- 1Department of Biological and Environmental Science and Technologies (DiSTeBA), University of Salento, Lecce, Italy
- 2Department of History, Society and Human Studies, University of Salento, Lecce, Italy
Childhood obesity represents a serious public health problem and this study evaluates the effectiveness of a 6-month educational intervention on lifestyle, nutrient adequacy, and diet quality in the school setting in improving the knowledge and behavior of primary school children regarding correct eating habits. The strategy was implemented over a 6-month period and participants were randomly assigned to either the intervention group (n = 200) or the non-intervention group (control group, n = 197). Participants had a mean body mass index of 18.3 ± 2.7 kg/m2 and its variation in the intervention group (−2.7 ± 0.5 kg/m2) was significantly different from that in the control group (3.41 ± 0.8 kg/m2). In the experimental group, there were significant differences between the proportion of children who were overweight, underweight, normal weight, or obese before and after intervention (p < 0.05). The best results were seen in the female sex, and after the intervention, there were no more girls with obesity. Furthermore, there were significant waist circumference decrement effects in the intervention group compared to the control group (p < 0.05). Finally, many of the participating children acquired healthy eating habits. Therefore, the quantitative results obtained suggest that a school intervention program represents an effective strategy to prevent and improve the problem of childhood overweight and obesity.
Introduction
Childhood overweight and obesity represent a major global health problem (1), and these conditions, if already present in childhood and adolescence, can certainly lead to serious chronic diseases (2, 3); when they persist in adulthood, cardiovascular disease, diabetes, and some cancers are their serious consequences (4–6).
Therefore, the monitoring of weight status in children is important for health disease prevention (7). The development of obesity in children is influenced by several modifiable behaviors and, in general, insufficient physical activity together with a high caloric intake are important factors contributing to the increase in obesity among young people (8, 9). In particular, dietary factors are importantly associated with childhood obesity (10) and the prevalence rates of diet-related diseases, such as obesity and diabetes in children and adolescents, push for the right priority to healthy diets (8, 9, 11). Many children, instead of a diet rich in fruits and vegetables, choose snacks with saturated trans fats and sugar (12), which lead to a higher energy intake (13) and consequently to overweight/obesity (12, 14, 15). The assumption of harmful behaviors, such as eating unhealthy foods, during the time spent in a sedentary lifestyle, has been shown to exacerbate the capacity to maintain an adequate body weight in children by creating a vicious cycle (16, 17). Both physical inactivity and sedentary/unhealthy behaviors increase the risk of being overweight and obese in childhood (18–20). Hence, the role of diet and physical activity in children has been investigated in previous studies (21, 22). Based on the above, Tabacchi et al. (21) suggested that raising children in an environment where both motor and cognitive skills are encouraged can improve food literacy and, furthermore, enhance school achievement.
Several lifestyle interventions were able to lower anthropometric and cardiometabolic risk factors (20, 23–26) and increase the body image satisfaction (27), but few interventions have considered changes in diet quality (28, 29). Unfortunately, children are frequently reluctant to comply with exhortation weight-related behaviors and response to behavioral treatment is generally limited and confined to the short term (30–32).
Obviously, as children spend a lot of their time in school, it is important to implement school programs aimed at defining and maintaining a healthy lifestyle (33–35), thus increasing the cognitive functioning and mental health and wellbeing (36). Therefore, the aim of our study was to evaluate the effect of a 6-month intervention on lifestyle, nutrient adequacy, and diet quality in children attending schools in Southern Italy.
Methods
Participants
To understand the effects of promoting nutrition adequacy, a sample of 398 children was selected from different schools. These schools are located in two cities with similar socioeconomic status and have not previously participated in health promotion programs. Schools were secondary-level public schools, with attendance from 8:00 to 13:00.
The sample was composed of 194 boys and 204 girls, who were allocated to a control group and a group participating in an intervention (n = 200 and n = 198, respectively). All children were healthy and free of any disability or musculoskeletal, cardiological, neurological, or respiratory diseases or dysfunctions. Before the inclusion of the children in our program, a parent or legal representative of each child signed informed consent. The study was conducted in accordance with the Helsinki Declaration and the European Union recommendations for Good Clinical Practice (document 111/3976/88, July 1990). The University's Research Ethics Committee approved the study.
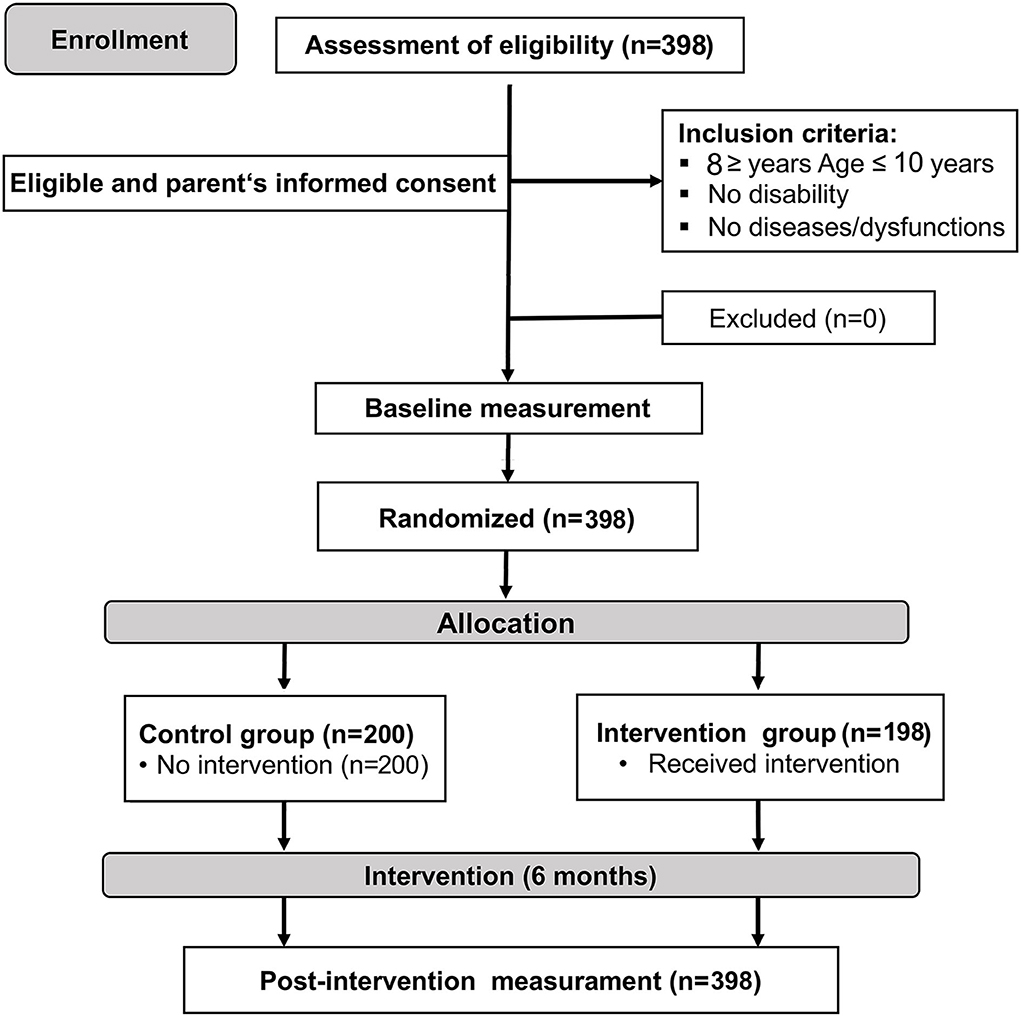
A randomized controlled trial study design, which is double-blinded, was employed; the design is shown in Figure 1.
