
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Med., 11 January 2023
Sec. Geriatric Medicine
Volume 9 - 2022 | https://doi.org/10.3389/fmed.2022.1106312
 Worapaka Manosroi1,2
Worapaka Manosroi1,2 Lattapol Koetsuk3
Lattapol Koetsuk3 Phichayut Phinyo2,4,5
Phichayut Phinyo2,4,5 Pojsakorn Danpanichkul6
Pojsakorn Danpanichkul6 Pichitchai Atthakomol2,3*
Pichitchai Atthakomol2,3*Prolonged length of stay (LOS) in osteoporotic femoral neck fracture patients increased the hospital care cost and demonstrated in-hospital complications. This study aimed to develop an ease-of use predictive model of prolonged LOS in osteoporotic femoral neck fracture patients. In this 5-year retrospective study, the medical charts of 255 patients admitted to hospital with an osteoporotic femoral neck fracture resulting from a simple fall from January 2014 to December 2018 were reviewed. Multivariable fractional polynomials (MFP) algorithms was applied to develop the predictive model from candidate predictors of prolonged LOS. The discrimination performance of predictive model was evaluated using the receiver operating characteristic curve (ROC). Internal validity was assessed using bootstrapping. From 289 patients who were hospitalized with an osteoporotic fracture of femoral neck throughout this study, 255 (88%) fulfilled the inclusion criteria. There was 54.90% (140 of 255 patients) of patients who had prolonged LOS. The predictors of the predictive model were age, BMI, ASA score class 3 or 4, arthroplasty and time from injury to surgery. The area under ROC curve of the model was 0.83 (95% confidence interval 0.77–0.88). Internal validation with bootstrap re-sampling revealed an optimism of −0.002 (range −0.300–0.296) with an estimated shrinkage factor of 0.907 for the predictive model. The current predictive model developed from preoperative predictors which had a good discriminative ability to differentiate between length of hospitalization less than 14 days and prolonged LOS in osteoporotic femoral neck patients. This model can be applied as ease-of use calculator application to help patients, their families and clinicians make appropriate decisions in terms of treatment planning, postoperative care program, and cost-effectiveness before patients receiving the definitive treatments.
Osteoporotic femoral neck fractures constitute approximately half of all osteoporotic hip fractures and are the type of fracture which has the highest demonstrated morbidity and mortality among all fractures (1–3). Osteoporotic femoral neck fracture are primarily caused by low energy trauma in the elderly, while in young adults the cause is typically the result of high-energy trauma such as motor vehicle accidents (4, 5). This type of injury usually requires surgery to restore normal function. In 1993 it was reported that the mortality rate of femoral neck fracture in elderly patients during the first year after surgery was approximately 30% (6). The causes of death were related to co-morbidities and postoperative complications (6). More recent data has indicated that the mortality rate of this type of fracture has declined to around 10% (7). One of the factors associated with the high mortality rates with this type of fracture is the length of stay (LOS). It has been reported that a hospital stays of more than 14 days (prolonged LOS) increases 30-day mortality in hip fracture patients (8).
Length of hospital stay is one of the important indicators in hip fracture care which are related to quality of treatment and which enable benchmarking (9). The burden of prolonged LOS in trauma patients is associated with in-hospital complications including urinary tract infection, pneumonia, sepsis, decubitus ulcer, delirium, and deep vein thrombosis (10). Increased hospital care cost has also been demonstrated in cases of prolonged LOS which had in-hospital complications (11). Therefore, earlier recognition of patients who are likely to have prolonged LOS can assist in the provision of effective and timely intervention. Earlier recognition can also help reduce the cost of hospitalization, the demand on medical resources and the incidence of patient in-hospital complications.
Various predictors for LOS in osteoporotic hip fractures have been reported including delay in time to surgery, previous hip fractures, cerebrovascular disease, smoking status, ASA classification, age and degree of decline in cognitive function (12–17). Some models to predict LOS in osteoporotic hip fracture patients have been proposed (18–20). One study created a model to predict LOS in hip fractures (both intertrochanteric and femoral neck types) (19). Another created a predictive model using multiple linear regression model but only in patients who underwent hip-replacement surgery (20). Another study developed a predictive model using machine learning algorithms in osteoporotic femoral neck fractures (18). However, although these proposed models are precise, they cannot be properly applied in clinical practice as the models use intra-and postoperative predictors to predict LOS which increases the time necessary to predict LOS (18). A practical predictive model should be able to be applied at an earlier time point to facilitate decisions by patients and their families as well as medical team preparations. A practical predictive model must be able to use preoperative predictors in model development.
Presently, there is no practical predictive model for prolonged LOS specifically for osteoporotic femoral neck fracture. This study aimed to develop an-easy-to-use model from preoperative predictors to predict prolonged LOS specifically for osteoporotic femoral neck fracture patients.
This prognostic prediction research was conducted using a retrospective observational cohort design at an academic university hospital. The institutional ethics committee approved the study protocol (ethical number: ORT-2564-08118). The reporting of this study is compliant with the Transparent Reporting of a multivariable prediction model for Individual Prognosis Or Diagnosis (TRIPOD) statement (21).
Data of the patient sample were extracted from the medical records of the hospital. Patients who had a fractured neck of femur (ICD-10 = S7200) and who were admitted to the hospital between January 2014 and December 2018 were identified using International Classification of Disease 10 (ICD-10) codes. Two of staff members and the chief orthopedic resident conducted the retrospective chart reviews manually. Any debatable data was discussed and resolved by three orthopedic staff members. All data collectors have trained how to evaluate and gather the data from hospital medical records under supervision of the orthopedic staff members. Patient inclusion criteria were Thai patients, minimum age 50 years, and an osteoporotic femoral neck fracture injury deriving from a simple fall. The exclusion criteria were a bilateral femoral neck fracture, a prior femoral neck fracture and fractures in more than one area. Any possible pathological fractures or fractures caused by a high-energy mechanism including but not limited to traffic accidents were excluded from the study. Patients who died before discharge were also excluded.
