
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
BRIEF RESEARCH REPORT article
Front. Nutr. , 06 August 2021
Sec. Eating Behavior
Volume 8 - 2021 | https://doi.org/10.3389/fnut.2021.673158
This article is part of the Research Topic The Effects of the COVID-19 Outbreak on Food Supply, Dietary Patterns, Nutrition and Health: Volume 1 View all 18 articles
Charitable food services, including food banks and pantries, support individual and households' food access, potentially maintaining food security and diet quality during emergencies. During the COVID-19 pandemic, the use of food banks and pantries has increased in the US. Here we examine perceptions of food banks and food pantries and their relationship to food security and fruit and vegetable (FV) intake during the first 6 months of the COVID-19 pandemic, using a statewide representative survey (n = 600) of residents of Vermont. The utilization of food pantries was more common among food insecure households and households with children. Among food insecure respondents, those who did not use a food pantry were significantly more likely to report consuming less FV during the pandemic. Further, we find respondents who are food insecure and using a food pantry report consuming more FV since the onset of the COVID-19 pandemic. We found that respondents who were both food insecure and reported not using a food pantry were significantly more likely to report both a reduction in fruit consumption (b = −0.58; p = 0.001) and a reduction in vegetable consumption (b = −0.415; p = 0.012). These results indicate that these services may support food access and one important dimension of diet quality (FV intake) for at-risk populations during emergencies.
The COVID-19 pandemic, associated shutdowns, and social distancing measures designed to slow its spread have profoundly impacted the US food system and food access. According to the Pew Research Center, job disruptions have been widespread; lower-income adults have been hardest hit, with half of their households reporting a job or wage loss due to the pandemic (1). These disruptions have been disproportionately acute among women, low-income communities, and people of color (1), which have catalyzed important changes in the food supply chain and food security. Recent research suggests that the food insecurity rates have reached levels unprecedented in recent history (2–4).
With the shift from worksites, schools, and restaurant dining, to greater at-home preparation and consumption, food procurement shifted and, in many cases, overwhelmed grocery stores (5). Simultaneously, food insecure populations turned to charitable feeding systems (e.g., food banks, pantries) (6). Demands for charitable food services are reported to have increased from 50 to 140% in the first months of the COVID-19 pandemic (7, 8). In the year prior to the pandemic, 18% of Vermonters reported experiencing food insecurity (2). Food insecurity rose by 32% in the first months following the outbreak (2). By June 2020, nationwide, more than 82% of food banks reported higher numbers of patrons than they did the year prior (9). A longitudinal population-level survey conducted in Vermont in March and May 2020 found that demand for charitable food services increased by 68%, from 7.1 to 12.0% (10). In October 2020, Feeding America reported they were on track to distribute 50% more food when comparing October 2019 and October 2020 (11).
Health inequalities in the US follow a socioeconomic continuum where low-income, low-resource households disproportionally experience higher levels of food-related health risks (12). Further, inequalities, lack of transportation, and geographic disparities magnify structural and environmental factors contributing to food insecurity and poor dietary health (13, 14). Compared to wealthier households, low-income households cook more meals at home (15) yet consume fewer fruits and vegetables (FV) (16) and are more likely not to meet the servings of FV recommended by the Dietary Guidelines for Americans (17). Nanney et al. (18) examined 269 food shelves using the HEI-2010 (Healthy Eating Index) and concluded that the majority of available food (89%) “needs improvement” for nutritional adequacy. Further, they found significant seasonal fluctuations with the month and quarter scores in July, August, and September significantly higher than in December.
Charitable food services vary in FV distribution from region to region. Vermont is known for its resilient local food system (19) and has several agencies, organizations, and programs to help address hunger issues in the state. According to the Hunger in America 2014 (13) report for Vermont Foodbank, of the 23 meal-based relief agencies analyzed, 42.1% aided clients in accessing local food resources. Further, many sites have introduced client choice (20) to provide food pantry patrons choice; many additional organizations have been transitioning to a client-choice model. This approach allows clients to take products they want and will use. By incorporating behavioral economic techniques, recent initiatives have shown success in nudging clients to select more fruits, vegetables, and nutrient-dense foods (21). COVID-19 has presented new challenges for these programs as they work to meet growing food needs while protecting staff, volunteers, and clients' health.
This study aims to understand charitable food programs' role during the first 6 months of the COVID-19 pandemic. Emerging international research suggests that COVID-19 mitigation has negatively impacted diet quality during the pandemic (22). We explore how FV intake changed among a representative sample of Vermonters and examine the emergency food system's role in maintaining access to FVs during a humanitarian crisis.
