- 1Department of Ultrasound, Shengjing Hospital of China Medical University, Shenyang, China
- 2Department of Urology, The First Hospital of China Medical University, Shenyang, China
- 3Key Laboratory of Health Ministry for Congenital Malformation, Department of Pediatric Surgery, Shengjing Hospital of China Medical University, Shenyang, China
- 4Department of Pediatric Surgery, Shengjing Hospital of China Medical University, Shenyang, China
Background: Congenital perineal hamartomas are rare, and reports of prenatal ultrasound diagnosis are limited. Perineal hamartomas are usually associated with other structural malformations, which complicate the therapeutic regime.
Case presentation: We report a case of perineal hamartomas associated with rectal duplication in a female fetus. A review of the literature on similar cases was also presented. A fetus was first diagnosed with a perineal mass at 33 weeks of gestation using ultrasound examination in our hospital. Two-dimensional ultrasonography showed a hyperechoic mass resembling a scrotum in the perineum of the fetus. The pedicle connected the mass to the fetal anus. The masses were excised after birth, and perineal hamartomas were confirmed by pathological diagnosis. Rectal duplication, an associated malformation, was found during the surgery. The rectal duplication cyst was removed at the same time.
Conclusion: Congenital perineal masses are rare and are usually associated with urogenital and anorectal malformations. Prenatal ultrasound should be used to assess the position and relationship between the mass and perineal organs, and to exclude other combined deformities.
Introduction
According to available reports, congenital perineal masses, including lipomas, hamartomas, and hemangiomas, are rare (1). Although most of them are benign, their unique location and rapid growth characteristics make complete surgical resection the best choice of treatment. Many perineal masses present as ambiguous genitalia that interfere with distinguishing the sex of the fetuses (2). In addition, perineal masses are associated with anorectal and urogenital malformations, which complicate the