- 1Department of Women & Children’s Health, School of Life Course & Population Sciences, King’s College London, London, United Kingdom
- 2School of Medicine and Population Health, Faculty of Health, University of Sheffield, Sheffield, United Kingdom
- 3GKT School of Medical Education, Faculty of Life Sciences & Medicine, King’s College London, London, United Kingdom
- 4Department of Population Health Sciences, School of Life Course & Population Sciences, King’s College London, London, United Kingdom
- 5The RESILIENT Study Patient & Public Involvement & Engagement Advisory Group, United Kingdom
- 6School of Nursing, Midwifery and Health Systems, College of Health and Agricultural Sciences, University College Dublin, Dublin, Ireland
- 7The Policy Institute, Faculty of Social Science & Public Policy, King’s College London, London, United Kingdom
- 8Department of Social Sciences, College of Health, Science and Society, University of the West of England Bristol, Bristol, United Kingdom
- 9The RESILIENT Study Technical Advisory Group, United Kingdom
- 10The Dartmouth Institute for Health Policy & Clinical Practice, Geisel School of Medicine, Dartmouth College, Hanover, NH, United States
- 11Department of Twin Research & Genetic Epidemiology, School of Life Course & Population Sciences, King’s College London, London, United Kingdom
- 12The RESILIENT Study Group, United Kingdom
- 13School of Psychology, Faculty of Health, Liverpool John Moores University, Liverpool, United Kingdom
Problem and background: During the COVID-19 pandemic, there was substantial reconfiguration of maternity care services, affecting both users and healthcare providers (HCPs), in the United Kingdom (UK) and globally.
Aim: To further our understanding of the impact of maternity service reconfigurations in the UK, from the perspective of maternity HCPs.
Methods: Scopus, MEDLINE, EMBASE, CINAHL, PsycINFO and the Cochrane COVID Study Register were searched for relevant studies reporting qualitative data from the UK, published in English between 01 June 2021 and 30 September 2023. Qualitative data on HCPs’ experiences of maternity care reconfiguration during the pandemic were extracted from 15 studies. Data were subjected to thematic synthesis according to key service reconfigurations.
Results: Nine themes were identified: Care-seeking and Care Experience: Changes to existing care, Limitations placed on the partner, Mental health and lack of support networks, and Barriers to successful implementation of reconfiguration strategies; Virtual Care: Impact on quality of care, Increased convenience and flexibility, and Digital exclusion; and Ethical Future of Maternity Care Services: Optimising patient care, and Service users and staff as the driving force for change. No studies reported on the concepts of Self-monitoring or COVID-19 vaccination.
Discussion and conclusion: The review findings highlight HCPs’ views of the need for greater inclusion of partners, choice of virtual or in-person care for women and birthing people; and a need for co-designed services for future policy-making.
1 Introduction
During the COVID-19 pandemic, maternity care was provided throughout as essential within National Health Service (NHS) provision (3). Nevertheless, substantial service reconfigurations were made.
Guidance from the Royal College of Obstetricians and Gynaecologists [RCOG] and the Royal College of Midwives [RCM] was published frequently, often updated weekly (1). Guidance aimed to: prevent transmission of the SARS-CoV-2 virus, adapt services to increased demand in acute care settings, and respond to heightened maternal vulnerability to severe COVID-19 associated with pregnancy (1). For women and birthing people, service reconfigurations included: a shift to virtual care provision for at least some antenatal care visits (2–5); fewer antenatal visits (20); alterations in some diagnostic care pathways (6, 7); exclusion of fathers, partners, and non-gestational parents from many aspects of care (3, 8–10); and restriction on choice of place of birth (11). Other changes to maternity services included: new satellite ‘Nightingale’ hospitals, reorganisation of existing hospital facilities, redeployment of maternity staff to other departments, and encouragement of newly-retired staff to return to work (2, 12, 13). Throughout the pandemic, maternity healthcare providers (HCPs) continued to work in high-risk areas, facing new challenges and rapid changes.
In their qualitative thematic synthesis of global literature, which included 17 studies published between 01 January 2020 and 13 June 2021, Flaherty et al. explored HCPs’ experiences of providing maternity care during the pandemic, identifying positive and negative impacts (14). Inconsistencies and recurrent changes in guidelines left HCPs feeling confused and unable to provide safe and effective care (14). HCP workload increased, and as the pandemic continued for longer than anticipated, acute changes became chronic. Staff burnout became evident, relating to staff shortages (15), the burden of additional tasks required to deliver new care practices, and the need for longer antenatal and postnatal appointments to address pregnant women and birthing people's questions and anxiety (14). Simultaneously, maternity HCPs reported enhanced camaraderie and bonding with colleagues, which led to a more positive working environment (14).
As the pandemic resolves, HCPs have reflected and considered the value of pandemic-related changes to maternity care (23). Thus, we updated the previous relevant systematic review (14), with literature published to September 2023, to inform future development and organisation of maternity services.
2 Methods
The review forms part of the RESILIENT study: Post pandemic planning for maternity care for local, regional, and national maternity systems across the four nations (NIHR134293) (16). The review was registered with PROSPERO [CRD42022355948] (17) and adheres to the PRISMA 2020 statement (18) (Supplementary Table S1).
2.1 Inclusion criteria
We followed the SPIDER (Sample, Phenomenon of Interest, Design, Evaluation, and Research Type) framework used in the original review (14).
Our sample included maternity HCPs directly involved in provision of maternity care during the COVID-19 pandemic. A range of professions were captured, including, but not limited to midwifery, nursing, and obstetrics. Whilst we sought studies published globally, in this review, we have restricted our sample to UK-based studies (see Search Strategy and Selection section for further detail). The phenomenon of interest was HCP experience of maternity care provision during the pandemic, including all antenatal care (except abortion), labour and childbirth, and up to six months postpartum. Care in all settings was considered. Qualitative study designs of interest included: descriptive, exploratory, and interpretive studies; ethnographic studies; observational or mixed-methods studies in which qualitative data had been extracted separately; survey designs with open-text questions when significant qualitative data had been collected and formally analysed; linguistic studies; and studies of public discourse. Only published literature was included.
Literature published between 01 June 2021 and 30 September 2023 [building on the previous review's (14) search, 01 January 2020 to 13 June 2021] was sought. The search strategy was restricted to English language.
2.2 Search strategy and selection
Systematic searches were undertaken of the electronic databases of Scopus, MEDLINE (Online counterpart of MEDLARS MEDical Literature Analysis and Retrieval System), EMBASE (Excerpta Medica dataBASE), CINAHL (Cumulative Index of Nursing and Allied Health Literature), PsycINFO and the Cochrane COVID Study Register. The search terms and keywords used in the Flaherty et al. review (14) were adopted (Supplementary Table S2).
EndNote Reference Manager was used to clean search result duplicates, and citations were uploaded to the Rayyan web-based systematic reviewing tool. Team members (TD, LP, GH, MW, SAS, HDM, PvD, LAM) independently screened each title and abstract, followed by full-text review. After each screening stage, disagreements were resolved through discussion with the wider team. Given the large number of studies meeting inclusion criteria, and the focus of RESILIENT on maternity care in the UK, a decision was made prior to data extraction to sub-divide the review by population of interest (women and birthing people or HCPs) and geography [UK, other high-income countries (HICs), or low- and middle-income countries]. The remaining studies have (19) or will be synthesised separately.
