
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Educ., 20 February 2025
Sec. STEM Education
Volume 10 - 2025 | https://doi.org/10.3389/feduc.2025.1477509
This article is part of the Research TopicBuilding Tomorrow’s Biomedical Workforce: Evaluation of How Evidence-Based Training Programs Align Skill Development and Career Awareness with a Broad Array of ProfessionsView all 18 articles
Compared to the general population, science trainees experience challenges and heightened stressors that often lead to adverse mental health outcomes. With COVID-19, the stressors of social distancing, isolation, truncated lab time, and uncertainty about the future have all likely exacerbated these issues. Now, more than ever, practical and effective interventions are vitally needed to address the core causes of stress among science trainees and increase their resilience. This paper introduces a new resilience program targeted to biomedical trainees and scientists - Becoming a Resilient Scientist Series (BRS), a 5-part workshop complemented by facilitated group discussions all aimed at bolstering resilience, particularly in the context of academic and research environments. To assess the program’s efficacy, participants completed resilience measures and related assessments before and after completing the series. The results suggest that BRS is associated with improvements in trainee resilience (primary outcome) and with reductions in perceived stress, anxiety, and work-related presenteeism, as well as enhancements in adaptability, self-awareness, and self-efficacy (secondary outcomes). Furthermore, program participants reported a high level of satisfaction, a strong willingness to recommend the program to others, and perceived positive changes in their resilience skills. To the best of our knowledge, this is the first resilience program designed explicitly for biomedical trainees and scientists, tailored to their unique professional culture and work environment.
Exploring the world through the lens of science inspires curiosity and innovation, but it also presents a distinct set of challenges - challenges that demand persistence, critical thinking, adaptability, and resilience in the face of setbacks and rejection. These challenges aren’t merely anecdotal; they are reflected in the data. In fact, 60% of students starting in science, technology, engineering, and mathematic disciplines (STEM1) and pre-med will change their major, at a rate 2 times higher than other disciplines (Frank, 2012; Drew, 2011). Grades for the same or comparable individuals often vary between STEM and non-STEM courses, with STEM courses typically showing lower averages (Coe, 2008).
But science is also challenging for other reasons. After surviving the undergraduate STEM attrition effect, many of aspiring scientists face mental health crises in the field caused by a myriad of academic stressors. These include imposter fears (vs. imposter syndrome, as the term syndrome seems to denote something is wrong with the individuals or that it is abnormal), isolation, constant looming deadlines, navigating complex relationships with advisers, intense competition, lack of work-life balance, uncertain job prospects, burnout, and bullying and harassment. For example, a survey of 4,300 academic scientists worldwide reported that at least half struggled with self-reported depression and anxiety, and 67% reported witnessing bullying or harassment, with 43% directly experiencing either bullying or harassment (Abbott, 2020). This effect is most pronounced among graduate students and trainees who are at 6 times greater risk for depression and anxiety than the general population (Evans et al., 2018). In Nature’s survey of doctoral students and their experiences (Woolston, 2019), 36% respondents reported seeking help for depression and anxiety that stem from their training. Almost half (45%) said their satisfaction with their PhD trajectory decreased as they progressed in their training. Similarly, Nagy et al. (2019) found that nearly half of the surveyed biomedical students met the criteria for at least one clinical diagnosis—a prevalence significantly higher than that of the general U.S. population and their same-age peers. The study also identified high levels of burnout, which were strongly associated with thoughts of dropping out and concerns about employment prospects.
With COVID-19, these negative effects were exacerbated by increased social isolation, truncated lab time, and financial stressors. In fact, in a survey of medical scientists including medical and graduate students, 23% of respondents considered leaving academia post COVID-19, due to lack of work-life balance (Matulevicius et al., 2021). This effect is even more pronounced among biomedical scientists (Chan et al., 2020). A survey conducted in the Netherlands during the height of the pandemic from March to May 2020 revealed that 47% of PhD trainees were at risk for psychiatric disorder, and approximately 40% experienced severe burnout symptoms (Mattijssen et al., 2020). As Chan et al. (2020) described it “…imagine the mental resilience needed to maintain focus on solving that equally important mystery in oncology, cardiology, neuroscience, or any other field that has been put on temporary hold due to the pandemic.”
It is no surprise that these stressors frequently contribute to burnout among biomedical students (Hish et al., 2019; Plieger et al., 2015), exacerbating the already high attrition rate in PhD programs, and the issue is more pronounced with women and underrepresented minority (URM) trainees, who leave science and academia at a disproportionate rate (Grogan, 2019; Maher et al., 2020). Without practical and effective interventions to address the stresses experienced by biomedical trainees, which exacerbate mental health crises, the field will suffer a brain drain and lose talented future scientists and potential for innovation. Now, more than ever, practical and effective interventions are vitally needed to address the core causes of biomedical trainee stress and to increase resilience among trainee populations.
While many of the findings, both for scientists in general and biomedical trainees in particular, raise alarms and call for immediate intervention to help those in the scientific workforce pipeline, academia’s responses have been largely muted. Inside Higher Ed declared a mental health crisis in graduate education and stated, “it is only with strong and validated interventions that academia will be able to provide help for those who are traveling through the bioscience workforce pipeline” (Flahtery, 2018). However, available interventions are often lacking, especially for biomedical science trainees. In fact, the results from the Graduate Student Depression and Anxiety Survey led by Evans and colleagues to recommend National Institutes of Health’s (NIH) own train-the-trainer model, where faculty, administrative, and support staff are trained by mental health professionals to recognize and respond to the trainee’s needs, be adapted “to help today’s PhDs compete in the ‘vast and ever-changing job market’” (Evans et al., 2018).
Here, we propose that to alleviate the current mental health crisis within graduate education, an effective intervention needs to address the unique challenges of academia, target the sources of depression and anxiety, and increase trainees’ ability to cope with stressors and adversity. One promising approach is to provide tailored training that increases trainees’ resilience. For example, a systematic review of resilience training and interventions (Joyce et al., 2018) revealed a large body of evidence highlighting the benefits of resilience training for mental health and well-being by mitigating the impact of stress and adversity. In a recent study of women who are thriving in undergraduate STEM majors, resilience was identified as a common and integral trait that allowed them to succeed (Thoman et al., 2020). In exploring why trainees withdraw early from their biomedical PhD programs, Maher et al. (2020) found that self-efficacy components related to resiliency played a role (see Diekman et al., 2017 for a broader analysis of reasons why women exit STEM majors).
Resilience is a form of mental and psychological strength that enables a person to adapt and adjust to difficult or stressful situations. According to the American Psychological Association, resilience is “the process of adapting well in the face of adversity, trauma, tragedy, threats, or significant sources of stress—such as family and relationship problems, serious health problems or workplace and financial stressors. It means ‘bouncing back’ from difficult experiences” (American Psychological Association, 2020). Because of their ability to adapt, resilient individuals tend to better regulate their behaviors, have a more optimistic outlook with greater life satisfaction, maintain positive self-views. They are also less likely to be depressed and anxious (Cohn et al., 2009; Fredrickson et al., 2008; Mak et al., 2011). Resilient individuals are also less likely to engage in presenteeism—that is, they remain fully functioning in the workplace rather than working while distracted (Thogersen-Ntoumani et al., 2017)—and they also avoid other self-defeating work behaviors (Seligman et al., 1986; Van Katwyk et al., 2000). Importantly, resilience is malleable and can be learned and nurtured (Kim-Cohen, 2007).