Data on general demographics, types of comorbidities, results of laboratory investigations and type of surgical treatment were manually assembled from retrospective chart reviews. In cases where data could not be extracted from medical charts, telephone contact with the patient or their family was made to obtain the information.
Length of hospital stay was measured in days and was defined as the difference between the discharge and admission date (20). Prolonged LOS was defined as patients with a hospital stay greater ≥14 days (8, 12, 14). Generally, the discharge criteria for osteoporotic femoral neck fracture patients after surgery in our institute were: First, the patient can perform weight-bearing as tolerated with gait aids in patients who have undergone arthroplasty or partial weight-bearing with gait aids in patients who have undergone internal fixation (multiple screw fixation/dynamic hip screw). For patients who had dependent mobility before the fracture, ambulation with a wheelchair after surgery was the goal. Additionally, the body temperature should be less than 37.5 degree Celsius with no purulent drainage, pain or tenderness, localized swelling, or redness at the surgical site.
• General factors
- Age at admission
- Gender
- Body mass index (BMI) at admission
- Independent mobility defined as a patient who could walk independently either with or without gait aids before the osteoporotic femoral neck fracture
• Types of comorbidities
- Active malignancy, dementia or Alzheimer’s disease, cerebrovascular disease, cardiovascular disease, congestive heart failure, chronic obstructive pulmonary disorder, diabetes mellitus, and current pneumonia
- American Society of Anesthesiologists (ASA) Physical Status Classification (ASA score) which were interpreted by anesthesiologists
The types of comorbidities in this study were determined based on the ICD-10 coding in the discharge summary.
• Laboratory investigation results
- Admission hemoglobin concentration
- Admission glomerular filtration rate (GFR)
• Characteristics of surgery
- Internal fixation, arthroplasty
- Time from injury to operation defined as the number of days from the date of the injury to the date of the operation.
Statistical analysis was performed using STATA program (Stata/MP 16.1 for Mac, Copyright 1985–2019, Stata Corp., LLC, College Station, TX, USA). P-values < 0.05 were considered statistically significant. Categorical variables are presented as frequencies and percentages. Normally distributed continuous variables are presented as mean and standard deviation (SD). Non-normally distributed continuous variables are presented as median and interquartile range (IQR). Fisher’s exact test was used in calculating the associations between prolonged LOS and categorical variables. Student’s t-test was used in calculating the associations with normally distributed continuous variables. The relationship between non-normally distributed variables was analyzed using the Mann–Whitney U-test.
The study sample size was determined based on the standard recommendation of 10 events of interest per predictor variable (22). Thus, 140 prolonged length of stay status osteoporotic femoral neck fracture patients were needed for modeling 14 predictors. All continuous clinical predictors were retained to maintain completeness of data during the categorization of the continuous variables.
To develop the predictive model, multivariable fractional polynomials (MFP) algorithms were applied to avoid unnecessary categorization or inappropriate modeling of the determinants–outcomes association that would violate the linearity assumption (23). The MFP function allows investigators to identify the most appropriate functional form for each included continuous predictor. Log cumulative odd ratios (beta-coefficient), 95% confidence intervals (CI), and P-values are reported. Multiple imputation was applied if a candidate predictor had missing data >5% (24). The collinearity of each candidate predictor was assessed. Predictors which had a variant inflation factor (VIF) value >5 were excluded from the multivariable analysis. MFP consisted of two steps. The first step of MFP was employing the initial model approach by simultaneously including all candidate predictors within the model. Then, backward elimination was done to remove non-significant (P-value > 0.05) and non-contributing factors from the model, yielding the final model. In our study, however, we decided to preserve some candidate predictors based on prior clinical knowledge and previous published findings. In the second step, we determined the fittest fractional transformation for continuous covariates to be included during statistical modeling using a closed test algorithm.
To evaluate the model performance and for internal validation, the receiver operating characteristic (ROC) curve was plotted to assess the performance of the model. Hosmer–Lemeshow goodness-of-fit statistical testing was performed for model calibration. The calibration plot is presented to show the agreement between the actual observed event occurrence and the decile of the model-predicted probabilities. Internal validation was performed with a bootstrap re-sampling procedure with 1,000 replicates. The model optimism and shrinkage factor were estimated. The predictive model was developed into a calculator application. The application shows the predicted odds ratio and probability of prolonged LOS following osteoporotic femoral neck fracture after the input of all parameters.
Of the 289 patients hospitalized with an osteoporotic femoral neck during the time frame of this study, 255 (88%) met the inclusion criteria. Of that total, 54.90% (140 of 255) of the osteoporotic femoral neck fracture patients had prolonged LOS. The majority, 181 (70.98%), were female. The mean age was 75.65 ± 10.23 years. Arthroplasty was performed in most patients (216 or 84.71%). The median length of stay was 14 days. Demographic data are shown in Table 1.
