- 1Department of Cardiology, The Second Affiliated Hospital of Harbin Medical University, Harbin, China
- 2Key Laboratory of Myocardial Ischemia, Ministry of Education, Harbin Medical University, Harbin, China
- 3Department of Epidemiology and Biostatistics, School of Public Health, Jiamusi University, Jiamusi, China
Background: Serum uric acid can act as a risk factor for cardiovascular disease (CVD) and as antioxidant defense. Vitamin D deficiency can activate the parathyroid to induce the release of parathyroid hormone, which was thought to increase serum uric acid level, and low vitamin D status may also be associated with risk of CVD. No known studies have explored the association between serum 25(OH) D, vitamin D intake, and HU for the American population.
Methods: We extracted 15,723 US adults aged 20–85 years from the National Health and Nutrition Examination Survey (NHANES) in 2007–2014. All dietary intakes were evaluated through 24-h dietary recalls. Multivariable logistic regression analysis was performed to examine the associations after adjustment for confounders.
Results: Compared to the lowest quintile (Q1), for males, adjusted odds ratios (ORs) of HU in Q2 to Q4 of serum 25(OH) D levels were 0.78 (95% CI, 0.65–0.93), 0.97 (0.81–1.16), and 0.72 (0.60–0.88); ORs in Q2–Q5 of total vitamin D intake were 0.83 (0.69–0.98), 0.69 (0.58–0.83), 0.66 (0.55–0.79), and 0.59 (0.48–0.71), respectively. In females, OR was 0.80 (0.66–0.97) of serum 25(OH) D for Q3, and ORs in Q5 of total vitamin D intake were 0.80 (0.65–0.98).
Conclusions: Our findings indicated that the serum 25(OH) D intakes of dietary vitamin D, supplemental vitamin D, and total vitamin D were inversely associated with HU in males. In females, a lower risk of HU with higher serum 25(OH) D, dietary vitamin D, and total vitamin D intake was found, but with no association between supplemental vitamin D intake and the risk of HU.
Introduction
Hyperuricemia (HU), which is caused by either overproduction or underexcretion of urate, has been always considered as a precursor of gout due to accumulation of uric acid crystals (1, 2). Several studies have confirmed an association between HU and cardiovascular disease (CVD), serum uric acid can act as a risk factor for CVD and as antioxidant defense (3), and HU has an raised frequency of occurrence among people with high risk of CVD (4). Moreover, recent epidemiologic studies link HU with other diseases such as chronic kidney disease and metabolic syndrome (5, 6). Nowadays, HU is becoming a serious public health problem, many epidemiological studies had shown a growing trend in the prevalence of HU and gout (7, 8).
Vitamin D, the fat-soluble vitamin, is obtained from food, supplements, and sun exposure. The serum concentration of 25-hydroxyvitamin D (25(OH) D) is the best indicator of vitamin D status (9). Several studies have indicated that low vitamin D status may also be associated with risk of CVD (10, 11), chronic kidney diseases (12, 13), and metabolic syndrome (14, 15). Furthermore, vitamin D deficiency can activate the parathyroid to induce the release of parathyroid hormone (16), which was thought to increase serum uric acid level (17–20). As previous clinical research suggested that parathyroid hormone increased the incidence of HU among postmenopausal women (18), parathyroid hormone has significant biologic influence on serum uric acid (17, 20).
No known studies have explored the association between serum 25(OH) D, vitamin D intake, and HU for the American population. Therefore, the purpose of this cross-sectional study is to assess this correlation using a large sample size (15,723 subjects) among both male and female in the United States (US), with a hypothesis that serum 25(OH) D and vitamin D intake is inversely correlated with HU.
Methods
Study Populations
Study participants comprised US adults aged 20–85 years who participated in the National Health and Nutrition Examination Survey (NHANES) 2007–2014. NHANES is a continuous survey with data released in two-year cycles of the US civilian, using a stratified, multistage sampling design to attain nationally representative estimates on diet and health indicators. The sample for NHANES is administered by the Centers for Disease Control and Prevention (CDC) (21). NHANES is a publicly available dataset, which resides in the public domain (available on the web at http://www.cdc.gov/nchs/nhanes.htm). Each survey participant completed a household interview and underwent a physical examination at a mobile examination center. Detailed descriptions of NHANES methods are published elsewhere (22, 23). NHANES protocols were approved by the National Center for Health Statistics Research ethics review board, and written informed consent was achieved for all participants (24).
A total of 22,673 adults from 2007 to 2014 aged 20–85 years with uric acid samples constituted the study sample. We excluded pregnant women (n = 247); participants taking medications that might affect uric acid metabolism, such as losartan, furosemide, and allopurinol (n = 1,404); and those with missing or incomplete essential information on demographic or total nutrient intakes dietary interview (n = 5,299). After exclusions, 15,723 adults (7,927 men and 7,796 women) were included in this analysis.
Study Variables
The major variables included concentrations of uric acid, serum 25(OH) D, and intake of vitamin D. HU was defined as serum uric acid ≥6.0 mg/dL in females and ≥7.0 mg/dL in males (25). Serum uric acid levels were measured using a Beckman UniCel® DxC800 Synchron or a Beckman Synchron LX20 (Beckman Coulter, Inc., Brea, CA, USA) after oxidation of uric acid by uricase to allantoin and hydrogen peroxide. Serum 25(OH)D measurements were performed at the National Center for Environmental Health, CDC, Atlanta, GA, using the DiaSorin radioimmunoassay (RIA) kit (Stillwater MN), and using a standardized liquid chromatography-tandem mass spectrometry (LC-MS/MS) method (26). The intake of total vitamin D, dietary vitamin D, supplemental vitamin D, energy, protein, carbohydrate, magnesium, zinc, fiber, and sugars was obtained from total nutrient intakes provided by the first 24-h dietary recall interviews, which was obtained in-person in the Mobile Examination Center (MEC). Total vitamin D includes both dietary vitamin D and supplemental vitamin D. All patients were interviewed through the first 24-h dietary recall, and a part of patients participated in second dietary surveys by the telephone interviews 3–10 days after the initial recall interview.