The research team, in collaboration with other researchers in the National Food Access and COVID research Team (NFACT) (22), developed and piloted a survey in March 2020 (23). After two rounds of data collection in March 2020 and June 2020, additional refinements to the pilot survey included food access, food security, food purchasing, food assistance program participation, dietary intake, perceptions of COVID-19, and individual social distancing behaviors, as well as household and individual sociodemographics (24). Data collection for this study was conducted in August and September 2020 (25). We obtained Institutional Review Board approval from the University of Vermont (IRB protocol 00000873). The survey was explicitly designed to measure critical outcomes (e.g., food access, food security, food purchasing, and dietary intake) both before the COVID-19 outbreak (dated as of March 11, 2020, the day the World Health Organization declared a global pandemic) (26) and since the pandemic began. The survey utilizes validated measures when possible (Supplementary Table 1). The survey was piloted in Vermont, with 25 eligible (18 or older) residents in late March, and validation methods (e.g., Cronbach alpha, factor analysis) were used to test the internal validity of questions with key constructs (alpha > 0.70) (2).
We deployed our online survey to a panel of respondents recruited by Qualtrics (Provo, UT). We developed a sampling strategy for achieving a general population sample reflecting characteristics of the state including income, race, and ethnicity in Vermont. This sample was achieved by matching sample recruitment quotas to the income, race (specifically White, Black or African American, American Indian and Alaska Native, Asian, Native Hawaiian or Other Pacific Islander, and Two or more races), and ethnicity (Hispanic, non-Hispanic) population profile of Vermont in the American Community Survey (ACS) (Supplementary Table 2) (27). A total of 600 people ages 18 and over responded to the survey, representing a margin of error (95% confidence level) for the adult population of Vermont ±4% (27).
We explore three self-reported dependent variables in this analysis (Supplementary Table 1). First, we measured food security status using the US Department of Agriculture's 6-item short-form food security module (28). We asked respondents to reflect on the year before the COVID-19 pandemic to collect pre-pandemic food security status. Further, the traditional 12-month period was modified to ~6 months to measure food security status since the start of the COVID-19 pandemic. Following standard scoring protocol, we summarized responses for each item, and classified respondents who answered one or two items affirmatively as living in food insecure households. Second, we measured current FV intake using the National Cancer Institute's two-item screener, modified to apply to the last month and with some example foods removed to shorten it (29). Finally, we examined the perceived change in FV consumption since the onset of the COVID-19 pandemic. Independent variables included multiple questions related to current food bank and food pantry use, specific charitable food system participant experiences, and transportation other than their own vehicle; we also captured several household and individual-level demographics (Table 1).
To examine differences in household food insecurity during the first 6 months of the COVID-19 pandemic, we created three categories of respondents: (1) households with food security, including households that were food secure before and since the onset of the COVID-19 pandemic and households who were food insecure at some point in the year before the COVID-19 pandemic began but were no longer food insecure during the first 6 months of the pandemic; (2) households with persistent food insecurity, food insecure both at some point in the year before the COVID-19 pandemic began and experiencing food insecurity at some point during the first 6 months of the pandemic; (3) households with new food insecurity, categorized as food secure at all times in the year before the COVID-19 pandemic began, but food insecure at some point since the start of the pandemic. We report statistical significance as anything p < 0.05.
To determine statistically significant differences between groups, we utilized SPSS Version 27 (30) and Stata Version 16 (31) to run descriptive statistics, chi-square tests, and multivariable logit models. Specifically, we used chi-square tests to analyze food pantry use related to each item of the food security module. In our multivariable regression models, we use a set of demographic controls including gender, children in the household, respondents over 55, respondents identifying as Black, Indigenous, or People of Color (BIPOC) and/or Hispanic, food security status (28), households with any job loss or negative change since the start of the pandemic, households making <$50,000 in 2019, and households using transportation for food access other than their own vehicle (e.g., public transportation, ride from a friend) since March 2020. It is important to note that although this survey is representative of Vermont state characteristics on race and ethnicity, the sample size is not sufficient to analyze racial and ethnic groups in a disaggregated format in models. Therefore, we have disaggregated race and ethnicity in all food security statistics in the results but use aggregated race and ethnicity for modeling. We used a multivariable logit model with these demographic controls to predict food pantry use (yes/no) since the start of the COVID-19 pandemic. Then, we use a multinomial logit model with demographic controls to predict a change in FV consumption since COVID-19 (decreased, stayed the same, or increased). Finally, we use a multivariable regression model to predict the current intake of FV, measured on a continuous scale, with demographic controls. All variables and their descriptions are included in Supplementary Table 1. Coefficients are reported as odds ratios for the logistic regression model only. We used all available data to estimate effect sizes and interactions and assumed any missing data were missing at random.
Our sample reflected the demographic composition of the Vermont population for income, race, and ethnicity distribution. The majority of our respondents identified as female (67.3%), non-Hispanic White, without children in the household, and had a household income below $75,000 (Table 1). Almost half of the respondents (46.2%) experienced a change in employment at some point between March and September 2020. Changes included loss of employment (24.8%), reduced hours or income (34.7%), and furlough (20.3%). Only 5.0% of respondents utilized transportation other than a personal vehicle between March and September 2020 (Table 1).
