
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
CASE REPORT article
Front. Med. , 12 January 2024
Sec. Dermatology
Volume 11 - 2024 | https://doi.org/10.3389/fmed.2024.1336688
This article is part of the Research Topic Current Concepts in Epidemiology, Diagnosis, Associated Co-Morbidities, and Therapeutics of Non-Melanoma Skin Cancers: Beyond Basal Cell and Squamous Cell Carcinomas View all 12 articles
Hidradenitis suppurativa (HS) is an uncommon, recurrent, inflammatory skin illness of the apocrine glands, with a questionable etiology. The disease is associated with a multitude of comorbidities, of which the appearance of malignancy is the most important. Squamous cell carcinoma is considered the most frequent malignancy that can appear in HS. A case report of a 72 years-old male is presented, who suffered over 40 years from persistent, extensive hidradenitis suppurativa in stage Hurley III, on the buttocks and perianal region, who recently presented two verrucous semi-consistent, skin-colored tumors on the right buttock. The biopsy and histopathological exam confirmed a verrucous type of squamous cell carcinoma. There are about 100 reported clinical cases of squamous cell carcinoma complicating hidradenitis suppurativa in the literature, but only a few describe a verrucous carcinoma as a clinical form. The particularity of the case is the rare appearance of multiple verrucous types of squamous cell carcinomas in a male patient, in Hurley Stage III, with a long HS disease duration, appearing on the perianal/gluteal region, being the first case report in our country. We suggest that a tumor screening should be done for all the patients with HS who have these risks.
Hidradenitis suppurativa is a chronic inflammatory disease, with the appearance of follicular obstructions, abscesses, fistulas, foul mucopurulent secretions, and vicious, often debilitating scarring of the apocrine gland areas of the skin (1). The average prevalence in Europe of the disease is about 1% (2). The first case was published in 1839 by Valpeau (3). The disease was described by Verneuil (3), mentioning that the chronic inflammatory lesions typically involve the folds and the buttock. The appearance of the clinical features can develop symptoms like pain, pruritus, and debilitating scars, with implications for the quality of life (4). The disease is at the border of different specialties like dermatology, general surgery, or plastic surgery and for this reason, a precise diagnosis is generally delayed (5). In the evolution of HS, a large number of associated diseases can occur. From these, the appearance of malignancies is the most important. In a recent review, Gierek et al. (6) highlighted that in the evolution of HS, the appearance of nonmelanoma skin cancer (NMSC), hematologic malignancies, and metastatic cancers are possible. From these, the most frequent complication is the development of squamous cell carcinoma (SCC). Also from this review, the authors analyzed 74 cases of SCC that appeared on HS, and they concluded that the majority of the primary squamous cell carcinomas were an ulcerated or nodule-type form (6). There are about 100 reported cases of squamous cell carcinoma complicating hidradenitis suppurativa in the literature, but only a few describe a verrucous carcinoma type as a clinical form (6). We present a clinical case of verrucous squamous cell carcinoma developing on chronic HS.
We present a clinical case of a 72 years-old, non-smoking, immune-competent normoponderal patient, who suffered over 40 years from persistent, extensive hidradenitis suppurativa on the buttocks and perianal region. He was treated for over 40 years with oral antibiotics and retinoids, local topical antibiotics, steroids, and a multitude of antiseptics without success. He had periods of remission and exacerbation. During the dermatological consultation, we found an active area of HS in stage Hurley III on the buttocks and perianal region and two verrucous semi-consistent, skin-colored tumors on the right buttock, having a base diameter of 2.5 and 3 cm, presenting spontaneous bleeding (Figure 1). These tumors developed relatively quickly in approximately 3 months. The patient is suffering from several chronic diseases, like chronic obstructive pulmonary disease, essential hypertonia, arthrosis, and osteoporosis, which were under medical control and are not related to HS. He is not suffering from diabetes. His family medical history was unremarkable. The results of routine laboratory testing like hematology and biochemistry were within the normal limits. The treatment decision was the surgical removal of the tumors. The histopathological examination of the two excised tumors confirmed the verrucous type of squamous cell carcinoma (Figure 2). Based on the clinical and histological examination, the patient was transferred to an oncology service for further examination and treatment options. Unfortunately, due to the advanced stage of the carcinoma, the evolution was fatal for the patient.
