- 1Department of Medical Education, Morehouse School of Medicine, Atlanta, GA, United States
- 2Clear Water Science Consulting Limited, New Territories, Hong Kong SAR, China
- 3Department of Microbiology, Biochemistry and Immunology, Morehouse School of Medicine, Atlanta, GA, United States
Introduction: Health informatics (HI) has the potential to address health disparities and improve healthcare outcomes; however, lack of diversity in the workforce, especially at advanced levels, feeds disparities, and creates inequities. Increasing participation from underrepresented minorities requires exposure and connection to the field and career opportunities including advanced degrees. Morehouse School of Medicine (MSM) created the no-cost, 5-week intensive online Bridge to Health Informatics (B2HI) program in 2021 to connect participants from backgrounds underrepresented in HI with industry-relevant skills, professional certification, business experience, and graduate training opportunities.
Methods: The curriculum included intensive training in knowledge and current trends, business propositions, and professional certifications. Successful completion of the B2HI provided scholars with guaranteed admissions into the Master of Science in Health Informatics (MSHI) degree program, which premiered at MSM in August 2021. We deployed several strategies to attract individuals interested in advancing their careers in HI. To assess the impact of the recruitment strategy and program, we analyzed applicant demographics, the interests of those accepted into the program, and feedback from participants via anonymous online surveys.
Results: In 2021, our recruitment efforts attracted 65 applications, over whom 90% self-identified as African American and the majority were working adults. Among the 46 applicants accepted and enrolled, 38 (83%) completed the program. Thirteen B2HI graduates enrolled in the first offerings (Fall 2021 and Spring 2022) of the online MSHI degree program, the highest number for the first sessions of our online master’s degree programs, indicating that B2HI connects scholars with advanced training. Participants indicated immense overall satisfaction with the program and had strong positive responses for increased interest and confidence to do advanced work in the subject.
Discussion: The data indicate that B2HI addresses key factors that hinder diversity in healthcare and informatics-related fields, including awareness, access, and social support, and connect students with the next stages of training toward careers that require an advanced degree. By providing opportunity, resources, and networks that help participants raise their potential to become leaders and decision-makers in the healthcare industry, programs like B2HI enable the collective effort to decrease health disparities.
1. Introduction
Health informatics combines the principles of computer, information, cognitive and social sciences to advance life sciences research, professional health education, public health, and patient care (Hassan, 2019; Informatics: Research and Practice|AMIA - American Medical Informatics Association, n.d.). It leverages informatics—the science of how to collect and use data, information, and knowledge—to provide patients with quality and equitable care, the primary objectives of healthcare (Gibbons, 2011).
Since the Health Information Technology for Economic Clinical Health Act of 2009, tools such as electronic health records (EHR’s) have gained widespread adoption to enable evidence-based clinical decisions, personalized treatments, feedback, and monitoring impacts of treatments and technologies (Rights (OCR), 2009). These tools can enable better collaboration among healthcare providers, leading to cost savings, patient participation, and a host of benefits that ultimately improve patient outcomes (Gibbons, 2011). These tools also have great potential reveal and address systemic issues in the healthcare system that perpetuate health inequities, yet doing so requires examining the social factors in society and the workforce that shape health.
Social determinants of health include race and ethnicity, socioeconomic status, disability, and rural residence (Veinot et al., 2019). They impact health outcomes significantly, and although huge strides have brought us toward a more equitable playing field, the bias that exists within society touches every facet of life including healthcare. At its core, the healthcare field in the US was built with inequities and bias, with the majority of doctors and researchers being White males. Historically, many doctors were prone to using science to justify racial bias and many of these biases perpetuate, consciously or subconsciously, leading to unevenly distributed access and quality of care (Nelson, 2019; Bailey et al., 2021; Togioka et al., 2022). Research asserts that due to these inequities, underserved communities and certain racial and ethnic groups face lower quality of life and life expectancy because of differences in healthcare available or provided (NORC at University of Chicago, 2013). In general, underserved communities are also more prone to ailments such as cancer, asthma, diabetes, obesity and other chronic diseases, and during the first 10 months of the COVID-19 pandemic, the mortality rate for Black Americans was 2.1 times higher than that of White Americans in the US (Johnson-Agbakwu et al., 2020; Phillips et al., 2020).
The field of HI has the mission and potential to evaluate, properly address, and potentially reverse the disparities perpetuated in healthcare. Infrastructures like evidence-based clinical decision support systems, which pinpoint diagnosis and treatments based on specific patient data, can help expose and redress systemic bias. Given that healthcare disparities are perpetuated by social determinants, redressing healthcare disparities requires a closer examination of the workforce.
The composition of the workforce mirrors the problem—if the makeup of healthcare professionals, trainees, researchers, and anyone serving this industry does not reflect the range of race, gender, social class, socioeconomic status, ethnicity, and other aspects of the population served by this field, we are unlikely to reduce health disparities at a sufficient pace.
Whether this is the case for the HI field is difficult to gauge as the demographics of the field are not well reported, which may be due to the relative newness of the HI field, and being a multidisciplinary field, it overlaps with other fields including medicine, healthcare, information technology, biomedical informatics, and computer science. Health informatics may also be known under different names among different groups of practitioners. One professional database illustrates the breakdown of health informatics professionals, yet reports that there are 134 health informatics specialists across the US, a gross undercount likely stemming from many professionals not labeling their profession with this term (Health Informatics Specialist Demographics and Statistics [2022]: Number of Health Informatics Specialists in the US, 2021).
