
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Nutr. , 26 November 2021
Sec. Nutrition and Sustainable Diets
Volume 8 - 2021 | https://doi.org/10.3389/fnut.2021.771492
This article is part of the Research Topic What, How, and Where to Eat is More than an Individual Choice: New Ways to Achieve Healthy Eating View all 11 articles
 Ayoub Al-Jawaldeh1
Ayoub Al-Jawaldeh1 Mandy Taktouk2
Mandy Taktouk2 Aya Chatila2
Aya Chatila2 Sally Naalbandian3
Sally Naalbandian3 Zahra Abdollahi4†
Zahra Abdollahi4† Buthaina Ajlan5†
Buthaina Ajlan5† Nawal Al Hamad6†
Nawal Al Hamad6† Majid M. Alkhalaf7†
Majid M. Alkhalaf7† Salima Almamary8†
Salima Almamary8† Rawan Alobaid9†
Rawan Alobaid9† Salah Abdulla Alyafei10†
Salah Abdulla Alyafei10† Mohammad Hosein Azizi11†
Mohammad Hosein Azizi11† Nimah M. Baqadir7†
Nimah M. Baqadir7† Rawhieh Barham12†
Rawhieh Barham12† Faisal F. Binsunaid13†
Faisal F. Binsunaid13† Leila El Ammari14†
Leila El Ammari14† Jalila El Ati15†
Jalila El Ati15† Maha Hoteit16†
Maha Hoteit16† Hanan Massad12†
Hanan Massad12† Marzeyeh Soleymani Nejad17†
Marzeyeh Soleymani Nejad17† Lara Nasreddine2*
Lara Nasreddine2*High intakes of trans fatty acids (TFA), particularly industrially-produced TFA, are implicated in the etiology of cardiovascular diseases, which represent the leading cause of mortality in the Eastern Mediterranean Region (EMR). This systematic review aims to document existing national TFA reduction strategies in the EMR, providing an overview of initiatives that are implemented by countries of the region, and tracking progress toward the elimination of industrially-produced TFA. A systematic review of published and gray literature was conducted using a predefined search strategy. A total of 136 peer-reviewed articles, gray literature documents, websites and references from country contacts were obtained, up until 2 August 2021. Randomized-control trials, case-control studies, and studies targeting unhealthy population groups were excluded. Only articles published after 1995, in English, Arabic or French, were included. Key characteristics of strategies were extracted and classified according to a pre-developed framework, which includes TFA intake assessment; determination of TFA levels in foods; strategic approach; implementation strategies (TFA bans/limits; consumer education, labeling, interventions in public institution settings, taxation), as well as monitoring and evaluation of program impact. Thirteen out of the 22 countries of the EMR (59%) have estimated TFA intake levels, 9 have determined TFA levels in foods (41%), and 14 (63.6%) have national TFA reduction initiatives. These initiatives were mainly led by governments, or by national multi-sectoral committees. The most common TFA reduction initiatives were based on TFA limits or bans (14/14 countries), with a mandatory approach being adopted by 8 countries (Bahrain, Iran, Jordan, KSA, Kuwait, Morocco, Oman and Palestine). Complementary approaches were implemented in several countries, including consumer education (10/14), food labeling (9/14) and interventions in specific settings (7/14). Monitoring activities were conducted by few countries (5/14), and impact evaluations were identified in only Iran and the UAE. The robustness of the studies, in terms of methodology and quality of assessment, as well as the lack of sufficient data in the EMR, remain a limitation that needs to be highlighted. Further action is needed to initiate TFA reduction programs in countries that are lagging behind, and to ensure rigorous implementation and evaluation of ongoing programs.
Cardiovascular diseases (CVD) represent the leading cause of mortality worldwide, causing ~17.9 million deaths each year and contributing to 31% of global deaths (1). High intake of trans fatty acids (TFA), particularly industrially produced TFA, were implicated in the etiology of CVD (2). Although available data on TFA intake globally is rather limited, it was recently reported that the 2017 global market volume of partially hydrogenated oils (PHOs), which is the major source of industrially produced TFA in food, was around 13.6 million tons (3). Wang et al. showed that compared to an optimal TFA intake of 0.5% of energy intake (%EI), excess TFA consumption was estimated to cause 537,200 coronary heart disease (CHD) deaths per year worldwide in 2010, representing 7.7% of global CHD mortality (4).
This is consistent with the unique cardiometabolic imprint of industrial TFA on both lipid and non-lipid pathways (4, 5). Physiologically, TFAs impact the lipid profile, raising the levels of the atherogenic low-density lipoprotein (LDL) cholesterol while also decreasing the levels of the cardioprotective high-density lipoprotein (HDL) cholesterol (2, 6). Randomized controlled trials have also shown that high TFA consumption produces adverse cardiovascular effects via pathways linked to the insulin resistance syndrome (5). A reduction in the population's intake of TFA has therefore been acknowledged as one of the policy priorities adopted by the World Health Organization (WHO) (5). One of the core indicators of the WHO global framework for monitoring non-communicable diseases (NCDs) by 2025, is the “adoption of national policies that virtually eliminate partially hydrogenated vegetable oils in the food supply and replace [them] with polyunsaturated fatty acids” (7). The elimination of industrially produced TFAs is in fact a relatively straightforward, low-cost and effective policy measure that is within reach of most countries, while carrying substantial long-term health benefits (3, 8, 9). However, most countries worldwide have yet to develop and implement strong policy measures to limit TFA intakes, and TFAs continue to be highly consumed around the world (10). In May 2018, the WHO has advocated for the global elimination of industrially produced TFA by 2023 and released the REPLACE action framework, with the aim of decreasing CVD-related mortality (3, 11). The REPLACE action framework consists of a roadmap for countries to implement immediate, complete and sustained elimination of industrial TFA from the food supply (12).
In the Eastern Mediterranean Region (EMR), a region that harbors a high burden of CVD, and where the consumption of TFA is high (13, 14), the WHO Regional Office for the Eastern Mediterranean, in collaboration with WHO Headquarters and Resolve to Save Lives, has been providing technical assistance to support country-level policy development and implementation. The WHO EMR regional nutrition strategy 2020–2030, has included specific objectives related to the virtual elimination of industrially-produced TFA from the food supply (15), and recommended a number of priority actions that will assist Member States in reaching these objectives (15). However, to date, there has been no comprehensive appraisal of the government-initiated public health strategies that are being adopted by countries of the region in order to eliminate TFA from the food supply and decrease the population's TFA intake. It is in this context that we conducted this systematic review, with the aim of identifying and documenting existing national TFA reduction strategies, providing an overview of initiatives that are implemented by countries of the EMR to reduce TFA intakes, and tracking progress toward the goal of TFA elimination by 2023.
The methodology and search strategy adopted in this study were similar to the approach described by Santos et al. (16) in their systematic review of salt reduction strategies. Accordingly, data related to TFA reduction initiatives were obtained through a series of steps, allowing for maximum coverage of the EMR and its 22 countries (17). This comprised a search of peer-reviewed and gray literature published up to 15 April 2021, in addition to seeking supplementary information by directly contacting program country leaders or focal points (Figure 1).
The present systematic review conforms to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement. A total of 12 electronic databases were searched between 17 February 2021 and 15 April 2021. These databases included: CAB Direct (18), Directory of Open Access Journals (19), Google (20), Ovid (21), National Library of Medicine (22), Elsevier (23), Clarivate (24), EBSCO (25), Al Manhal (26), EBSCO (27), E-Marefa (28) and Ministry of Higher Education and Scientific Research of Iraq (29); the last four being databases specific to the Arab region. In addition to using controlled vocabulary (MeSH in PubMed and MEDLINE), a comprehensive list of search terms was used in the title/abstract/keyword fields to cover the four concepts (1) TFA, (2) reduction OR intake, (3) policy, and (4) EMR countries. MEDLINE (Ovid) was searched first using a combination of MeSH terms and keywords. The search strategy was mapped to PubMed after making the necessary changes. To search the remaining databases, MeSH terms were searched as keywords in title-abstract-keyword fields whenever applicable. Google Scholar was searched using title field only. Appendix A shows the detailed list of search terms used in PubMed. Moreover, an example of a database search on PubMed is shown in Supplementary Table 1. The search excluded any material published before 1995. Only English, Arabic and French languages were considered. Newly published articles after the initial search were identified by email alerts (up until 2 August 2021).
A search of the gray literature was also performed, using OpenGrey (30), Google (31), World Healh Organization (32), World Health Organization Regional Office for the Eastern Mediterranean (33) and governmental websites (e.g., Ministries of Health). The search was limited to materials published post 1995 in English, Arabic and French languages only.
EndNote X9 (Version 18.0.0.10063) was used for the export of all identified articles after conducting the search on online databases and gray literature. Two independent researchers (MT and AC) screened the titles, abstracts and full text articles of the potentially relevant articles, according to the inclusion and exclusion criteria mentioned in the below section. The two researchers discussed and resolved the minor discrepancies that resulted from the two screening stages.
Articles were included in this review if they provided information on TFA baseline assessment [intake; levels in foods; knowledge, attitudes and behavior (KAB)], or the development, implementation, monitoring or evaluation of national TFA reduction initiatives at the national level. National TFA reduction initiatives were defined as having a governmental entity involved (12, 34, 35), in addition to one or more of the following components: (1) a national action plan to reduce the population TFA intake (12); (2) a program of work on TFA replacement (e.g., banning the use of partially hydrogenated oils; setting limits for industrial TFA in food products) (36); (3) consumers' education programs or awareness campaigns with the aim of improving KAB toward TFA (12); (4) labeling schemes specific to TFA or mandatory declaration of TFA on nutrition labels (12, 36); (5) taxation policies targeting high-TFA foods, or unhealthy foods defined by their high TFA content (12); and (6) TFA reduction initiatives in specific settings (schools, hospitals, workplaces) (12).
Articles based on randomized-control trials or case-control studies, as well as those targeting unhealthy individuals or specific populations (pregnant women, individuals on therapeutic diets etc.) were excluded. Individual articles were also excluded if they were published before 1995, or in any language besides English, Arabic, or French.
Data extraction was conducted independently by two researchers (MT and AC), and then a third researcher (LN) reviewed the data for accuracy. The researchers discussed the few discrepancies until reaching consensus. For each national TFA reduction initiative, the key characteristics were entered into a database constructed by the researchers, and examined in relation to baseline assessments (population TFA intake; TFA levels in food products, KAB related to TFA), leadership and strategic approach, implementation strategies (TFA bans or limits; consumer education, food labeling, interventions in public institution settings, taxation), monitoring (population intake, levels in food products, KAB), and evaluation of program impact (12, 34, 36, 37).
To seek supplementary information regarding national TFA reduction initiatives, a questionnaire was developed by the research team based on relevant literature (6, 37, 38) (Supplementary Questionnaires). After its development, the questionnaire was reviewed by a nutritionist and a public health professional for content validity. The questionnaire was then sent to country experts or program leaders in various countries of the EMR to verify and obtain supplementary country-specific data. Country experts or program leaders were invited to fill the questionnaire and/or pass on the questionnaire to their contacts to obtain additional information and deliver the needed details. The database was then updated accordingly with the additional obtained data.
For each identified national TFA reduction strategy, the core characteristics were entered into the database, according to the developed framework that includes baseline assessments; leadership/strategic approach; the different types of implementation strategies; monitoring data; and evaluation of program impact. Countries were then categorized as “having a developed strategy” for TFA elimination/reduction, “having a planned strategy” or “having no strategy.” Strategies were considered to be “planned” if the TFA reduction initiatives were still being developed or if an action plan had been already developed but without evidence of implementation. A quantitative evaluation of the proportion of countries reporting on each core characteristic was performed, and expressed as percentages.