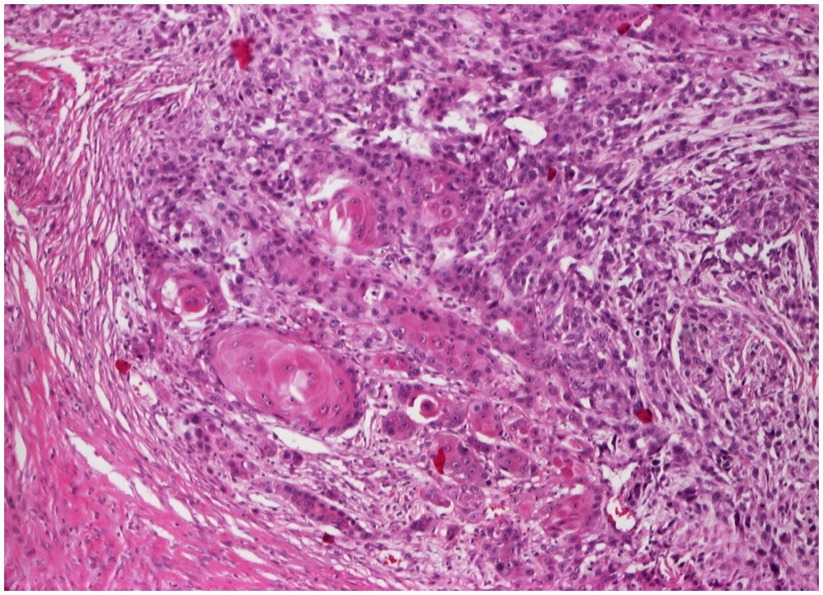
Figure 2. Biopsy, buttocks (H&E 10×): poorly differentiated verrucous squamous cell carcinoma with marked cytonuclear pleomorphism and atypical mitoses infiltrating into the dermis.
Hidradenitis suppurativa (HS) is a chronic and exhausting dermatologic disease of the apocrine glands, characterized by the formation of multiple inflammatory lesions, abscesses, fistulas, and scars, especially arising on folds and buttocks. The exact prevalence of HS is unknown, it has been estimated to be as high as 4.1%, and it is three times more frequent in women than in men (7). The etiology is still unclear, but the illness is frequently associated with smoking, poor hygiene, immunocompromised status, and diseases like metabolic, cardiovascular, endocrine, gastrointestinal, rheumatologic, and psychiatric ones, and also with reduced cutaneous levels of calprotectin, zinc, or ascorbate, which all together compromise the life quality of these patients (4). The clinical aspect of HS is multiform, from inflammatory lesions to nodules, abscesses, fistulas, and scars that can be present, as is well defined by the Hurley staging. The differential diagnoses can include bacterial, especially Staphylococcal skin infections, with or without elementary lesions like abscesses, carbuncles, and furuncles, and cutaneous Crohn’s disease. Also, different types of cysts, like Bartholin or epidermoid cysts can resemble HS (8). Squamous cell carcinoma (SCC) is the second most common skin cancer, accounting for 20% of skin cancers (9). Squamous cell carcinomas comprise different types of cancers that are formed on the surface of the skin and mucous membranes (10). The most important general risk factors for the development of SCC on the skin, are sun exposure, age, and phototype of the skin, especially in cases of phototype I–III was described the mutation in the suppressor protein (TP53) (11). Squamous cell carcinomas may arise in a multitude of chronic inflammatory dermatoses, wounds, and scars such as thermal burn scars, discoid lupus erythematosus, chronic ulcerations, chronic radiodermatitis, precancers, etc. (12–19). In the literature, we have found published cases of SCC as a severe complication of chronic HS lesions. The relationship between HS lesions and SCC is poorly understood and must be further explored (20). The development of SCC in cases of HS, is multifactorial. HS is more prevalent in women, but the appearance of SCC on the disease is more frequent in men (6). Immunosuppression due to chronic disease is one of the risk factors. Also, the location of HS lesions is important, because most of the published cases of SCC on HS lesions are located in the gluteal and perianal region (21–26). Gierek et al. (6), found that 94.59% of the cases of SCC were developed in the perianal/gluteal region of HS. Most of the reported cases were in Hurley stage III of the disease and were males, like in our presented case (25, 27–29). Also, Gierek et al. (6), concluded that the average age of the patient with SCC in HS lesions was 52.6 years, and the mean time from onset SCC was 25.79 years (range 8 years to 53 years), and most of the patients were in Hurley Stage III (97.2%). In two articles the authors suggest the presence of the HPV virus as a causative factor for the appearance of SCC in HS (30, 31). We cannot prove this hypothesis in our case. The studied references present mostly ulcerated, nodular, and metastatic clinical forms of SCC developed from HS. Cosman et al. (32), present a paper about a verrucous form, mentioning that their case is the second published with this clinical form, like in our case presentation. Also, we did not find any references about the presence of two SCC tumors at the same time in a patient with HS. New ultrasound techniques are used to diagnose the possible transformation of HS into squamous cell carcinoma. Wortsman (33) describes the ultrasound diagnostic criteria for HS and suggests new scores for the severity of the disease. Zussino et al. (34) describe the usefulness of color Doppler in the staging and the follow-up of the evolution of HS. Nazzaro et al. (35) comparing the clinical forms and sonographic scores in hidradenitis suppurativa, propose a new ultrasound scoring system for the follow-up on the evolution of HS, including malignant transformation. Treatment of HS is difficult due to a lack of effective medical therapies. Modern possibilities, like biological therapies, open a new era in the treatment of this disease (36). The treatment of this complication is surgical and depending on the staging of the tumor, is oncologic. Considering the high mortality rate in these cases, we suggest screening for an early diagnosis for the possibility of the appearance of SCC lesions in all HS patients (37).
