- 1Clinical Ergospirometry, Exercise and Rehabilitation Laboratory, 1st Critical Care Department, Evangelismos Hospital, School of Medicine, National and Kapodistrian University of Athens, Athens, Greece
- 2Department of Film Studies, Aristotle University of Thessaloniki, Thessaloniki, Greece
- 3Virtual Reality Applications (ViRA), Athens, Greece
Background: Over the past few years, technological innovations have been increasingly employed to augment the rehabilitation of stroke patients. Virtual reality (VR) has gained attention through its ability to deliver a customized training session and to increase patients’ engagement. Virtual reality rehabilitation programs allow the patient to perform a therapeutic program tailored to his/her needs while interacting with a computer-simulated environment.
Purpose: This study aims to investigate the effectiveness of a fully immersive rehabilitation program using a commercially available head-mounted display in stroke patients.
Methods: A systematic search was conducted in three databases, namely, PubMed, Google Scholar, and PEDro. Four hundred thirty-two references were identified. The keywords used for the literature search were in English, which are given as follows: immersive, virtual reality, neurorehabilitation, stroke, and head-mounted display. Additionally, applicable articles were identified through screening reference lists of relevant articles.
Results: Only 12 studies used head-mounted display for immersing the patient into the virtual world. Apart from the feasibility of this new technology, a range of benefits were identified, especially in terms of functional ability as measured by FIM or Barthel, the Action Research arm Test, Box and Block Test, Fugl-Meyer assessment of physical performance, strength, and balance outcomes.
Conclusion: The results from this review support the potential beneficial effect of fully immersive virtual reality in the rehabilitation of stroke patients, maximizing recovery through increased motivation and adherence.
Introduction
Stroke is a neurological disease that has been described as a leading cause of disability with substantial economic cost for rehabilitation (Gbd 2016 Stroke Collaborators, 2019). Stroke survivors face a wide range of disabilities from cognition to paresis that led to reduced functional ability and quite often to loss of independence. Functional decline is apparent even 5 years post-stroke, leading to long-term deficits, especially regarding activities of daily living (Dhamoon et al., 2009).
There is high-quality evidence that supports the use of rehabilitation intervention to improve physical functioning even in severe stroke survivors (McGlinchey et al., 2020). Different rehabilitation techniques have been used to accelerate recovery. All of them have induced substantial beneficial effects. Technological innovations have offered severe advantages in facing the complicity of stroke rehabilitation. Virtual reality (VR) interventions have been used the past few years as a therapeutic means to improve physical recovery through enhancing neuronal plasticity and relearning movement patterns and motor skills (Raffin and Hummel, 2018). Additionally, the gamification of rehabilitation has increased motivation and adherence, both of which are key aspects of a successful recovery (Dias et al., 2019). It is believed that VR has the means to incorporate key elements in the rehabilitation program such as motor-cognitive training, different neuroscience principles, motivational game themes, and empowerment techniques and advance the whole process of recovery (Perez-Marcos et al., 2018). Immersion is a vital component of the whole experience and is a key component to the feeling of presence. Although full immersion in the virtual environment enhances the experience and strengthens the engagement of the patient, it seems to face certain challenges regarding the inclusion of haptic devices (Rose et al., 2018). The term “virtual reality” has been excessively used, but often describes different systems from display monitors to head-mounted displays (HMD). In a recent study, Huygelier et al. (2021) tried to underline the differences between mixed reality systems and virtual reality, in an effort to distinguish to what extent virtual information and real information are mixed. The term “fully immersive” environment presupposes stereoscopic vision and the complete disconnection of the user from his physical environment. Another term frequently used under the umbrella of VR is that of augmented reality. In this study, virtual information is superimposed over the real world. Different terminologies could create further confusion in relation to the degree of immersion being achieved, yet this could be overcome by looking into the input devices being used. It is well noted by Huygelier et al. (2021) that it is important to start using a consistent terminology regarding VR technologies as there is a continuous evolution in the field. Systematic reviews that have been published examining the effectiveness of virtual reality have included both fully and semi-immersive studies, in which different types of visualization devices have been used such as PC (desktop VR) and TV monitor. Over the past decades, technological innovation has included from commercial gaming systems to custom-made specific VR (Huygelier et al., 2021).
The objective of this systematic review was to investigate the effectiveness of a fully immersive VR rehabilitation program using a head-mounted display on upper limb function, gait, and balance in stroke patients.
