
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Nutr. , 16 September 2021
Sec. Clinical Nutrition
Volume 8 - 2021 | https://doi.org/10.3389/fnut.2021.730205
This article is part of the Research Topic Dietary Strategies for Healthy Aging – Caloric Restriction and Beyond View all 12 articles
Background: The possible effects of dietary fiber intake on hypertension have not been clarified fully. The association of dietary fiber intake with hypertension risk in midlife women was analyzed in this study.
Methods: Baseline data were obtained from the Study of Women's Health Across the Nation (SWAN). Smooth curve, linear regression, and logistic regression analyses were performed to investigate the associations of four indices of daily dietary estimate (DDE) of dietary fiber (dietary fiber intake, dietary fiber intake from beans, dietary fiber intake from vegetables/fruit, and dietary fiber intake from grains) with blood pressure in midlife women. For this research purpose, diastolic blood pressure (DBP) ≥90 mmHg was defined as diastolic hypertension, and systolic blood pressure (SBP) ≥140 mmHg was defined as systolic hypertension.
Results: This study included 2,519 participants with an average age of 46. The smooth curve showed approximate negative correlations between three fiber indices (DDE dietary fiber, DDE fiber from vegetables/fruit, and DDE fiber from grains) and blood pressure, including DBP and SBP (all P < 0.005). There were also approximate negative correlations between two fiber indices (DDE dietary fiber and DDE fiber from grains) and the risk of diastolic hypertension and systolic hypertension (all P < 0.05). Furthermore, multiple linear regression analysis suggested that DDE dietary fiber (Sβ = −0.057, 95% CI −0.194 – −0.012, P = 0.027), DDE fiber from vegetables/fruit (Sβ = −0.046, 95% CI −0.263 – −0.007, P = 0.039), and DDE fiber from grains (Sβ = −0.073, 95% CI −0.600 – −0.099, P = 0.006, Model 4) were still negatively correlated with DBP after adjusting for confounding factors. Only DDE fiber from grains was independently and negatively associated with SBP (Sβ = −0.060, 95% CI −0.846 – −0.093, P = 0.015) after these same confounding factors were adjusted for. Importantly, multiple logistic regression analysis suggested that only higher DDE fiber from grains was independently associated with a reduced risk of diastolic hypertension (OR = 0.848, 95% CI 0.770–0.934, P = 0.001, Model 4) and systolic hypertension (OR = 0.906, 95% CI 0.826–0.993, P = 0.034, Model 4) after the adjustments were made for confounding factors.
Conclusions: We found that dietary fiber intake, especially DDE fiber from grains, contributes to a lower risk of systolic hypertension and diastolic hypertension in midlife women.
Patients with hypertension tend to experience headaches, dizziness, and other symptoms for decades, and the damage caused by hypertension to the cardiovascular system is continuous and aggravating (1, 2). High blood pressure that is not well-controlled contributes significantly to an increased risk of serious diseases, such as myocardial infarction, ischemic and hemorrhagic stroke, aortic dissection or aneurysm, chronic kidney disease, and peripheral artery disease (3). There are many risk factors that are known to be associated with hypertension, such as age, heredity, environment, and lifestyle (4). Unhealthy lifestyles, including a high-salt diet, lack of exercise, fatigue, and high pressure from work and other areas of life, are the most important modifiable factors for developing hypertension (5). Using antihypertensive drugs can alleviate damage to target organs by hypertension and prevent adverse cardiovascular events. However, many individuals are either not aware of their blood pressure condition or are not aware of their true blood pressure values due to inadequate or discontinued antihypertensive treatment. Furthermore, although there are vast options for antihypertensive drugs, some patients with hypertension have difficulty controlling their blood pressure within the normal range by using current drugs, motivating further research in this field. Thus, early prevention of the formation of hypertension is still particularly important at present.
Importantly, the positive effects of dietary fiber supplementation on cardiovascular protection have been recognized for a few years (6–11). Some investigations on the role of dietary fiber intake in patients with hypertension have also been reported. For instance, one previous study reported an association of fiber intake with the prevention of cardiovascular disease, including hypertension (6). Oat, a fiber-rich food, has also been found to have beneficial effects on controlling blood pressure among patients with hypertension (7). However, studies on the exact relationship between dietary fiber intake and hypertension risk are few, and it has been studied inadequately (6). Lifestyle and eating habits in the middle-aged population tend to cause people to be at high risk of hypertension.
Accordingly, in this study, data analysis from a subset of the Study of Women's Health Across the Nation (SWAN) was performed to evaluate the relationships of four indices of daily dietary estimate (DDE) of dietary fiber (dietary fiber intake, dietary fiber intake from beans, dietary fiber intake from vegetables/fruit, and dietary fiber intake from grains) with blood pressure in midlife women.