Food education program
Before the start of the project, all teachers and parents in the intervention schools received on-site training to provide them with general information on the nature and significance of the intervention and to support their role in educating the children. The intervention conducted aimed at improving sugar-containing beverages consumption, high-caloric snack consumption, and promoting the consumption of vegetables and fruit. The goal of this program is to decrease energy intake while improving food quality. Therefore, information on portion control was provided with no indication of kilocalories or grams of food consumption. Food education and a healthy lifestyle (e.g., food choices, food labels, the five meals, consumption of fruits and vegetables, and sleep quality) were discussed with the active involvement of everyone.
The educational intervention covered 12 lessons for the subject's biology and alimentation implemented by classroom teachers. The first part (six lessons) aimed at increasing awareness and information regarding energy balance-related behaviors, with supporting materials, such as a pocket-sized diary, to monitor own behavior. The second part (six lessons) aimed at facilitation of choice to improve one of the behaviors, setting personal goals, identifying barriers, improving self-efficacy, and evaluating the change process. In this way, the children and families understand how to organize their weekly meal planning without detailed prescriptions. The control schools followed their regular curriculum.
Measures
All measures were recorded at baseline (T0) and 6 months from baseline (T1) at the completion of the intervention.
Body weight and height were ascertained, in duplicate, with standard techniques. Waist circumference was measured, in duplicate, at the iliac crest, and at mid-respiration using a non-elastic measuring tape. The ratio between waist circumference and height (WHR) was calculated. The cut-off used to represent CV risk for WHR was 0.500 (37).
For children and adolescents, the Center for Disease Control and Prevention defines overweight as a body mass index (BMI: weight in kilograms divided by height in meters squared) between the 85th and 95th percentiles and obesity as a BMI at or above the 95th percentile for sex and age (38).
The parents completed structured no validated questionnaires, which included the eating habits of their children (food frequency questionnaire) and their familiarity with certain food items. This questionnaire was administered twice to the parents of the children, the first time at the beginning of the study and the second time at the end of the intervention; in both cases, 48 h were given for completion. The data collected with the questionnaire were analyzed by extrapolating the frequency of each item considered in the proposed survey. Descriptive data was represented by the percentage.
Statistical analysis
Means and standard deviations were described for the total sample and for both the participants and control groups. All data have been tested for normality using the Kolmogorov–Smirnov test. To identify differences between groups, the t-test has been performed. For the association of different items of the questionnaire, a chi-square test was performed. The significance level was set to p < 0.05.
Results
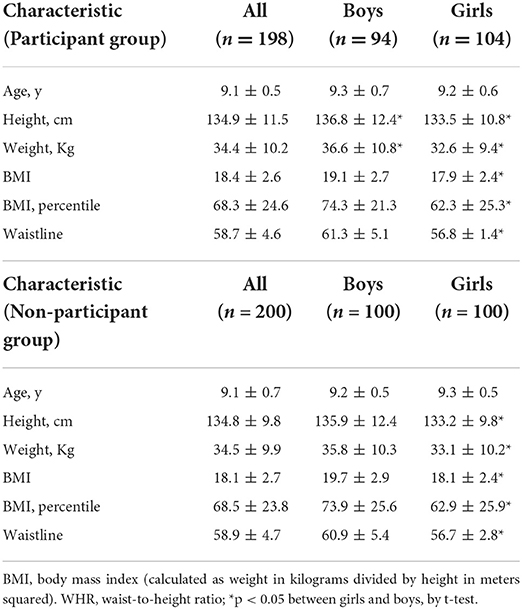
The sample consisted of 397 children who were randomly divided into two groups, the intervention group, and the control group. Table 1 shows the characteristics of the 197 children in the intervention group and the 200 children who made up the control group. The mean age was 9.5 ± 0.5 years for both sexes.
Coherent with the random assignment of children to the intervention and control groups, no significant differences were observed between these groups in terms of average weight, height, BMI, and proportion of overweight or obese children (p > 0.05; Table 1).
Statistically significant differences between the sexes were noted, being the boys taller and heavier than the girls. Boys also have a larger waistline (p < 0.05; Table 1).
Interestingly, while BMI increases in the untreated group, it significantly decreases in the intervention group (Figure 2).
