
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Nutr. , 10 November 2021
Sec. Clinical Nutrition
Volume 8 - 2021 | https://doi.org/10.3389/fnut.2021.736900
Objective: To investigate whether a healthy lifestyle is associated with the lower childhood obesity regardless of birth weight.
Methods: Participants were selected from a large-scale cross-sectional study conducted in the seven provinces across China. Birth weight and lifestyle factors were collected through a questionnaire. A weighted healthy lifestyle score was calculated and categorized into favorable, intermediate, and unfavorable lifestyles.
Results: A total of 47,768 participants were enrolled in this study. Overall, 16.4% of the participants followed a favorable lifestyle, 62.8% followed an intermediate lifestyle, and 20.8% followed an unfavorable lifestyle. Compared with the participants who were born normal birth weight (NBW), participants who were born high birth weight (HBW) (OR = 1.58; 95% CI 1.48–1.77) and very high birth weight (VHBW) (OR = 1.79; 95% CI: 1.47–2.18) had higher obesity risk, however, the participants who were born low birth weight (LBW) had lower obesity risk (OR = 0.81; 95% CI: 0.68–0.96). Participants with an unfavorable lifestyle were associated with a higher risk of childhood obesity compared with the participants with favorable lifestyle (OR = 1.25; 95%CI: 1.14–1.38). Participants who were born VHBW and with an unfavorable lifestyle had 2.76 times (95% CI: 1.78–4.28) further risk of childhood obesity compared with the participants who were born NBW and with a favorable lifestyle. However, adherence to a favorable lifestyle seems to counteract the elevated risk of childhood obesity by VHBW (OR = 1.37; 95% CI: 0.84–2.24).
Conclusion: Both the HBW and unfavorable lifestyle were significantly associated with risk of childhood obesity. Adherence to a favorable lifestyle decreased the risk of childhood obesity among the participants with VHBW. A more longitudinal study is required to repeat the finding to inform tailored prevention programs.
Childhood obesity is a major health problem both in the developed and developing countries (1). In the United States, the prevalence of obesity was 16.9% (95% CI, 14.9–19.2%) in children and adolescents aged 2–19 years (2). Similarly, the prevalence of childhood obesity has substantially increased over the past 30 years in China. According to a series, cross-sectional surveys of the Chinese National Survey on Students' Constitution and Health from 1985 to 2014, overweight and obesity prevalence continually increased from 1.1% in 1985 to 20.4% in 2014 in Chinese school-aged children (3). Childhood obesity has significantly adverse effect on both the physical and psychological health (4). Children with obesity are likely to remain obese even into adulthood and are more likely to develop non-communicable diseases, such as diabetes mellitus and cardiovascular diseases at a younger age (5–8). Our previous study had observed that compared with the children with normal weight, children with overweight (OR = 1.49, 95% CI 1.01, 3.10) and obesity (OR = 1.86, 95% CI 1.12, 3.10) were associated with a higher risk of impaired fasting glycemia (8).
Many factors play an important role in the occurrence of childhood obesity. Both the birth weight and lifestyle factors were associated with the childhood obesity. Studies showed that birth weight was associated with a later risk for obesity. The vast majority of studies observed that the higher birth weight (HBW) had a positive association with the risk of childhood obesity and diabetes, such as studies from 11 European countries (9), the United States (10), Turkey (11), China (12), and Korea (13). There is mounting evidence that children with a favorable lifestyle, such as having a healthy diet, adequate sleeping time, regular physical activity (PA), and appropriate screen time had a lower risk of obesity (14–16). Recently, the studies have combined these lifestyle factors to calculate a lifestyle score to assess the association of lifestyle and health outcomes in children and adolescents, such as cardiometabolic problems and obesity (17). In addition, usually the risk factors do not affect obesity alone, they work together complexly, interacting or having combined effects to impact on the risk of obesity. Therefore, we speculated that it is possible that the increased risk of high birth weight on childhood obesity could be offset by a healthy lifestyle. However, the evidence is still limited.
The purpose of the study is to test the hypothesis that adherence to a healthy lifestyle may offset the increased risk of childhood obesity caused by HBW using the data from a national large-scale cross-sectional study.
This study is based on the data of a large-scale cross-sectional study conducted in the seven provinces across mainland China that received approval from the Ethical Committee of the Peking University (IRB00001052-13034). All the participant students and their parents provided informed consents voluntarily.
The cross-sectional study was performed from September to October 2013, which selected participants aged 6–18 years from the seven provinces across the mainland China, including Tianjin, Shanghai, Liaoning, Chongqing, Hunan, Ningxia, and Guangdong. This survey used a standardized and uniform protocol in all the selected schools across the selected provinces. A multistage cluster random sampling method was used to the selected participants. Briefly, first, three to four districts from each province were randomly selected. Second, 12–16 schools were chosen from each district. Third, two to three classes per grade were selected randomly, after excluding students with the serious organic diseases or those who refused to sign informed consent, all the students aged 6–18 years from the selected classes were selected as the participants in the survey. A staff member who was not involved in the survey performed the randomization process. Details of the design have been described carefully in a previous study (18). In this study, we enrolled 47,768 students aged 6–18 years with the gestational age ≥37 weeks into the final analysis.