While resilience training is gradually gaining traction in academic settings, it has already been shown to be effective in workplace and military settings (e.g., U.S. Army’s Ready and Resilient Campaign, Reivich et al., 2011). Studies have found that resilience training can increase positive affect and a sense of well-being while reducing symptoms of depression and anxiety (Forbes and Fikretoglu, 2018; Robertson et al., 2015). Additionally, it has been associated with improved work performance and organizational commitment (Youssef and Luthans, 2007). An in-depth systematic review of resilience training interventions in the workplace demonstrated increased personal resilience, mental health, and subjective well-being. Participants also experienced other tangible benefits including increased self-efficacy, optimism, and performance (Robertson et al., 2015). It has been estimated that the cost-savings for resilience intervention training is $1,846 per person over 8-weeks due to the reduction in stress tied to depression or trait anxiety, as well as increased presenteeism of workers (Johnson et al., 2015).
Given the constant stressors and frequent rejection inherent in scientific academic settings, along with the high prevalence of depression and anxiety among graduate trainees, there is a pressing need for resilience training. Such training needs to focus on increasing individuals’ ability to adapt to adversity, effectively “bounce back,” and reduce stress, depression, and anxiety, and other self-defeating work behaviors, with a particular emphasis on the unique challenges faced by biomedical trainees. The objective of the current paper is to investigate whether a novel resilience program tailored for biomedical trainees and scientists can enhance their resilience, and hence, their persistence in science.
The Becoming a Resilient Scientist Series (BRS) originally evolved from several standalone webinars conducted by the NIH Office of Intramural Training and Education (OITE) to help trainees manage stress. As the demand for these webinars increased at the start of the pandemic, the questions and responses from the trainees clearly indicated that a more cohesive and comprehensive set of lectures and intervention was needed. Thus, the BRS was created in 2020 as a step toward meeting the needs of the trainee and helping alleviate and address common stressors and increase resilience for those pursuing science.
The BRS program employs multimodal cognitive-behavioral concepts that emphasize community, mindfulness, self-compassion, and cognitive behavioral changes—all of which are thought to increase resilience. The intervention focuses on several broad themes across all sessions, including the importance of learning and practicing resilience skills and the ongoing nature of resilience-building, cultural awareness, the role of identity in the scientific community, and the critical role of community support. The program also emphasizes the potential benefits of therapy and mental health care while acknowledging possible barriers, such as stigma, cost, and the fear of losing productive work time. The program’s goal is to help participants identify and replace maladaptive coping strategies with more adaptive behaviors that support self-efficacy and persistence in STEM fields.
The program is a series of five 2-h workshops; each workshop is followed by an optional one-hour facilitated small-group discussion. The five units are separated by one- to two-week intervals, to enable trainees to learn the content, process it on their own, and explore it with their peers in the facilitated small-group discussion. Each workshop and related discussion session can be a stand-alone, but trainees who attend the entire program can refine and integrate the insights and skills they have learned as material is reintroduced and reiterated throughout the series.
The BRS comprises five parts, each designed to benefit trainees in research and academic settings (see Supplementary material for a full description of each session). Part one serves as the program’s foundation, addressing well-being practices, emotional literacy, and the development of a growth mindset. Trainees learn how to effectively cope with setbacks and disappointments by fostering resilience through habits like self-care, mindfulness, journaling, and seeking community support. Part two centers on countering cognitive distortions and imposter fears, offering strategies to combat negative self-talk and cultivate a growth mindset. Part three emphasizes self-advocacy and effective communication in academic and research hierarchies, teaching trainees how to set boundaries, communicate expectations, and address difficult issues. It particularly acknowledges the importance of mentorship, especially for marginalized trainees. Part four addresses the challenges of receiving feedback and staying receptive to it, and part five delves into effective mentoring and relationship management, with a focus on improving interactions with principal investigators, supervisors, seeking additional mentors, and addressing toxic environments.2
In the current paper, we evaluate the effectiveness of BRS as a resilience intervention program for biomedical science trainees who participated in the program during the COVID-19 pandemic. Given the severity of the pandemic, including widespread isolation, salient injustice issues, and concerns for various other mental health issues of the trainees at that time, a conscious and ethical decision was made to make the program open for all trainees who wanted to participate (vs. a waitlist control). Although each workshop in the series could function as a stand-alone, we hypothesized that those who consistently participated in the program by attending more than half of the sessions would have more chances to integrate and practice the skills they learned, and therefore, would show greater increases in the primary outcome of resilience and associated secondary outcomes compared to those attending fewer than half of the sessions. Thus, the evaluation considers a “dose” effect independent of time on the primary and secondary outcomes, rather than a comparison to a waitlist control group who did not receive the training.
To that end, there are four major goals. First, we evaluate whether individuals who completed more than half (more than three sessions) of the BRS exhibited significantly higher increases in resilience levels compared to those who completed less than half. Second, since the program focused on themes of adjusting and adapting to adversity, stress, increasing self-awareness, believing in one’s ability to achieve goals, and other coping strategies, we expected corresponding changes on various correlates of resilience—decrease in perceived stress, depression, anxiety, work presenteeism, and increases in the ability to shift and persist during stressful events, self-efficacy, and self-awareness. Third, since the change in resilience should drive the changes in the secondary outcomes, we hypothesized that resilience should mediate the changes in the secondary outcome measures. Lastly, we describe participants’ reported satisfaction with the program and whether self-reported changes differed for those completing the majority of sessions compared to those who completed fewer than half of the BRS program.
Biomedical trainee participants were recruited from the NIH Intramural Research Program (IRP) and from various extramural institutions who were invited to participate in the program by the NIH’s OITE. For IRP trainees, the announcement for the program was made via OITE trainee listservs, and all IRP trainees (from postbaccalaureate to postdocs) were invited to participate. The trainees from extramural institutions were recruited by their institution, various listservs, and social media, and similar to NIH trainees, ranged from undergraduate to postdocs and medical students.
The current evaluation of the BRS program was implemented in two rounds, with the first round (BRS1) held from January to May 2021 across six sessions and the second round (BRS2) was held from September 2021 to December 2021 across five sessions. The workshop component was held once every 3 weeks for the first round (BRS1) and every 2 weeks for the second round (BRS2) via Zoom, and the small group discussions were held a week later. Trainees participated in the optional small group discussion sessions at their institution via Zoom or at one of the open sessions hosted at NIH via Zoom. Small discussion sessions were led by trained facilitators with a discussion guide. Because the content of the additional session in BRS1 was folded into other sessions of BRS2 and because there were no differences in data or attendance rates between the two sessions, the two rounds of BRS were collapsed into one.
Each webinar session had on average, 363 attendees, with an additional 350 watching the recording.3 In addition, on average, 371 trainees attended the small group discussion sessions.
