
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
PERSPECTIVE article
Front. Educ., 01 March 2024
Sec. Language, Culture and Diversity
Volume 9 - 2024 | https://doi.org/10.3389/feduc.2024.1357946
This article is part of the Research TopicExploring implicit biases in the educational landscapeView all 7 articles
 Mary Moore1
Mary Moore1 Martha Cuccia2
Martha Cuccia2 Alicia Edwards3
Alicia Edwards3 Chindo Hicks4
Chindo Hicks4 Angela McLean5
Angela McLean5 Christian Nieves-Rivera4,6,7
Christian Nieves-Rivera4,6,7 Gabrielle Sheets4
Gabrielle Sheets4 Kelly Jean Sherman8
Kelly Jean Sherman8 Allison Augustus-Wallace9
Allison Augustus-Wallace9 Fern Tsien4*
Fern Tsien4*In the United States, great inequities exist within the science, technology, engineering, and math (STEM) fields in individuals who self-identify as belonging to underrepresented groups (e.g., from socioeconomically disadvantaged backgrounds, people with disabilities, and Black/African American, Hispanic/Latino, American Indian, Alaska Native, Native Hawaiian, or Pacific Islander). Underrepresentation in STEM careers has been documented to be due to a lack of qualified and diverse teaching personnel, limited access to resources in disadvantaged schools, and implicit bias within US institutions. In recognition of these inequities, an interprofessional team of biomedical faculty members and diversity, equity and inclusion (DEI) educators from the Louisiana State University Health Science Center (LSUHSC) in New Orleans developed and implemented a STEM educational training pipeline for elementary, middle, and high school (K-12), undergraduate, and medical students, with accompanying DEI training for LSUHSC mentors and staff to mitigate implicit bias and promote a welcoming environment for participants from different backgrounds. Our findings focus on one social determinant of health: access and quality of education. Other institutions can implement a program as described in the present study to address the educational and health inequities in their own communities.
Health disparities in the US exist among individuals from socioeconomically disadvantaged backgrounds, people with disabilities, and those who self-identify as Black/African American (AA), Hispanic/Latino (HL), American Indian/Alaska Native (AI/AN), Native Hawaiian, or Pacific Islander (NH/PI) (Williams et al., 2016, 2017; Lee et al., 2018; Spruce, 2019; Sacca et al., 2022; Anderson et al., 2023). Health disparities have been defined as “differences in the incidence, prevalence, mortality, and burden of diseases and other adverse health conditions that exist among specific population groups in the United States” (National Heart, Lung, and Blood Institute, and National Institutes of Health, 2014). Social determinants of health (SDOH), which are the conditions in which people live, learn, work, play, and worship, are known to affect health outcomes (Thornton et al., 2016; Lee et al., 2018; Spruce, 2019; Office of Disease Prevention and Health Promotion et al., 2022). SDOH have a major impact on people’s health, wellbeing, and quality of life, and its inequities create health disparities (Thornton et al., 2016; Lee et al., 2018; Spruce, 2019; Office of Disease Prevention and Health Promotion et al., 2022). The US Department of Health and Social Services categorizes SDOH into 5 domains: (1) economic stability (i.e., employment and access to affordable healthy foods and housing), (2) access and quality of health care, (3) neighborhood and built environment (e.g., violence, unsafe air, or water), (4) social and community context (e.g., children whose parents are incarcerated or deported, bullying, and other lack of community support), and (5) access and quality of education (Thornton et al., 2016; Lee et al., 2018; Spruce, 2019; Office of Disease Prevention and Health Promotion et al., 2022). The present study focuses on one social determinant of health: access and quality of education. The long term goal of our project is that although the intervention we address primarily targets a single social determinant, it will have long term effects across other SDOH (Thornton et al., 2016; Office of Disease Prevention and Health Promotion et al., 2022).