Data on the students aged 6–18 years were collected using the standard questionnaires that were filled in by the participants and one of their parents. Data of the intake frequency of common eaten foods in the Chinese children, sleep duration, PA, and screen time were reported by the participants. However, the demographic information, feeding situation, parental education attainment, the delivery method, birth weight, gestation age, family history of the diseases, and body mass index of mother were reported by their parents.
Dietary consumption, including fruits, vegetables, meats, dairy, sugar-sweetened beverages, desserts, and fried foods were reported by the participants. They reported the frequency (day) and amount (servings) over the past a week (7 days). The average daily intake of the single food was calculated by (day × amount in each of those days) ÷ 7 (19). PA was collected using the International Physical Activity Questionnaire Short Form (IPAQ-SF) (20).
Data of birth weight and gestational age were collected using a standard parent/guardian questionnaire. Most of the parents/guardians (70.9%) reported birth weight and gestational age of their child according to the birth certificate that was made by the hospital after birth. For those who do not have the birth certificate, we required parents/guardians reported birth weight and gestational age of their child based on the measurement by themselves. Moreover, we repeated the questionnaire survey after 6 months later, and found that the difference of the birth weight and gestational age between these two surveys was <10%. After excluding the participants with gestational age <37 weeks, all the participants were categorized into low birth weight (LBW) (birth weight <2,500 g), normal birth weight (NBW) (birth weight: 2,500–3,999 g), high birth weight (HBW) (birth weight: 4,000–4,499 g), and very high birth weight (VHBW) (birth weight ≥ 4,500 g) according to their birth weight (21).
A healthy lifestyle score was calculated using four well-established obesity risk factors (diet, PA, screen time, and sleep duration) assessed at the baseline survey through a questionnaire (22–24). Participants scored one point for each of the four healthy behaviors defined according to the national recommendations for the children and adolescents listed later. Regular PA was defined as if the participants meeting the recommendation of the American Heart Association, which recommends at least 150 min of the moderate PA per week or 75 min of vigorous PA per week, or an equivalent combination (25). Screen time was defined as screen time <2 h per day and screen time ≥2 h per day based on the sum of the time spent watching TV and the tablet or smartphone. Sleep duration was defined as an adequate sleep and inadequate sleep according to the recommendation of the Canadian sedentary behavior guidelines for the children and youth (26). Healthy diet was based on the seven common eaten foods (including fruit, vegetable, sugar-sweetened beverage, meat, milk, dessert, and fry foods) that have been documented associated with childhood obesity (27–31). A healthy diet was defined if the students whose consumption of at least four of seven common eaten foods following recommendations on the Dietary Guidelines for the Chinese Residents (2016) (32). The lifestyle index scores ranged from zero to four, with the higher score indicating healthier lifestyles, and were further categorized as unfavorable lifestyles (zero or one healthy lifestyle factors), intermediate lifestyles (two healthy lifestyle factors), and favorable lifestyles (three or four healthy lifestyle factors). A weighted standardized healthy lifestyle score was then derived based on β coefficients of each lifestyle factor in the binary logistic regression model with all the four lifestyles factors and the adjustment for age, sex, region, and ethnicity. The original binary lifestyle variables were multiplied by the β coefficients, summed, divided by the sum of the β coefficients, and multiplied by 100. The weighted standardized lifestyle score was categorized as favorable, intermediate, and unfavorable based on the distribution of the unweight lifestyle score (33).
The Chinese BMI percentile criterion for screening overweight and obesity in the children and adolescents was used to define the obesity among the students aged 6–18 years (34). Participants with age- and sex-specific BMI ≥ 95th percentile were defined as obesity.
Height and weight were measured by a trained team following a standardized procedure. Height was assessed by the portable stadiometer (model TZG, Hengsheng Physical Examination Equipment Co., Ltd. China) to the nearest 0.1 centimeter, with the participants standing straight without shoes and wearing light clothes only. Weight was assessed by the lever-type weight scale (model RGT-140, Hengsheng Physical Examination Equipment Co., Ltd. China) to the nearest 0.1 kg. Both the height and weight were measured twice, and the average value was calculated. About 5% of the participants would be rechecked per day for both height and weight. If the error exceeds 10%, all the participants would be measured again.