Nearly one in three (29.0%) respondent households were food insecure at some point between March and September 2020. Among those experiencing food insecurity since the start of the pandemic (n = 165), 72.1% also experienced food insecurity at some point in the year before the pandemic; in comparison, 27.9% were newly food insecure (Table 1).
The 2020–2025 Dietary Guidelines for Americans (DGA), released on December 28, 2020, recommend that people needing 2,000 calories per day should include at least 2 cups of fruit and 2.5 cups of vegetables in their daily diets. During the COVID-19 pandemic, 15.5% of respondents met the recommendation for fruit intake, and ~27.7% of respondents met the recommendations for vegetables (Table 1).
Multinomial logit models predicted factors contributing to more, less, or the same FV consumption during the first 6 months of COVID-19 (p ≤ 0.001, Table 2). Respondents who were food insecure and did not use a food pantry since the beginning of the COVID-19 pandemic reported consuming significantly less FV (b = 2.29; p < 0.001). Further, among respondents who utilized food pantries since the start of the COVID-19 pandemic, both food insecure and food secure participants also reported consuming significantly less FV (b = 1.72; p < 0.001 and b = 1.174; p = 0.034). Conversely, we found BIPOC/Hispanic respondents were more likely to have increased their FV intake (b = 0.96; p = 0.026) during the first 6 months of the pandemic as compared to non-Hispanic White respondents. Finally, we found that food insecure respondents who reported utilizing a food pantry reported consuming significantly more FV since the start of the COVID-19 pandemic (b = 1.138; p = 0.17)
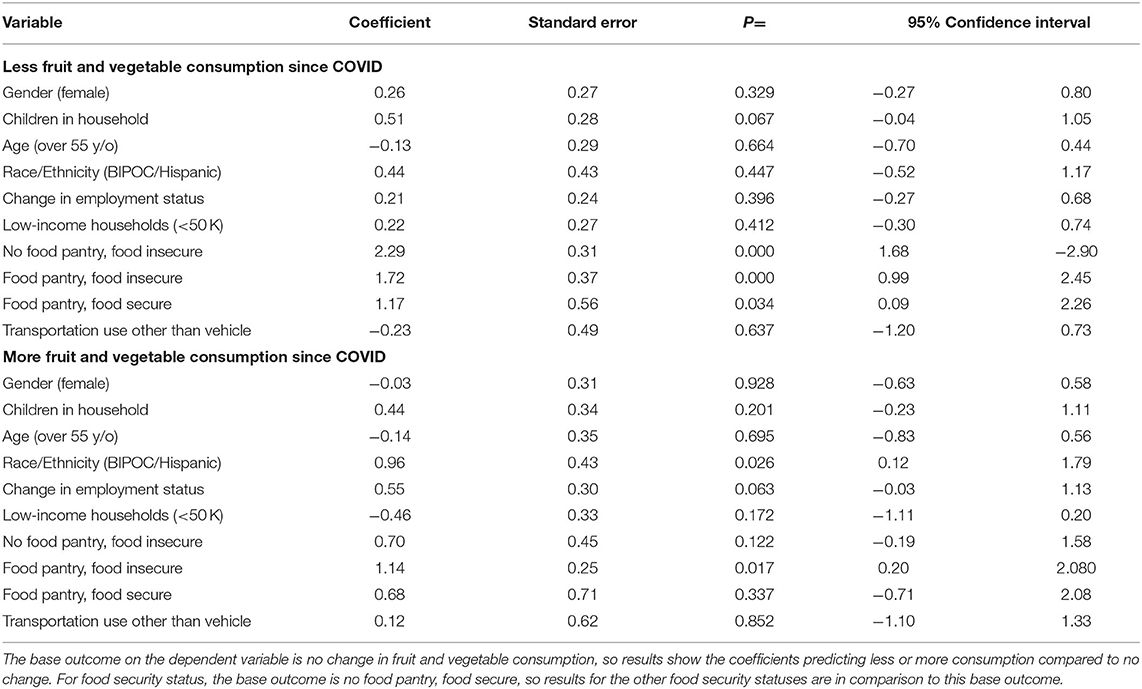
Table 2. Multinomial logit model predicting change in fruit and vegetable consumption during the first 6 months of the COVID-19 pandemic.
Using multivariable regression models, we found that respondents in households with children (b = 0.29; p = 0.039), those who use a form of transportation other than their own vehicle (b = 0.63; p = 0.020), and those over 55 years old (b = 0.27; p = 0.049) reported having higher fruit intake during the first 6 months of the pandemic than respondents from households without children, those who used their own vehicle, and those aged 18–55 years (Table 3). We found that respondents from low-income households (b = −0.39; p = 0.002) and respondents in food insecure households (b = −0.57; p = 0.001) were more likely to report consuming less fruit than higher income and food secure households. We found that respondents over 55 years old (b = 0.34; p = 0.013) reported having higher vegetable intake in the first 6 months of the pandemic compared to younger respondents and those from low-income households (b = −0.63; p = 0.000). Finally, we found that respondents who were both food insecure and reported not using a food pantry were significantly more likely to report both a reduction in fruit consumption (b = −0.58; p = 0.001) and a reduction in vegetable consumption (b = 0.415; p = 0.012).