Prior to the start of the first BRS session, all participants who logged into the webinar were asked to complete a pre-program survey assessing current resilience levels (primary outcome) and secondary outcomes, such as perceived stress, anxiety and depression levels, work presenteeism, their current ability to shift and persist during stressful events, self-awareness, and self-efficacy (see measures below). Following completion of the BRS program, all participants who attended at least one workshop received an email with a link to the post-program survey. The post-program survey was identical to the pre-program survey but also included questions regarding program satisfaction, self-perceived changes, how many workshops were attended, demographics, and open-ended comments. The NIH Institutional Review Board granted an IRB exemption for this study, and the participants were provided with an online written consent at the beginning of each survey. The average length of time between pre- and post-survey was 4 months (the duration of BRS series), and the post-survey was open for 6 weeks after the conclusion of the series.
At the post-program assessment, participants reported on the workshops they attended. Those who participated in more than three workshops were classified as “consistent attenders,” having attended more than half of the BRS program sessions; otherwise, participants were classified as “inconsistent attenders.”
Resilience was measured by the 10-item Connor-Davidson Resilience Scale (CD-RISC-10, full scale; Connor and Davidson, 2003). Participants were asked to rate the frequency (0 = “not true at all” to 4 = “true nearly all the time”) in which they endorsed resilience related thoughts, beliefs, or behaviors in the last month (e.g., “I am able to adapt when changes occur”). In the current study, the items had good internal consistency with Cronbach’s α = 0.83 (pre-program assessment) and 0.87 (post-program assessment). The 10 items were averaged to create a score from 1 to 5, where higher scores indicate greater resilience.
To optimize time and encourage higher survey completion rate among participants, most secondary outcomes were assessed using abbreviated version of well-validated measures of distress, well-being, and work engagement. The selected items were chosen based on their face validity or the subscales that were most relevant. When full scales were used, this is explicitly indicated.
Perceived stress was measured by a subset of 4 items from the 10-item Perceived Stress Scale (PSS; Cohen et al., 1983) that focused on the control aspects of stress. Participants were asked to rate the frequency in which they experience stress-related feelings and thoughts (“how often have you felt that you were unable to control the important things in your life”) in the past month. Participants used a scale ranging from “never” (=0) to “very often” (=4). In the current study, the four items had acceptable internal consistency with Cronbach’s α = 0.73 (pre-program assessment) and.77 (post-program assessment). The four items were averaged to create a score from 1 to 5, where the higher number indicates greater perceived stress.
Anxiety was measured by a subset of 3 items from the 7-item Generalized Anxiety Disorder Scale (GAD-7; Spitzer et al., 2006), that focused on non-physical symptom items. Participants were asked to rate the frequency in which they experienced various anxiety symptoms (“Not being able to stop or control worrying”) in the past 2 weeks on a scale ranging from “not at all” (=1) to “almost every day” (=4). In the current study, the items had good internal consistency with Cronbach’s α = 0.76 (pre-program assessment) and 0.77 (post-program assessment). The three items were averaged to create a score from 1 to 4, where the higher number indicates greater anxiety levels.
Depression was measured by a subset of 4 items of the 9-item Patient Health Questionnaire (PHQ-9; Kroenke et al., 2001) that focused on general non-clinical depressive symptoms. Participants were asked to rate the frequency in which they experienced various depressive symptoms (“feeling down, depressed, or hopeless”) in the past 2 weeks on a scale ranging from “not at all” (=1) to “almost every day” (=4). In the current study, the items had good internal consistency with Cronbach’s α =0.81 (pre-program assessment) and 0.79 (post-program assessment). The four items were averaged to create a score from 1 to 4, where the higher number indicates greater (non-clinical) depression levels.
Presenteeism was measured by the 6-item Job Stress Related Presenteeism Scale (JSRP, Full scale; Gilbreath and Frew, 2008). Participants were asked to rate the extent to which they had engaged in thoughts or behaviors related to presenteeism (“I’m unable to concentrate on my job because of work-related stress”) on a scale ranging from “never” (=1) to “all the time” (=5). In the current study, the items had good internal consistency with Cronbach’s α = 0.83 (pre-program assessment) and.85 (post-program assessment). The six items were averaged to create a score from 1 to 5, where the higher number indicates greater job stress-related presenteeism.
The ability to shift and persist during stressful times was measured by the 14-item Shift-and-Persist Scale (Full scale; Chen et al., 2015). Participants were asked to rate the extent to which various statements describe them (“When something stressful happens in my life, I think about what I can learn from the situation”) on a scale of “not at all” (=1) to “a lot” (=4). In the current study, the items had good internal consistency with Cronbach’s α = 0.82 (pre-program assessment) and.82 (post-program assessment). Excluding 6 distractor items, four items were average to create a shift sub-scale score from 1 to 4, and four items were average for a persist sub-scale score from 1–4. The higher scores indicate a greater ability to shift and/or persist during stressful times.
The belief in one’s ability to achieve their goals in the face of adversity was measured by the 8-item New General Self Efficacy Scale (Full scale; Chen et al., 2001). Participants were asked to indicate their agreement with statements such as, “I will be able to successfully overcome many challenges,” on a scale from “strongly disagree” (=1) to “strongly agree” (=5). In the current study, the items had good internal consistency with Cronbach’s α = 0.89 (pre-program assessment) and.89 (post-program assessment). The eight items were averaged to create a score from 1 to 5. The higher scores indicate greater self-efficacy or the belief that one can overcome obstacles and achieve goals.
The awareness and reflection of one’s internal states with attention to learning and self-awareness at work were measured by a subset of items from the Self-Awareness Outcomes Questionnaire (SAOQ; Sutton, 2016), specifically the reflective self-development (RSD) and proactive at work (PRO) subscales. Because BRS focused on self-development and being proactive at work, the other subscales, acceptance and emotional costs, were not included as it may not be relevant to increased resilience. Participants were asked to rate the frequency in which they endorse statements such as “I focus on ways of amending my behavior that would be useful” on a scale of “never” (=1) to “almost always” (=5). In the current study, the items had good internal consistency with Cronbach’s α = 0.85 (pre-program assessment) and.87 (post-program assessment). Each subscale item was averaged to create a score from 1 to 5. The higher scores indicate greater self-awareness and reflection of oneself and self-awareness at work.
During the post-program survey, participants were asked to evaluate the BRS program with respect to overall satisfaction, likelihood they would recommend the training to a friend or colleague, and whether they found the program valuable on 5-point Likert scales.
To assess self-perceived changes, participants were asked during the post-program survey if they had become more resilient, better scientists, managed conflict and stress better, and if they had gained important skills on a 5-point Likert scale, ranging from 1–5 (e.g., “Since participating in the resilience series, I have become more resilient in my work and/or life”). Furthermore, participants assessed their perceived knowledge on how to be a resilient science before and after participating in the program.
To assess program’s impact on different demographic groups, participants self-reported their gender and race/ethnicity. The race/ethnicity options were White, Asian, Black/African American, Hispanic/Latino/Spanish, American Indian/Alaska Native, Native Hawaiian/Pacific Island, other, and prefer not to say. Those who selected multiple race/ethnic identities were coded as multi-racial.
All analyses were conducted using SPSS. Prior to addressing study aims, we assessed whether there were observed differences across trainee populations (i.e., NIH intramural trainees and extramural trainees) and BRS round (i.e., BRS1 and BRS2). There were no differences observed with regards to consistent participation, primary and secondary outcomes, and program satisfaction/perceived changes. Thus, data were collapsed across trainee populations and BRS round.
