intake. In line with our findings, some studies have reported improved symptoms or decreased incidence/risk of schizophrenia with higher dietary fruit intake (40), possibly due to the antioxidant and anti-inflammatory activity of a diet rich in fruits (66). Differently, the association between psychosis and total dietary carbohydrates and fat intakes is unclear, with some studies showing a positive association (67, 68), while others a negative association or no association (40). In addition, it has been reported that altered iron homeostasis is implicated in neuropsychiatric disorders (69). In particular, iron reductions can result in changes in dopamine neurotransmission and altered neurodevelopment (70). Indeed, prospective studies have shown a significant relationship between maternal iron deficiency and the risk of schizophrenia in offspring (71, 72). Interestingly, first-episode schizophrenia individuals with high levels of negative symptoms showed lower levels of blood iron compared to healthy controls (12). Similarly, a magnetic resonance imaging (MRI) study found a decreased iron concentration in gray matter nuclei including the bilateral substantia nigra in first-episode schizophrenia individuals compared to healthy controls (14). In line with these results, we found that higher levels of PLEs (in particular, the negative domain of PLEs) are associated with a reduced average daily iron intake. Overall, our findings suggest a possible link between reduced iron intake and PLEs, possibly influencing dopaminergic neurotransmission in the brain and therefore accounting for these subclinical symptoms in the general population.
Some limitations of the current study should be addressed. First, loneliness, conspiratorial beliefs and food intake were only measured once, therefore we cannot assess within-person changes over time. Second, conspiratorial beliefs and food intake were not time-locked. Third, our findings are correlational, and we cannot make causal arguments. Fourth, our measures were based on self-reports, which may have lower reliability and validity.
Conclusion
In conclusion, loneliness predicted the endorsement of conspiracy theories during the COVID-19 lockdown. Strikingly, the proneness to experience subclinical psychotic symptoms played an underlying mediating role. In addition, these subclinical symptoms were associated with lower fruit, carbohydrate, and iron intakes, as well as with higher fat intake. Our results contribute to the study of beliefs in conspiracy theory and add insights into how they can affect individuals’ mental health and relationships. Moreover, these results open the avenue for potential novel intervention strategies to manage and optimize food intake in individuals with PLEs. In future research, experimental designs should be used to test the possible causal effects shown in this study.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by The Humbold Ethics Committee approved the study. The patients/participants provided their written informed consent to participate in this study.
Author contributions
DT and SP: conceptualization and project administration. DT: investigation, writing – original draft preparation, and visualization. DT, AL, and SP: methodology. DT, A-KM, and AL: formal analysis. A-KM, AL, DT, and SP: writing – review and editing. SP: supervision and funding acquisition. All authors have read and agreed to the published version of the manuscript.
Funding
This study was funded by the grants from the German Ministry of Education and Research (BMBF) and the State of Brandenburg (SP: DZD and FKZ; 82DZD03C2G, 82DZD03D03, DZDG16001, and 82DZD0C2G).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fnut.2022.1006043/full#supplementary-material