Variables that had been demonstrated to be correlated with the vitamin D (serum 25(OH) D and the intake of vitamin D) status as well as HU were included in regression models to control for possible confounding. The covariates including age, race/ethnicity (defined as non-Hispanic white, non-Hispanic black, Mexican American, and others), education (classified into above high school, high school graduation/general educational development (GED), marital status (grouped into married or living with partner, and living alone), weight, height, and blood pressure were conducted following standardized protocol. Body mass index (BMI) was calculated as weight divided by height2 (kg/m2). Smoking status was grouped as never, current, and former smoker, and participants were divided into never drinkers and current drinkers. Hypertension was identified as systolic blood pressure ≥140 mmHg or diastolic blood pressure ≥90 mmHg (n = 3,071), and participants taking antihypertensive medications (n = 2,442). Diabetes status was achieved through self-report (n = 1,656), and participants taking anti-diabetic medications (n = 100). Laboratory analysis covariates included serum creatinine, serum total cholesterol (STC), serum calcium, glucose, serum triglycerides (STG), and high-density lipoprotein cholesterol (HDL-C).
Statistical Analyses
All statistical analyses were conducted using SAS version 9.4 (SAS Institute Inc., Cary, NC, USA). The continuous variables were presented as median (interquartile range) or mean (standard deviation). Covariates were compared among five groups with differing serum 25(OH) D levels. The categorical variables were characterized by percentage. Differences between continuous variables were assessed by the Wilcoxon rank-sum test and Kruskal–Wallis H test, depending on heteroscedasticity and the skewed distributed data. Differences between categorical variables were evaluated using the chi-square test. Multivariable logistic regression analysis was used to estimate the odds ratio (OR) and 95% confidence interval (CI) of HU, according to the serum 25(OH) D status and vitamin D intake quintile for males and females separately, with the lowest quintile being considered as the references, respectively. Covariates were chosen based on some published studies. Survey weights were not used. Model 1 controlled for age and race/ethnicity. Based on model 1, Model 2 additionally adjusted for drinking status, smoking status, diabetes status, and hypertension status. Based on model 2, Model 3 further controlled for creatinine, total cholesterol, glucose, BMI, HDL-C, triglycerides, serum calcium, magnesium intake, zinc intake, and fiber intake. A sensitivity analysis was undertaken using the second 24-h dietary recall data. P-value < 0.05 (two-sided) was considered as statistically significant.