Normally distributed continuous variables were shown as mean and SD, and categorical variables were shown as percentages. The Student's t-test was used to compare the mean age between subjects with obesity and subjects with non-obesity. The chi-squared test was used to compare the difference of distribution of the categorical variables between subjects with the obesity and subjects with non-obesity. The binary logistic regression models were used to examine the association of the birth weight, lifestyle, and the combination of birth weight and lifestyle categories (nine categories with NBW and favorable lifestyle as the reference group) with the risk of obesity in children and adolescents aged 6–18 years. All the logistic regression models were adjusted for age, sex, region, and ethnicity. All the analyses were performed using IBM SPSS Statistics version 25.0 and P < 0.05 with two-sided were considered to be statistically significant.
Basic characteristics of the subjects are provided in Table 1. A total of 47,768 subjects were enrolled into this study, including 5,426 (11.4%) subjects with obesity and 42,342 (88.6%) subjects with non-obesity. The mean age was younger in the subjects with obesity compared with those in the subjects with non-obesity (10.0 vs. 10.7 years; P < 0.001). The distribution of sex, region, healthy diet, regular screen time, the number of healthy lifestyle factors, birth weight category, and obesity of the mother was different between obesity and non-obesity (P < 0.05). However, the proportion of ethnicity, regular PA, and adequate sleep time was similar between obesity and non-obesity (P > 0.05). Most participants engaged in either one (25.7%) or two (45.4%) of four healthy lifestyle factors, only 2.7% of participants engaged in the four healthy lifestyle factors. For the weighted lifestyle score, 20.8% were categorized as following an unfavorable lifestyle (scores ranging from 0 to 41), 62.8% followed an intermediate lifestyle (scores ranging from 42 to 87), and 16.4% followed a favorable lifestyle (scored ranging from 88 to 100). Of 3.4% participants who were born LBW, 86.5% of participants who were born NBW, 8.7% of the participants who were born HBW, and 1.4% of the participants who were born VHBW.
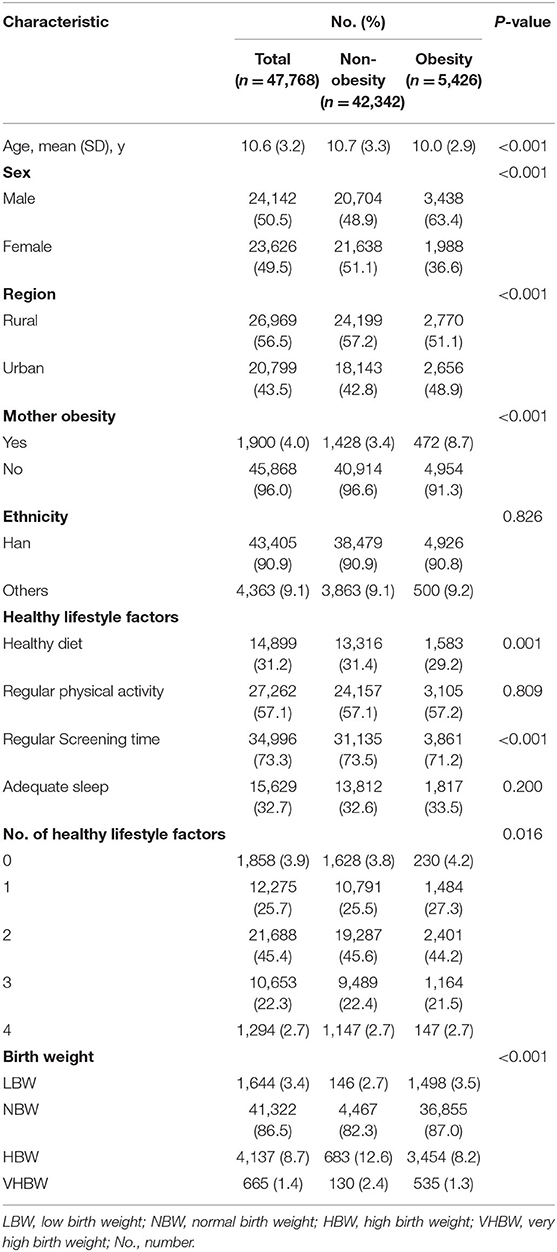
Table 1. Basic characteristics of study population in a study of the association between birth weight and lifestyle with obesity in the children and adolescents.
As shown in Table 2, compared with the participants who were born NBW, participants who were born LBW had lower risk of childhood obesity (OR = 0.81; 95% CI: 0.68–0.96; P = 0.017), however, the participants who were born HBW (OR = 1.58; 95% CI: 1.44–1.73; P < 0.001) and VHBW (OR = 1.78; 95% CI: 1.46–2.18; P < 0.001) had a higher risk of childhood obesity after an adjusted for age, sex, region, mother obesity, and ethnicity. Additional adjustment for the weighted lifestyle factors did not change these associations, indicating that the obesity risk was statistically independent of the lifestyle factors.