2.3 Data extraction and synthesis
Data were extracted independently by two reviewers (EB, YP) into a pre-designed Microsoft Excel data extraction sheet, and checked by wider-team members during regular discussions. Extracted information included: characteristics of studies (e.g., reference, aims, setting, and dates of data collection) and participants (e.g., number, setting), data collection method, details of analyses, and themes identified, all taken from the results sections of included papers. Then, each paper was imported into NVivo qualitative research software for coding and synthesis of Discussion sections. Of note, Results sections were not coded to avoid replicating codes/themes and rendering logic circular.
In line with the previous reviews (7, 14), methodological quality was assessed independently by two team members (EB, YP) and checked for correctness by other authors, using an adapted version of a 12-item EPPI-Centre (Evidence for Policy and Practice Information and Co-ordinating Centre) tool which captures information on the reliability and validity of study methods and reporting, for qualitative evidence synthesis (20). Data were included for synthesis, regardless of quality, to provide relevant ‘views/experiences’ data. We did, however, interrogate our final results to ensure that inclusion of low-quality papers, if any, did not compromise the integrity of resulting themes (that is, the removal of codes derived from low quality studies was not found to affect the overall set of derived themes).
Thematic Synthesis (21) was undertaken based on a set of a priori concepts which address RESILIENT aims: (1) Care-seeking and care experience, (2) Virtual care, (3) Self-monitoring, (4) COVID-19 vaccination, and (5) Ethical future of maternity care services. Extracted data from each study were aligned with one or more of these key concepts, then data under each concept were coded, and descriptive themes generated inductively. Data were synthesised independently by two reviewers (EB, YP), to ensure cohesion and congruity in coding, with regular discussion to resolve any conflicts and agree on derived themes.
3 Results
3.1 Search and selection
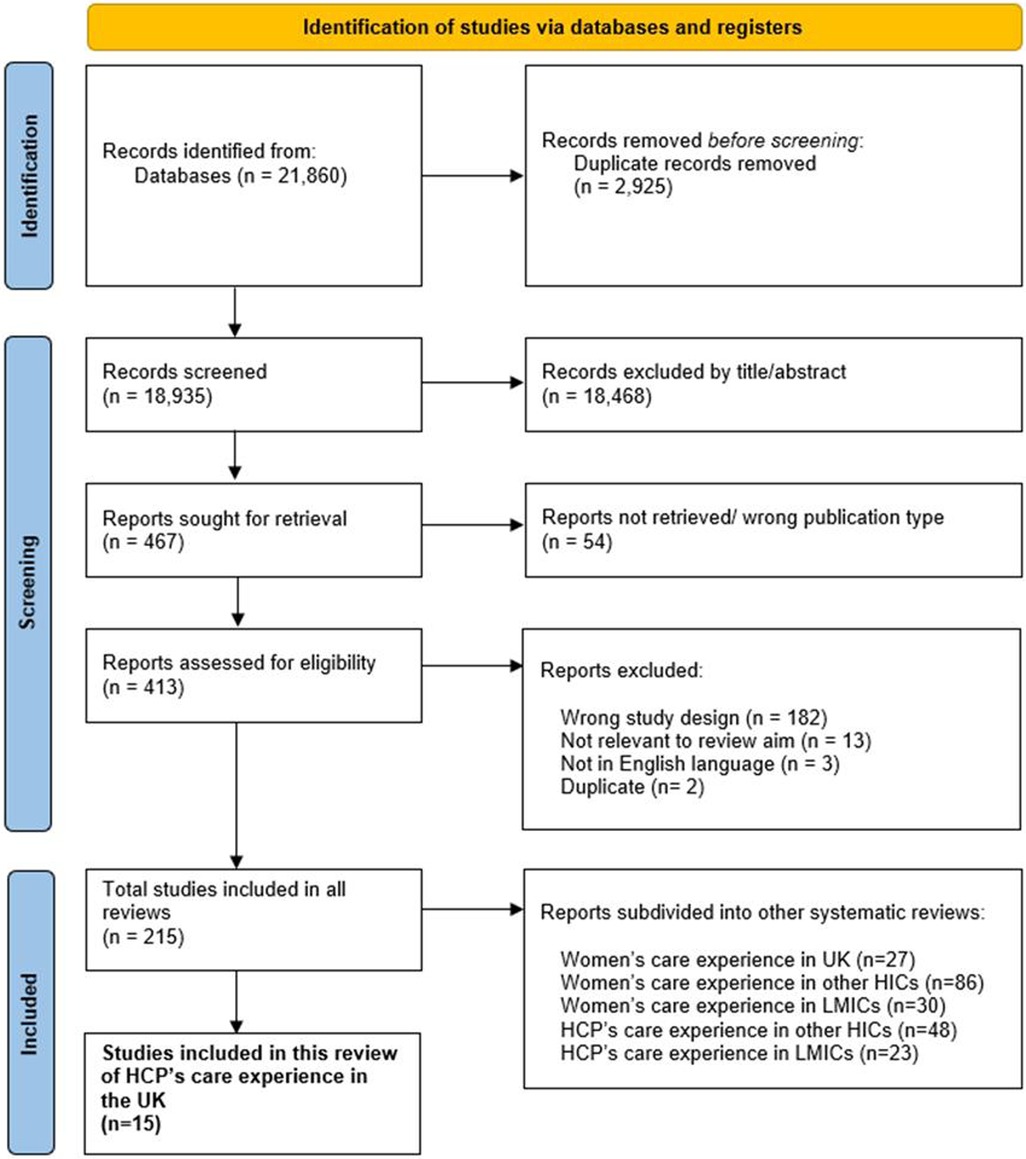
Figure 1 illustrates the search and selection process (18). The initial literature search yielded 21,860 records. Records were removed if they were: duplicates (n = 2,925); ineligible at title/abstract screening (n = 18,468); could not be retrieved (n = 54); or were ineligible at full-text review (n = 200; see Figure 1 for reasons). Thereafter, 215 records met inclusion criteria, of which 15 studies of UK HCPs’ experiences of delivering maternity care during the pandemic are reported here (4, 5, 22–34).
3.2 Description of included studies
The 15 included studies were exclusively UK-based, apart from one; this compared care between the UK and the Netherlands (31), and presented data all together. One study (18) presented data from maternity and children's healthcare professionals, commenting on each set of professionals.
There were 940 participants, with additional unspecified numbers from 224 maternity units (23, 30) and eight maternity care policy organisations (30). Data collection ranged from February 2020 to November 2021, extended by 11 months beyond the original review (14). Study methodology varied: semi-structured interviews (n = 8) (5, 22, 24–26, 28, 29, 34), semi-structured interviews alongside analysis of policy and guidance documents (n = 2) (30, 31), mixed-method survey with free-text analysis (n = 3) (23, 27, 32), both interviews and a mixed-method survey (n = 1) (4), and a focus group with midwives (n = 1) (33). For data analysis, most studies utilised thematic analysis (n = 7) (22, 25–28, 32, 33); other methodologies included: content analyses (n = 1) (30), descriptive analysis (n = 2), 23,34 framework analyses (n = 2) (4, 31), or grounded theory analyses (n = 3) (5, 24, 29). For detailed characteristics of included studies and their key findings, see Supplementary Table S3.
3.3 Quality assessment
Study quality varied. Eight studies met all 12 quality criteria (5, 22–24, 29, 31, 33, 34); two studies met 11/12 criteria (27, 30) as they did not actively involve participants in the design and conduct of the study; one study met 10/12 criteria (4), two studies met 9/12 criteria (26, 28), one study met 8/12 criteria (25), and one study met 7/12 criteria (32). As such, all studies were deemed to be of moderate-high quality; for details, see Supplementary Table S4.