Although more individuals who identify AA, HL, AI/AN, and NH/PI are currently pursuing advanced degrees, disparities still exist in the science, technology, engineering, and math (STEM) fields: only 1.6% of tenured US professors are AA, 2.7% are HL, and 0.4% are AI/AN-NH/PI (Sacca et al., 2022; The National Science Foundation, 2023). Many factors contribute to this phenomenon, including a lack of qualified and diverse teaching personnel and limited access to STEM education resources in disadvantaged schools (Stoeger et al., 2016; Wilson-Kennedy et al., 2018; U.S. Census Bureau, 2020; Gonzales et al., 2021). The US Department of Education’s Civil Rights Data Collection reports that due to a lack of access to quality, early STEM education, a large proportion of underrepresented K-12 students achieves lower standardized test scores and lower acceptance rates to top-ranking colleges. Additionally, inadequate mentor support and implicit bias in institutions may impact outcomes, especially for females and students from disadvantaged groups (National Center for Education Statistics, 2014; Dixson et al., 2016; Stoeger et al., 2016; Wilson-Kennedy et al., 2018; Subotnik et al., 2019; Nation and Hansen, 2021).
Recognizing these educational challenges, a collaborative team of LSUHSC faculty members and diversity, equity and inclusion (DEI) educators developed and implemented a STEM educational pipeline training program for elementary, middle, and high school (K-12), undergraduates, and medical students. Within this program, LSUHSC faculty and staff mentors complete DEI training to mitigate implicit bias and promote a welcoming environment for participants from different backgrounds inclusive of race, ethnicity, gender, sexual orientation, socioeconomic status, citizenship, education, religion, ability, and age. The goals of the program are to improve STEM academic achievement, introduce students to diverse mentors and role models, and increase awareness of future STEM careers.
The Louisiana State University Health Sciences Center (LSUHSC) in New Orleans, LA is comprised of six schools (Medicine, Graduate Studies, Public Health, Nursing, Allied Health Professions, and Dentistry). Each of these schools has its own Diversity, Equity, and Inclusion (DEI) Committee comprised of faculty and trainees who report to the LSUHSC DEI Office. The campus DEI Office leads diversity initiatives by hosting workshops, organizing a health equity campaign with local community partners, and developing a bias/discrimination reporting system. The School of Medicine’s Office of Diversity and Community Engagement (ODCE), established in 1981, is comprised of comprehensive community outreach programs, including partnerships with New Orleans Public Schools, local Historically Black Colleges and Universities (HBCUs), and the Area Health Education Center (AHEC) Southeast Louisiana program for rural scholars. For more than 20 years, LSUHSC has received federal, local, foundational, and institutional funding to support educational pipeline programs for K-12, undergraduate, and medical students (Figure 1). Anonymous formative and summative evaluations by participants have measured satisfaction of the program, demographics, learning gains, topic retention, and long-term tracking of career plans (Table 1).
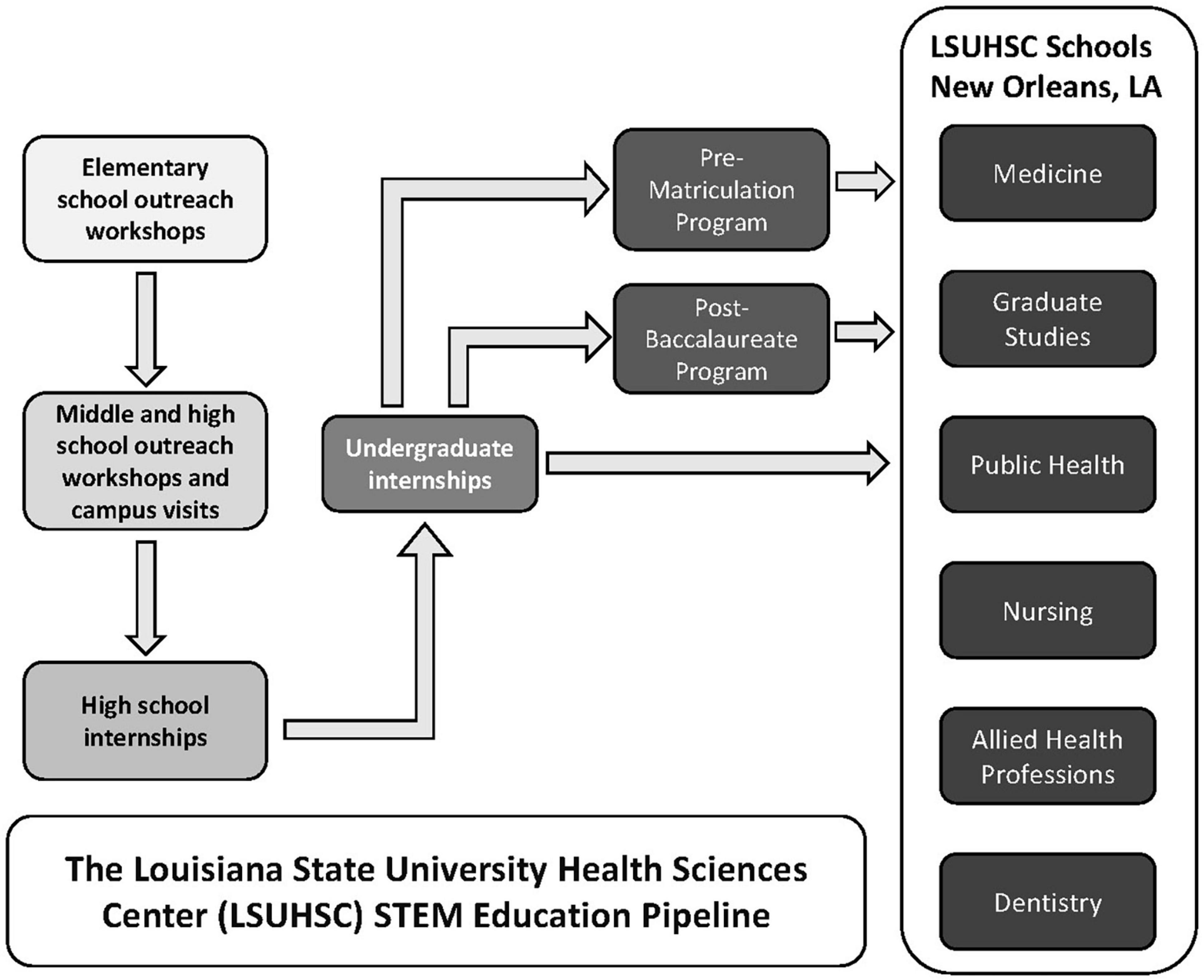
