
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Nutr., 12 November 2021
Sec. Eating Behavior
Volume 8 - 2021 | https://doi.org/10.3389/fnut.2021.774328
This article is part of the Research TopicThe Effects of the COVID-19 Outbreak on Food Supply, Dietary Patterns, Nutrition and Health: Volume 2View all 11 articles
 Tham T. Nguyen1†
Tham T. Nguyen1† Minh H. Nguyen2†
Minh H. Nguyen2† Thu T. M. Pham1,3
Thu T. M. Pham1,3 Vinh-Tuyen T. Le4,5
Vinh-Tuyen T. Le4,5 Tan T. Nguyen6,7
Tan T. Nguyen6,7 Thuc C. Luong8,9
Thuc C. Luong8,9 Binh N. Do10,11
Binh N. Do10,11 Hung K. Dao12
Hung K. Dao12 Huu C. Nguyen13,14
Huu C. Nguyen13,14 Tung H. Ha15
Tung H. Ha15 Linh V. Pham16,17
Linh V. Pham16,17 Phuoc B. Nguyen18
Phuoc B. Nguyen18 Hoai T. T. Nguyen19
Hoai T. T. Nguyen19 Thinh V. Do20
Thinh V. Do20 Hung Q. Nguyen21
Hung Q. Nguyen21 Manh V. Trinh22
Manh V. Trinh22 Thuy T. Le23,24
Thuy T. Le23,24 Anh L. Tra25
Anh L. Tra25 Thao T. P. Nguyen26
Thao T. P. Nguyen26 Kien T. Nguyen27
Kien T. Nguyen27 Dung T. Phan28,29
Dung T. Phan28,29 Khue M. Pham1,30
Khue M. Pham1,30 Chyi-Huey Bai2,3,31
Chyi-Huey Bai2,3,31 Tuyen Van Duong32*
Tuyen Van Duong32*Background: The COVID-19-induced lockdown has been implemented in many countries, which may cause unfavorable changes in lifestyles and psychological health. People's health literacy, healthy diet, and lifestyles play important roles in mitigating the negative impacts of the pandemic. Therefore, we aimed to examine associations of COVID-19 lockdown with changes in eating behavior, physical activity, and mental health; and the modification effects by digital healthy diet literacy (DDL) and eHealth literacy (eHEALS) on the associations.
Methods: We conducted an observational study on 4,348 outpatients from 7th April to 31st May 2020. Data from 11 hospitals in Vietnam included demographic characteristics, DDL, eHEALS, eating behavior, physical activity, and mental health changes. Multiple logistic regression and interaction models were performed to examine associations.
Results: Patients under lockdown had a lower likelihood of having “unchanged or healthier” eating behavior (odds ratio, OR, 0.38; 95% confidence interval, 95%CI, 0.29 to 0.51; p < 0.001), “unchanged or more” physical activity (OR, 0.79; 95% CI, 0.69 to 0.90; p < 0.001), and “stable or better” mental health (OR, 0.77; 95% CI, 0.67 to 0.89; p < 0.001), as compared to those after lockdown. In interaction models, as compared to patients after lockdown and with the lowest DDL score, those under lockdown and with a one-score increment of DDL had a higher likelihood of having “unchanged or healthier” eating behavior (OR, 1.05; 95% CI, 1.02 to 1.07; p < 0.001), and “stable or better” mental health (OR, 1.02; 95% CI, 1.01 to 1.04; p < 0.001). Similarly, as compared to patients after lockdown and with the lowest eHEALS score, those under lockdown and with a one-score increment of eHEALS had a higher likelihood of having an “unchanged or more” physical activity (OR, 1.03; 95% CI, 1.01 to 1.05; p < 0.001).
Conclusion: The COVID-19 lockdown measure could negatively affect eating behavior, physical activity, and mental health among outpatients. Better DDL and eHEALS were found to mitigate the negative impacts of the lockdown, which may empower outpatients to maintain healthy lifestyles and protect mental health. However, this study holds several limitations that may undermine the certainty of reported findings.
New waves of COVID-19 outbreaks continuously re-emerged in many countries around the world (1, 2). Although vaccination programs have been deployed globally, the disproportionate distribution of vaccines (3, 4) and the emergence of new COVID-19 variants make the pandemic still uncontrolled (5, 6). Affected countries have been applying strict prevention measures such as lockdown, home confinement, and social distancing (7). Although these measures have effectively prevented the spread of the virus, it causes significant changes in people's lives, including working from home and lack of connection with family and friends (8, 9). In addition, lockdown or home confinement measures make people feel bored and isolated, negatively affecting their psychological health (10, 11). These adverse impacts on mental health can cause harmful lifestyle changes such as increasing unhealthy eating habits (12–15), sedentary behavior, or sleeping disorders (16). Recent literature also indicated that the isolation and COVID-19 lockdown had negative impacts on eating habits and emotional processing (17, 18). Furthermore, movement restrictions and difficulty accessing fresh food during the lockdown period could significantly affect people's eating patterns and physical activity habits (19–25). Therefore, it is urgent to assess the impacts of COVID-19 lockdown on changes in eating behavior, physical activity, and mental health and find protective factors that could mitigate such impacts.
The advent of the Internet and the advancement of smartphones and computer technology make it easier for people to access health information (26, 27). People could use and access web-based resources at any time to seek health advice, disease information, and check physician's consultation (28, 29). However, accessing health information and support through the Internet also has potential risks. With the ease of delivering health information through social networks and websites, it is difficult for people to recognize and evaluate which information is high-quality and reliable (30). Notably, the COVID-19 pandemic has caused an “infodemic” with a plethora of false and fake news about the disease (31, 32). This information could lead to worry and fear in the community, distrust in the government's epidemic containment efforts, and wrong health decisions (33–35). Therefore, improving skills to find, evaluate, and understand health information on the Internet is essential, especially during the COVID-19 lockdowns.
Digital healthy diet literacy (DDL) and eHealth literacy (eHEALS) have potential impacts in improving healthy lifestyles and general health during the pandemic. DDL is the ability to find, understand, evaluate, and apply healthy eating information from web-based sources to improve the eating behaviors” (36). Meanwhile, eHEALS is defined as the capacity to seek, understand, and appraise online health information and apply it to solve health issues (37). Recent literature showed that DDL was found to be associated with a higher likelihood of healthier eating, better mental health, and quality of life during the pandemic (36, 38, 39). Meanwhile, people with higher eHEALS were more likely to have better psychological health, engage in positive health-related behaviors (e.g., healthy eating, physical activity) (40–43). In addition, previous research also indicated that DDL and eHEALS could help to mitigate the negative impacts of COVID-19 on quality of life among outpatients (39). Therefore, DDL and eHEALS roles should be investigated and paid more attention to in the lockdown period.
During the pandemic, people seeking medical care have faced many challenges, such as limited access to medical care, delays in treatment, fear of COVID-19 infection, and worry about their health (35, 44, 45). As a result, maintaining healthy lifestyles and stabilizing mental health is essential to improve their health and overcome difficulties, especially in the lockdown period (46). Therefore, we conducted this study to examine the associations of COVID-19 induced lockdown with changes in eating behavior, physical activity, and mental health; and further determine whether DDL and eHEALS could modify these associations among outpatients from 11 hospitals across Vietnam.
A cross-sectional survey was conducted in outpatients from eleven hospitals across Vietnam. Participants were recruited at selected hospitals using the convenience sampling method from 7th April to 31st May 2020. The Vietnamese Government announced a nationwide lockdown from 1 to 22 April to contain the spread of the COVID-19 pandemic (47, 48). During the lockdown period, all people are ordered not to leave their homes except for emergency cases, buying essential goods or medicine, and are prohibited from gathering more than two people in public. If going outside, people must wear a mask and keep a safe distance of two meters from others. The stringent social distancing and isolation measures yielded positive results, and no confirmed COVID-19 cases were recorded in Vietnam from mid-April to the end of May 2020 (49). After 22 April 2020, Vietnam began to gradually lift strict movement restrictions, including allowing businesses activities and schools in many parts of Viet Nam to re-open, and resuming domestic travel across the country. However, epidemic prevention measures continued to be implemented according to the “5K Rule” of the Vietnam Ministry of Health, including wearing a mask when going out, washing hands regularly with soap or sanitizer, keeping a safe distance from others, not gathering in crowds, and making a medical declaration (50).