Results
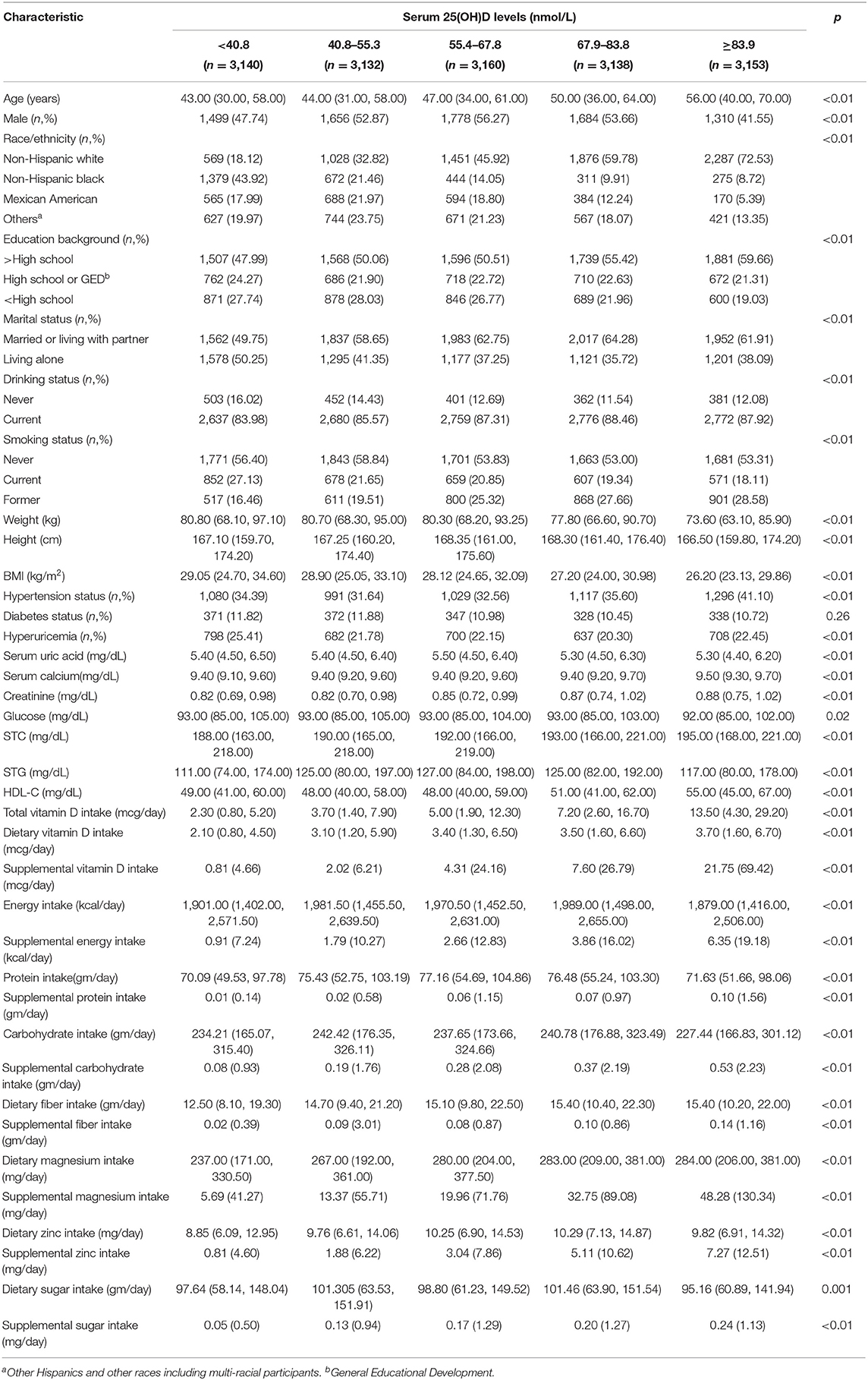
A total of 15,723 adult subjects were eventually enrolled in this study, which consisted of 7,927 males and 7,796 females. The characteristics of study participants were grouped into five levels, according to the levels of serum 25-hydroxyvitamin D (25(OH) D) quintile, as shown in Table 1. Significant differences were detected across all quintiles of serum 25(OH)D levels for age, race/ethnicity, gender, smoking status, drinking status, education background, marital status, hypertension status, hyperuricemia status, serum uric acid, creatinine, serum total cholesterol (SCT), glucose, body mass index (BMI), high-density lipoprotein cholesterol (HDL-C), serum triglycerides (STG), serum calcium, energy intake, protein intake, carbohydrate intake, magnesium intake, zinc intake, total vitamin D intake, dietary vitamin D intake, supplemental vitamin D intake, fiber intake and sugar intake. Participants with higher serum 25(OH) D levels were more likely to be older, non-Hispanic white, and above high school and have higher serum calcium, creatinine, STC, and intakes of total vitamin D, dietary vitamin D, supplemental vitamin D, dietary fiber intake, dietary magnesium intake, and supplemental intakes of energy, protein, carbohydrate, fiber, magnesium, zinc and sugars and were less likely to be currently smoking and to have hyperuricemia less likely to have lower weight, BMI, and serum uric acid.
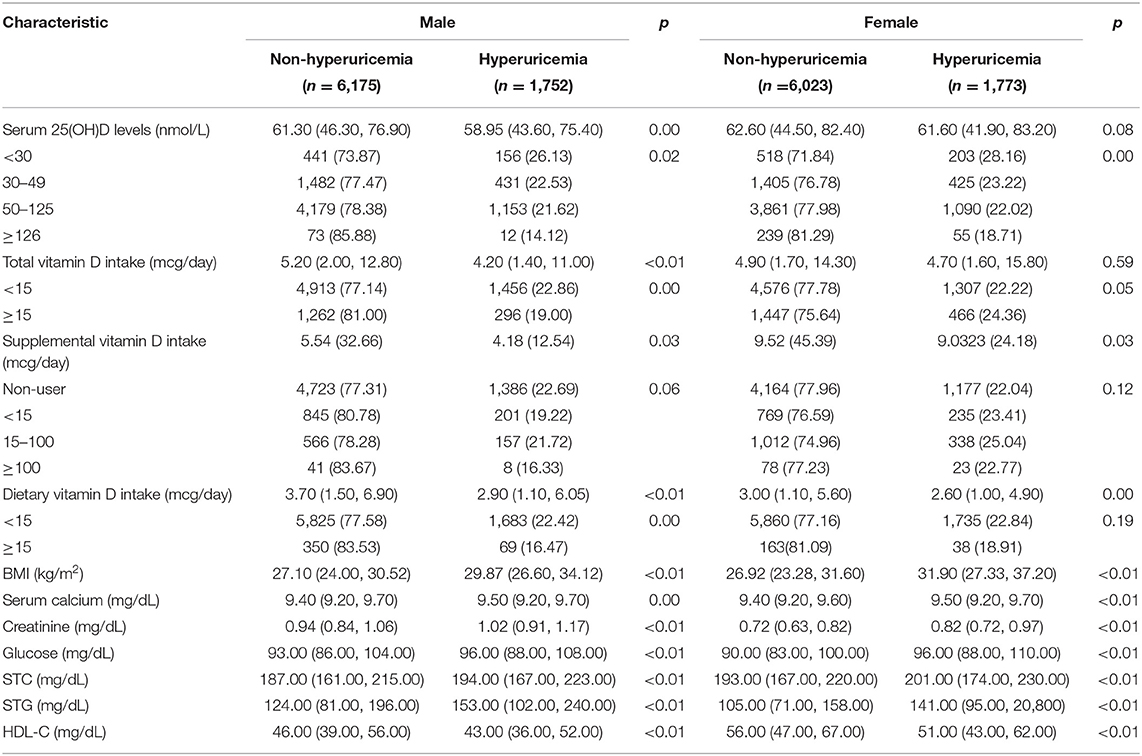
The results comparing the vitamin D status and other indicators between HU and non-HU for both sexes are shown in Table 2. For male, serum 25(OH) D levels and intakes of total vitamin D, dietary vitamin D, and supplemental vitamin D indicators were significantly different between HU and non-HU. Compared to the participants without HU, participants with HU had lower serum 25(OH) D levels and lower intakes of total vitamin D and dietary vitamin D. For female, serum 25(OH) D levels and intakes of dietary vitamin D and supplemental vitamin D indicators were significantly different between HU and non-HU. Participants with HU had lower serum 25(OH) D levels and intakes of dietary vitamin D. Patients with HU had higher levels of BMI, serum calcium, creatinine, STC, STG, and glucose and lower level of HDL cholesterol than those participants without HU for both sexes.