Figure 1. The Louisiana State University Health Sciences Center (LSUHSC) STEM Education Pipeline. Science, technology, engineering, and math (STEM) opportunities at LSUHSC for elementary, middle, high school, undergraduates, and medical students described in the present manuscript. Not all STEM pipeline programs at LSUHSC are listed.
During the academic year (August to May), LSUHSC faculty, trainees, and staff of varying backgrounds teach K-12 students via practical experiments to enhance their science curriculum, improve classroom/standardized test scores, and provide guidance regarding career goals. LSUHSC incentivizes trainees (e.g., medical, nursing, public health, dental and graduate students, residents, and post-doctoral fellows) to provide assistance to faculty members. For instance, medical and nursing students earn service hours for their participation and public health graduate students accrue service hours as they utilize their skills in health promotion. In addition, two courses offer credit to trainees. In the “Interdisciplinary Approach to Science Outreach” course, trainees (1) learn effective collaborative teaching skills with an emphasis on inclusive environments, (2) design science activities for outreach presentations, (3) organize and facilitate their modules for K-12 classes at partnering schools, and (4) inform the community about health and STEM professions. In the “Science Teaching” course, LSUHSC trainees implement already developed curricula (either at the K-12 school or as a field trip to the LSUHSC campus), and offer educational and career advice. These opportunities serve a dual purpose: as future researchers and health professionals, it is essential for trainees to receive training in STEM and health communication with lay audiences; simultaneously, they serve as role models and assist K-12 students with interactive methods to facilitate understanding and retention.
The above mentioned courses and the Science Youth Initiative (SYI) K-12 Program are implemented in collaboration with teachers from the New Orleans Metropolitan area. Starting in the fourth grade, these programs engage in curriculum-related activities with students from underserved communities (e.g., extracting DNA from strawberries, use of organ models). Middle and high school students participate in day-long campus workshops, conducting experiments which complement their curriculum and relate to current and relevant topics (e.g., forensics, cancer research). The ODCE conducts tours of LSUHSC training facilities and laboratories, demonstrating the value of teamwork among health professionals (interprofessional education). A wide variety of STEM and health science careers (e.g., medicine, research, audiology, nursing, health policy, epidemiology) are highlighted. Additionally, LSUHSC facilitators help middle and high school students develop their critical thinking, inductive/deductive reasoning, and test-taking skills. For example, experiments instruct in the use of the scientific method and laboratory proficiency (e.g., DNA analysis using gel electrophoresis, staining of normal and cancer cells, microscope visualization). Organs from the LSUHSC Anatomy and Pathology Departments are utilized to teach topics such as lung disease and alcohol abuse. LSUHSC-created educational videos reinforce the newly acquired information. Surplus laboratory equipment (i. e., thermal cyclers, centrifuges) and supplies (i. e., Eppendorf tubes, flasks), are donated or loaned to the partnering high schools once teachers are trained in their proper use.