A total of 136 peer-reviewed articles, gray literature documents, websites and references from country contacts were obtained from the literature search; 94 were peer-reviewed articles of potential relevance and 42 were additional sources obtained from country contacts via the completed questionnaires, links, webpages, and references from within the included studies (Figure 1).
Out of the 22 countries of the EMR, thirteen (59%) did not have any population estimate of TFA intakes (with the exception of estimates based on Bayesian modeling and which were not considered in this review) (10). In contrast, nine countries (41%), including Egypt, Iran, Jordan, Lebanon, Morocco, Pakistan, Sudan, Tunisia, and the UAE, have estimated population TFA intakes (Supplementary Table 2). Some of the available studies estimated TFA intakes at the national level for specific population groups (e.g., adults) or the entire population (per capita), while others reported the intakes within specific regions of the countries (4, 12, 14, 39–51). Except for Jordan, where TFA intake assessment was based on a household budget survey, all the other countries had evaluated TFA intakes based on dietary assessment methodologies (e.g., 24-h recalls, food frequency questionnaires, diet history questionnaires) (Supplementary Table 2). Total diet studies investigating dietary exposure to TFA are lacking in the region.
The available estimates of TFA intakes from various countries are presented in Figure 2, which focuses on national studies, and Figure 3, which illustrates data stemming from regional studies within countries. Based on national per capita estimates of TFA intakes (entire population), the highest level was observed in Egypt (6.5% EI), while the lowest was reported from Morocco (0.34% EI) (Figure 2). As for regional studies conducted amongst adults (Figure 3), the highest levels were observed in Lebanon (2.3–2.4% EI), while the lowest were noted among females in Sudan (0.1% EI) (Figure 3). Few countries have evaluated TFA intake among children and adolescents. In Iran this was reported at 2.2% EI in girls and around 2.3% in boys (Figure 3). In Jordan, TFA intake was estimated to range between 0.8 and 1.3 g/day among 6–18 year old children (46), and in Lebanon, average intake of TFA was reported at 0.16 g/day in 5–10 year old children (47). The contributions of these estimates to energy intake were not reported.
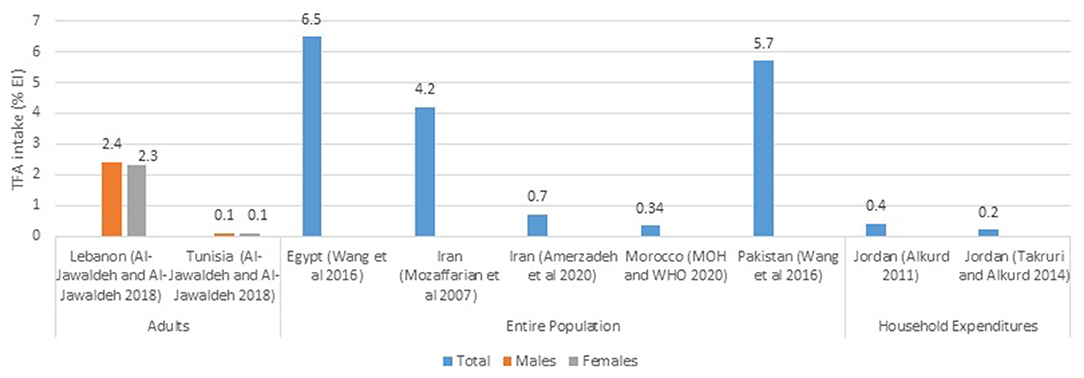
Figure 2. TFA intake estimates (%EI) based on national studies in countries of the EMR. EI, energy intake; EMR, Eastern Mediterranean Region; MOH, Ministry of health; TFA, trans fatty acids; WHO, World Health Organization. References: For Adults: Lebanon and Tunisia (dietary assessment): Al-Jawaldeh and Al-Jawaldeh (14). For Entire Population: Egypt and Pakistan (dietary assessment): Wang et al. (4); Iran (dietary assessment): Mozaffarian et al. (39); Iran (consumption data): Amerzadeh and Takian (41); Morocco (consumption data): Ministry of Health-Morocco and World Health Organization (49). For Household Expenditures: Jordan: Alkurd (44) and Takruri and Alkurd (45).
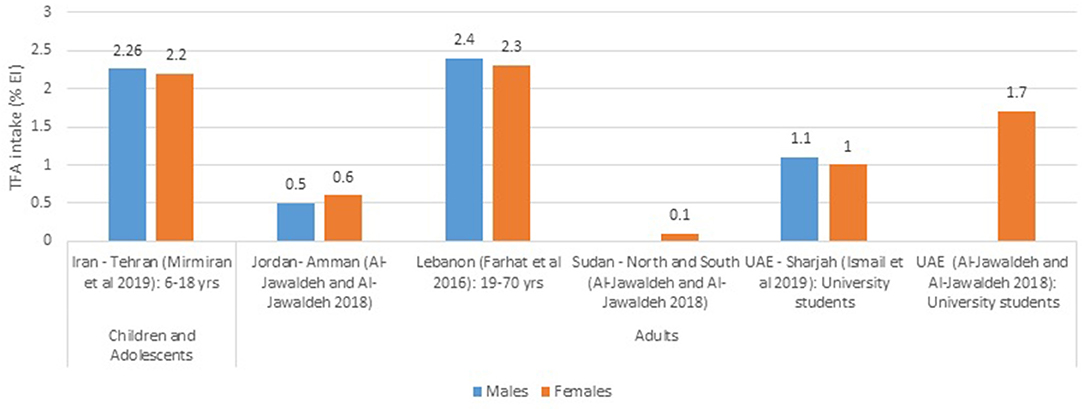
Figure 3. TFA intake estimates (%EI) based on regional studies in countries of the EMR. EI, energy intake; EMR, Eastern Mediterranean Region; MOH, Ministry of health; TFA, trans fatty acids; WHO, World Health Organization. References: For Children and Adolescents: Iran (dietary assessment): Mirmiran et al. (43). For Adults: Jordan and Sudan (dietary assessment): Al-Jawaldeh and Al-Jawaldeh (14); Lebanon (dietary assessment): Farhat et al. (48); UAE (dietary assessment): Ismail et al. (51) and Al-Jawaldeh and Al-Jawaldeh (14).
Several countries in the EMR (9/22 countries; 41%), including Egypt, Iran, Jordan, Kingdom of Saudi Arabia (KSA), Kuwait, Lebanon, Morocco, Pakistan, and Tunisia, have evaluated TFA levels in local foods and commodities (Supplementary Table 3) (14, 39, 49, 52–94). The majority of available TFA content data were derived based on chemical analysis of food products (39, 49, 52–56, 58, 60–70, 72–74, 77, 79–97), while very few studies have collected TFA content data based on food labels and packages (55, 75, 76). Most of the available studies have reported very high levels in fast foods (fried meats, sausages, French fries), pastries, potato chips, biscuits, wafers, cakes, donuts, chocolates, traditional sweets, as well as dairy products (milk, cream, cheeses). Interestingly, available data indicate that the levels of TFA in imported foods were higher as compared to locally produced items. For instance, Mashai et al. (72) showed that the levels of TFA in five imported popcorn items ranged from 2% to over 40% as compared to 1.26% in a locally produced popcorn. In addition, in KSA, Jradi et al. (76) have randomly collected 1,153 foods from fourteen stores in the Saudi market. Results showed that from the 228 products that had hydrogenated fat, 67.5% were imported, while 32.5% were locally produced (76).
Iran was the only country that showed decreasing TFA levels in vegetable oil, margarines and shortenings over time (Supplementary Table 3). Acknowledging that different countries/studies may have used various methods for the chemical determination of TFA levels in foods, the WHO has spearheaded the development of a standardized chemical analysis protocol for TFA assessment (98). This has been already implemented in Egypt and Jordan (94, 97), as well as Lebanon and Morocco (data not published yet) (Supplementary Table 3).
As for baseline data on KAB, this was collected in eight EMR countries (32%), including Iran, Iraq, Jordan, KSA, Oman, Pakistan and the UAE. Most of the KAB surveys included questions relating to (1) knowledge of TFA food sources and content, familiarity with the maximum daily allowance of TFA and the adverse health effects of high TFA intakes; and (2) consumers' behavior such as the use of partially hydrogenated oils and fats when cooking, or the consumption of high TFA food products (Supplementary Table 4) (75, 99–107). No studies assessed the attitudes of consumers toward TFA.
As shown in Table 1, national TFA reduction initiatives were identified in 14 out of the 22 countries of the EMR (63.6%). These countries include Bahrain, Egypt, Iran, Iraq, Jordan, KSA, Kuwait, Morocco, Oman, Pakistan, Palestine, Qatar, Tunisia and the UAE. GINA database has included a TFA reduction policy for Lebanon (151). More specifically, it referred to limiting the import, fabrication and marketing of high TFA products−2014. However, the GINA database has also specified that this initiative was not adopted in the country (151). Accordingly, and given that no other TFA reduction initiatives were identified during our systematic search, Lebanon was not considered as having national TFA reduction initiatives in this review. Similarly, it was reported that Afghanistan and Syria are preparing broad national nutrition or food policies, which will include TFA reduction (108), and that legislation/standards related to TFA limits in fats and oils and/or the use of PHOs are being developed or updated in Sudan (108, 109). However, no further details were found, and accordingly Afghanistan, Sudan and Syria were not considered as having TFA reduction initiatives in this review.
National strategies or action plans that express a commitment to reduce TFA in the food supply were identified in 12 countries of the region, as shown in Table 2. The identified recommendations and strategies were mainly led by governments, or by national multi-sectoral national committees that include governmental entities, as well as representatives from the food industry, academia and NGOs. In Pakistan, the responsibility for formulating and enacting TFA legislation has recently been transferred from provincial authorities to the Pakistan Standards and Quality Control Authority and a national action plan for industrial TFA elimination is being developed (108, 109). Six countries have specified targets for their population TFA intake (1% of EI or less), including Bahrain, Egypt, Iran, Jordan, KSA, and Morocco. As shown in Table 2, TFA reduction strategies in countries of the region were part of broader strategies or action plans targeting NCD or healthy diets and lifestyle.
All of the 14 countries listed in Table 1 (100%) are implementing some form of TFA limits or bans, with varying degrees in implementation and policy scope. In addition, except for Egypt, Iraq and Morocco, the other countries are implementing complementary TFA reduction interventions, with the most common being consumer education (10/14 countries; 71%), followed by food labeling (9/14 countries; 64%) and initiatives in specific settings (7/14 countries; 50%). Taxation was the least common implementation strategy. In fact, except for Qatar, where taxation of high TFA products is planned, and for Oman where taxation on the use of hydrogenated oils, was included as part of the National plan for the prevention and control of chronic non-communicable diseases 2016–2025 (not adopted yet) (143), none of the other countries have included taxation-based initiatives. Table 1 displays the details of the initiatives implemented in the various EMR countries.
Initiatives based on TFA bans or limits included the setting of limits for TFA levels in fats and oils, and other foods (such as bakery products, biscuits, cakes, snacks, and fast foods), and/or the banning or replacement of PHOs.
Iran is the first country in the region to have developed TFA regulation, a process that was initiated in 2005, when the standards for frying oil and mixed liquid oils were revised, setting the maximum level of TFA at 10%, down from over 20% (120). The 2% limit in oils and fats was later adopted, and became effective in 2016 (4, 110). In 2015, the Gulf Cooperation Council (GCC) Standardization Organization (GSO) has set TFA limits of 2% of total fat in vegetable oils and soft spreadable margarines, and 5% of total fat in other foods. The implementation of the regulation took effect in 2016 in Bahrain, while in KSA, UAE and Kuwait, it came into force in 2017. In Qatar, the GSO standard has been submitted to the cabinet in 2020 for endorsement (108), and in Oman, a ministerial decree has been issued stating that the Directorate of Standards should follow all GSO-approved standards.