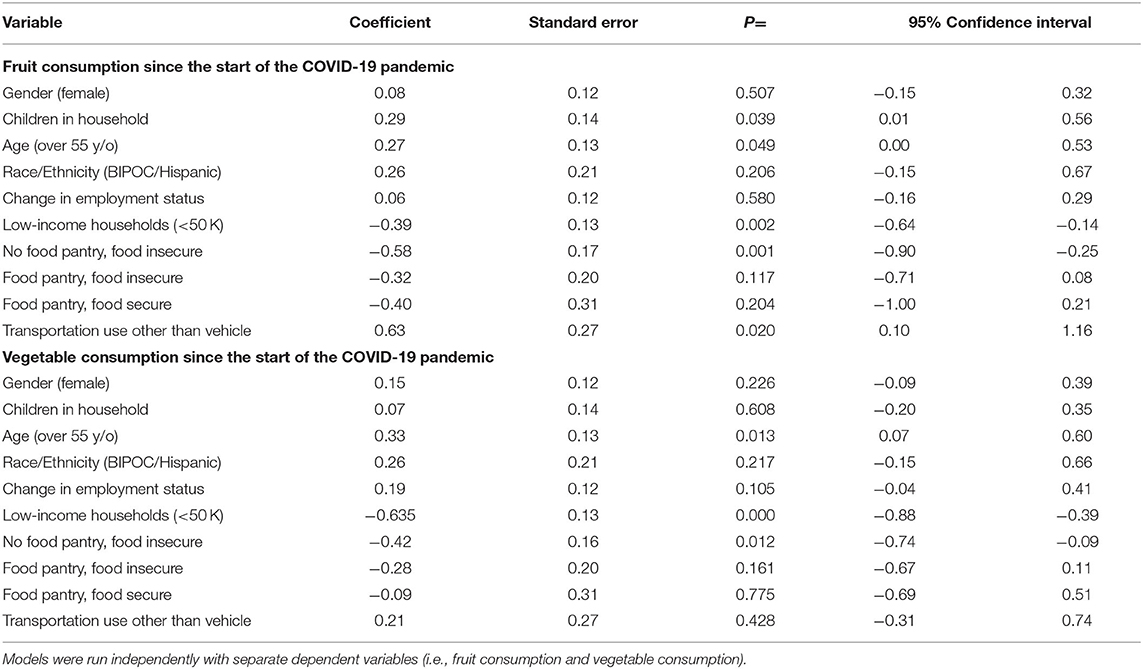
Table 3. Multivariable regression models predicting fruit and vegetable consumption during the first 6 months of COVID-19.
Food pantry users were significantly more likely to be food insecure (p < 0.001) than non-pantry users. While low-income households (earning <$50,000 annually) were more likely to use food pantries, we also found that, for low-income households, using food pantries was associated with greater affirmative responses for each food security item [Chi-squared p < 0.001 for all differences (Supplementary Figure 1; Supplementary Table 3)]. Expressly, as compared to respondents not using a food pantry, 21% fewer respondents from low-income households who utilized a food pantry since March 2020 agreed that the food they had did not last and they did not have money to get more (20.0%; 41.2%) and that they could afford to eat a balanced meal (20.2%; 40.7%). Among those earning $50,000 annually or less, 60% fewer respondents whose households utilized food pantries agreed that adults in their household had cut the size of their meals or skipped meals because there was not enough money for food as compared to respondents whose households did not utilize food pantries (15.6%; 21.1%). Among the same subset of respondents, four percent fewer respondents whose households utilized a food bank or food pantry reported that they had to eat less (17.0%; 20.8%) or cut the size of their meals or skip meals (17.1%; 21.3%) because there was not enough money for food.
About one in seven respondents (14.5%) reported that their household utilized a food bank or food pantry between March and September 2020 (Table 4). Those with increased odds of utilizing these food distribution services were food insecure (OR = 6.55, 95% CI = 3.52, 12.20) and low-income households (OR = 3.85, 95% CI = 2.01, 7.38), and respondents using transportation other than their own vehicle (OR = 4.68, 95% CI = 1.87, 11.70) (Table 4).