Since 2003, the collective mission of the LSUHSC Science Youth Initiative (SYI) and Summer Research Internship (SRI) high school programs is to provide research training/professional development and ensure that all students are encouraged to build their skills, knowledge, and confidence as they move forward in their STEM career goals. All high school interns receive on-line training prior to arriving on campus and up to 2 weeks of basic laboratory preparation before starting on their projects (e.g., reviewing research articles, learning methodology). Students receive professional development seminars on resume writing, laboratory and biological safety, formulating a research hypothesis, experimental design, data interpretation/reaching a conclusion, scientific communication skills (presentation and manuscript writing), responsible conduct in research, and DEI in research; as they master tasks and concepts, their responsibilities increase. Students are offered networking opportunities (e.g., community outreach, workshops with admissions directors and professionals of different careers) with fellow high school students, other summer interns (undergraduates and medical students), and LSUHSC trainees, faculty, and staff.
The LSUHSC STEM Program offers high school students comprehensive training in scientific skills for up to 2 years: (1) during the academic year, interns report after school to an assigned laboratory, where they conduct supervised research projects (2) during the summer, they work full-time and participate in activities with the rest of the interns. Clinical shadowing opportunities are also available to New Orleans area high school students. Since 1982, the ODCE faculty and staff have led the Summer Science Program (SSP), providing high school students with 5 weeks of mentorship, clinical shadowing, and professional development activities for careers in medicine, nursing, and allied health professions.
As undergraduates, students may participate in the Research Experiences for Undergraduates (REU) Program or the SRI program to learn hard scientific skills (hypothesis and research design, methodology, scientific communication), soft skills (time management), professional development (resume/CV writing, career guidance), and to network while providing community outreach. Computational or wet-laboratory projects can be chosen based on student research interests. To support STEM, health sciences, and biomedical pipeline and workforce development initiatives, LSUHSC has established long-standing collaborations with local institutions, including HBCUs.
Institutions of higher learning are increasingly teaching non-traditional students (National Center for Education Statistics, 2014; Wouters, 2020; Sutherland et al., 2023). Non-traditional students may (1) vary in their social, familial and educational backgrounds, (2) tend to have previous work experience, (3) be age 23 years or older at their time of enrollment, and (4) vary in their life situation and/or motivation to study (Gilardi and Guglielmetti, 2011; National Center for Education Statistics, 2014; Wouters, 2020; Sutherland et al., 2023). Non-traditional pre-matriculated medical students can benefit from increased access to mentor guidance, networking with faculty and peers, and gaining understanding of the curriculum prior to navigating medical school (Wouters, 2020; Sutherland et al., 2023). Both the LSUHSC ODCE and the School of Medicine’s Admissions Office direct the Pre-Matriculation Program, which is open to all admitted medical students, but geared toward students (non-traditional included) who consider themselves disadvantaged. Since 1985, the LSUHSC Pre-Matriculation Program has mentored more than 500 incoming medical students; more than 95% have successfully completed their medical degrees.
Furthermore, medical students may participate in a paid internship, an Honors Research Program, or receive credit via various Research Elective courses. Research topics (including health disparities, bioinformatics, translational medicine, and epidemiology) are conducted under the supervision of LSUHSC faculty mentors. Future physicians are trained in (1) communicating health and research topics to the lay community, (2) responsible conduct in research, (3) DEI sensitivity when conducting research, and (4) competitive residency application preparation.