therapeutic regime (3). Herein, we report a case in which a female fetus was diagnosed with congenital perineal masses that resembled male genital organs on prenatal ultrasound examination. These masses were verified as hamartomas by pathological examination after birth. Rectal duplication, an associated malformation, was found and removed at the same time. Rectal duplication cysts are rare (only 4%) among the congenital gastrointestinal cysts (4), which are described as congenital spherical or tubular cysts located in the presacral space (5).
Case presentation
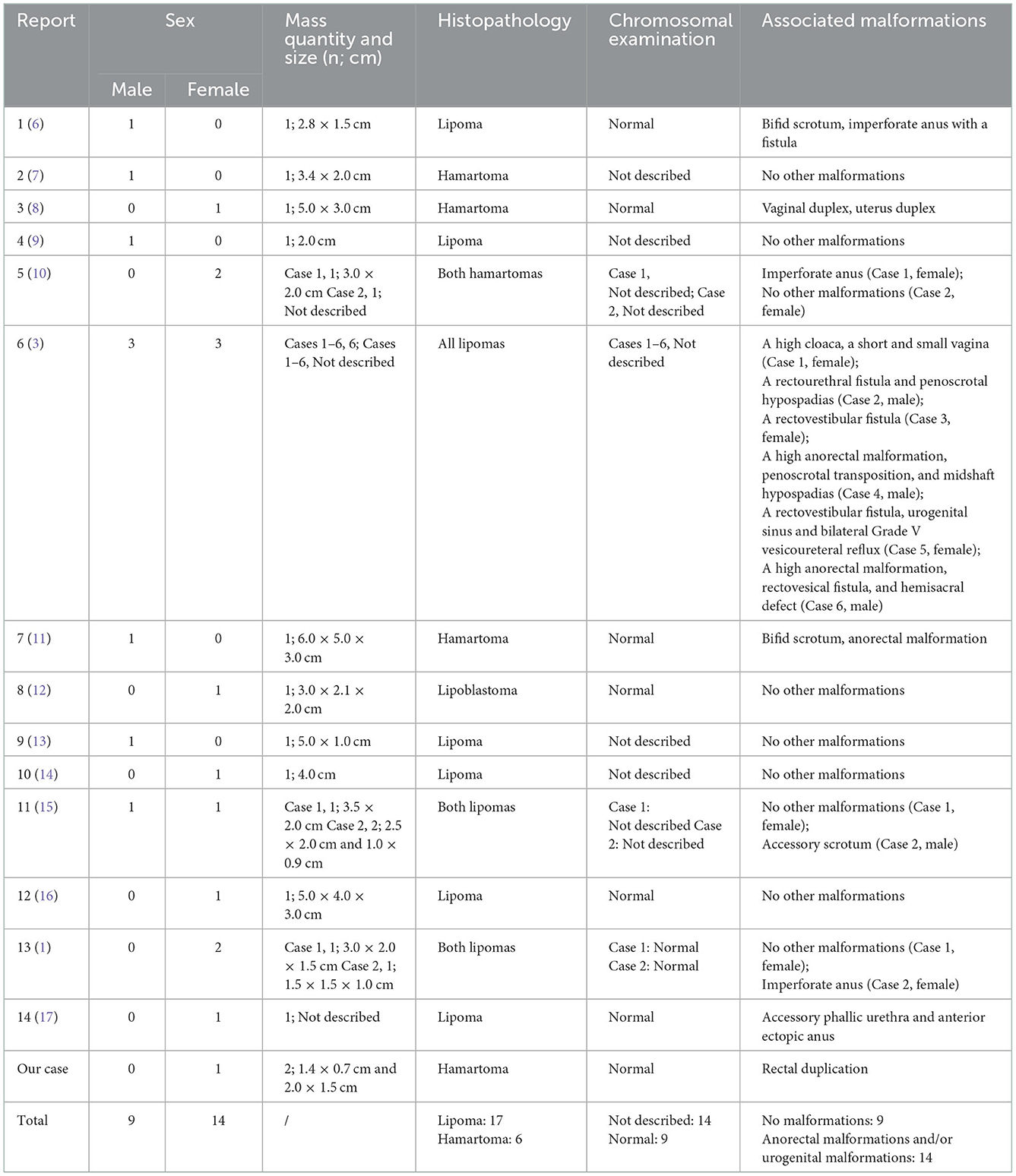
A 34-year-old woman, gravida 2, para 1, was transferred to Shengjing hospital of China Medical University at 33 weeks of gestation. At 24 weeks of pregnancy, the patient was informed that she was pregnant with a boy during an ultrasound examination at the district hospital. However, during the 32-week ultrasound examination, the doctor found abnormalities in the perineum of the fetus. A detailed ultrasound examination was performed at 33 weeks in Shengjing hospital, and a perineal scan revealed that the fetus was female, not male. Two-dimensional ultrasound showed a hyperechoic mass (1.7 × 1.2 cm) resembling a scrotum in the perineum of the fetus (Figure 1A). The pedicle connected the mass to fetal skin around anus. Dynamic observation revealed another small hyperechoic mass (0.8 × 0.7 cm) protruding from the fetal anus, connecting to the other end of the pedicle. The masses floated in the amniotic fluid with no obvious blood flow on color Doppler flow imaging (CDFI). Three-dimensional ultrasound showed scrotum-like masses and their relationship with other organs (Figure 1B). The mother underwent amniocentesis, and no abnormalities were found on a comparative genomic hybridization (CGH) array.
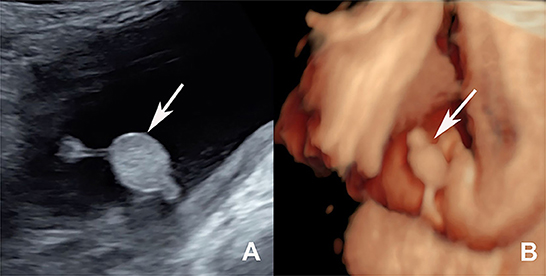
Figure 1. (A) Two-dimensional ultrasound showed a hyperechoic mass resembling a scrotum (the white arrow shows) in the perineum of the fetus. (B) Three-dimensional ultrasound showed the scrotum-like masses (the white arrow shows) and their relationship with other organs vividly at 33 weeks gestation.