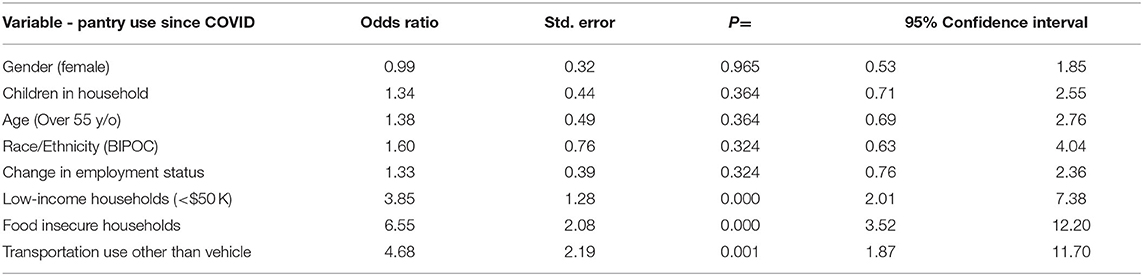
Table 4. Multivariate analysis predicting odds of food pantry use since the start of the COVID-19 pandemic.
We found that the vast majority of respondents (85%) who utilized food pantries during the first 6 months of the pandemic (n = 86) agreed or strongly agreed that food pantries have been helpful (Supplementary Figure 2). Approximately one-third of pantry users indicated concerns, including that pantries run out of food often (35%), have long lines and wait times (34%), and have inconvenient or irregular hours (30%). Other concerns among food pantry users included pantries not having the food their family likes (22%) or good quality food (22%) and not knowing how to prepare food the pantry provides (12%).
To our knowledge, this is the first study to examine the relationship between the charitable food system (food banks, pantries/shelves) and FV consumption during the COVID-19 pandemic. Overall, we find that 14.5% of our respondents utilized a food pantry which mirrors increased demand nationally as evidenced by media outlets' reports (7–9). Among food insecure respondents, we found those who did not use a food pantry were significantly more likely to report consuming less FV during the pandemic. Additionally, we found that respondents who are food insecure and using a food pantry report consuming more FV since the onset of the pandemic. Furthermore, we found that respondents who were both food insecure and reported not using a food pantry were significantly more likely to report both a reduction in fruit consumption and a reduction in vegetable consumption. These results suggest that utilization of food banks and food pantries has a relationship with perceptions of FV access and reported intake.
Although low-income households were more likely to prepare home cooked meals before the COVID-19 pandemic (15), disparities exist in FV intake across socioeconomic status. Home cooked meals are generally associated with higher FV intake (32). While most households do not eat enough FV—low-income households and those with food insecurity are especially at risk of low FV intake and limited dietary variety. Higher FV intake is associated with a reduced risk of cardiovascular disease, cancer, co-morbidities, and all-cause mortality (33). Our results suggest that the food bank/food pantry system may play a role in blunting the adverse effects of a humanitarian crisis like the COVID-19 pandemic by increasing food access for low-income households and thereby mitigating reductions in their overall FV intake.
Although we found an association between food security status and pantry use, Robaina and Martin (32) demonstrated that our low-income pantry users answered specific statements within the USDA Food Security Module at a significantly lower affirmative rate compared to low-income non-users. We recognize that the USDA defines food security based on Anderson's 1990 Report (34), where food security is acquired “without resorting to emergency food supplies” (34). Our findings demonstrate that the food bank/food pantry system may have helped maintain several components of food access and FV intake among food insecure users of this system. Our results suggest that although food bank use does not impact the overall food security rate, food security indicators such as “food did not last” and they “could not afford a balanced meal” are associated with positive outcomes among those using food pantries. Further evidence that use of food banks/food pantries may improve food access includes our findings that 85% of users found food pantries helpful.
As expected, both food insecure and low-income populations are at greater odds of using a food bank/food pantry as compared to food secure and higher income households. We also found the population using any form of transportation other than their own vehicle to be more likely to use a food bank/food pantry, probably due at least in part to the greater reliance on public transportation among low-income persons in the US (35, 36). Further, studies suggest associations between unemployment and significantly lower levels of car ownership especially among BIPOC and female head of household families (37). With state and local social distancing requirements informing distribution, many food pantries have shifted from a super-market-type layout to a drive-up operation where volunteers assembled pre-packaged food boxes and placed them in the patron's vehicle (9). Patrons who rely on public transportation may experience barriers to this new food distribution model. Future studies should include inquiries into the patrons experience with pre-packaged food box distribution.
Although FV intake did not differ between non-Hispanic White and respondents from racial and ethnic minority populations at the time of our survey, BIPOC/Hispanic respondents were more likely to report a significant increase in FV intake during the first 6 months of the COVID-19 pandemic. This is notable and important since increasing FV intake is a national public health goal, and FV intake tends to be lower among some racial and ethnic groups (38). The FV intake among BIPOC respondents mirrors findings in France by Marty et al. (39), who found an increase in FV consumption during the lockdown. However, their subjects also increased their consumption of sugary foods, sodium, and alcoholic beverage, which our study did not capture (40).