Mentors are chosen based on (1) research experience, (2) teaching achievements, (3) positive reviews from previously mentored high school, undergraduate, or medical students, (4) motivation to empower students of differing backgrounds, (5) previous publications or presentations coauthored with high school, undergraduate, and medical students, and (6) the completion of at least two in-person mentor training workshops before students arrive. LSUHSC incentivizes these initiatives, with mentoring and service included as prerequisites for faculty promotion and tenure. In-person training courses (facilitated by the ODCE or the DEI Office) include workshops on microaggressions and implicit bias. These workshops are facilitated by DEI education leaders at the institutional, state, and national level, with the intention to promote respectful behaviors and to nurture trainees from a wide variety of backgrounds. These 3-h workshops are offered once a month during the academic year, and include videos, seminars, interactive activities, and panel discussions. Facilitators discuss identity, privilege, grit, impostor syndrome, and discrimination, promoting respectful interactions. By gaining a better appreciation of shared experiences and differences, expectations of respect, and the need to belong, faculty and their staff are provided advice on how to create respectful and inclusive workplaces. Additionally, staff training includes individuals who work with participants outside the laboratory (i.e., food services, parking, security, campus assistance, and the wellness center). Anonymous questionnaires determine satisfaction and learning outcomes.
All LSUHSC faculty mentors and staff are required to complete yearly online training, covering sexual harassment, assault, and other forms of harassment and discrimination. These topics are reinforced with mentors and staff during the in-person DEI workshops. All adults supervising students under the age of 18 require a criminal background check and the completion of an online training module by the Louisiana Department of Children and Family Services.
A symbiotic relationship currently exists between the health science professionals at LSUHSC in New Orleans and the lay public. Since 2006, the Science Youth Initiative has served more than 2400 K-12 students, of which 68% self-identify as underrepresented. Quantitative and qualitative analyses demonstrate that the program improves science and math test scores and promotes greater interest in STEM. Age-appropriate anonymous pre- and post-questionnaires demonstrate statistically significant knowledge gains in curricular concepts. Participants express confidence in their understanding of the material and enjoy interacting with the LSUHSC near-peer facilitators. Teachers report improvements in classroom grades and standardized testing scores.
Over 150 high school students, more than 500 undergraduates and over 675 medical students have been immersed in the clinical/research setting since the inception of the SRI and REU programs, where they met peers, faculty, and role models, strengthened resumes, and presented their research at the end-of-the-summer symposium. Participants in these programs also engage in community outreach, providing health information and explaining their projects while serving as role models to the younger generations; more than 60% percent of the interns are from underrepresented backgrounds in STEM. Students’ evaluations report that they “felt like part of the research team” and “felt like a scientist.” As a result of the ODCE clinical shadowing program, more than 400 high school students in the New Orleans area have successfully enrolled in STEM and health programs (Medicine, Nursing, Graduate Studies, Dentistry, and Allied Health) at LSUHSC and other institutions, nationally and abroad. Additional robust programs at the six LSUHSC schools (Medicine, Graduate Studies, Allied Health Professions, Public Health, Nursing and Dentistry) which enhance the diversity of the STEM workforce are not mentioned in the present manuscript.
By the conclusion of the mentor workshops, statistically significant increases in DEI related self-awareness were reported by faculty and staff regarding (1) the importance of improving diversity and recognizing biases and stereotypes, (2) appropriate interaction with people from different cultures, and (3) the acknowledgment of implicit bias when mentoring students from groups underrepresented in STEM fields (Harrison-Bernard et al., 2020).
During the COVID-19 pandemic, concerted efforts were made to support the pipeline programs via a remote learning model. Virtual Summer Program project topics included bioinformatics, protein modeling, and data analytics research, and workshops were held via Zoom. Despite the lack of on-campus research activities during the COVID-19 pandemic, students and mentors readily adapted to the virtual model (Erickson et al., 2022; Sims et al., 2022; Hess et al., 2023).
Academic health science centers provide patient care, train scientists and health professionals, and facilitate basic research; interprofessional teams of different backgrounds can educate and serve as role models. STEM activities, which may include interactive tours of the facilities, and laboratory demonstrations, can be developed collaboratively with schools to complement the K-12 and undergraduate curricula, minimize stereotypes and promote enthusiasm to collaborate with others (Gunaldo et al., 2018, 2020). Educational resources (e.g., laboratory equipment and supplies) can be provided to supplement those at local schools, reducing educational inequities. Local, foundation, and federal funding exists to support these initiatives, providing supplies, administrative assistance, and student stipends. Effective and nurturing mentors have been well documented to be essential for student success (Gonzales et al., 2021; Alvarez-Berrios and Haynes, 2023). Furthermore, many female faculty mentors self-identify as transformational leaders with positive and strong views on guiding and empowering other women in STEM leadership (Francis and Askew, 2022; Alvarez-Berrios and Haynes, 2023). Our program and others suggest a link between student success and improvements in self-perception including sense of belonging, science identity, and self-efficacy (Connors et al., 2021; Callahan et al., 2022; Erickson et al., 2022; Sims et al., 2022; Alvarez-Berrios and Haynes, 2023; Hess et al., 2023).