The association between lifestyle and risk of the childhood obesity was presented in Table 3. The risk of childhood obesity was significantly higher (OR = 1.25; 95% CI: 1.14–1.37; P < 0.001) in the participants with an unfavorable lifestyle compared with the participants with favorable lifestyle after adjusted for age, sex, region, mother obesity, and ethnicity. Additional adjustment of the birth weight category resulted in an OR of 1.25 (95% CI: 1.14–1.38; P < 0.001), consistent with the independence of birth weight and lifestyle risk factors.
When the birth weight category and lifestyle category were combined there was a monotonic association with increasing birth weight and unhealthy lifestyle (Figure 1). Of the participants who were born VHBW and with an unfavorable lifestyle had a significantly higher obesity risk than the participants who were born NBW and with a favorable lifestyle (OR = 2.76; 95% CI: 1.78–4.28; P < 0.001). However, adherence to a favorable lifestyle seems to counteract the elevated risk of childhood obesity by VHBW (OR = 1.37; 95% CI: 0.84–2.24). Consistent association was also observed when compared with the participants who were born NBW and with an unfavorable lifestyle (Supplementary Figure 1). There was no significant interaction between birth weight category and weighted healthy lifestyle category (P = 0.273) indicating that the association with lifestyle factors did not vary substantially on the basis of the birth weight.
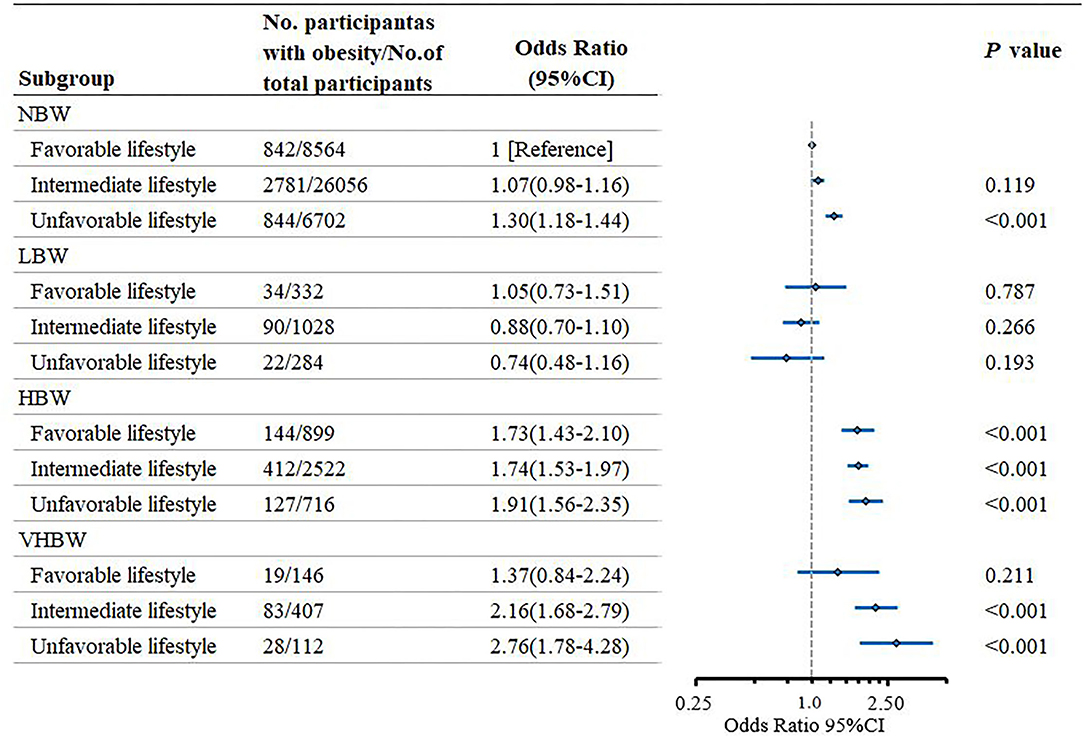
Figure 1. Risk of obesity according to the birth weight and lifestyle in the children and adolescents.
Table 4 presented the association between lifestyle and childhood obesity risk stratified by the birth weight category. Among the participants who were born VHBW, participants with a favorable lifestyle had a lower risk of obesity than the participants with an unfavorable lifestyle (OR = 0.50; 95% CI: 0.26–0.95; P = 0.036). Among the participants who were born NBW, compared with the participants with unfavorable lifestyle, participants with favorable lifestyle also had significantly lower risk of childhood obesity (OR = 0.77; 95% CI: 0.69–0.85; P < 0.001).