To analyze the baseline data from the SWAN study, a longitudinal, multicenter, and population-based study of the natural history of late midlife women was performed. Between 1995 and 1997, a telephone screening interview was used to determine the eligibility of an individual for the study cohort. Participants from community-based samples were collected at seven collection points across the United States using various sampling frames and recruitment strategies. In summary, 16,065 women completed the telephone screening interview, and only 3,302 (20.6%) women were recruited to the SWAN cohort at baseline. Women who met the inclusion criteria were as follows: (1) had a range of ages from 42 to 53 years; (2) had not used reproductive hormones in the previous 3 months; and (3) had an intact uterus and at least one intact ovary. The institutional review boards at all the sites approved the study protocol, and all included individuals at each site gave informed consent. The SWAN study contained detailed information regarding demographic characteristics, lifestyle, self-reported health, health examination, and medical history. For research purposes, 783 women were excluded due to missing information. A total of 2,519 women were included in this study. The exclusion criteria are described in detail in Figure 1.
The measurement of blood pressure in all the included subjects was carried out according to a standardized protocol (12). Subjects did not consume caffeinated beverages or smoke for at least 30 min before measuring blood pressure. The measurements were performed with readings taken on the right arm, with the participant seated and feet flat on the floor for at least 5 min before measuring blood pressure (12). A standard mercury sphygmomanometer was used to record systolic blood pressure (SBP) and diastolic blood pressure (DBP) at the first and the fifth phase Korotkoff sounds. The average of two sequential blood pressure values, with a minimum of a 2-min rest period between measures, was recorded. Using the average of these two sequential blood pressure values, the mean SBP and DBP were calculated (13). For our research purposes, DBP ≥ 90 mmHg was defined as diastolic hypertension, and SBP ≥ 140 mmHg was defined as systolic hypertension (13).
A modified 1995 Block Food Frequency Questionnaire (FFQ) was used to evaluate daily dietary intake with 103 food items (14, 15) based on the Second National Health and Nutrition Examination Survey (NHANES) (14, 16, 17). Four indices of DDE of dietary fiber (dietary fiber intake, dietary fiber intake from beans, dietary fiber intake from vegetables/fruit, and dietary fiber intake from grains) were computed based on a database of food composition from the data of the United States Department of Agriculture (USDA) linked to data of food frequency (18).
For research purposes, body mass index (BMI) was calculated as weight (kg) divided by height (meters) squared. Smoking status was divided into “current smoker” and “not current smoker”. Medical history (cholesterol medications ever taken, blood pressure medications ever taken, diuretics ever taken, and birth control pills ever taken) was classified as “Yes” and “No”. In addition, biochemical parameters including blood C-reactive protein (CRP), total cholesterol, triglycerides, low-density lipoprotein cholesterol (LDL-C), high-density lipoprotein cholesterol (HDL-C), glucose, and insulin were detected in the SWAN study.
First, we performed a smooth curve to estimate the associations of four indices of DDE of dietary fiber (dietary fiber intake, dietary fiber intake from beans, dietary fiber intake from vegetables/fruit, and dietary fiber intake from grains) with blood pressure. Then, multiple linear regression models were used to explore the associations between these four fiber indices and SBP and DBP. Furthermore, multiple logistic regression models were also used to explore the relationships between the four DDE fiber indices and systolic hypertension (SBP ≥ 140 mm Hg) and diastolic hypertension (DBP ≥ 90 mm Hg). In addition, we implemented a stratified analysis to estimate the relationships between the four fiber indices and blood pressure stratified by age, race, BMI, and smoking status. In multivariate analysis, the following five models were used: Crude Model: adjustment for nothing; Model 1: adjustment for age and race; Model 2: adjustment for age, race, DDE fat, DDE carb, and DDE protein; Model 3: adjustment for age, race, DDE fat, carb, protein, smoking status, and BMI; and Model 4: adjustment for age, race, DDE fat, carb, protein, smoking status, BMI, blood CRP, total cholesterol, triglycerides, LDL-C, HDL-C, glucose, and insulin. All of the analyses were performed using EmpowerStats 3.0 (Chinese version). A P ≤ 0.05 was considered to be statistically significant.
A total of 2,519 subjects were included, with an average age of 46. As shown in Table 1, the mean values of SBP and DBP were 114 and 74 mmHg, respectively. The mean values of DDE dietary fiber, DDE fiber from beans, DDE fiber from vegetables/fruit, and DDE fiber from grains in the included participants were 11.52, 1.22, 5.36, and 3.91, respectively.
Smooth curves were identified between the four DDE fiber indices and blood pressure. The smooth curve suggested approximate negative correlations between three fiber indices (DDE dietary fiber, DDE fiber from vegetables/fruit, and DDE fiber from grains) and blood pressure, including DBP and SBP (Figure 2, all P < 0.005). Importantly, there were approximate negative correlations between two fiber indices (DDE dietary fiber and DDE fiber from grains) and the risk of diastolic hypertension and systolic hypertension (Figure 3, all P < 0.05).
