- Department of Anatomy and Neurobiology, Boston University Aram V. Chobanian & Edward Avedisian School of Medicine, Boston, MA, United States
Bloom’s Taxonomy is an andragogical tool that classifies educational objectives, learning activities, and assessments into distinct levels of cognitive thinking. Preclinical medical sciences educators aim to promote higher-order thinking in their curricula to help students develop clinical decision-making skills and foster deep learning. However, many courses and curricula remain focused on lower levels of Bloom’s Taxonomy because they are easier to implement and assess. Meanwhile, many service-learning opportunities for medical students focus on developing affective faculties over higher-level cognitive processing of curricular material. We describe a model program in which undergraduate pre-medical education (UPE) and undergraduate medical education (UPE/UME) students at Boston University Charles River Campus (BU CRC) and Boston University Aram V. Chobanian & Edward Avedisian School of Medicine (BU Chobanian & Avedisian SOM) simultaneously engaged in service-learning and the Create level of Bloom’s Taxonomy by developing a supplementary high school (HS) medical science curriculum based on content and instructional models from their preclinical courses. Activities such as mock patient cases, simulated patient interviews, and physical examination training contributed toward a HS curriculum that promotes healthy habits; increases community public health self-efficacy; sparks interest in Science, Technology, Engineering, Math and Medicine (STEMM) concepts; and educates about medical careers through engaging lessons and activities focused on human anatomy and physiology.
1 Introduction
At the core of any undergraduate pre-medical education (UPE) and undergraduate medical education (UME) curriculum are the objectives to comprehend, as well as apply, a vast amount of anatomical and physiological information. A good scientific foundation forms the knowledge base needed to understand the mechanisms of disease and treatment, while critical thinking is essential for clinical decision-making in the forms of diagnosis, selecting treatments, and interpreting results.
Published in 1956, the Taxonomy of Educational Objectives outlined by Benjamin Bloom and his colleagues describes three domains of learning: cognitive, affective, and psychomotor (Bloom, 1956). The cognitive domain encompasses intellectual skills foundational to academic learning, and thus is often the major focus of most educational curricula. Bloom’s Taxonomy is a hierarchical framework featuring six distinct levels of processing within the cognitive domain, progressing from simple recall to complex creation. Curricular designs that move students through each stage help ensure a comprehensive development of cognitive skills, preparing learners to apply their knowledge effectively in varied contexts (Adams, 2015).
The six levels of Bloom’s Taxonomy are:
1. Remembering – involves recalling factual information and basic concepts.
2. Understanding – entails interpreting information and explaining ideas.
3. Applying – using information, methods, and concepts in new situations, such as problem-solving.
4. Analyzing – breaking down information into its components to explore relationships between concepts.
5. Evaluation – assessing new situations based on defined criteria and assessment algorithms, such as evaluating the effectiveness or validity of a solution.
6. Creating – synthesizing knowledge to generate novel ideas, perspectives, and/or products.
Generally, Levels 1–2 (Remembering and Understanding) are considered as lower-order thinking on the taxonomy while Levels 3–6 (Applying to Creating) are considered as higher-order (Thompson and Lake, 2023).
As the upper levels of Bloom’s Taxonomy are better aligned with critical decision-making and long-term retention, medical science educators have been interested in devising and modifying training curricula to promote immersion at these hierarchical levels. However, research has found that many medical programs focus disproportionately on the lower levels of Bloom’s Taxonomy, with few opportunities to take learning to the higher levels (Blanco et al., 2014).
Separately, medical institutions have introduced service-learning programs as components of their preclinical curricula because of the benefits to both the community and the medical students (Stewart and Wubbena, 2014). These programs involve direct student involvement with partnered organizations to address local community needs, and typically enhance the preclinical learning experience by explicitly fostering faculties in the affective domain of learning as outlined by Bloom and his colleagues, including altruism and dutifulness (Bloom, 1956; Bartz et al., 2022).
However, the utilization of service-learning programs to enhance cognitive, particularly within the Create level of Bloom’s Taxonomy, has not been well documented in the current literature. In this paper, we describe the adaptation of the Anatomy Academy curriculum (Diaz et al., 2019; Adams et al., 2021; Wisco et al., 2022) entirely designed by UPE/UME students specifically for a community partner in Boston, MA. This serves as a model of curriculum generation and self-directed learning for service-learning experiences for UPE/UME students that provides unique learning opportunities via simultaneous development of cognitive faculties at the Create level and meeting the needs of local communities.
2 Andragogical framework
2.1 Anatomy academy: a health education program that fosters interest in STEMM
Anatomy Academy is a community-based educational program that originated in Los Angeles, CA in 2012, designed to improve the health self-efficacy of K-12 students and improve the overall community public health awareness. Anatomy Academy aims to promote healthy lifestyle habits, spark interests in STEMM, and help students learn about medical careers through engaging lesson plans and hands-on activities focused on human anatomy and physiology. UPE/UME students at Boston University Charles River Campus (BU CRC) and at Boston University Chobanian and Avedisian School of Medicine (BU Chobanian & Avedisian SOM) serve as program Coordinators and Mentors through the Anatomy Academy Clubs on both campuses and are involved with creating and updating curricular materials that are modeled after their own course learning experiences.