Footnotes
References
1. Pišl V, Vevera J. Conspiracy theories as a natural part of pandemics. Cas Lek Cesk. (2021) 160:37–9.
2. Kuhn SAK, Lieb R, Freeman D, Andreou C, Zander-Schellenberg T. Coronavirus conspiracy beliefs in the German-speaking general population: endorsement rates and links to reasoning biases and paranoia. Psychol Med. (2021). [Epub ahead of print]. doi: 10.1017/S0033291721001124
3. van Prooijen JW, Douglas KM. Belief in conspiracy theories: basic principles of an emerging research domain. Eur J Soc Psychol. (2018) 48:897–908. doi: 10.1002/ejsp.2530
4. Ahadzadeh AS, Ong FS, Wu SL. Social media skepticism and belief in conspiracy theories about COVID-19: the moderating role of the dark triad. Curr Psychol. (2021). [Epub ahead of print]. doi: 10.1007/s12144-021-02198-1
5. De Coninck D, Frissen T, Matthijs K, d’Haenens L, Lits G, Champagne-Poirier O, et al. Beliefs in conspiracy theories and misinformation about COVID-19: comparative perspectives on the role of anxiety, depression and exposure to and trust in information sources. Front Psychol. (2021) 12:646394. doi: 10.3389/fpsyg.2021.646394
6. Ullah I, Khan KS, Tahir MJ, Ahmed A, Harapan H. Myths and conspiracy theories on vaccines and COVID-19: potential effect on global vaccine refusals. Vacunas. (2021) 22:93–7. doi: 10.1016/j.vacun.2021.01.001
7. Ferreira S, Campos C, Marinho B, Rocha S, Fonseca-Pedrero E, Barbosa-Rocha N. What drives beliefs in COVID-19 conspiracy theories? The role of psychotic-like experiences and confinement-related factors. Soc Sci Med. (2021) 292:114611. doi: 10.1016/j.socscimed.2021.114611
8. Pytlik N, Soll D, Mehl S. Thinking preferences and conspiracy belief: intuitive thinking and the jumping to conclusions-bias as a basis for the belief in conspiracy theories. Front Psychiatry. (2020) 11:568942. doi: 10.3389/fpsyt.2020.568942
9. Terenzi D, Mainetto E, Barbato M, Rumiati RI, Aiello M. Temporal and effort cost decision-making in healthy individuals with subclinical psychotic symptoms. Sci Rep. (2019) 9:2151. doi: 10.1038/s41598-018-38284-x
10. Mossaheb N, Becker J, Schaefer MR, Klier CM, Schloegelhofer M, Papageorgiou K, et al. The community assessment of psychic experience (CAPE) questionnaire as a screening-instrument in the detection of individuals at ultra-high risk for psychosis. Schizophr Res. (2012) 141:210–4. doi: 10.1016/j.schres.2012.08.008
11. Kelleher I, Cannon M. Psychotic-like experiences in the general population: characterizing a high-risk group for psychosis. Psychol Med. (2011) 41:1–6. doi: 10.1017/S0033291710001005
12. Kim SW, Stewart R, Park WY, Jhon M, Lee JY, Kim SY, et al. Latent iron deficiency as a marker of negative symptoms in patients with first-episode schizophrenia spectrum disorder. Nutrients. (2018) 10:1707. doi: 10.3390/nu10111707
13. Shah HE, Bhawnani N, Ethirajulu A, Alkasabera A, Onyali CB, Anim-Koranteng C, et al. Iron deficiency-induced changes in the hippocampus, corpus striatum, and monoamines levels that lead to anxiety, depression, sleep disorders, and psychotic disorders. Cureus. (2021) 13:e18138. doi: 10.7759/cureus.18138
14. Xu M, Guo Y, Cheng J, Xue K, Yang M, Song X, et al. Brain iron assessment in patients with First-episode schizophrenia using quantitative susceptibility mapping. Neuroimage Clin. (2021) 31:102736. doi: 10.1016/j.nicl.2021.102736
15. Pai N, Vella SL. COVID-19 and loneliness: a rapid systematic review. Aust N Z J Psychiatry. (2021) 55:1144–56. doi: 10.1177/00048674211031489
16. Probst T, Budimir S, Pieh C. Depression in and after COVID-19 lockdown in Austria and the role of stress and loneliness in lockdown: a longitudinal study. J Affect Disord. (2020) 277:962–3. doi: 10.1016/j.jad.2020.09.047
17. Narita Z, Stickley A, DeVylder J. Loneliness and psychotic experiences in a general population sample. Schizophr Res. (2020) 218:146–50. doi: 10.1016/j.schres.2020.01.018
18. Lim MH, Eres R, Vasan S. Understanding loneliness in the twenty-first century: an update on correlates, risk factors, and potential solutions. Soc Psychiatry Psychiatr Epidemiol. (2020) 55:793–810. doi: 10.1007/s00127-020-01889-7
19. Graeupner D, Coman A. The dark side of meaning-making: how social exclusion leads to superstitious thinking. J Exp Soc Psychol. (2017) 69:218–22. doi: 10.1016/j.jesp.2016.10.003
20. Williams KD. Williams - Ostracism. Annu Rev Psychol. (2007) 58:425–52. doi: 10.1146/annurev.psych.58.110405.085641
21. McGinty EE, Presskreischer R, Han H, Barry CL. Psychological distress and loneliness reported by US adults in 2018 and April 2020. JAMA. (2020) 324:93–4. doi: 10.1001/jama.2020.9740
22. Losecaat Vermeer AB, Muth A, Terenzi D, Park SQ. Curiosity for information predicts wellbeing mediated by loneliness during COVID-19 pandemic. Sci Rep. (2022) 12:7771. doi: 10.1038/s41598-022-11924-z
23. Stefanis NC, Hanssen M, Smirnis NK, Avramopoulos DA, Evdokimidis IK, Stefanis CN, et al. Evidence that three dimensions of psychosis have a distribution in the general population. Psychol Med. (2002) 32:347–58. doi: 10.1017/S0033291701005141
24. Schlier B, Jaya ES, Moritz S, Lincoln TM. The Community Assessment of Psychic Experiences measures nine clusters of psychosis-like experiences: a validation of the German version of the CAPE. Schizophr Res. (2015) 169:274–9. doi: 10.1016/j.schres.2015.10.034
25. Bukenaite A, Stochl J, Mossaheb N, Schäfer MR, Klier CM, Becker J, et al. Usefulness of the CAPE-P15 for detecting people at ultra-high risk for psychosis: psychometric properties and cut-off values. Schizophr Res. (2017) 189:69–74. doi: 10.1016/j.schres.2017.02.017
26. Molz G, Stiller MS, Krüppel J, Weiher M. On the measurement of conspiracy thinking: a validation of the german version of the “generic conspiracist belief scale”. J Political Psychol. (2020) 1:5–24.