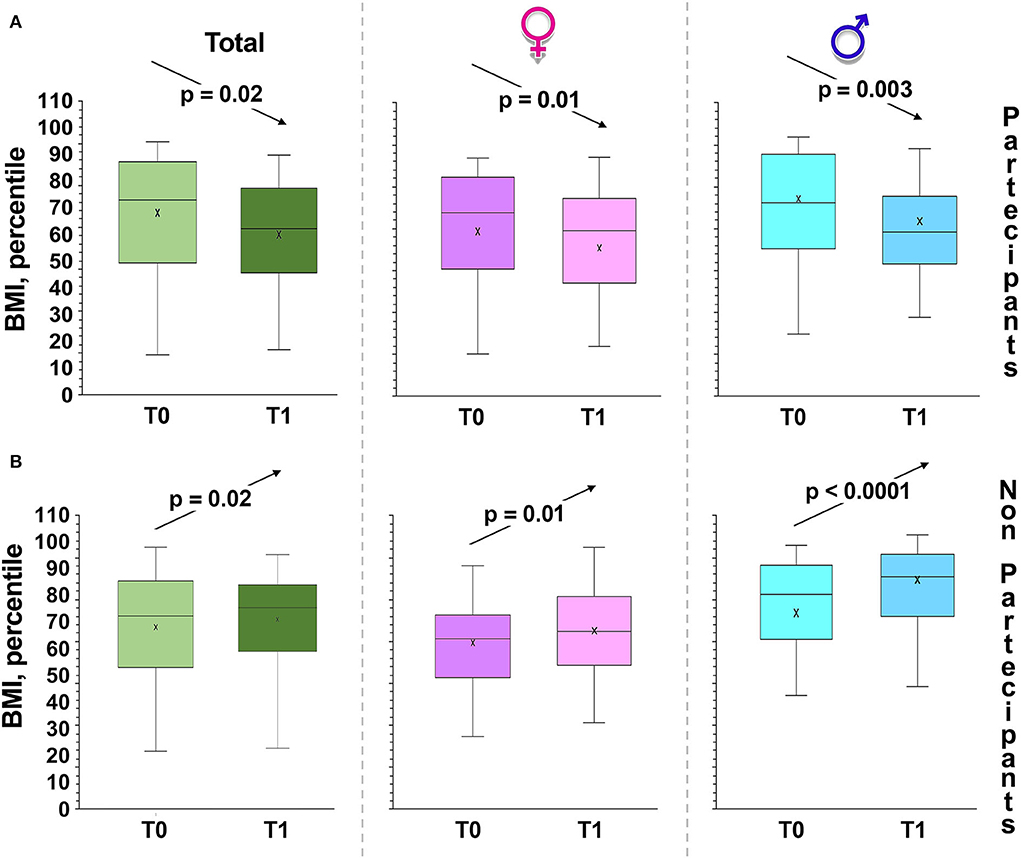
Figure 2. Changes in BMI, percentile over time. Box and whiskers representation of body mass index (BMI: weight in kilograms divided by height in meters squared) of intervention group (A) and control children (B), recorded at baseline (T0), at 6 months from baseline (T1, at the completion of the intervention). The sample was also divided between girls and boys. In this representation, the central box covers the middle 50% of the data values, between the upper and lower quartiles. The bars extend out to the extremes, while the central line is at the median. p-values were obtained by Student's paired t-test.
As regards the detection of percentiles in the different age groups, we have highlighted that overweight and obesity in children increased with age (Figure 2). In fact, before our educative intervention, 18.5% of the children were underweight. We also highlighted significant differences between the proportions of overweight, underweight, normal weight, or obese children before and after intervention in the experimental group (Figure 2; χ2, p = 0.0001).
The most striking results were obtained in females, since girls with obesity were no longer detectable after intervention (Figure 3).
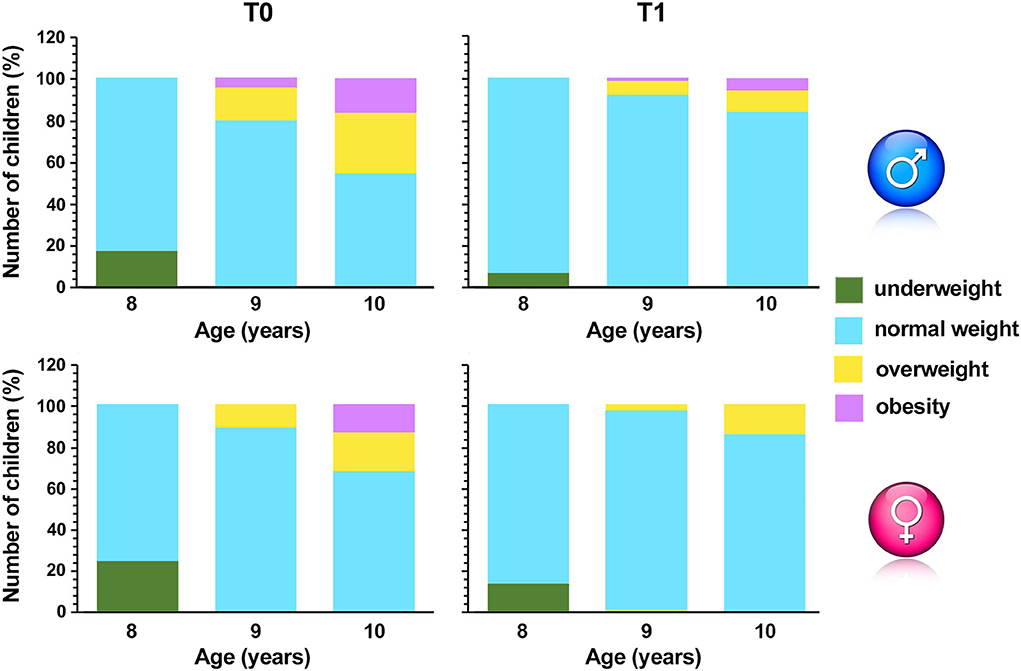
Figure 3. Percentage of overweight, underweight, normal weight or with obesity children pre (T0) and post (T1) intervention. The sample was also divided between girls and boys and different age groups.
Another indicator of obesity was also measured; in the experimental group, the waist circumference substantially declined (p < 0.001) (Figure 4A). In contrast, in the group that is not participating in the intervention, waist circumference significantly increases, especially in boys (Figure 4B).