As for regulating the use of PHO, KSA has become the first country to implement a complete ban on the use of PHO in food products (0 g) in 2020 (108, 110, 128, 129, 132). In Oman a Ministerial Decree to prohibit the use of PHOs is in preparation (155, 156). Iran implements a restriction of PHO use rather than a ban, while Iraq has removed the subsidy on PHOs, and replaced them by other types of oil (14, 50, 113, 122). In Oman, there has been a proposal to tax PHOs, but this has not been adopted or implemented yet (143). Jordan banned the use of PHOs in dairy products (50, 123, 124) and Pakistan has prohibited their use in formula milk (146). Initiatives that included TFA limits/bans were mandatory in 8 countries, including Bahrain, Iran, Jordan, KSA, Kuwait, Morocco, Oman and Palestine (8/14 countries; 57%) (Table 1).
Ten out of the 14 countries (71%) have implemented consumer education campaigns. These countries include Bahrain, Iran, Jordan, KSA, Kuwait, Oman, Palestine, Qatar, Tunisia, and the UAE (Table 1). While most awareness and educational campaigns were led solely by governmental entities, NGOs were collaborators in both Bahrain and Oman. Half of the countries had their consumer education initiatives specific to TFA (Bahrain, Kuwait, Palestine, Tunisia, and the UAE). The other half had broader campaigns in relation to saturated fats, salt, sugar and healthy lifestyle (Iran, Jordan, KSA, Oman, and Qatar).
Nine countries (64%), including Bahrain, Iran, Jordan, KSA, Kuwait, Oman, Pakistan, Qatar and the UAE, were found to have labeling initiatives specific to TFA. These initiatives were mandatory in Bahrain, Iran, KSA, Kuwait, Oman, Qatar and the UAE (7/9 countries; 78%), with the mandatory traffic light labeling scheme being implemented in Iran. In Jordan, and as part of the “National Strategy and Plan of Action Against Diabetes, Hypertension, Dyslipidemia and Obesity,” labeling of food products with TFA was set to be mandatory as of 2015, however this initiative has not been adopted yet (4, 127) (Table 1).
Seven countries (50%) are implementing TFA reduction initiatives in specific settings. These include Bahrain, Iran, Jordan, KSA, Kuwait, Oman and Qatar. Bahrain is targeting school canteens through the use of a prohibited food list and by introducing modifications to food preparation methods. Iran is implementing TFA educational interventions in schools and workplaces, while in Jordan, TFA reduction interventions are being implemented in public hospitals and royal medical services (108). Under the Nutrition-Friendly Schools Initiative, Kuwaiti schools are being targeted to raise nutrition and health awareness, with a focus on TFA intake reduction (136, 140). In Qatar, the adoption of the School Canteen Guidelines is mandatory in governmental schools, while the implementation of educational sessions in workplaces remain voluntary.
Other initiatives that have been implemented and shared with various governmental entities in KSA (hospitals, universities, military, or public places) include the replacement of PHOs and saturated fatty acids with unsaturated fatty acids (UFA) in offered foods (135). Similarly, the elimination of TFA in foods offered in governmental institutions in Kuwait has been proposed, although not adopted yet (138). In Oman, and as part of the National Plan for the Prevention and Control of Chronic Non-communicable Diseases 2016–2025, limiting high TFA items in schools is planned, but has not been implemented yet (143) (Table 1). Interventions or policy actions targeting the food service sector (such as restaurants and coffee-shops) were not identified in any country of the region.
Monitoring activities are being conducted in Iran and several GCC countries including Bahrain, KSA, Kuwait, and Qatar. In Iran, post marketing surveillance is conducted by the Food and Drug Organization on an annual basis. Accordingly, samples of edible oils and fats (frying oil, consumer edible vegetable oil, Margarine, minarine, and shortening), are analyzed to determine TFA levels (40). The Iran Standard Organization also monitors the TFA content in bakery products, biscuits and confectionary products. Ghazavi et al. collected samples of traditional sweets with nutritional labeling, and compared the TFA information on the label with actual TFA levels based on chemical analysis. Results showed that there was 81.8% discrepancy between the analytical levels and those listed on the label (65).
In Bahrain, monitoring activities focus on the monitoring of TFA content in samples of bakery products, and fats and oils via direct chemical analyses. Moreover, the listing and proper labeling of TFA on prepackaged products (both locally produced and imported) is being monitored in Bahrain. In KSA, the SFDA, in collaboration with the Ministry of Municipal and Rural Affairs, is responsible for monitoring and inspection activities, targeting food products that are locally produced or imported. Laboratory analyses are conducted in the SFDA laboratories. In 2020, SFDA launched a campaign to ensure that manufacturers and importers of food products comply with the Saudi Technical Regulation SFDA.FD 2483 “Trans fats (fatty acids).” The inspection focused on local and imported food products such as margarine, donuts, cakes, biscuits, pies, frozen pastries, cheese, chocolates, ice cream, and other items. The total number of samples that were chemically analyzed was of 2,697 (129, 159), and the percentage of violation was estimated at 20% (200 local products and 332 imported products). An older campaign conducted in 2018 to monitor compliance to TFAs limit in food products, showed that 94% of the 400 samples that were tested were compliant with the standards (110). In 2016–2017, Jradi et al. (76) conducted a study to assess compliance with SFDA nutritional facts requirements: only 38% met the SFDA requirements for nutritional information (energy, protein, carbohydrate, sugar, total fat, saturated fat, TFA, and sodium). Among the missing nutrients, TFA was the most frequently omitted (54.5%) from the nutritional facts.
In Kuwait, the National Technical Food Committee has developed a plan to monitor the implementation of the TFA standards (136). In collaboration with the food laboratory—Ministry of Health (MOH)- measures have been put in place to monitor, inspect and evaluate the compliance of the food industry by chemically analyzing TFA content in randomly selected samples of potentially high TFA food sources. In this context, a capacity-building program has been conducted by the Department of Standards and Inspection to enhance the inspectors' capabilities, and assure compliance of the food industry with the various GSO standards and technical regulations (Trans Fatty Acids GSO 2483/2015; Requirements of nutritional labeling. GSO 2233/2012; Nutritional and Health Claims Requirements. GSO 2333/2013). In addition, the TFA content declared on the nutrition facts is monitored to evaluate compliance with the technical regulation for TFA.
In Qatar, the Health Promotion and NCD Section of the Public Health Department at the Ministry of Public Health plays a role in the development of the School Canteen Guidelines, led by the Ministry of Education and Higher Education. The Health Promotion and NCD section of the Public Health Department at the MOPH has also developed and implemented the Food & Beverage Guidelines in Cafeterias and Vending Machines in all healthcare settings and workplaces that are part of the Workplace Wellness Program. An annual evaluation tool is administered to all hospitals and workplaces that are implementing the guidelines.
Very few countries have assessed the impact of TFA reduction initiatives on the population's intake levels. In addition, the majority of countries have only one estimate of TFA intake, and therefore the investigation of trend in TFA intake is not possible. The two exceptions are Iran and UAE. In Iran, the intake of TFA for the entire population (per capita) was estimated at 4.2% EI in 2001–2003, i.e., prior to policy implementation (39). This intake had decreased to 0.7% in 2018 as reported by Amerzadeh and Takian (41), post policy implementation. In the UAE, a study conducted amongst female university students had estimated TFA intake at 1.7% in 2014 (14) before the implementation of TFA reduction initiatives. Intake level has decreased to 1% in 2017–2018 in the same population group, post policy implementation (51).
Data on the impact of TFA reduction initiatives on the levels of TFA in food products is also scarce. Available evidence suggests that the legislations that were implemented in Iran resulted in a significant reduction in the level of TFAs content in edible oil. In fact, initiatives aimed at reducing the level of TFA in edible oils were launched in 2005, when the standards for frying oil and mixed liquid oils were revised to reduce the maximum level of TFA (to <10%, down from over 20%) (120), and when the Ministry of Commerce started the gradual replacement of hydrogenated oils by non-hydrogenated (specifically olive oil) and liquid frying oils (14, 50, 113). Peymani et al. assessed the impact of this policy on the levels of TFA in edible oils. Samples were collected randomly over a 6-year period, from 2002 to 2008, from different national edible oil manufacturers. Tests were conducted by the national referral laboratory in <city>Tehran</city>, Iran. Results showed that the TFA composition (%) of edible oil represented 27–29% in 2002–2003, 31.2% in 2004–2005, decreasing to 13.7% in 2007 and 5.6% in 2008 (121). Another study was conducted in 2014 by the Post Marketing Surveillance (PMS) in Iran: It targeted households in six provinces of Iran, whereby information on the types of fats and oils used for cooking as well as the purchase pattern and their amounts were obtained using questionnaires. In addition, the fatty acid profiles of consumed fats and oils were determined (40). The analysis of TFA in different kinds of oils (frying oil, consumer edible vegetable oil, margarine, minarine, and shortening) was performed. Results showed that the TFA content of edible oils has been reduced to <5% TFAs (40).
This systematic review is the first to focus on TFA reduction initiatives in the EMR, a region that is currently witnessing an increasing burden of cardiovascular morbidity and mortality (13). It showed that out of the 22 countries of the EMR, nine have assessed TFA intake in the population (41%), nine (41%) have evaluated TFA levels in food items, and fourteen (63.6%) have implemented national TFA reduction initiatives. The most common TFA reduction initiatives were based on TFA limits or bans in an effort to decrease/eliminate TFAs from the food supply, while the least common was taxation.
Based on available national studies conducted in countries of the region, the population's TFA intake levels were found to range between 0.34% EI in Morocco and 6.5% EI in Egypt (4, 49), while subnational studies reported estimates ranging between 0.1% EI in Sudan and 2.3–2.4% EI in Lebanon (14, 48). Available data highlight very high intake levels in Egypt (6.5% EI) (4) and Pakistan (5.7% EI) (4). These estimates are 5–6 fold higher than the upper limit of 1% EI specified by the WHO (160, 161) and the American Heart Association (162), and significantly higher that the optimal level defined by the Global Burden of Disease (GBD) collaborators, in their evaluation of dietary risk factors (0.5% EI, with an optimal range of 0–1% EI) (163). Based on the 2019 GBD data, the Institute for Health Metrics and Evaluation (IHME) has assessed the burden of CHD attributable to high TFA intake (>0.5% EI) in each country worldwide (4, 12). Accordingly, the top ten countries included three from the EMR: Egypt was ranked at the top of the list as the country with the highest burden of CHD due to high TFA intake in the world (8.4% of CHD deaths), Iran ranked as the third (6.96% of CHD deaths) and Pakistan as the ninth (4.94% of CHD deaths) (12).
Countries that had very low estimates of TFA intake included Morocco (0.34% EI) (49), Jordan (0.5–0.6% EI) (14) and Sudan (0.1% EI) (14). It is important to mention that dietary estimates of TFA intake should be interpreted with caution. These are in fact limited by the available food composition databases that either have a large number of missing data for TFA levels in foods, or are not culture-specific (164). Without country- or region-specific data, TFA elimination would often not be recognized as a priority for time and resource investment (12). Acknowledging this challenge, the WHO has published a standardized protocol for TFA analysis (98) that can be adapted for measuring TFA levels in national food supplies in different settings (12), and the WHO EMRO has supported the launch of TFA analysis projects in several Member States. This endeavor has been already completed in Egypt, Lebanon, Morocco (data not published yet), and Jordan (94). Such data should help in enhancing the robustness and accuracy of future TFA dietary assessment in countries of the region.