The HS Anatomy Academy lessons are weekly 1 hour long sessions that take place after the HS students are released from school. These sessions are held 10 times per semester on a two-semester academic calendar. The UPE/UME students serving the community as program Coordinators and Mentors of K-12 students also function as creators and teachers of the content. In the context of their own education, they are operating at the highest levels of Bloom’s Taxonomy, thus benefiting their own preclinical education.
During each lesson, two UPE/UME mentors lead the session while the other UPE/UME mentors help facilitate the dissemination of content through engaging activities. UPE/UME student teachers serve as patient actors during the beginning of the sessions when the HS students practice interviewing a patient. Typically, the class is arranged with two to three HS students sitting together with one or two UPE/UME students. This allows the HS students to ask the UPE/UME students questions throughout the lesson and encourages the HS students to stay on task.
2.2 Match Charter Public High School (MCPHS)
The High School (HS) Anatomy Academy program is currently offered to students in grades 9–12 at the Match Charter Public High School (MCPHS) in Boston, MA. The university-community partnership with MCPHS significantly benefits the community by addressing educational, health, and professional development needs. This collaboration provides high school students with exposure to medical professions, fostering interest in healthcare careers and improving health literacy in a predominantly minority community and serving the need for more ethnic and gender diversity in science and medicine.
The MCPHS serves a diverse student body of 1,225 students from pre-kindergarten-12. The school boasts a minority student enrollment of 99% and maintains a student-teacher ratio of 10:1, with 124 full-time teachers and 2 school counselors. Academically, the school faces challenges, with only 16% of students achieving proficiency in math and 31% in reading, figures that are consistent with district averages but lower than state averages, where 33 and 47% of students are proficient in math and reading, respectively. The student population is evenly split by gender, with 51% female and 49% male students. In state rankings, Match Charter Public School falls between #719–958 for elementary schools and #369–492 for middle schools in Massachusetts, based on performance metrics including state-required tests and graduation rates, as well as their preparedness for high school. The Anatomy Academy program’s implementation in a high school with a significant proportion of students from minority backgrounds addresses the critical need for greater ethnic and gender diversity in science and medicine (Match Charter Public School, n.d.).
3 Learning objectives
The structure of the Anatomy Academy curriculum benefits both the HS students that go through the program and the UPE/UME students that create the curriculum and teach the program. Thus, there are learning objectives for both the HS students and the UPE/UME students.
HS student learning objectives
1. HS students will develop increased awareness of health and confidence in a clinical setting.
2. HS students will have opportunities to develop their self-efficacy with regard to increased knowledge of careers in medicine that inform an interest in exploring and pursuing healthcare careers.
3. HS students will become proficient at basic patient intake interview skills.
4. HS students will be able to describe the basic conceptual physiology of common diseases that family members and friends can understand.
5. HS students will reinforce foundational human anatomy concepts taught in their regular school curriculum.
6. HS students will demonstrate best practices for starting and maintaining a healthy lifestyle (e.g., vaccination, hand washing, visiting a PCP, smoking cessation).
UPE/UME student learning objectives
1. UPE/UME students will apply their knowledge and understanding of scientific principles taught in their program curricula.
2. UPE/UME students will increase in confidence of bedside manners and patient interviewing skills as a result of teaching HS students foundational patient interaction techniques.
3. UPE/UME students will have greater confidence in performing physical exam maneuvers after teaching foundational maneuvers to HS students.
4. UPE/UME students will create curricula for the HS students that they teach based on their knowledge and understanding of scientific and physical exam skills.
4 Experiences to date
4.1 Incorporating UPE/UME student experiences into the design of a curriculum
The highest-order level of thinking in Bloom’s Taxonomy – Create – involves reorganizing ideas and elements into new structures to synthesize original ideas, projects, and/or solutions. This level of engagement leads to enhancements in problem-solving abilities and preparation for real-world challenges. Currently, the literature on creation opportunities in a curriculum predominantly documents instances of students generating question repositories, or presenting knowledge in alternative media formats (van der Vleuten and Swanson, 1990; Feijóo-García and Gardner-McCune, 2019). However, the benefits of such products are often limited to the boundaries of the institution’s student body and faculty. For instance, supplemental practice question banks primarily improve the course for instructors and future cohorts. In contrast, service-learning experiences offer UPE/UME students opportunities to create products that benefit local community members outside the school. These experiences are uniquely valuable to medical student education, as the affective faculties fostered through service-learning promote public health self-efficacy and cultural competence.
The UPE curriculum for healthcare classes varies by course and College, but all relevant courses focus on introducing pertinent basic anatomical and physiological concepts to students, rather than developing patient interviewing skills and survey medical careers. Thus, when UPE students help develop the HS Anatomy Academy curriculum, they also gain a unique opportunity to explore the relation of concepts in human biology to medicine. The incorporation of peer tutors, interactive sessions, and clinical relevance into the Anatomy Academy curriculum aligns with recommended best practices for optimizing anatomy instruction, scaled down to a high school level (Baker, 2022).