27. Drinkwater KG, Dagnall N, Denovan A, Neave N. Psychometric assessment of the Generic Conspiracist Beliefs Scale. PLoS One. (2020) 15:e0230365. doi: 10.1371/journal.pone.0230365
28. Brotherton R, French CC, Pickering AD. Measuring belief in conspiracy theories: the generic conspiracist beliefs scale. Front Psychol. (2013) 4:279. doi: 10.3389/fpsyg.2013.00279
29. Levenstein S, Prantera C, Varvo V, Scribano ML, Berto E, Luzi C, et al. Development of the perceived stress questionnaire: a new tool for psychosomatic research. J Psychosom Res. (1993) 37:19–32. doi: 10.1016/0022-3999(93)90120-5
30. Fliege H, Rose M, Arck P, Levenstein S, Klapp BF. Validierung des “perceived stress questionnaire”(PSQ) an einer deutschen Stichprobe. [Validation of the “Perceived Stress Questionnaire”(PSQ) in a German sample.]. Diagnostica. (2001) 47:142–52. doi: 10.1026//0012-1924.47.3.142
31. Østerås B, Sigmundsson H, Haga M. Psychometric properties of the perceived stress questionnaire (PSQ) in 15–16 years old Norwegian adolescents. Front Psychol. (2018) 9:1850. doi: 10.3389/fpsyg.2018.01850
32. Lubben JE. Assessing social networks among elderly populations. Fam Community Health. (1988) 11:42–52. doi: 10.1097/00003727-198811000-00008
33. Döring N, Bortz J. Psychometrische einsamkeitsforschung: deutsche neukonstruktion der UCLA loneliness scale. [Psychometric research on loneliness: a new German version of the University of California at Los Angeles (UCLA) Loneliness Scale.]. Diagnostica. (1993) 39:224–39.
34. Hendy HM. Which comes first in food-mood relationships, foods or moods? Appetite. (2012) 58:771–5. doi: 10.1016/j.appet.2011.11.014
35. Dehne LI, Klemm Ch, Henseler G, Bögl KW, Hermann-Kunz E. DerBundeslebensmittelschlüssel (BLS II.2). Bundesgesundheitsblatt. (1997) 40:203–6. doi: 10.1007/bf03044213
36. Agnoli C, Pounis G, Krogh V. Dietary pattern analysis. In: Pounis G editor. Analysis in Nutrition Research: Principles of Statistical Methodology and Interpretation of the Results. Cambridge, MA: Academic Press (2018). doi: 10.1016/B978-0-12-814556-2.00004-X
37. Strang S, Hoeber C, Uhl O, Koletzko B, Münte TF, Lehnert H, et al. Impact of nutrition on social decision making. Proc Natl Acad Sci USA. (2017) 114:6510–4. doi: 10.1073/pnas.1620245114
38. Terenzi D, Liu L, Bellucci G, Park SQ. Determinants and modulators of human social decisions. Neurosci Biobehav Rev. (2021) 128:383–93. doi: 10.1016/j.neubiorev.2021.06.041
39. Rosseel Y. Lavaan: an R package for structural equation modeling. J Stat Softw. (2012) 48:1–36. doi: 10.18637/jss.v048.i02
40. Aucoin M, Lachance L, Cooley K, Kidd S. Diet and psychosis: a scoping review. Neuropsychobiology. (2020) 79:20–42. doi: 10.1159/000493399
41. Głąbska D, Guzek D, Groele B, Gutkowska K. Fruit and vegetable intake and mental health in adults: a systematic review. Nutrients. (2020) 12:115. doi: 10.3390/nu12010115
42. Terenzi D, Muth AK, Park SQ. Nutrition and gut–brain pathways impacting the onset of Parkinson’s disease. Nutrients. (2022) 14:2781. doi: 10.3390/nu14142781
43. Simonelli-Muñoz AJ, Fortea MI, Salorio P, Gallego-Gomez JI, Sánchez-Bautista S, Balanza S. Dietary habits of patients with schizophrenia: a self-reported questionnaire survey. Int J Ment Health Nurs. (2012) 21:220–8. doi: 10.1111/j.1447-0349.2012.00821.x