Very few studies have reported on TFA intake amongst children and adolescents in the EMR, although evidence suggests that this age group may have the highest TFA intake level given their tendency to consume “fashionable” processed foods as well as fast foods (165). In Iran, TFA intake amongst 6–18 year old children and adolescents was reported at 2.2–2.3% EI in 2019 (43). This estimate highlights that TFA intake remains high in this age group, even after the implementation of TFA reduction initiatives which have been launched as of 2005 (4, 14, 41, 50, 57, 105, 108, 110, 113–121). More attention should be devoted to this age group, and their food consumption patterns, since high TFA intakes in this period of the lifecycle may increase the risk for early onset CVD and related comorbidities (165).
The number of countries adopting TFA limits or bans to reduce TFA levels in the food supply is estimated at 14 (63.6%), with significant disparities between countries in policy scope and coverage. The main disparities were noted in whether the limits/bans were mandatory or not (8 mandatory vs. 6 voluntary), and the number and types of foods targeted by the standards. Iran is the first country to have adopted TFA limits and regulations in the region, while KSA is the first to have implemented a best-practice policy according to the WHO (12). A best-practice policy is defined as “Legislative or regulatory measures that limit industrially produced TFA in foods in all setting. The two best-practice policies for TFA elimination are: Mandatory national limit of 2 g of industrially produced TFA per 100 g of total fat in all foods; and Mandatory national ban on the production or use of PHO as an ingredient in all foods.” Countries of the GCC have all adopted or are on the way of implementing the GSO standards for TFA which set TFA limits at 2% of total fat in vegetable oils and soft spreadable margarines, and 5% of total fat in other foods (12). More work needs to be done in the other EMR countries that do not have any TFA replacement strategy. In fact, policy interventions to eliminate industrial TFAs from food have been proposed as the most effective public health approach for reducing TFA intake and reducing the burden of NCDs (166). Based on several modeling studies, a recent systematic review showed that policies that set TFA limits are likely to be cost-saving in addition to having the greatest impact on lower socioeconomic groups (9). These are vital considerations for policymakers in countries of the region in terms of deciding whether or not to adopt a TFA reduction policy (9). Downs et al. argued that TFA bans make sense from both an economic standpoint as well as an ethical perspective, given that they could contribute to reducing social inequities (9). It is however also acknowledged that the adoption of a TFA removal policy will also require substantial political commitment and a high level of public pressure for change, which may not be readily available or achievable in many countries of the region (6).
Besides TFA limits or bans, complementary TFA reduction approaches have been implemented in several countries of the region. This is a positive finding given that multicomponent interventions, including a legislative ban on high TFA products, may increase the impact and effectiveness of TFA reduction strategies (6). Consumer education was the most common complementary approach in countries of the EMR, with the aim of raising awareness about TFA, its main dietary sources and its adverse health effects. For instance, the reduction of TFA intake has been included in country-specific food-based dietary guidelines in Jordan and Qatar. Such guidelines and their communication to the public has been recognized as a practical and effective approach in improving the consumer's dietary knowledge and attitudes (167, 168). While none of the countries had assessed consumers' attitude toward TFA, the few available studies that have assessed consumers' knowledge had in fact shown that consumers have poor or little knowledge related to the sources of TFA (101) and the potential health effects of excessive TFA consumption (102). From the few available studies on practices, one study conducted in KSA, has shown that the vast majority of adolescents and adults are not interested in checking TFA-related information on the food label (75). While, few studies have shown that a large percentage of consumers (31.5–45%) continue to use high TFA sources (e.g., hydrogenated vegetable oils) in Iran and Pakistan (99, 105, 106), other studies reported much smaller estimates (0–7.3%) in Iran, Iraq, KSA and the UAE (100, 103, 104, 107). It is recommended that countries of the region consult findings stemming from the available knowledge and practice investigations when developing or further tailoring their consumer education initiatives in order to address culture-specific gaps in knowledge and identify barriers against TFA reduction. Acknowledging that labeling can be an important element of national strategies aimed at improving the population's diets and reducing TFA intake (6), a promising finding of this review is the fact that TFA-specific labeling initiatives are being implemented or planned in 9 countries of the region. Of these, front of pack labeling, which is recognized as being easily understood by the consumer (169), is being implemented in Iran. The fact that taxation was the least implemented/adopted in the region is in line with reports from other parts of the world (6).
This review showed that a number of countries have included a legislative component within their TFA reduction strategies, instead of implementing solely voluntary initiatives. Previous studies have shown that mandatory or legislative approaches tend to be more effective, producing more significant reductions in TFA intake levels within the population, compared to voluntary approaches (6). A recent systematic review has concluded that, although all policy approaches may lead to reductions in TFA levels in foods and subsequent intakes, stronger policies (i.e., mandatory TFA limits or bans) will have more pronounced effects than voluntary food reformulation or labeling approaches (6).
The implementation of clear monitoring activities is essential to demonstrate program effectiveness, and to incite greater impact on TFA reduction (12). In the EMR, five countries only (Iran, Bahrain, KSA, Kuwait, and Qatar) have established mechanisms for the monitoring of TFA content in edible oils, fats, bakery and snack products, using laboratory analyses. The lack of laboratory capacity to perform TFA measurements in foods, especially in lower-resourced countries, may in fact be a barrier to monitoring and enforcement (12). Some countries in the region have mandatory labeling (TFA declaration on nutrient facts panels and/ or PHO on the ingredients list), which should ensure compliance with regulations. However, even when labeling requirements are already in place, it is crucial for countries to be able to confirm, through laboratory testing, that the food industry is complying with the information on the labels. For those countries that do not have mandatory labeling requirements, these have to rely solely on laboratory testing of TFA levels to monitor compliance. More work needs to be done to support countries, particularly in low resource settings, in conducting TFA laboratory analyses. An additional measure that can be explored is the identification of laboratories in the region that have demonstrated capacities for analyzing TFAs in foods and which can support laboratory testing in neighboring countries (12).
Data on the impact of TFA reduction initiatives is scarce in the region. Except for Iran and the UAE, where there is evidence of a decrease in the population's TFA intake after the implementation of TFA reduction strategies (14, 39, 41, 51), none of the other countries have conducted impact evaluation. The impact on TFA levels in foods is also sparsely described, with only Iran having provided such evidence (41, 116, 170). The scarcity of data may be partially due to the fact that many reduction initiatives in the region are relatively recent and there has been insufficient time to assess impact. There is a need for well-designed impact evaluations in countries of the region. The WHO analytical protocol for TFA analysis (98) provides a valuable tool for such undertakings, allowing for the implementation of standardized methodologies in the analysis of TFA in foods and hence the documentation of change in TFA levels over time. Standardized comparable dietary approaches to measuring TFA intake in the population are also needed. Although dietary approaches carry their own inherent limitations in TFA intake assessment (164), if the adopted method of assessment is consistent, it can still be a useful measure of change over time (171, 172). Since the regular measurement of changes in population TFA intake and in TFA levels in foods may be complex and costly, the incorporation of process evaluations that examine the strategy implementation and its progress, collects process indicators, and identifies existing barriers and facilitators of implementation is also vital in providing real-time information and identifying specific areas for improvement (173).
This review has a number of strengths and limitations. This is the first systematic review of existing TFA reduction initiatives in countries of the EMR, their implementation and progress over time. In addition to the systematic search of databases and gray literature, additional input was sought from focal points or program leaders in the various countries that were identified as having existing TFA reduction initiatives, to verify and obtain supplementary country-specific data. Although not all country contacts were identified and there were some non-respondents, the triangulation of data from multiple sources allowed us to document the existing initiatives and implementation of strategies, and present the information in a relatively standardized manner. Through this, it is unlikely that any major TFA reduction initiatives were omitted, although this possibility cannot be totally disregarded. While one of the major strengths of the review is the fact that it included a comprehensive search of the gray literature, comprising governmental reports, presentations or questionnaires completed by country program leaders, a potential limitation associated with this approach is the fact that the methodological rigor within some of the reports is not ascertained. More specifically, the robustness of the studies, their methodology and the quality of the data used for the assessment of TFA intake and TFA levels in foods were not assessed and hence should be interpreted with caution. It is also important to note that studies that have reported on TFA intake were scarce and that dietary estimation of TFA intake levels is by itself limited by the scarcity of up-to date, culture-specific food composition databases.
Despite the ongoing TFA reduction initiatives in several countries of the region, this study showed that intake estimates from several countries of the EMR remain high, exceeding the WHO upper limit of 1%. This review has also shown that 14 countries (63.6%) have adopted TFA limits or bans to reduce TFA levels in the food supply, albeit with significant disparities between countries in policy scope and coverage. It is recommended that all countries of the region align with the global best practice policies by implementing a ban on PHO and setting mandatory national limit of 2 g of industrially produced TFA per 100 g of total fat in all foods (12). Further action is needed to make sure that countries strengthen their regulatory capacities to help accelerate implementation, compliance monitoring and enforcement of TFA policy actions, and meet the targeted elimination of industrially produced TFA in 2023.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
AA-J and LN: conceptualization, investigation, resources, and supervision. LN: methodology and writing—original draft preparation. SN: systematic database search. MT, AC, and LN: data curation. MT and AA-J: writing—review and editing. AA-J: project administration. ZA, BA, NA, MMA, SA, RA, SAA, MHA, NB, RB, FB, LE, JE, MH, HM, and MN: critical review of country-specific data and of manuscript. All authors have read and agreed to the published version of the manuscript.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fnut.2021.771492/full#supplementary-material
CHD, coronary heart disease; CVD, cardiovascular diseases; DV, daily value; EI, energy intake; EMR, Eastern Mediterranean Region; EMRO, Regional Office for the Eastern Mediterranean; FBDG, food-based dietary guideline; FNA, Food and nutrition authority; GBD, global burden of disease; GCC, Gulf Cooperation Council; GINA, Global database on the implementation of nutrition action; GSO, GCC standardization organization; HDL, high-density lipoprotein; KAB, knowledge, attitudes and behavior; KP, Khyber Pakhtunkhwa; KSA, Kingdom of Saudi Arabia; LDL, low-density lipoprotein; MOCI, Ministry of commerce and industry; MOH, Ministry of health; MOHAP, Ministry of health and prevention; MOHME, Ministry of health and medical education; MOHP, Ministry of health and population; MOPH, Ministry of public health; NA, not available; NCD, non-communicable disease; NFP, nutrition focal point; NGO, non-governmental organization; PHFS, Patient helping fund society; PHOs, partially hydrogenated oils; PMS, post marketing surveillance; PSQCA, Pakistan standard and quality control authority; SFA, Saturated fatty acid; SFDA, Saudi food and drug authority; TFA, Trans fatty acid; UAE, United Arab Emirates; UFA, Unsaturated fatty acid; WHO, World Health Organization.
1. World Health Organization. Cardiovascular Diseases. Available online at: https://www.who.int/health-topics/cardiovascular-diseases#tab=tab_1 (accessed 25 January 2021).
2. Verneque BJF, Machado AM, de Abreu Silva L, Lopes ACS, Duarte CK. Ruminant and industrial trans-fatty acids consumption and cardiometabolic risk markers: a systematic review. Crit Rev Food Sci Nutr. (2020) 1–11. doi: 10.1080/10408398.2020.1836471. [Epub ahead of print].
3. Persistence Research Market. PHO and Non PHO Based Oils and Fats Market: Global Industry Analysis 2013–2017 and Forecast 2018–2026. New York, NY: Persistence Research Market (2018).