Due to a convenience sample, we aimed to recruit as many participants as possible to reduce the sampling bias and increase the representativeness of the sample. Inclusion criteria were those who visited the outpatient department (OPD) of studied hospitals at the time of this study, aged 18–85, without emergency conditions (e.g., stroke, traumatic brain injury, etc.), and who agreed to participate in the survey. In addition, we excluded patients who had communication difficulties (e.g., deafness or blindness). Finally, we collected and analyzed the data of 4,348 participants. Figure 1 showed the number of patients at each hospital participating in this study (39).
This study was approved by the Ethics Committee of Hanoi University of Public Health (IRB Number: 133/2020/YTCC-HD3).
At OPDs of studied hospitals, research assistants (physicians, nurses, and healthcare students) informed patients about the purposes of this study and invited them to participate in the investigation. Informed consent forms were signed before participants carried out the survey. Data was obtained through structured self-administered questionnaires. During the waiting time for examination, participants could take the survey using their smartphone to fill out the online questionnaire via QR code or the printed ones provided at OPDs. The online and printed versions of the questionnaire have the same structure and code. Throughout the time of the survey, research assistants supervised and assisted participants in completing the investigation. Printed questionnaires were checked as participants completed to ensure that all questions were answered. There was no missing data for the online version as all questions included the forced answering option. Therefore, the missing data in this study were minimal. We used the pair-wise deletion method to handle missing data. It took around 10–15 min for each survey. The patient's data was then coded and analyzed for study purposes only.
Demographic characteristics were obtained regarding age, gender, marital status (never married vs. ever married), education levels (junior high school or lower vs. senior high school vs. college/university or higher), occupational status (no job vs. has a job), ability to pay for medical care (easy vs. difficult), social status (low vs. middle or high). We calculated body mass index (BMI, kg/m2) based on self-reported body weight (kg) and height (cm) and then categorized into three groups: underweight (BMI <18.5), normal weight (18.5 ≤ BMI <25.0), and overweight/obese (BMI ≥ 25.0). The questionnaire used the 14 items of the Charlson Comorbidity Index (51) to assess patients' comorbidities. We then categorized the comorbidity into two groups: “none” vs. “one or more” diseases. Participants with any symptoms resembling COVID-19 (Slike-CV19S), including fever, cough, dyspnea, myalgia, fatigue, sputum production, confusion, headache, sore throat, rhinorrhea, chest pain, hemoptysis, diarrhea, and vomiting (52), were classified as having Slike-CV19S.
The national lockdown measure was implemented in Vietnam from April 1–22, 2020 (47, 48). The execution time was categorized into two groups: “under lockdown” vs. “after lockdown,” where patients who conducted the survey in the lockdown period were classified as those under lockdown.
The questionnaire asked participants about the changes in their current eating and physical activity behaviors compared to those before the COVID-19 pandemic. Patients responded on a five-point scale (never, stopped, less active, unchanged, and more active) for physical activity and a three-point scale (less healthy, unchanged, and healthier) for eating behavior. The World Health Organization (WHO) suggested that individuals should maintain unchanged or improve healthy lifestyles (healthy eating, physical activity) to stay healthy during the pandemic, especially in the lockdown period (46). In this study, participants with “never” and “unchanged” responses to physical activity were those who did not change their physical activity before and during the pandemic. However, a “never” reply was considered a negative behavior. In contrast, an “unchanged” response which means maintaining physical activity at a constant intensity, was considered a positive behavior during the pandemic. Therefore, we categorized physical activity and eating behavior changes into two groups: negative behaviors “never/stopped or less active” vs. positive behaviors “unchanged or more active” for physical activity, and negative behaviors “less healthy” vs. positive behaviors “unchanged or healthier” for eating behavior (43, 53).
We assessed the changes in participants' mental health using the question “How has your mental health changed compared to that before the pandemic?” Patients answered this question with three options, including 1 = “worse,” 2 = “stable,” and 3 = “better.” To ease for analysis, we categorized mental health changes into two groups: “worse” vs. “stable or better” (38).
This study assessed the DDL and health literacy (HL) using the DDL-4 questionnaire and HLS-SF12 questionnaire, respectively. These instruments were developed, validated, and commonly used in previous studies in Vietnam (36, 38, 39, 43, 54–57). In the current study, the Cronbach's α of DDL-4 and HLS-SF12 tools were 0.96 and 0.95, respectively. The patients were asked to rank their difficulty to perform each questionnaire item on four-point responses from 1 = “very difficult” to 4 = “very easy.” We then transformed DDL and HL scores into unified metrics with the ranges from 0 to 50, where participants with a greater DDL score or HL score had better DDL or HL. The formula was documented in prior papers (36, 58).
Our study evaluated the eHEALS of participants using an eHealth literacy scale. This instrument consists of eight items, which were validated and utilized in the Vietnamese context (39, 43). The Cronbach's α of eHEALS was 0.96 in this study. Patients ranked their agreement with eight opinions regarding their ability to identify and evaluate health information from online sources. The responses range from 1 = “strongly disagree” to 5 = “strongly agree.” The sum scores were from 8 to 40, in which patients with a greater eHEALS score had better eHEALS.
The fear of COVID-19 scale (FCoV-19S) with seven items was used to assess the fear level of patients. This questionnaire was developed, validated, and used during the pandemic in different countries (59, 60), including Vietnam previous (39, 61). The Cronbach's α of this tool was 0.92 in our study. Patients ranked their consent with seven statements regarding their feelings related to COVID-19 infectability. The possible answers range from 1 = “strongly disagree” to 5 = “strongly agree.” The answers were added up, and the sum scores were from 7 - 35, in which participants with a higher score presented a greater degree of fear of COVID-19.
First, we presented independent variables (IVs) as the mean, standard deviation, frequency, and proportion appropriately. Missing data were handled by the pair-wise deletion method. Second, the Chi-squared test and one-way ANOVA test were appropriately performed to compare the proportion of three outcomes (changes in eating behavior, physical activity, and mental health) by different IVs. We used the Benjamini-Hochberg method to decrease the false discovery rate (FDR) when performing multiple comparisons. The raw p-values were adjusted to control the level of FDR at 5% using the Benjamini-Hochberg method. Third, we used unadjusted and adjusted logistic regression models to explore the associations of lockdown, DDL, and eHEALS with three outcomes. We chose IVs linked to outcomes at p < 0.2 in simple logistic regression models to put in adjusted models. We also performed the Spearman correlation test to check relationships between IVs to avoid multicollinearity. If a moderate or high (rho ≥ 0.30) correlation was found between two IVs, we selected a representative one to adjust the final models. Finally, we performed interaction models to examine the modification effects of DDL and eHEALS on the associations between COVID-19 lockdown and three outcomes. If DDL or eHEALS was not associated with outcomes in adjusted logistic regression models, we did not perform the interaction analyses between lockdown and DDL or eHEALS for those outcomes. Unadjusted interaction models were run with three terms that were X1, X2, and X1 × X2. In which X1 is the main effect of lockdown (“Under lockdown × lowest DDL” or “under lockdown × lowest eHEALS”), X2 is the main effects of DDL or eHEALS (“After lockdown × 1-point increment of DDL” or “after lockdown × 1-point increment of eHEALS”), and X1 × X2 is the interaction term (“Under lockdown × 1-point increment of DDL” or “under lockdown × 1-point increment of eHEALS”). Adjusted interaction models were tested with three interaction terms and potential confounders. For visualizing interactions, we conducted the simple slope analyses using PROCESS Marco version 3.5 in SPSS. Before performing simple slope tests, DDL and eHEALS were centralized with a new mean of zero. The graphs were drawn by calculating the expected probability of outcomes by the lockdown variable at three values of DDL or eHEALS (the mean, −1 SD, and +1 SD from the mean). We also reported the coefficients of conditional effects to calculate the odds ratios for the impacts of COVID-19 lockdown on outcomes at three values of DDL or eHEALS. The p < 0.05 was defined as a significant level. All analyses were conducted by the IBM SPSS Version 26.0 (IBM Corp, Armonk, NY, United States).