Since the national enrollment of underrepresented students in STEM higher education and careers remains low (Connors et al., 2021; Callahan et al., 2022; The National Science Foundation, 2023), programs similar to ours are vital and could be successfully implemented by other institutions of higher learning, even under highly variable conditions (Nation and Hansen, 2021). Our program has shown farther reaching impacts than simply advancing educational achievement (e.g., Ph.D, MPH, MS, MD) among our participants. Follow-up efforts from participants since 2003 have revealed long term impacts of the program: many past participants have STEM careers in academia (e.g., professors, researchers), government (e.g., health policy directors, epidemiologists), industry (e.g., engineers, research technicians), healthcare (e.g., physicians, nurses), and law (e.g., patent agents, forensic scientist). Many have presented at local, national, and international meetings, and have published their results as co-authors with their LSUHSC mentors. Our participants report that their educational/career paths have led to employment opportunities, economic stability and improved quality of life. More than 90% of the program alumni who respond to the surveys follow a STEM related educational/career path. The small percentage of alumni who do not pursue STEM careers report that they still greatly benefit from the program’s opportunity to work in a professional setting, career development workshops, and networking experiences. Our efforts focus on one social determinant of health: access and quality of education. Other institutions can implement a program as described in the present study to address the educational and health inequities in their own communities.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving humans were approved by the Louisiana State University Health Sciences Center Internal Review Board. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin.
MM: Data curation, Formal analysis, Investigation, Methodology, Software, Writing – original draft. MC: Investigation, Project administration, Supervision, Writing – original draft, Writing – review and editing. AE: Writing – review and editing. CH: Resources, Software, Writing – review and editing. AM: Funding acquisition, Project administration, Supervision, Writing – review and editing. CN-R: Project administration, Resources, Writing – review and editing. GS: Project administration, Resources, Writing – original draft, Writing – review and editing. KS: Conceptualization, Data curation, Funding acquisition, Methodology, Project administration, Supervision, Writing – review and editing. AA-W: Writing – original draft. FT: Conceptualization, Funding acquisition, Investigation, Methodology, Project administration, Supervision, Writing – original draft, Writing – review and editing.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was supported by the NSF REU (Awards # DBI-1359140, 1659752, and 2051440), NSF BIORETS (Award # 2341385), NIH NCI (Awards# R25CA087994-05 and P20CA202922-04), NIH NINDS, NEI (Award # R25 NS114309), the Patrick F. Taylor Foundation, the Entergy Charitable Foundation, the Baptist Community Ministries, the Joe W. and Dorothy Dorsett Brown Foundation, and the School of Medicine, Louisiana State University Health Sciences Center. Louisiana Office of Public Health, Bureau of Community Preparedness.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Alvarez-Berrios, M. P., and Haynes, G. (2023). Puerto rican students rising in STEM: Findings from a multicampus collaborative CURE program to promote student success. CBE Life Sci. Educ. 22, 1–10. doi: 10.1187/cbe.23-05-0083
Anderson, K. K., Maresh, S., Ward, A., Koller, E. A., Connor, P., Evans, M., et al. (2023). The COVID-19 pandemic’s impact on all-cause mortality disparities in medicare: By race, income, chronic health, mental/behavioral health, disability. Gen. Hosp. Psychiatry 81, 57–67. doi: 10.1016/j.genhosppsych.2023.01.013