4. Wang Q, Afshin A, Yakoob MY, Singh GM, Rehm CD, Khatibzadeh S, et al. Impact of nonoptimal intakes of saturated, polyunsaturated, and trans fat on global burdens of coronary heart disease. J Am Heart Assoc. (2016) 5:e002891. doi: 10.1161/JAHA.115.002076
5. Mozaffarian D, Willett WC. Trans fatty acids and cardiovascular risk: a unique cardiometabolic imprint? Curr Atheroscler Rep. (2007) 9:486–93. doi: 10.1007/s11883-007-0065-9
6. Hyseni L, Bromley H, Kypridemos C, O'Flaherty M, Lloyd-Williams F, Guzman-Castillo M, et al. Systematic review of dietary trans-fat reduction interventions. Bull World Health Organ. (2017) 95:821–30. doi: 10.2471/BLT.16.189795
7. World Health Organization. Web-Based Consultation on the Development of a Global Monitoring Framework and Targets for the Prevention and Control of NCDs. New York, NY: World Health Organization (2012). Available online at: https://www.who.int/nmh/events/2012/ncd_discussion_paper/en/
8. Mozaffarian D, Jacobson MF, Greenstein JS. Food reformulations to reduce trans fatty acids. N Engl J Med. (2010) 362:2037–39. doi: 10.1056/NEJMc1001841
9. Downs SM, Bloem MZ, Zheng M, Catterall E, Thomas B, Veerman L, et al. The impact of policies to reduce trans fat consumption: a systematic review of the evidence. Curr Dev Nutr. (2017) 1:117–26. doi: 10.3945/cdn.117.000778
10. Micha R, Khatibzadeh S, Shi P, Fahimi S, Lim S, Andrews KG, et al. Global, regional, and national consumption levels of dietary fats and oils in 1990 and 2010: a systematic analysis including 266 country-specific nutrition surveys. BMJ. (2014) 348:g2272. doi: 10.1136/bmj.g2272
11. World Health Organization. WHO Plan to Eliminate Industrially-Produced Trans-Fatty Acids From Global Food Supply. Available online at: https://www.who.int/news/item/14-05-2018-who-plan-to-eliminate-industrially-produced-trans-fatty-acids-from-global-food-supply (accessed 1 June (2021)
12. World Health Organization. Countdown to 2023: WHO Report on Global Trans-Fat Elimination 2019. Geneva: World Health Organization (2019). Available online at: https://apps.who.int/iris/bitstream/handle/10665/331300/9789241516440-eng.pdf?sequence=1&isAllowed=y
13. Mokdad A, Tehrani-Banihashemi A, Moradi-Lakeh M, El Bcheraoui C, Charara R, Afshin A, et al. Burden of cardiovascular diseases in the Eastern Mediterranean Region, 1990-2015: findings from the global burden of disease 2015 study. Int J Public Health. (2018) 63:S1. 137–49. doi: 10.1007/s00038-017-1012-3
14. Al Jawaldeh A, Al-Jawaldeh H. Fat intake reduction strategies among children and adults to eliminate obesity and non-communicable diseases in the Eastern Mediterranean region. Child Basel. (2018) 5:89–107. doi: 10.3390/children5070089
15. World Health Organization Regional Office for the Eastern Mediterranean. Strategy on Nutrition for the Eastern Mediterranean Region 2020–2030. Cairo: World Health Organization (2019). Available online at: https://applications.emro.who.int/docs/9789290222996-eng.pdf
16. Santos JA, Tekle D, Rosewarne E, Flexner N, Cobb L, Al-Jawaldeh A, et al. A systematic review of salt reduction initiatives around the world: a midterm evaluation of progress towards the 2025 global non-communicable diseases salt reduction target. Adv Nutr. (2021) 12:1768–80. doi: 10.1093/advances/nmab008
17. World Health Organization Regional Office for the EasternMediterranean. Countries in the Eastern Mediterranean Region. Available online at: http://www.emro.who.int/countries.html (accessed October 7, 2021).
18. CAB International. CAB Direct. Available online at: https://www.cabdirect.org/ (accessed February 17, 2021).
19. Directory of Open Access Journals. Available online at: https://www.doaj.org/ (accessed February 17, 2021).
20. Google. Google Scholar. Available online at: https://scholar.google.com/ (accessed February 17, 2021).
21. Ovid. MEDLINE. Available online at: https://ovidsp.dc2.ovid.com/ovid-a/ovidweb.cgi (accessed February 18, 2021).
22. National Library of Medicine. Pubmed. Available online at: https://pubmed.ncbi.nlm.nih.gov/ (accessed February 18, 2021).
23. Elsevier. Scopus. Available online at: https://www.scopus.com/standard/marketing.uri#basic (accessed February 18, 2021).
24. Clarivate. Web of Science Core Collections. Available online at: https://www.webofscience.com/wos/woscc/basic-search (accessed February 19, 2021).
25. EBSCO. Food Science and Technology Abstracts. Available online at: https://web.a.ebscohost.com/ehost/search/basic?vid=0&sid=6fc621d0-de07-408a-9c52-1aa847338022%40sdc-v-sessmgr03 (accessed February 19, 2021).
26. Al, Manhal,. Available online at: https://platform.almanhal.com/ (accessed February 19, 2021).
27. EBSCO. Arab World Research Source. Available online at: https://web.b.ebscohost.com/ehost/search/basic?vid=0&sid=c408c320-39e4-4969-8c91-4e9e892fd2c0%40pdc-v-sessmgr03 (accessed February 20, 2021).
28. E-Marefa. Available online at: https://search.emarefa.net/en (accessed February 20, 2021).
29. Ministry of Higher Education and Scientific Research of Iraq. Iraqi Academic Scientific Journals. Available online at: https://www.iasj.net/iasj?func=search&uiLanguage=en (accessed February 20, 2021).
30. OpenGrey. Available online at: http://www.opengrey.eu/ (accessed March 1, 2021).
31. Google. Available online at: https://www.google.com/ (accessed March 8, 2021).
32. World Healh Organization. Global Database on the Implementation of Nutrition Action. Available online at: https://extranet.who.int/nutrition/gina/en/policies/summary (accessed March 15, 2021).
33. World Health Organization Regional Office for the Eastern Mediterranean. Available online at: http://www.emro.who.int/index.html (accessed March 22, 2021).
34. Resolve to save lives-an initiative of vital strategies. 7-Step Guide for Country Policy Makers to Develop and Implement a Trans Fat Elimination Policy: Fact Sheet. New York, NY: Resolve to Save Lives. Available online at: https://linkscommunity.org/assets/PDFs/7-step-trans-fat-elimination-guide_fact-sheet.pdf
35. World Health Organization. REPLACE Trans Fat. Available online at: https://www.who.int/teams/nutrition-and-food-safety/replace-trans-fat (accessed July 26, 2021).
36. Resolve to save lives-an initiative of vital strategies. Policy Inventory for Effective Trans Fat Regulations: Fact Sheet. New York, NYUS: Resolve to Save Lives. Available online at: https://linkscommunity.org/assets/PDFs/policy-inventory-for-effective-tfa-regulations_fact-sheet.pdf
37. Colón-Ramos U, Monge-Rojas R, Campos H. Impact of WHO recommendations to eliminate industrial trans-fatty acids from the food supply in Latin America and the Caribbean. Health Policy Plan. (2014) 29:529–41. doi: 10.1093/heapol/czt034
38. Downs SM, Thow AM, Leeder SR. The effectiveness of policies for reducing dietary trans fat: a systematic review of the evidence. Bull World Health Organ. (2013) 91:262–69. doi: 10.2471/BLT.12.111468
39. Mozaffarian D, Abdollahi M, Campos H, Houshiarrad A, Willett W. Consumption of trans fats and estimated effects on coronary heart disease in Iran. Eur J Clin Nutr. (2007) 61:1004–10. doi: 10.1038/sj.ejcn.1602608
40. Esmaeili M, Abdollahi M, Abdollahi Z, Salehi F, Ajami M, Houshiarrad A. Effect of Policymaking to Reduce TFA Intake in 6 Provinces of Iran. Tehran: National Nutrition and Food Technology Research Institute (2014).
41. Amerzadeh M, Takian A. Reducing sugar, fat, and salt for prevention and control of noncommunicable diseases (NCDs) as an adopted health policy in Iran. Med J Islam Repub Iran. (2020) 34:136–43. doi: 10.47176/mjiri.34.136
42. Hosseini H, Abedi A, Abdollahi Z, Hajfaraji M, Mohammadi A. Fatty Acid Compositions of Frequently Consumed Edible Fat and Oil in Iran With Special Emphasis on Trans Fatty Acids. Tehran: Department of Research of Food Technology, National Nutrition and Food Technology Research Institute, Shahid Beheshti University of Medical Sciences (2013).
43. Mirmiran P, Ziadlou M, Karimi S, Hosseini-Esfahani F, Azizi F. The association of dietary patterns and adherence to WHO healthy diet with metabolic syndrome in children and adolescents: Tehran lipid and glucose study. BMC Public Health. (2019) 19:1457. doi: 10.1186/s12889-019-7779-9
44. Alkurd RA. Estimated intakes of fats, cholesterol, fiber, sodium, calcium, potassium, and magnesium in Jordan. Aust J Basic Appl Sci. (2011) 5:3171–78. Available online at: http://citeseerx.ist.psu.edu/viewdoc/download?doi=10.1.1.378.4001&rep=rep1&type=pdf
45. Takruri HR, Alkurd RA. Intakes of fats, cholesterol, fiber and micronutrients as risk factors for cardiovascular disease in Jordan. Jordan J Biol Sci. (2014) 7:119–26. doi: 10.12816/0008225
46. Tayyem RF, Albataineh SR, Allehdan SS, Badran EF. Development and validation of a food frequency questionnaire for assessing nutrient intake during childhood in Jordan. Nutr Hosp. (2020) 37:1095–106. doi: 10.20960/nh.03079
47. Moghames P, Hammami N, Hwalla N, Yazbeck N, Shoaib H, Nasreddine L, et al. Validity and reliability of a food frequency questionnaire to estimate dietary intake among Lebanese children. Nutr J. (2016) 15:1–12. doi: 10.1186/s12937-015-0121-1
48. Farhat AG, Jaalouk D, Moukarzel SR, Ayoub JJ. Consumption of trans fatty acid and omega 6 to omega 3 ratio in Lebanese adults. Nutr Food Sci. (2016) 46:120–29. doi: 10.1108/NFS-07-2015-0089
49. Ministry of Health-Morocco World Health Organization. Reduction, Replacement or Elimination Trans Fatty Acids in Foods. Rabat: Ministry of Health-Morocco (2020).