44. Mucheru D, Hanlon MC, Campbell LE, McEvoy M, MacDonald-Wicks L. Social dysfunction and diet outcomes in people with psychosis. Nutrients. (2017) 9:80. doi: 10.3390/nu9010080
45. Hahn LA, Galletly CA, Foley DL, Mackinnon A, Watts GF, Castle DJ, et al. Inadequate fruit and vegetable intake in people with psychosis. Aust N Z J Psychiatry. (2014) 48:1025–35. doi: 10.1177/0004867414553950
46. Roberts CJ, Campbell IC, Troop N. Increases in weight during chronic stress are partially associated with a switch in food choice toward increased carbohydrate and saturated fat intake. Eur Eat Disord Rev. (2014) 22:77–82. doi: 10.1002/erv.2264
47. Bordier C, Klein S, le Conte Y, Barron AB, Alaux C. Stress decreases pollen foraging performance in honeybees. J Exp Biol. (2018) 221:jeb171470. doi: 10.1242/jeb.171470
48. Carol EE, Spencer RL, Mittal VA. Acute physiological and psychological stress response in youth at clinical high-risk for psychosis. Front Psychiatry. (2021) 12:641762. doi: 10.3389/fpsyt.2021.641762
49. Schirmbeck F, van der Burg NC, Blankers M, Vermeulen JM, McGuire P, Valmaggia LR, et al. Impact of comorbid affective disorders on longitudinal clinical outcomes in individuals at ultra-high risk for psychosis. Schizophr Bull. (2022) 48:100–10.
50. Prochwicz K, Kłosowska J, Dembiñska A. The mediating role of stress in the relationship between attention to threat bias and psychotic-like experiences depends on coping strategies. Front Psychiatry. (2020) 11:307. doi: 10.3389/fpsyt.2020.00307
51. Cools R, Blackwell A, Clark L, Menzies L, Cox S, Robbins TW. Tryptophan depletion disrupts the motivational guidance of goal-directed behavior as a function of trait impulsivity. Neuropsychopharmacology. (2005) 30:1362–73. doi: 10.1038/sj.npp.1300704
52. Bartoshuk LM, Duffy VB, Hayes JE, Moskowitz HR, Snyder DCDJ, de Jonghe BC, et al. Food cravings in pregnancy: preliminary evidence for a role in excess gestational weight gain. Appetite. (2016) 105:259–65. doi: 10.1016/j.appet.2016.04.040
53. Stahl SM. Beyond the dopamine hypothesis of schizophrenia to three neural networks of psychosis: dopamine, serotonin, and glutamate. CNS Spectr. (2018) 23:187–91. doi: 10.1017/S1092852918001013
54. Kapur S, Mizrahi R, Li M. From dopamine to salience to psychosis-linking biology, pharmacology and phenomenology of psychosis. Schizophr Res. (2005) 79:59–68. doi: 10.1016/j.schres.2005.01.003
55. Dagnall N, Drinkwater K, Parker A, Denovan A, Parton M. Conspiracy theory and cognitive style: a worldview. Front Psychol. (2015) 6:206. doi: 10.3389/fpsyg.2015.00206
56. Barron D, Furnham A, Weis L, Morgan KD, Towell T, Swami V. The relationship between schizotypal facets and conspiracist beliefs via cognitive processes. Psychiatry Res. (2018) 259:15–20. doi: 10.1016/j.psychres.2017.10.001
57. Swami V, Furnham A. Political paranoia and conspiracy theories. In: van Prooijen JW, van Lange PAM editors. Power, Politics, and Paranoia: Why People are Suspicious of their Leaders. Cambridge, MA: Cambridge University Press (2014). doi: 10.1017/CBO9781139565417.016
58. van Prooijen JW. Why education predicts decreased belief in conspiracy theories. Appl Cogn Psychol. (2017) 31:50–8. doi: 10.1002/acp.3301
59. Ståhl T, van Prooijen JW. Epistemic rationality: skepticism toward unfounded beliefs requires sufficient cognitive ability and motivation to be rational. Pers Individ Dif. (2018) 122:155–63. doi: 10.1016/j.paid.2017.10.026