Callahan, K. P., Peterson, C. N., Martinez-Vaz, B. M., Huisinga, K. L., Galport, N., Koletar, C., et al. (2022). External collaboration results in student learning gains and positive STEM attitudes in CUREs. CBE Life Sci. Educ. 21, 1–11. doi: 10.1187/cbe.21-06-0167
Connors, P. K., Lanier, H. C., Erb, L. P., Varner, J., Dizney, L., Flaherty, E. A., et al. (2021). Connected while Distant: Networking CUREs across classrooms to create community and empower students. Integr. Comp. Biol. 61, 934–943. doi: 10.1093/icb/icab146
Dixson, D. D., Worrell, F. C., Olszewski-Kubilius, P., and Subotnik, R. F. (2016). Beyond perceived ability: The contribution of psychosocial factors to academic performance. Ann. N. Y. Acad. Sci. 1377, 67–77. doi: 10.1111/nyas.13210
Eller, L. S., Lev, E. L., and Bakken, L. L. (2022). Development and testing of the clinical research appraisal inventory-short form. J. Nurs. Meas. 22, 106–119. doi: 10.1891/1061-3749.22.1.106
Erickson, O. A., Cole, R. B., Isaacs, J. M., Alvarez-Clare, S., Arnold, J., Augustus-Wallace, A., et al. (2022). How do we do this at a distance?! A descriptive study of remote undergraduate research programs during COVID-19. CBE Life Sci. Educ. 21:ar1. doi: 10.1187/cbe.21-05-0125
Francis, K. A., and Askew, K. (2022). The role of mentoring in STEM faculty leadership to broadening participation in STEM faculty and students. J. Soc. Sci. 18, 181–190. doi: 10.3844/jssp.2022.181.190
Gilardi, S., and Guglielmetti, C. (2011). University life of non-traditional students: Engagement styles and impact on attrition. J. Higher Educ. 82, 33–53. doi: 10.1080/00221546.2011.11779084
Gonzales, L. D., Hall, K., Benton, A., Kanhai, D., and Núñez, A. M. (2021). Comfort over change: A case study of diversity and inclusivity efforts in U.S. Higher Educ. Innovat. Higher Educ. 46, 445–460. doi: 10.1007/s10755-020-09541-7
Gunaldo, T., Augustus-Wallace, A., Schilling, D., Hicks, M., Goumas, A., and Levitzky, E. (2020). Gaining an understanding of interprofessional roles and responsibilities among pre-professional health students. Health Int. Pract. Educ. 4:1191. doi: 10.7710/1191
Gunaldo, T. P., Augustus-Wallace, A., Goumas, A., Cheramie, T., Brisco, S., and Levitzky, E. (2018). Integrating interprofessional education into an academic enrichment program. Health Interprofess. Pract. 3:12. doi: 10.7710/2159-1253.1168
Harrison-Bernard, L. M., Augustus-Wallace, A. C., Souza-Smith, F. M., Tsien, F., Casey, G. P., and Gunaldo, T. P. (2020). Knowledge gains in a professional development workshop on diversity, equity, inclusion, and implicit bias in academia. Adv. Physiol. Educ. 44, 286–294. doi: 10.1152/ADVAN.00164.2019
Hess, R. A., Erickson, O. A., Cole, R. B., Isaacs, J. M., Alvarez-Clare, S., Arnold, J., et al. (2023). Virtually the same? Evaluating the effectiveness of remote undergraduate research experiences. CBE Life Sci. Educ. 22, 1–12. doi: 10.1187/cbe.22-01-0001
Lee, J., Schram, A., Riley, E., Harris, P., Baum, F., Fisher, M., et al. (2018). Addressing health equity through action on the social determinants of health: A global review of policy outcome evaluation methods. Int. J. Health Policy Manag. 7, 581–592. doi: 10.15171/ijhpm.2018.04
Nation, J. M. B., and Hansen, A. K. (2021). Perspectives on community STEM: Learning from partnerships between scientists, researchers, and youth. Integr. Comp. Biol. 61, 1055–1065. doi: 10.1093/icb/icab092
National Center for Education Statistics (2014). Nontraditional undergraduates/definitions and data. Available online at: https://nces.ed.gov/pubs/web/97578e.asp (accessed December 15, 2023).
National Heart, Lung, and Blood Institute, and National Institutes of Health (2014). About health disparities. Available online at: https://www.nhlbi.nih.gov/health/educational/healthdisp/about-health-disparities.htm (accessed December 1, 2024).
Office of Disease Prevention and Health Promotion, Office of the Assistant Secretary for Health, Office of the Secretary, and U.S. Department of Health and Human Services (2022). Social determinants of health - healthy people 2030. Available online at: https://health.gov/healthypeople/priority-areas/social-determinants-health (accessed January 19, 2024).