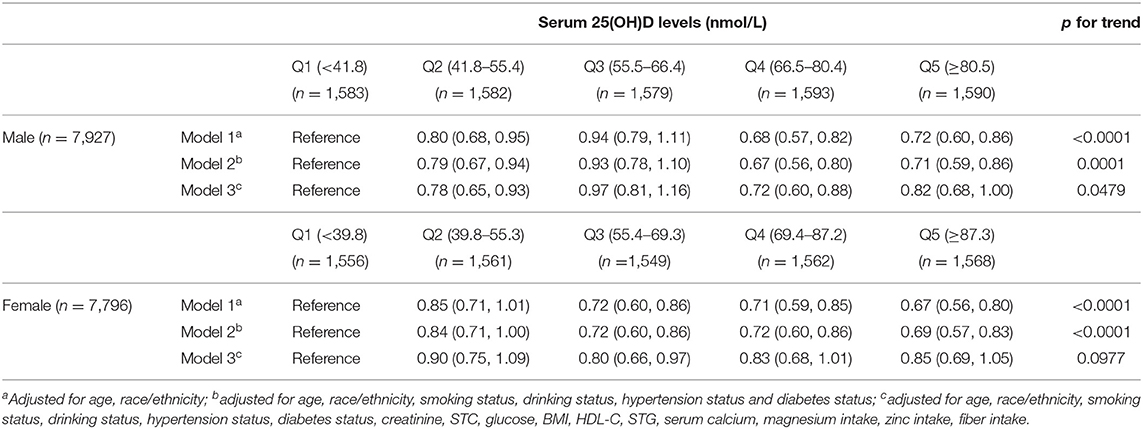
The association between serum 25(OH) D levels and HU was observed in the multivariable model, as is shown in Table 3. There was an inverse trend between higher serum 25(OH) D levels and risk of HU, after controlling for age, race/ethnicity, drinking status, smoking status, diabetes status, hypertension status, creatinine, SCT, glucose, BMI, HDL-C, STG, serum calcium, magnesium intake, zinc intake, and fiber intake. In males, compared with the lowest quintile (Q1; serum 25(OH) D levels <41.8 nmol/L), the adjusted odds ratios (ORs) of HU in Q2–Q4 were 0.78 (95% CI, 0.65–0.93), 0.97 (95% CI, 0.81–1.16), and 0.72 (95% CI, 0.60–0.88), respectively, and that of Q5 was 0.82 (95% CI, 0.68–1.00); p for the trend was 0.0479. In females, compared with Q1 (respondents with serum 25(OH) D levels <39.8 nmol/L), OR was 0.80 (95% CI, 0.66–0.97) for Q3 (55.4–69.3 nmol/L), and p for the trend was 0.0977.
There was an inverse trend between higher dietary vitamin D intakes and risk of HU, as is shown in Table 4. In males, compared with Q1 (respondents consuming <1.1 mcg dietary vitamin D daily), the adjusted ORs of HU in Q3 (consuming 2.6–4.5 mcg dietary vitamin D daily), Q4 (consuming 4.6–7.6 mcg daily), and Q5 (consuming 7.7 mcg or greater) were 0.69 (95% CI, 0.58–0.83), 0.68 (95% CI, 0.57–0.82), and 0.57 (95% CI, 0.47–0.69), respectively, p for trend < 0.0001. In females, compared with Q1 (respondents consuming <0.9 mcg daily), the OR of HU was 0.81 (95% CI, 0.67–0.98) for Q4 (consuming 3.7–6.2 mcg dietary vitamin D daily), and p for trend was 0.0024.
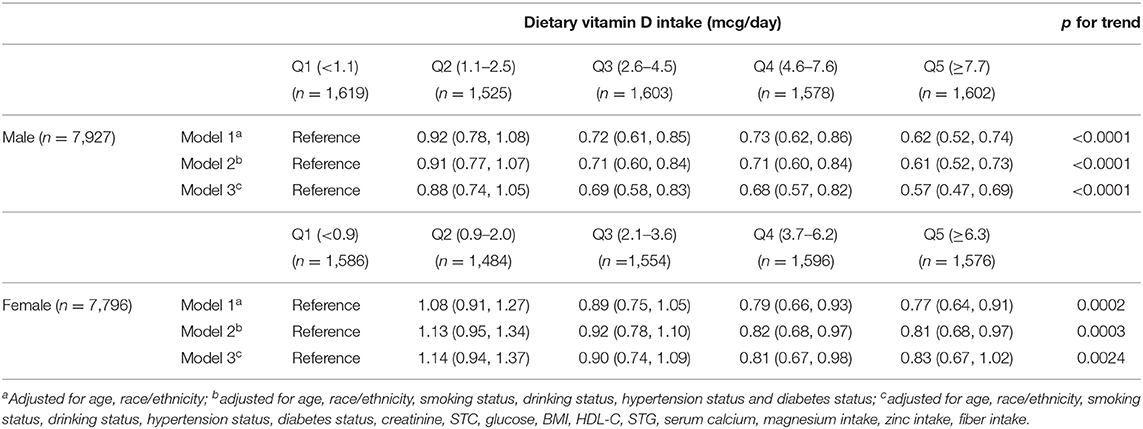
Table 4. Adjusted odds ratios of hyperuricemia among participants associated with dietary vitamin D intake.