The particularity of the case is the rare appearance of multiple verrucous types of squamous cell carcinomas on a chronic, recurrent, inflammatory dermatologic disease like HS, which is the first case published in our country. The potential risk factors such as sex, advanced stage, chronic evolution, and specific localization as perianal/gluteal and buttock region should be considered in the malignant transformation of HS. We recommend a dermatological cancer screening to all patients with HS who have these risks.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving humans were approved by the Dermamed Private Office Ethics Committee. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
GF: Conceptualization, Formal analysis, Funding acquisition, Investigation, Methodology, Resources, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing, Project administration. LF: Conceptualization, Formal analysis, Investigation, Methodology, Resources, Validation, Visualization, Writing – original draft, Writing – review & editing. LI: Visualization, Writing – review & editing, Data curation, Software. JF: Conceptualization, Formal analysis, Investigation, Methodology, Validation, Visualization, Writing – original draft, Writing – review & editing. IB: Conceptualization, Formal analysis, Investigation, Methodology, Validation, Writing – original draft, Writing – review & editing.
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Fimmel, S, and Zouboulis, CC. Comorbidities of hidradenitis suppurativa (acne inversa). Dermatoendocrinology. (2010) 2:9–16. doi: 10.4161/derm.2.1.12490
2. Zouboulis, CC, Desai, N, Emtestam, L, Hunger, RE, Ioannides, D, Juhász, I, et al. European S1 guideline for the treatment of hidradenitis suppurativa/acne inversa. J Eur Acad Dermatol Venereol. (2015) 29:619–44. doi: 10.1111/jdv.12966
3. Narla, S, Lyons, AB, and Hamzavi, LH. The most recent advances in understanding and managing hidradenitis suppurativa. F1000Res. (2020) 9:1049. doi: 10.12688/f1000research.26083.1
4. Cartron, A, and Driscoll, MS. Comorbidities of hidradenitis suppurativa: a review of the literature. Int J Womens Dermatol. (2019) 5:330–4. doi: 10.1016/j.ijwd.2019.06.026
5. Revuz, J. Hidradenitis suppurativa. J Eur Acad Dermatol Venereol. (2009) 23:985–98. doi: 10.1111/j.1468-3083.2009.03356.x
6. Gierek, M, Niemiec, P, Szyluk, K, Ochala-Gierek, G, and Bergler-Czop, B. Hidradenitis suppurativa and squamous cell carcinoma: a systematic review of the literature. Postepy Dermatol Alergol. (2023) 40:350–4. doi: 10.5114/ada.2023.126563
7. Chapman, S, Delgadillo, D, Barber, C, and Khachemoune, A. Cutaneous squamous cell carcinoma complicating hidradenitis suppurativa: a review of the prevalence, pathogenesis, and treatment of this dreaded complication. Acta Dermatovenerol Alp Pannonica Adriat. (2018) 27:25–8. doi: 10.15570/actaapa.2018.5
8. Jemec, GBE. Clinical practice. Hidradenitis suppurativa. N Engl J Med. (2012) 366:158–64. doi: 10.1056/NEJMcp1014163
9. Waldman, A, and Schmults, C. Cutaneous squamous cell carcinoma. Hematol Oncol Clin North Am. (2019) 33:1–12. doi: 10.1016/j.hoc.2018.08.001
10. Pena, ZG, Sivamani, RK, Konia, TH, and Eisen, DB. Squamous cell carcinoma in the setting of chronic hidradenitis suppurativa: report of a patient and update of the literature. Dermatol Online J. (2015) 21. doi: 10.5070/D3214026278
11. Wikonkal, NM, and Brash, DE. Ultraviolet radiation induced signature mutations in photocarcinogenesis. J Investig Dermatol Symp Proc. (1999) 4:6–10. doi: 10.1038/sj.jidsp.5640173
12. Rosen, T. Squamous cell carcinoma: complication of chronic skin disorders in black patients. J Natl Med Assoc. (1986) 78:1203–5.