3.4 Synthesis and findings
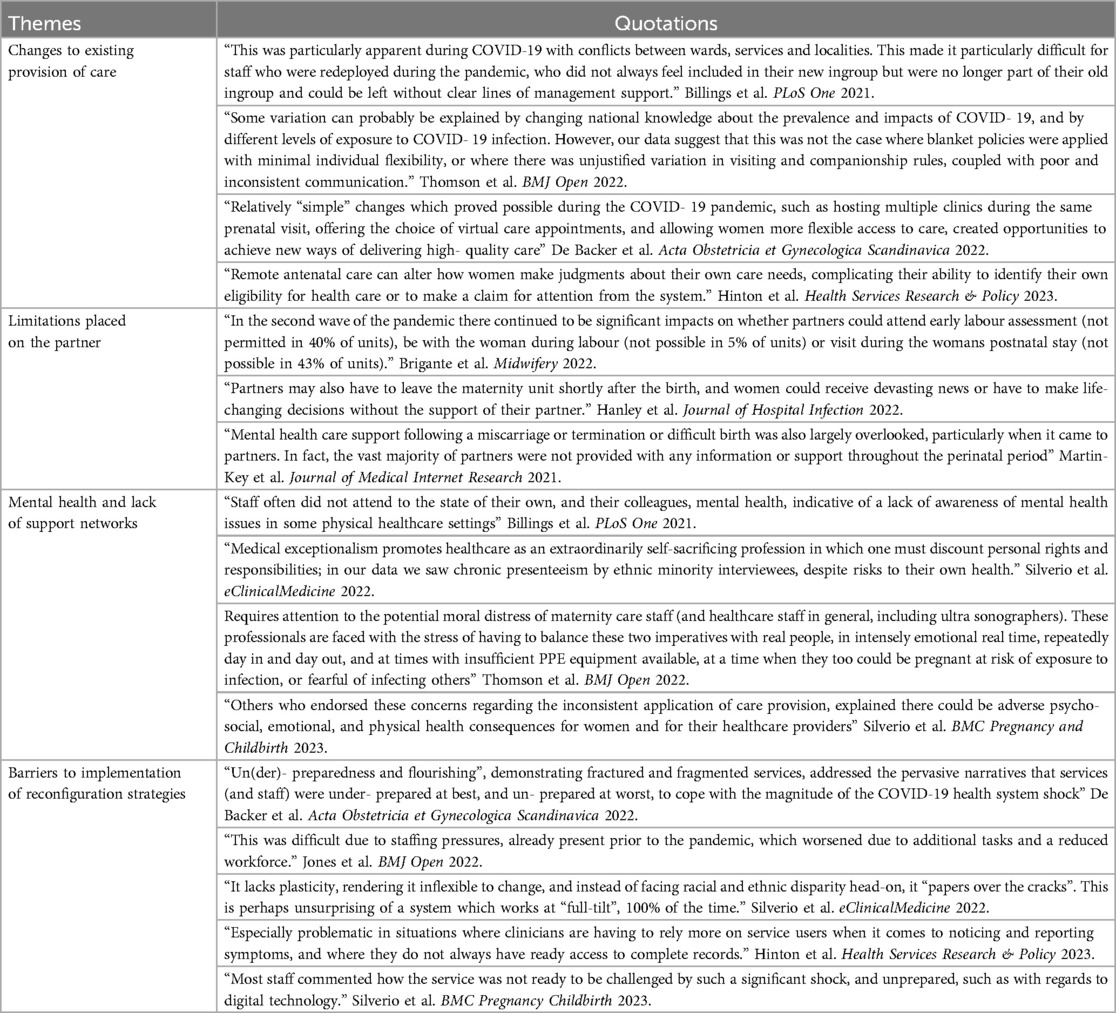
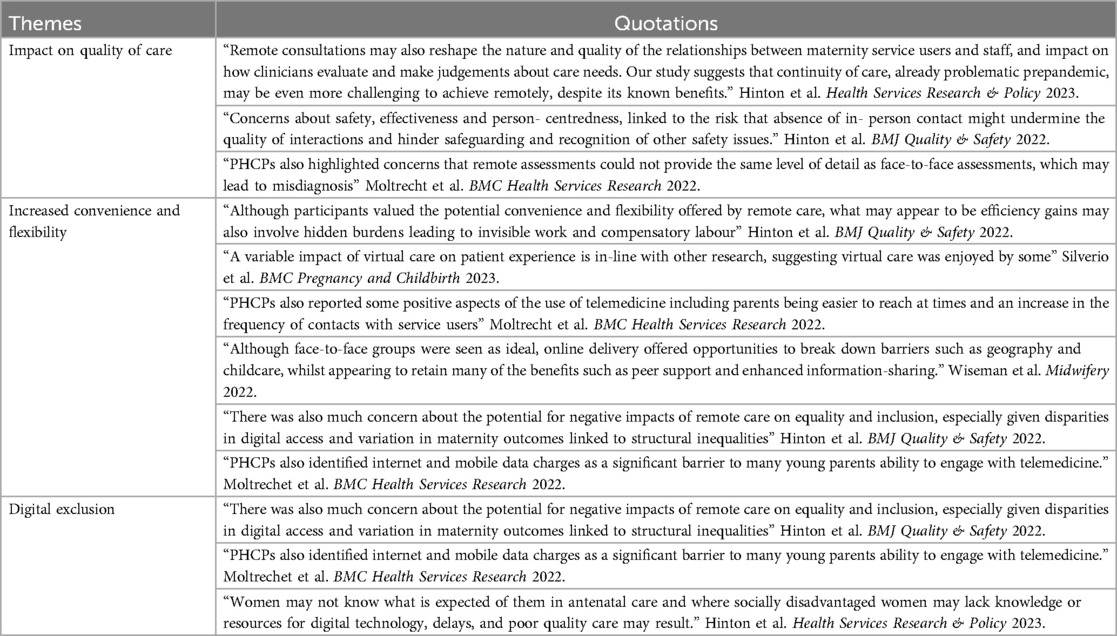
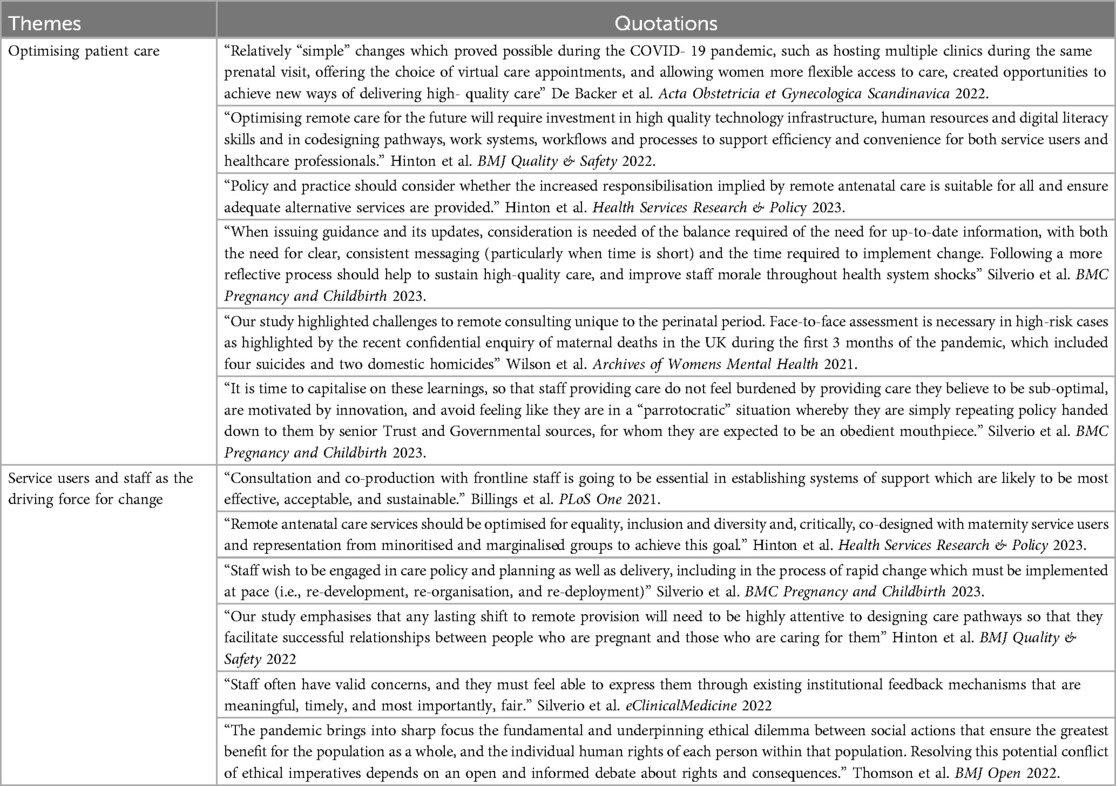
Our synthesis identified nine themes within three of the five RESILIENT concepts: care-seeking and care experience, virtual care, and ethical future of maternity care services (Supplementary Table S5). No studies reported on the RESILIENT concepts of self-monitoring or COVID-19 vaccination. Passages of text from the original discussion sections are presented in Tables 1–3 to support synthesised findings.