The primary pre-clinical course for UME student instruction at BU Chobanian & Avedisian SOM is the Principles Integrating Science, Clinical Medicine, and Equity (PISCEs), which features three foundational modules followed by eight systems-based (e.g., cardiovascular, neuro/psych) modules. Longitudinal threads that include oncology, infectious disease, anatomy, microbiology, pharmacology, and pathology, as well as the school’s health equity curricular themes are woven into the modules. The preclinical curriculum, called the Advanced Integration in Medicine, focus on integrated cases based on the BU Core patient presentations organized by clinical areas and disciplines (Chobanian and Avedisian SOM Curriculum, n.d.). PISCEs employs a flipped classroom andrological design and an instructional approach through Case-Based and Team-Based Learning that teaches the thought process of diagnostic schema.
The HS Anatomy Academy program mimics the college and medical school educational environment; therefore, the HS students are taught foundational knowledge through pre-class work, and in-person instruction provided by UPE/UME students is dedicated toward guiding the HS students through mock or real anonymized patient cases from initial presentation to discharge. This instructional style helps prepare the UPE students for future medical school instruction, and the UME students for their clerkship years by helping them reason through the clinical decision-making that they will use via teaching. The process for all students promotes cognitive operations at higher levels of Bloom’s Taxonomy, transitioning students from Remembering and Understanding (pre-class work) to Applying, Analyzing, and Evaluating (in-class patient cases), and finally to Creating (the HS curricula).
4.2 Outreach/service-learning that improves public health self-efficacy
We illustrate the creation of the HS Anatomy Academy curriculum as an example of how UPE/UME students at any institution can reinforce the concepts they are learning in classes through the creation of a product that benefits a community’s public health self-efficacy.
Modeling UPE courses that provide an overview of key topics in healthcare, and the instructional approach utilized in PISCEs, UPE/UME introduced a new organ system in each weekly session to the HS students at MCPHS. The depth of material was adjusted accordingly to the developmental understanding of HS students. We applied a four-part framework to each session to maintain course consistency. In each class, students were introduced to one new disease, one new diagnostic technique, one new physiological concept, and one relevant treatment, management, or prevention strategy. This incremental presentation of new information was designed to minimize cognitive load on the HS students, freeing more bandwidth for reviewing and reinforcing previously covered material.