In 4,348 participants, the means of age (year), DDL scores, and eHEALS scores were 42.8 ± 16.7, 25.9 ± 12.2, and 27.9 ± 6.9, respectively. Out of all outpatients, 38.0% (1,654/4,348) were male, 17.8% (772/4,348) were never married, 89.1% (3,874/4,348) had a job, 62.5% (2,712/4,348) found it difficult to pay for medical care, 28.8% (1,254/4,348) had one or more comorbidities, 37.0 % (1,609/4,348) took the survey by online questionnaires. The percentages of outpatients with unchanged or healthier eating behavior, unchanged or more physical activity, and stable or better mental health were 92.5% (4,002/4,348), 42.1% (1,833/4,348), and 62.2% (2,705/4,348), respectively. The proportions of unchanged or healthier eating behavior, unchanged or more physical activity, and stable or better mental health were varied by different categories of age, gender (only for physical activity), marital status, education, occupation, ability to pay for medical care, social status (only for mental health), BMI (only for physical activity), COVID-19 lockdown, Slike-CV19S, comorbidity, health literacy, and fear of COVID-19 (only for mental health) (Benjamini-Hochberg adjusted p < 0.05) (Table 1). In addition, two groups “under lockdown” and “after lockdown” had differences in several characteristics, including age, gender, marital status, education, ability to pay for health care, social status, BMI, Slike-CV19S, comorbidity, HL, and fear of COVID-19 (Table 1).
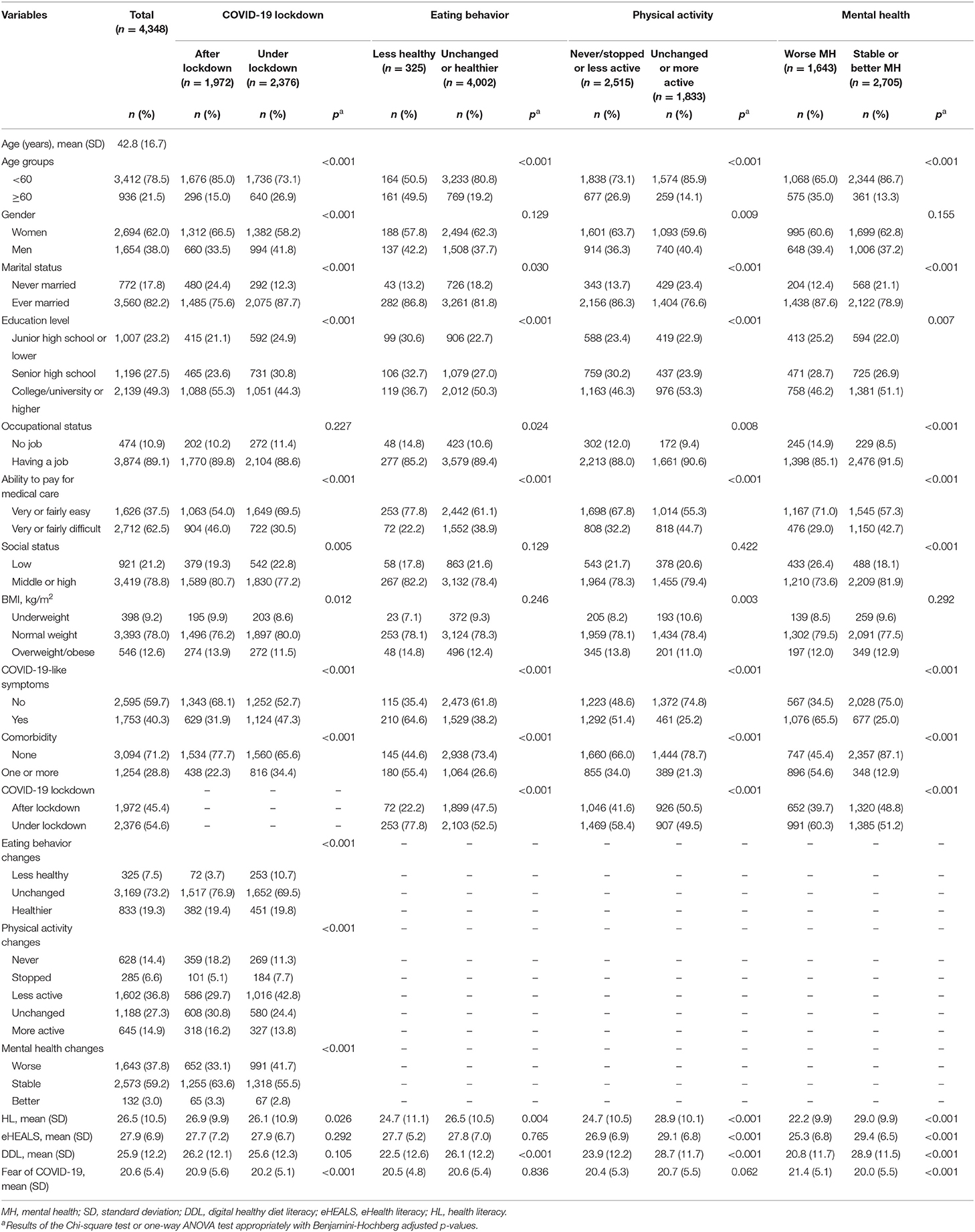
Table 1. Characteristics of outpatients by COVID-19 lockdown, and changes in eating behavior, physical activity, mental health (n = 4,348).
After checking Spearman correlations between IVs, we found that age moderately correlates with education levels (rho = −0.34); ability to pay for medical care moderately correlates with social status (rho = 0.30); health literacy moderately correlates with comorbidities (rho = −0.38), and COVID-19-like symptoms (rho = −0.34) (Supplementary Table 1). Therefore, age, gender, ability to pay for medical care, health literacy, and other confounding factors associated with outcomes at p <0.2 were added to adjusted logistic regression models (Supplementary Table 2).
The results of adjusted logistic regression models showed that patients under lockdown had a lower likelihood of having unchanged or healthier eating behavior (odds ratio, OR, 0.38; 95% confidence interval, 95% CI, 0.29 to 0.51; p < 0.001), unchanged or more physical activity (OR, 0.79; 95% CI, 0.69 to 0.90; p < 0.001), and stable or better mental health (OR, 0.77; 95% CI, 0.67 to 0.89; p < 0.001) (Table 2). Conversely, participants with a higher DDL had a higher likelihood of having unchanged or healthier eating behavior (OR, 1.02; 95% CI, 1.01 to 1.03; p = 0.043), and stable or better mental health (OR, 1.02; 95% CI, 1.01 to 1.03; p < 0.001), while participants with a higher eHEALS had a higher likelihood of having unchanged or more physical activity (OR, 1.01; 95% CI, 1.00 to 1.03; p = 0.043), and stable or better mental health (OR, 1.06; 95% CI, 1.05 to 1.08; p < 0.001) (Table 2).
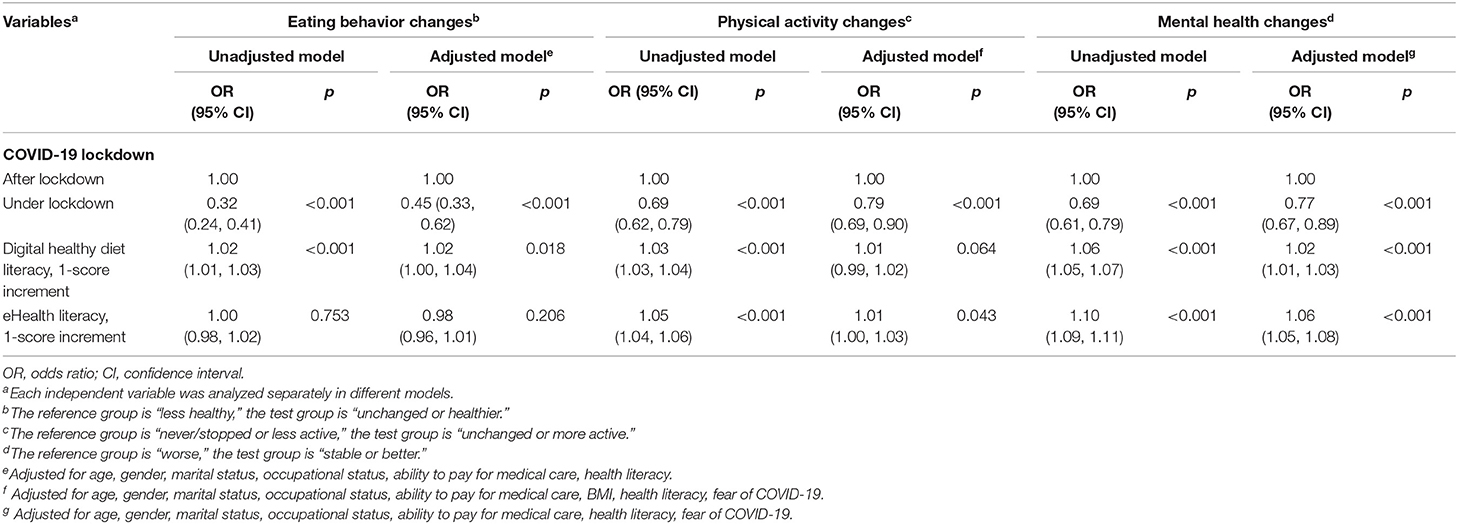
Table 2. Associations of COVID-19 lockdown, digital healthy diet literacy, eHealth literacy with changes in eating behavior, physical activity, and mental health (n = 4,348).