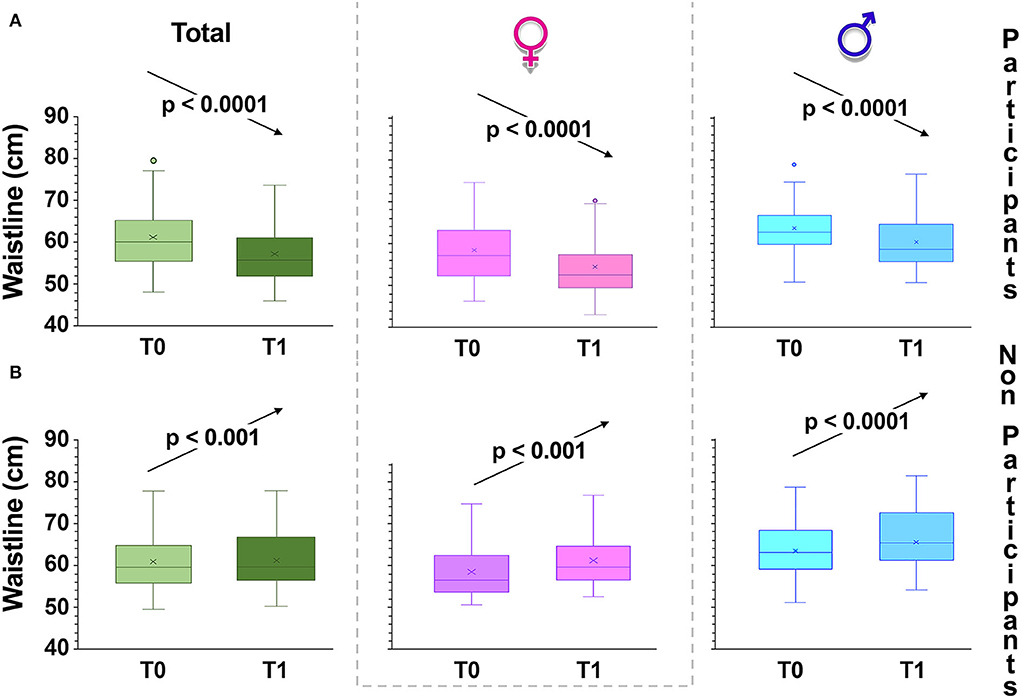
Figure 4. Changes in waist circumference over time. Box and whiskers representation of waist circumference of intervention group (A) and control children (B), recorded at baseline (T0) and 6 months from baseline (T1, at the completion of the intervention). The sample was also divided according to gender. In this representation, the central box covers the middle 50% of the data values, between the upper and lower quartiles. The bars extend out to the extremes, while the central line is at the median. Those values which are beyond 1.5 times the interquartile range beyond the central box are plotted as individual points. p-values were obtained by Student's paired t-test.
WHR also includes height and is, in normal-weight children as well, an important indicator of excess upper body fat (37). Hence, WHR allows to identify children at risk of developing metabolic complications (39), with a cut-off value greater than 0.500 (37, 40). In T1, mean WHR decreased from 0.43 ± 0.06 to 0.41 ± 0.03 (p < 0.001) (males: 0.45 ± 0.013; to 0.42 ± 0.01; p < 0.01; females from 0.42 ± 0.03 to 0.41 ± 0.03; p < 0.05) in the participating group, while it remained unchanged in the control group. Furthermore, the number of children who had a ratio >0.50 in T0 also decreased significantly (χ2, p = 3.46·10−5).
Questionnaire results
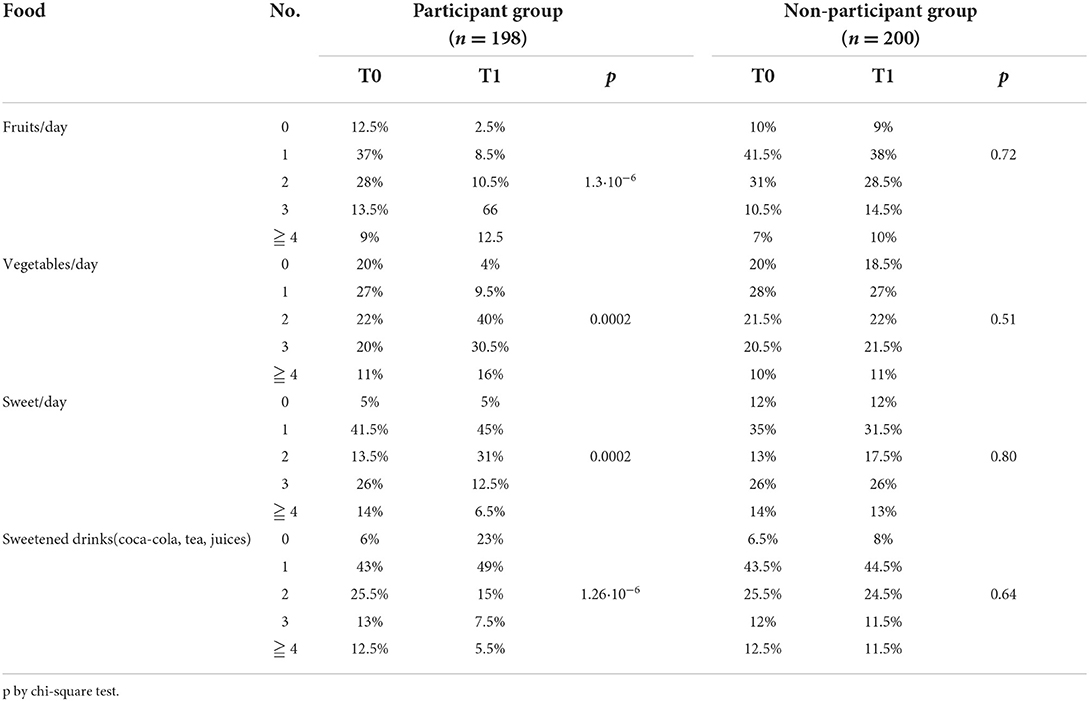
The data collected in T0 and T1 using the questionnaires were analyzed by extrapolating the frequency of each item considered in the proposed survey and presented as a percentage (Tables 2, 3). Our questionnaires show that only 42% of our population (n = 398) ate breakfast regularly. A more equal distribution of the mid-morning meal was observed, with 32.6% “yes,” 35.6% “sometimes,” and 31.8% “no” (Table 2). An afternoon snack was consumed by 79% of the children (Table 2). The first choice was sweets for both midmorning and afternoon snack (48.5 and 52.25%, respectively), among biscuits, chips, and cold cuts (Table 2).