3.5 Concept 1: care-seeking and care experience
Fourteen studies (4, 5, 22–34) contributed data to this concept, with four themes: 1.1 Changes to existing provision of care, 1.2 Limitations placed on the partner, 1.3 Mental health and lack of support networks, and 1.4 Barriers to implementation of reconfiguration strategies (Table 1 for supportive quotations).
3.5.1 Changes to existing provision of care
Studies described a reduction in midwifery-led care due to closure of community-based services and a move towards centralised obstetric-led and hospital-based care (23, 28, 31, 32). These changes were perceived to cause a reduction in mothers’ and gestational parents’ choice in birth planning, as well as emotional distress (22, 26, 31, 32). There were challenges in providing care, given rapid changes to protocols, lack of adequate guidance for staff regarding implementation (5, 23, 25), and less time allotted for discussion of care plans (23, 24, 26, 30, 34). However, one study found evidence of some positive effects: staff adapted rapidly, particularly in later lockdowns (11).
3.5.2 Limitations placed on the partner
Studies showed distinct variation between hospitals in visitation rights and involvement of fathers, partners, and non-gestational parents during care appointments and birth (23, 25–27, 30, 31). Exclusion of these individuals was perceived as having negative and adverse effects on women and birthing people's healthcare experiences and emotional state. One study described how paternal mental health was often unaddressed when poor maternal or neonatal outcomes occurred (27).
3.5.3 Mental health and lack of support networks
Nine contributing studies (5, 22, 24–28, 32) outlined the impact of reconfigurations on staff mental health, independent of fathers', partners', and non-gestational parents’ involvement described above. Some staff described a negative impact on morale because they could not provide the standard of care and enhanced support that their service-users deserved (22, 24–28, 32). Particular concerns were raised about a lack of guidance for staff about how they could address service-users’ perinatal mental health (27, 30, 32). Importantly, several studies described HCPs selflessly prioritising the physical and mental health of women and birthing people over their own (22, 26, 30).
3.5.4 Barriers to implementation of reconfiguration strategies
Data from nine studies (5, 23, 24, 26, 28, 29, 31, 33, 34), illustrated how challenges for staff were exacerbated by the pandemic, rather than created anew (24, 26, 29, 33). The “unrealistic work pressures” (24), highlighted across studies, were attributed to increased work demands, reduced staffing, finite resources, and limited guidance on how to adjust practice and cope with difficulties (24, 26). These made it difficult for staff to adapt to new and ever-changing policies, impeding successful implementation of reconfiguration strategies.
3.6 Concept 2: virtual care
Nine studies (4, 5, 23, 25, 27, 28, 32–34) contributed data to this concept, describing how some maternity care changed from in-person to virtual, by telephone or video-conference. Three themes were identified: 2.1 Impact on quality of care, 2.2 Increased convenience and flexibility, and 2.3 Digital exclusion (Table 2 for supportive quotations).
3.6.1 Impact on quality of care
In seven studies (4, 5, 23, 25, 27, 28, 34), concerns were raised about potential harmful consequences of virtual (vs. in-person) delivery on quality of care. HCPs felt positive and trusting patient-provider relationships were harder to establish during virtual care (23, 27, 28, 34). Patient safety was questioned with particular reference to mental health assessments; HCPs felt sensitive information might be less likely to be divulged by service-users over telephone or video calls. Additionally, concerns were expressed for children's welfare in the absence of a full assessment of home circumstances or domestic violence (4, 25, 28).
3.6.2 Increased convenience and flexibility
In contrast, the shift to virtual care had some benefits. Some HCPs commented on being able to provide greater continuity of care, and more frequent contact with service-users (28).
3.6.3 Digital exclusion
HCPs perceived the main barrier service-users faced accessing virtual maternity care was their limited access to the internet and/or electronic devices (including smartphones) (4, 25, 27, 28, 34), as well as limited technology skills and English-language skills (25, 27). Also, HCPs described their own difficulties with access, such as lack of compatible software resources on home devices, and unsuitable home-working environments which hindered hybrid-working (4, 5, 25, 27, 28). Others suggested the transition to virtual care required additional work and time to operationalise (4, 5).
3.7 Concept 3: ethical future of maternity care services
All fifteen studies (4, 5, 22–34) provided data for this concept, describing how maternity services should be built back in a fairer and ethical way, to prevent further exacerbation of health inequities. This concept was coded into two themes: 3.1 Optimising patient care, and 3.2 Service users and staff as the driving force for change (Table 3 for supportive quotations).
3.7.1 Optimising patient care
Hybrid care delivery was described by HCPs as giving mothers and gestational parents the opportunity to choose face-to-face appointments should they wish (24, 25, 32), increasing their autonomy and potentially, their satisfaction with care (4). To facilitate a move to hybrid delivery, HCPs emphasised the need for adequate technology and for digital inequities to be addressed, to prevent exclusion of certain groups (service-users and staff) (27, 28, 34). Nevertheless, HCPs emphasised the need to retain in-person care for high-risk and vulnerable women and birthing people, such as those with complex medical, physical, or social needs (5, 32).
3.7.2 Service-users and staff as the driving force for change
Finally, to build an ethical future of maternity care services, HCPs reported it was crucial to involve staff and service-users in policy-making, particularly through collaboration which considered local context and its challenges and opportunities. Input from those with lived experience of maternity care was seen as vital to ensure service delivery kept their needs and values at the forefront (4, 27, 31, 34). Involvement and consideration of at-risk and vulnerable populations was emphasised, particularly in times of crisis (5, 31).
4 Discussion
4.1 Main findings
This systematic review of 15 qualitative studies (4, 5, 22–34) of HCPs’ experiences of providing maternity care during the COVID-19 pandemic in the UK, builds on a previous qualitative evidence synthesis (14).