We acknowledge that charitable food services are part of a broader system of food access and food security. The charitable food system is designed as an emergency stop-gap and is valuable in crises like the one presented by the COVID-19 pandemic, but does not replace the central role of federal nutrition assistance programs, which are purposely designed to supplement the diverse needs of the most vulnerable Americans. Researchers (41) indicate that the chronic reliance on charitable food services can worsen food security for many households and limit access to culturally and medically appropriate foods. An additional important role of the charitable food system is to help link people to other programs in times of need. It remains to be investigated the extent to which this occurred during the COVID-19 pandemic.
We note a few limitations. First, although our approach's strength was the use of quota sampling to achieve alignment between the sample and the population of Vermont with respect to race, ethnicity, and income, respondents may have differed in other ways. Prior work has demonstrated differences between participants in online survey research and the general population, including greater participation among women, which we saw in our sample (42, 43). Online surveys may lead to response bias and the over-representation of females. Second, self-reported dietary data are subject to recall and response bias (44). Although the two-item FV intake instrument that we used has adequate reliability, it has low validity for measuring precise intake levels (29). We used this instrument to compare individuals concerning FV intake rather than estimate actual intake in line with recommendations (29). Further, our study was conducted in August and September when the availability of local FV is at an annual peak. Research is needed that utilizes a more robust and inclusive measure of dietary intake and dietary quality. Finally, these cross-sectional data do not allow rigorous evaluation of a causal link between food pantry use and food security or FV intake. Future research should address these limitations and consider the longer-term associations between food pantry use, food security, and dietary intake in crisis contexts.
This study documented use and experiences with the charitable food system, including associations with food security and FV intake outcomes, among a statewide sample in Vermont, US, in the first 6 months of the COVID-19 pandemic. We found that food bank/food pantry use significantly increased in Vermont since the start of the COVID-19 pandemic. The results document improved FV intake among low-income households that utilized food pantries as compared with low-income households that did not. Taken together, the results suggest that the charitable food system is an important way in which people can supplement their food budget and maintain food access during a humanitarian crisis. However, it is essential to note that Vermont's resilient food system and support programs may have impacted these results and the seasonal abundance when this survey was conducted. Additional research should be conducted more fully to understand these relationships over time and in greater depth. Increased analysis of the food provided through food pantries serving diverse populations may be important to assess the overall accessibility of healthy, culturally, and medically acceptable foods for at-risk populations. The heightened usage of the charitable food system during the COVID-19 pandemic highlights not only the importance of food pantries but reinforces the need for funding, maintenance, and preparedness of these emergency programs.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
The studies involving human participants were reviewed and approved by Institutional Review Board approval was obtained from the University of Vermont under protocol 00000873. Consent was obtained from all participants prior to data collection. The patients/participants provided their written informed consent to participate in this study.
FB, KR, EB, and MN wrote the original manuscript, provided data curation, code, codebooks, resources, read, edited, and approved the final manuscript. FB and KR provided conceptualization. FB and MN provided methods and data curation. MN, FB, and EB acquired funding. All authors contributed to the article and approved the submitted version.
Funding for this work was provided by the University of Vermont's College of Agriculture and Life Sciences and Office of the Vice President of Research, the Gund Institute for Environment at the University of Vermont, and the USDA Agricultural Research Service Center for Food Systems Research.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fnut.2021.673158/full#supplementary-material
1. Groshen E. How Did COVID-19's Job Disruptions Vary by Gender, Race and Hispanic Ethnicity in May 2020? | The ILR School. Available online at: https://www.ilr.cornell.edu/work-and-coronavirus/work-and-jobs/how-did-covid-19s-job-disruptions-vary-gender-race-and-hispanic-ethnicity-may-2020 (accessed February 26, 2021).
2. Niles MT, Bertmann F, Belarmino EH, Wentworth T, Biehl E, Neff R. The early food insecurity impacts of COVID-19. Nutrients. (2020) 12:2096. doi: 10.3390/nu12072096
3. McCartney M. Margaret McCartney: Clean eating and the cult of healthism. BMJ. (2016) 354:4095. doi: 10.1136/bmj.i4095
4. Wolfson JA, Leung CW. Food insecurity during COVID-19: an acute crisis with long-term health implications. Am J Public Health. (2020) 24:e1–3. doi: 10.2105/AJPH.2020.305953
5. Hobbs JE. Food supply chains during the COVID-19 pandemic. Can J Agric Econ Can Agroeconomie. (2020) 68:171–6. doi: 10.1111/cjag.12237
6. Schwartz M, Levi R, Lott M, Arm K, Seligman H. Healthy eating research nutrition guidelines for the charitable food system. Healthy Eat Res. (2020).
7. Kulish N. ‘Never Seen Anything Like It': Cars Line Up for Miles at Food Banks. The New York Times (2020). Available online at: https://www.nytimes.com/2020/04/08/business/economy/coronavirus-food-banks.html (accessed January 13, 2021).
8. Lakhani N. “A Perfect Storm”: US Facing Hunger Crisis as Demand for Food Banks Soars. The Guardian (2020). Available online at: https://www.theguardian.com/environment/2020/apr/02/us-food-banks-coronavirus-demand-unemployment (accessed January 13, 2021).