Compared to Q1, adjusted ORs in Q2–Q5 of the total vitamin D intake were 0.83 (95% CI, 0.69–0.98), 0.69 (95% CI, 0.58–0.83), 0.66 (95% CI, 0.55–0.79), and 0.59 (95% CI, 0.48–0.71), respectively, with p for trend of < 0.0001 in males. In females, compared to Q1, the adjusted ORs of HU were 0.80 (95% CI, 0.65–0.98) for Q5 (those consuming 19.6 mcg or greater), and the p for trend was 0.0076. More detailed information is presented in Table 5.
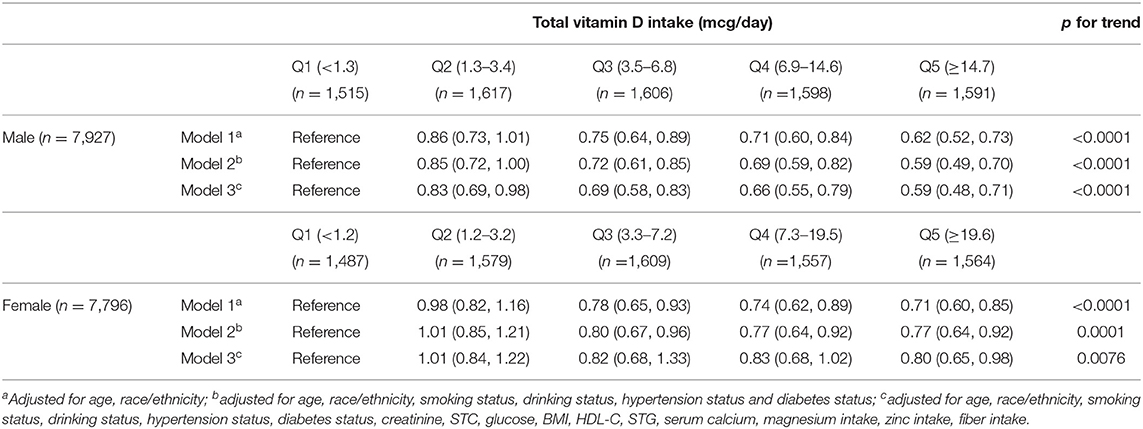
Table 5. Adjusted odds ratios of hyperuricemia among participants associated with total vitamin D intake.
In males, compared with the supplemental vitamin D non-user, the adjusted odds ratios (ORs) were 0.77 (95% CI, 0.65–0.92) among those consuming <15 mcg supplemental vitamin D daily, and the p for trend was 0.0268. Nevertheless, there was no significant relationship between supplemental vitamin D intake and HU in females, after adjusting for all confounding factors, as is shown in Table 6. All model fitness was assessed by a likelihood ratio test (p < 0.0001).
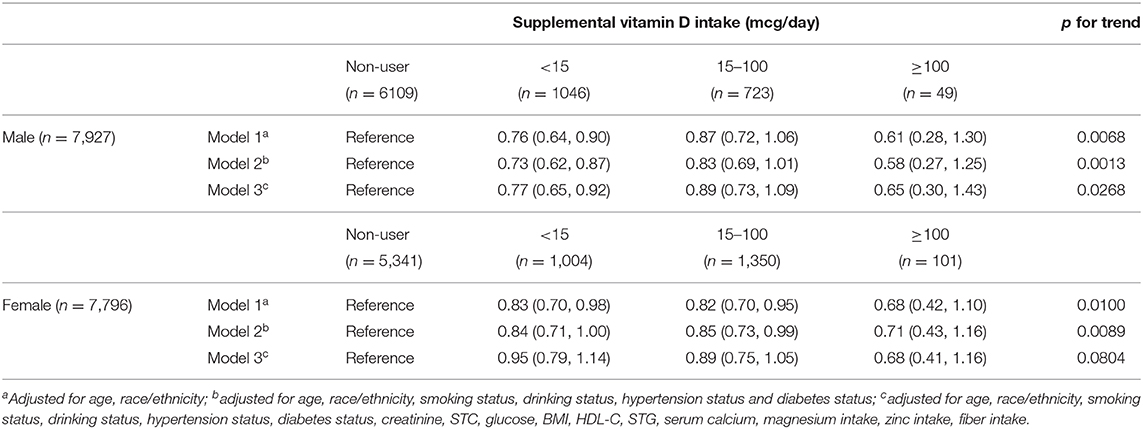
Table 6. Adjusted odds ratios of hyperuricemia among participants associated with supplemental vitamin D intake.
A sensitivity analysis was undertaken using the second 24-h dietary recall data from 2007 to 2014. Thirteen thousand nine hundred seventy eight adults (6,890 male and 7,088 female) were included in sensitivity analysis. We used the mean of the nutrient intake from the two dietary recalls and adjusted for the same covariates of the primary analyses. By and large, the relationships between the intake of dietary vitamin D, supplemental vitamin D, and total vitamin D with HU risk were not altered.
Discussion
In this large population-based study, a significant negative association between serum 25(OH) D (Q1 vs. Q2, Q4), dietary vitamin D intake (Q1 vs. Q3–Q5), supplemental vitamin D intake (non-user vs. <15 mcg/day), and total vitamin D intake (Q1 vs. Q2–Q5) with the risk of HU was found in men. We observed inverse associations between serum 25(OH) D (Q1 vs. Q3), dietary vitamin D intake (Q1 vs. Q4), and total vitamin D intake (Q1 vs. Q5) with HU in women among US adults.