50. Al Jawaldeh A, Al-Jawaldeh H. Scaling up obesity and NCD prevention in the Eastern Mediterranean region through fat reduction intake strategies at population levels. Preprints. (2018) 2018:2018040218. doi: 10.20944/preprints201804.0218.v1
51. Ismail LC, Hashim M, Jarrar AH, Mohamad MN, Saleh ST, Jawish N, et al. Knowledge, attitude, and practice on salt and assessment of dietary salt and fat intake among university of sharjah students. Nutrients. (2019) 11:941–55. doi: 10.3390/nu11050941
52. Abd El-Gawad IA, Hamed EM, Zidan MA, Shain AA. Fatty acid composition and quality characteristic of some vegetable oils used in making commercial imitation cheese in Egypt. J Nutr Food Sci. (2015) 5:380–84. doi: 10.4172/2155-9600.1000380
53. Sadek MAS, Daoud JR, Ahmed HY, Mosaad GM. Nutritive value and trans fatty acid content of fast foods in Qena city, Egypt. Nutr Food Sci. (2018) 48:498–509. doi: 10.1108/NFS-11-2017-0235
54. Taher E, El-Essawy H, Saudi A, Aly S. Fatty acid profile of some fat rich foods with special reference to their trans fatty acids content. Int J Pharm Chem Sci. (2018) 7:31–7. Available online at: https://www.researchgate.net/publication/327557156_Fatty_Acid_Profile_of_Some_Fat_Rich_Foods_with_Special_Reference_to_their_Trans_Fatty_Acids_Content
55. Abdel-Moemin AR. Consumer satisfaction and nutrient profile of reformulated dry soups. Agricultura. (2014) 11:27–34. Available online at: https://www.dlib.si/stream/URN:NBN:SI:DOC-KLVSNLI8/3b109178-5cc3-4ea6-b2bd-46bd54eebabb/PDF
56. Jamali A, Moslemi M, Akramzadeh N, Khaneghah AM, Dadgarnejad M. Safety factors of oils marketed in Iran and applicable strategies in control of food derived cardiovascular diseases. Curr Nutr Food Sci. (2020) 16:571–77. doi: 10.2174/1573401315666181204110604
57. Saghafi Z, Zargaraan A, Tabibiazar M, Hosseini H. Is trans fatty acid still an issue for policy makers in Iran? A technical report. Nutr Food Sci Res. (2018) 5:47–51. doi: 10.29252/nfsr.5.2.47
58. Farmani J, Gholitabar A. Characterization of vanaspati fat produced in Iran. J Am Oil Chem Soc. (2015) 92:709–16. doi: 10.1007/s11746-015-2641-4
59. Butt MS, Sultan MT. Levels of trans fats in diets consumed in developing economies. J AOAC Int. (2009) 92:1277–83. doi: 10.1093/jaoac/92.5.1277
60. Hajimahmoodi M, Arami S, Nosrati M, Moghaddam G, Sadeghi N, Oveisi MR, et al. Trans fatty acid content of iranian edible oils. Food Nutr Sci. (2013) 4:1167–74. doi: 10.4236/fns.2013.411150
61. Chaharmahali NV, Asadollahi S, Hosseini E. Measurement and comparison of trans fatty acids amount in some of the vegetable oils, frying oils and animal and vegetable fats in Iran. Int J Bio-Inorg Hybr Nanomater. (2018) 7:59–64. Available online at: http://ijbihn.iauvaramin.ac.ir/article_661308_2c4be74369787ba8fb04bbb56c17c91c.pdf
62. Abedi AS, Hosseini H, Mohammadi A, Abdollahi Z, Hajifaraji M, Khaneghah AM. Fatty acid (FA) compositions and trans content of frequently consumed edible oils and fats from iran' market. Curr Nutr Food Sci. (2016) 12:56–64. doi: 10.2174/1573401311666150930215645
63. Stender S. Trans fat in foods in Iran, South-Eastern Europe, caucasia and central Asia: a market basket investigation. Food Policy. (2020) 96:101877–86. doi: 10.1016/j.foodpol.2020.101877
64. Pasdar Y, Bahrami G, Alghasi S, Darbandi M, Hemati Azandaryani A, Bahrami S, et al. Trans fatty acids contents among selected foods in Western Iran. Int J Health Life Sci. (2016) 2:32–41. Available online at: https://en.civilica.com/doc/752250/
65. Ghazavi N, Rahimi E, Esfandiari Z, Shakerian A. Accuracy of the amount of trans-fatty acids in traffic light labelling of traditional sweets distributed in Isfahan, Iran. ARYA Atheroscler. (2020) 16:79–84. doi: 10.22122/arya.v16i2.2005
66. Nazari B, Asgary S, Azadbakht L. Fatty acid analysis of Iranian junk food, dairy, and bakery products: special attention to trans-fats. J Res Med Sci. (2012) 17:952–57. Available online at: https://www.proquest.com/docview/1312683984/citation/F4F1B50C56764213PQ/1?accountid=8555
67. Teimouri M, Najafi M, Eskandarion MR, Parto F. Assessment of Trans Fatty Acids content in Iranian food products. Innov Food Technol. (2014) 2:93–100. doi: 10.22104/JIFT.2014.69
68. Bahrami G, Mirzaeei S, Kiani A, Atefi G. Assessment of profile of fatty acids and trans fats in hydrogenated oils in Iran. J Kermanshah Univ Med Sci. (2003) 7:1–2. doi: 10.22110/JKUMS.V7I1.860
69. Pasdar Y, Bahrami G, Karvand F, Khodadoost M, Rezaei M, Niazi S. Determining the fatty acid content of the most common meat products in Kermanshah, Iran. Jorjani Biomed J. (2013) 1:42–51. Available online at: http://goums.ac.ir/jorjanijournal/article-1-120-en.html
70. Asgary S, Nazari B, Sarrafzadegan N, Parkhideh S, Saberi S, Esmaillzadeh A, et al. Evaluation of fatty acid content of some Iranian fast foods with emphasis on trans fatty acids. Asia Pac J Clin. (2009) 18:187–92. doi: 10.6133/APJCN.2009.18.2.06
71. Asgary S, Nazari B, Sarrafzadegan N, Saberi S, Azadbakht L, Esmaillzadeh A. Fatty acid composition of commercially available Iranian edible oils. J Res Med Sci. (2009) 14:211–15. Available online at: https://pdfs.semanticscholar.org/f3b0/fab82f684f81734bcadf0a38adfd37114863.pdf?_ga=2.224134749.756192505.1636364596-1571069892.1585236721
72. Mashai R, Ai-Ismail K, Al-Domi H, Al-Mousa T. Variability in trans fatty acid content of selected local and imported foods in Jordan. Riv Ital Sostanze Gr. (2012) 89:193–200. Available online at: https://www.academia.edu/21339388/Variability_in_trans_fatty_acid_content_of_selected_local_and_imported_foods_in_Jordan
73. Bakeet ZAN, Alobeidallah FMH, Shaista A. Fatty acid composition with special emphasis on unsaturated trans fatty acid content in margarines and shortenings marketed in Saudi Arabia. Int J Biosci. (2013) 3:86–93. Available online at: https://www.cabdirect.org/cabdirect/abstract/20133097510
74. Alfawaz MA. Trans fatty acids in a selection of foods and oils available in Riyadh markets. Bull Fac Agric Cairo Univer. (2004) 55:315–30.
75. Kamel S, Al Otaibi H. Trans-fats declaration, awareness and consumption in Saudi Arabia. Curr Res Nutr Food Sci. (2018) 6:748–56. doi: 10.12944/CRNFSJ.6.3.17
76. Jradi H, AlMughthem A, Bawazir AA. Does the Current Scope of Nutrition Labelling Provided in the Saudi Markets Cope With the Increasing Trend of Chronic Disease? Durhan: Research square (2020). doi: 10.21203/rs.2.23201/v1
77. Al-Amiri HA, Ahmed N, Al-Sharrah T. Fatty acid profiles, cholesterol composition, and nutritional quality indices of 37 commonly consumed local foods in Kuwait in relation to cardiovascular health. medRxiv. (2020) 1–28. doi: 10.1101/2020.11.18.20233999
78. Nasreddine L, Naja F, Sibai A-M, Helou K, Adra N, Hwalla N. Trends in nutritional intakes and nutrition-related cardiovascular disease risk factors in Lebanon: the need for immediate action. Leb Med J. (2014) 62:83–91. doi: 10.12816/0004102
79. Saadeh C, Toufeili I, Zuheir Habbal M, Nasreddine L. Fatty acid composition including trans-fatty acids in selected cereal-based baked snacks from Lebanon. J Food Compost Anal. (2015) 41:81–5. doi: 10.1016/j.jfca.2015.01.014
80. Saade CN. Fatty Acid Composition, Including Trans Fatty Acids, of Some Local and Regional Bakery and Snack Products in the Lebanese Market-by Carol Nakhle Saade. Beirut: American University of Beirut (2007).
81. Sherazi S, Kandhro A, Mahesar S, Bhanger M, Talpur MY, Arain S. Application of transmission FT-IR spectroscopy for the trans fat determination in the industrially processed edible oils. Food Chem. (2009) 114:323–27. doi: 10.1016/j.foodchem.2008.09.058
82. Tarar OM, Ahmed KM, Nishtar NA, Achakzai AB, Gulzar Y, Delles C, et al. Understanding the complexities of prevalence of trans fat and its control in food supply in Pakistan. J Clin Hypertens. (2020) 22:1338–46. doi: 10.1111/jch.13943
83. Anwar F, Bhanger M, Iqbal A, Sultana B. Fatty acid composition of different margarines and butters from Pakistan with special emphasis on trans unsaturated contents. J Food Qual. (2006) 29:87–96. doi: 10.1111/j.1745-4557.2006.00058.x
84. Mahesar S, Kandhro AA, Cerretani L, Bendini A, Sherazi S, Bhanger M. Determination of total trans fat content in Pakistani cereal-based foods by SB-HATR FT-IR spectroscopy coupled with partial least square regression. Food Chem. (2010) 123:1289–93. doi: 10.1016/j.foodchem.2010.05.101
85. Karim Z, Khan KM, Ahmed S, Karim A. Assessment of trans fatty acid level in French fries from various fast food outlets in Karachi, Pakistan. J Am Oil Chem Soc. (2014) 91:1831–36. doi: 10.1007/s11746-014-2530-2
86. Sherazi S, Kandhro AA, Mahesar S, Talpur MY, Latif Y. Variation in fatty acids composition including trans fat in different brands of potato chips by GC-MS. Pak J Anal Environ Chem. (2010) 11:36–41. Available online at: https://www.researchgate.net/publication/236021398_Variation_in_Fatty_Acids_Composition_Including_Trans_Fat_in_Different_Brands_of_Potato_Chips_by_GC-MS
87. Kandhro A, Sherazi S, Mahesar S, Bhanger M, Talpur MY, Arain S. Monitoring of fat content, free fatty acid and fatty acid profile including trans fat in Pakistani biscuits. J Am Oil Chem Soc. (2008) 85:1057–61. doi: 10.1007/s11746-008-1297-8
88. Shah F, Rasool G, Sharif MK, Pasha I, Ahmad S, Sharif HR. Determination of trans fat in traditional Pakistani breakfast and snack foods. Int Food Res J. (2016) 23:849–53.