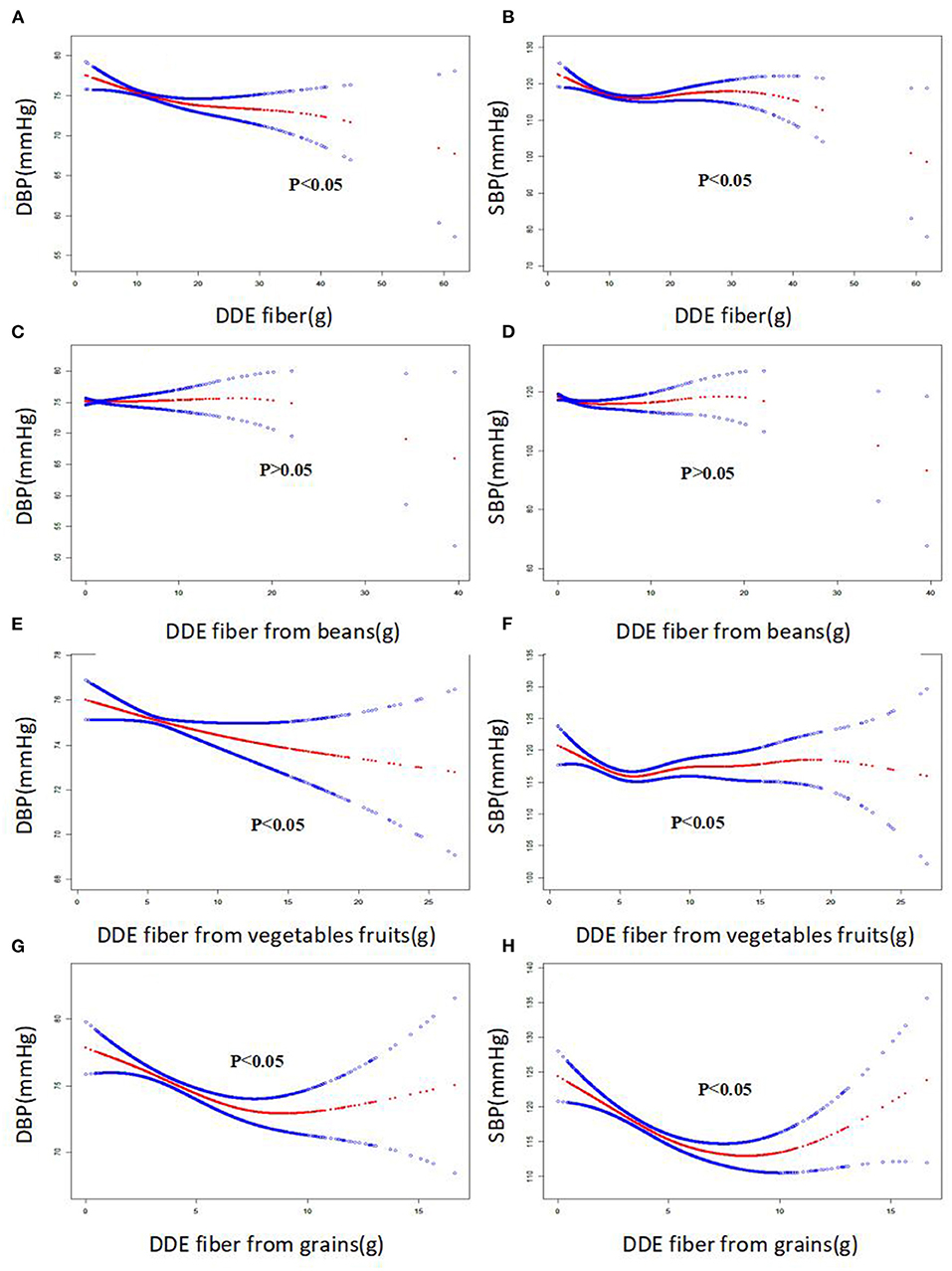
Figure 2. The smooth curve of the associations between dietary fiber intake and systolic blood pressure and diastolic blood pressure (SBP and DBP, respectively).