Methods
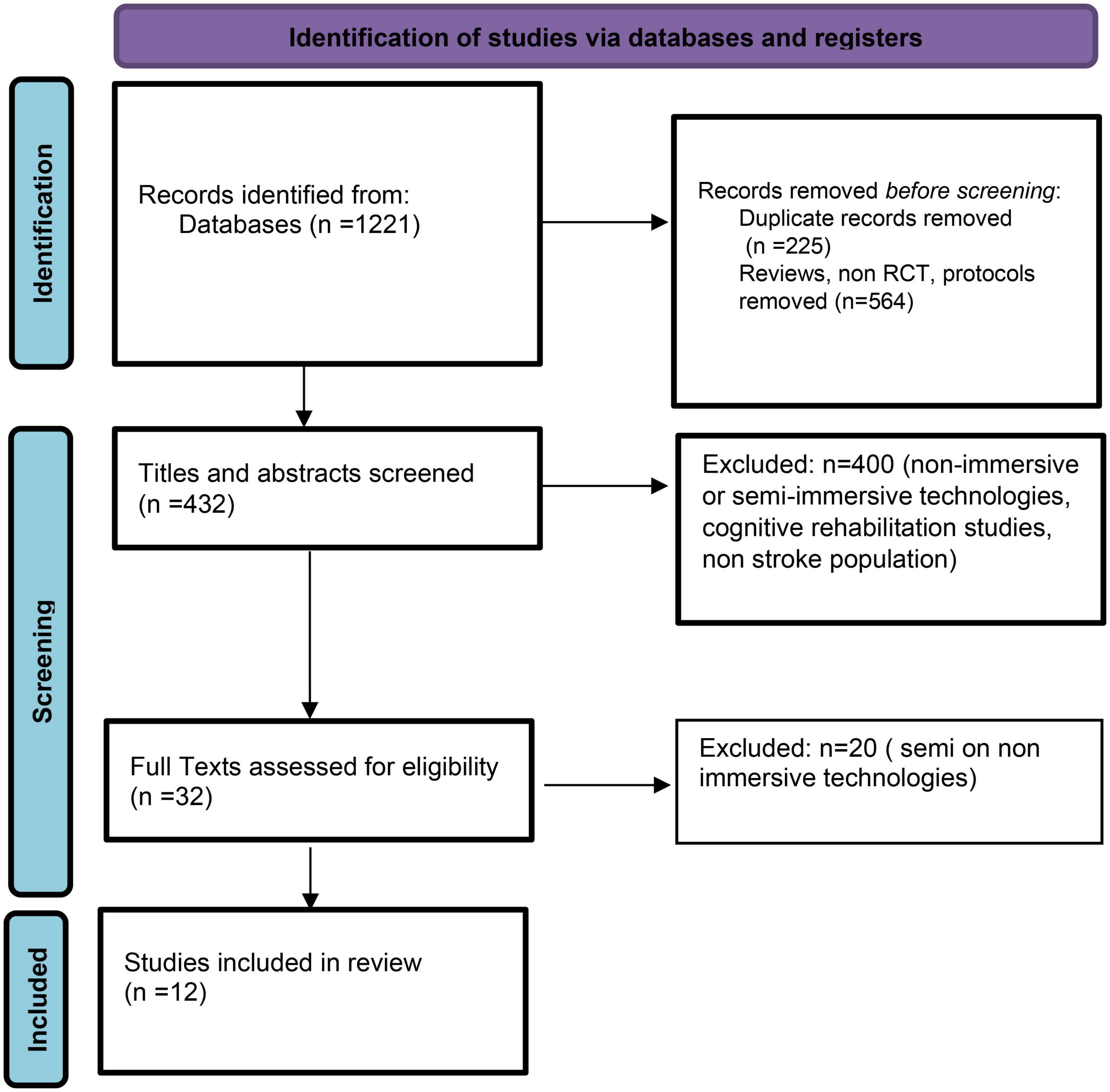
The current review was conducted following the preferred reporting items for systematic reviews and meta-analyses (PRISMA) statement. The protocol was not registered.
Searching strategy
The electronic databases of PubMed, PEDro, and Google Scholar were systematically searched for studies published till January 2021. Additionally, we thoroughly examined the reference lists from the studies included to identify further relevant studies. The keywords used for this systematic review were “virtual reality,” “immersive,” “stroke,” “rehabilitation,” “Recovery,” “Oculus,” and “Head Mounted Display,” These were used with certain combinations such as [(immersive virtual reality) OR (Head Mounted Display)] AND [(stroke rehabilitation) OR (stroke recovery)]. The search was performed by two of the authors who additionally screened the titles and the abstracts for inclusion.
Eligibility criteria and study selection
Only randomized control studies with fully immersive VR technologies (head-mounted display) that were published in English in peer-reviewed journals and measured rehabilitation in physical functions (muscle strength, activities of daily living, functional ability, gait parameters, and balance) after stroke were included. The studies with psychiatric disorders and those that assessed only cognitive outcomes were excluded. Studies that provided only neurocognitive rehabilitation were also excluded.
Methodological quality
The quality of the included studies was evaluated by the Physiotherapy Evidence Database (PEDro) Scale. Total scores from 6 to 10 were considered high quality, 4 to 5 were considered fair quality, and ≤3 were considered poor quality. Two authors conducted a blinded rating of the methodological quality of the studies. Different rates and unclear issues were discussed.