Sacca, L., Shegog, R., Hernandez, B., Peskin, M., Rushing, S., Jessen, C., et al. (2022). Barriers, frameworks, and mitigating strategies influencing the dissemination and implementation of health promotion interventions in indigenous communities: A scoping review. Implement. Sci. 17:18. doi: 10.1186/s13012-022-01190-y
Seymour, E., Wiese, D., Hunter, A., and Daffinrud, S. (2000). Creating a better mousetrap: On-line student assessment of their learning gains. Available online at: https://salgsite.net/about* (accessed December 15, 2023).
Sims, Z. K., Cousin, L., Suppiah, V., Stanley, N., Li, J., Quinn, G., et al. (2022). Improving multi-site interaction through remote learning technology: Report from a training program to increase underrepresented undergraduate and medical students in health disparities research. J. Cancer Educ. 37, 1466–1471. doi: 10.1007/s13187-021-01985-5
Slater, E., Norris, C., and Morris, J. (2021). The validity of the science teacher efficacy belief instrument (STEBI-B) for postgraduate, pre-service, primary teachers. Heliyon 7:e07882. doi: 10.1016/j.heliyon.2021.e07882
Spruce, L. (2019). Back to basics: Social determinants of health. AORN J. 110, 60–69. doi: 10.1002/aorn.12722
Stoeger, H., Schirner, S., Laemmle, L., Obergriesser, S., Heilemann, M., and Ziegler, A. (2016). A contextual perspective on talented female participants and their development in extracurricular STEM programs. Ann. N. Y. Acad. Sci. 1377, 53–66. doi: 10.1111/nyas.13116
Subotnik, R. F., Stoeger, H., and Luo, L. (2019). Exploring compensations for demographic disadvantage in science talent development. N. Dir. Child Adolesc. Dev. 2019, 101–130. doi: 10.1002/cad.20321
Sutherland, K., Brock, G., de Villiers Scheepers, M. J., Millear, P. M., Norman, S., Strohfeldt, T., et al. (2023). Non-traditional students’ preferences for learning technologies and impacts on academic self-efficacy. J. Comput. Higher Educ. doi: 10.1007/s12528-023-09354-5 Online ahead of print.
The National Science Foundation (2023). Characteristics of scientists and engineers with U. S. doctorates. Alexandria, VA: National Science Foundation.
Thornton, R. L. J., Glover, C. M., Cené, C. W., Glik, D. C., Henderson, J. A., and Williams, D. R. (2016). Evaluating strategies for reducing health disparities by addressing the social determinants of health. Health Affairs 35, 1416–1423. doi: 10.1377/hlthaff.2015.1357
U.S. Census Bureau (2020). Population estimates, American fact finder. Available online at: https://data.census.gov/ (accessed September 22, 2023).
Williams, D. R., Priest, N., and Anderson, N. (2017). Understanding Associations between race, socioeconomic status and health: Patterns and prospects. Physiol. Behav. 176, 139–148. doi: 10.1037/hea0000242.Understanding
Williams, D. R., Priest, N., and Anderson, N. B. (2016). Understanding associations among race, socioeconomic status, and health: Patterns and prospects. Health Psychol. 35, 407–411. doi: 10.1037/hea0000242
Wilson-Kennedy, Z. S., Kanipes, M. I., and Byrd, G. S. (2018). Transforming STEM education through collaborative leadership at historically black colleges and universities. CBE Life Sci. Educ. 17, 1–3. doi: 10.1187/cbe.18-06-0088
Keywords: diversity equity and inclusion, STEM, K-12, academic health center, mentor training, pipeline, pathway
Citation: Moore M, Cuccia M, Edwards A, Hicks C, McLean A, Nieves-Rivera C, Sheets G, Sherman KJ, Augustus-Wallace A and Tsien F (2024) How can academic health science centers help to increase diversity in the STEM professions?. Front. Educ. 9:1357946. doi: 10.3389/feduc.2024.1357946
Received: 19 December 2023; Accepted: 13 February 2024;
Published: 01 March 2024.
Edited by:
Nishtha Lamba, Middlesex University Dubai, United Arab EmiratesReviewed by:
Anthony Paul Breitbach, Saint Louis University, United StatesCopyright © 2024 Moore, Cuccia, Edwards, Hicks, McLean, Nieves-Rivera, Sheets, Sherman, Augustus-Wallace and Tsien. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Fern Tsien, Zm1pbGxlQGxzdWhzYy5lZHU=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.