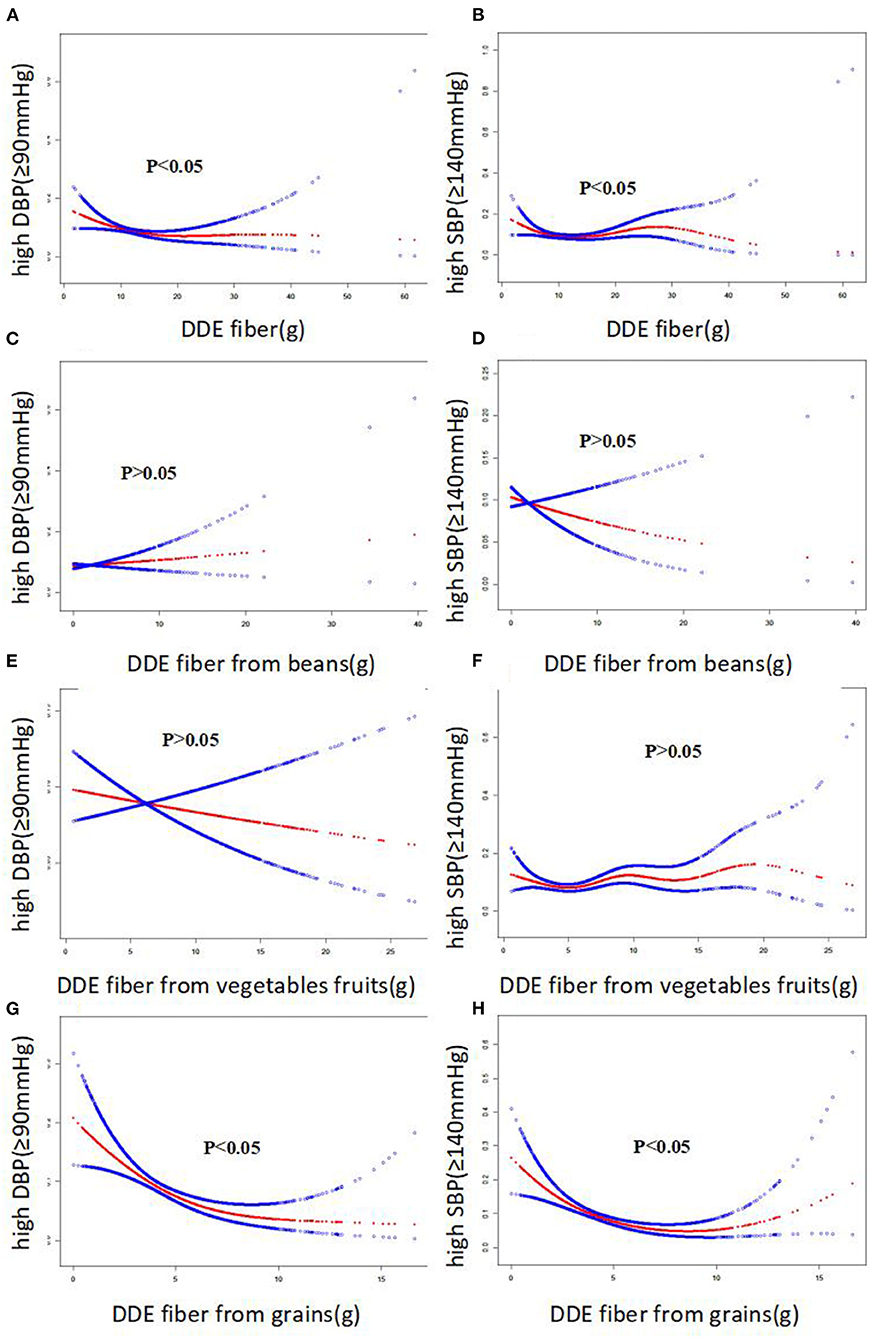
Figure 3. The smooth curve of the associations between dietary fiber intake and risk of systolic and diastolic hypertension, respectively.
To explore the correlation between the intake of dietary fiber and blood pressure, a multiple linear regression analysis was performed. As shown in Table 2, after adjusting for confounding factors, including age, race, DDE fat, carb, protein, smoking status, BMI, blood CRP, glucose, insulin, LDL-C, HDL-C, triglycerides and total cholesterol, DDE dietary fiber (Sβ = −0.057, 95% CI −0.194 – −0.012, P = 0.027), DDE fiber from vegetables/fruit (Sβ = −0.046, 95% CI −0.263 – −0.007, P = 0.039), and DDE fiber from grains (Sβ = −0.073, 95% CI −0.600 – −0.099, P = 0.006) were still negatively correlated with DBP in Model 4. However, we observed that only DDE fiber from grains was independently and negatively associated with SBP (Sβ = −0.060, 95% CI −0.846 – −0.093, P = 0.015) after these same confounding factors were adjusted.
Multiple logistic regression models were used to further prove the correlation between dietary fiber intake and hypertension risk. As shown in Table 3, our results only suggested that higher DDE fiber from grains was independently associated with a reduced risk of diastolic hypertension (OR = 0.848, 95% CI 0.770–0.934, P = 0.001, Model 4) after adjustments were made for confounding factors, including age, race, DDE fat, carb, protein, smoking status, BMI, blood CRP, glucose, insulin, LDL-C, HDL-C, triglycerides, and total cholesterol. Similarly, our results also showed that higher DDE fiber from grains was associated with a reduced risk of systolic hypertension (OR = 0.906, 95% CI 0.826–0.993, P = 0.034, Model 4) after adjusting for these same confounding factors.
Multiple linear regression models were used to further explore whether the associations between DDE fiber from grains and blood pressure were affected by sex, race, BMI, and smoking status. As shown in Table 4, we observed no significant effect modifiers between DDE fiber from grains and DBP after stratifying the analysis by age (interaction P = 0.724), race (interaction P = 0.125), BMI (interaction P = 0.815), and smoking status (interaction P = 0.347). We also observed no significant effect modifiers between DDE fiber from grains and SBP after stratification of the analysis by age (interaction P = 0.629), race (interaction P = 0.114), BMI (interaction P = 0.829), and smoking status (interaction P = 0.664).