13. Katz, RD, and Goldberg, NH. Marjolin ulcer arising within hidradenitis: a case report and literature review. Ann Plast Surg. (2009) 62:173–4. doi: 10.1097/SAP.0b013e31817d87b3
14. Nijhawan, PK, and Elkin, PL. 59-year-old man with right hip pain. Mayo Clin Proc. (1998) 73:541–4. doi: 10.4065/73.6.541
15. Yon, JR, Son, JD, Fredericks, C, Morton, M, Kingsley, S, Gupta, S, et al. Marjolin’s ulcer in chronic hidradenitis suppurativa: a rare complication of an often neglected disease. J Burn Care Res. (2017) 38:121–4. doi: 10.1097/BCR.0000000000000399
16. Beard, CJ, Gathings, RM, and Bandino, JP. Exophytic mass arising within hidradenitis suppurativa: answer. Am J Dermatopathol. (2019) 41:235–6. doi: 10.1097/DAD.0000000000001064
17. Novick, M, Gard, DA, Hardy, SB, and Spira, M. Burn scar carcinoma: a review and analysis of 46 cases. J Trauma. (1977) 17:809–17. doi: 10.1097/00005373-197710000-00010
18. Knackstedt, TJ, Collins, LK, Li, Z, Yan, S, and Samie, FH. Squamous cell carcinoma arising in hypertrophic lichen planus: a review and analysis of 38 cases. Dermatol Surg. (2015) 41:1411–8. doi: 10.1097/DSS.0000000000000565
19. Boozalis, E, Shah, AA, Wigley, F, Kang, S, and Kwatra, SG. Morphea and systemic sclerosis are associated with an increased risk for melanoma and nonmelanoma skin cancer. J Am Acad Dermatol. (2019) 80:1449–51. doi: 10.1016/j.jaad.2018.10.022
20. Jourabchi, N, Fischer, AH, Cimino-Mathews, A, Waters, KM, and Okoye, GA. Squamous cell carcinoma complicating a chronic lesion of hidradenitis suppurativa: a case report and review of the literature. Int Wound J. (2017) 14:435–8. doi: 10.1111/iwj.12671
21. Lavogiez, C, Delaporte, E, Darras-Vercambre, S, Martin de Lassalle, E, Castillo, C, Mirabel, X, et al. Clinicopathological study of 13 cases of squamous cell carcinoma complicating hidradenitis suppurativa. Dermatology. (2010) 220:147–53. doi: 10.1159/000269836
22. Kohorst, JJ, Shah, KK, Hallemeier, CL, Baum, CL, and Davis, MDP. Squamous cell carcinoma in perineal, perianal, and gluteal hidradenitis suppurativa: experience in 12 patients. Dermatol Surg. (2019) 45:519–26. doi: 10.1097/DSS.0000000000001713
23. Chandramohan, K, Mathews, A, Kurian, A, Thomas, S, and Ramachandran, K. Squamous cell carcinoma arising from perineal lesion in a familial case of hidradenitis suppurativa. Int Wound J. (2009) 6:141–4. doi: 10.1111/j.1742-481X.2009.00582.x
24. Pérez-Diaz, D, Calvo-Serrano, M, Mártinez-Hijosa, E, Fuenmayor-Valera, L, Muñoz-Jiménez, F, Turégano-Fuentes, F, et al. Squamous cell carcinoma complicating perianal hidradenitis suppurativa. Int J Color Dis. (1995) 10:225–8. doi: 10.1007/BF00346224
25. Maclean, GM, and Coleman, DJ. Three fatal cases of squamous cell carcinoma arising in chronic perineal hidradenitis suppurativa. Ann R Coll Surg Engl. (2007) 89:709–12. doi: 10.1308/003588407X209392
26. Gur, E, Neligan, PC, Shafir, R, Reznick, R, Cohen, M, and Shpitzer, T. Squamous cell carcinoma in perineal inflammatory disease. Ann Plast Surg. (1997) 38:653–7. doi: 10.1097/00000637-199706000-00016