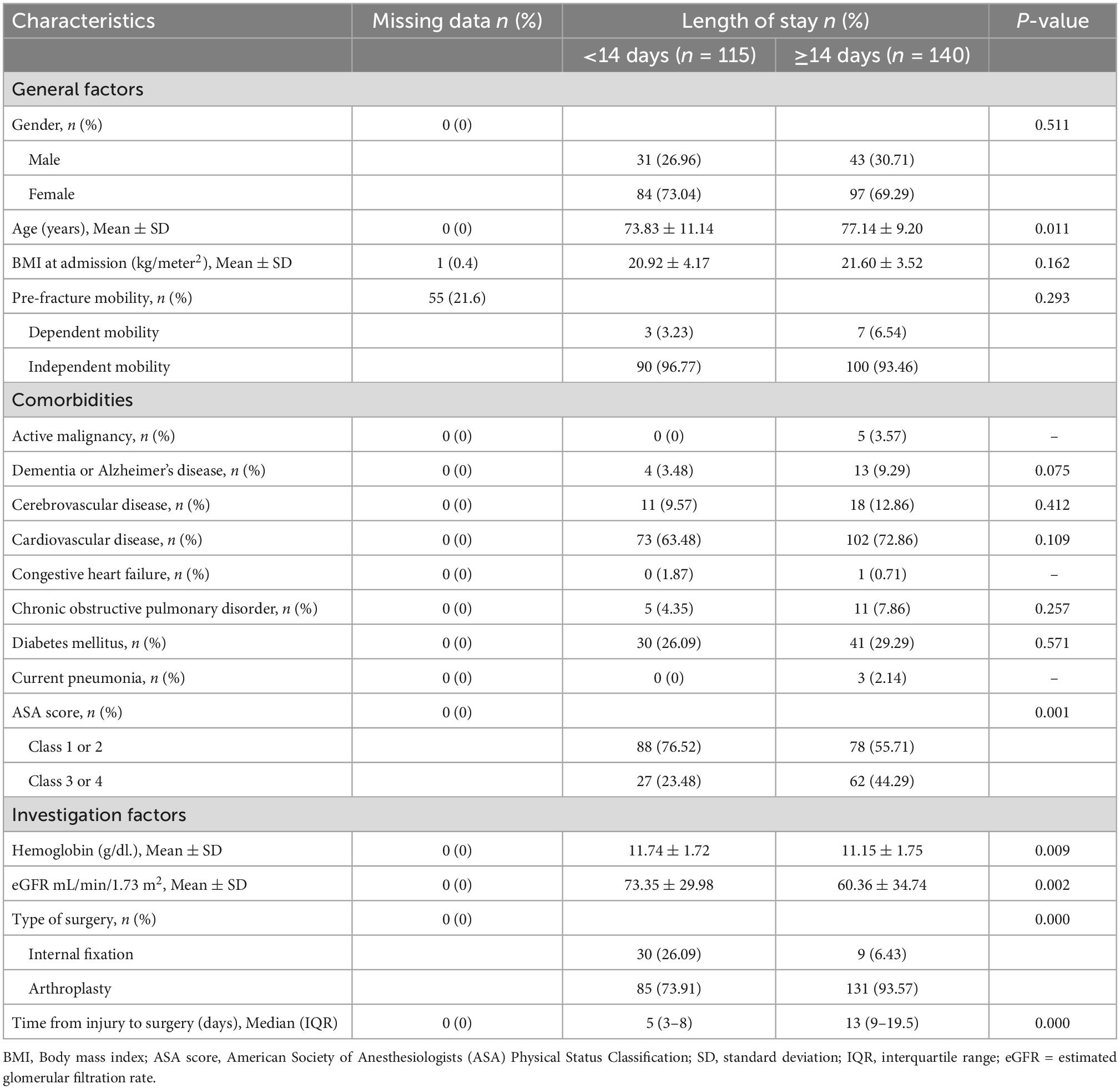
Table 1. Baseline clinical characteristics and candidate predictors for prolonged length of stay of patients with osteoporotic femoral neck fracture (n = 255).
All candidate predictors exhibited a variant inflation factor (VIF) value <5. Multiple imputation was applied to the “dependent mobility” predictor. Multivariable fractional polynomial logistic regression was applied to all candidate predictors at the initial model. The area under the ROC curve of the initial model was 0.84. After back elimination, the final model predictors were age, BMI, ASA score class 3 or 4, arthroplasty and time from injury to surgery. The area under ROC curve of the final model was 0.83 (95% CI 0.77–0.88) (Table 2).
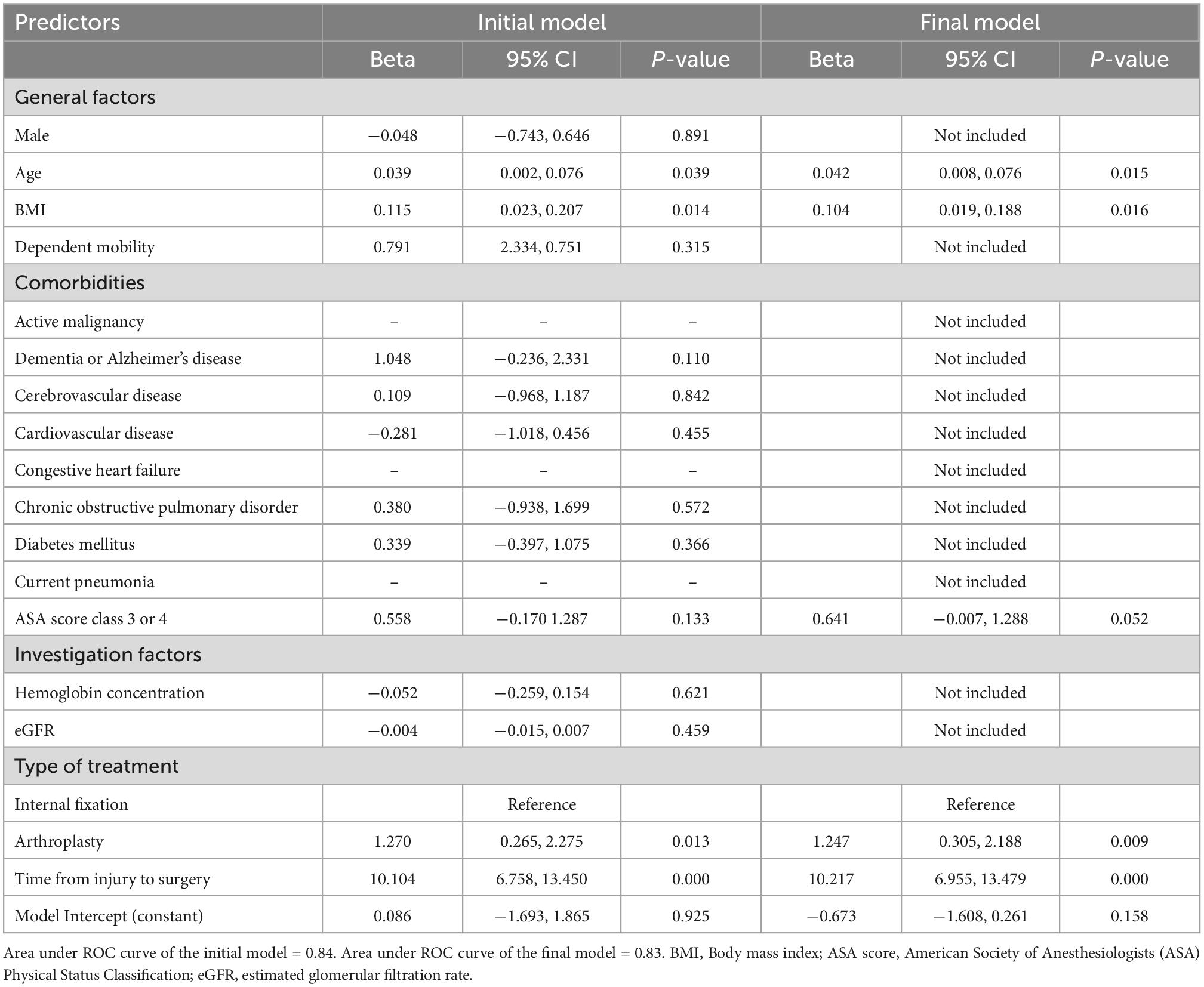