Results
Selection of studies
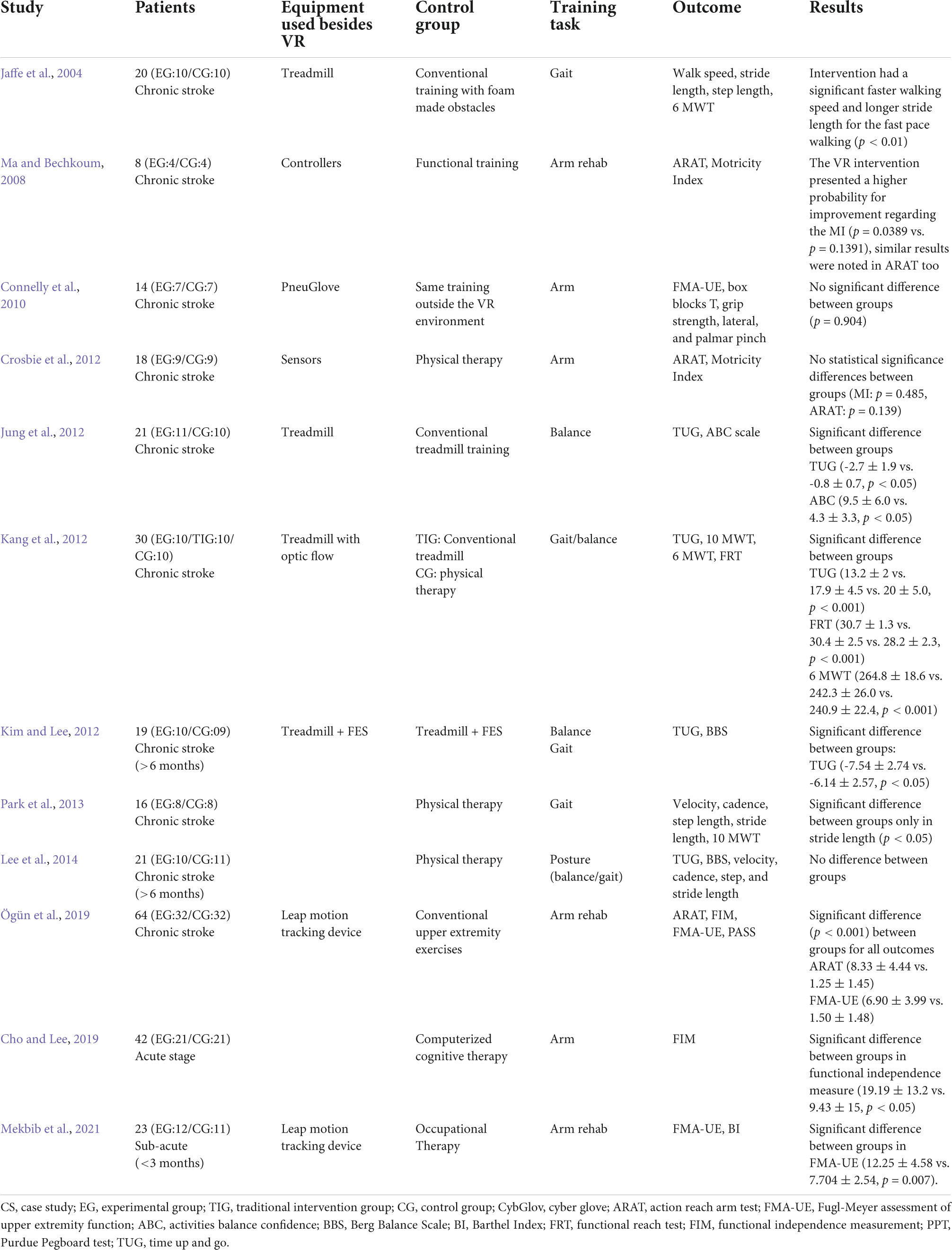
From the initial search, 1,221 articles were identified. Non-RCT, cases of series, protocols, and duplicates were excluded. Four hundred thirty-two articles were remained to be investigated regarding the type of immersion used. After screening the titles, the abstracts and in a few cases the whole article for eligibility criteria, 12 studies (Table 1) were selected to be included in this systematic review. The selection process is summarized according to PRISMA guidelines as a flowchart (Figure 1).
Methodological quality
All studies included were assessed for methodological quality using the PEDro Scale (Table 2). Five studies (Crosbie et al., 2012; Kang et al., 2012; Lee et al., 2014; Ögün et al., 2019; Mekbib et al., 2021) were considered “high quality” and seven studies (Jaffe et al., 2004; Ma and Bechkoum, 2008; Connelly et al., 2010; Jung et al., 2012; Kim and Lee, 2012; Park et al., 2013; Cho and Lee, 2019) were considered “moderate quality.” The mean score of the methodological quality for the included studies was 5.67.