Key findings included reduction in provision of community midwifery services leading to perceived loss of autonomy for women and birthing people, challenges with providing good quality care, and inadequate guidance and support for staff regarding protocol changes and safety measures. Altered care-provision and limitations placed on the role of fathers, partners, and non-gestational parents during appointments and birth were perceived by HCPs to be detrimental for women's emotional and physical wellbeing. Staff reported loss of morale, unrealistic work pressures, and reduced staffing—making it difficult to successfully implement reconfiguration strategies.
Studies evaluating experiences of virtual care highlighted HCPs’ concerns about care quality, compared to in-person care, especially for high-risk and vulnerable groups. Participants felt that comprehensive mental health and wellbeing assessments cannot be completed virtually, potentially jeopardising women and birthing peoples’ safety, and leaving staff feeling they were unable to fulfil their duty of care. Access to digital devices and reliable internet connectivity were highlighted as problematic. However, HCPs expressed that virtual care increased convenience and flexibility, and some HCPs found it easier to provide continuity of care and more frequent contact with women and birthing parents.
HCPs perceive an ethical future for maternity care services in the UK to include: personalisation of care to suit individuals’ needs, the offer of in-person care when necessary, and the offer of hybrid care for others who prefer to avoid coming to hospital. The synthesis emphasised the importance of a co-designed and collaborative approach to designing future maternity care, by including both service-users and HCPs in the decision-making process.
4.2 Interpretation
To our knowledge, this is the only UK-focused systematic review of HCPs’ qualitative experiences of delivering maternity care during all three COVID-19 pandemic lockdowns.
We add 15 UK publications (4, 5, 22–34) to the single UK study included in the previous qualitative thematic synthesis by Flaherty et al. (14), comprehensively enhancing our understanding of the impact of the COVID-19 pandemic on UK HCPs’ experiences of providing care during an unprecedented health system shock. Adhering to the aims of RESILIENT, data were synthesised according to our five pre-defined concepts; however, our findings resonate with those of HCPs internationally. The six themes identified in Flaherty et al.'s review drawing on the global literature align primarily with our core concepts of Care-seeking and care experience: altered maternity care, altered care structures and provision, capacity to provide care, professional and personal impact, professional impact, and personal burden (14). We expand, by adding themes related to virtual care and, importantly, HCPs’ views on an ethical future for UK maternity care services (7). However, no data were found to align with the RESILIENT concepts of Self-monitoring or Vaccination.
Our findings align with those of service-users and specific groups of HCPs studied by other researchers. An online survey of parents in Northern England found a reduction in women and birthing people's choices and autonomy over their care (particularly with respect to birth-planning), which jeopardised their overall satisfaction and wellbeing (35). Others reported how it was difficult for HCPs to work in ways which incorporated infection control measures, whilst meeting the needs of women and birthing people, particularly given restricted personal engagement and the ability to provide supportive touch (36, 37). The negative consequences of restrictions placed on fathers', partners', and non-gestational parents’ involvement have been echoed in several other works (6, 38, 39), including potentially reducing these individuals’ ability to bond with their baby, and to offer support to the mother or gestational parent (40)
A key finding of our review was the challenge faced by staff in fulfilling their duty of care, in the face of staff shortages and limited resources. This issue has been recognised and debated by the UK Government (41). Staff surveys in the global setting have attributed staff shortages to heightened stress levels and burn-out (42). Several studies document an increase in depression, anxiety, and stress among HCPs during the pandemic, along with post-traumatic stress symptoms (43, 44).
Our findings that staff had concerns about developing trusting and meaningful relationships with women and birthing people through telephone or video consultation was echoed by service-users, who felt virtual antenatal consultations provided impersonal care and had a negative impact on how much information women and birthing people chose to disclose to their HCP (45). Workforce surveys and those from the UK's communications regulator have associated digital poverty during the COVID-19 pandemic with disabilities and lower socioeconomic background and housing tenure (46). An extensive narrative review of telemedicine in the United States of America emphasised the need for equitable access to digital technology, as well as its potential (47). With a global shift to virtual care delivery in a post-pandemic world, it is crucial to carefully consider the ramifications of using digital technology for groups that are already marginalised and prone to digital exclusion (34). It is crucial to understand the multilayered aspects involved in the adoption and implementation of this technology, from the perspective of all stakeholders, and it should not replace traditional face-to-face care, but rather complement it (51, 52). Finally, the strong desire of women and birthing people to have a model of maternity care that supports women-led decision making (48) speaks to the collaborative working and co-design expressed by HCPs in the literature we reviewed.
Although the roll-out of the COVID-19 vaccination program began in the UK in December 2020, and management of routine self-monitoring of symptoms for pregnancy complications (such as gestational diabetes and hypertension) were major maternity service reconfigurations during the pandemic, the paucity of literature reporting HCPs’ views on these concepts may indicate that staff did not perceive them to have had a major impact on their day-to-day lives, or that this was not a research priority in studies with HCPs. Other research with service users has shown self-monitoring of symptoms during pregnancy to be associated with implementation and resourcing issues (49). Within the RESILIENT programme of work, we have found in interviews with HCPs, policymakers, women, and partners that vaccination, particularly mandatory vaccination programs for staff was a contentious issue (50). We would endorse future research to confirm these findings within other contexts.
4.3 Strengths and limitations
This review benefits from robust data extraction and synthesis, with all studies screened for inclusion independently by at least two authors; while data extraction, quality-assessment, and synthesis were conducted independently by two authors. We evaluated HCPs’ experiences of care provision over all three pandemic lockdowns in the UK. Importantly, we gathered information on how HCPs believed maternity care can be improved in the future, and their emphasis that these should be informed by their own experiences. Given the sheer volume of literature published in the last three years about the impact of the pandemic on experiences of maternity care, and the focus of RESILIENT on the pandemic in the UK, we limited the scope of this review to UK studies only. Nevertheless, Flaherty et al. (14) reported similar views of HCPs in their review of global literature; with no thematic differences between HICs and LMICs, and we plan to complete the additional RESILIENT study systematic reviews in describing longer-term experiences internationally, imminently. Whilst we can take these findings from the UK as a critical case (53) from which we can extrapolate to other settings we realise they may not be wholly generalisable to HCPs’ experiences in other parts of the world, particularly where the system is not modelled on being ‘free-at-point-of-use’. Future publications of the RESILIENT study as well as other research should focus on comparing experiential literature between different healthcare settings. Finally, although our search strategy for the population of interest included a range of professional roles within maternity care, it may not represent the whole maternity workforce in the UK, particularly as specific social determinants (such as gender, ethnicity, or geographic location of individual Trusts) were not considered. This work would be complemented by further local and context-specific research.
5 Conclusion
Based on our synthesis of HCPs’ experiences of providing maternity care during COVID-19 in the UK, we make the following practical recommendations:
1. Maternity services should be optimised by providing more choice in care delivery. Pandemic preparedness plans for maternity care should prevent extensive centralisation of maternity care services and removal of services such as home births, along with ensuring that harsh restrictions are not place on birth partners.
2. Future maternity services should be co-designed with staff and service-users, to reflect their collective experiences and understanding of the context in which they provide and receive care, respectively. Taking into account staff experiences in designing services has the potential to improve workplace wellbeing and maternity staff retention, thereby positively affecting women's maternity care experience.