Table 2. Multivariable fractional polynomials logistic regression model of the initial model and the final model for prolonged length of stay in patients with osteoporotic femoral neck fracture.
The fittest fractional transformation for continuous variables from the final model is shown in Table 3. The calibration of the final model is presented with calibration plots (Figure 1). The Hosmer–Lemeshow goodness-of-fit statistic was insignificant for the final model (p = 0.491). Internal validation with bootstrap re-sampling revealed an optimism of −0.002 (range −0.300–0.296) with an estimated shrinkage factor of 0.907 for the final model.
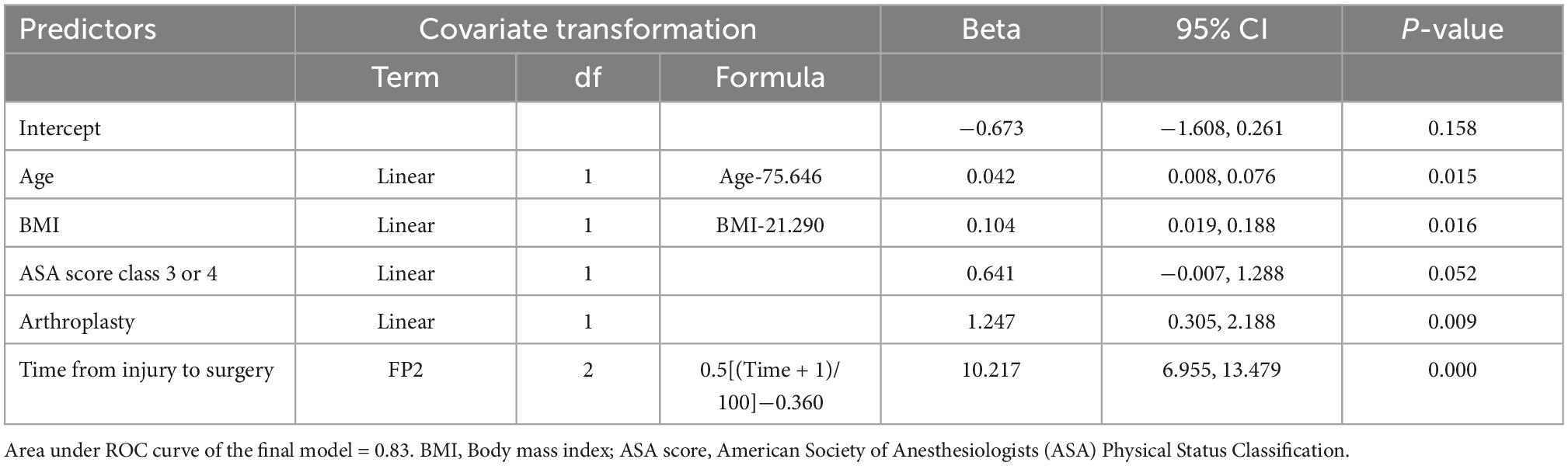
Table 3. Multivariable fractional polynomial logistic regression model for prolonged length of stay in patients with osteoporotic femoral neck fracture (final model).