27. Mendonça, H, Rebelo, C, Fernandes, A, Lino, A, and Garcia e Silva, L. Squamous cell carcinoma arising in hidradenitis suppurativa. J Dermatol Surg Oncol. (1991) 17:830–2. doi: 10.1111/j.1524-4725.1991.tb03269.x
28. Altunay, IK, Gökdemir, G, Kurt, A, and Kayaoglu, S. Hidradenitis suppurativa and squamous cell carcinoma. Dermatol Surg. (2002) 28:88–90. doi: 10.1046/j.1524-4725.2002.01090.x
29. Shukla, VK, and Hughes, LE. A case of squamous cell carcinoma complicating hidradenitis suppurativa. Eur J Surg Oncol. (1995) 21:106–9. doi: 10.1016/S0748-7983(05)80084-8
30. Segura Palacios, JM, García Montero, P, Fúnez Liébana, R, and Repiso Jiménez, JB. Human papilloma virus and the risk of squamous cell carcinoma arising in hidradenitis suppurativa. Actas Dermosifiliogr. (2018) 109:457–9. doi: 10.1016/j.ad.2017.06.019
31. Yen, CF, Chang, Y, and Lee, YY. Image gallery: squamous cell carcinoma arising in long-standing hidradenitis suppurativa. Br J Dermatol. (2018) 179:e226. doi: 10.1111/bjd.17031
32. Cosman, B, O'Grady, T, and Pekarske, S. Verrucous carcinoma arising in hidradenitis suppurativa. Int J Color Dis. (2000) 15:342–6. doi: 10.1007/s003840000256
33. Wortsman, X. Update on ultrasound diagnostic criteria and new ultrasound severity and activity scorings of hidradenitis suppurativa: modified SOS-HS and US-HSA. J Ultrasound Med. (2024) 43:207–13. doi: 10.1002/jum.16351
34. Zussino, M, Nazzaro, G, Moltrasio, C, and Marzano, AV. Coexistence of steatocystoma multiplex and hidradenitis suppurativa: assessment of this unique association by means of ultrasonography and color doppler. Skin Res Technol. (2019) 25:877–80. doi: 10.1111/srt.12751
35. Nazzaro, G, Passoni, E, Muratori, S, Moltrasio, C, Guanziroli, E, Barbareschi, M, et al. Comparison of clinical and sonographic scores in hidradenitis suppurativa and proposal of a novel ultrasound scoring system. Ital J Dermatol Venerol. (2021) 156:235–9. doi: 10.23736/S2784-8671.18.06196-5
36. Martora, F, Megna, M, Battista, T, Potestio, L, Annunziata, MC, Marasca, C, et al. Adalimumab, ustekinumab, and secukinumab in the management of hidradenitis suppurativa: a review of the real-life experience. Clin Cosmet Investig Dermatol. (2023) 16:135–48. doi: 10.2147/CCID.S391356
Keywords: hidradenitis suppurativa, squamous cell carcinoma, verrucous carcinoma, inflammatory lesions, comorbidities
Citation: Fekete GL, Fekete L, Iantovics LB, Fekete JE and Brihan I (2024) Multiple verrucous squamous cell carcinomas developing on chronic hidradenitis suppurativa lesions—a rare case report from Romania. Front. Med. 11:1336688. doi: 10.3389/fmed.2024.1336688
Received: 11 November 2023; Accepted: 02 January 2024;
Published: 12 January 2024.
Edited by:
Lawrence Chukwudi Nwabudike, National Institute for Diabetes, Nutrition and Metabolic Diseases Prof. Dr. N. Paulescu, RomaniaReviewed by:
Gianluca Nazzaro, IRCCS Ca’ Granda Foundation Maggiore Policlinico Hospital, ItalyCopyright © 2024 Fekete, Fekete, Iantovics, Fekete and Brihan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: László Fekete, ZGVybWFmZWsxOTYyQGdtYWlsLmNvbQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.