A female neonate was delivered, weighing 3,240 g at GA 40 + 2 weeks. Her Apgar scores were 10 and 10 at 1 and 5 min, respectively. Perineal examination revealed two soft spherical masses protruding from the patient's anus and connected by a pedicle. The masses were 2.5 × 1.5 cm and 1.4 × 0.7 cm in size (Figure 2A). The neonate underwent an abdominal ultrasound examination, and no other abnormalities were found. We also performed a postnatal ultrasound on the perineal masses. Sonography showed two well-defined hyperechoic masses connected by a pedicle, and CDFI detected blood flow signals in the masses. The results of the sacrococcygeal magnetic resonance imaging (MRI) were normal. Surgery was performed under general anesthesia 1 day after birth. The masses were originated from the peri-anal skin at 4:00 in lithotomy position, and the anal sphincter was not involved. Histopathological examination of the masses suggested hamartomas composed of hyperplastic lymph vessels and adipose tissues (Figure 2B). After the masses were removed, a cavity was discovered along the posterior rectal wall (Figure 2C). The contrast agent showed an irregular cystic mass connected to the posterior wall of the rectum, and rectal duplication was suspected (Figure 2D). An en bloc excision of the cystic mass and the posterior wall of the rectum was performed. Rectal duplication was confirmed by histopathological examination. At the time of writing this report, the patient was 2.5 years old, and recovered well after surgery without other abnormalities.
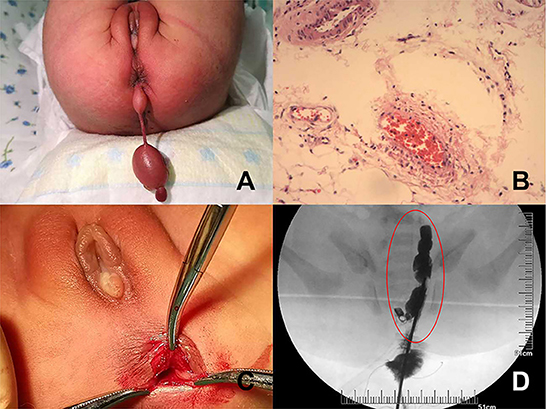
Figure 2. (A) Gross appearance of the perineal masses at birth. (B) The histological examination results of the perineal masses show hyperplastic lymph vessels and adipose tissue that conformed to hamartomas. (C) After the mass was removed, a cavity can be seen clinging to the posterior wall of the rectum. (D) Under contrast agent, the radiography shows an irregular cystic mass located in the presacral space.
Discussion
Perineal masses include lipomas, hamartomas, hemangiomas, and other types of tumors (1). Perineal hamartomas are rarely found in the fetus; however, their prenatal ultrasound appearance is not significantly different from other benign perineal masses like lipomas. Perineal masses often interfere with the identification of the sex of the fetus and are sometimes misdiagnosed as ambiguous genitalia (AG) (2). AG is a morphological diagnosis defined as genitalia not typical of a male or female. Findings mimicking AG, such as penoscrotal anomalies, anorectal malformations, and perineal tumors, may prevent accurate identification of the fetal sex (6). In our case, the perineal hamartomas mimicked the male scrotum, thus confusing sex diagnosis. As a result of the misdiagnosis, the perineal mass was missed in the second-trimester ultrasound examination. After careful scanning, we found that the fetus had normal female external genitalia, and the so-called “scrotum” originated from the fetus' anus. Thus, prenatal examination of the genitalia should be performed carefully to avoid missed diagnosis of fetal sex and perineal mass.
Only a few studies have reported congenital perineal masses. We found 23 similar cases (including our case) are summarized in Table 1. Histopathological diagnoses included lipomas (17/23) and hamartomas (6/23). The chromosomal examinations were normal in 8 cases and 14 cases were not described. In our case, the chromosomal examination was normal. Fourteen cases (60.9%) had urogenital or anorectal defects, including imperforate anus (1, 6, 10), rectovestibular fistula, rectovesical fistula, rectourethral fistula, urogenital sinus, penoscrotal hypospadias, penoscrotal transposition, vesicoureteral reflux (3), vaginal duplex, uterus duplex (8), bifid scrotum (6, 11), accessory scrotum (15), and so on. Therefore, the appearance of a perineal mass might serve as a marker for predicting anorectal defects or urogenital defects. Most perineal masses are benign tumors that can be radically excised; however, surgery will be complicated if there are other associated malformations. Therefore, the prenatal detection of other associated malformations is critical for prognostic assessment. In our case, we performed a comprehensive scanning of the perineal organs. There were no other abnormalities in utero on comprehensive sonographic scanning and no other abnormalities on MRI after birth. However, rectal duplication was observed during postnatal surgery. This suggests that prenatal ultrasound examination was limited to the examination of the perineal organs and structures. Pediatric surgeons should be aware of the possibility of other associated malformations, even if prenatal examinations are normal.