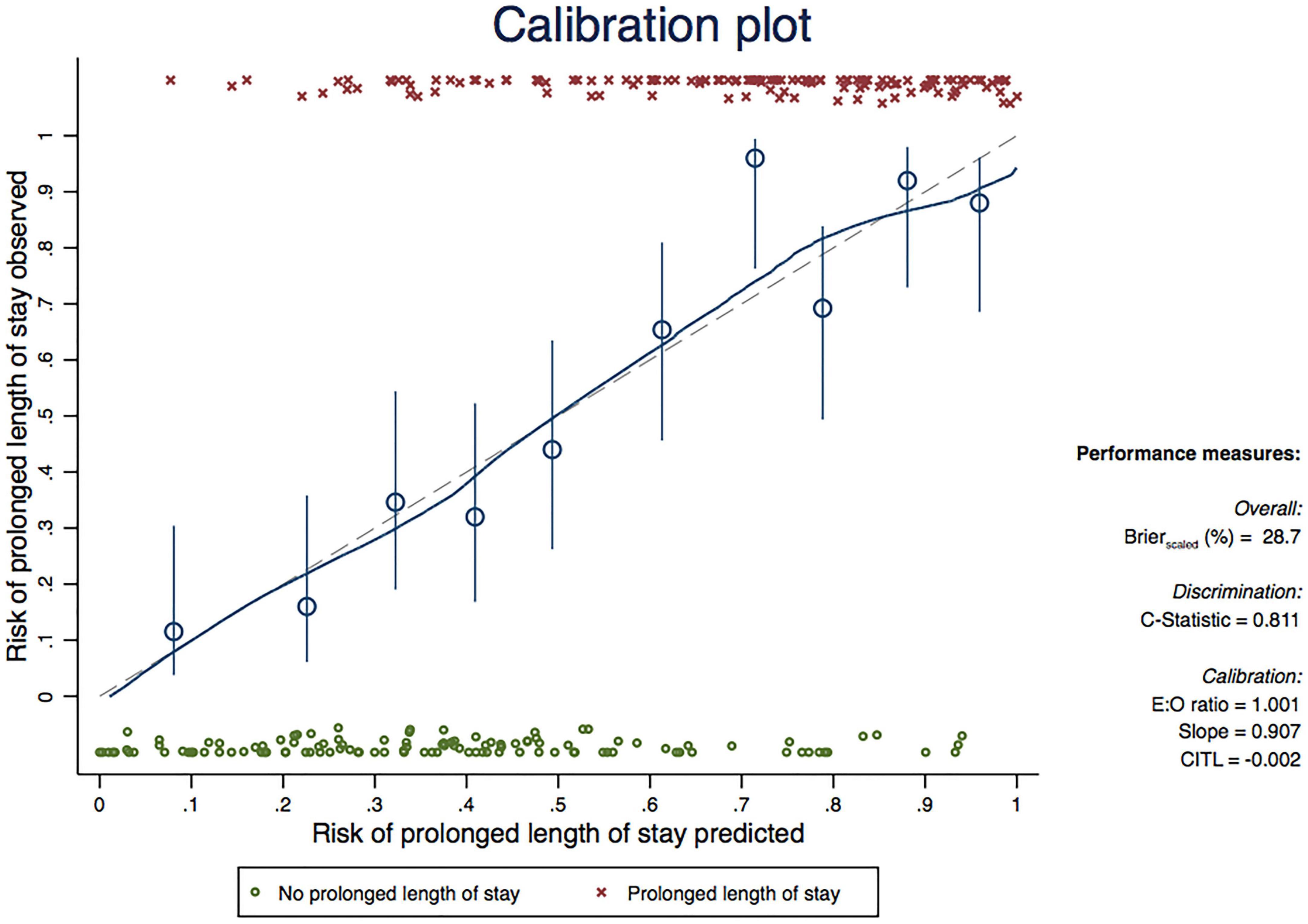
Figure 1. Calibration plot comparing observed and predicted risk of prolonged length of stay in patients with osteoporotic femoral neck fracture (based on final model).
The final model was developed into a calculator application of the predicted odds ratio and probability of prolonged LOS following osteoporotic femoral neck fracture (Supplementary Appendix 1). For example, the predicted odds ratio and probability of prolonged LOS following osteoporotic femoral neck fracture of a patient who will receive arthroplasty who is age 85, has ASA score class 3, is scheduled for surgery 4 days after falling and BMI = 25 kg/m2 are 1.820 and 0.645, respectively (Figure 2).
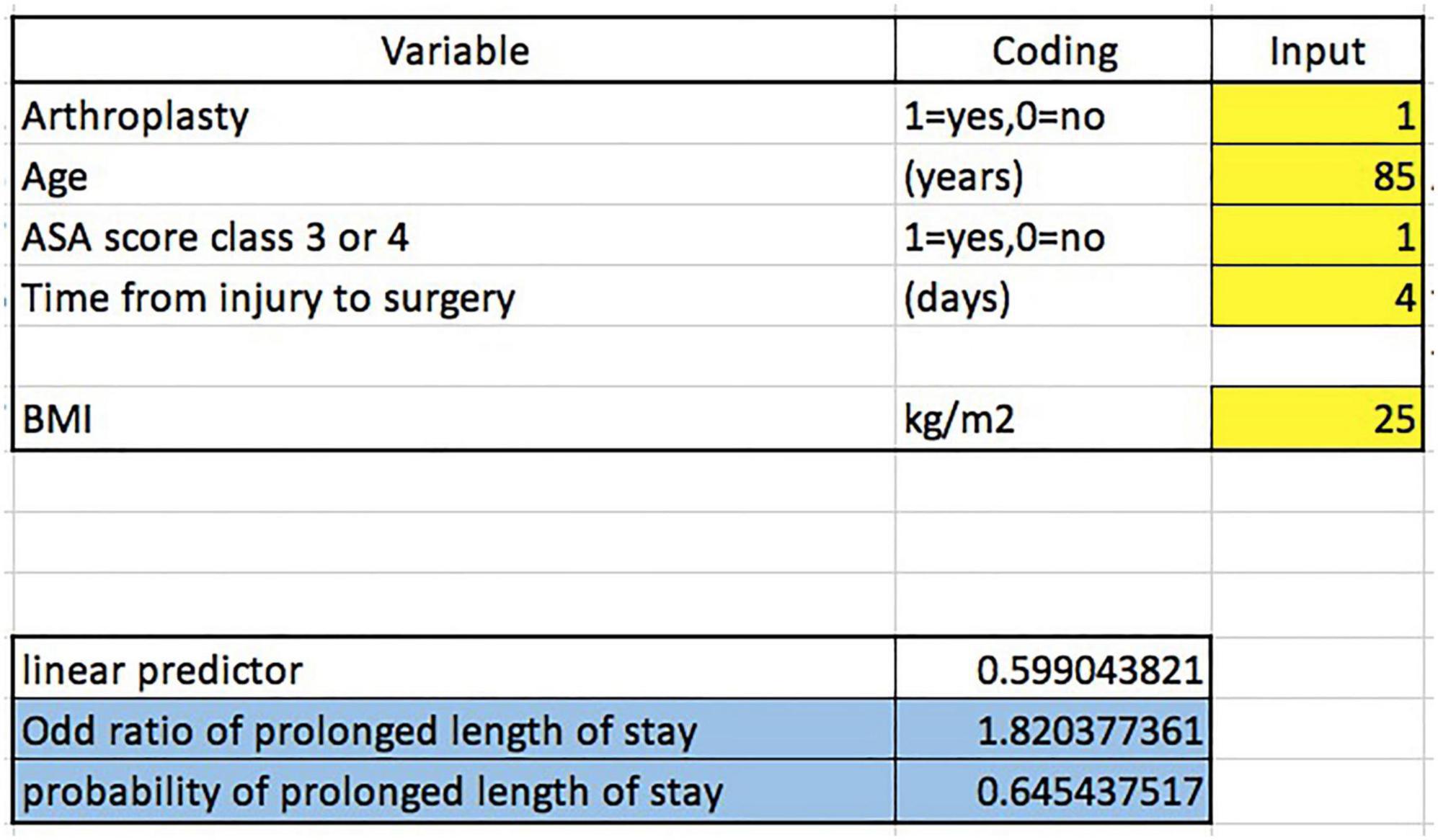
Figure 2. The predicted odds ratio and probability of prolonged LOS for an osteoporotic femoral neck fracture patient who will receive arthroplasty who is age 85, has an ASA score class three, is schedule for surgery 4 days after falling and has a BMI = 25 kg/m2.