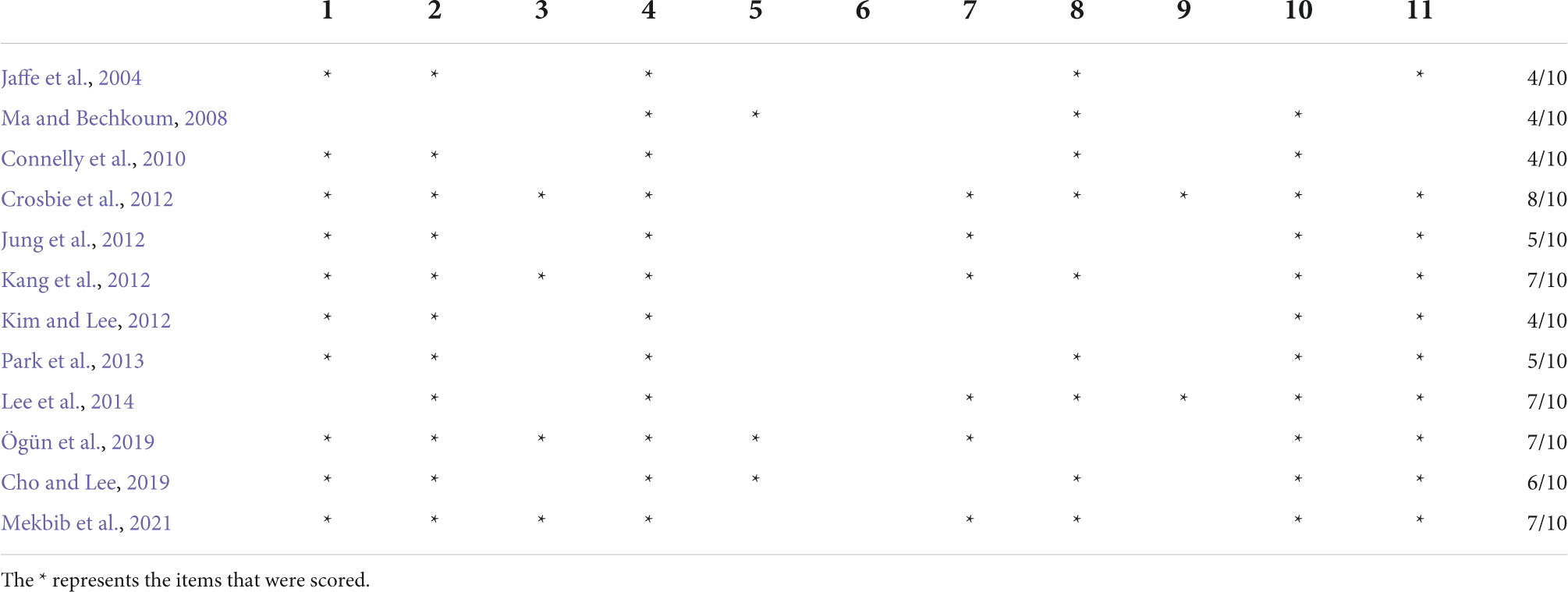
Table 2. Quality of the RCT studies of stroke patients on PEDro Scale (item 1 does not contribute to total score).
Type of virtual environment and gamification scenarios
Full immersion of the patient in the training environment was achieved through a head-mounted display (HMD). This equipment displays the virtual environment and completely isolates patients from the surrounding environment, providing a better sense of presence (Radianti et al., 2020). Additionally, a series of input devices such as a real-time motion tracking devices were used offering a more augmented environment or different kinds of magnets were used to track motion (Ma and Bechkoum, 2008; Connelly et al., 2010). In recent years, devices such as the leap motion have been introduced to provide a sense of crabbing an object without employing a different device to track the motion (Ögün et al., 2019; Mekbib et al., 2021). In terms of upper limb rehabilitation, different special gloves (Connelly et al., 2010; Crosbie et al., 2012) were used to facilitate training, while in terms of gait, a treadmill (Jung et al., 2012; Kang et al., 2012; Kim and Lee, 2012) was often used. It is well-established that all studies offer a different degree of intrinsic feedback, with all having visual and auditory and some somatosensory ones. Extrinsic feedback, in the form of grading one’s performance, was an important feature that facilitates the objective progression of the task while keeping the patient motivated and interested. Progression often had to do with increasing walking distance or the distance from the handling object or even decreasing the time needed to perform the task.