9. Pandemic Growing, Need Strain U,.S. Food Bank Operations - WSJ. Available online at: https://www.wsj.com/articles/pandemic-growing-need-strain-u-s-food-bank-operations-11594891802 (accessed January 13, 2021).
10. Niles MT, Josephson AL, Bertmann F, Belarmino EH, Neff R. COVID-19 and Food Insecurity Impacts: A Follow Up Vermont Study. College of Agriculture and Life Sciences Faculty Publications (2020). p. 26. Available online at: https://scholarworks.uvm.edu/calsfac/26
11. Feeding America. The Food Bank Response to COVID, by the Numbers | Feeding America. Available online at: https://www.feedingamerica.org/hunger-blog/food-bank-response-covid-numbers (accessed January 13, 2021).
12. Drewnowski A, Specter SE. Poverty and obesity: the role of energy density and energy costs. Am J Clin Nutr. (2004) 79:6–16. doi: 10.1093/ajcn/79.1.6
13. Feeding America. Hunger In America Study | Feeding America. Available online at: https://www.feedingamerica.org/research/hunger-in-america (accessed January 13, 2021).
14. Clark-Barol M, Gaddis J, Barrett C. Food agency in low-income households: a qualitative study of the structural and individual factors impacting participants in a community-based nutrition program. Appetite. (2021) 158:105013. doi: 10.1016/j.appet.2020.105013
15. Trubek AB, Carabello M, Morgan C, Lahne J. Empowered to cook: the crucial role of “food agency” in making meals. Appetite. (2017) 116:297–305. doi: 10.1016/j.appet.2017.05.017
16. Hoisington A, Manore MM, Raab C. Nutritional quality of emergency foods. J Am Diet Assoc. (2011) 111:573–6. doi: 10.1016/j.jada.2011.01.007
17. United States Department of Agriculture. Home | Dietary Guidelines for Americans. Available online at: https://www.dietaryguidelines.gov/ (accessed January 13, 2021).
18. Nanney MS, Grannon KY, Cureton C, Hoolihan C, Janowiec M, Wang Q, et al. Application of the healthy eating index-2010 to the hunger relief system. Public Health Nutr. (2016) 19:2906–14. doi: 10.1017/S136898001600118X
19. Skog KL, Eriksen SE, Brekken CA, Francis C. Building resilience in social-ecological food systems in Vermont. Sustainability. (2018) 10:4813. doi: 10.3390/su10124813
20. Verpy H, Smith C, Reicks M. Attitudes and behaviors of food donors and perceived needs and wants of food shelf clients. J Nutr Educ Behav. (2003) 35:6–15. doi: 10.1016/S1499-4046(06)60321-7
21. Feeding America. The Power of Nudges: Making the Healthy Choice the Easy Choice in Food Pantries. Hunger and Health. Available online at: https://hungerandhealth.feedingamerica.org/resource/the-power-of-nudges-making-the-healthy-choice-the-easy-choice-in-food-pantries/ (accessed January 15, 2021).
22. Cheikh Ismail L, Osaili TM, Mohamad MN, Al Marzouqi A, Jarrar AH, Abu Jamous DO, et al. Eating habits and lifestyle during COVID-19 lockdown in the United Arab Emirates: a cross-sectional study. Nutrients. (2020) 12:3314. doi: 10.3390/nu12113314
23. Niles MT, Bertmann F, Morgan EH, Wentworth T, Biehl E, Neff R. Food Access and Security During Coronavirus: A Vermont Study. College of Agriculture and Life Sciences Faculty Publications (2020). p. 21. Available online at: https://scholarworks.uvm.edu/calsfac/21
24. Niles MT, Belarmino EH, Bertmann F, Biehl E, Acciai F, Josephson A, et al. Food insecurity during COVID-19: a multi-state research collaborative. medRxiv [Preprint]. (2020). doi: 10.1101/2020.12.01.20242024
25. Niles MT, Belarmino EH, Bertmann F. COVID-19 Impacts on Food Security and Systems: A Third Survey of Vermonters. College of Agriculture and Life Sciences Faculty Publications (2020). p. 27. Available online at: https://scholarworks.uvm.edu/calsfac/27
26. World Health Organization. WHO Director-General's Opening Remarks at the Media Briefing on COVID-19. (2020). Available online at: https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 (accessed January 13, 2021).
27. Vermont Department of Health. Vermont Population Estimates. Vermont Department of Health (2016). Available online at: https://www.healthvermont.gov/health-statistics-vital-records/vital-records-population-data/vermont-population-estimates (accessed January 13, 2021).
28. United States Department of Agriculture. Food Security Survey Module: Six-Item Short Form. SNAP Education Connection. Available online at: https://snaped.fns.usda.gov/library/materials/food-security-survey-module-six-item-short-form (accessed January 13, 2021).