89. Aftab A, Sherazi S, Rubina S, Razia S, Arfa Y. Consequence of fatty acids profile including trans fat in chocolate and pastry samples. Int Food Res J. (2013) 20:601–05. Available online at:https://www.semanticscholar.org/paper/Consequence-of-fatty-acids-profile-including-trans-Aftab-Sherazi/17701e734d0c97aad1f029d01801d52d13a2e615
90. Kandhro A, Sherazi S, Mahesar S, Bhanger M, Talpur MY, Rauf A. GC-MS quantification of fatty acid profile including trans FA in the locally manufactured margarines of Pakistan. Food Chem. (2008) 109:207–11. doi: 10.1016/j.foodchem.2007.12.029
91. Bhanger MI, Anwar F. Fatty acid (FA) composition and contents of trans unsaturated FA in hydrogenated vegetable oils and blended fats from Pakistan. J Am Oil Chem Soc. (2004) 81:129–34. doi: 10.1007/s11746-004-0870-2
92. Naz R, Anjum FM, Rasool G, Nisar MA, Batool R, Saeed F. Total trans fat content in commercially available hydrogenated vegetable oils. Pak J Nutr. (2012) 11:145–49. doi: 10.3923/pjn.2012.145.149
93. Selmi S, Ghiloufi R, El-Ati J. Trans fatty acids content of selected popular Tunisian fast food. J New Sci. (2019) 68:4232–39. Available online at: https://www.jnsciences.org/agri-biotech/99-volume-68/600-trans-fatty-acids-content-of-selected-popular-tunisian-fast-food.html
94. Al-Ismail KM, Takruri HR, Tayyem RF, Al-Dabbas MM, Abdelrahim DN. Trans fatty acids content of sweets and appetisers traditionally consumed in Jordan. Riv Ital Sostanze Gr. (2021) 98:129–35. Available online at: https://www.innovhub-ssi.it/kdocs/2012987/2021_vol._982_-_art._06_-_al-ismail.pdf
95. Dashti B, Al-Awadi F, Sawaya W, Al-Otaibi J, Al-Sayegh A. Fatty acid profile and cholesterol content of 32 selected dishes in the state of Kuwait. Food Chem. (2003) 80:377–86. doi: 10.1016/S0308-8146(02)00277-7
96. Sawaya WN, Al-Awadhi F, Naeemi I, Al-Sayegh A, Ahmad N, Khalafawi MS. Dietary fat profiles of composite dishes of the Arabian Gulf country of Kuwait. J Food Compost Anal. (1998) 11:200–11. doi: 10.1006/jfca.1997.0557
97. Ismail G, Naga RAE, Zaki MES, Jabbour J, Al-Jawaldeh A. Analysis of fat content with special emphasis on trans isomers in frequently consumed food products in Egypt: the first steps in the trans fatty acid elimination roadmap. Nutrients. (2021) 13:3087–95. doi: 10.3390/nu13093087
98. World Health Organization. Protocol for Measuring Trans Fatty Acids in Foods. (2021). Available online at: https://www.who.int/docs/default-source/documents/replace-transfats/a-food-analysis-lab-protocol.pdf?sfvrsn=b27e4111_2
99. Dogani F, Najjari F, Naghizadeh MM, Dehghan A, Jeihooni AK, Askari A, et al. Analyzing food patterns and preferences of urban population of fasa (phase i of studying the nutritional healthy city in fasa). Gazi Med J. (2019) 30:352–57. doi: 10.12996/gmj.2019.91
100. Borzouei A, Azadbakht L. Describing the dietary habits of Isfahan young girls: assessing the status of tea consumption, processed foods, fats and cooking methods. Health Syst Res. (2010) 6:2. Available online at: https://www.sid.ir/en/Journal/ViewPaper.aspx?ID=201295
101. Al-Akash HY, AbuRuz ME, Arrah A. The university of Jordan students' concerns and awareness about trans-fatty acids. Adv Studies Biol. (2017) 9:63–81. doi: 10.12988/asb.2017.713
102. Manickavasagan A, Al-Mahdouri AA, Al-Mufargi AMS, Al-Souti A, Al-Mezeini ASM, Essa MM. Healthy eating knowledge among college students in Muscat: a self reported survey. Pak J Nutr. (2014) 13:397–403. doi: 10.3923/pjn.2014.397.403
103. Ministry of Health-Iraq World Health Organization. Noncommunicable Diseases Risk Factors STEPS SURVEY IRAQ 2015. (2015). Available online at: https://www.who.int/ncds/surveillance/steps/Iraq_2015_STEPS_Report.pdf
104. Ministry of Health-Saudi Arabia World Health Organization. WHO STEPwise Approach to NCD Surveillance: Country-Specific Standard Report. (2005). Available online at: https://www.who.int/ncds/surveillance/steps/2005_SaudiArabia_STEPS_Report_EN.pdf
105. Rashid A, Amjad S, Nishtar MK, Nishtar NA. Trans-Fatty acid (TFA) elimination in Pakistan: a situational analysis. J Pak Med Assoc. (2020) 70:S1–30. Available online at: https://www.semanticscholar.org/paper/Trans-Fatty-Acid-%28TFA%29-elimination-in-Pakistan%3A-A-Rashid-Amjad/2f2eddad70f9314a8580a2a88b23d45a1042b42b
106. Global Alliance for Improved Nutrition (GAIN) SUN Business Network (SBN). Mapping of Industrially-Produced Trans-Fatty Acids (iTFA) in Pakistan. Global Alliance for Improved Nutrition (2020). Available online at: https://sunbusinessnetwork.org/mapping-industrially-produced-trans-fatty-acids-in-pakistan/
107. Ministry of Health Prevention-UAE. UAE Nutritional Status Study. Abu Dhabi: Statistic and Research Center (2020)
108. Al-Jawaldeh A, Hammerich A, Doggui R, Engesveen K, Lang K, McColl K. Implementation of who recommended policies and interventions on healthy diet in the countries of the eastern mediterranean region: from policy to action. Nutrients. (2020) 12:3700. doi: 10.3390/nu12123700
109. World Health Organization Regional Office for the Eastern Mediterranean. Summary Report of the Virtual Meeting on Implementation of Trans Fatty Acid Elimination in the Eastern Mediterranean Report 10–11 August 2020. Cairo: World Health Organization (2020).
110. NCD Alliance. Trans Fat Free by 2023: Case Studies in Trans Fat Elimination. Geneva: NCD Alliance (2019). Available online at: https://ncdalliance.org/sites/default/files/resource_files/NCDA%20Trans%20Fats%20Acids_Case%20Studies_Web_single%20pages_FINAL.pdf
111. GCC Standardization Organization (GSO). Trans Fatty Acids GSO 2483/2015 (E). Riyadh (2015). Available online at: https://www.gso.org.sa/store/gso/standards/GSO:693058/GSO%202483:2015?lang=en
112. GCC Standardization Organization (GSO). Requirements of Nutritional Labelling. Final Draft of Standard FDS. Prepared by GSO Technical Committee No. TC05. GSO 05/FDS 2233. (2018). Available online at: https://members.wto.org/crnattachments/2018/TBT/SAU/18_5864_00_e.pdf
113. Morocco O. Moving forward on salt and fat reduction in the Region. East Mediter Health J. (2015) 21:374–76. doi: 10.26719/2015.21.5.374
114. World Health Organization Regional Office for the Eastern Mediterranean. Policy Statement and Recommended Actions for Reducing Fat Intake and Lowering Heart Attack Rates in the Eastern Mediterranean Region. Geneva: World Health Organization (2014). Available online at: https://applications.emro.who.int/docs/policy_brief_Fat_reduction_2014_EN.pdf?ua=1%20&ua=1&ua=1
115. Tehran: Iranian National Standardization Organization. Consumer Edible Vegetable Oil: Specifications and Test Methods. INSO 9131. First Revision. Available online at: http://standard.isiri.gov.ir/StandardView.aspx?Id=44637 (accessed May 10, 2021).
116. Moslemi M, Kheirandish M, Mazaheri RNF, Hosseini H, Jannat B, Mofid V, et al. National food policies in the islamic republic of iran aimed at control and prevention of noncommunicable diseases. East Medit Health J. (2020) 26:1556–64. doi: 10.26719/emhj.20.024
117. Tehran: Iranian National Standardization Organization. Vegetable Butter (Margarine): Specifications and Test Methods. INSO 143. Fifth Revision. Available online at: http://standard.isiri.gov.ir/StandardView.aspx?Id=43121 (accessed May 10, 2021).
118. Tehran: Iranian National Standardization Organization. Edible Fats and Oils – Minarine: Specifications and Test Methods. INSO 10500. First Revision. Available online at: http://standard.isiri.gov.ir/StandardView.aspx?Id=43120 (accessed May 10, 2021).
119. World Health Organization. Cutting Into Trans Fat Consumption in Iran. Available online at: https://www.who.int/news-room/feature-stories/detail/cutting-into-trans-fat-consumption-in-iran (accessed April 28, 2021).
120. World Health Organization. Report on the Consultation on Developing Strategic Directions for Salt and Fat Reduction in the Eastern Mediterranean Region, <city>Cairo</city>, Egypt, 28–29 November 2012. Cairo: World Health Organization (2013). Available online at: https://apps.who.int/iris/handle/10665/116172
121. Peymani P, Joulaie H, Zamiri N, Ahmadi SM, Dinarvand R, Hosseini H, et al. Iran's experience on reduction of trans-fatty acid content in edible oils. Middle East J Sci Res. (2012) 11:1207–11. doi: 10.3923/pjn.2012.768.773
122. World Health Organization Regional Office for the Eastern Mediterranean. Report on the Technical Consultation on Salt and Fat Reduction Strategies in the Eastern Mediterranean Region,<city>Tunis</city>, Tunisia 30–31 March 2015. World Health Organization (2015). Available online at: https://applications.emro.who.int/docs/IC_Meet_Rep_2015_EN_16339.pdf
123. Prime Ministry-Directorate of the Official Journal. Withdraw the Jordanian Technical Base. Jordan: Government of the Hashemite Kingdom of Jordan (2016).
124. World Health Organization Regional Office for the Eastern Mediterranean. Nutrition: Success Stories–Jordan. Available online at: http://www.emro.who.int/nutrition/success-stories/index.html (accessed August 18, 2021).
125. Ministry of Health-Jordan. Low Salt, Low Sugar, Low Saturated and Trans Fat Consumption Guideline for Health Care Providers for Training of Trainees (TOT) and Pamphlet for Consumers. Amman: Ministry of Health (2015).
126. Ministry of Health-Jordan. Food-Based Dietary Guidelines for Jordanians. Amman: Nutrition Department (2020). Available online at: https://www.moh.gov.jo/EchoBusV3.0/SystemAssets/PDFs/Jordan%20Guide%20Book_Website.pdf
127. World Health Organization Global Database on the Implementation of Nutrition Action (GINA). Policy–The National Strategy And Plan of Action Against Diabetes, Hypertension, Dyslipidemia And Obesity in Jordan. (2015). Available online at: https://extranet.who.int/nutrition/gina/en/node/25926
128. World Health Organization Global Database on the Implementation of Nutrition Action (GINA). Policy–SFDA.FD 2483/2018 [Trans Fatty Acids]–Saudi Arabia. (2018). Available online at: https://extranet.who.int/nutrition/gina/en/node/36039
129. Bin Sunaid FF, Al-Jawaldeh A, Almutairi MW, Alobaid RA, Alfuraih TM, Bin Saidan FN, et al. Saudi Arabia's healthy food strategy: progress & hurdles in the 2030 road. Nutrients. (2021) 13:2130–43. doi: 10.3390/nu13072130
130. World Health Organization Regional Office for the Eastern Mediterranean. Summary Report on the Regional Workshop on Healthy Diet with a Focus on Trans-Fatty Acid Elimination Beirut Lebanon 19–21 March 2019. Cairo: World Health Organization (2019). Available online at: https://apps.who.int/iris/bitstream/handle/10665/331993/WHOEMNUT283E-eng.pdf?sequence=1&isAllowed=y
131. Saudi Drug Authority. Healthy Food Strategy. Riyadh: SFDA (2018). Available online at: https://old.sfda.gov.sa/ar/awareness/Documents/SFDA-HealthyFoodStrategy.pdf
132. Saudi Food Drug Authority. SFDA Prevents “Partially Hydrogenated Oils”(PHOs) in the Food Industry Gives a Period to the Manufacturers to Comply with the Saudi Technical Regulations. Riyadh: SFDA (2018). Available online at: https://old.sfda.gov.sa/en/food/news/Pages/f6-12-2018a2.aspx
133. Ministry of Health-Kingdom of Saudi Arabia. The Healthy Food Guide for the Health Practitioner. Riyadh: Ministry of Health-Kingdom of Saudi Arabia (2020).