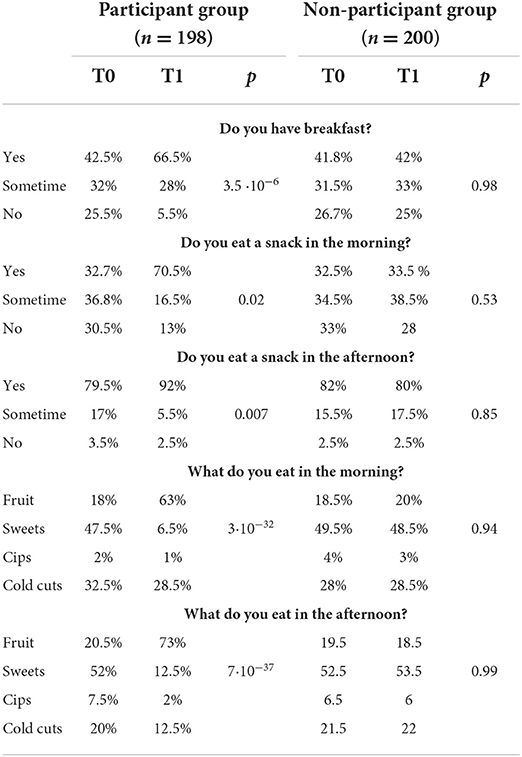
Table 2. Changes in dietary parameters after lifestyle intervention in children (p by chi-square test).
Since one of the lifestyle-related risk factors of being overweight is skipping breakfast (41, 42), we have considered this risk factor as an objective of our preventive program. In T0 the children who never had breakfast were 25.5% of the participating group and after the intervention (T1) this percentage dropped to 5.5%. Consistently, the children who reported having breakfast every day in T0 were 42.5% and this had increased to 66.5% in T1 (χ2 = 33.156, p < 0.0001). The children in the control group maintained the same percentages (Table 2).
In T0, while as mentioned earlier there was an equal distribution of the mid-morning snack, the afternoon snack was consumed by 80.8% of children (Table 2). In T1, the children of the experimental group who eat a snack in midmorning and, in the afternoon, increased further (Table 2; χ2 = 5.302, p = 0.020, χ2 = 9.453, p = 0.007, respectively).
Among fruit, chips, and cold cuts, the first choice for a midmorning (48%) or afternoon snack (52%) was sweets (Table 2). In T1, children in the experimental group preferred to eat fruit for both snacks (Table 2; χ2 = 10.805, p < 0.0001, χ2 = 16.133, p < 0.0001, respectively).
An important aspect of the food education program was to consume healthy and complete meals consisting of a first course, second course, vegetables, and fruits. From the data analysis, it emerged that 80% of the population consumes vegetables almost every day; and even 20% never eat vegetables (Table 3). After our intervention, the consumption of vegetables increased significantly among the children participating in the program (Table 3; χ2 = 9.311, p = 0.0002). Although experts advise against them, 12.5% of children drink sugar-added and non-nutritious drinks every day (Table 3). In T1 this percentage decreases significantly, in the experimental group; in addition, 23% of children no longer drink sugar-added drinks (Table 3; p = 0.0001).
Discussion
As the number of overweight and obese children has increased in recent decades, the need to support healthy nutrition and physical activity in children has never been more urgent.
Thus, the present study aims to investigate the effectiveness of an education program, regarding correct eating habits on children's weight status.
In Europe, higher levels of children overweight and obesity have been reported in southern countries (42), particularly for those children growing up in low-income families (43). This socio-economic variability of childhood obesity and its relationships with lifestyle has also been reported in Italy (44), with prevalence higher in southern regions where socio-economic conditions are worse than those in northern regions (45). Following the recommendations of the WHO European Ministerial Conference on the fight against obesity (46), the Italian Minister of Health financed the National Nutritional Surveillance System called “OKkio alla SALUTE” (47, 48), which made it possible to make comparisons between Italian countries within the European Region (49).
In our study, we find that the number of overweight students was about 20% (22% of males and 18.5% of females), a percentage which is in line with what was previously reported for our region (49). More precisely, the percentages of 11-year-old students who were overweight were: males 14.5, 21.3, and 28.5%; females 11.6, 13.5, and 21.1% in the north, center, and south of the country, respectively (47–49). The percentage of obesity reported here is also in agreement with Lauria's study (49): 12% and 6% for males and females, respectively. It is interesting to note that the percentages of children with overweight and obesity increased significantly from 8 to 10 years.
Since this study was conducted from 2017 to 2018, these higher rates of obesity are not caused by the COVID-19 pandemic-dependent lockdown but were due to pre-existing socio-economic conditions and other health indicators.
In childhood obesity, the inadequate intake of fruit and vegetables and the consumption of too many high-calorie snacks play a very important role, with 41% of total calories coming from chips, chocolate bars, soft drinks, fruit drinks, sugars, syrups, preserves, fats, and oils (50).
As known, family, friends, school, marketing, and the media influence children's food choices. To prevent childhood obesity, it is useful to combine family and school programs and nutrition education with adequate physical activity (21). Habits that protect against childhood obesity include having breakfast and eating family meals and being physically active. In this context, we examined the effects of a 6-month pilot intervention on students from schools located in two small towns with similar socio-economic conditions. This intervention had the aim of educating on a healthy diet according to the dictates of the Mediterranean diet (especially breakfast, mid-morning snacks, and fruit-based afternoon snack; vegetables for lunch and dinner; drinking water instead of sugary drinks) and to carry out at least 60 min of physical activity per day.
An important source of primary nutrients in the diet of both adults and young people is breakfast (51–53), which has been shown to be able to produce many benefits (53). Daily breakfast consumption also has a protective action against obesity and overweight (54) with a clear inverse association with body fat (55). Indeed, obese children have been reported to skip breakfast (42, 55, 56) and had a high risk of chronic diseases, such as type 2 diabetes (57), dyslipidemia, or cardiovascular disease (54). Finally, breakfast consumption also has a positive effect on children's cognitive performance (58). Unfortunately, in agreement with previous studies (59, 60), only 42.5% of children said they had breakfast every day. In T1, however, this percentage increased to 66.5%.
We suggested that the children eat five meals a day, introducing the consumption of mid-morning and afternoon snacks into their diet. Some healthy eating habits were acquired in most cases: eating fruit as a midmorning and afternoon snacks and avoiding the consumption of cold cuts and sweet foods. It is worth noting that 63% and 73% of children chose fruits for morning and afternoon snacks respectively, and 78.5 ate fruits more than three times a day. These results showed better percentages than the international data of “NCD Risk Factor Collaboration (NCD-RisC) (1),” in which 35.4% of adolescents (aged 11–15) consumed at least one portion of fruit daily, and 27.3% ate vegetables at least once a day (1). On the contrary, 18% of adults treated in the Obesity Unit of Hospital of Torino reported a decrease in fruits and vegetables consumption during the COVID lockdown (61).