In the interaction model between COVID-19 lockdown and DDL on eating behavior changes, as compared to patients after the lockdown and with the lowest DDL score, those under lockdown and with the lowest DDL score had a lower likelihood of maintaining unchanged or healthier eating behavior (OR, 0.12; 95% CI, 0.06 to 0.23; p < 0.001), while those under lockdown and with one DDL-point increment had a higher likelihood of having unchanged or healthier eating behavior (OR, 1.05; 95% CI, 1.02 to 1.07; p < 0.001) (Table 3). Figure 2 illustrated the change in the expected probability of unchanged or healthier eating by COVID-19 lockdown at three levels of DDL (the mean, −1 SD, and +1 SD from the mean). The negative impact of COVID-19 lockdown on unchanged or healthier eating was attenuated by higher DDL values from 1 SD below the mean (OR = 0.22, 95% CI, 0.15 to 0.34, p < 0.001), the mean (OR = 0.39, 95% CI, 0.30 to 0.54, p < 0.001), to 1 SD above the mean (OR = 0.70, 95% CI, 0.50 to 0.99, p = 0.048) (Supplementary Table 3). Overall, the significant interaction suggested that when DDL was higher, the inverse association between COVID-19 lockdown and eating behavior changes became weaker.
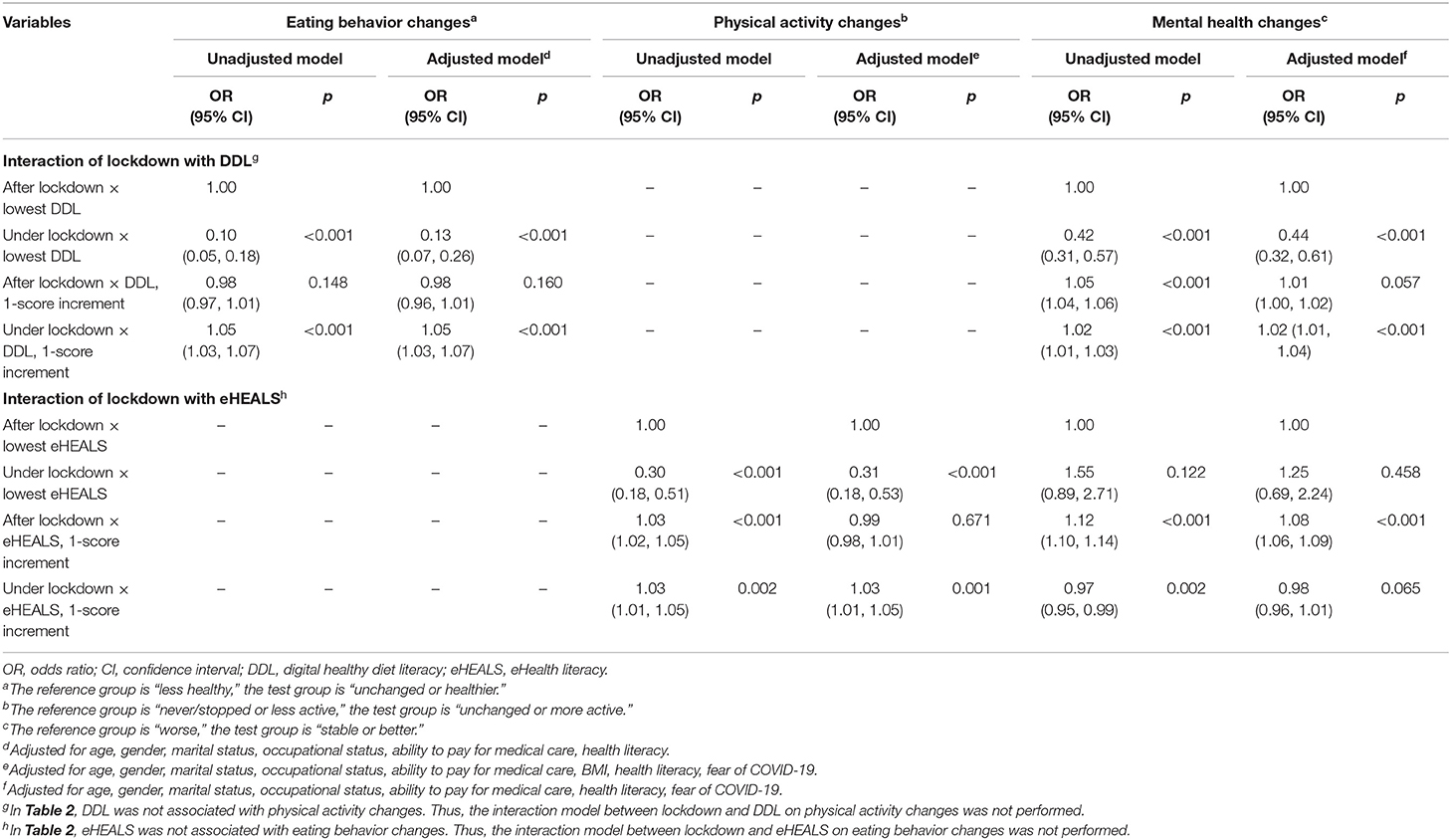
Table 3. Interactions of COVID-19 lockdown with digital healthy diet literacy and eHealth literacy on changes in eating behavior, physical activity, and mental health (n = 4,348).
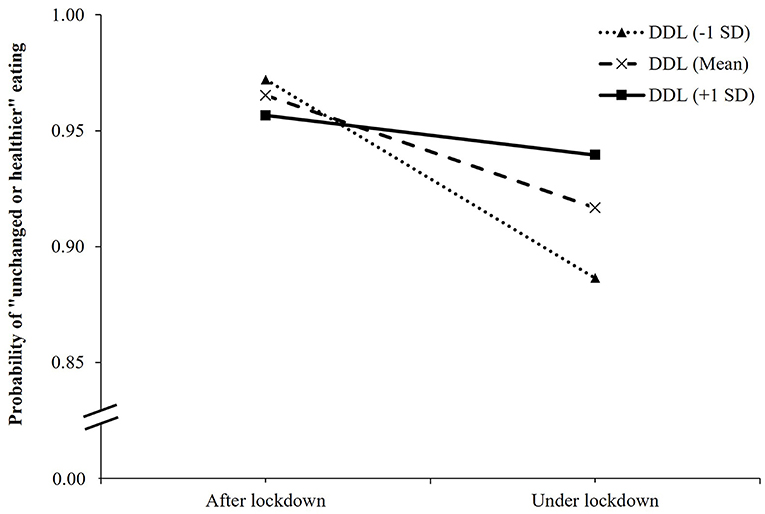
Figure 2. Simple slope plot for interaction between lockdown and digital healthy diet literacy on eating behavior changes among outpatients (n = 4,348). DDL, digital healthy diet literacy; SD, standard deviation.