To the best of our knowledge, this is the first study revealing the association of serum 25(OH) D, dietary vitamin D intake, supplemental vitamin D intake, and total vitamin D intake with HU in both male and female of US adults, and the largest population-based study using a nationally representative sample. Some studies have reported that serum 25(OH) D was associated with the metabolic syndrome (14, 15), and vitamin D insufficiency has been found in chronic kidney diseases (12, 27); therefore, we adjusted for metabolic risk factors such as STG, STC, HDL-C, glucose, BMI, hypertension status, and diabetes status and adjusted for creatinine considering renal dysfunction. The previous study has examined that magnesium intake significantly interacted with vitamin D status (28); we adjusted for magnesium intake and also adjusted for the intakes of zinc and fiber for other covariates including age, race/ethnicity, smoking status, drinking status, and serum calcium in multivariate logistic regression models. Coinciding with our results, a research among postmenopausal Chinese Han women found a significant association between the vitamin D insufficiency and elevated uric acid (29). Another similar study among elderly Egyptians found that the low level of vitamin D was significantly associated with high uric acid level (30). However, a study in France which enrolled 192 women ≥65 years revealed that the proportion of women with elevated serum uric acid level was significantly greater in those who received both calcium and vitamin D compared with those who received placebo (31). Major reasons for the inconsistent results can be explained due to the difference in age of the research participants and different countries. Our study also did not observe associations of the supplemental vitamin D intake with HU risk in females.
The Food and Nutrition Board (FNB) committee noted that serum levels of 50 nmol/L or more are sufficient for most people and serum concentrations >125 nmol/L can be associated with adverse effects. In our study, the adjusted OR was 0.78 among those serum 25(OH) D levels of 41.8–55.4 nmol/L, compared with respondents' serum levels <41.8 nmol/L for males, and OR was 0.80 among those serum 25(OH) D levels of 55.4–69.3 nmol/L, compared with respondents' serum levels <39.8 nmol/L for females. The recommended dietary allowance (RDA) for vitamin D was 15 mcg/day for US adults aged 19–70 years and 20 mcg/day for aged 70 years and above. In our results, the OR was 0.80 among those consuming more than 19.6 mcg vitamin D daily, compared with respondents consuming <1.2 mcg vitamin D daily for females. Our results suggested that adequate vitamin D may have a potential function for preventing or decreasing the risk of HU. The underlying mechanism for the association between vitamin D status and the risk of HU was not completely explained, and several hypotheses have been proposed. First, previous studies showed that serum 25-hydroxy vitamin D level insufficiency can activate parathyroid to induce the release of parathyroid hormone. Meanwhile, HU and gout have become more frequent in patients with hyperparathyroidism, and parathyroidectomy can reduce serum uric acid levels in these cases. Increased parathyroid hormone levels are thought to reduce uric acid excretion in the kidney. Furthermore, several studies showed a significant association between parathyroid hormone and serum uric acid levels. Previous clinical trials of 1,637 postmenopausal women found that parathyroid hormone increased the incidence of hyperuricemia in a dose-response fashion (18, 19), and serum uric acid levels decrease after cessation of treatment (19). A nationally representative population study among 8,316 participants, from the US and male and female, indicated that serum uric acid levels and the frequency of hyperuricemia increased with increasing parathyroid hormone levels (20). Therefore, serum 25-hydroxy vitamin D is likely inversely associated with elevated serum uric acid levels. Further studies are required to investigate the biological mechanism between vitamin D status and HU.
In addition, a systematic review found that moderate to high doses of vitamin D supplementation may reduce cardiovascular diseases (32), and it was reported that higher vitamin D intake is associated with lower cardiovascular disease risk in US males (10). Meanwhile, numerous studies have demonstrated that elevated serum uric acid level was a risk factor for cardiovascular diseases and independently associated with cardiovascular mortality (33–37). A large prospective long study of 83,683 Austrian males found that serum uric acid was independently related to mortality from cardiovascular disease, suggesting the clinical importance of monitoring and intervention based on serum uric acid, which was easily and routinely measured (37). Our results show significantly higher levels of STC, STG, and glucose and a lower level of HDL in patients with HU than those participants without HU. Previous studies show that serum uric acid levels were positively associated with triglycerides and systolic blood pressure and negatively associated with HDL cholesterol (38). Thus, it is necessary to clarify the effect of vitamin D supplementation on HU and consequently the effect of serum uric acid, lowering treatment on the prevention of cardiovascular diseases.
The main strengths of our study are as follows. Firstly, this is the first study that directly investigated the relationship between serum 25(OH) D intake, dietary vitamin D intake, supplemental vitamin D intake, total vitamin D intake, and the risk of HU in both male and female, based on a large (15,723 subjects) and nationally representative sample among US adults. Secondly, we adjusted for a considerable number of potential confounding variables. Thirdly, the use of trained staff to evaluate the main information of the research object and conduct interviews in accordance with a standardized program has improved the accuracy and effectiveness of the data. Nevertheless, our study has several limitations. Firstly, our study was a cross-sectional design study, which limited the definition of the causal correlational relationship between vitamin D status and HU; further prospective longitudinal studies would be important to support these conclusions. Secondly, although we adjusted several main covariates in the analysis, the associations reported may partially be due to the potential confusion by other unobserved variables and residual confounding. Thirdly, the data on sun exposure were not available. However, we used a direct measure of serum 25(OH) D, which reflected cumulative sun exposure and dietary vitamin D intake, and we also used the data of supplemental vitamin D intake. Finally, further future prospective studies and clinical trials are needed to investigate the underlying mechanisms of those associations.
Conclusions
Our findings indicated that the serum 25(OH) D, dietary vitamin D intake, supplemental vitamin D intake, and total vitamin D intake were inversely related to risk of HU in men. We observed a lower risk of HU with higher serum 25(OH) D, dietary vitamin D intake, and total vitamin D intake and no association between supplemental vitamin D intake and the risk of HU in women among US adults, independent of some major confounding factors.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Author Contributions
Y-YZ, H-BQ, and J-WT designed the study and wrote the manuscript. Y-YZ analyzed and interpreted the data. All authors read and approved the final manuscript.