Therefore, our intervention gave an encouraging result within a scenario in which foods rich in fibers have been replaced by products rich in fat and sugars, with a high level of processing (62). Most of these products contain additives to make them durable and hyper-palatable. However, they have very low nutritional quality, and their consumption tends to limit the consumption of unprocessed or minimally processed foods (63). Consumption of ultra-processed foods has been pointed out as a risk factor for increasing obesity, as measured by BMI, among children, adolescents, and adults (41).
The present study has some limitations, primarily the different ages of the participants. However, the weight loss was substantial as well some lifestyle indicators have undergone significant improvements. Another limitation of the present study is the lack of data on the socio-economic, cultural, and educational levels of parents. Larger studies with long-term follow-up are therefore needed to corroborate our findings.
Conclusion
We evaluated the effect of a 6-month-long intervention on lifestyle and diet quality in schools in Southern Italy. The children and adolescents participating in the study achieved a reduction in BMI, waist circumference, and better adherence to nutritional recommendations assessed by the diet quality indices. The school intervention program represents an effective strategy for preventing the problem of childhood overweight and obesity.
Data availability statement
The datasets presented in this article are not readily available because of participant privacy. Requests to access the datasets should be directed to YW50b25lbGxhLm11c2NlbGxhQHVuaXNhbGVudG8uaXQ=.
Ethics statement
The studies involving human participants were reviewed and approved by IRB of Department of Biological and Environmental Science and Technologies (DiSTeBA), University of Salento, Via Prov. le Lecce-Monteroni, 73100 Lecce, Italy. Written informed consent to participate in this study was provided by the participants' legal guardian/next of kin.
Author contributions
AM, VC, and SM: conceptualization. ADM, VC, AM, and SM: data curation. VC, GM, and ADM: investigation. AM and SM: project administration and original draft. AM: supervision and writing. SM: writing—review and editing. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128.9 million children, adolescents, and adults. Lancet. (2017) 390:2627–42. doi: 10.1016/S0140-6736(17)32129-3
2. Biro FM, Wien M. Childhood obesity and adult morbidities. Am J Clin Nutr. (2010) 91:1499–505. doi: 10.3945/ajcn.2010.28701B
3. Reinehr T, Tittel SR, Holle R, Wiegand S, Gellhaus I, Hebebrand J, et al. Comparison of cardiovascular risk factors between children and adolescents with classes III and IV obesity: findings from the APV cohort. Int J Obes (Lond). (2021) 45:1061–73. doi: 10.1038/s41366-021-00773-x
4. Nejat EJ, Polotsky AJ, Pal L. Predictors of chronic disease at midlife and beyond—the health risks of obesity. Maturitas. (2010) 65:106–11. doi: 10.1016/j.maturitas.2009.09.006
5. Guh DP, Zangh W, Bansback N, Amarsi Z, Birmingham CL, Anis AH, et al. The incidence of co-morbidities related to obesity and overweight: a systematic review and meta-analysis. BMC Public Health. (2009) 9:88. doi: 10.1186/1471-2458-9-88
6. Van Kruijsdijk RC, Van der Wall E, Visseren FL. Obesity and cancer: the role of dysfunctional adipose tissue. Cancer Epidemiol Biomarkers Prev. (2009) 18:2569–78. doi: 10.1158/1055-9965.EPI-09-0372
7. Li K, Haynie D, Lipsky L, Palla H, Iannotti RJ, Simons-Morton B, et al. Assessment of adolescent weight status: similarities and differences between CDC, IOTF, and WHO references. Prev Med. (2016) 87:151–4. doi: 10.1016/j.ypmed.2016.02.035
8. Ingle L, Sleap M, Tolfrey K. The effect of a complex training and detraining programme on selected strength and power variables in early pubertal boys. J Sports Sci. (2006) 24:987–97. doi: 10.1080/02640410500457117
9. Van der Heijden GJ, Wang ZYJ, Chu ZL. Strength exercise improves muscle mass and hepatic insulin sensitivity in obese youth. Med Sci Sports Exerc. (2010) 42:1973–80. doi: 10.1249/MSS.0b013e3181df16d9
10. Kim J, Lim H. Nutritional management in childhood obesity. J Obes Metab Syndr. (2019) 28:225–35. doi: 10.7570/jomes.2019.28.4.225
11. Nishtar S, Gluckman P, Armstrong T. Ending childhood obesity: a time for action. Lancet. (2016) 387:825–7. doi: 10.1016/S0140-6736(16)00140-9
12. Hörmann-Wallner M, Krause R, Alfaro B, Jilani H, Laureati M, Almli VL, et al. Intake of fibre-associated foods and texture preferences in relation to weight status among 9-12 years old children in 6 European countries. Front Nutr. (2021) 18:633807. doi: 10.3389/fnut.2021.633807
13. Giménez-Legarre N, Miguel-Berges ML, Flores-Barrantes P, Santaliestra-Pasías AM, Moreno LA. Breakfast characteristics and its association with daily micronutrients intake in children and adolescents-a systematic review and meta-analysis. Nutrients. (2020) 12:3201. doi: 10.3390/nu12103201
14. Heald FP. Fast food and snack food: beneficial or deleterious. J Adolesc Health. (1992) 13:380–3. doi: 10.1016/1054-139X(92)90033-8
15. Albertini A, Tripodi A, Fabbri A, Mattioli M, Cavrini G, Cecchetti R, et al. Prevalence of obesity in 6- and 9-year-old children living in Central-North Italy Analysis of determinants and indicators of risk of overweight. Obes Rev. (2008) 9:4–10. doi: 10.1111/j.1467-789X.2007.00414.x
16. Pagani LS, Fitzpatrick C, Barnett TA, Dubow E. Prospective associations between early childhood television exposure and academic, psychosocial, and physical well-being by middle childhood. Arch Pediatr Adolesc Med. (2010) 164:425–31. doi: 10.1001/archpediatrics.2010.50