29. Yaroch AL, Tooze J, Thompson FE, Blanck HM, Thompson OM, Colón-Ramos U, et al. Evaluation of three short dietary instruments to assess fruit and vegetable intake: the National Cancer Institute's food attitudes and behaviors survey. J Acad Nutr Diet. (2012) 112:1570–7. doi: 10.1016/j.jand.2012.06.002
30. SPSS Statistics. SPSS Statistics - Overview. (2020). Available online at: https://www.ibm.com/products/spss-statistics (accessed February 19, 2021).
32. Mills S, Brown H, Wrieden W, White M, Adams J. Frequency of eating home cooked meals and potential benefits for diet and health: cross-sectional analysis of a population-based cohort study. Int J Behav Nutr Phys Act. (2017) 14:109. doi: 10.1186/s12966-017-0567-y
33. Aune D, Giovannucci E, Boffetta P, Fadnes LT, Keum N, Norat T, et al. Fruit and vegetable intake and the risk of cardiovascular disease, total cancer and all-cause mortality-a systematic review and dose-response meta-analysis of prospective studies. Int J Epidemiol. (2017) 46:1029–56. doi: 10.1093/ije/dyw319
34. Committee on National Statistics Division of Behavioral and Social Sciences and Education Food and Nutrition Board National Research Council Institute of Medicine. Defining and Measuring Food Security. Research Opportunities Concerning the Causes and Consequences of Child Food Insecurity and Hunger: A Workshop Summary. National Academies Press (US) (2013). Available online at: http://www.ncbi.nlm.nih.gov/books/NBK201388/ (accessed January 15, 2021).
35. Robaina KA, Martin KS. Food insecurity, poor diet quality, and obesity among food pantry participants in Hartford, CT. J Nutr Educ Behav. (2013) 45:159–64. doi: 10.1016/j.jneb.2012.07.001
36. Sanchez TW. Poverty, policy, and public transportation. Transp Res Part Policy Pract. (2008) 42:833–41. doi: 10.1016/j.tra.2008.01.011
37. Duque V, Pilkauskas NV, Garfinkel I. Assets among low-income families in the Great Recession. PLoS ONE. (2018) 13:e0192370. doi: 10.1371/journal.pone.0192370
38. Storey M, Anderson P. Income and race/ethnicity influence dietary fiber intake and vegetable consumption. Nutr Res. (2014) 34:844–50. doi: 10.1016/j.nutres.2014.08.016
39. Lucile M, de Lauzon-Guillain B, Labesse M, Nicklaus S. Food choice motives and the nutritional quality of diet during the COVID-19 lockdown in France. Appetite. 157:105005. doi: 10.1016/j.appet.2020.105005
40. Hoy MK, Goldman JD, Moshfegh AJ. Differences in fruit and vegetable intake of U.S. adults by sociodemographic characteristics evaluated by two methods. J Food Compos Anal. (2017) 64:97–103. doi: 10.1016/j.jfca.2017.06.012
41. Leddy AM, Weiser SD, Palar K, Seligman H. A conceptual model for understanding the rapid COVID-19-related increase in food insecurity and its impact on health and healthcare. Am J Clin Nutr. (2020) 112:1162–9. doi: 10.1093/ajcn/nqaa226
42. Huff C, Tingley D. “Who are these people?” Evaluating the demographic characteristics and political preferences of MTurk survey respondents. Res Polit. (2015) 2:2053168015604648. doi: 10.1177/2053168015604648
43. Coppock A, McClellan OA. Validating the demographic, political, psychological, and experimental results obtained from a new source of online survey respondents. Res Polit. (2019) 6:2053168018822174. doi: 10.1177/2053168018822174
44. Thompson FE, Subar AF. Chapter 1 - dietary assessment methodology. In: Coulston AM, Boushey CJ, Ferruzzi MG, Delahanty LM, editors. Nutrition in the Prevention and Treatment of Disease (Fourth Edition). Academic Press (2017). p. 5–48. Available online at: http://www.sciencedirect.com/science/article/pii/B9780128029282000011 (accessed January 13, 2021).
Keywords: food security, coronavirus, food pantry, emergency food assistance, nutrition security
Citation: Bertmann F, Rogomentich K, Belarmino EH and Niles MT (2021) The Food Bank and Food Pantries Help Food Insecure Participants Maintain Fruit and Vegetable Intake During COVID-19. Front. Nutr. 8:673158. doi: 10.3389/fnut.2021.673158
Received: 26 February 2021; Accepted: 13 July 2021;
Published: 06 August 2021.
Edited by:
Igor Pravst, Institute of Nutrition, SloveniaReviewed by:
Dan Remley, The Ohio State University, United StatesCopyright © 2021 Bertmann, Rogomentich, Belarmino and Niles. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Farryl Bertmann, ZmJlcnRtYW5AdXZtLmVkdQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.