To address aims 1 and 2, we matched pre-and-post surveys and conducted a paired sample t-test to assess pre-program changes in resilience (primary outcome) and secondary outcomes at the post-program assessment. Furthermore, an independent sample t-test was used to explore the impact of consistent and inconsistent attendance on primary and secondary outcomes at the post-program assessment. All analyses include effect size (Cohen’s d) to highlight the magnitude of an effect, offering insights into its practical significance and real-world relevance. We followed the convention of using 0.2 as small, 0.5 as medium, and 0.8 as large effect sizes.
To address aim 3, we conducted a bootstrapped mediational analysis (Preacher and Hayes, 2004) to test indirect effect of consistent and inconsistent attendance on the secondary outcomes mediated by resilience.
To address aim 4, we constructed descriptive statistics for program satisfaction assessments and reported the percent rating the program “good” (=3) to “excellent” (=5). Independent t-tests were conducted to assess differences in program satisfaction and self-perceived changes following program completion between those who attended the program workshops consistently and those who were inconsistent attenders.
Given the attrition of females and underrepresented trainees in science, we further explored how trainee’s gender and race may influence the effects of BRS as an ancillary analysis.
A total of 625 trainees completed the post-program survey across the two rounds of BRS.4 There were 440 females (70.4%), 154 males (24.6%), and 31 unknown (4.9%) gender. Two hundred and ninety-five trainees identified as white (47.2%), 313 racially and ethnically diverse/multiracial (49.4%), and 22 did not specific their race or ethnicity. Of those, using a unique self-guided ID, we were able to match up a total of 341 participants with their pre-and post-program surveys (216 in Spring 2021; 125 in Fall 2021). In the pre-and-post matched sample, there were 255 females (74.8%), 75 males (22%), and 11 unknown (3.3%). One hundred ninety-five trainees identified as white (57.2%), 142 as racially and ethnically diverse/multiracial (41.6%), and 4 (1.2%) did not specify their race or ethnicity.5
To address aim 1, we conducted a paired sample t-test to assess pre-program changes in resilience at the post-program assessment. As predicted, there was a significant increase in RISC-10 resilience scores pre vs. post BRS program participation (Mpre = 2.47 vs. Mpost = 2.80; p < 0.001, d = 0.73), such that participants resilience increased post BRS participation (Table 1). The medium-to-large effect size (Cohen’s d = 0.73) demonstrate that this improvement is both statistically significant and practically meaningful. The observed 8.25% change in self-reported resilience indicates an improvement in participants’ perceived ability to adapt to adversity, stress, and challenges. This increase suggests participants are more consistently view themselves as resilient, with the magnitude of the effect indicating that the changes are likely noticeable in their daily lives and interactions.6
Unsurprisingly, the matched pre-and-post sample had less than 14% individuals who attended 3 or less sessions and coded as “inconsistent attenders.” To explore the effect of consistent vs. inconsistent attendance on resilience more robustly, we used the post-program only sample and conducted an independent sample t-test to assess whether the resilience score differed for those who attended the BRS program consistently as compared to those who inconsistent attenders. As expected, we observed significantly higher RISC-10 resilience scores for consistent attenders (M = 2.82, SD = 0.50) vs. inconsistent attenders (M = 2.69, SD = 0.52, t (623) = 2.51, p = 0.012, d = 0.26) (see Table 2).
With respect to secondary outcomes in the pre-and-post matched sample, we observed a significant decrease in perceived stress, anxiety, and depression and an increase in participants’ self-perceived ability to shift and persist, self-efficacy, self-awareness related to reflective self-development, and being proactive at work (Table 1). This suggests that those who consistently attend BRS from the start of the series are seeing significant changes in all secondary outcome measures.
Similarly, in the post-program sample, the consistent attenders were significantly lower in perceived stress, and higher ability to persist, self-efficacy, self-awareness related to reflective self-development. We saw marginal decreases in depression, self-awareness related to being proactive at work (Table 2). However, we did not see differences in anxiety, work presenteeism, or the ability to shift during stressful events.
Mediational analyses based on 5,000 bootstrapped samples using bias-corrected and accelerated 95% confidence intervals (Preacher and Hayes, 2004; Preacher et al., 2007) was conducted to test resilience (RISC-10) as a mediator of the relationship between attendance and secondary outcomes (Figure 1). In these analyses, mediation is significant when confidence intervals for the indirect effect do not include 0. As expected, resilience fully mediated depression, the ability to persist, self-efficacy, and perceptions of being proactive at work as well as reflective self-development components of self-awareness (Tables 3, 4). It also partially mediated perceived stress. These results indicate that the increase in resilience by consistent attenders also account for the various secondary outcomes, including reduction in perceived stress, depression, and the increase in the ability to persist during stressful times, self-efficacy, and self-awareness.
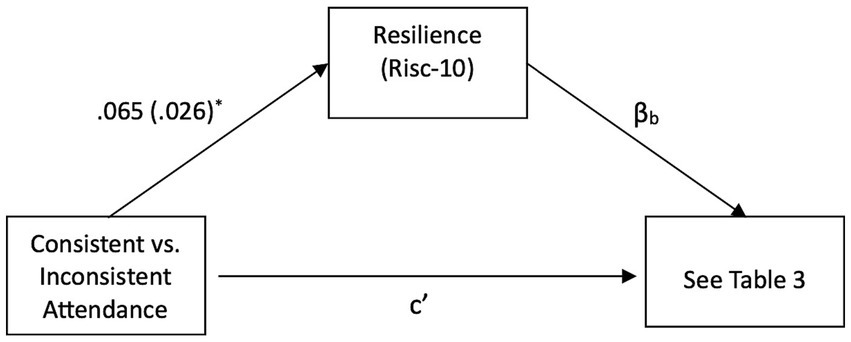
Figure 1. Mediational pathway between consistent vs. inconsistent attendance, resilience, and secondary outcomes.
Most of the participants rated the program good to excellent overall (M = 4.43, SD = 0.75; 97.9% ≥ 3), found the program valuable (M = 4.60, SD = 0.68; 98.0% ≥ 3), and would recommend it to a friend or a colleague (M = 4.71, SD = 0.61; 98.5% ≥ 3). Almost all of these satisfaction scores hovered around the top of the scale point at 5. There was also a significant increase in self-reported knowledge of how to become a more resilient scientist compared to before the program, (t (610) = 51.39, p < 0.001; d = 2.08; Mchange = 2.42, SDchange = 1.16).
As expected, compared to inconsistent attenders, consistent attenders reported significantly higher ratings of the BRS program, value, and were more likely to recommend the program to a colleague or a friend. Moreover, those who attended consistently were more likely to report that their perceived resilience had increased, that they gained important skills that help with school or home, and that they developed a greater ability to manage stress and conflict. However, we did not see a difference in their self-perceived ability to become a better scientist (Table 5).
Because BRS had high proportion of trainees from diverse backgrounds, we explored whether there is a differential effect of BRS by race/ethnicity (dichotomized as white vs. trainees from racially and ethnically diverse groups, N = 295 and 305, respectively). Although we did not find a significant differences in the pre-and-post matched measures on race/ethnicity, we found significant differences in self-perceived ratings in the post-survey for ethnicity. For example, two-way between group analyses of self-perceived resilience change (gaining important skills; the ability to manage stress and conflict; and the ability to become a better scientist) on race/ethnicity by attendance revealed no significant interactions (all ps > 0.1) but significant main effects (all ps < 0.01), albeit moderate to small effect sizes. The results are presented in Table 6. There were no significant effects of gender.