17. Eichinger M, Schneider S, De Bock F. Subjectively and objectively assessed social and physical environmental correlates of preschoolers' accelerometer-based physical activity. Int J Behav Nutr Phys Act. (2017) 14:153. doi: 10.1186/s12966-017-0577-9
18. Hills AP, Andersen LB, Byrne NM. Physical activity and obesity in children. Br J Sports Med. (2011) 45:866–70. doi: 10.1136/bjsports-2011-090199
19. Reilly JJ, Hughes AR, Gillespie J, Malden S, Martin A. Physical activity interventions in early life aimed at reducing later risk of obesity and related non-communicable diseases: a rapid review of systematic reviews. Obes Rev. (2019) 20 Suppl 1:61–73. doi: 10.1111/obr.12773
20. Battaglia G, Giustino V, Tabacchi G, Lanza M, Schena F, Biino V, et al. Interrelationship between age, gender, and weight status on motor coordination in Italian children and early adolescents aged 6-13 years old. Front Pediatr. (2021) 965:738294. doi: 10.3389/fped.2021.738294
21. Tabacchi G, Battaglia G, Alesi M, Paoli A, Palma A, Bellafiore M, et al. Food literacy predictors and associations with physical and emergent literacy in pre-schoolers: results from the training-to-health project. Public Health Nutr. (2020) 23:356–65. doi: 10.1017/S1368980019002404
22. Obradovic Salcin L, Karin Z, Miljanovic Damjanovic V, Ostojic M, Vrdoljak A, Gilic B, et al. Physical activity, body mass, and adherence to the Mediterranean diet in preschool children: a cross-sectional analysis in the split-Dalmatia county (Croatia). Int J Environ Res Public Health. (2019) 16:3237. doi: 10.3390/ijerph16183237
23. Bonavolontà V, Cataldi S, Maci D, Fischetti F. Physical activities and enjoyment during the lockdown: effect of home-based supervised training among children and adolescents. J Human Sport Exerc. (2020) 15:1338–43. doi: 10.14198/jhse.2020.15.Proc4.31
24. Ojeda-Rodríguez A, Morell-Azanza L, Azcona-Sanjulián MC, Martínez JA, Ramírez MJ, Marti A, et al. Reduced serotonin levels after a lifestyle intervention in obese children: association with glucose and anthropometric measurements. Nutr Hosp. (2018) 35:279–85. doi: 10.20960/nh.1439
25. Morell-Azanza L, García-Calzón S, Rendo-Urteaga T, Martin-Calvo N, Chueca M, Martínez JA, et al. Serum oxidized low-density lipoprotein levels are related to cardiometabolic risk and decreased after a weight loss treatment in obese children and adolescents. Pediatr Diabetes. (2016) 18:392–8. doi: 10.1111/pedi.12405
26. De Miguel-Etayo P, Moreno LA, Santabarbara J, Martín-matillas M, Piqueras MJ, Rocha-silva D, et al. Anthropometric indices to assess body-fat changes during a multidisciplinary obesity treatment in adolescents: EVASYON Study. Clin Nutr. (2015) 34:523–8. doi: 10.1016/j.clnu.2014.06.004
27. Latino F, Greco G, Fischetti F, Cataldi S. Multilateral training improves body image perception in female adolescents. J Hum Sport Exerc. (2019) 14(Proc4):S927–36. doi: 10.14198/jhse.2019.14.Proc4.55
28. Waling M, Lind T, Hernell O, Larsson CA. one-year intervention has modest effects on energy and macronutrient intakes of overweight and obese Swedish children. J Nutr. (2010) 140:1793–8. doi: 10.3945/jn.110.125435
29. Waling M, Larsson C. Improved dietary intake among overweight and obese children followed from 8 to 12 years of age in a randomised controlled trial. J Nutr Sci. (2012) 1:1–11. doi: 10.1186/s13052-022-01205-w
30. Nicolucci A, Maffeis C. The adolescent with obesity: what perspectives for treatment? Ital J Pediatr. (2022) 48:9.
31. Beamish AJ, Reinehr T. Should bariatric surgery be performed in adolescents? Eur J Endocrinol. (2017) 176:D1–D15. doi: 10.1530/EJE-16-0906
32. Knop C, Singer V, Uysal Y, Schaefer A, Wolters B, Reinehr T, et al. Extremely obese children respond better than extremely obese adolescents to lifestyle interventions. Pediatr Obes. (2015) 10:7–14. doi: 10.1111/j.2047-6310.2013.00212.x
33. Greco G, Cataldi S, Fischetti F. Karate as anti-bullying strategy by improvement resilience and self-efficacy in school-age youth. J Phys Educ Sport. (2019) 19:1863–70. doi: 10.7752/jpes.2019.s5276
34. Von Hippel PT, Powell B, Downey DB, Rowland NJ. The effect of school on overweight in childhood: gain in body mass index during the school year and during summer vacation. Am J Public Health. (2007) 97:696–702. doi: 10.2105/AJPH.2005.080754
35. Ip P, Ho FK, Louie LH, Chung TW, Cheung YF, Lee SL, et al. Childhood obesity and physical activity friendly school environments. J Pediatr. (2017) 191:110–6. doi: 10.1016/j.jpeds.2017.08.017
36. Claver F, Jiménez R, Gil-Arias A, Moreno A, Moreno MP. The cognitive and motivation intervention program in youth female volleyball players. J Hum Kinet. (2017) 59:55–65. doi: 10.1515/hukin-2017-0147
37. McCarthy HD, Ashwell M. A study of central fatness using waist-to-height ratios in UK children and adolescents over two decades supports the simple message–'keep your waist circumference to less than half your height'. Int J Obes (Lond). (2006) 30:988–92. doi: 10.1038/sj.ijo.0803226
38. Kuczmarski RJ, Ogden CL, Grummer-Strawn LM, Flegal KM, Guo SS, Wei RCDC, et al. growth charts: United States. Adv Data. (2000) 8:1–27.
39. McCarthy HD, Jarrett KV, Crawley HF. The development of waist circumference percentiles in British children aged 5.0–16.9 y. Eur J Clin Nutr. (2001) 55:902–7. doi: 10.1038/sj.ejcn.1601240
40. Zhu Y, Shao Z, Jing J, Ma J, Chen Y, Li X, et al. Body mass index is better than other antropometric indices for identifyng dislipidemia in chinese children with obesity. PLoS ONE. (2016) 11:e0149392. doi: 10.1371/journal.pone.0149392
41. Costa CS, Del-Ponte B, Assunção MCF, Santos IS. Consumption of ultra-processed foods and body fat during childhood and adolescence: a systematic review. Public Health Nutr. (2018) 21:148–59. doi: 10.1017/S1368980017001331
42. Duncan JS, Schofield G, Duncan EK, Rush EC. Risk factors for excess body fatness in New Zealand children. Asia Pac J Clin Nutr. (2008) 17:138–47.