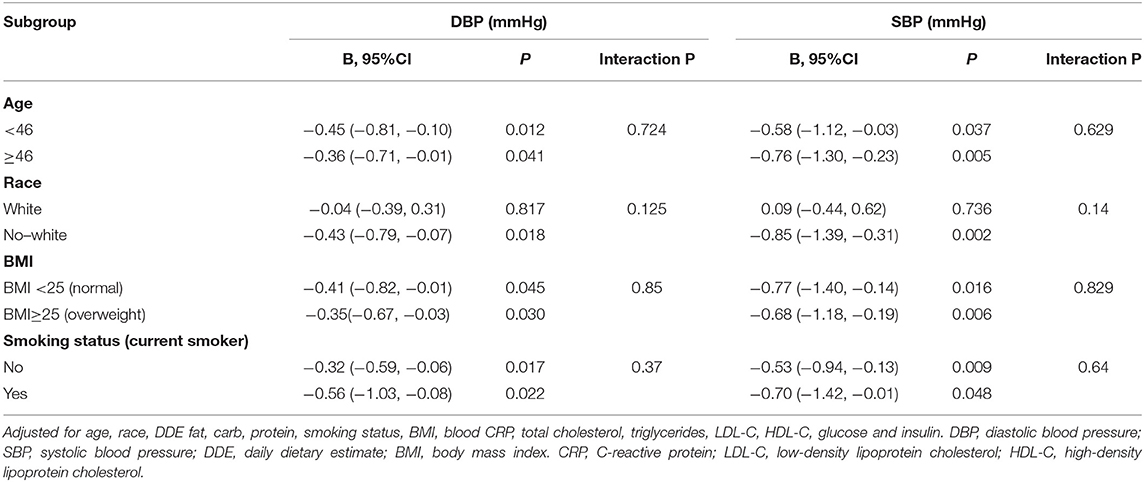
Table 4. Multiple linear regression analysis for relationship between DDE fiber from grains and blood pressure stratified by age, race, BMI and current smoker prespectively.
Multiple logistic regression models were also performed to further investigate whether the associations between DDE fiber from grains and the risk of hypertension were affected by sex, race, BMI, and smoking status (Table 5). We observed no significant effect modifiers between DDE fiber from grains and the risk of diastolic hypertension after the stratified analysis by age (interaction P = 0.898), race (interaction P = 0.225), BMI (interaction P = 0.716), or smoking status (interaction P = 0.450). We also observed no significant effect modifiers between DDE fiber from grains and the risk of systolic hypertension after the stratified analysis by race (interaction P = 0.265), BMI (interaction P = 0.117), or smoking status (interaction P = 0.221). Importantly, age (<46 and ≥46 years) was an effect modifier of the association between DDE fiber from grains and the risk of systolic hypertension (interaction P = 0.009).
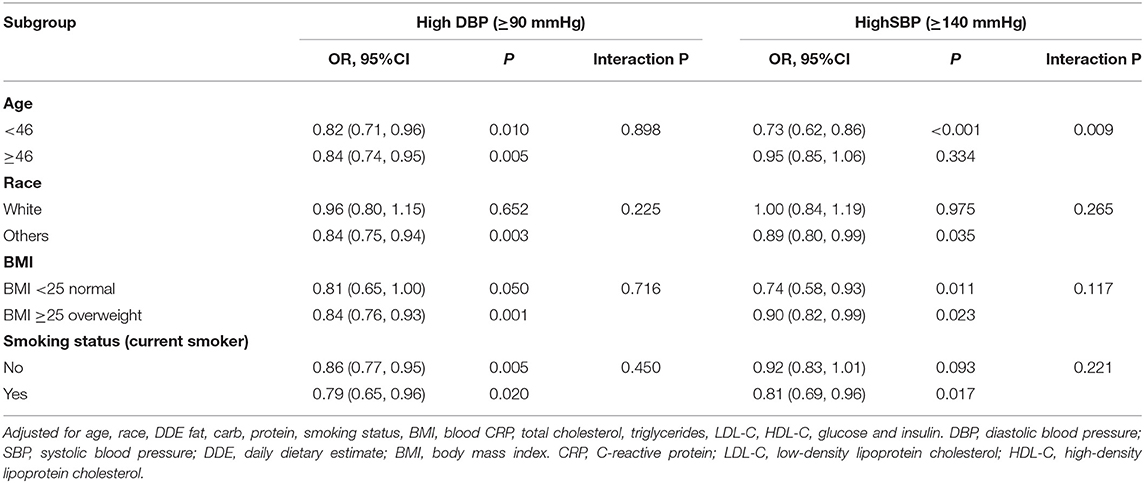
Table 5. Multiple logistic regression analysis for relationship between DDE fiber from grains and risk of hypertension stratified by age, race, BMI and current smoker prespectively.