The results show that the BRS can be an intervention program with a moderate to large impact on the trainees. In addition to being highly rated, the program appears to enhance resilience, self-efficacy, and self-awareness. For those who completed both pre-and-post program measures, BRS improved their self-perceived ability to shift and persist, self-efficacy, and self-awareness while decreasing self-reported anxiety, depression, perceived stress, and presenteeism. After the intervention, participants reported that they were better managing stress and conflict, that they found what they learned valuable, and that they had become more resilient.
As expected, we saw greater effects among those who attend more sessions indicating that the program is effective and is especially beneficial for those who consistently attended (i.e., “higher dose”). In the post-program survey only sample, consistent attenders showed increased resilience, ability to persist, self-efficacy, proactive and reflective self-development components of self-awareness, and saw decreases in perceived stress and marginal decrease in depression. We found that the program’s impact of resilience fully mediated its effects on depression, ability to persist, self-efficacy, and self-awareness, and partially mediated perceived stress. This hints at the underlying mechanism that the increase in resilience is driving the corresponding changes on the secondary outcomes. We speculate that perceived stress may only be partially mediated by resilience, because BRS had another important component—a sense of community and that the trainees are not alone. In fact, in our comment section, the most frequently mentioned comments were that the trainees were glad that they are not alone or that their experiences are not unique. Part of the mechanism driving the reduction in perceived stress may not only be from the increase in resilience but also from a sense of relief or comfort that the experience is shared by others (see Neff, 2003). That sense of not being alone may also reduce feelings of shame which may further improve one’s ability to ask for help and work on building effective coping strategies. Furthermore, of those who attended more than half also found the program more valuable and were more likely to recommend to their friend or colleague; however, it should be noted that those who attended less than half still rated the series highly, found it valuable, and likely to recommend it to a friend or a colleague.
Although BRS seems to be beneficial for all trainees taken together, it seems to have been especially beneficial for trainees from racially and ethnically diverse groups. Compared to white trainees, racially and ethnically diverse trainees self-reported and perceived much greater changes in their perception of resiliency, gained important skills that helped them in their work and home, learned to manage stress and conflict better, and reported that they became a better scientist as a result, despite not showing greater changes in resilience measures. We speculate that, similar to the not being alone effect noted above, that racially and ethnically diverse trainees may find comfort in knowing that their experiences and challenges are shared and recognized by others. BRS explicitly address the challenges that marginalized trainees face in science and research community—especially the role of bias, microaggression, stereotype threat, and how it can lead to attributional ambiguity (Crocker et al., 1991). These findings indicate that BRS could be an important and effective tool in retaining diverse trainees in biomedical science.
It appears that BRS can fill a critical void that currently exists in the biomedical training community. It is empowering trainees to effectively deal with the stressors of academics and research by giving them a sense of agency and the best strategies and tools to cope with those stressors, as well as setbacks and other adversities. It is a step toward reducing the mental health crisis among trainees in biomedical sciences, and when scaled up, could provide a large benefit, and help prevent attrition of trainees in science.
The BRS series is a program designed to help trainees struggling with stressors and raise their resilience during a time when the alarm bells started sounding regarding the graduate mental health crisis in science and when the pandemic was exacerbating that effect. The program was an attempt at meeting the crucial needs of the trainees, and helping them alleviate and address common stressors, providing them with coping skills, and ultimately increasing resilience for those pursuing biomedical science. And it appears that the program can be successful at meeting those goals and is addressing the needs of the trainees and improving their well-being.
However, some may question if the beneficial changes in this intervention program were primarily driven by the changes in the pandemic-stressors and passage of time. The BRS1 started before the COVID-19 vaccine was available, at the height of the pandemic when trainees were grappling with uncertainty and isolation and concluded during a potentially more hopeful period of as vaccines started becoming widely available. While this alternative explanation cannot be ruled out, if this were the case, BRS2 should not show the same results. BRS2 started as the vaccines were becoming widely available and pandemic-related pressures were easing. Yet we did not see any differences between BRS1 and BRS2. This consistency between two distinct cohorts suggests that the observed improvements are unlikely to be solely attributable to the effects of the pandemic (i.e., effects of history or regression to the mean) and that it is more likely that the intervention is targeting the needs of the trainees.
However, it is important to acknowledge the limitations of COVID-related confounds in this study. Although we included measures of perceived stress, we did not collect COVID-specific stress data, which limits our ability to disentangle the effects of pandemic-related stressors from the intervention’s impact. Additionally, the lack of a control group prevents us from definitively attributing the observed increases in resilience to the intervention alone. Regression to the mean, in particular, is a plausible explanation given that the program began at a time when baseline resilience may have been unusually low due to pandemic-related challenges. However, the consistent results observed in two separate cohorts of BRS starting at different times during the pandemic with varying stress levels, significantly reduce the likelihood that regression to the mean alone accounts for the findings. Such replication across the two distinct groups suggests that the observed improvements are not random fluctuations or statistical artifact but rather that the intervention is contributing meaningfully to the observed improvements.
These limitations underscore the importance of interpreting the results with caution. While the consistency of findings across BRS1 and BRS2 strengthens the case for the intervention’s effectiveness, future studies should incorporate a control group and include COVID-specific stress measures or other relevant contextual factors to better isolate the program’s impact and to rule out confounds, especially regression to the mean. Such methodological improvements will help clarify the unique contribution of the intervention to trainees’ resilience.
Another alternative explanation for the result could be that the participants who were consistent attenders were inherently different at baseline. In order to rule out this explanation, we conducted pre-program measure differences between consistent vs. inconsistent attenders on all primary and secondary measures. We did not find any significant pre-measure differences (all ps > 0.2). Therefore, it appears that both consistent and inconsistent attenders were equivalent on our primary and secondary measures at the baseline (at the beginning of the program) and the program attendance or dosage effect is seemingly driving the effect. On the other hand, we cannot say for sure that those who attended all sessions and those who missed one or more were identical in all possible ways. Given the severity of the pandemic, including widespread isolation, salient racial injustice issues, and concerns for various other mental health issues of the trainees at that time, a decision was made to make the program open for all trainees who wanted to participate. Hence, a critical decision was made to forgo a control comparison condition (i.e., waitlist control) and, therefore, drop the quasi-experimental design to allow for broad and open participation. A more ethical decision was made at the expense of establishing the causal impact of the intervention program, and we are unable to rule out some confounding variables which underscores the need for cautious interpretation. Thus, acknowledging this weakness, future studies might compare the efficacy of this intervention with that of other interventions or introduce a waitlist control.
While we utilized a well-known and validated survey instruments for this study, we had to make compromises in the interest of survey length and administration time. We deliberately selected only a subset of questions that were face valid on the instruments and calculated means accordingly. This approach may have impacted the psychometric properties of the measures, as they were originally designed to be evaluated as a whole. While the subset of questions retained their essential reliability and validity, the overall robustness of the measures may have been affected. This limitation underscores the need for caution when interpreting the results, especially in cases where a more comprehensive evaluation of psychometric properties is required (i.e., clinical anxiety vs. non-physical component anxiety measured in this study). However, these limitations were necessary to balance practicality and participation in our study, and we are confident that they do not detract from the overall effectiveness of the program.