The studies included in the review made a significant effort to enhance motor learning principles as seen in more conventional rehabilitation strategies. In most of the studies, information regarding progression, use of different tasks, and task specificity are well-described. Task variations regarding balance and gait rehabilitation involved obstacle negotiation (Jaffe et al., 2004) and treadmill training (Connelly et al., 2010; Jung et al., 2012; Kang et al., 2012). Through the HMD, the patients experienced a normal view next to their own while walking in a simulated park or street. This visual feedback acted as a continuous stimulus to correct one’s movement. All subjects who used a treadmill wore a suspension device for safety purposes. Treadmill with the optic flow program (Kang et al., 2012) employed computer hardware for the output and was applied to the HMD. Speed, controlled through the optic flow, was continuously increased. Jaffe et al. used a park simulation presented through the HMD device. Upper extremity rehabilitation included picking up, reaching, moving different objects, and dual-task training. Different scenarios were used such as: decorating a tree with leaves and fruits or picking up vegetables from a bowl and putting them back (Ögün et al., 2019), a drumming game (Ögün et al., 2019), catching fruits that fall off a tree with a basket (Ma and Bechkoum, 2008), fishing games, or hitting mice with a virtual hammer (Ma and Bechkoum, 2008; Crosbie et al., 2012).
Upper limb functionality
Five studies aimed to assess the effectiveness of a fully immersive program on arm’s functional recovery. It was noted that three studies (Ma and Bechkoum, 2008; Ögün et al., 2019; Mekbib et al., 2021) pointed out the significant difference between groups in favor of the VR program. While the other two (Connelly et al., 2010; Crosbie et al., 2012) didn’t reach statistical significance, they pointed out that the VR intervention was more effective. Muscle strength was assessed only in two studies (Connelly et al., 2010; Kim and Lee, 2012). In terms of upper limb rehabilitation, it was demonstrated a significant improvement over time in the palmar pinch, which is used in all daily activities that include picking up and releasing objects. In this study, the use of a pneumo-glove was essential for this measurement. In terms of gait rehabilitation, Kim and Lee (2012) reported a significant change in the tibialis anterior and quadriceps femoris muscles of the affected side when VR was used along with functional electrical stimulation.
The instruments that were mostly used were the Fugl-Meyer Upper Extremity (FM-UE) function (Connelly et al., 2010; Ögün et al., 2019; Mekbib et al., 2021) and the Action Reach Arm Test (ARAT) (Ma and Bechkoum, 2008; Crosbie et al., 2012; Ögün et al., 2019). Additionally, the Motricity Index (Ma and Bechkoum, 2008; Crosbie et al., 2012); the Box Block Test (Connelly et al., 2010); and muscle strength by measuring grip strength, lateral pinch, and palmar pinch strength (Connelly et al., 2010) were used.
Functional ability
Three studies (Ögün et al., 2019; Mekbib et al., 2021; Cho and Lee, 2019) examined the improvement of functional ability and used the functional independence measurement (FIM), Barthel Index (BI), and performance assessment of self-care skills (PASS). All instruments have been developed to assess an individual’s independence in performing activities of daily living. All studies found statistically significant improvement of the VR intervention in relation to the control.
Balance-gait
Balance was examined in four studies by the Time-Up and Go Test (TUG) (Jung et al., 2012; Kim and Lee, 2012; Park et al., 2013; Lee et al., 2014). The test was significantly improved in three of the studies (Jung et al., 2012; Kang et al., 2012; Kim and Lee, 2012), while in only one study (Lee et al., 2014), the intervention group showed better results without reaching statistical significance. Berg Balance Scale (BBS) was also used in two studies (Kim and Lee, 2012; Kim and Lee, 2012) with improvement in the intervention group although present not being able to reach statistical significance again.
Gait (Jaffe et al., 2004; Kang et al., 2012; Park et al., 2013; Lee et al., 2014) was assessed by numerous parameters such as velocity, cadence, step length, and stride length. Endurance was examined either by 6 MWT (Jaffe et al., 2004; Kang et al., 2012) or by 10 MWT (Kang et al., 2012; Lee et al., 2014). Patients demonstrated clinically meaningful changes in the gait parameters in all training groups, and in some of them, there was a statistically significant difference in favor of the experimental group.
Safety side effects
Only two studies examined the appearance of any side effects from the immersion into virtual reality (Jaffe et al., 2004; Crosbie et al., 2012). Jaffe et al. (2004) reported no incidence of falling due to the dynamic nature of the exercise, and Crosbie et al. (2012) mentioned only the appearance of dizziness in two patients.
Discussion
The purpose of this systematic review was to assess the effectiveness of a fully immersive virtual reality rehabilitation program using a head-mounted display on upper limb function, gait, and balance in stroke patients. As we were interested in the physical interaction of the user within the digital environments, and to assess its effectiveness, the focus on fully immersive technologies was most appropriate. Thus, in this systematic review, we included only fully immersive studies. Although we noted a variety regarding the haptic devices used in studies that aimed at arm’s functional rehabilitation and the duration of the programs in general, the results suggested a positive impact of the immersive VR applications on upper extremity function, gait, and balance in stroke patients. Even in more dynamic activities such as walking, VR interventions were safely delivered with positive effects on velocity and step-stride length. Jaffe et al. (2004) stated that patients did not mention any dizziness even one that suffered claustrophobia episodes at home. Thus, VR interventions could also involve both dynamic and stationary activities. When VR was used in upper limb rehabilitation, only two patients reported dizziness and headache (Crosbie et al., 2012). The presence of cybersickness often concerns investigators when using fully immersive technologies. Yet, it has been found, not only for stroke patients but also for older adults, that immersion causes minimal cybersickness (Despoti et al., 2022) and led to a positive attitude toward this intervention (Huygelier et al., 2019; Specht et al., 2021).