Our study included baseline data from SWAN including 2,519 subjects to investigate the correlation between dietary fiber intake and hypertension risk. Our results uncovered that DDE fibers from grains were negatively associated with the risk of hypertension after adjusting for confounders. This is the first study to show that increased intake of DDE fiber from grains may contribute to a reduced risk of hypertension in midlife women.
Dietary fiber intake has great benefits for preventing many chronic diseases, such as cardiovascular diseases and malignant tumors. Studies on the beneficial effect of dietary fiber on blood pressure began to be investigated in experimental animals. For example, previous evidence has suggested that increased intake of certain fibers has beneficial effects on improved blood pressure in rats (19). Obata et al. observed that one type of fiber, the husk of Psyllium seeds, can lower blood pressure in hypertensive rats who were fed a high-salt diet (19). A few years later, Li et al. performed a study on model rats who were fed corn starch, white rice, and rye for 16 weeks. They found that the rye diet lowered SBP significantly after 12 weeks of treatment. This diet also lowered serum levels of triglycerides, LDL cholesterol, and total cholesterol in the animals. They concluded that the intake of dietary fiber could contribute beneficial effects to blood lipids and blood pressure (20). Galisteo et al. also found a similar result in obese rats fed a diet containing 3.5% Plantago ovata for 25 weeks (21). They observed that consumption of a fiber-enriched diet could prevent hypertension, endothelial dysfunction, and obesity in rats. Recently, one study also reported that the short-term intake of cocoa fiber products could lower blood pressure in rats (22).
For the clinical studies, for example, Saltzman and his team investigated the role of oat fiber in hypertension (23). They observed that an oat-rich diet did contribute to a reduction in SBP without changing the levels of DBP (23). In addition, the diet also decreased the levels of blood lipids. Keenan et al. observed that oat cereal supplements could lower the need for improving arterial blood pressure and antihypertensive medication in hypertensive patients (24), and also found beneficial effects of oat fiber in hypertensive patients with grade 1 hypertension. These patients were given soluble oat fiber for 3 months, and this fiber led to a significant decrease in blood pressure (25). Consistent with these previous findings and mechanisms, we found that increased dietary fiber intake, especially DDE fiber from grains, is related to a lower risk of systolic hypertension and diastolic hypertension in midlife women. However, we did not find that increasing the intake of dietary fiber from beans and vegetables/fruit was associated with reduced hypertension risk. Elevated dietary fiber intake from grains contributed to a decreased risk of hypertension. This is a very interesting discovery, and more future studies may be necessary to explain the difference.
However, the potential antihypertensive mechanisms of dietary fiber intake have not been elucidated until now. Insulin resistance has been found to be associated with the development of hypertension, and dietary fiber intake might improve blood pressure by modulating insulin metabolism (26, 27). Reduced levels of serum cholesterol are associated with improved endothelial function, which mediates vasodilation and reduces blood pressure (28–30). The weight loss caused by dietary fiber has also been considered the underlying mechanism for the lowering of high blood pressure (31–33). However, these known mechanisms are not enough to explain the protective effect of dietary fiber intake on improving blood pressure. Therefore, more studies are necessary to fully elucidate new mechanisms.
Our study has several notable strengths. First, our study results were from the SWAN study, a multicenter and population-based study of the natural history of late midlife women. The SWAN study has high-quality data, including demographic characteristics, lifestyle, self-reported health, health examination, and medical history, with various sampling frames and recruitment strategies. Second, we comprehensively analyzed the relationship between the main sources of dietary fiber (beans, fruits/vegetables, and grains) and blood pressure. In this cross-sectional study, we are the first to find that increased intake of DDE fiber from grains, rather than the intake of DDE fiber from beans and fruits/vegetables, contributed to a reduced risk of hypertension in midlife women from the United States. Third, enough confounding factors, including demographic characteristics and lifestyle, and biochemical indices, were adjusted by multivariable analysis, which ensures the reliability of our results.
Of course, this study also has several limitations. On the one hand, our data did not distinguish between essential hypertension and secondary hypertension. The diagnosis of hypertension was determined by temporary blood pressure measurement at baseline in the SWAN study. The positive effect of dietary fiber on secondary hypertension caused by other diseases may be insignificant. On the other hand, the results of our study are only applicable to midlife women. The effect of dietary fiber on lowering blood pressure in men and different age groups (minors and the elderly) should be further confirmed in the future. In addition, although 3,302 subjects were included in the SWAN study, only 2,519 subjects were eventually included in our study because approximately 783 individuals were excluded due to missing data.
Our results further suggested that fiber intake, especially the DDE fiber from grains, is associated with the risk of hypertension after controlling for potential confounders.
The original contributions presented in the study are included in the article/supplementary files, further inquiries can be directed to the corresponding author/s.
The studies involving human participants were reviewed and approved by The institutional review boards at all sites have approved the study protocol and all included individual at each site gave informed consent. The patients/participants provided their written informed consent to participate in this study.