Currently there are no models which can predict prolonged LOS in osteoporotic femoral neck fracture patients during the preoperative period. Our results demonstrate that age, BMI, ASA score class 3 or 4, arthroplasty and time from injury to surgery are strong predictors of prolonged LOS. This predictive model could help patients, their families and clinicians in making the decisions related to treatment planning, postoperative care programs and maximizing cost-effectiveness. This model has shown good to excellent discriminative performance and was well calibrated during internal validation.
Many factors have been reported to be predictors of prolonged LOS in patients with hip fractures or who are receiving hip surgeries. Those factors, similar to our study, include age, time to surgery, and ASA score as factors influencing LOS (12–14, 16, 17, 25–30). Additionally, many types of comorbidities, e.g., such as anemia, urinary disorders, cardiovascular diseases, chronic obstructive pulmonary disease, chronic cognitive impairment/dementia, and acute renal failure (12, 16, 17, 20, 31) have been reported to be predictors related to prolonged LOS. We found that ASA score alone can be used to represent the overall comorbidity situation as it is a grading system for evaluating the preoperative health of surgical patients (32). One study reported a negative association between BMI and increased LOS (18). That result is in discordance with our study which showed high BMI is related to increased LOS. There are, however, several hypotheses supporting our results. First, higher BMI is associated with metabolic syndrome, indicating an increased risk of several postoperative complications in geriatric hip fracture patients (33, 34). Second, high BMI can make the surgical approach more difficult (35) which could disturb soft tissue vascularity leading to increased time for postoperative wound care. There is evidence that patients with hip arthroplasty have 3.3 days longer hospitalization compared to patients with osteosynthesis (27) which supports our finding that performing arthroplasty increases the risk of prolonged LOS. As to the choice of implants in a femoral neck fracture, internal fixation is generally recommended in cases of non-displaced fracture as there is a lower chance of disrupting the femoral head blood supply. In displaced femoral neck fractures, arthroplasty is recommended for older individuals with displaced fractures (36). Our results show time to surgery to be the only modifiable predictor associated with prolonged LOS in patients with femoral neck fracture.
Our predictive model had good to excellent ability to differentiate osteoporotic femoral neck patients who would have prolonged LOS during their admission from patients who would have LOS <14 days with the area under the ROC curve of 0.83 (95% CI 0.77–0.88). That good to excellent discriminative performance might be explained by the appropriate fractional polynomial modeling of the predictors. Our model was also well calibrated during internal validation (optimism of −0.002, range −0.300–0.296). Compared to other predictive models, our model has a higher accuracy than the multiple linear regression model from Trunfio et al. which achieved an overall accuracy of between 0.651 and 0.718 (20) and is comparable to the model by Knoll et al. which had an accuracy of within 3 days of the true LOS for 0.758 of their series (19). There are numerous variations among predictive models in terms of inclusion criteria, candidate predictors and type of regression model that could potentially affect the accuracy of each model (19, 20).
Strengths of this study include the following. First, this model is specific to osteoporotic femoral hip fracture patients without the limitation to specific treatments as in previous models (20). Thus, patients who plan to receive multiple screw fixation can use our model to predict the probability of prolonged LOS (19). Second, the point of prediction of the calculator application based on this model can predict probability of prolonged LOS at the day of admission. The predictors, including age, BMI and ASA score of patients, can be simply included in the calculator application. Whether to perform multiple screw fixation or arthroplasty is dependent on the patient’s age and fracture configuration (36), while time from injury to surgery is dependent on the preoperative patient’s condition and the schedule of the operating theater. Using this new model, patients and their families can make decisions regarding treatment after discussion with the medical team. In cases where a prolonged length of stay is predicted and they cannot afford the cost of hospitalization, they can seek other less expensive medical institution options.
There are some limitations in this study. First, some intra- or postoperative predictors reported in previous studies (12, 18), e.g., excessive intravenous glucose and sodium chloride infusion after surgery, excessive intraoperative bleeding, postoperative acute renal failure, ventilator use >48 hours, postoperative pneumonia, and other postoperative complications, could potentially increase the discriminative performance of the model. However, we considered that the benefit from prediction of prolonged LOS at the date of admission to be more valuable than prediction of prolonged LOS made during the postoperative period. For that reason, we did not include these predictors in our model. Second, although our predictive model has good to excellent discriminative performance and well-calibrated internal validation, for generalizability, temporal and external validation of the predictive model should be assessed. Third, we could not include all types of comorbidities as candidate predictors due to the limitation of sample size.