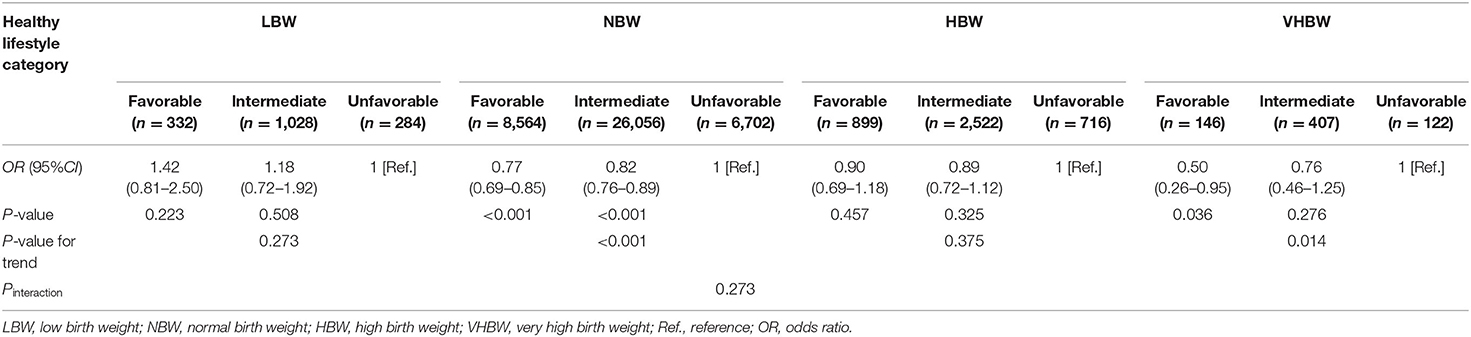
Table 4. Risk of obesity according to a healthy lifestyle category within each birth weight in the children and adolescents.
Using the data from a large-scale cross-sectional study in the Chinese children and adolescents aged 6–18 years old, this study observed that high birth weight and healthy lifestyle were independently associated with the risk of childhood obesity. Participants with HBW and unfavorable lifestyle had a significantly higher risk of childhood obesity compared with those with NBW and a favorable lifestyle. There was no significant interaction between HBW and healthy lifestyle, and a favorable lifestyle was associated with a lower risk of the childhood obesity regardless of the birth weight.
The increased risk of the HBW on childhood obesity was similar to the previous meta-analysis, which combined data from 162,129 mothers and their children from 37 pregnancy and birth cohort studies from Europe, North America, and Australia, and found that the participants with high birth weight had 0.72 times higher risk of obesity in the late childhood (10–18 years) compared with the participant with NBW (35). Although the majority of the previous studies had observed that the healthy lifestyle factors was negatively associated with the risk of childhood obesity (16, 36, 37), there was no study that examined the association between lifestyle factors and childhood obesity using a combined-weighted lifestyle score. In this study, we combined four lifestyle factors of obesity and calculated a weighted lifestyle score, and found that the participants with an unfavorable lifestyle had 0.26 times higher risk of childhood obesity than those with a favorable lifestyle. They were indicating that a healthy lifestyle may decrease the risk of obesity in childhood.
In contrast, we observed that the low-birth weight was a protective factor of childhood obesity, which was consistent with the previous studies (38–40). This finding suggests that the participants with poor nutritional status during pregnancy might still exhibit these conditions when they reach the school age.
To our knowledge, no previous study had investigated the association of the combined birth weight and lifestyle with the risk of childhood obesity. A previous study examined the association of the combined polygenic risk score and lifestyle with the childhood obesity in 997 children, and found that among children with high-polygenic risk, a healthy lifestyle was associated with an 85% lower risk of obesity compared with an unhealthy lifestyle (OR = 0.15; 95% CI: 0.04–0.59; P = 0.007) (41). However, the lifestyle score in their study was calculated as the sum of seven lifestyle factors, including slowness in eating, satiety responsiveness, food responsiveness, screen time, PA, sugar-sweetened beverages consumption, and sleep duration, but not weighted used the β coefficient of each factor with obesity in the logistic regression model. Furthermore, the previous study had limited statistical power due to the limited sample size. Thus, the effect of lifestyle on childhood obesity may be misassessed. Compared with the previous study, this study used a large-scale national sample, and a weighted lifestyle score that investigated the association of HBW and lifestyle with the risk of childhood obesity.
This study found that HBW increased the risk of obesity, and the increased risk might be largely offset by the favorable lifestyle in childhood, especially for those with VHBW. Compared with the participants who were born NBW, participants who were born VHBW increased 79% risk of the childhood obesity. Fortunately, if these participants adherence to a favorable lifestyle in their later life, they might decrease 50% risk of childhood obesity compared with those adherences to an unfavorable lifestyle. These findings indicate that the increased risk of the childhood obesity caused by HBW might be largely offset by a favorable lifestyle in the later life. Furthermore, participants who were born VHBW and adherence to a favorable lifestyle did not significantly increase the risk of childhood obesity compared with the participants who were born NBW and adherence to a favorable lifestyle. This finding furthermore supported that the increased risk of childhood obesity caused by HBW might be largely offset by a favorable lifestyle in their later life. These findings have an important public health implication because individuals who were born HBW have a higher risk of childhood obesity, but the elevated risk could be reduced if they adhere to a favorable lifestyle in their later life.