In the study by Jaffe et al. (2004), patients had to step over obstacles either real ones for the control group or virtually displayed for the experimental group. Although both groups improved, the VR group demonstrated a greater improvement during fast speed walking, as a gait variable. This could probably be the result of the constant exercise offered by the treadmill and the HMD in contrast to the specific hallway in the control group. The better performance could be also attributed to the different stimuli (auditory and visual) offered by the immersive VR environment. It should be noted that the patients in the VR group had even the ability of a lateral view of their legs. The same positive results were seen when the optic flow was used (Kang et al., 2012). Being able to offer different stimuli by altering the optic flow delivered in the immersive environment can increase neural action, especially in motion-sensitive cortical areas (Rutschmann et al., 2000). A recent case study further assessed the use of evolved augmented reality with the use of an optical see-through head-mounted display (OST-HMD). This provided a wider field of view (43 × 29 degrees) compared to other devices and thus could display more virtual objects in a real-world environment such as real-life obstacles and barriers (like blocks and floor mats) that were used in this specific study (Held et al., 2020). Positive results encourage further investigation of the beneficial effect of such devices in the gait rehabilitation of stroke patients.
It is worth mentioning that although a few studies didn’t demonstrate significant differences between groups in the outcomes assessed, the virtual reality intervention group was able to show a significant difference over time. In the study by Crosbie et al. (2012), although the intervention group didn’t present a significant improvement in Motricity Index for upper limb motor function, it did manage to maintain it at follow-up, whereas the control decreased it to baseline.
The gamification of VR rehabilitation interventions is believed to motivate patients to actively participate with pleasure thus increasing the tasks performed and augmenting their recovery. When participants are more interested, they are more concentrated and more persistent in completing their tasks. Certain benefits in psychological outcomes should always be acknowledged as a positive component, especially in neurological patients who often are faced with a long recovery (Qian et al., 2020). Our results are in agreement with those of previous systematic reviews or narrative ones that have examined semi-immersive VR interventions (Yates et al., 2016; Porras et al., 2018; Rutkowski et al., 2020) and with a scoping review that assessed the application of HMD in adult physical rehabilitation (Saldana et al., 2020). The authors did state that the use of HMD as a low-cost, portable tool seems to have additional benefits, but the generalization of the findings is yet to be discussed due to the relatively low level of evidence and the small number of participants (Saldana et al., 2020). Another key aspect noted also by Porras et al. (2018) is the additional benefits of incorporating VR in conventional rehabilitation, such as motivation and engagement.
A few limitations should be noted. One of them is that the population included in most of the studies was small ranging from 8 to 65 stroke patients. Furthermore, patients were included not only immediately after the incidence of the stroke but even being at a more chronic state without determining the exact time that has passed. Time is a key component in the functional rehabilitation of stroke patients as improvements are diminished after a few months. Another important information that is not being shared in most of the studies is the type of stroke: an ischemic or hemorrhagic one. Often, patients from both types were included.
The VR is a continuously developing technology that could offer additional stimulus to traditional rehabilitation strategies augmenting the whole process. As benefits were seen both in upper and lower rehabilitation, the combination should be considered in future studies. Additionally, future studies should be aimed at exploring the use of such technologies in a clinical environment and possibly incorporating both physical and cognitive interventions. Rehabilitation also needs to target sensory deficits, and recent studies have suggested VR’s potential to improve the sensory area. Whether employing sensory and physical tasks in a combined way during VR rehabilitation to further benefit physical components remains to be decided (Tinga et al., 2016).
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
IP carried out the literature search, summarized the results, wrote the manuscript, and prepared the tables and figures. ND and EK interpreted the results and supervised the process. AD and DT carried out the literature research and appraised the articles. NL, GR, and AP interpreted the results and prepared the tables. SN appraised the articles and supervised the process. All authors contributed to the article and approved the submitted version.
Funding
This research was co-funded by the “Research-Create-Innovate” program, ESPA 2014-2020, and the European Union.