HS Anatomy Academy also employed a case-based instructional approach, first introducing students to a patient case, followed by pertinent physiology and covering management of the condition last (Figure 1). This approach aimed to enhance student engagement, especially since the hour-long sessions were held after a full day of regular classes. Educating students about their health and promoting health consciousness is one of the core goals of the program; thus, sessions begin with the aspects of medicine likely to be most interesting and engaging for the HS students. At the conclusion of each session, relevant physiological concepts were presented and connected to the material taught in their core science classes. Therefore, the UPE/UME students coordinated their curricular creations with both the MCPHS science and BU Chobanian & Avedisian SOM preclerkship curricula. The purposeful coordination educates HS students about medical diseases and reinforces their understanding of basic high school science. Additionally, the curriculum introduced students to healthcare careers and stimulated their interest in the medical field specifically.
In a typical one-hour session, students engaged with a mock patient presentation through an interactive actor session. Groups of approximately three HS students and two UPE/UME mentors simulated a clinical encounter, with one UPE/UME student acting as the patient and the HS students taking on the role of healthcare providers. The other UPE/UME student assisted in guiding the history-taking process. After this interactive session, the class reconvened, and the UPE/UME students reviewed the key history points gathered during the acting session. They then provided a brief interactive lecture in which the new physiology, diagnostic, treatment techniques for the session are introduced (Figures 2–4). All HS-UPE/UME interactivity were monitored by teachers and approved by faculty advisors of BU Chobanian & Avedisian SOM.
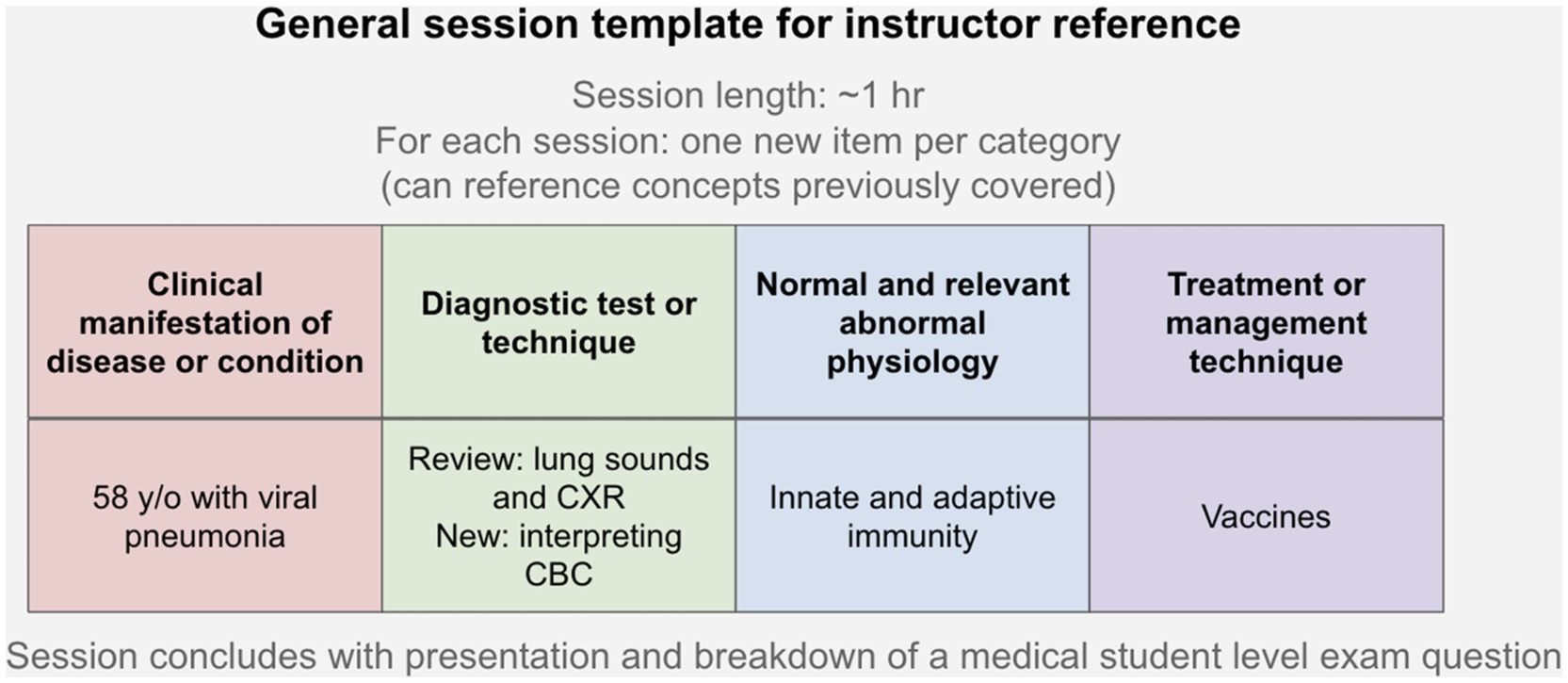
Figure 2. Visual representation of: (top row) the general framework applied to all HS Anatomy Academy sessions, and (bottom row) application of each framework component to the infectious diseases session.
Figure 3. A slide from the HS Anatomy Academy curriculum’s infectious disease session that introduces the students to an infectious disease doctor, a less commonly recognized subspecialty of medicine.
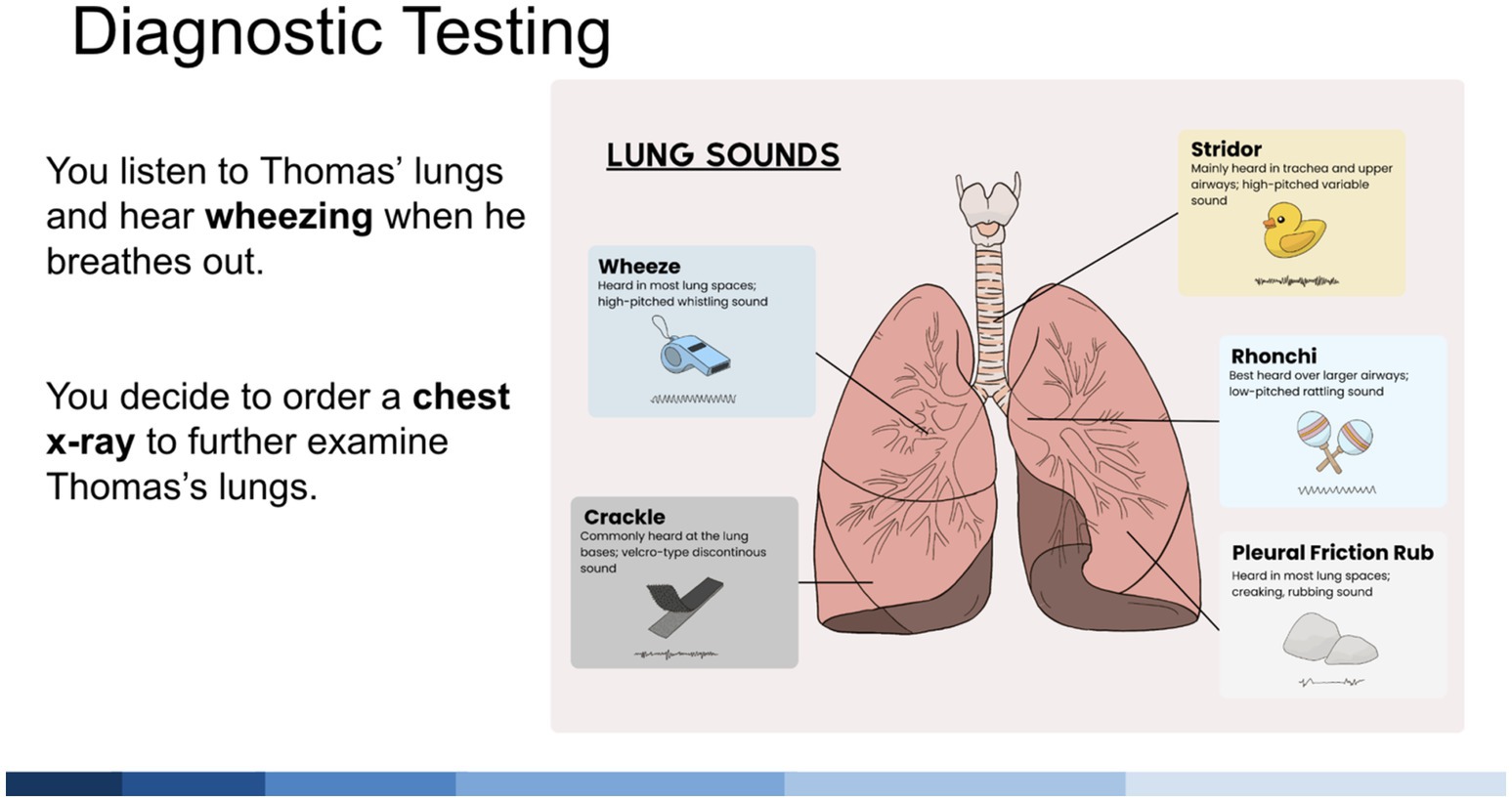
Figure 4. A slide from the HS Anatomy Academy curriculum’s pulmonary session that introduces the students to basic anatomy and physiology of the lower airway from a clinical perspective.