Despite there was no study examining the association of birth weight and lifestyle with the risk of childhood obesity, a previous study conducted by Qiao et al. explored the joint association of birth weight and PA/sedentary behavior with childhood obesity and found that the moderate and vigorous PA is more important than high birth weight as a correlate of obesity in children (42). It was inconsistent with the findings from this study, we found that the increased risk of childhood obesity caused by an unfavorable lifestyle seems to be less than that caused by high birth weight. We speculated that the differences in population and measurement methods of PA might explain the inconsistent results. In the study by Qiao et al., participants were from 12 countries (Australia, Brazil, Canada, China, Colombia, Finland, India, Kenya, Portugal, South Africa, the United Kingdom, and the United States) and an ActiGraph GT3X+ accelerometer was used to assess the PA level. However, this study only selected participants from the Chinese children and adolescents and IPAQ-short form was used to assess the level of PA.
This study has several limitations. First, the association observed in this study comes from a cross-sectional study that prevents us from making causal inferences. Second, the data of birth weight was retrospectively collected from the parents of participants. Thus, the association in this study might be overestimated or underestimated. However, birth weight was obtained from their birth certificate or the health clinic card. Third, although analyses were adjusted for many variables that potentially caused bias, the unmeasured confounding and reverse causation remains. Four, lifestyle factors were collected using a self-reported questionnaire, which possibly remained recall bias and resulted in the misclassification errors. However, the misclassification errors are likely to make these findings toward the null. Five, other lifestyle or environmental factors might also be associated with the risk of childhood obesity. Six, the association has not been validated in other independent population.
In conclusion, this study used the data from a large-scale cross-sectional study in the Chinese children and adolescents aged 6–18 years, and found that the high birth weight and healthy lifestyle were independently associated with the risk of childhood obesity, and the increased risk caused by the high birth weight might be largely offset by a favorable lifestyle in children. These findings have important implications for the population with high birth weight to adherence to a healthy lifestyle to prevent obesity in their later life.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by the Ethical Committee of the Peking University. Written informed consent to participate in this study was provided by the participants' legal guardian/next of kin.
JM, Z-yZ, and Z-hW were co-investigators and designed the study. Z-hW and Y-hD carried out the initial analysis. R-bX and Y-dY supervised data analysis. Z-hW take full responsibility for the complete work. All the authors were involved in writing the paper and had final approval of the submitted and published versions.
This project was supported by the Research Special Fund for Public Welfare Industry of Health (Grant Number 201202010).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The authors greatly appreciate the Educational Administration Leaderships and primary and middle school health nurses. The authors also acknowledge all the participants and investigators for their cooperation and efforts.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fnut.2021.736900/full#supplementary-material
1. Ng M, Fleming T, Robinson M, Thomson B, Graetz N, Margono C, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. (2014) 384:766–81. doi: 10.1016/S0140-6736(14)60460-8
2. Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011–2012. J Am Med Assoc. (2014) 311:806–14. doi: 10.1001/jama.2014.732