Although the program is largely successful, there was significant attrition. In both rounds of BRS, we started with approximately 600 trainees, and by the end of the series, we had approximately 250 trainees in attendance. We speculate that there are two reasons for this. First is the time commitment and pressure from others to work while in the lab during the workday. As the attrition occurred, small group facilitators informally reached out to a subset of trainees, querying why they stopped attending. Many trainees mentioned that the time commitment interfered with lab work commitments, and they chose to prioritize lab work. Some said their PI/supervisor did not support them attending a webinar during the day when they should be focused on lab work. It is essential to acknowledge that the impact of this time commitment and the pressure to prioritize lab work may introduce a selection bias in our study. It is possible that our sample may not fully represent trainees who are heavily or overcommitted to lab work, those who prioritize it over self-care/improvement, or those who lack support for their well-being and resilience from their PIs/supervisors. However, we contend that this underscores the potential benefits of mandating resilience training as a vital component of the curriculum. This step is crucial as we strive to foster a cultural shift in the field of science. Many trainees were hesitant to commit 3–6 h per month to improving their resilience because of fears that participation would interfere with their lab work. We need to change the culture of long hours and complete dedication to lab work to also emphasizing the importance of self-care and self-improvement. After all, one must be well to do well.
The second possibility for attrition is motivation. Although many trainees were excited to start, they may have lacked the motivation and commitment to complete the entire series. Hence, it is possible that only the motivated trainees completed the program and benefited from it. Nevertheless, this explanation for attrition does not undermine the effectiveness of the BRS program. The social psychological literature on behavior and attitude change state that one needs to be willing (i.e., motivated) and able first before any actual changes can occur (e.g., theory of planned behavior; Ajzen, 1991). The effectiveness of BRS is likely driven by providing the tools and the skills the trainees need to implement and make the changes. Those who are willing and able are more likely to practice those skills and see corresponding changes in their resilience. Our data hint that this could be the case—those who attend more than half of the sessions (likely more motivated and committed) report more benefits than those who attend less than half. Furthermore, our pre-and-post sample group demonstrated the greatest positive changes in all secondary outcomes, and they were also the group who attended the majority the BRS sessions. In fact, while we saw changes in anxiety, work presenteeism, and the ability to shift during stressful times in our pre-and-post matched-sample, we did not find the corresponding changes between consistent and inconsistent attenders on post-program only sample. It is possible that these variables require consistent effort and motivation to improve. Hence, it is unlikely that any intervention program, no matter how effective, will have a large impact on those who are unmotivated and unwilling to change.
The results of the BRS align with existing research on strategies to prevent burnout among science trainees. For instance, Prendergast et al. (2024) demonstrated that a reflection-based intervention effectively reduced burnout in second-year medical students. Similarly, a survey by Hish et al. (2020) found that social engagement was rated as a highly effective method for alleviating burnout symptoms, while earlier work by Hish et al. (2019) highlighted the mediating role of mastery and advisor support in the relationship between stress and burnout. These findings raise an important question: Did BRS primarily reduce burnout? It is plausible that BRS contributed to mitigating burnout, as it incorporates strategies commonly found in burnout interventions, such as increasing self-reflection, mindfulness, social connection, and self-efficacy. However, while burnout and resilience are related concepts, they remain distinct constructs with unique definitions, characteristics, and implications. Burnout is characterized as a state of chronic, unmanaged work-related stress (see World Health Organization, 2019). In contrast, resilience refers to the capacity to adapt and thrive in the face of adversity. Importantly, resilience can act as a protective factor not only against burnout but also against other challenges, such as anxiety, depression, and stress and increases the ability to shift, persist, and self-awareness—all of which were assessed in our study. Since we did not directly measure burnout but rather examined some of its symptoms, it would be inappropriate to draw definitive conclusions about the program’s impact on burnout. Instead, our findings suggest that BRS may increase resilience, which in turn could help address multiple factors associated with burnout. This distinction underscores the broader applicability of resilience-based interventions beyond addressing burnout alone.
The BRS has shown its effectiveness as an intervention, and it could be a valuable tool for trainees as they navigate the unique challenges of academic scientific settings. Furthermore, the program is readily available to a wide range of trainees since it is free of charge and easy to participate in. Trainees have the option of joining live sessions twice a year with small discussion groups via Zoom, or they can watch recordings at any time at their convenience. The program’s affordability and accessibility are particularly advantageous to trainees who are constrained by financial and scheduling limitations. Given the program’s accessibility, there is little reason why trainees and extramural institutes should not explore the possibility of incorporating it in their training (see Supplementary material on how OITE can aid in BRS adaptation at various extramural institutions).
The BRS program has been shown to be effective in enhancing resilience among trainees, and especially beneficial for individuals from diverse backgrounds. By providing trainees with the tools to manage stress, cope with failure, and maintain a healthy work-life balance, the program has the potential to retain a talented biomedical workforce while nurturing a group of resilient future scientists. Considering the mental health crisis that many biomedical and science trainees face, the BRS program may be an important component of addressing these issues in the sciences more broadly. With its proven effectiveness, accessibility, and potential to improve trainee well-being, the BRS program offers a promising solution to some of the challenges facing the scientific community.
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found below: https://doi.org/10.7910/DVN/9NSWXO.
The studies involving humans were approved by National Institutes of Health IRB. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
HH: Conceptualization, Data curation, Formal analysis, Methodology, Writing – original draft, Writing – review & editing. UK: Project administration, Writing – review & editing. LM: Conceptualization, Writing – review & editing. AS: Conceptualization, Writing – review & editing. SM: Conceptualization, Funding acquisition, Methodology, Project administration, Resources, Writing – review & editing.
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. We acknowledge the National Institute of General Medical Sciences (NIGMS) for providing initial funding to open the Becoming a Resilient Scientist (BRS) series to the extramural community. We appreciate the on-going support of the NIH Immediate Office of the Director, NIH Office of Research on Women’s Health, NIH Office of AIDS Research, NIH Office of Behavioral and Social Sciences Research, and other NIH Institutes and Centers.
This paper is dedicated to the memory of Wes Beckstead (1983–2011) who greatly influenced the work of SLM in developing support structures for NIH intramural trainees. We thank Drs. Laura Koehly, Janetta Lun, Brett Pelham, and the OITE staff for valuable input on this project, and Dr. Michael Gottesman for supporting the development of well-being programs for the NIH intramural scientists. Finally, we are deeply grateful for the energy and enthusiasm of the facilitators, mentors, and trainees who participated in BRS and who continue to influence the work of the NIH OITE through their participation and feedback.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/feduc.2025.1477509/full#supplementary-material
1. ^Although the focus on Becoming a Resilient Scientist was for biomedical sciences, we embrace an inclusive definition of sciences which includes other behavioral and social sciences.
2. ^The first round of BRS had an additional unit on Emotions and Emotional Intelligence. However, in the subsequent sessions, the content of the session was embedded into the other five lectures to shorten the series without losing content.