Patient and public involvement and engagement
This systematic review was periodically reviewed by the Patient and Public Involvement and Engagement (PPIE) group of the wider RESILIENT Study which comprises 15 participants. The group was involved throughout, from conception of the project and research questions, through to checking findings for relevance. Meetings were held three times per year, were well-attended (with at least 8/15 members present at each), and had good representation of birthing and non-birthing parents, healthcare workers, and community support, from multiple ethnic backgrounds, birth histories, and living in different parts of the UK. Each meeting allowed for in-depth discussion and reflection of the work by the wider PPIE team, with suggested changes incorporated. Additionally, one member of the PPIE team was part of the smaller authorship team of this paper and reviewed and edited this manuscript in detail.
Author Contributions
TD: Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Project administration, Resources, Software, Visualization, Writing – original draft. EB: Data curation, Formal Analysis, Investigation, Visualization, Writing – original draft. YP: Data curation, Formal Analysis, Investigation, Writing – review & editing. GH: Data curation, Formal Analysis, Investigation, Methodology, Project administration, Resources, Software, Writing – review & editing. LP: Conceptualization, Data curation, Investigation, Project administration, Software, Writing – review & editing. HDM: Conceptualization, Investigation, Project administration, Resources, Software, Validation, Writing – review & editing. MW: Investigation, Writing – review & editing. MH: Validation, Writing – review & editing. VS: Conceptualization, Resources, Methodology, Writing – review & editing. HB: Conceptualization, Funding acquisition, Validation, Writing – review & editing. KSS: Conceptualization, Validation, Writing – review & editing. ADVC: Conceptualization, Funding acquisition, Validation, Writing – review & editing. ECN: Conceptualization, Validation, Writing – review & editing. ELD: Funding acquisition, Validation, Writing – review & editing. PvD: Conceptualization, Funding acquisition, Investigation, Validation, Writing – review & editing. SAS: Conceptualization, Funding acquisition, Resources, Validation, Writing – review & editing. LAM: Conceptualization, Funding acquisition, Investigation, Project administration, Resources, Supervision, Validation, Visualization, Writing – review & editing.
The RESILIENT Study Group consists of:
Chief Investigator: Prof. Laura A. Magee (King's College London); and Co-Investigators: Prof. Debra E. Bick (The University of Warwick), Dr. Harriet Boulding (King's College London), Dr. Kathryn Dalrymple (King's College London), Ms. Tisha Dasgupta (King's College London), Prof. Emma L. Duncan (King's College London), Dr. Abigail Easter (King's College London), Prof. Julia Fox-Rushby (King's College London), Miss. Gillian Horgan (King's College London), Prof. Asma Khalil (St. George's University Hospitals NHS Foundation Trust & Liverpool Women's NHS Foundation Trust), Ms. Alice McGreevy (King's College London), Dr. Hiten D. Mistry (King's College London), Prof. Eugene C. Nelson (Dartmouth College), Prof. Lucilla Poston (King's College London), Mr. Paul Seed (King's College London), Sergio A. Silverio (King's College London & University of Liverpool), Dr. Marina Soley-Bori (King's College London), Dr. Florence Tydeman (King's College London), Ms. Aricca D. Van Citters (Dartmouth College), Dr. Sara L. White (King's College London), Prof. Ingrid Wolfe (King's College London), Prof. Yanzhong Wang (King's College London), & Prof. Peter von Dadelszen (King's College London).
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. The RESILIENT Study was funded by the National Institute of Health and Care Research [NIHR] Health Services & Delivery Research programme (ref:-NIHR134293) awarded to LAM, SS, HB, ADVC, ELD, PvD, & Members of The RESILIENT Study Group. TD is in receipt of a Health Practices, Innovation & Implementation [HPII] Doctoral Fellowship (ref:- ES/P00703/1), funded by the Economic & Social Research Council [ESRC] as part of the London Interdisciplinary Social Science Doctoral Training Partnership [LISS DTP]. The funders had no role in the work or write-up associated with this manuscript.
Acknowledgments
We would like to extend our thanks to all members of The RESILIENT Study Group, The RESILIENT Study Patient & Public Involvement & Engagement Advisory Group, and The RESILIENT Study Technical Advisory Group for their assistance with reviewing the results of this review on an ongoing basis.
Conflict of interest
Three studies included in the qualitative evidence synthesis were authored by at least one member of the review team (SAS, LAM, or the wider RESILIENT Study Group). However, data extraction, quality assessment, and synthesis of these papers were not conducted by any of the authors, rather by TD, EB, and YP who have no competing interests. The RESILIENT Study has been adopted by the National Institute for Health and Care Research Applied Research Collaboration South London [NIHR ARC South London] at King's College Hospital NHS Foundation Trust. The views expressed are those of the authors and not necessarily those of the NIHR or the Department of Health and Social Care.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fgwh.2024.1470674/full#supplementary-material
Abbreviations
CINAHL, cumulative index of nursing and allied health literature; COVID-19, coronavirus disease 2019 caused by the SARS-CoV-2 virus infection; ENTREQ, enhancing transparency in reporting the synthesis of qualitative research; EMBASE, excerpta medica database; EPPI-Centre, evidence for policy and practice information and co-ordinating centre; HCP, healthcare provider; HICs, high income countries; LMICs, low- and middle-income countries; MEDLINE, online counterpart of MEDLARS MEDical literature analysis and retrieval system; NHS, National Health Service; PRISMA, preferred reporting items for systematic reviews and meta-analyses; RCM, Royal College of Midwives; RCOG, Royal College of Obstetricians and Gynaecologists; RESILIENT: The RESILIENT study, post pandemic planning for maternity care for local, regional, and national maternity systems across the four nations; SPIDER, sample, phenomenon of interest, design, evaluation, and research; UK, United Kingdom; WHO, World Health Organization.
References
1. Royal College of Obstetricians & Gynaecologists and Royal College of Midwives. Information for Healthcare Professionals Coronavirus (COVID-19) Infection in Pregnancy. London: Royal College of Obstetricians & Gynaecologists (2020).