Throughout the presentation, HS students were engaged with open-ended questions designed to stimulate critical thinking and apply clinical information to the case. Example questions include: “Do you think it’s normal to hear crackling when you listen to someone’s lungs with a stethoscope?” or “Have you heard of an infectious disease doctor before?.” Additionally, multiple-choice questions, modeled after medical student board exams, were posed to reinforce the material covered in the presentation (Figure 5). These questions were tackled in small groups, aiming to solidify the students’ understanding. Each learning session also included at least one hands-on activity to further retain HS student engagement while encouraging them to draw connections between the information presented and real-life disease management. For example, HS students were asked to create a working model of the lungs out of a balloon and a water bottle.
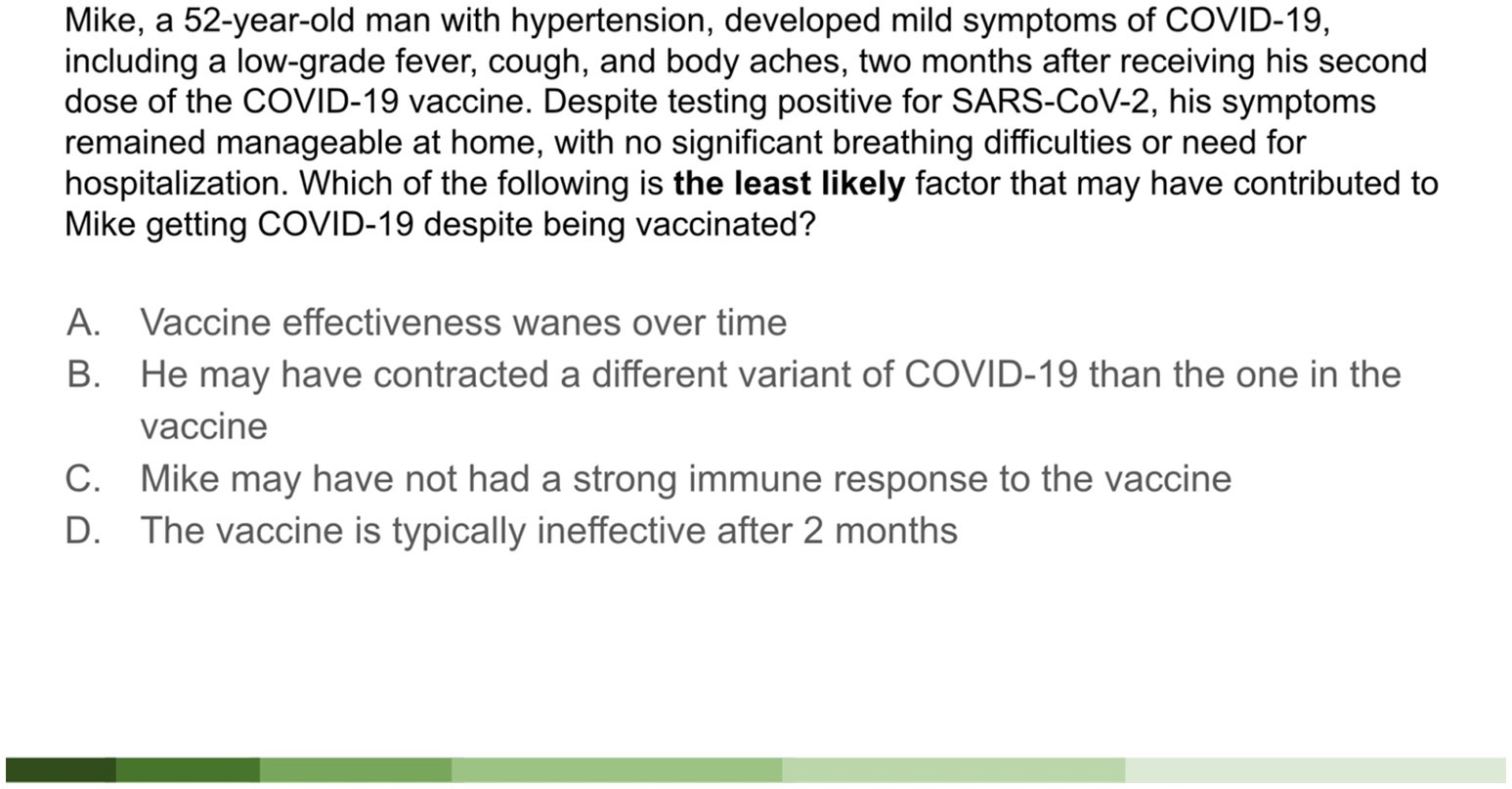
Figure 5. A slide from the HS Anatomy Academy infectious diseases presentation displaying a mock UPE/UME student-level exam question. The UPE/UME mentors will help the HS students dissect the question stem line-by-line and walk students through understanding each answer choice.