3. ^The number that watched the recording is a best estimate. The webinars were conducted over zoom and required pre-registration and the registration link also served as link to the webinar video. Zoom does not account for who pre-registered and watched the video after the live webinar.
4. ^Participants who identified as a facilitator, faculty, or administrator were removed from the analysis as the goal of this study was to look at the impact of the program on trainees.
5. ^Because we do not know the exact demographics makeup of the community of the trainees we are recruiting from, we are unable to tell if the demographic in our sample is representative. However, if we infer from demographics of the broader scientific trainee community, females and racially and ethnically diverse trainees are well represented in our sample (see National Science Foundation, 2022).
6. ^To provide additional context, we compared our sample’s RISC-10 scores with the known means for the general U.S. community population (M = 32.1, SD = 5.4; Campbell-Sills et al., 2009) and college undergraduates (M = 27.2, SD = 5.8; Campbell-Sills and Stein, 2007). We computed the recommended sum score of the RISC-10 (range: 10–40) and found that before BRS, the sample had an average score of 24.7 (SD = 5.7) and post BRS score of 28.0 (SD = 5.3). These scores are notably lower than the general population and below the average for college undergraduates. Previous research on the on RISC-10 have shown that certain trainee populations, such as nursing (e.g., Aloba et al., 2016), medical school students (e.g., Houpy et al., 2017), and those who are having difficulty dealing with stress (Davidson, 2018), have even lower resilience scores. Consistent with this, it is not surprising that our sample—comprising primarily of biomedical trainees, including undergraduates, postdocs, and medical school trainees during a pandemic—also reported lower resilience scores. Alarmingly, pre-BRS scores seem to indicate that the trainees in our sample were in the bottom 25% quartile of the population (see Davidson, 2018). Notably, the post-program increase in RISC-10 scores brings our sample much closer to the average for college undergraduates and 50% quartile of the population. This suggests that the biomedical trainees may face unique stressors that influence their resilience compared to other groups.
Abbott, A. (2020). Huge survey reveals pressures of scientist’s lives. Nature 577, 460–461. doi: 10.1038/d41586-020-00101-9
Ajzen, I. (1991). The theory of planned behavior. Organ. Behav. Hum. Decis. Process. 50, 179–211. doi: 10.1016/0749-5978(91)90020-T
Aloba, O., Olabisi, O., and Aloba, T. (2016). The 10-item Connor–Davidson resilience scale. J. Am. Psychiatr. Nurses Assoc. 22, 43–51. doi: 10.1177/1078390316629971
American Psychological Association. (2020). Available at: https://www.apa.org/topics/resilience/building-your-resilience.
Campbell-Sills, L., Forde, D. R., and Stein, M. B. (2009). Demographic and childhood environmental predictors of resilience in a community sample. J. Psychiatr. Res. 43, 1007–1012. doi: 10.1016/j.jpsychires.2009.01.013
Campbell-Sills, L., and Stein, M. B. (2007). Psychometric analysis and refinement of the connor–Davidson resilience scale (CD-RISC): validation of a 10-item measure of resilience. J. Trauma. Stress 20, 1019–1028. doi: 10.1002/jts.20271
Chan, C., Oey, N. E., and Tan, E. K. (2020). Mental health of scientists in the time of COVID-19. Brain Behav. Immun. 88:956. doi: 10.1016/j.bbi.2020.05.039
Chen, E., McLean, K. C., and Miller, G. E. (2015). Shift-and-persist strategies: associations with socioeconomic status and the regulation of inflammation among adolescents and their parents. Psychosom. Med. 77, 371–382. doi: 10.1097/PSY.0000000000000157
Chen, G., Gully, S. M., and Eden, D. (2001). Validation of a new general self-efficacy scale. Organ. Res. Methods 4, 62–83. doi: 10.1177/109442810141004
Coe, R. (2008). Comparability of GCSE examinations in different subjects: an application of the Rasch model. Oxf. Rev. Educ. 34, 609–636. doi: 10.1080/03054980801970312
Cohen, S., Kamarck, T., and Mermelstein, R. (1983). A global measure of perceived stress. J. Health Soc. Behav. 24:385. doi: 10.2307/2136404
Cohn, M. A., Fredrickson, B. L., Brown, S. L., Mikels, J. A., and Conway, A. M. (2009). Happiness unpacked: Positive emotions increase life satisfaction by building resilience. Emotion, 9, 361–368. doi: 10.1037/a0015952
Connor, K. M., and Davidson, J. R. (2003). Development of a new resilience scale: the Connor-Davidson resilience scale (CD-RISC). Depress. Anxiety 18, 76–82. doi: 10.1002/da.10113
Crocker, J., Voelkl, K., Testa, M., and Major, B. (1991). Social stigma: the affective consequences of attributional ambiguity. J. Pers. Soc. Psychol. 60, 218–228. doi: 10.1037/0022-3514.60.2.218
Davidson, J. R. (2018). Connor-Davidson resilience scale (CDRISC) manual. Unpublished. Available at: https://www.cdrisc.com.
Diekman, A. B., Steinberg, M., Brown, E. R., Belanger, A. L., and Clark, E. K. (2017). A goal congruity model of role entry, engagement, and exit: understanding communal goal processes in STEM gender gaps. Personal. Soc. Psychol. Rev. 21, 142–175. doi: 10.1177/1088868316642141
Drew, C. (2011). Why science majors change their mind: it’s just so darn hard. The New York Times. Available at: https://www.nytimes.com/2011/11/06/education/edlife/why-science-majors-change-their-mind-its-just-so-darn-hard.html.
Evans, T. M., Bira, L., Gastelum, J. B., Weiss, L. T., and Vanderford, N. L. (2018). Evidence for a mental health crisis in graduate education. Nat. Biotechnol. 36, 282–284. doi: 10.1038/nbt.4089
Flahtery, C. (2018). Mental health crisis for grad students. Inside Higher Ed. Available at: https://www.insidehighered.com/news/2018/03/06/new-study-says-graduate-students-mental-health-crisis.
Forbes, S., and Fikretoglu, D. (2018). Building resilience: the conceptual basis and research evidence for resilience training programs. Rev. Gen. Psychol. 22, 452–468. doi: 10.1037/gpr0000152
Frank, A. (2012). Science: It's really, really hard, and That's something to celebrate. Available at: https://www.npr.org/sections/13.7/2012/02/14/146857164/science-its-really-really-hard-and-thats-something-to-celebrate.
Fredrickson, B., Cohn, M., Coffey, K., Pek, J., Finkel, S., and Judd, C. M. (2008). Open hearts build lives: positive emotions, induced through loving-kindness meditation, build consequential personal resources. J. Pers. Soc. Psychol. 95, 1045–1062. doi: 10.1037/a0013262
Gilbreath, B., and Frew, E. J. (2008). The stress-related presenteeism scale [measurement instrument]. Pueblo, CO: Hasan School of Business, Colorado State University.