43. Rossen LM, Schoendorf KC. Measuring health disparities: trends in racialethnic and socioeconomic disparities in obesity among 2- to 18-year old youth in the United States, 2001-2010. Ann Epidemiol. (2012) 22:698–704. doi: 10.1016/j.annepidem.2012.07.005
44. Lauria L, Spinelli A, Cairella G, Censi L, Nardone P, Buoncristiano M, et al. 2015 Dietary habits among children aged 8-9 years in Italy. Ann Ist Super Sanita. (2012) 51:371–81. doi: 10.4415/ANN_15_04_20
45. Nardone P, Spinelli A, Lauria L, Buoncristiano M, Bucciarelli M, Galeone D, et al. Sociodemographic variation in childhood overweight and obesity in Italy in 2014. Epidemiol Prev. (2015) 39:64.
46. WHO. European Ministerial Conference. WHO on Counteracting Obesity. Report of a WHO conference. Geneva: World Health Organization (2007). p. 1–30.
47. Binkin N, Fontana G, Lamberti A, Cattaneo C, Baglio G, Perra AA, et al. national survey of the prevalence of childhood overweight and obesity in Italy. Obes Rev. (2010) 11:2–10. doi: 10.1111/j.1467-789X.2009.00650.x
48. Spinelli A, Baglio G, Cattaneo C, Fontana G, Lamberti A. Promotion of healthy lifestyle and growth in primary school children (OKkio alla SALUTE). Ann Ig. (2008) 20:337–44.
49. Lauria L, Spinelli A, Buoncristiano M, Nardone P. Decline of childhood overweight and obesity in Italy from 2008 to 2016: results from 5 rounds of the population-based surveillance system. BMC Public Health. (2019) 19:618. doi: 10.1186/s12889-019-6946-3
50. Roblin L. Childhood obesity: food, nutrient, and eating-habit trends and influences. Appl Physiol Nutr Metab. (2007) 32:635–45. doi: 10.1139/H07-046
51. O'Neil A, Quirk SE, Housden S, Brennan SL, Williams LJ, Pasco JA, et al. Relationship between diet and mental health in children and adolescents: a systematic review. Am J Public Health. (2014) 104:e31–42. doi: 10.2105/AJPH.2014.302110
52. Szajewska H, Ruszczynski M. Systematic review demonstrating that breakfast consumption influences body weight outcomes in children and adolescents in Europe. Crit Rev Food Sci Nutr. (2010) 50:113–9. doi: 10.1080/10408390903467514
53. Coulthard JD, Palla L, Pot GK. Breakfast consumption and nutrient intakes in 4-18-year-olds: UK National Diet and Nutrition Survey Rolling Programme (2008-2012). Br J Nutr. (2017) 118:280–90. doi: 10.1017/S0007114517001714
54. Monzani A, Ricotti R, Caputo M, Solito A, Archero F, Bellone S, et al. Systematic review of the association of skipping breakfast with weight and cardiometabolic risk factors in children and adolescents. What should we better investigate in the future? Nutrients. (2019) 11:387. doi: 10.3390/nu11020387
55. Gilardini L, Croci M, Pasqualinotto L, Caffetto K, Invitti C. Dietary habits and cardiometabolic health in obese children. Obes Facts. (2015) 8:101–9. doi: 10.1159/000381157
56. Karatzi K, Moschonis G, Choupi E, Manios Y. Late-night overeating is associated with smaller breakfast, breakfast skipping, and obesity in children: The Healthy Growth Study. Nutrition. (2017) 33:141–4. doi: 10.1016/j.nut.2016.05.010
57. Donin AS, Nightingale CM, Owen CG, Rudnicka AR, Perkin MR, Jebb SA, et al. Regular breakfast consumption and type 2 diabetes risk markers in 9- to 10-year-old children in the child heart and health study in England (CHASE): a cross-sectional analysis. PLoS Med. (2014) 11:e1001703. doi: 10.1371/journal.pmed.1001703
58. Rampersaud GC. Benefits of breakfast for children and adolescents: update and recommendations for practitioners. Am J Lifestyle Med. (2009) 3:86–103. doi: 10.1177/1559827608327219
59. Adolphus K, Lawton CL, Champ CL, Dye L. The effects of breakfast and breakfast composition on cognition in children and adolescents: a systematic review. Adv Nutr. (2016) 7:590S−612S. doi: 10.3945/an.115.010256
60. Vereecken C, Dupuy M, Rasmussen M, Kelly C, Nansel TR, Al Sabbah H, et al. Breakfast consumption and its socio-demographic and lifestyle correlates in schoolchildren in 41 countries participating in the HBSC study. Int J Public Health. (2009) 54:180–90. doi: 10.1007/s00038-009-5409-5
61. Pellegrini M, Ponzo V, Rosato R, Scumaci E, Goitre I, Benso A, et al. Changes in weight and nutritional habits in adults with obesity during the “lockdown” period caused by the COVID-19 virus emergency. Nutrients. (2020) 12:2016. doi: 10.3390/nu12072016
62. Popkin BM. Global nutrition dynamics: the world is shifting rapidly toward a diet linked with noncommunicable diseases. Am J Clin Nutr. (2006) 84:289–98. doi: 10.1093/ajcn/84.2.289
Keywords: children obesity, overweight, BMI, waist circumference, school-based intervention
Citation: Marsigliante S, Ciardo V, Di Maglie A, My G and Muscella A (2022) Efficacy of school-based intervention programs in reducing overweight: A randomized trial. Front. Nutr. 9:1001934. doi: 10.3389/fnut.2022.1001934
Received: 24 July 2022; Accepted: 31 August 2022;
Published: 29 September 2022.
Edited by:
Badicu Georgian, Transilvania University of Braşov, RomaniaReviewed by:
Eduardo Melguizo Ibáñez, Universidad Granada, SpainGiuseppe Battaglia, University of Palermo, Italy
Zeki Akyildiz, Gazi University, Turkey
Copyright © 2022 Marsigliante, Ciardo, Di Maglie, My and Muscella. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Antonella Muscella, YW50b25lbGxhLm11c2NlbGxhQHVuaXNhbGVudG8uaXQ=
 Santo Marsigliante
Santo Marsigliante Vito Ciardo1
Vito Ciardo1 Antonio Di Maglie
Antonio Di Maglie Antonella Muscella
Antonella Muscella