60. Papanastasiou E, Mouchlianitis E, Joyce DW, McGuire P, Banaschewski T, Bokde ALW, et al. Examination of the neural basis of psychoticlike experiences in adolescence during reward processing. JAMA Psychiatry. (2018) 75:1043–51. doi: 10.1001/jamapsychiatry.2018.1973
61. Gu S, He Z, Sun L, Jiang Y, Xu M, Feng G, et al. Effects of coronavirus-19 induced loneliness on mental health: sleep quality and intolerance for uncertainty as mediators. Front Psychiatry. (2021) 12:738003. doi: 10.3389/fpsyt.2021.738003
62. Wang J, Mann F, Lloyd-Evans B, Ma R, Johnson S. Associations between loneliness and perceived social support and outcomes of mental health problems: a systematic review. BMC Psychiatry. (2018) 18:156. doi: 10.1186/s12888-018-1736-5
63. Epley N, Akalis S, Waytz A, Cacioppo JT. Creating social connection through inferential reproduction: loneliness and perceived agency in gadgets, gods, and hreyhounds. Psychol Sci. (2008) 19:114–20. doi: 10.1111/j.1467-9280.2008.02056.x
64. Ingram J, Maciejewski G, Hand CJ. Changes in diet, sleep, and physical activity are associated with differences in negative mood during COVID-19 lockdown. Front Psychol. (2020) 11:588604. doi: 10.3389/fpsyg.2020.588604
65. Begdache L, Sadeghzadeh S, Derose G, Abrams C. Diet, exercise, lifestyle, and mental distress among young and mature men and women: a repeated cross-sectional study. Nutrients. (2021) 13:24. doi: 10.3390/nu13010024
66. Cha HY, Yang SJ. Anti-inflammatory diets and schizophrenia. Clin Nutr Res. (2020) 9:241–57. doi: 10.7762/cnr.2020.9.4.241
67. Strassnig M, Brar JS, Ganguli R. Nutritional assessment of patients with schizophrenia: a preliminary study. Schizophr Bull. (2003) 29:393–7. doi: 10.1093/oxfordjournals.schbul.a007013
68. Dipasquale S, Pariante CM, Dazzan P, Aguglia E, McGuire P, Mondelli V. The dietary pattern of patients with schizophrenia: a systematic review. J Psychiatr Res. (2013) 47:197–207. doi: 10.1016/j.jpsychires.2012.10.005
69. Zheng W, Monnot AD. Regulation of brain iron and copper homeostasis by brain barrier systems: implication in neurodegenerative diseases. Pharmacol Ther. (2012) 133:177–88. doi: 10.1016/j.pharmthera.2011.10.006
70. Hare DJ, Double KL. Iron and dopamine: a toxic couple. Brain. (2016) 139:1026–35. doi: 10.1093/brain/aww022
71. Insel BJ, Schaefer CA, McKeague IW, Susser ES, Brown AS. Maternal iron deficiency and the risk of schizophrenia in offspring. Arch Gen Psychiatry. (2008) 65:1136–44. doi: 10.1001/archpsyc.65.10.1136
Keywords: conspiratorial beliefs, psychotic-like experiences, loneliness, diet, COVID-19
Citation: Terenzi D, Muth A-K, Losecaat Vermeer A and Park SQ (2022) Psychotic-like experiences in the lonely predict conspiratorial beliefs and are associated with the diet during COVID-19. Front. Nutr. 9:1006043. doi: 10.3389/fnut.2022.1006043
Received: 28 July 2022; Accepted: 14 October 2022;
Published: 28 October 2022.
Edited by:
Carol Coricelli, Western University, CanadaReviewed by:
Sara Sorella, University of Trento, ItalyFrancantonio Devoto, University of Milan-Bicocca, Italy
Copyright © 2022 Terenzi, Muth, Losecaat Vermeer and Park. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Damiano Terenzi, ZGFtaWFub3RlcmVuemlAZ21haWwuY29t; Soyoung Q. Park, c295b3VuZy5xLnBhcmtAZ21haWwuY29t
 Damiano Terenzi
Damiano Terenzi