Here, we report a case of perineal hamartomas associated with rectal duplication, for the first time. Rectal duplication is uncommon. Patients with rectal duplication present with chronic constipation, acute urine retention, and other clinical manifestations (18). In our case, the perineal masses and rectal duplication were removed simultaneously 1 day after birth, and the neonate was followed up to 2.5 years of age without obvious symptoms.
The embryogenesis of congenital perineal masses can be poorly interpreted. However, congenital perineal masses can destroy the continuity of the sacrococcygeal region, leading to combined defects of the anorectal and genitourinary organ systems (15, 19). In addition, since the embryologic development of the urogenital sinus, rectum, anus, and perineum are closely related, the associated anomalies in cases with perineal masses can be explained (8).
Three-dimensional ultrasound plays an important role in auxiliary diagnosis. We used the three-dimensional surface imaging technology to vividly display the perineal masses, which also clearly showed the origin and location of the mass and its relationship with other organs. Three-dimensional ultrasound is also conducive to enhancing diagnostic confidence and facilitating better communication with patients.
Conclusion
In conclusion, prenatal ultrasound examination plays a leading role in distinguishing the origin of perineal hamartomas and evaluating the associated abnormalities. This could provide an efficient basis for clinical counseling and postnatal treatment.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding authors.
Ethics statement
Written informed consent was obtained from the individual(s), and minor(s)' legal guardian/next of kin, for the publication of any potentially identifiable images or data included in this article.
Author contributions
YZ and LC were responsible for the original draft preparation and editing. MZ, WM, and YZ participated in data collection. LC, DW, and ZY were responsible for conceptualization, manuscript editing, and manuscript review. All authors have read and approved the final manuscript.
Funding
This study was supported by the National Natural Science Foundation of China (Nos. 82272022 and 82173372) and National Key Research and Development Program (2021YFC2701003).
Acknowledgments
We thank the Prenatal Diagnosis Center of Sheng Jing Hospital, China Medical University.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Guerra-Junior G, Aun AM, Miranda ML, Beraldo LP, Guimaraes Moraes S, Baptista MT, et al. Congenital perineal lipoma presenting as ambiguous genitalia. Eur J Pediatr Surg. (2008) 18:269–71. doi: 10.1055/s-2008-1038366
2. Achermann JC, Eugster EA, Shulman DI. Ambiguous genitalia. J Clin Endocrinol Metab. (2011) 96:33A, 4A. doi: 10.1210/jcem.96.3.zeg33a
3. Wester T, Rintala RJ. Perineal lipomas associated with anorectal malformations. Pediatr Surg Int. (2006) 22:979–81. doi: 10.1007/s00383-006-1800-y
4. Castro-Pocas FM, Araujo TP, Silva JD, Goncalves VS. Endoscopic ultrasonography and rectal duplication cyst in an adult. Endosc Ultrasound. (2017) 6:336–9. doi: 10.4103/2303-9027.190918
5. Anastasiadou S, Tekkis P, Kontovounisios C. An unusual rectal duplication cyst. Surg Case Rep. (2019) 5:75. doi: 10.1186/s40792-019-0631-8
6. Inde Y, Terada Y, Ikegami E, Sekiguchi A, Nakai A, Takeshita T. Bifid scrotum and anocutaneous fistula associated with a perineal lipomatous tumor complicated by temporary bilateral cryptorchidism in utero mimicking ambiguous genitalia: 2-D/3-D fetal ultrasonography. J Obstet Gynaecol Res. (2014) 40:843–8. doi: 10.1111/jog.12232