Full slide decks from the pulmonary and the infectious disease lessons are provided as Supplementary materials.
To further enhance the HS students’ medical reasoning and exposure to clinical skills, three of the ten HS Anatomy Academy sessions per academic year were held at the Clinical Skills Simulation Center (CSSC) at BU Chobanian & Avedisian SOM. UPE/UME mentors met with the HS students at MCPHS and accompanied their commute to the CSSC via on-campus shuttles, a transportation solution that incurs no cost to MCPHS nor the UPE/UME mentors.
The CSSC is equipped with adult auscultation mannequins capable of producing normal and abnormal cardiovascular and pulmonary physical exam sounds, as well as functional patient exam rooms fitted with exam tables and aneroid sphygmomanometers. During the HS Anatomy Academy clinical skills sessions at the CSSC, groups of approximately four HS students and one UPE/UME mentor rotated between exam room stations dedicated to specific physical examination skills, such as cardiovascular auscultation, blood pressure management, and patient intake interviewing. Through these interactive activities, UPE/UME mentors reinforced their own patient care skills taught in their preclinical curriculum by teaching HS students the foundational bedside manner and examination maneuvers used in primary care settings.
4.3 Alignment with recommended quality assurance standards
The HS Anatomy Academy curriculum aligns closely with key recommendations from well–regarded literature on curriculum quality assurance, including the 2022 FIP Global Framework for Quality Assurance of Pharmacy Education (Chung Sea Law, 2010; Ebel et al., 2019; Meštrović et al., 2022; Ibad, 2024):
1. Anatomy Academy employs competency-based education by designing sessions that introduce a new disease, diagnostic technique, physiological concept, and management strategy, which build both the foundational and applied knowledge of students incrementally. This alignment with the FIP’s emphasis on defining and systematically assessing competencies ensures that high school students gradually acquire essential health-related skills.
2. Anatomy Academy tailors the depth of instructional material to the developmental understanding of a high school audience. This aligns with the FIP’s recommendation for contextual relevance, which encourages educational content to be accessible and meaningful for learners at different stages.
3. End-of-class reflections among UME and UPE mentors, along with formal assessments at the conclusion of the academic year, demonstrate a commitment to the FIP principle of continuous improvement and are elaborated upon in Section 4.4.
4. The program exemplifies FIP’s call for stakeholder involvement as it involves coordination among local educational institutions (MCPHS and BU Chobanian & Avedisian SOM) to align content with both high school science and medical preclerkship curricula. This collaborative approach not only ensures curricular relevance but also fosters global collaboration, with potential for scalability and adaptation by other institutions.
5. The incorporation of clinical skills training into the curriculum demonstrates an integration of technology and innovative teaching methods, another FIP priority, by utilizing simulation techniques that promote active learning and student engagement.
In summary, the HS Anatomy Academy curriculum exemplifies several FIP recommendations for enhancing quality in education, particularly through competency-based, contextually relevant, and continuously improving teaching methods that are responsive to the needs of students and communities alike.
4.4 Future directions
The quality of the HS Anatomy Academy curriculum will be assured and assessed through progressive monitoring of the HS students’ learning, monthly discussions between the program directors and UPE/UME mentors, and a formal narrative analysis at the end of the 2024 academic year. Additionally, as informal progress assessments of the curriculum, UPE/UME mentors involved in teaching a session meet for 10 min at the conclusion of class to discuss HS student learning and engagement throughout the session. The mentors will share how students learned and retained information throughout the session, and which activities promoted their learning. Such preliminary results will help fine-tune the curriculum as it executed during its debut year. For instance, if the HS students are not able to engage effectively with the multiple-choice questions embedded in the session presentations because they are too difficult or too easy, questions for future sessions will be modified accordingly.
Additionally, we will formally assess the program’s efficacy in meeting our learning objectives for both the UPE/UME mentors and HS student mentees via a mixed-methods approach. Mentors and students will respond to surveys involving a combination of Likert-scale questions and free text (please refer to the Supplementary materials). The UPE/UME mentor survey will evaluate the mentors’ perceived impact of their involvement with HS Anatomy Academy in their confidence in recalling medical knowledge, explaining medical concepts to patients, and bedside manners. The HS student survey will evaluate the student’s perceived impact of their HS Anatomy Academy experience in their confidence in recalling medical knowledge, explaining medical concepts to family and friends, and understanding of healthcare career avenues. We will carefully review the results of the surveys and make adjustments to our program as needed.
5 Discussion
It is established that encouraging learning engagement beyond the levels of Remember and Understand into Apply, Analyze, and Evaluate along Bloom’s Taxonomy yields a greater understanding of the material (Thompson and Lake, 2023). Similarly, the value of service-learning opportunities for medical student education is already well documented. Service learning has been shown to not only increase medical students’ sense of social responsibility, but also volunteerism has been shown to have a positive effect on medical students’ grades and USMLE scores (Blue et al., 2006; Meili et al., 2011).