Conflict of interest
Author AP was employed by Virtual Reality Applications.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Cho, D. R., and Lee, S. H. (2019). Effects of virtual reality immersive training with computerized cognitive training on cognitive function and activities of daily living performance in patients with acute stage stroke: A preliminary randomized controlled trial. Medicine 98:e14752. doi: 10.1097/MD.0000000000014752
Connelly, L., Jia, Y., Toro, M. L., Stoykov, M. E., Kenyon, R. V., and Kamper, D. G. (2010). A pneumatic glove and immersive virtual reality environment for hand rehabilitative training after stroke. IEEE Trans. Neural. Syst. Rehabil. Eng. 18, 551–559. doi: 10.1109/TNSRE.2010.2047588
Crosbie, J. H., Lennon, S., McGoldrick, M. C., McNeill, M. D., and McDonough, S. M. (2012). Virtual reality in the rehabilitation of the arm after hemiplegic stroke: a randomized controlled pilot study. Clin. Rehabil. 26, 798–806. doi: 10.1177/0269215511434575
Despoti, A., Karatzanos, E., Patsaki, I., Tzoumi, D., Roussou, G., Leventakis, N., et al. (2022). Immersive virtual reality in cognitive rehabilitation: A systematic review. Health Res. J. 8, 225–241. doi: 10.12681/healthresj.28872
Dhamoon, M. S., Moon, Y. P., Paik, M. C., Boden-Albala, B., Rundek, T., Sacco, R. L., et al. (2009). Long-term functional recovery after first ischemic stroke: the Northern Manhattan Study. Stroke 40, 2805–2811. doi: 10.1161/STROKEAHA.109.549576
Dias, P., Silva, R., Amorim, P., Lains, J., Roque, E., Pereira, I. S. F., et al. (2019). Using Virtual reality to increase motivation in poststroke rehabilitation. IEEE Comput. Graph. Appl. 39, 64–70. doi: 10.1109/MCG.2018.2875630
Gbd 2016 Stroke Collaborators. (2019). Global, regional, and national burden of stroke, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 18, 439–458.
Held, J. P. O., Yu, K., Pyles, C., Veerbeek, J. M., Bork, F., Heining, S.M., et al. (2020). Augmented reality-based rehabilitation of gait impairments: Case report. JMIR Mhealth. Uhealth. 8:e17804. doi: 10.2196/17804
Huygelier, H., Mattheus, E., Vanden Abeele, V., van Ee, R., and Gillebert, C. R. (2021). The Use of the Term Virtual Reality in Post-Stroke Rehabilitation: A Scoping Review and Commentary. Psychol. Belgica 61, 145–162. doi: 10.5334/pb.1033
Huygelier, H., Schraepen, B., van Ee, R. I, Vanden Abeele, V., and Gillebert, C. R. (2019). Acceptance of immersive headmounted virtual reality in older adults. Sci. Rep. 9:4619. doi: 10.1038/s41598-019-41200-6
Jaffe, D. L., Brown, D. A., Pierson-Carey, C. D., Buckley, E. L., and Lew, H. L. (2004). Stepping over obstacles to improve walking in individuals with poststroke hemiplegia. J. Rehabil. Res. Dev. 41, 283–292. doi: 10.1682/jrrd.2004.03.0283
Jung, J., Yu, J., and Kang, H. (2012). Effects of virtual reality treadmill training on balance and balance self efficacy in stroke patients with a history of falling. J. Phys. Ther. Sci. 24, 1133–1136. doi: 10.1589/jpts.24.1133
Kang, H. K., Kim, Y., Chung, Y., and Hwang, S. (2012). Effects of treadmill training with optic flow on balance and gait in individuals following stroke: randomized controlled trials. Clin. Rehabil. 26, 246–255. doi: 10.1177/0269215511419383
Kim, I. C., and Lee, B. H. (2012). Effects of augmented reality with functional electric stimulation on muscle strength, balance and gait of stroke patients. J. Phys. Ther. Sci. 24, 755–762.
Lee, C. H., Kim, Y., and Lee, B. H. (2014). Augmented reality based-postural control training improves gait function in patients with stroke: Randomized controlled trial. Hong Kong Physiothera. J. 32, 51–57. doi: 10.1016/j.hkpj.2014.04.002
Ma, M., and Bechkoum, K. (2008). “Serious games for movement therapy after stroke,” in Proceedings of the IEEE International Conference on Systems, Man and Cybernetics, Melbourne, 1872–1877.