In the interaction model between COVID-19 lockdown and DDL on mental health changes, as compared patients after the lockdown and with the lowest DDL score, those under lockdown and with the lowest DDL score had lower odds of stable or better mental health (OR, 0.44; 95% CI, 0.32 to 0.61; p < 0.001), while those under lockdown and with one DDL-point increment had a higher likelihood of stable or better mental health (OR, 1.02; 95% CI, 1.01 to 1.04; p < 0.001) (Table 3). Figure 3 showed the change in the expected probability of stable or better mental health by COVID-19 lockdown at three values of DDL. The negative impact of COVID-19 lockdown on stable or better mental health was attenuated by higher DDL values from 1 SD below the mean (OR = 0.60, 95% CI, 0.50 to 0.72, p < 0.001), the mean (OR = 0.79, 95% CI, 0.69 to 0.91, p = 0.001), to 1 SD above the mean (OR = 1.05, 95% CI, 0.84 to 1.30, p = 0.665) (Supplementary Table 3). Overall, the significant interaction suggested that when DDL was higher, the inverse association between COVID-19 lockdown and mental health changes became weaker.
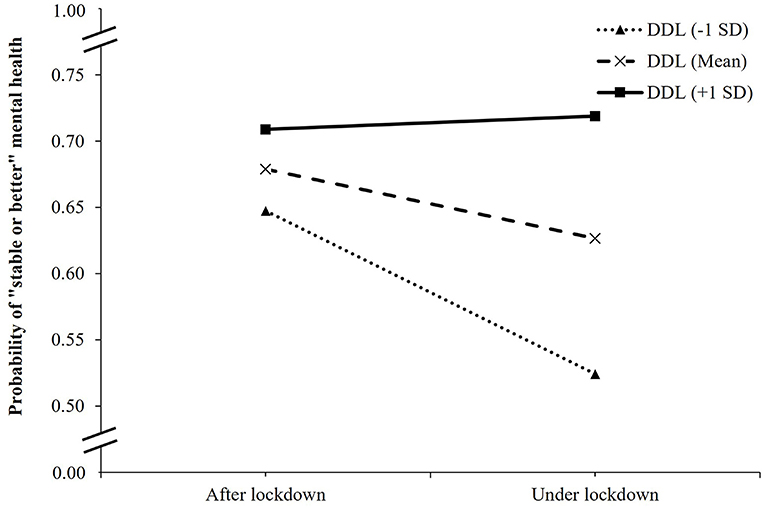
Figure 3. Simple slope plot for interaction between lockdown and digital healthy diet literacy on mental health changes among outpatients (n = 4,348). DDL, digital healthy diet literacy; SD, standard deviation.
In the interaction model between COVID-19 lockdown and eHEALS on physical activity changes, as compared to patients after the lockdown and with the lowest eHEALS score, those under lockdown and with the lowest eHEALS score had a lower likelihood of maintaining unchanged or more physical activity (OR, 0.31; 95% CI, 0.18 to 0.53; p < 0.001), while those under lockdown and with one eHEALS-point increment had higher odds of having an unchanged or more physical activity (OR, 1.03; 95% CI, 1.01 to 1.05; p < 0.001) (Table 3). Figure 4 showed the change in the expected probability of unchanged or more physical activity by COVID-19 lockdown at three values of eHEALS. The negative impact of COVID-19 lockdown on unchanged or more physical activity was attenuated by higher eHEALS values from 1 SD below the mean (OR = 0.62, 95% CI, 0.52 to 0.75, p < 0.001), the mean (OR = 0.78, 95% CI, 0.68 to 0.89, p < 0.001), to 1 SD above the mean (OR = 0.98, 95% CI, 0.82 to 1.17, p = 0.837) (Supplementary Table 3). Overall, the significant interaction suggested that when eHEALS was higher, the inverse association between COVID-19 lockdown and physical activity changes became weaker.
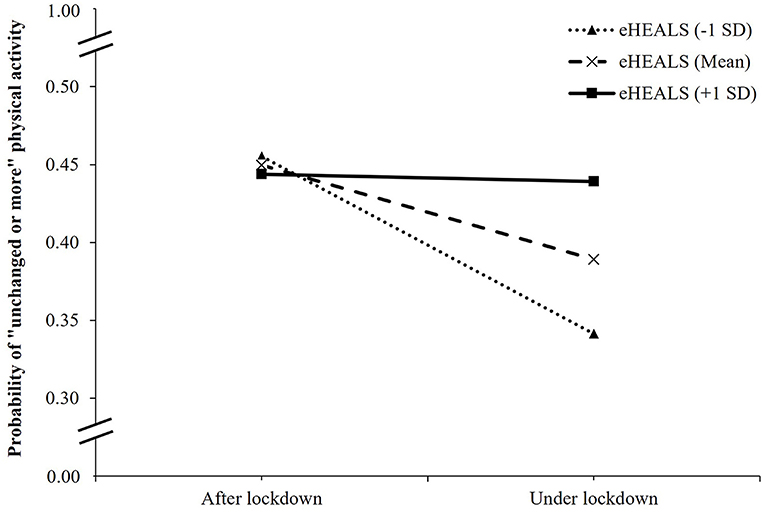
Figure 4. Simple slope plot for interaction between lockdown and eHealth literacy on physical activity changes among outpatients (n = 4,348). Note: eHEALS, eHealth literacy; SD, standard deviation.
Our findings highlighted the impacts of COVID-19 induced lockdown on changes in eating behavior, physical activity, mental health, and the modification effect of DDL and eHEALS on these associations in outpatients.
The current study found that the lockdown measure was negatively associated with maintaining unchanged or healthier eating behavior, unchanged or more physical activity, and stable or better mental health. A previous systematic review of 64 articles indicated that as compared with pre-lockdown, there was a decrease in physical activity in different populations during the lockdown period (25). Other studies conducted in different countries also showed that the COVID-19 lockdown or home confinement measures had harmful impacts on mental health and health-related behaviors with higher percentages of psychological disorders, physical inactivity, and unhealthy eating habits (11, 19, 23, 24, 62, 63). During the COVID-19 lockdown, restrictions on outside activities and travel, and limited food availability could cause negative changes in physical activity and dietary patterns (20–22, 25). In addition, the lockdown measure could adversely affect patients' mental health due to the difficulty in accessing medical care, delay in treatment, and feelings of boredom or isolation in the home confinement period (10, 11, 35). However, the current study did not study the potential impact of hospitalization and reasons of hospital visits on health-related behaviors, which might have biased the reported results. Therefore, appropriate strategies should be promoted to improve healthy lifestyles and psychological health during the COVID-19 lockdown.
Our study indicated that patients with higher DDL were more likely to have unchanged or healthier eating habits and stable or better psychological health during the pandemic. These findings are consistent with prior studies on front-line medical staff and healthcare students amidst the pandemic (36, 38). Importantly, we found that DDL could help to mitigate the adverse impacts of the lockdown measure on eating behavior and mental health. These findings could be explained that although there was a limited food availability and accessibility, patients with higher DDL may have the ability to evaluate and find for themselves a proper diet and avoid unhealthy foods (e.g., snacks, processed food) through reliable online health information sources during the COVID-19 lockdown. Meanwhile, higher DDL was found to be linked with higher health-related quality of life (39) and healthier eating behavior (36). Furthermore, the beneficial impacts of better dietary intake on psychological health were also documented in previous studies (53, 64, 65). Therefore, by improving the quality of life and diet, DDL could help patients to maintain stable or better mental health during the lockdown period.
Moreover, the results of this study demonstrated that higher eHEALS was associated with a higher likelihood of having unchanged or more physical activity and stable or better mental health. The role of eHEALS in maintaining positive health-related behaviors and protecting mental health has been reported in previous research (40–43). Furthermore, in the interaction model, higher eHEALS could attenuate the harmful effects of COVID-19 induced lockdown on physical activity habits. An explanation for this association is that during the lockdown period, as people have to stay at home and restrict travel, they are more likely to engage in sedentary behaviors and increase screen time (66–68), which in the long term can cause weight gain and chronic diseases (63, 69). Patients with higher eHEALS have higher health awareness, and they have the skills to seek and identify suitable methods to help them maintain physical activity during the home confinement time. Maintaining a healthy diet and staying physically active are essential to improve physical and mental health during the pandemic, especially among people with health problems (46). Therefore, as the lockdown measure was implemented in many countries, enhancing EHL and DDL is critical to help patients to evaluate and identify trusted health information and make the right decisions about their health-related behavior and health.