Funding
This research was funded by the Natural Science Foundation of Heilongjiang Province of China (YQ2019H032); China Postdoctoral Science Foundation (2019M661308); Postdoctoral Science Foundation of Heilongjiang Province of China (LBH-Z19180); Foundation of Heilongjiang Educational Committee (UNPYSCT-2018113); and Doctoral Research Fund Project of Jiamusi University (JMSUBZ2019-08).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. Bardin T, Richette P. Definition of hyperuricemia and gouty conditions. Curr Opin Rheumatol. (2014) 26:186. doi: 10.1097/BOR.0000000000000028
2. Terkeltaub RA. Clinical practice. Gout. N Engl J Med. (2003) 349:1647–55. doi: 10.1056/NEJMcp030733
3. Molino-Lova R, Prisco D, Pasquini G, Vannetti F, Paperini A, Zipoli R, et al. Higher uric acid levels are associated with better functional recovery in elderly patients receiving cardiac rehabilitation. Nutr Metab Cardiovasc Dis. (2013) 23:1210–5. doi: 10.1016/j.numecd.2013.04.009
4. Keenan RT, Pillinger MH. Hyperuricemia, gout, and cardiovascular disease: an important “muddle”. Bull NYU Hosp Jt Dis. (2009) 67:285–90.
5. Borghi C, Rosei EA, Bardin T, Dawson J, Mancia G. Serum uric acid and the risk of cardiovascular and renal disease. J Hypertens. (2015) 33: 1729–41. doi: 10.1097/HJH.0000000000000701
6. Sluijs I, Beulens JWJ, Van dA DL, Spijkerman AMW, Schulze MB, Van dS YT. Plasma uric acid is associated with increased risk of type 2 diabetes independent of diet and metabolic risk factors. J Nutr. (2012) 143:80–5. doi: 10.3945/jn.112.167221
7. Zhu Y, Pandya BJ, Choi HK. Prevalence of gout and hyperuricemia in the US general population: the national health and nutrition examination survey 2007–2008. Arthritis Rheumatol. (2011) 63:3136–41. doi: 10.1002/art.30520
8. Liu B, Wang T, Zhao HN, Yue WW, Yu HP, Liu CX, et al. The prevalence of hyperuricemia in China: a meta-analysis. BMC Public Health. (2011)11:1–10. doi: 10.1186/1471-2458-11-832
9. Institute of Medicine Food and Nutrition Board. Dietary Reference Intakes for Calcium and Vitamin D. Washington, DC: National Academy Press (2010).
10. Sun Q, Shi L, Rimm EB, Giovannucci EL, Hu FB, Manson JE, et al. Vitamin D intake and risk of cardiovascular disease in US men and women. Am J Clin Nutr. (2011) 94:534–42. doi: 10.3945/ajcn.110.008763
11. Leu M, Giovannucci E. Vitamin D: epidemiology of cardiovascular risks and events. Best Pract Res Clin Endocrinol Metab. (2011) 25:633–46. doi: 10.1016/j.beem.2011.04.001
12. Li YC. Vitamin D: roles in renal and cardiovascular protection. Curr Opin Nephrol Hypertens. (2012) 21:72–9. doi: 10.1097/MNH.0b013e32834de4ee
13. Rouached M, El Kadiri Boutchich S, Al Rifai AM, Garabédian M, Fournier A. Prevalence of abnormal serum vitamin D, PTH, calcium, and phosphorus in patients with chronic kidney disease: results of the study to evaluate early kidney disease. Kidney Int. (2008) 74:389–90. doi: 10.1038/ki.2008.169
14. Chowdhury TA, Boucher BJ, Hitman GA. Vitamin D and type 2 diabetes: is there a link? Prim Care Diabetes. (2009) 3:115–6. doi: 10.1016/j.pcd.2009.03.004
15. Lu L, Yu Z, Pan A, Hu FB, Franco OH, Li H, et al. Plasma 25-hydroxyvitamin D concentration and metabolic syndrome among middle-aged and elderly Chinese individuals. Diabetes Care. (2009) 32:1278–83. doi: 10.2337/dc09-0209
16. Emilion E, Emilion R. Estimation of the 25(OH) Vitamin D threshold below which secondary hyperparathyroidism may occur among African Migrant Women in Paris. Int J Vitam Nutr Res. (2011) 81:218–24. doi: 10.1024/0300-9831/a000073
17. Dalbeth N, Horne A, Gamble GD, Ames R, Reid IR. The effect of calcium supplementation on serum urate: analysis of a randomized controlled trial. Rheumatology. (2009) 48:195–7. doi: 10.1093/rheumatology/ken416
18. Miller PD, Schwartz EN, Chen P, Misurski DA, Krege JH. Teriparatide in postmenopausal women with osteoporosis and mild or moderate renal impairment. Osteoporos Int. (2007) 18:59–68. doi: 10.1007/s00198-006-0189-8
19. Neer RM, Arnaud CD, Zanchetta JR, Prince R, Gaich GA, Reginster JY, et al. Effect of parathyroid hormone (1-34) on fractures and bone mineral density in postmenopausal women with osteoporosis. N Engl J Med. (2001) 344:1434–41. doi: 10.3171/foc.2001.11.2.8
20. Hui JY, Choi JW, Mount DB, Zhu Y, Zhang Y, Choi HK. The independent association between parathyroid hormone levels and hyperuricemia: a national population study. Arthritis Res Ther. (2012) 14:R56. doi: 10.1186/ar3769
21. National Health and Nutrition Examination Survey Data. Centers for Disease Control and Prevention (CDC). Available online at: http://www.cdc.gov/NCHS/nhanes.htm (accessed August 30, 2017).