The current predictive model, developed from preoperative predictors including age, BMI, ASA score class 3 or 4, arthroplasty and time from injury to surgery, had a good ability to differentiate between length of hospitalization less than 14 days and prolonged LOS in osteoporotic femoral neck patients. Clinical implementation of this model can be accomplished as an ease-of use calculator application which can help patients, their families and clinicians make appropriate decisions regarding treatment, postoperative care and cost-effectiveness before deciding on a definitive course of treatment.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by the Faculty of Medicine, Chiang Mai University. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
PA and WM initiated conception and design of the study, performed the collection and acquisition of data, performed the data analysis with interpretation, wrote the manuscript, and were responsible for critical revision. LK was involved in the process of data collection, acquisition, interpretation, and manuscript editing. PP performed the data analysis, interpreted the data, and edited the manuscript. PD participated in data interpretation and manuscript editing. All authors contributed to the article and approved the submitted version.
We are grateful to Dr. G. Lamar Robert, Ph.D. and Dr. Chongchit S. Robert, Ph.D., for editing the manuscript.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2022.1106312/full#supplementary-material
Supplementary Appendix 1 | Calculator application of the predicted odds ratio and probability of prolonged LOS following osteoporotic femoral neck fracture.
1. Glinkowski W, Narloch J, Krasuski K, Sliwczynski A. The increase of osteoporotic hip fractures and associated one-year mortality in Poland: 2008-2015. J Clin Med. (2019) 8:1487. doi: 10.3390/jcm8091487
2. Panula J, Pihlajamäki H, Mattila VM, Jaatinen P, Vahlberg T, Aarnio P, et al. Mortality and cause of death in hip fracture patients aged 65 or older: a population-based study. BMC Musculoskelet Disord. (2011) 12:105. doi: 10.1186/1471-2474-12-105
3. Atthakomol P, Manosroi W, Phinyo P, Pipanmekaporn T, Vaseenon T, Rojanasthien S. Predicting survival in thai patients after low impact hip fracture using flexible parametric modelling: a retrospective cohort study. J Clin Densitom. (2021) 24:603–12. doi: 10.1016/j.jocd.2021.01.007
4. Johnell O, Kanis J. An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos Int. (2006) 17:1726–33. doi: 10.1007/s00198-006-0172-4
5. Protzman R, Burkhalter W. Femoral-neck fractures in young adults. J Bone Joint Surg Am. (1976) 58:689–95.
6. Keene G, Parker M, Pryor G. Mortality and morbidity after hip fractures. BMJ. (1993) 307:1248–50. doi: 10.1136/bmj.307.6914.1248
7. Pan L, Ning T, Wu H, Liu H, Wang H, Li X, et al. Prognostic nomogram for risk of mortality after hip fracture surgery in geriatrics. Injury. (2022) 53:1484–9. doi: 10.1016/j.injury.2022.01.029
8. Nikkel L, Kates S, Schreck M, Maceroli M, Mahmood B, Elfar J. Length of hospital stay after hip fracture and risk of early mortality after discharge in New York state: retrospective cohort study. BMJ. (2015) 351:h6246. doi: 10.1136/bmj.h6246
9. Voeten S, Krijnen P, Voeten D, Hegeman J, Wouters M, Schipper I. Quality indicators for hip fracture care, a systematic review. Osteoporos Int. (2018) 29:1963–85. doi: 10.1007/s00198-018-4558-x
10. Mathew PJ, Jehan F, Kulvatunyou N, Khan M, Tang A, Gries L, et al. The burden of excess length of stay in trauma patients. Am J Surg. (2018) 216:881–5. doi: 10.1016/j.amjsurg.2018.07.044
11. Leal J, Gray AM, Prieto-Alhambra D, Arden NK, Cooper C, Javaid MK, et al. Impact of hip fracture on hospital care costs: a population-based study. Osteoporos Int. (2016) 27:549–58. doi: 10.1007/s00198-015-3277-9
12. Schneider A, Denyer S, Brown N. Risk factors associated with extended length of hospital stay after geriatric hip fracture. J Am Acad Orthop Surg Glob Res Rev. (2021) 5:e2100073. doi: 10.5435/JAAOSGlobal-D-21-00073
13. Craigven S, Rehena S, Kenny T, Howe C, Howe T, Joyce K. Shorter acute hospital length of stay in hip fracture patients after surgery predicted by early surgery and mobilization. Arch Osteoporos. (2021) 16:162. doi: 10.1007/s11657-021-01027-z
14. Raksakietisak M, Lurngnateetape A, Riansuwan K, Noiwan N, Chaiyarak C, Keawmoon K, et al. Patients with osteoporotic hip fractures: factors affecting length of hospital stay (LOS) and outcome. J Med Assoc Thai. (2012) 95:917–24.