Unfortunately, opportunities to reinforce knowledge and understanding of preclinical undergraduate and medical school courses at the Create level of Bloom’s Taxonomy are uncommon, and the vast majority do not involve service learning. For instance, the Mohammed Bin Rashid University of Medicine found increased student satisfaction and perceived depth of knowledge upon completion of a program in which preclinical students generated weekly formative multiple-choice practice questions for each other. However, the results were based on subjective measures rather than objective student performance on an end-of-module assessment, and the program does not provide any benefit to individuals or communities outside the academic course (Lakhtakia et al., 2022). Such limitations are echoed by medical and non-medical programs at other institutions, in which the student-generated products primarily serve the academic community they emerge and thus align better with curricular improvement initiatives rather than community outreach (Zurcher et al., 2016; Sibomana et al., 2020).
Meanwhile, a longitudinal service-learning program developed by Baylor University offers avenues for students to positively impact local communities by connecting participants with a network of approved community sites curated by the program directors, spanning various social determinants of health from food insecurity to incarceration. However, the program is primarily focused on helping students gain exposure to the structure and operation of community programs, rather than Create a novel product or idea to help serve the communities being addressed (Wong et al., 2022).
An earth sciences outreach program conducted by Louisiana State University (LSU) was among the only studies we encountered that included both Creation and service-learning opportunities. In the program, LSU undergraduates create presentations on volcanoes for K-12 students to enhance the grade students’ understanding of the topic. However, impact on the K-12 students was determined subjectively and indirectly via focus group interviews with the K-12 instructors. Furthermore, it was only predicted, not determined, that the creation opportunity for LSU undergraduates would lead to improved retention and understanding of materials (Nunn and Braud, 2013).
The HS Anatomy Academy curriculum described in this paper provides a model opportunity to merge service learning projects with the Create level of Bloom’s Taxonomy for the preclinical and premedical undergraduate fields. Developed according to the unique needs and requests of MCPHS students, our materials expand on the model employed at LSU by supplementing presentations of anatomy and physiology with hands-on learning with elementary skills in patient examination, mock patient interviews, and discussions of healthcare professions. Furthermore, higher-order learning can be motivating to prime future healthcare professional generations to Create at earlier stages in their career journeys, which will benefit both student academic growth and their broader communities.
While evaluations of the Anatomy Academy program described in this paper are presently being conducted, based on existing research surrounding Bloom’s Taxonomy and service-learning programs we predict that this curricular model will be more effective than other service learning programs in deepening the understanding of taught materials for both the HS and UME students involved in the program. Other universities and health professions schools may consider implementing our dual learning model for their community partnerships.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
AS: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Resources, Validation, Writing – original draft, Writing – review & editing. MT: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Resources, Validation, Writing – original draft, Writing – review & editing. SA: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Resources, Writing – original draft, Writing – review & editing. KC: Data curation, Investigation, Methodology, Resources, Visualization, Writing – original draft, Writing – review & editing. JW: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. The authors acknowledge the generosity of the John E. and Sarah M. McGinty Foundation; the Campbell Foundation; and the anonymous benefactors who donated to the Boston University Aram V. Chobanian & Edward Avedisian School of Medicine, Anatomy and Neurobiology Start-up fund to support student mentored research.
Acknowledgments
The HS Anatomy Academy curriculum is a collaboration between UPE students at BU CRC and UME students at BU Chobanian & Avedisian SOM, tailored to meet the needs of a high school located in the same city. It is only one instance of such a system; since each institution and surrounding environment have unique characteristics, the logistics of implementing outreach/service-learning opportunities with options for volunteers to engage in creation of curricula will vary based on specific community needs and other location-specific factors. However, the general approach can be applied at any undergraduate and health sciences institution, with the instructional materials tailored to high schools, grade schools, or community members at large.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/feduc.2024.1446513/full#supplementary-material
References
Adams, N. E. (2015). Bloom’s taxonomy of cognitive learning objectives. J. Med. Libr. Assoc. 103, 152–153. doi: 10.3163/1536-5050.103.3.010
Adams, J., Nelson, H., Strong, E., Wisco, J., and Klappa, S. (2021). Mentors’ experience in teaching basic science concepts in the community outreach program, anatomy academy: a phenomenological study. HAPS ED 27–35, 27–35. doi: 10.21692/haps.2020.017
Baker, K. G. (2022). Twelve tips for optimising medical student retention of anatomy. Med. Teach. 44, 138–143. doi: 10.1080/0142159X.2021.1896690
Bartz, D., Pelletier, A., Alexander, E. K., Osman, N. Y., and Johnson, N. R. (2022). Service learning and the medical student affective domain. Clin. Teach. 19, 247–250. doi: 10.1111/tct.13478
Blanco, M. A., Capello, C. F., Dorsch, J. L., Perry, G., and Zanetti, M. L. (2014). A survey study of evidence-based medicine training in US and Canadian medical schools. J. Med. Libr. Assoc. 102, 160–168. doi: 10.3163/1536-5050.102.3.005
Bloom, B. S. (Ed.) (1956). Taxonomy of educational objectives: The classification of educational goals. Handbook I: Cognitive domain. New York, NY, US: David McKay Company.