Grogan, K. E. (2019). How the entire scientific community can confront gender bias in the workplace. Nat. Ecol. Evol. 3, 3–6. doi: 10.1038/s41559-018-0747-4
Hish, A. J., Nagy, G. A., Fang, C. M., Kelley, L., Nicchitta, C. V., Dzirasa, K., et al. (2020). Acceptability and perceived effectiveness of approaches to support biomedical doctoral student wellness: One size doesn’t fit all. International Journal of Doctoral Studies, 15, 653. doi: 10.28945/4669
Hish, A. J., Nagy, G. A., Fang, C. M., Kelley, L., Nicchitta, C. V., Dzirasa, K., et al. (2019). Applying the stress process model to stress-burnout and stress-depression relationships in biomedical doctoral students: a cross-sectional pilot study. CBE Life Sci. Educ. 18, 1–11. doi: 10.1187/cbe.19-03-0060
Houpy, J. C., Lee, W. W., Woodruff, J. N., and Pincavage, A. T. (2017). Medical student resilience and stressful clinical events during clinical training. Med. Educ. Online 22:1320187. doi: 10.1080/10872981.2017.1320187
Johnson, J. R., Emmons, H. C., Rivard, R. L., Griffin, K. H., and Dusek, J. A. (2015). Resilience training: a pilot study of a mindfulness-based program with depressed healthcare professionals. Explore 11, 433–444. doi: 10.1016/j.explore.2015.08.002
Joyce, S., Shand, F., Tighe, J., Laurent, S. J., Bryant, R. A., and Harvey, S. B. (2018). Road to resilience: a systematic review and meta-analysis of resilience training programmes and interventions. BMJ Open 8:e017858. doi: 10.1136/bmjopen-2017-017858
Kim-Cohen, J. (2007). Resilience and developmental psychopathology. Child Adolesc. Psychiatr. Clin. N. Am. 16, 271–283. doi: 10.1016/j.chc.2006.11.003
Kroenke, K., Spitzer, R. L., and Williams, J. B. (2001). The PHQ-9: validity of a brief depression severity measure. J. Gen. Intern. Med. 16, 606–613. doi: 10.1046/j.1525-1497.2001.016009606.x
Maher, M. A., Wofford, A. M., Roksa, J., and Feldon, D. F. (2020). Exploring early exits: doctoral attrition in the biomedical sciences. J. Coll. Stud. Retention Res. Theory Pract. 22, 205–226. doi: 10.1177/1521025117736871
Mak, W. W. S., Ng, I. S. W., and Wong, C. C. Y. (2011). Resilience: enhancing well-being through the positive cognitive triad. J. Couns. Psychol. 58, 610–617. doi: 10.1037/a0025195
Mattijssen, L., Van Vliet, N., Van Doorn, T., Kanbier, N., and Teelken, C. PNN PhD survey: asking the relevant questions. Mental wellbeing, workload, burnout, research environment, progress of the PhD project, considering to quit. Promovendi Netwerk Nederland (2020).
Matulevicius, S. A., Kho, K. A., Reisch, J., and Yin, H. (2021). Academic medicine faculty perceptions of work-life balance before and since the COVID-19 pandemic. JAMA Netw. Open 4, –e2113539. doi: 10.1001/jamanetworkopen.2021.13539
Nagy, G. A., Fang, C. M., Hish, A. J., Kelly, L., Nicchitta, C. V., Dzirasa, K., et al. (2019). Burnout and mental health problems in biomedical doctoral students. CBE Life Sci. Educ. 18, 1–14. doi: 10.1187/cbe.18-09-0198
National Science Foundation (2022). Survey of graduate students and Postdoctorates in science and engineering. Available at: https://www.nsf.gov/statistics/srvygradpostdoc/.
Neff, K. D. (2003). Self-compassion: an alternative conceptualization of a healthy attitude toward oneself. Self Identity 2, 85–101. doi: 10.1080/15298860309032
Plieger, T., Melchers, M., Montag, C., Meermann, R., and Reuter, M. (2015). Life stress as potential risk factor for depression and burnout. Burn. Res. 2, 19–24. doi: 10.1016/j.burn.2015.03.001
Preacher, K. J., and Hayes, A. F. (2004). SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behav. Res. Methods Instrum. Comput. 36, 717–731. doi: 10.3758/BF03206553
Preacher, K. J., Rucker, D. D., and Hayes, A. F. (2007). Addressing moderated mediation hypotheses: theory, methods, and prescriptions. Multivar. Behav. Res. 42, 185–227. doi: 10.1080/00273170701341316
Prendergast, M., Cardoso Pinto, A. M., Harvey, C.-J., and Muir, E. (2024). Burnout in early year medical students: experiences, drivers and the perceived value of a reflection-based intervention. BMC Med. Educ. 24:7. doi: 10.1186/s12909-023-04948-0
Reivich, K. J., Seligman, M. E. P., and McBride, S. (2011). Master resilience training in the U.S. Army. Am. Psychol. 66, 25–34. doi: 10.1037/a0021897
Robertson, I., Cooper, C., Sarkar, M., and Curran, T. (2015). Resilience training in the workplace from 2003 to 2014: a systematic review. J. Occup. Organ. Psychol. 88, 533–562. doi: 10.1111/joop.12120
Seligman, M., Schulman, P., and Sarason, I. G. (1986). Explanatory style as a predictor of productivity and quitting among life insurance sales agents. J. Pers. Soc. Psychol. 50, 832–838. doi: 10.1037/0022-3514.50.4.832
Spitzer, R. L., Kroenke, K., Williams, J. B., and Löwe, B. (2006). A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch. Intern. Med. 166, 1092–1097. doi: 10.1001/archinte.166.10.1092
Sutton, A. (2016). Measuring the effects of self-awareness: construction of the self-awareness outcomes questionnaire. Eur. J. Psychol. 12, 645–658. doi: 10.5964/ejop.v12i4.1178
Thogersen-Ntoumani, C., Black, J., Lindwall, M., Whittaker, A., and Balanos, G. (2017). Presenteeism, stress resilience, and physical activity in older manual workers: a person-centred analysis. Eur. J. Ageing 14, 385–396. doi: 10.1007/s10433-017-0418-3
Thoman, S. E., DiBona, T., Abelar, J., and Robnett, R. D. (2020). STEMing from scholarship and resilience: a case study focusing on US undergraduate women who are thriving in STEM. Int. J. Gend. Sci. Technol. 12, 122–151.
Van Katwyk, P. T., Fox, S., Spector, P. E., and Kelloway, E. K. (2000). Using the job-related affective well-being scale (JAWS) to investigate affective responses to work stressors. J. Occup. Health Psychol. 5, 219–230. doi: 10.1037/1076-8998.5.2.219
World Health Organization. Burn-out an occupational phenomenon: International classification of diseases. (2019). Available at: https://www.who.int/news/item/28-05-2019-burn-out-an-occupational-phenomenon-international-classification-of-diseases.
Keywords: resilience, resiliency, biomedical science trainees, intervention program, culture of science
Citation: Han HA, Klenke U, McNulty LC, Scheiner A and Milgram SL (2025) Becoming a resilient scientist series: an intervention program. Front. Educ. 10:1477509. doi: 10.3389/feduc.2025.1477509
Received: 07 August 2024; Accepted: 30 January 2025;
Published: 20 February 2025.
Edited by:
Rebekah L. Layton, University of North Carolina at Chapel Hill, United StatesReviewed by:
M. Zachary Rosenthal, Duke University, United StatesCopyright © 2025 Han, Klenke, McNulty, Scheiner and Milgram. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: H. Anna Han, YW5uYS5oYW5AbmloLmdvdg==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.