All authors contributed to the article and approved the submitted version.
This study was supported by grants from the Natural Science Foundation of Jiangxi Province Youth Fund Project (20192BAB215012), the Science and Technology Research Youth Project of Education Department of Jiangxi Province (GJJ180124), the Natural Science Foundation of China (82060122), and the Key Project of Jiangxi Provincial Department of Education (GJJ180014).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
We would like to thank Zhile Lv for her encouragement and help during the writing of the manuscript.
1. Poulter N, Marmot MG. Hypertension and the probability of an incapacitating event over a defined period: impact of treatment. Eur Heart J. (1992) 13:39–44. doi: 10.1093/eurheartj/13.suppl_H.39
2. Simko F, Pechanova O. Potential roles of melatonin and chronotherapy among the new trends in hypertension treatment. J Pineal Res. (2009) 47:127–33. doi: 10.1111/j.1600-079X.2009.00697.x
3. Antza C, Cifkova R, Kotsis V. Hypertensive complications of pregnancy: a clinical overview. Metabolism. (2018) 86:102–11. doi: 10.1016/j.metabol.2017.11.011
4. Kornitzer M, Dramaix M, De Backer G. Epidemiology of risk factors for hypertension: implications for prevention and therapy. Drugs. (1999) 57:695–712. doi: 10.2165/00003495-199957050-00003
5. Lu FH, Tang SJ, Wu JS, Yang YC, Chang CJ. Hypertension in elderly persons: its prevalence and associated cardiovascular risk factors in Tainan City, southern Taiwan. J Gerontol A Biol Sci Med Sci. (2000) 55:M463–8. doi: 10.1093/gerona/55.8.M463
6. Aleixandre A, Miguel M. Dietary fiber and blood pressure control. Food Funct. (2016) 7:1864–71. doi: 10.1039/C5FO00950B
7. Hartley L, May MD, Loveman E, Colquitt JL, Rees K. Dietary fibre for the primary prevention of cardiovascular disease. Cochrane Database Syst Rev. (2016) 2016:CD011472. doi: 10.1002/14651858.CD011472.pub2
8. de GROOT A, LUYKEN R, PIKAAR NA. Cholesterol-lowering effect of rolled oats. Lancet. (1963) 2:303–4. doi: 10.1016/S0140-6736(63)90210-1
9. Tosh SM, Brummer Y, Miller SS, Regand A, Defelice C, Duss R, et al. Processing affects the physicochemical properties of beta-glucan in oat bran cereal. J Agric Food Chem. (2010) 58:7723–30. doi: 10.1021/jf904553u
10. Grundy MM, Fardet A, Tosh SM, Rich GT, Wilde PJ. Processing of oat: the impact on oat's cholesterol lowering effect. Food Funct. (2018) 9:1328–43. doi: 10.1039/C7FO02006F
11. Brown L, Rosner B, Willett WW, Sacks FM. Cholesterol-lowering effects of dietary fiber: a meta-analysis. Am J Clin Nutr. (1999) 69:30–42. doi: 10.1093/ajcn/69.1.30
12. El Khoudary SR, Wildman RP, Matthews K, Thurston RC, Bromberger JT, Sutton-Tyrrell K. Progression rates of carotid intima-media thickness and adventitial diameter during the menopausal transition. Menopause. (2013) 20:8–14. doi: 10.1097/gme.0b013e3182611787
13. Salvi P. Mean arterial pressure. Pulse Waves: How Vascular Hemodynamics Affects Blood Pressure. 1st ed. Springer Publishing Co: Verlage, Italia. (2012). p. 3–7. doi: 10.1007/978-88-470-2439-7_2
14. Block G, Hartman AM, Dresser CM, Carroll MD, Gannon J, Gardner L, et al. data-based approach to diet questionnaire design and testing. Am J Epidemiol. (1986) 124:453–69. doi: 10.1093/oxfordjournals.aje.a114416
15. Subar AF, Thompson FE, Kipnis V, Midthune D, Hurwitz P, McNutt S, et al. Comparative validation of the Block, Willett, and National Cancer Institute food frequency questionnaires: the Eating at America's Table Study. Am J Epidemiol. (2001) 154:1089–99. doi: 10.1093/aje/154.12.1089
16. Kweon S, Kim Y, Jang MJ, Kim Y, Kim K, Choi S, et al. Data resource profile: the Korea National Health and Nutrition Examination Survey (KNHANES). Int J Epidemiol. (2014) 43:69–77. doi: 10.1093/ije/dyt228
17. Block G, Thompson FE, Hartman AM, Larkin FA, Guire KE. Comparison of two dietary questionnaires validated against multiple dietary records collected during a 1-year period. J Am Diet Assoc. (1992) 92:686–93.