22. National Center for Health Statistics Centers for Disease Control and Prevention. Plan and Operation of the Third National Health and Nutrition Examination Survey (NHANES III, 1988-94): Reference Manuals and Reports: Weighting and Estimation Methodology Report. Hyattsville, MD: US Dept of Health & Human Services, Public Health Service, Centers for Disease Control & Prevention (1998).
23. National Health and Nutrition Examination Survey: questionnaires datasets and related documentation. National Center for Health Statistics. Available online at: http://www.cdc.gov/nchs/nhanes/nhanes_questionnaires.htm (accessed June 7, 2017).
24. NCHS Research Ethics Review Board (ERB) Approval. Centers for Disease Control and Prevention (CDC). Available online at: https://www.cdc.gov/nchs/nhanes/irba98.htm (accessed June 7, 2017).
25. Bomback AS, Derebail VK, Shoham DA, Anderson CA, Steffen LM, Rosamond WD, et al. Sugar-sweetened soda consumption, hyperuricemia, and kidney disease. Kidney Int. (2010) 77:609–16. doi: 10.1038/ki.2009.500
26. Centers for Disease Control and Prevention: The National Health and Nutrition Examination Survey Laboratory Procedure Manual Serum 25-Hydroxyvitamin D Diasorin (formerly Incstar) 25-OH-D assay. Atlanta, GA: CDC (2008).
27. Levin A, Bakris GL, Molitch M, Smulders M, Tian J, Williams LA, et al. Prevalence of abnormal serum vitamin D, PTH, calcium, and phosphorus in patients with chronic kidney disease: results of the study to evaluate early kidney disease. Kidney Int. (2007) 71:31–8. doi: 10.1038/sj.ki.5002009
28. Deng X, Song Y, Manson JE, Signorello LB, Zhang SM, Shrubsole MJ, et al. Magnesium, vitamin D status and mortality: results from US National Health and Nutrition Examination Survey (NHANES) 2001 to 2006 and NHANES III. BMC Med. (2013) 11:187. doi: 10.1186/1741-7015-11-187
29. Peng H, Li H, Li C, Chao X, Zhang Q, Zhang Y. Association between vitamin D insufficiency and elevated serum uric acid among middle-aged and elderly Chinese Han Women. PLoS ONE. (2013) 8:e61159. doi: 10.1371/journal.pone.0061159
30. Abokhosheim K, Mohamed M, Bedewy R. MARSLAND PRESS multidisciplinary academic journal publisher relation between serum uric acid and vitamin D among Elderly Egyptians. J Am Sci. (2013) 12:984.
31. Brazier M, Grados F, Kamel S, Mathieu M, Morel A, Maamer M, et al. Clinical and laboratory safety of one year's use of a combination calcium + vitamin D tablet in ambulatory elderly women with vitamin D insufficiency: results of a multicenter, randomized, double-blind, placebo-controlled study. Clin Ther. (2005) 27:1885–93. doi: 10.1016/j.clinthera.2005.12.010
32. Wang L, Manson JE, Song Y, Sesso HD. Systematic review: vitamin D and calcium supplementation in prevention of cardiovascular events. Ann Intern Med. (2010) 152:315–23. doi: 10.7326/0003-4819-152-5-201003020-00010
33. Fang J, Alderman MH. Serum uric acid and cardiovascular mortality the NHANES I epidemiologic follow-up study, 1971–1992. National Health and Nutrition Examination Survey. JAMA. (2000) 283:2404–10. doi: 10.1001/jama.283.18.2404
34. Verdecchia P, Schillaci G, Reboldi G, Santeusanio F, Porcellati C, Brunetti P. Relation between serum uric acid and risk of cardiovascular disease in essential hypertension. The PIUMA study. Hypertension. (2000) 36:1072–8. doi: 10.1161/01.HYP.36.6.1072
35. Baker JF, Krishnan E, Chen L, Schumacher HR. Serum uric acid and cardiovascular disease: recent developments, and where do they leave us? Am J Med. (2005) 118:816–26. doi: 10.1016/j.amjmed.2005.03.043
36. Mazza A, Pessina AC, Pavei A, Scarpa R, Tikhonoff V, Casiglia E. Predictors of stroke mortality in elderly people from the general population. The CArdiovascular STudy in the ELderly. Eur J Epidemiol. (2001) 17:1097–104. doi: 10.1023/A:1021216713504
37. Strasak A, Ruttmann E, Brant L, Kelleher C, Klenk J, Concin H, et al. Serum uric acid and risk of cardiovascular mortality: a prospective long-term study of 83,683 Austrian men. Clin Chem. (2008) 54:273–84. doi: 10.1373/clinchem.2007.094425
Keywords: hyperuricemia, vitamin D, cardiovascular disease, NHANES, cross-sectional study
Citation: Zhang Y-Y, Qiu H-B and Tian J-W (2020) Association Between Vitamin D and Hyperuricemia Among Adults in the United States. Front. Nutr. 7:592777. doi: 10.3389/fnut.2020.592777
Received: 10 August 2020; Accepted: 20 October 2020;
Published: 20 November 2020.
Edited by:
Marcelo Perim Baldo, Unimontes, BrazilReviewed by:
Divanei Zaniqueli, Federal University of Espirito Santo, BrazilVenkata Saroja Voruganti, University of North Carolina at Chapel Hill, United States
Copyright © 2020 Zhang, Qiu and Tian. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jin-Wei Tian, dGlhbmppbndlaWRyMjAwOUAxNjMuY29t
†These authors have contributed equally to this work
 Yi-Ying Zhang
Yi-Ying Zhang Hong-Bin Qiu3†
Hong-Bin Qiu3† Jin-Wei Tian
Jin-Wei Tian