2. Jardine J, Relph S, Magee LA, von Dadelszen P, Morris E, Ross-Davie M, et al. Maternity services in the UK during the coronavirus disease 2019 pandemic: a national survey of modifications to standard care. BJOG. (2021) 128(5):880–9. doi: 10.1111/1471-0528.16547
3. Silverio SA, Backer KD, Easter A, von Dadelszen P, Magee LA, Sandall J. Women’s experiences of maternity service reconfiguration during the COVID-19 pandemic: a qualitative investigation. Midwifery. (2021) 102:103116. doi: 10.1016/j.midw.2021.103116
4. Hinton L, Dakin FH, Kuberska K, Boydell N, Willars J, Draycott T, et al. Quality framework for remote antenatal care: qualitative study with women, healthcare professionals and system-level stakeholders. BMJ Qual Saf. (2022) 33(5):1–13. doi: 10.1136/bmjqs-2021-014329
5. Silverio SA, De Backer K, Brown JM, Easter A, Khazaezadeh N, Rajasingam D, et al. Reflective, pragmatic, and reactive decision-making by maternity service providers during the SARS-CoV-2 pandemic health system shock: a qualitative, grounded theory analysis. BMC Pregnancy Childbirth. (2023) 23(1):1–15. doi: 10.1186/s12884-023-05641-2
6. Silverio SA, Easter A, Storey C, Jurković D, Sandall J. PUDDLES Global Collaboration. Preliminary findings on the experiences of care for parents who suffered perinatal bereavement during the COVID-19 pandemic. BMC Pregnancy Childbirth. (2021) 21(1):840. doi: 10.1186/s12884-021-04292-5
7. George-Carey R, Memtsa M, Kent-Nye FE, Magee LA, Oza M, Burgess K, et al. Women’s experiences of early pregnancy loss services during the pandemic: a qualitative investigation. Women Birth. (2024) 37(2):394–402. doi: 10.1016/j.wombi.2023.12.004
8. Montgomery E, De Backer K, Easter A, Magee LA, Sandall J, Silverio SA. Navigating uncertainty alone: a grounded theory analysis of women’s psycho-social experiences of pregnancy and childbirth during the COVID-19 pandemic in London. Women Birth. (2023) 36(1):e106–17. doi: 10.1016/j.wombi.2022.05.002
9. Greenfield M, Darwin Z. LGBTQ+ new and expectant parents’ experiences of perinatal services during the UK’s first COVID-19 lockdown. Birth. (2024) 51(1):134–43. doi: 10.1111/birt.12780
10. Keely A, Greenfield M, Darwin Z. “We should be working together, and it felt like they disrupted that”: pregnant women and partners’ experiences of maternity care in the first UK COVID-19 pandemic lockdown. Int J Environ Res Public Health. (2023) 20(4):1–15. doi: 10.3390/ijerph20043382
11. Greenfield M, Payne-Gifford S, McKenzie G. Between a rock and a hard place: considering “freebirth” during COVID-19. Front Glob Womens Health. (2021) 2:603744. doi: 10.3389/fgwh.2021.603744
12. Kasaven LS, Raynaud I, Jalmbrant M, Joash K, Jones BP. The impact of the COVID-19 pandemic on perinatal services and maternal mental health in the UK. BJPsych Open. (2023) 9(1):1–6. doi: 10.1192/bjo.2022.632
13. National Health Service. Supporting Pregnant Women Using Maternity Services During the Coronavirus Pandemic: Actions for NHS Providers Executive Summary. London: NHS England (2020).
14. Flaherty SJ, Delaney H, Matvienko-Sikar K, Smith V. Maternity care during COVID-19: a qualitative evidence synthesis of women’s and maternity care providers’ views and experiences. BMC Pregnancy Childbirth. (2022) 22(438):1–32. doi: 10.1186/s12884-022-04724-w
15. British Medical Association. Delivery of Healthcare During the Pandemic BMA Covid Review 3. London: British Medical Association (2022).
16. RESILIENT. School of Life Course & Population Sciences. London: King’s College London (2021). Available online at: https://www.kcl.ac.uk/slcps/our-departments/resilient (cited September 15, 2023).
17. Dasgupta T, Peterson L, Silverio SA, Easter A, Boulding H, Mistry H, et al. Post-pandemic Planning for Maternity Care for Local, Regional, and National Maternity Systems Across the Four Nations. York: PROSPERO (2022). Available online at: https://www.crd.york.ac.uk/PROSPERO/display_record.php?RecordID=355948 (cited March 07, 2024).
18. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. (2021) 10(1):1–9. doi: 10.1136/bmj.n71
19. Dasgupta T, Horgan G, Peterson L, Mistry HD, Balls E, Wilson M, et al. Women and birth women’s experiences of maternity care in the United Kingdom during the COVID-19 pandemic: a follow-up systematic review and qualitative evidence synthesis. Women Birth. (2024) 37(3):101588. doi: 10.1016/j.wombi.2024.02.004
20. Thomas J, Sutcliffe K, Harden A, Oakley A, Oliver S, Rees R, et al. Children and Healthy Eating: A Systematic Review of Barriers and Facilitators. York: The University of York (2003). Available online at: https://www.ncbi.nlm.nih.gov/books/NBK70020/ (cited June 12, 2023).
21. Thomas J, Harden A. Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Med Res Methodol. (2008) 8:1–10. doi: 10.1186/1471-2288-8-45
22. Billings J, Seif NA, Hegarty S, Ondruskova T, Soulios E, Bloomfield M, et al. What support do frontline workers want? A qualitative study of health and social care workers’ experiences and views of psychosocial support during the COVID-19 pandemic. PLoS One. (2021) 16(9):e0256454. doi: 10.1371/journal.pone.0256454
23. Brigante L, Morelli A, Jokinen M, Plachcinski R, Rowe R. Impact of the COVID-19 pandemic on midwifery-led service provision in the United Kingdom in 2020–21: findings of three national surveys. Midwifery. (2022) 112:103390. doi: 10.1016/j.midw.2022.103390
24. De Backer K, Brown JM, Easter A, Khazaezadeh N, Rajasingam D, Sandall J, et al. Precarity and preparedness during the SARS-CoV-2 pandemic: a qualitative service evaluation of maternity healthcare professionals. Acta Obstet Gynecol Scand. (2022) 101(11):1227–37. doi: 10.1111/aogs.14438
25. Hanley SJ, Jones AB, Oberman J, Baxter E, Sharkey D, Gray J, et al. Implementation of public health England infection prevention and control guidance in maternity units in response to the COVID-19 pandemic. J Hosp Infect. (2022) 129:219. doi: 10.1016/j.jhin.2022.04.018
26. Jones IHM, Thompson A, Dunlop CL, Wilson A. Midwives’ and maternity support workers’ perceptions of the impact of the first year of the COVID-19 pandemic on respectful maternity care in a diverse region of the UK: a qualitative study. BMJ Open. (2022) 12(9):e064731. doi: 10.1136/bmjopen-2022-064731
27. Martin-Key NA, Spadaro B, Schei TS, Bahn S. Proof-of-concept support for the development and implementation of a digital assessment for perinatal mental health: mixed methods study. J Med Internet Res. (2021) 23(6):1–17. doi: 10.2196/27132
28. Moltrecht B, de Cassan S, Rapa E, Hanna JR, Law C, Dalton LJ. Challenges and opportunities for perinatal health services in the COVID-19 pandemic: a qualitative study with perinatal healthcare professionals. BMC Health Serv Res. (2022) 22(1):1026. doi: 10.1186/s12913-022-08427-y
29. Silverio SA, De Backer K, Dasgupta T, Torres O, Easter A, Khazaezadeh N, et al. On race and ethnicity during a global pandemic: an ‘imperfect mosaic’ of maternal and child health services in ethnically-diverse South London, United Kingdom. EClinicalMedicine. (2022) 48:101433. doi: 10.1016/j.eclinm.2022.101433
30. Thomson G, Balaam MC, Harris RN, Crossland N, Moncrieff G, Heys S, et al. Companionship for women/birthing people using antenatal and intrapartum care in England during COVID-19: a mixed-methods analysis of national and organisational responses and perspectives. BMJ Open. (2022) 12(1):e051965. doi: 10.1136/bmjopen-2021-051965
31. van den Berg LMM, Balaam M-C, Nowland R, Moncrieff G, Topalidou A, Thompson S, et al. The United Kingdom and The Netherlands maternity care responses to COVID-19: a comparative study. Women Birth. (2022) 36:127–35. doi: 10.1016/j.wombi.2022.03.010
32. Wilson CA, Dalton-Locke C, Johnson S, Simpson A, Oram S, Howard LM. Challenges and opportunities of the COVID-19 pandemic for perinatal mental health care: a mixed-methods study of mental health care staff. Arch Womens Ment Health. (2021) 24(5):749–57. doi: 10.1007/s00737-021-01108-5
33. Wiseman O, Emmett L, Hickford G, Knight M, Lazar J, Yuill C, et al. The challenges and opportunities for implementing group antenatal care (‘pregnancy circles’) as part of standard NHS maternity care: a co-designed qualitative study. Midwifery. (2022) 109:103333. doi: 10.1016/j.midw.2022.103333
34. Hinton L, Kuberska K, Dakin F, Boydell N, Martin G, Draycott T, et al. A qualitative study of the dynamics of access to remote antenatal care through the lens of candidacy. J Health Serv Res Policy. (2023) 28(4):222–32. doi: 10.1177/13558196231165361
35. Stacey T, Darwin Z, Keely A, Smith A, Farmer D, Heighway K. Experiences of maternity care during the COVID-19 pandemic in the north of England. Br J Midwifery. (2021) 29(9):516–23. doi: 10.12968/bjom.2021.29.9.516
36. O’Connell M, Crowther S, Ravaldi C, Homer C. Midwives in a pandemic: a call for solidarity and compassion. Women Birth. (2020) 33(3):205. doi: 10.1016/j.wombi.2020.03.008
37. Horsch A, Lalor J, Downe S. Moral and mental health challenges faced by maternity staff during the COVID-19 pandemic. Psychol Trauma. (2020) 12:S141–2. doi: 10.1037/tra0000629
38. Andrews K, Ayers S, Williams LR. The experience of fathers during the COVID-19 UK maternity care restrictions. Midwifery. (2022) 113:103434. doi: 10.1016/j.midw.2022.103434
39. Fumagalli S, Ornaghi S, Borrelli S, Vergani P, Nespoli A. The experiences of childbearing women who tested positive to COVID-19 during the pandemic in northern Italy. Women Birth. (2022) 35(3):242–53. doi: 10.1016/j.wombi.2021.01.001
40. Vasilevski V, Sweet L, Bradfield Z, Wilson AN, Hauck Y, Kuliukas L, et al. Receiving maternity care during the COVID-19 pandemic: experiences of women’s partners and support persons. Women Birth. (2022) 35(3):298. doi: 10.1016/j.wombi.2021.04.012
41. Waitzman E. Staff Shortages in the NHS and Social Care Sectors. London: House of Lords Library (2022). Available online at: https://lordslibrary.parliament.uk/staff-shortages-in-the-nhs-and-social-care-sectors/ (cited March 07, 2024).