In the present study, although the magnitude of changes in eating behavior, physical activity, and mental health during and after the lockdown was not substantial, statistically significant results also indicated a negative impact of COVID-19 lockdown on such changes in the short term. In the long run, when the COVID-19 pandemic is uncertain and the lockdown is prolonged, those changes may be more significant and worse without appropriate interventions. Therefore, with a relatively large sample size collected in many hospitals, our research has suggested timely evidence about the adverse impact of lockdowns and protective factors, which may help policymakers develop proper strategies to improve lifestyles and psychological health. In addition, some findings of this study (e.g., associations of DDL and eHEALS with physical activity changes) indicated that a 1-point increase in DDL or eHEALS resulted in a 1% increase in the proportion of unchanged or more physical activity. Although the size of the effects was not large, it would be meaningful if DDL and eHEALS enhancement interventions were implemented comprehensively. It could help people and patients to improve all skills in DDL or eHEALS, not just a specific skill. Therefore, DDL or eHEALS could be enhanced better, leading to a broader and more significant impact of DDL or eHEALS on the outcomes. Besides, mitigating the adverse impact of COVID-19 lockdown may depend on other factors, such as social security policies, food security, unemployment. Therefore, the results of the current study on improving DDL or eHEALS could provide substantive implications, helping patients to improve health-related behaviors and mental health, not only during the lockdown period but also in normal life.
Our study has several drawbacks. First, the causal relationship cannot be inferred from a cross-sectional study. Second, given the urgency of providing timely preliminary evidence for interventions in the initial stage of the pandemic, we used the consecutive convenience sampling method to recruit as many participants as possible. However, we had no data about patients approached in this survey, and only patients who agreed to join and completed the study were recorded. In addition, the total number of patients who visited hospitals during the study period was not recorded and not available on the system. Therefore, we cannot calculate the response rate of this study, which may affect the generalizability of our findings. Third, we used secondary data to analyze the associations in the present study, leading to an increase in the false discovery rate when testing multiple hypotheses on the same sample. Thus, the Benjamini-Hochberg method was used to adjust the p-value. Fourth, changes in eating behavior, physical activity, and mental health were assessed using single-item questionnaires, which may be subjective and cause reporting bias. In addition, the current study evaluated the change in physical activity with five answer options: never, stopped, less active, unchanged, and more active. However, the response “never” is an absolute answer that has not changed before and during the pandemic. Besides, it was also assumed that people who were never physically active might improve their behavior over time during the pandemic, while they could not make their physical activity worse than “never.” Due to a cross-sectional study, we classified the “never” response as a negative behavior, which may cause some bias in the classification of physical activity changes. Therefore, results related to physical activity in this study should be applied with caution. Future studies also need to use a better approach for the assessment and classification of these outcomes. Next, we collected data using online and printed versions of the questionnaire, which may affect the results of this study. In addition, because comorbidities and health literacy were moderately correlated (rho = −0.38), we chose health literacy to adjust in the final models. However, it is suspected that the findings of this study may be affected by comorbidities. Therefore, we conducted the sensitivity analyses, which added comorbidities (“none” vs. “one or more”) and questionnaire types (“online” vs. “printed”) to adjust in final models. The results showed that the associations and interactions remained significant (Supplementary Tables 4, 5). Finally, other variables influencing outcomes of this study, such as food insecurity, financial difficulty, social support, should be studied in future research.
The COVID-19 induced lockdown could negatively affect changes in eating behavior, physical activity, and mental health among outpatients. Digital healthy diet literacy and eHealth literacy could help to alleviate the adverse impacts of the COVID-19 induced lockdown on eating behavior, physical activity, and psychological health. Therefore, health organizations and policymakers should promote appropriate interventions to enhance DDL and eHEALS, which help patients to maintain their healthy lifestyles and protect mental health during the lockdown period. However, this study holds several limitations that may undermine the certainty of reported findings.
The raw data supporting the conclusions of this article will be made available on reasonable request to the corresponding author.
The studies involving human participants were reviewed and approved by Hanoi University of Public Health, Vietnam (IRB Number: 133/2020/YTCC-HD3). The patients/participants provided their written informed consent to participate in this study.
ThamN, MN, TP, V-TL, TaN, TL, BD, HD, HN, TH, LP, PN, HoN, TDo, HuN, MT, TL, AT, ThaoN, KN, DP, KP, C-HB, and TDu: conceptualization, methodology, validation, investigation, data curation, and writing review and editing draft. MN, ThamN, and TDu: formal analysis and writing-original draft. MN, TP, and ThaoN: project administration. TDu: supervision and funding acquisition. All authors have read and approved the final manuscript.
This research was funded by Hai Phong University of Medicine and Pharmacy and Taipei Medical University (108-6202-008-112; 108-3805-022-400).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The authors sincerely thank the support of experts, researchers, and patients participating in this study from eleven hospitals.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fnut.2021.774328/full#supplementary-material
1. Mahase E. Covid-19: what new variants are emerging and how are they being investigated? BMJ. (2021) 372:n158. doi: 10.1136/bmj.n158
2. Dyer O. Covid-19: variants are spreading in countries with low vaccination rates. BMJ. (2021) 373:n1359. doi: 10.1136/bmj.n1359
3. Mathieu E, Ritchie H, Ortiz-Ospina E, Roser M, Hasell J, Appel C, et al. A global database of COVID-19 vaccinations. Nat Hum Behav. (2021) 5:947–53. doi: 10.1101/2021.03.22.21254100
4. World Health Organisation. Coronavirus Disease (COVID-19): Vaccines. (2021). Available online at: https://www.who.int/news-room/q-a-detail/coronavirus-disease-(covid-19)-vaccines? (accessed March 15, 2021).
5. Anderson RM, Vegvari C, Truscott J, Collyer BS. Challenges in creating herd immunity to SARS-CoV-2 infection by mass vaccination. Lancet. (2020) 396:1614–6. doi: 10.1016/S0140-6736(20)32318-7
6. McKie R. Would Herd Immunity Stop the Spread of Coronavirus? (2020). Available online at: https://www.theguardian.com/world/2020/oct/11/would-herd-immunity-stop-the-spread-of-coronavirus (accessed May 15, 2021).
7. Oraby T, Tyshenko MG, Maldonado JC, Vatcheva K, Elsaadany S, Alali WQ, et al. Modeling the effect of lockdown timing as a COVID-19 control measure in countries with differing social contacts. Sci Rep. (2021) 11:3354. doi: 10.1038/s41598-021-82873-2
8. World Health Organisation. Impact of COVID-19 on People's Livelihoods, Their Health and Our Food Systems. (2020). Available online at: https://www.who.int/news/item/13-10-2020-impact-of-covid-19-on-people%27s-livelihoods-their-health-and-our-food-systems (accessed June 15, 2021).
9. World Health Organization. Mental Health & COVID-19. (2021). Available online at: https://www.who.int/teams/mental-health-and-substance-use/covid-19 (accessed April 15, 2021).
10. Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. (2020) 395:912–20. doi: 10.1016/S0140-6736(20)30460-8
11. Ammar A, Trabelsi K, Brach M, Chtourou H, Boukhris O, Masmoudi L, et al. Effects of home confinement on mental health and lifestyle behaviours during the COVID-19 outbreak: insights from the ECLB-COVID19 multicentre study. Biol Sport. (2021) 38:9–21. doi: 10.1101/2020.05.04.20091017
12. Hootman KC, Guertin KA, Cassano PA. Stress and psychological constructs related to eating behavior are associated with anthropometry and body composition in young adults. Appetite. (2018) 125:287–94. doi: 10.1016/j.appet.2018.01.003
13. Penaforte FRO, Minelli MCS, Anastácio LR, Japur CC. Anxiety symptoms and emotional eating are independently associated with sweet craving in young adults. Psychiatry Res. (2019) 271:715–20. doi: 10.1016/j.psychres.2018.11.070
14. Moynihan AB, van Tilburg WA, Igou ER, Wisman A, Donnelly AE, Mulcaire JB. Eaten up by boredom: consuming food to escape awareness of the bored self. Front Psychol. (2015) 6:369. doi: 10.3389/fpsyg.2015.00369
15. Khalid S, Williams CM, Reynolds SA. Is there an association between diet and depression in children and adolescents? A systematic review. Br J Nutr. (2016) 116:2097–108. doi: 10.1017/S0007114516004359
16. Van Dyk TR, Becker SP, Byars KC. Rates of mental health symptoms and associations with self-reported sleep quality and sleep hygiene in adolescents presenting for insomnia treatment. J Clin Sleep Med. (2019) 15:1433–42. doi: 10.5664/jcsm.7970
17. Cecchetto C, Aiello M, Gentili C, Ionta S, Osimo SA. Increased emotional eating during COVID-19 associated with lockdown, psychological and social distress. Appetite. (2021) 160:105122. doi: 10.1016/j.appet.2021.105122
18. Osimo SA, Aiello M, Gentili C, Ionta S, Cecchetto C. The influence of personality, resilience, and alexithymia on mental health during COVID-19 pandemic. Front Psychol. (2021) 12:630751. doi: 10.3389/fpsyg.2021.630751
19. Yang GY, Lin XL, Fang AP, Zhu HL. Eating habits and lifestyles during the initial stage of the COVID-19 lockdown in China: a cross-sectional study. Nutrients. (2021) 13:970. doi: 10.3390/nu13030970
20. Jia P, Liu L, Xie X, Yuan C, Chen H, Guo B, et al. Changes in dietary patterns among youths in China during COVID-19 epidemic: the COVID-19 impact on lifestyle change survey (COINLICS). Appetite. (2021) 158:105015. doi: 10.1016/j.appet.2020.105015
21. Hall G, Laddu DR, Phillips SA, Lavie CJ, Arena R. A tale of two pandemics: how will COVID-19 and global trends in physical inactivity and sedentary behavior affect one another? Prog Cardiovasc Dis. (2021) 64:108–10. doi: 10.1016/j.pcad.2020.04.005
22. Grant F, Scalvedi ML, Scognamiglio U, Turrini A, Rossi L. Eating Habits during the COVID-19 Lockdown in Italy: the nutritional and lifestyle side effects of the pandemic. Nutrients. (2021) 13:2279. doi: 10.3390/nu13072279
23. Galali Y. The impact of COVID-19 confinement on the eating habits and lifestyle changes: a cross sectional study. Food Sci Nutr. (2021) 9:2105–13. doi: 10.1002/fsn3.2179
24. Ammar A, Brach M, Trabelsi K, Chtourou H, Boukhris O, Masmoudi L, et al. Effects of COVID-19 home confinement on eating behaviour and physical activity: results of the ECLB-COVID19 international online survey. Nutrients. (2020) 12:1583.
25. Stockwell S, Trott M, Tully M, Shin J, Barnett Y, Butler L, et al. Changes in physical activity and sedentary behaviours from before to during the COVID-19 pandemic lockdown: a systematic review. BMJ Open Sport Exerc Med. (2021) 7:e000960. doi: 10.1136/bmjsem-2020-000960
26. Warren E, Footman K, Tinelli M, McKee M, Knai C. Do cancer-specific websites meet patient's information needs? Patient Educ Couns. (2014) 95:126–36. doi: 10.1016/j.pec.2013.12.013
27. El-Gayar O, Timsina P, Nawar N, Eid W. Mobile applications for diabetes self-management: status and potential. J Diabetes Sci Technol. (2013) 7:247–62. doi: 10.1177/193229681300700130
28. Ziebland S, Chapple A, Dumelow C, Evans J, Prinjha S, Rozmovits L. How the internet affects patients' experience of cancer: a qualitative study. BMJ. (2004) 328:564. doi: 10.1136/bmj.328.7439.564
29. Dadaczynski K, Okan O, Messer M, Leung AYM, Rosário R, Darlington E, et al. Digital health literacy and web-based information-seeking behaviors of university students in Germany during the COVID-19 pandemic: cross-sectional survey study. J Med Internet Res. (2021) 23:e24097. doi: 10.2196/preprints.24097
30. Liebl P, Seilacher E, Koester MJ, Stellamanns J, Zell J, Hübner J. What cancer patients find in the internet: the visibility of evidence-based patient information - analysis of information on German websites. Oncol Res Treat. (2015) 38:212–8. doi: 10.1159/000381739
31. Hua J, Shaw R. Corona Virus (COVID-19) “Infodemic” and emerging issues through a data lens: the case of China. Int J Environ Res Public Health. (2020) 17:2309. doi: 10.3390/ijerph17072309
32. Zarocostas J. How to fight an infodemic. Lancet. (2020) 395:676. doi: 10.1016/S0140-6736(20)30461-X
33. Islam MS, Sarkar T, Khan SH, Mostofa Kamal AH, Hasan SMM, Kabir A, et al. COVID-19-related infodemic and its impact on public health: a global social media analysis. Am J Trop Med Hyg. (2020) 103:1621–9. doi: 10.4269/ajtmh.20-0812
34. Ahmad AR, Murad HR. The impact of social media on panic during the COVID-19 pandemic in Iraqi Kurdistan: online questionnaire study. J Med Internet Res. (2020) 22:e19556. doi: 10.2196/19556
35. Riera R, Bagattini  M, Pacheco RL, Pachito DV, Roitberg F, Ilbawi A. Delays and disruptions in cancer health care due to COVID-19 pandemic: systematic review. JCO Glob Oncol. (2021) 7:311–23. doi: 10.1200/GO.20.00639
36. Duong TV, Pham KM, Do BN, Kim GB, Dam HTB, Le VT, et al. Digital healthy diet literacy and self-perceived eating behavior change during COVID-19 pandemic among undergraduate nursing and medical students: a rapid online survey. Int J Environ Res Public Health. (2020) 17:7185. doi: 10.3390/ijerph17197185
37. Norman CD, Skinner HA. eHealth literacy: essential skills for consumer health in a networked world. J Med Internet Res. (2006) 8:e9. doi: 10.2196/jmir.8.2.e9
38. Vu DN, Phan DT, Nguyen HC, Le LT, Nguyen HC, Ha TH, et al. Impacts of digital healthy diet literacy and healthy eating behavior on fear of COVID-19, changes in mental health, and health-related quality of life among front-line health care workers. Nutrients. (2021) 13:2656. doi: 10.3390/nu13082656
39. Nguyen MH, Pham TTM, Nguyen KT, Nguyen YH, Tran TV, Do BN, et al. Negative impact of fear of COVID-19 on health-related quality of life was modified by health literacy, eHealth literacy, and digital healthy diet literacy: a multi-hospital survey. Int J Environ Res Public Health. (2021) 18:4929 doi: 10.3390/ijerph18094929
40. Yang BX, Xia L, Huang R, Chen P, Luo D, Liu Q, et al. Relationship between eHealth literacy and psychological status during COVID-19 pandemic: a survey of Chinese residents. J Nurs Manag. (2021) 29:805–12. doi: 10.1111/jonm.13221
41. Tsukahara S, Yamaguchi S, Igarashi F, Uruma R, Ikuina N, Iwakura K, et al. Association of eHealth literacy with lifestyle behaviors in university students: questionnaire-based cross-sectional study. J Med Internet Res. (2020) 22:e18155. doi: 10.2196/18155
42. Yang SC, Luo YF, Chiang CH. Electronic health literacy and dietary behaviors in Taiwanese college students: cross-sectional study. J Med Internet Res. (2019) 21:e13140. doi: 10.2196/13140
43. Do BN, Tran TV, Phan DT, Nguyen HC, Nguyen TTP, Nguyen HC, et al. Health literacy, eHealth literacy, adherence to infection prevention and control procedures, lifestyle changes, and suspected COVID-19 symptoms among health care workers during lockdown: online survey. J Med Internet Res. (2020) 22:e22894. doi: 10.2196/22894
44. World Health Organisation. COVID-19: Vulnerable and High Risk Groups. (2020). Available online at: https://www.who.int/westernpacific/emergencies/covid-19/information/high-risk-groups (accessed May 8, 2020).
45. Barach P, Fisher SD, Adams MJ, Burstein GR, Brophy PD, Kuo DZ, et al. Disruption of healthcare: will the COVID pandemic worsen non-COVID outcomes and disease outbreaks? Prog Pediatr Cardiol. (2020) 59:101254. doi: 10.1016/j.ppedcard.2020.101254
46. World Health Organisation. Coronavirus Disease (COVID-19) Advice for the Public. (2020). Available online at: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public (accessed May 10, 2020).