McGlinchey, M. P., James, J., McKevitt, C., Douiri, A., and Sackley, C. (2020). The effect of rehabilitation interventions on physical function and immobility-related complications in severe stroke: a systematic review. BMJ Open 10:e033642. doi: 10.1136/bmjopen-2019-033642
Mekbib, D. B., Debeli, D. K., Zhang, L., Fang, S., Shao, Y., Yang, W., et al. (2021). A novel fully immersive virtual reality environment for upper extremity rehabilitation in patients with stroke. Ann. N. Y. Acad. Sc.i. 1493, 75–89. doi: 10.1111/nyas.14554
Ögün, M. N., Kurul, R., Yaşar, M. F., Turkoglu, S. A., Avci, Ş, and Yildiz, N. (2019). Effect of Leap Motion-based 3D Immersive Virtual Reality Usage on Upper Extremity Function in Ischemic Stroke Patients. Arq. Neuropsiquiatr. 77, 681–688. doi: 10.1590/0004-282X20190129
Park, Y. H., Lee, C. H., and Lee, B. H. (2013). Clinical usefulness of the virtual reality-based postural control training on the gait ability in patients with stroke. J. Exerc. Rehabil. 9, 489–494. doi: 10.12965/jer.130066
Perez-Marcos, D., Bieler-Aeschlimann, M., and Serino, A. (2018). Virtual reality as a vehicle to empower motor-cognitive neurorehabilitation. Front. Psychol. 9:2120. doi: 10.3389/fpsyg.2018.02120
Porras, D. C., Siemonsma, P., Inzelberg, R., Zeilig, G., and Plotnik, M. (2018). Advantages of virtual reality in the rehabilitation of balance and gait: Systematic review. Neurology 90, 1017–1025. doi: 10.1177/2040622319868379
Qian, J., McDonough, D. J., and Gao, Z. (2020). The effectiveness of virtual reality exercise on individual’s physiological, psychological and rehabilitative outcomes: A systematic review. Int. J. Environ. Res. Public Health 17:4133. doi: 10.3390/ijerph17114133
Radianti, J., Majchrzak, T. A., Fromm, J., and Wohlgenannt, I. (2020). A systematic review of immersive virtual reality applications for higher education: Design elements, lessons learned, and research agenda. Comput. Educ. 147:103778. doi: 10.1016/j.compedu.2019.103778
Raffin, E., and Hummel, F. C. (2018). Restoring motor functions after stroke: Multiple approaches and opportunities. Neuroscientist 24, 400–416. doi: 10.1177/1073858417737486
Rose, T., Nam, C. S., and Chen, K. B. (2018). Immersion of virtual reality for rehabilitation - Review. Appl. Ergon. 69, 153–161. doi: 10.1016/j.apergo.2018.01.009
Rutkowski, S., Rutkowska, A., Kiper, P., Jastrzebski, D., Racheniuk, H., Turolla, A., et al. (2020). Virtual reality rehabilitation in patients with chronic obstructive pulmonary disease: a randomized controlled trial. Int. J. Chron. Obstruct. Pulmon. Dis. 15, 117–124. doi: 10.2147/COPD.S223592
Rutschmann, R. M., Schrauf, M., and Greenlee, M. W. (2000). Brain activation during dichoptic presentation of optic flow stimuli. Exp. Brain Res. 134, 533–537. doi: 10.1007/s002210000502
Saldana, D., Neureither, M., Schmiesing, A., Jahng, E., Kysh, L., Roll, S. C., et al. (2020). Applications of head-mounted displays for virtual reality in adult physical rehabilitation: a scoping review. Am. J. Occup. Ther. 74, 1–15. doi: 10.5014/ajot.2020.041442
Specht, J., Schroeder, H., Krakow, K., Meinhardt, G., Stegmann, B., and Meinhardt-Injac, B. (2021). Acceptance of immersive head-mounted display virtual reality in stroke patients. Comput. Hum. Behav. Rep. 4:100141. doi: 10.1016/j.chbr.2021.100141
Tinga, A. M., Visser-Meily, J. M., van der Smagt, M. J., Van der Stigchel, S., van Ee, R., and Nijboer, T. C. (2016). Multisensory stimulation to improve low- and higher-level sensory deficits after stroke: a systematic review. Neuropsychol. Rev. 26, 73–91. doi: 10.1007/s11065-015-9301-1
Keywords: virtual reality, immersive, stroke, physical rehabilitation, functional ability
Citation: Patsaki I, Dimitriadi N, Despoti A, Tzoumi D, Leventakis N, Roussou G, Papathanasiou A, Nanas S and Karatzanos E (2022) The effectiveness of immersive virtual reality in physical recovery of stroke patients: A systematic review. Front. Syst. Neurosci. 16:880447. doi: 10.3389/fnsys.2022.880447
Received: 21 February 2022; Accepted: 01 September 2022;
Published: 22 September 2022.
Edited by:
Notger G. Müller, University of Potsdam, GermanyReviewed by:
Soha Saleh, Kessler Foundation, United StatesRaymond van Ee, Radboud University, Netherlands
Copyright © 2022 Patsaki, Dimitriadi, Despoti, Tzoumi, Leventakis, Roussou, Papathanasiou, Nanas and Karatzanos. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Irini Patsaki, aXBhdHNha2lAeWFob28uZ3I=
 Irini Patsaki
Irini Patsaki Nefeli Dimitriadi
Nefeli Dimitriadi Akylina Despoti1
Akylina Despoti1 Argyro Papathanasiou
Argyro Papathanasiou Serafeim Nanas
Serafeim Nanas