15. Lari A, Haidar A, AlRumaidhi Y, Awad M, AlMutairi O. Predictors of mortality and length of stay after hip fractures - A multicenter retrospective analysis. J Clin Orthop Trauma. (2022) 28:101853. doi: 10.1016/j.jcot.2022.101853
16. Garcia AE, Bonnaig JV, Yoneda ZT, Richards JE, Ehrenfeld JM, Obremskey WT, et al. Patient variables which may predict length of stay and hospital costs in elderly patients with hip fracture. J Orthop Trauma. (2012) 26:620–3. doi: 10.1097/BOT.0b013e3182695416
17. Clague J, Craddock E, Andrew G, Horan M, Pendleton N. Predictors of outcome following hip fracture. Admission time predicts length of stay and in-hospital mortality. Injury. (2002) 33:1–6. doi: 10.1016/s0020-1383(01)00142-5
18. Zhong H, Wang B, Wang D, Liu Z, Xing C, Wu Y, et al. The application of machine learning algorithms in predicting the length of stay following femoral neck fracture. Int J Med Inform. (2021) 155:104572. doi: 10.1016/j.ijmedinf.2021.104572
19. Knoll OM, Lakomkin N, Shen MS, Adebayo M, Kothari P, Dodd AC, et al. A predictive model for increased hospital length of stay following geriatric hip fracture. J Clin Orthop Trauma. (2019) 10(Suppl. 1):S84–7. doi: 10.1016/j.jcot.2019.03.024
20. Trunfio T, Borrelli A, Improta G. Is it possible to predict the length of stay of patients undergoing hip-replacement surgery? Int J Environ Res Public Health. (2022) 19:6219. doi: 10.3390/ijerph19106219
21. Collins G, Reitsma J, Altman D, Moons K. Transparent reporting of a multivariable prediction model for individual prognosis or diagnosis (TRIPOD): the TRIPOD statement. BMJ. (2015) 350:g7594. doi: 10.1136/bmj.g7594
22. Concato J, Peduzzi P, Holford T, Feinstein A. Importance of events per independent variable in proportional hazards analysis. I. Background, goals, and general strategy. J Clin Epidemiol. (1995) 48:1495–501. doi: 10.1016/0895-4356(95)00510-2
23. Zhang Z. Multivariable fractional polynomial method for regression model. Ann Transl Med. (2016) 4:174. doi: 10.21037/atm.2016.05.01
24. Madley-Dowd P, Hughes R, Tilling K, Heron J. The proportion of missing data should not be used to guide decisions on multiple imputation. J Clin Epidemiol. (2019) 110:63–73. doi: 10.1016/j.jclinepi.2019.02.016
25. Husted H, Holm G, Jacobsen S. Predictors of length of stay and patient satisfaction after hip and knee replacement surgery: fast-track experience in 712 patients. Acta Orthop. (2008) 79:168–73. doi: 10.1080/17453670710014941
26. Ricci W, Brandt A, McAndrew C, Gardner M. Factors affecting delay to surgery and length of stay for patients with hip fracture. J Orthop Trauma. (2015) 29:e109–14. doi: 10.1097/BOT.0000000000000221
27. Kristan A, Omahen S, Tosounidis T, Cimerman M. When does hip fracture surgery delay affects the length of hospital stay? Eur J Trauma Emerg Surg. (2022) 48:701–8. doi: 10.1007/s00068-020-01565-0
28. Lefaivre K, Macadam S, Davidson D, Gandhi R, Chan H, Broekhuyse H. Length of stay, mortality, morbidity and delay to surgery in hip fractures. J Bone Joint Surg Br. (2009) 91:922–7. doi: 10.1302/0301-620X.91B7.22446
29. Basques B, Bohl D, Golinvaux N, Leslie M, Baumgaertner M, Grauer J. Postoperative length of stay and 30-day readmission after geriatric hip fracture: an analysis of 8434 patients. J Orthop Trauma. (2015) 29:e115–20. doi: 10.1097/BOT.0000000000000222
30. Castelli A, Daidone S, Jacobs R, Kasteridis P, Street A. The determinants of costs and length of stay for hip fracture patients. PLoS One. (2015) 10:e0133545. doi: 10.1371/journal.pone.0133545
31. Scala A, Ponsiglione A, Loperto I, Della Vecchia A, Borrelli A, Russo G, et al. Lean six sigma approach for reducing length of hospital stay for patients with femur fracture in a university hospital. Int J Environ Res Public Health. (2021) 18:2843. doi: 10.3390/ijerph18062843
32. Horvath B, Kloesel B, Todd M, Cole D, Prielipp R. The evolution, current value, and future of the American society of anesthesiologists physical status classification system. Anesthesiology. (2021) 135:904–19. doi: 10.1097/ALN.0000000000003947
33. Malik A, Quatman C, Phieffer L, Ly T, Wiseman J, Khan S. The impact of metabolic syndrome on 30-day outcomes in geriatric hip fracture surgeries. Eur J Orthop Surg Traumatol. (2019) 29:427–33. doi: 10.1007/s00590-018-2298-4
34. Cichos K, Churchill J, Phillips S, Watson S, McGwin G Jr, Ghanem E, et al. Metabolic syndrome and hip fracture: epidemiology and perioperative outcomes. Injury. (2018) 49:2036–41. doi: 10.1016/j.injury.2018.09.012
35. Atthakomol P, Oflazoglu K, Eberlin K, Winograd J, Chen N, Lee S. Obesity status is a risk factor for secondary surgery after neurolysis, direct nerve repair or nerve grafting in traumatic brachial plexus injury: a retrospective cohort study. BMC Surg. (2020) 20:73. doi: 10.1186/s12893-020-00737-4
Keywords: osteoporosis, femoral neck fracture, predictive model, length of hospital stay (LOS), prolonged
Citation: Manosroi W, Koetsuk L, Phinyo P, Danpanichkul P and Atthakomol P (2023) Predictive model for prolonged length of hospital stay in patients with osteoporotic femoral neck fracture: A 5-year retrospective study. Front. Med. 9:1106312. doi: 10.3389/fmed.2022.1106312
Received: 23 November 2022; Accepted: 20 December 2022;
Published: 11 January 2023.
Edited by:
Vered Hermush, Technion – Israel Institute of Technology, IsraelReviewed by:
Revital Feige Gross Nevo, Independent Researcher, Petach Tikva, IsraelCopyright © 2023 Manosroi, Koetsuk, Phinyo, Danpanichkul and Atthakomol. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Pichitchai Atthakomol,  p.atthakomol@gmail.com
p.atthakomol@gmail.com
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.