47. Prime Minister of Vietnam. PM Orders Strict Nationwide Social Distancing Rules, Starting April 1. 2020. Available online at: https://vietnamlawmagazine.vn/pm-orders-strict-nationwide-social-distancing-rules-starting-april-1-27108.html (accessed March 31, 2020).
48. Prime Minister of Vietnam. Gov't Extends Social Distancing for at Least One Week in 28 Localities. (2020). Available online at: http://news.chinhphu.vn/Home/Govt-extends-social-distancing-for-at-least-one-week-in-28-localities/20204/39735.vgp (accessed April 20, 2020).
49. Vietnam Ministry of Health. Vietnam COVID-19 Data. (2021). Available online at: https://ncov.vncdc.gov.vn/viet-nam.html (accessed April 30, 2021).
50. Vietnam Ministry of Health. Prime Minister Instructed to Continue Measures to Prevent and Control the COVID-19 Epidemic in the New Situation. (2020). Available online at: https://covid19.gov.vn/thu-tuong-chi-thi-tiep-tuc-cac-bien-phap-phong-chong-dich-covid-19-trong-tinh-hinh-moi-1717039716.htm (accessed April 15, 2021).
51. Quan HD, Li B, Couris CM, Fushimi K, Graham P, Hider P, et al. Updating and validating the Charlson comorbidity index and score for risk adjustment in hospital discharge abstracts using data from 6 countries. Am J Epidemiol. (2011) 173:676–82. doi: 10.1093/aje/kwq433
52. BMJ Editorial Team. Overview of Novel Coronavirus (2019-nCoV). BMJ Best Practice (2020). Available online at: https://bestpractice.bmj.com/topics/en-gb/3000165 (accessed March 10, 2020).
53. Nguyen MH, Pham TTM, Pham LV, Phan DT, Tran TV, Nguyen HC, et al. Associations of underlying health conditions with anxiety and depression among outpatients: modification effects of suspected COVID-19 symptoms, health-related and preventive behaviors. Int J Public Health. (2021) 66:634904. doi: 10.3389/ijph.2021.634904
54. Duong TV, Nguyen TTP, Pham KM, Nguyen KT, Giap MH, Tran TDX, et al. Validation of the short-form health literacy questionnaire (HLS-SF12) and its determinants among people living in rural areas in Vietnam. Int J Environ Res Public Health. (2019) 16:3346. doi: 10.3390/ijerph16183346
55. Van Hoa H, Giang HT, Vu PT, Van Tuyen D, Khue PM. Factors associated with health literacy among the elderly people in Vietnam. Biomed Res Int. (2020) 2020:3490635. doi: 10.1155/2020/3490635
56. Do BN, Nguyen PA, Pham KM, Nguyen HC, Nguyen MH, Tran CQ, et al. Determinants of health literacy and its associations with health-related behaviors, depression among the older people with and without suspected COVID-19 symptoms: a multi-institutional study. Front Public Health. (2020) 8:581746. doi: 10.3389/fpubh.2020.581746
57. Nguyen TT, Le NT, Nguyen MH, Pham LV, Do BN, Nguyen HC, et al. Health literacy and preventive behaviors modify the association between pre-existing health conditions and suspected COVID-19 symptoms: a multi-institutional Survey. Int J Environ Res Public Health. (2020) 17:8598. doi: 10.3390/ijerph17228598
58. Duong TV, Aringazina A, Kayupova G, Nurjanah, Pham TV, Pham KM, et al. Development and validation of a new short-form health literacy instrument (HLS-SF12) for the general public in six Asian countries. Health Lit Res Pract. (2019) 3:e91–102. doi: 10.3928/24748307-20190225-01
59. Ahorsu DK, Lin CY, Imani V, Saffari M, Griffiths MD, Pakpour AH. The Fear of COVID-19 scale: development and initial validation. Int J Ment Health Addict. (2020) 1–9. doi: 10.1007/s11469-020-00270-8
60. Perz CA, Lang BA, Harrington R. Validation of the fear of COVID-19 scale in a US college sample. Int J Ment Health Addict. (2020) 1–11. doi: 10.1007/s11469-020-00356-3
61. Nguyen HT, Do BN, Pham KM, Kim GB, Dam HTB, Nguyen TT, et al. Fear of COVID-19 scale-associations of its scores with health literacy and health-related behaviors among medical students. Int J Environ Res Public Health. (2020) 17:4164. doi: 10.3390/ijerph17114164
62. Ruiz-Roso MB, Knott-Torcal C, Matilla-Escalante DC, Garcimartín A, Sampedro-Nuñez MA, Dávalos A, et al. COVID-19 lockdown and changes of the dietary pattern and physical activity habits in a cohort of patients with type 2 diabetes mellitus. Nutrients. (2020) 12:2327. doi: 10.3390/nu12082327
63. Jia P, Zhang L, Yu W, Yu B, Liu M, Zhang D, et al. Impact of COVID-19 lockdown on activity patterns and weight status among youths in China: the COVID-19 impact on lifestyle change survey (COINLICS). Int J Obes. (2021) 45:695–9. doi: 10.1038/s41366-020-00710-4
64. Pham KM, Pham LV, Phan DT, Tran TV, Nguyen HC, Nguyen MH, et al. Healthy dietary intake behavior potentially modifies the negative effect of COVID-19 lockdown on depression: a hospital and health center survey. Front Nutr. (2020) 7:581043. doi: 10.3389/fnut.2020.581043
65. Li Y, Lv MR, Wei YJ, Sun L, Zhang JX, Zhang HG, et al. Dietary patterns and depression risk: a meta-analysis. Psychiatry Res. (2017) 253:373–82. doi: 10.1016/j.psychres.2017.04.020
66. Górnicka M, Drywień ME, Zielinska MA, Hamułka J. Dietary and lifestyle changes during covid-19 and the subsequent lockdowns among polish adults: a cross-sectional online survey PLifeCOVID-19 study. Nutrients. (2020) 12:2324. doi: 10.3390/nu12082324
67. Greaney ML, Kunicki ZJ, Drohan MM, Ward-Ritacco CL, Riebe D, Cohen SA. Self-reported changes in physical activity, sedentary behavior, and screen time among informal caregivers during the COVID-19 pandemic. BMC Public Health. (2021) 21:1292. doi: 10.1186/s12889-021-11294-7
68. Schmidt SCE, Anedda B, Burchartz A, Eichsteller A, Kolb S, Nigg C, et al. Physical activity and screen time of children and adolescents before and during the COVID-19 lockdown in Germany: a natural experiment. Sci Rep. (2020) 10:21780. doi: 10.1038/s41598-020-78438-4
Keywords: lockdown, mental health, digital healthy diet literacy, eHealth literacy, eating behavior, outpatient, physical activity
Citation: Nguyen TT, Nguyen MH, Pham TTM, Le V-TT, Nguyen TT, Luong TC, Do BN, Dao HK, Nguyen HC, Ha TH, Pham LV, Nguyen PB, Nguyen HTT, Do TV, Nguyen HQ, Trinh MV, Le TT, Tra AL, Nguyen TTP, Nguyen KT, Phan DT, Pham KM, Bai C-H and Duong TV (2021) Negative Impacts of COVID-19 Induced Lockdown on Changes in Eating Behavior, Physical Activity, and Mental Health as Modified by Digital Healthy Diet Literacy and eHealth Literacy. Front. Nutr. 8:774328. doi: 10.3389/fnut.2021.774328
Received: 11 September 2021; Accepted: 22 October 2021;
Published: 12 November 2021.
Edited by:
Igor Pravst, Institute of Nutrition, SloveniaReviewed by:
Silvio Ionta, University of Lausanne, SwitzerlandCopyright © 2021 Nguyen, Nguyen, Pham, Le, Nguyen, Luong, Do, Dao, Nguyen, Ha, Pham, Nguyen, Nguyen, Do, Nguyen, Trinh, Le, Tra, Nguyen, Nguyen, Phan, Pham, Bai and Duong. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Tuyen Van Duong, ZHVvbmd0dXllbnZuYUBnbWFpbC5jb20=
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.