135. World Health Organization Global Database on the Implementation of Nutrition Action (GINA). Policy–A Guide for Healthy Food Terms and Conditions in Government Subsistence Purchase Contracts–Saudi Arabia. (2019). Available online at: https://extranet.who.int/nutrition/gina/en/node/40344
136. Ministry of Health-Kuwait Gulf Health Council United Nations Development Programme World Health Organization Secretariat of the UN Inter-Agency Task Force on NCDS. The Case for Investment in Prevention and Control of Non-Communicable Diseases in Kuwait. Kuwait: Ministry of Health-Kuwait (2021).
137. World Health Organization Global Database on the Implementation of Nutrition Action (GINA). Policy–Kuwaiti Technical Regulation of Trans Fatty Acids (KWS GSO 2483/2017). (2017). Available online at: https://extranet.who.int/nutrition/gina/en/node/38174
138. World Health Organization Global Database on the Implementation of Nutrition Action (GINA). Policy–Kuwait Action PIan for SFA Intake Reduction and TFA Elimination. Kuwait Salt lntake Reduction Strategy Preliminary Plan – Kuwait (2012). Available online at: https://extranet.who.int/nutrition/gina/en/node/36226
139. Health-Kuwait AoFaNMo. The Role of Administration of Food and Nutrition Ministry of Health in Controlling and Prevention of Non-Communicable Diseases in Kuwait. (2021). Kuwait City: Ministry of Health.
140. World Health Organization Regional Office for the Eastern Mediterranean. Health Profile 2015: Kuwait. Cairo: World Health Organization (2016). Available online at: https://rho.emro.who.int/sites/default/files/Profiles-briefs-files/EMROPUB_EN_19271-KUW.pdf
141. World Health Organization Global Database on the Implementation of Nutrition Action (GINA). Ministerial Decision No. 2019/95 Omani Standard for Bread – Oman. (2019). Available online at: https://extranet.who.int/nutrition/gina/en/node/39755
142. World Health Organization Global Database on the Implementation of Nutrition Action (GINA). Policy–Summary of Proposed Implementation Mechanisms to Reduce Saturated and Trans Fat Consumption 2016-2020–Oman. (2016). Available online at: https://extranet.who.int/nutrition/gina/en/node/38166
143. World Health Organization Global Database on the Implementation of Nutrition Action (GINA). Policy–National Plan for the Prevention and Control of Chronic Non-Communicable Diseases 2016–2025. Oman (2016). Available online at: https://extranet.who.int/nutrition/gina/en/node/39383
144. GCC Standardization Organization (GSO). Labeling of Prepackaged Food Stuffs GSO 9/2013 (E). Riyadh (2013). Available online at: https://www.gso.org.sa/store/standards/GSO:615544/GSO%209:2013?lang=en
145. World Health Organization Global Database on the Implementation of Nutrition Action (GINA). Policy–Combating the Epidemic of Non-Communicable Diseases in Oman by Changing the Nutritional Quality of the Food Chain – Oman. (2014). Available online at: https://extranet.who.int/nutrition/gina/en/node/39432.
146. World Health Organization Global Database on the Implementation of Nutrition Action (GINA). Policy–Punjab Pure Food Rules–Pakistan. (2011). Available online at: https://extranet.who.int/nutrition/gina/en/node/38485
147. State of Palestine Ministry of Health. Certification Form for Mandatory Technical Instructions. State of Palestine; Ministry of Health (2021).
148. State of Palestine Ministry of Health. National Nutrition Policy, Strategies and Action Plan (NNPSAP) (2017–2022). State of Palestine, Ministry of Health (2016).
149. World Health Organization Global Database on the Implementation of Nutrition Action (GINA). Policy–Stratégie de Prévention et de Lutte contre l'Obésité – Tunisia. (2013). Available online at: https://extranet.who.int/nutrition/gina/en/node/23769
150. World Health Organization Global Database on the Implementation of Nutrition Action (GINA). Policy–National Action Plan in Nutrition–UAE. (2017). Available online at: https://extranet.who.int/nutrition/gina/en/node/37425
151. World Health Organization Global Database on the Implementation of Nutrition Action (GINA). Policy–Non Communicable Disease Prevention and Control Plan (NCD-PCP) for Lebanon 2015-2020 – Lebanon. (2014). Available online at: https://extranet.who.int/nutrition/gina/en/node/26377
152. World Health Organization Global Database on the Implementation of Nutrition Action (GINA). Policy–Egypt National Multisectoral Action Plan for Prevention and Control of Noncommunicable Diseases (EgyptMAP-NCD) – Egypt. (2017). Available online at: https://extranet.who.int/nutrition/gina/en/node/25915
153. World Health Organization Global Database on the Implementation of Nutrition Action (GINA). Policy–The National Strategy for Healthy Food and Physical Activity 2015-2025–Saudi Arabia. (2018). Available online at: https://extranet.who.int/nutrition/gina/en/node/39384
154. World Health Organization Global Database on the Implementation of Nutrition Action (GINA). Policy–Prevention des Maladies Non Transmissibles: Plan d'action Multisectoriel Pour la Promotion d'un Mode de vie sain 2015-2020 – Morocco. (2015). Available online at: https://extranet.who.int/nutrition/gina/en/node/36194
155. Sultanate of Oman. National Nutrition Strategy 2020-2030, National Plan for Prevention of NCD (2016-2025). Sultanate of Oman (2016).
156. Al Shabiba. Muscat-Atyab Products Are Free of Hydrogenated Oils. Available online at: https://shabiba.com/article/230570https:/alroya.om/post/240669/300-%d9%85%d9%86%d8%aa%d8%ac-%d9%85%d9%86-%d8%a3%d8%b7%d9%8a%d8%a7%d8%a8-%d8%a8%d9%84%d8%a7-%d8%b2%d9%8a%d9%88%d8%aa-%d9%85%d9%87%d8%af%d8%b1%d8%ac%d8%a9-%d9%84%d8%b3%d9%84%d8%a7%d9%85%d8%a9-%d8%a7%d9%84%d9%85%d8%b3%d8%aa%d9%87%d9%84%d9%83 (accessed May 17, 2021).
157. Ministry of Health-Palestine. National Health Strategy. Ministry of Health-Palestine (2019). Available online at: http://site.moh.ps/Content/Books/Byh2ENRn64uTVaLncGL6AjD1Z3dzHMEuLvgQDEC55ujpNihg8YPEVv_OTxQv6uPfFIRmT9xs7dwgvatwShEN8VoqHs83y5NWwua3THGRD73OO.pdf
158. World Health Organization Global Database on the Implementation of Nutrition Action (GINA). Policy–Stratégie Nationale Multisectorielle de Prévention et Contrôle des Maladies Non Transmissibles (MNT) – Tunisia. (2018). Available online at: https://extranet.who.int/nutrition/gina/en/node/39424
159. Saudi Food and Drug Authority. Campaign to Control Trans Fats in Food Products. Riyadh: SFDA (2020).
160. World Health Organization. Healthy Diet. Fact Sheet No. 394. (2020). Available online at: https://www.who.int/en/news-room/fact-sheets/detail/healthy-diet (accessed July 29, 2021.
161. World Health Organization. Draft Guidelines on Saturated Fatty Acid and Trans-Fatty Acid Intake for Adults and Children: Draft for Public Consultation. World Health Organization (2018). Available online at: https://extranet.who.int/dataform/upload/surveys/666752/files/Draft%20WHO%20SFA-TFA%20guidelines_04052018%20Public%20Consultation(1).pdf
162. Lichtenstein AH, Appel LJ, Brands M, Carnethon M, Daniels S, Franch HA, et al. Diet and lifestyle recommendations revision 2006: a scientific statement from the American heart association nutrition committee. Circulation. (2006) 114:82–96. doi: 10.1161/CIRCULATIONAHA.106.176158
163. Afshin A, Sur PJ, Fay KA, Cornaby L, Ferrara G, Salama JS, et al. Health effects of dietary risks in 195 countries, 1990–2017: a systematic analysis for the global burden of disease study 2017. Lancet. (2019) 393:1958–72.
164. Wanders AJ, Zock PL, Brouwer IA. Trans fat intake and its dietary sources in general populations worldwide: a systematic review. Nutrients. (2017) 9:840–53. doi: 10.3390/nu9080840
165. Te Morenga L, Montez JM. Health effects of saturated and trans-fatty acid intake in children and adolescents: systematic review and meta-analysis. PLoS ONE. (2017) 12:e0186672. doi: 10.1371/journal.pone.0186672
166. Mozaffarian D, Stampfer MJ. Removing industrial trans fat from foods. BMJ. (2010) 340:c1826. doi: 10.1136/bmj.c1826
167. Serra-Majem L, Tomaino L, Dernini S, Berry EM, Lairon D, Ngo de la Cruz J, et al. Updating the mediterranean diet pyramid towards sustainability: focus on environmental concerns. Int J Environ Res Public Health. (2020) 17:8758–77. doi: 10.3390/ijerph17238758
168. Fernandez ML, Raheem D, Ramos F, Carrascosa C, Saraiva A, Raposo A. Highlights of current dietary guidelines in five continents. Int J Environ Res Public Health. (2021) 18:2814–22. doi: 10.3390/ijerph18062814
169. Al-Jawaldeh A, Rayner M, Julia C, Elmadfa I, Hammerich A, McColl K. Improving nutrition information in the eastern Mediterranean region: implementation of front-of-pack nutrition labelling. Nutrients. (2020) 12:330–45. doi: 10.3390/nu12020330
170. Takian A, Amerzadeh M. An International Comparative Policy Analysis to Accelerate Actions against Non-Communicable Diseases: The Experience of Iran. Prince Mahidol Award Confrence (PMAC) (2019).
171. McLean RM. Measuring population sodium intake: a review of methods. Nutrients. (2014) 6:4651–62. doi: 10.3390/nu6114651
172. World Health Organization. Reducing Salt Intake in Populations: Report of a WHO Forum and Technical Meeting, 5-7 October 2006, Paris, France. Geneva: World Health Organization (2007). Available online at: https://www.who.int/dietphysicalactivity/Salt_Report_VC_april07.pdf
173. World Health Organization. Module 1: review. how-to guide for landscape assessment and roadmap development for elimination of trans fats. In: REPLACE Trans Fat: An Action Package to Eliminate Industrially Produced Trans-Fatty Acids. Geneva: World Health Organization (2019). Available online at: https://www.who.int/docs/default-source/replace-transfat/replace-module-1-re.pdf?sfvrsn=1885eaed_2
Keywords: trans fat, reduction, strategy, implementation, evaluation, Eastern Mediterranean Region
Citation: Al-Jawaldeh A, Taktouk M, Chatila A, Naalbandian S, Abdollahi Z, Ajlan B, Al Hamad N, Alkhalaf MM, Almamary S, Alobaid R, Alyafei SA, Azizi MH, Baqadir NM, Barham R, Binsunaid FF, El Ammari L, El Ati J, Hoteit M, Massad H, Nejad MS and Nasreddine L (2021) A Systematic Review of Trans Fat Reduction Initiatives in the Eastern Mediterranean Region. Front. Nutr. 8:771492. doi: 10.3389/fnut.2021.771492
Received: 06 September 2021; Accepted: 27 October 2021;
Published: 26 November 2021.
Edited by:
Ana Lúcia De Saccol, UFN–Universidade Franciscana, BrazilReviewed by:
Aida Turrini, Independent Researcher, Rome, ItalyCopyright © 2021 Al-Jawaldeh, Taktouk, Chatila, Naalbandian, Abdollahi, Ajlan, Al Hamad, Alkhalaf, Almamary, Alobaid, Alyafei, Azizi, Baqadir, Barham, Binsunaid, El Ammari, El Ati, Hoteit, Massad, Nejad and Nasreddine. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Lara Nasreddine, bG4xMEBhdWIuZWR1Lmxi
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.