7. Upadhyaya P, Spilde TL, Tsao K, Ostlie DJ. Anorectal hamartoma in a neonate: a unique anorectal mass. J Pediatr Surg. (2007) 42:E31–3. doi: 10.1016/j.jpedsurg.2007.06.021
8. Liu SP, Yang JX, Cao DY, Lang JH. Congenital perineal mass with cervovaginal duplication: a case report and literature review. J Pediatr Adolesc Gynecol. (2014) 27:102–3. doi: 10.1016/j.jpag.2013.06.014
9. Bataille D, Donner C, Cassart M, Pardou A, Nagy N, Van Hoorde E, et al. Perineal lipoma in a newborn boy–a case report. Eur J Pediatr Surg. (2007) 17:136–8. doi: 10.1055/s-2007-965010
10. Chu SM, Ming YC, Chao HC, Luo CC. An accessory labioscrotal fold associated with anorectal malformation in female neonates. J Pediatr Surg. (2009) 44:E17–9. doi: 10.1016/j.jpedsurg.2008.12.028
11. Ramzisham AR, Thambidorai CR. Perineal hamartoma with accessory scrotum, anorectal anomaly, and hypospadias-a rare association with embryological significance: case report. Pediatr Surg Int. (2005) 21:478–81. doi: 10.1007/s00383-005-1416-7
12. Ahn KH, Boo YJ, Seol HJ, Park HT, Hong SC, Oh MJ, et al. Prenatally detected congenital perineal mass using 3D ultrasound which was diagnosed as lipoblastoma combined with anorectal malformation: case report. J Korean Med Sci. (2010) 25:1093–6. doi: 10.3346/jkms.2010.25.7.1093
13. Kim SH, Cho YH, Kim HY. Does this baby have a tail?: a case of congenital isolated perineal lipoma presenting as human pseudo-tail. Ann Surg Treat Res. (2016) 90:53–5. doi: 10.4174/astr.2016.90.1.53
14. Ogasawara Y, Ichimiya M, Nomura S, Muto M. Perineal lipoma in a neonate. J Dermatol. (2001) 28:165–7. doi: 10.1111/j.1346-8138.2001.tb00113.x
15. Sule JD, Skoog SJ, Tank ES. Perineal lipoma and the accessory labioscrotal fold: an etiological relationship. J Urol. (1994) 151:475–7. doi: 10.1016/S0022-5347(17)34996-0
16. Wax JR, Pinette MG, Mallory B, Carpenter M, Winn S, Cartin A. Prenatal sonographic diagnosis of a perineal lipoma. J Ultrasound Med. (2010) 29:1257–9. doi: 10.7863/jum.2010.29.8.1257
17. Mahalik SK, Mahajan JK, Sodhi KS, Garge S, Vaiphei K, Rao KL. Rare association in a female DSD case of phallus, accessory phallic urethra, perineal lipoma and anterior ectopic anus. J Pediatr Urol. (2013) 9:e39–42. doi: 10.1016/j.jpurol.2012.07.002
18. Rajah S, Ramanujam TM, Anas SR, Jayaram G, Baskaran P, Ganesan J, et al. Duplication of the rectum: report of four cases and review of the literature. Pediatr Surg Int. (1998) 13:373–6. doi: 10.1007/s003830050343
Keywords: congenital mass, perineal mass, hamartoma, ultrasound, prenatal
Citation: Zhang Y, Zhang M, Ma W, Yuan Z, Wang D and Chen L (2023) Congenital perineal hamartomas with rectal duplication: A case report. Front. Med. 9:1066559. doi: 10.3389/fmed.2022.1066559
Received: 11 October 2022; Accepted: 27 December 2022;
Published: 12 January 2023.
Edited by:
Zaleha Abdullah Mahdy, National University of Malaysia, MalaysiaReviewed by:
Muluwas Amentie Zelka, Addis Ababa University, EthiopiaCornelius E. Sloots, Sophia Children's Hospital, Netherlands
Copyright © 2023 Zhang, Zhang, Ma, Yuan, Wang and Chen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Dajia Wang,  ZGFqaWF3YW5nY211QDE2My5jb20=; Lizhu Chen,
ZGFqaWF3YW5nY211QDE2My5jb20=; Lizhu Chen,  YWxpY2VjbHpAc2luYS5jb20=
YWxpY2VjbHpAc2luYS5jb20=
†These authors have contributed equally to this work
 Yixin Zhang
Yixin Zhang Mo Zhang
Mo Zhang Wei Ma3
Wei Ma3 Zhengwei Yuan
Zhengwei Yuan