Blue, A. V., Geesey, M. E., Sheridan, M. E. B., and Basco, W. T. J. (2006). Performance outcomes associated with medical school community service. Acad. Med. 81, S79–82. doi: 10.1097/00001888-200610001-00020
Chobanian and Avedisian SOM Curriculum. (n.d.). Available at: https://www.bu.edu/academics/camed/programs/busm-curriculum/
Chung Sea Law, D. (2010). Quality assurance in post-secondary education: the student experience. Qual. Assur. Educ. 18, 250–270. doi: 10.1108/09684881011079125
Diaz, M. M., Ojukwu, K., Padilla, J., Steed, K. S., Schmalz, N. A., Tullis, A., et al. (2019). Who is the teacher and who is the student? The dual service-and engaged-learning pedagogical model of anatomy academy. J. Med. Educat. Curri. Develop. 6, 1–14. doi: 10.1177/2382120519883271
Ebel, R., Ahmed, S., Thornton, A., Watt, C., Dring, C., and Sames, A. (2019). Curriculum assessment practices that incorporate learning outcomes in higher education: a systematic literature review. NACTA J. 64:236+.
Feijóo-García, P. G., and Gardner-McCune, C. (2019). Improving Functional Programming Understanding through Student-Created Instructional Videos. In Proceedings of the 2019 ACM Conference on Innovation and Technology in Computer Science Education (ITiCSE '19). Association for Computing Machinery, New York, NY, USA, 304.
Ibad, W. (2024). The concept of quality in curriculum: a review of the literature on determining curriculum quality. JKPI 14, 104–117. doi: 10.15642/jkpi.2024.14.2.104-117
Lakhtakia, R., Otaki, F., Alsuwaidi, L., and Zary, N. (2022). Assessment as learning in medical education: feasibility and perceived impact of student-generated formative assessments. JMIR Med Educ 8:e35820. doi: 10.2196/35820
Match Charter Public School. (n.d.). U.S. News and World Report. Available at: https://www.usnews.com/education/k12/massachusetts/match-charter-public-school-9243
Meili, R., Fuller, D., and Lydiate, J. (2011). Teaching social accountability by making the links: qualitative evaluation of student experiences in a service-learning project. Med Teach 33, 659–666. doi: 10.3109/0142159X.2010.530308
Meštrović, A., Mukhalalati, B. A. S., Arakawa, N., Al-Haqan, A., Alves da Costa, F., Bates, I., et al. (2022). International Pharmaceutical Federation (FIP) The FIP global competency framework for Educators & Trainers in pharmacy (FIP-GCFE). The Hague: FIP.
Nunn, J. A., and Braud, J. (2013). A service-learning project on volcanoes to promote critical thinking and the earth science literacy initiative. J. Geosci. Educ. 61, 28–36. doi: 10.5408/11-271.1
Sibomana, I., Karenzi, I. D., Niyongombwa, I., Byiringiro, J. C., Gashegu, J., and Ntirenganya, F. (2020). Use of student-generated multiple choice questions to enhance team-based learning of anatomy at the University of Rwanda. Adv. Med. Educ. Pract. 1, 825–832. doi: 10.2147/AMEP.S274298
Stewart, T., and Wubbena, Z. (2014). An overview of infusing service-learning in medical education. Int. J. Med. Educ. 5, 147–156. doi: 10.5116/ijme.53ae.c907
Thompson, A. R., and Lake, L. P. O. (2023). Relationship between learning approach, Bloom’s taxonomy, and student performance in an undergraduate human anatomy course. Adv. Health Sci. Educ. Theory Pract. 28, 1115–1130. doi: 10.1007/s10459-023-10208-z
van der Vleuten, C. P. M., and Swanson, D. B. (1990). Assessment of clinical skills with standardized patients: state of the art. Teach. Learn. Med. 2, 58–76. doi: 10.1080/10401339009539432
Wisco, J. J., Steed, K. S., Read, C. C., Banner, E., and Schmalz, N. A. (2022). Building a service-learning community partnership to expand the classroom learning experience. Boston University Faculty Forum, Boston, MA Abstr 2022 (poster).
Wong, C. K., Berens, P. M., Katta, M. V., Lie, M., Fall, D., Shah, A., et al. (2022). From education to action: development and evaluation of a student-directed service learning program. Med. Teach. 44, 541–545. doi: 10.1080/0142159X.2021.2005242
Keywords: Bloom’s Taxonomy, create level, outreach, service-learning, self-directed learning
Citation: Salas A, Tan M, Andrienko S, Cengiz K and Wisco JJ (2024) Reaching the top of Bloom’s Taxonomy: an innovative pilot program for preclinical undergraduate and medical school students to create curricula for STEMM outreach/service-learning programs. Front. Educ. 9:1446513. doi: 10.3389/feduc.2024.1446513
Edited by:
Jodye I. Selco, California State Polytechnic University, Pomona, United StatesReviewed by:
Arijana Mestrovic, Near East University, CyprusCarla Morais, University of Porto, Portugal
Copyright © 2024 Salas, Tan, Andrienko, Cengiz and Wisco. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jonathan J. Wisco, amp3aXNjb0BidS5lZHU=
†These authors have contributed equally to this work
 Abigail Salas
Abigail Salas Mingqian Tan
Mingqian Tan Sofia Andrienko
Sofia Andrienko Kayra Cengiz
Kayra Cengiz Jonathan J. Wisco
Jonathan J. Wisco