18. Tricarico JM, Slimko ML, Graves WB, Eve MD, Thurston JA. Elevating dairy research and extension through partnership: outcomes from the United States Department of Agriculture and National Dairy Council collaborative meeting to develop a coordination roadmap. J Dairy Sci. (2019) 102:9518–24. doi: 10.3168/jds.2019-16579
19. Obata K, Ikeda K, Yamasaki M, Yamori Y. Dietary fiber, psyllium, attenuates salt-accelerated hypertension in stroke-prone spontaneously hypertensive rats. J Hypertens. (1998) 16:1959–64. doi: 10.1097/00004872-199816121-00016
20. Li J, Wang J, Kaneko T, Qin LQ, Sato A. Effects of fiber intake on the blood pressure, lipids, and heart rate in Goto Kakizaki rats. Nutrition. (2004) 20:1003–7. doi: 10.1016/j.nut.2004.08.010
21. Galisteo M, Sánchez M, Vera R, González M, Anguera A, Duarte J, et al. Diet supplemented with husks of Plantago ovata reduces the development of endothelial dysfunction, hypertension, and obesity by affecting adiponectin and TNF-alpha in obese Zucker rats. J Nutr. (2005) 135:2399–404. doi: 10.1093/jn/135.10.2399
22. Sánchez D, Quiñones M, Moulay L, Muguerza B, Miguel M, Aleixandre A. Soluble fiber-enriched diets improve inflammation and oxidative stress biomarkers in Zucker fatty rats. Pharmacol Res. (2011) 64:31–5. doi: 10.1016/j.phrs.2011.02.005
23. Saltzman E, Das SK, Lichtenstein AH, Dallal GE, Corrales A, Schaefer EJ, et al. An oat-containing hypocaloric diet reduces systolic blood pressure and improves lipid profile beyond effects of weight loss in men and women. J Nutr. (2001) 131:1465–70. doi: 10.1093/jn/131.5.1465
24. Pins JJ, Geleva D, Keenan JM, Frazel C, O'Connor PJ, Cherney LM. Do whole-grain oat cereals reduce the need for antihypertensive medications and improve blood pressure control? J Fam Pract. (2002) 51:353–9.
25. He J, Streiffer RH, Whelton PK. Effect of dietary fiber supplementation on blood pressure: a randomised, double-blind, placebo-controlled trial. J Hypertens. (2004) 22:73–80. doi: 10.1097/00004872-200401000-00015
26. Cassano V, Crescibene D, Hribal ML, Pelaia C, Armentaro G, Magurno M, et al. Uric acid and vascular damage in essential hypertension: role of insulin resistance. Nutrients. (2020) 12:2509. doi: 10.3390/nu12092509
27. Ferri C, Bellini C, Desideri G, Valenti M, De Mattia G, Santucci A, et al. Relationship between insulin resistance and nonmodulating hypertension: linkage of metabolic abnormalities and cardiovascular risk. Diabetes. (1999) 48:1623–30. doi: 10.2337/diabetes.48.8.1623
28. Theilmeier G, Verhamme P, Dymarkowski S, Beck H, Bernar H, Lox M, et al. Hypercholesterolemia in minipigs impairs left ventricular response to stress: association with decreased coronary flow reserve and reduced capillary density. Circulation. (2002) 106:1140–6. doi: 10.1161/01.CIR.0000026805.41747.54
29. Vogel RA, Corretti MC, Plotnick GD. Changes in flow-mediated brachial artery vasoactivity with lowering of desirable cholesterol levels in healthy middle-aged men. Am J Cardiol. (1996) 77:37–40. doi: 10.1016/S0002-9149(97)89131-X
30. Anderson TJ Meredith IT Yeung AC Frei B Selwyn AP Ganz P. The effect of cholesterol-lowering and antioxidant therapy on endothelium-dependent coronary vasomotion. N Engl J Med. (1995) 332:488–93. doi: 10.1056/NEJM199502233320802
31. Lattimer JM, Haub MD. Effects of dietary fiber and its components on metabolic health. Nutrients. (2010) 2:1266–89. doi: 10.3390/nu2121266
32. Slavin JL. Dietary fiber and body weight. Nutrition. (2005) 21:411–8. doi: 10.1016/j.nut.2004.08.018
Keywords: dietary fiber, blood pressure, hypertension, midlife women, smooth curve
Citation: Du P, Luo K, Wang Y, Xiao Q, Xiao J, Li Y and Zhang X (2021) Intake of Dietary Fiber From Grains and the Risk of Hypertension in Late Midlife Women: Results From the SWAN Study. Front. Nutr. 8:730205. doi: 10.3389/fnut.2021.730205
Received: 24 June 2021; Accepted: 12 August 2021;
Published: 16 September 2021.
Edited by:
Sergio Davinelli, University of Molise, ItalyReviewed by:
Maria Montserrat Diaz Pedrosa, State University of Maringá, BrazilCopyright © 2021 Du, Luo, Wang, Xiao, Xiao, Li and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yong Li, bHlsZnkwNjA2QDE2My5jb20=; Xingjian Zhang, bGZ5emhhbmdib0AxNjMuY29t
†These authors share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.