42. Semaan A, Audet C, Huysmans E, Afolabi B, Assarag B, Banke-Thomas A, et al. Voices from the frontline: findings from a thematic analysis of a rapid online global survey of maternal and newborn health professionals facing the COVID-19 pandemic. BMJ Glob Health. (2020) 5(6):e002967. doi: 10.1136/bmjgh-2020-002967
43. Schmitt N, Mattern E, Cignacco E, Seliger G, König-Bachmann M, Striebich S, et al. Effects of the COVID-19 pandemic on maternity staff in 2020 – a scoping review. BMC Health Serv Res. (2021) 21(1):1364. doi: 10.1186/s12913-021-07377-1
44. Slade P, Balling K, Sheen K, Goodfellow L, Rymer J, Spiby H, et al. Work-related post-traumatic stress symptoms in obstetricians and gynaecologists: findings from INDIGO, a mixed-methods study with a cross-sectional survey and in-depth interviews. BJOG. (2020) 127(5):600–8. doi: 10.1111/1471-0528.16076
45. Karavadra B, Stockl A, Prosser-Snelling E, Simpson P, Morris E. Women’s perceptions of COVID-19 and their healthcare experiences: a qualitative thematic analysis of a national survey of pregnant women in the United Kingdom. BMC Pregnancy Childbirth. (2020) 20(1):1–8. doi: 10.1186/s12884-020-03283-2
46. Dafoulas G, Ueno A. Digital Poverty in the UK: Analysis of Secondary Data. London: The British Academy (2022). Available online at: https://www.thebritishacademy.ac.uk/publications/digital-poverty-in-the-uk-analysis-of-secondary-data/ (cited March 06, 2024).
47. Kern-Goldberger AR, Srinivas SK. Telemedicine in obstetrics. Clin Perinatol. (2020) 47(4):743–57. doi: 10.1016/j.clp.2020.08.007
48. Vedam S, Stoll K, McRae DN, Korchinski M, Velasquez R, Wang J, et al. Patient-led decision making: measuring autonomy and respect in Canadian maternity care. Patient Educ Couns. (2019) 102(3):586–94. doi: 10.1016/j.pec.2018.10.023
49. Wilson H, Tucker KL, Chisholm A, Hodgkinson J, Lavallee L, Mackillop L, et al. Self-monitoring of blood pressure in pregnancy: a mixed methods evaluation of a national roll-out in the context of a pandemic. Pregnancy Hypertens. (2022) 30:7. doi: 10.1016/j.preghy.2022.07.006
50. Dasgupta T, Easter A, Boulding H, Sutedja T, Khalil A, Mistry H, et al. Post-pandemic maternity care planning for vaccination: a qualitative study of the experiences of women, partners, health care professionals, and policy makers in the United Kingdom. Vaccines. (2024) 12(9):1042–16. doi: 10.3390/vaccines12091042
51. Binsar F, Hamsal M, Ediansyah E. Paradoxes in Telemedicine Services: Analysis of Challenges and Opportunities for the Future of Digital Health—a Systematic Literature Review. Preprints (2024). doi: 10.20944/preprints202409.0879.v1
52. Petretto DR, Carrogu GP, Gaviano L, Berti R, Pinna M, Petretto AD, et al. Telemedicine, e-health, and digital health equity: a scoping review. Clin Pract Epidemiol Ment Health. (2024) 20:e17450179279732. doi: 10.2174/0117450179279732231211110248
Keywords: COVID-19, maternity services, healthcare professionals, systematic review, qualitative research
Citation: Dasgupta T, Bousfield E, Pathak Y, Horgan G, Peterson L, Mistry HD, Wilson M, Hill M, Smith V, Boulding H, Sheen KS, Van Citters AD, Nelson EC, Duncan EL, von Dadelszen P, The RESILIENT Study Group, Silverio SA and Magee LA (2024) Healthcare providers’ experiences of maternity care service delivery during the COVID-19 pandemic in the United Kingdom: a follow-up systematic review and qualitative evidence synthesis. Front. Glob. Womens Health 5:1470674. doi: 10.3389/fgwh.2024.1470674
Received: 25 July 2024; Accepted: 11 November 2024;
Published: 28 November 2024.
Edited by:
Ozgur Karcioglu, University of Health Sciences, TürkiyeReviewed by:
Céline Miani, Bielefeld University, GermanyRizka Ayu Setyani, Sebelas Maret University, Indonesia
Copyright: © 2024 Dasgupta, Bousfield, Pathak, Horgan, Peterson, Mistry, Wilson, Hill, Smith, Boulding, Sheen, Van Citters, Nelson, Duncan, von Dadelszen, The RESILIENT Study Group, Silverio and Magee. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Sergio A. Silverio, U2VyZ2lvLlNpbHZlcmlvQGtjbC5hYy51aw==
†These authors share first authorship
‡These authors share senior authorship
 Tisha Dasgupta1,†
Tisha Dasgupta1,† Hiten D. Mistry
Hiten D. Mistry Harriet Boulding
Harriet Boulding Kayleigh S. Sheen
Kayleigh S. Sheen Aricca D. Van Citters
Aricca D. Van Citters Emma L. Duncan
Emma L. Duncan Peter von Dadelszen
Peter von Dadelszen Sergio A. Silverio
Sergio A. Silverio Laura A. Magee
Laura A. Magee