3. Dong YP, Lau WC, Dong B, Zou Z, Yang Y, Wen B, et al. Trends in physical fitness, growth, and nutritional status of Chinese children and adolescents: a retrospective analysis of 1.5 million students from six successive national surveys between 1985 and 2014. Lancet Child Adolesc Health. (2019) 3:871–80. doi: 10.1016/S2352-4642(19)30302-5
4. Sahoo K, Sahoo B, Choudhury AK, Sofi NY, Kumar R, Bhadoria AS. Childhood obesity: causes and consequences. J Family Med Primary Care. (2015) 4:187–92. doi: 10.4103/2249-4863.154628
5. McCrindle BW. Cardiovascular consequences of childhood obesity. Can J Cardiol. (2015) 31:124–30. doi: 10.1016/j.cjca.2014.08.017
6. Sanders RH, Han A, Baker JS, Cobley S. Childhood obesity and its physical and psychological co-morbidities: a systematic review of Australian children and adolescents. Eur J Pediatr. (2015) 174:715–46. doi: 10.1007/s00431-015-2551-3
7. Praveen PA, Tandon N. Childhood obesity and type 2 diabetes in India. WHO South-East Asia J Public Health. (2016) 5:17–21. doi: 10.4103/2224-3151.206547
8. Wang Z, Zou Z, Wang H, Jing J, Luo J, Zhang X, et al. Prevalence and risk factors of impaired fasting glucose and diabetes among Chinese children and adolescents: a national observational study. Br J Nutr. (2018) 120:813–9. doi: 10.1017/S0007114518002040
9. Rito AI, Buoncristiano M, Spinelli A, Salanave B, Kunesova M, Hejgaard T, et al. Association between characteristics at birth, breastfeeding and obesity in 22 countries: the WHO European Childhood Obesity Surveillance Initiative - COSI 2015/2017. Obes Facts. (2019) 12:226–43. doi: 10.1159/000500425
10. Kapral N, Miller SE, Scharf RJ, Gurka MJ, DeBoer MD. Associations between birthweight and overweight and obesity in school-age children. Pediatr Obes. (2018) 13:333–41. doi: 10.1111/ijpo.12227
11. Vehapoglu A, Goknar N, Turel O, Torun E, Ozgurhan G. Risk factors for childhood obesity: do the birth weight, type of delivery, and mother's overweight have an implication on current weight status? World J Pediatr. (2017) 13:457–64. doi: 10.1007/s12519-017-0030-9
12. Cai L, Tao J, Li X, Lin L, Ma J, Jing J, et al. Association between the full range of birth weight and childhood weight status: by gestational age. Eur J Clin Nutr. (2019) 73:1141–8. doi: 10.1038/s41430-018-0343-3
13. Lee JW, Lee M, Lee J, Kim YJ, Ha E, Kim HS. The protective effect of exclusive breastfeeding on overweight/obesity in children with high birth weight. J Korean Med Sci. (2019) 34:e85. doi: 10.3346/jkms.2019.34.e85
14. Li L, Shen T, Wen LM, Wu M, He P, Wang Y, et al. Lifestyle factors associated with childhood obesity: a cross-sectional study in Shanghai, China. BMC Res Notes. (2015) 8:6. doi: 10.1186/s13104-014-0958-y
15. Felso R, Lohner S, Hollody K, Erhardt E, Molnar D. Relationship between sleep duration and childhood obesity: systematic review including the potential underlying mechanisms. Nutr Metab Cardiovasc Dis. (2017) 27:751–61. doi: 10.1016/j.numecd.2017.07.008
16. Ojeda-Rodriguez A, Zazpe I, Morell-Azanza L, Chueca MJ, Azcona-Sanjulian MC, Marti A. Improved diet quality and nutrient adequacy in children and adolescents with abdominal obesity after a lifestyle intervention. Nutrients. (2018) 10:101500. doi: 10.3390/nu10101500
17. Bawaked RA, Fernandez-Barres S, Navarrete-Munoz EM, Gonzalez-Palacios S, Guxens M, Irizar A, et al. Impact of lifestyle behaviors in early childhood on obesity and cardiometabolic risk in children: results from the Spanish INMA birth cohort study. Pediatric Obesity. (2020) 15:e12590. doi: 10.1111/ijpo.12590
18. Dong YH, Zou ZY, Yang ZP, Wang ZH, Jing J, Luo JY, et al. Association between high birth weight and hypertension in children and adolescents: a cross-sectional study in China. J Hum Hypertens. (2017) 31:737–43. doi: 10.1038/jhh.2017.22
19. Rehm CD, Penalvo JL, Afshin A, Mozaffarian D. Dietary Intake Among US Adults, 1999–2012. J Am Med Assoc. (2016) 315:2542–53. doi: 10.1001/jama.2016.7491
20. Craig CL, Marshall AL, Sjostrom M, Bauman AE, Booth ML, Ainsworth BE, et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. (2003) 35:1381–95. doi: 10.1249/01.MSS.0000078924.61453.FB
21. Behrman R, Kliegman R, Jenson H. Nelson's Textbook of Pediatrics. 17th ed. Philadelphia, PA: Saunders (2003).
22. Liberali R, Kupek EM, Assis AA. Dietary patterns and childhood obesity risk: a systematic review. Childhood Obesity. (2020) 16:70–85. doi: 10.1089/chi.2019.0059
23. Salvo D, Ranjit N, Nielsen A, Akhavan N, van den Berg A. Characterizing micro-scale disparities in childhood obesity: examining the influence of multilevel factors on 4-year changes in BMI, healthy eating, and physical activity, among a cohort of children residing in disadvantaged urban enclaves. Front Public Health. (2019) 7:301. doi: 10.3389/fpubh.2019.00301
24. Parkes A, Green M, Pearce A. Do bedroom screens and the mealtime environment shape different trajectories of child overweight and obesity? Research using the Growing Up in Scotland study. Int J Obes. (2020) 44:790–802. doi: 10.1038/s41366-019-0502-1
25. Lloyd-Jones DM, Hong Y, Labarthe D, Mozaffarian D, Appel LJ, Van Horn L, et al. Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association's strategic Impact Goal through 2020 and beyond. Circulation. (2010) 121:586–613. doi: 10.1161/CIRCULATIONAHA.109.192703
26. Tremblay MS, Leblanc AG, Janssen I, Kho ME, Hicks A, Murumets K, et al. Canadian sedentary behaviour guidelines for children and youth. Appl Physiol Nutr Metab. (2011) 36:59–71. doi: 10.1139/H11-012
27. Essman M, Popkin BM, Corvalan C, Reyes M, Taillie LS. Sugar-sweetened beverage intake among chilean preschoolers and adolescents in 2016: a cross-sectional analysis. Nutrients. (2018) 10:111767. doi: 10.3390/nu10111767
28. Leung CW, DiMatteo SG, Gosliner WA, Ritchie LD. Sugar-sweetened beverage and water intake in relation to diet quality in US children. Am J Prev Med. (2018) 54:394–402. doi: 10.1016/j.amepre.2017.11.005
29. Gil JM, Takourabt S. Socio-economics, food habits and the prevalence of childhood obesity in Spain. Child Care Health Dev. (2017) 43:250–8. doi: 10.1111/cch.12408
30. Noor S, Dehghan M, Lear SA, Swaminathan S, Ibrahim Q, Rangarajan S, et al. Relationship between diet and acculturation among South Asian children living in Canada. Appetite. (2020) 147:104524. doi: 10.1016/j.appet.2019.104524
31. Liu D, Zhao LY, Yu DM, Ju LH, Zhang J, Wang JZ, et al. Dietary patterns and association with obesity of children aged 6(-)17 years in medium and small cities in China: findings from the CNHS 2010(-)2012. Nutrients. (2018) 11:10003. doi: 10.3390/nu11010003
32. Wang SS, Lay S, Yu HN, Shen SR. Dietary Guidelines for Chinese Residents (2016): comments and comparisons. J Zhejiang Univ Sci B. (2016) 17:649–56. doi: 10.1631/jzus.B1600341
33. Jiao L, Mitrou PN, Reedy J, Graubard BI, Hollenbeck AR, Schatzkin A, et al. A combined healthy lifestyle score and risk of pancreatic cancer in a large cohort study. Arch Intern Med. (2009) 169:764–70. doi: 10.1001/archinternmed.2009.46
34. Ji CY, Working Group on Obesity in C. Report on childhood obesity in China (1)–body mass index reference for screening overweight and obesity in Chinese school-age children. Biomed Environ Sci. (2005) 18:390–400.
35. Voerman E, Santos S, Patro Golab B, Amiano P, Ballester F, Barros H, et al. Maternal body mass index, gestational weight gain, and the risk of overweight and obesity across childhood: an individual participant data meta-analysis. PLoS Med. (2019) 16:e1002744. doi: 10.1371/journal.pmed.1002744
36. Pham TTP, Matsushita Y, Dinh LTK, Do TV, Nguyen TTT, Bui AT, et al. Prevalence and associated factors of overweight and obesity among schoolchildren in Hanoi, Vietnam. BMC Public Health. (2019) 19:1478. doi: 10.1186/s12889-019-7823-9
37. An R. Diet quality and physical activity in relation to childhood obesity. Int J Adolesc Med Health. (2017) 29:45. doi: 10.1515/ijamh-2015-0045
38. Frye C, Heinrich J. Trends and predictors of overweight and obesity in East German children. Int J Obes Relat Metab Disord. (2003) 27:963–9. doi: 10.1038/sj.ijo.0802321
39. Loaiza S, Atalah E. Birth weight and obesity risk at first grade of high school in a non-concurrent cohort of Chilean children. Public Health Nutr. (2013) 16:228–32. doi: 10.1017/S136898001200362X
40. Singhal A, Wells J, Cole TJ, Fewtrell M, Lucas A. Programming of lean body mass: a link between birth weight, obesity, and cardiovascular disease? Am J Clin Nutr. (2003) 77:726–30. doi: 10.1093/ajcn/77.3.726
41. Fang J, Gong C, Wan Y, Xu Y, Tao F, Sun Y. Polygenic risk, adherence to a healthy lifestyle, and childhood obesity. Pediatr Obes. (2019) 14:e12489. doi: 10.1111/ijpo.12489
Keywords: birth weight, obesity, preventive medicine, lifestyle, child health
Citation: Wang Z-h, Zou Z-y, Dong Y-h, Xu R-b, Yang Y-d and Ma J (2021) A Healthy Lifestyle Offsets the Increased Risk of Childhood Obesity Caused by High Birth Weight: Results From a Large-Scale Cross-Sectional Study. Front. Nutr. 8:736900. doi: 10.3389/fnut.2021.736900
Received: 06 July 2021; Accepted: 06 October 2021;
Published: 10 November 2021.
Edited by:
Clelia Madeddu, University of Cagliari, ItalyCopyright © 2021 Wang, Zou, Dong, Xu, Yang and Ma. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zheng-he Wang, d3poMTE2MDg2QHNtdS5lZHUuY24=; Jun Ma, bWFqdW50QGJqbXUuZWR1LmNu
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.