Based on historical data from related healthcare, biomedical, and informatics professions, we suspect lack of diversity among professionals working in HI, especially in roles that require an advanced degree. A 2022 report on the representation and incomes of Black physicians in the US showed that in 2018, 5.4% of physicians in the US identified as Black while 13.2% of the US population reported as Black alone (US Census Bureau, 2019; Ly, 2022). Though the situation has improved from 1900 when 1.3% of physicians in the US identified as Black, representation among physicians fails to reflect the population it serves. Similarly, a 2020 survey by the National Council of State Boards of Nursing found that 6.7% of nurses identify as African American (American Association of Colleges of Nursing, 2022). Taking a closer look at fields that merge computation with medicine, biology, or healthcare, a survey of biomedical informatics doctoral graduates from 2002 to 2017 showed that 5.7% of graduates identified as Hispanic, 3.2% as Black, and 2.8% self-described as others, including multi-racial and indigenous American. Throughout the years surveyed, the combined representation of graduates identifying as White and Asian dominated, from 85.4% in 2002 to 84.8% in 2017 (Wiley et al., 2020).
Lack of diversity in healthcare need not deliberately incite harm to have discriminatory effects or to negatively impact health outcomes (Southerland et al., 2018; Togioka et al., 2022). False beliefs, misguided risk analysis, and algorithms on biased or incomplete data can lead to unintended disparities for members of different racial groups (Hoffman et al., 2016; Eberly et al., 2019; Vyas et al., 2020). One survey published in 2016 found that false beliefs about biological differences between black bodies and white bodies, e.g., “black people’s skin is thicker than white people’s skin” perpetuate among laypeople and the medical community, and are associated with the undertreatment of pain (Hoffman et al., 2016). A 10-year study of patients self-referred to an emergency department with a diagnosis of heart failure found that Black and LatinX patients with heart failure were less likely to be admitted for cardiology care, leading to racial differences in outcomes (Eberly et al., 2019). A 2020 review of diagnostic algorithms illuminates the race-adjusted algorithms and race-corrected standards developed for many disciplines in medicine, including heart disease, lung disease, fractures and osteoporosis, urinary infections, cancer risks, and vaginal birth risks after C-sections (Vyas et al., 2020). The consequences for practice are that many patients are classified as “low-risk” based on perceived membership in a racial or ethnic group, rendering them lower priority for receiving treatment. Algorithm developers offered little or no explanation about why racial or ethnic differences might exist, while others offered rationales often traceable to outdated, suspect racial science, or to biased data. Experts argue that the medical community should not ignore race, but must distinguish between using these data for statistics, which are vital for epidemiologic analyses, versus for prescriptive clinical guidelines, where it can exacerbate inequities (Vyas et al., 2020).
Reducing disparities rooted in racialized factors therefore requires “race and gender concordance” between patients and the workforce, i.e., those who decide what data to record, analyze data, develop algorithms, make decisions, and apply them in practice (Togioka et al., 2022). Improving representation is prerequisite to achieving the cultural awareness, sensitivity, and humility to design and apply health informatics tools and principles in ways that reduce rather than exacerbate inequities.
Professional development programs and task forces can combat underrepresentation. At this time, however, there is limited evidence of increasing persistence in HI careers among members of underrepresented racial and ethnic groups (Moscato et al., 2014; Bakken, 2020). For example, the federal government funded Scholarships for Disadvantaged Students in health professions and nursing programs, but none of these scholars pursued a career in HI (USF Health, 2018; Scholarships for Disadvantaged Students|Benefits.gov, n.d.). The AMIA First Look Program inspired more optimism, exposing 87 women to HI within 4 years, 41% of whom self-identified with marginalized communities (Bright et al., 2022). Post-program follow-up showed that just three were pursuing graduate degrees in informatics.
Educators point to exposure being the pre-requisite to raising awareness, interest, and intention to persist in an informatics field, one that is heavy in computation and challenging subject matter. Recent programs in bioinformatics and biotechnology show promise. The NIH MARC to Assist Bioinformatics program provided students with 10 weeks of intensive training and an internship. Pre- and post-program surveys showed that the majority of participants raised their self-reported competencies in computational skills from “novice” to “basic” or “advanced” by the end of the program, preparing them to master skills specific to bioinformatics (Mendez et al., 2016). These programs show promise as interventions that impact the skills and preparation of students from racial and ethnic groups underrepresented in these fields. Each has their strengths and limits for the nature of exposure, resources offered, and connection with additional training and career opportunities.
Herein, we detail our new program, Bridge to Health Informatics (B2HI), an intensive 5-week online summer program that is part of a deliberate, targeted, and integrated strategy by Morehouse School of Medicine (MSM) to increase diversity in HI. The program premiered in June of 2021 and aims to increase awareness, interest, and preparation among underrepresented racial and ethnic groups in HI. The curriculum included intensive training in knowledge, business propositions, and professional certifications. Graduates of B2HI were automatically admitted into the Master of Science in Health Informatics (MSHI) degree program, which premiered at MSM in August 2021, thus providing a seamless transition from the summer program to a dedicated advanced training program that would further prepare and connect students with meaningful and financially rewarding career opportunities in HI.
We created the B2HI program in 2021 following the success of another field-specific bridge program, Bridges to Biotechnology and Bioentrepreneurship (B2BB). We suspected that potential students lacked awareness of the opportunities in biotechnology when enrollment in the Master of Science in Biotechnology (MSBT) program during its first academic year, 2019–2020, was surprisingly low, given the value of the program in raising preparation for lucrative career fields and its asynchronous schedule conducive to the schedule of working adults. We thus created B2BB in 2020. After this first session, enrollment in MSBT shot up from seven students in 2019–2020 to 32 students for the 2020–2021 academic year, with approximately 70% having completed B2BB (Howard et al., 2021). We concluded that the field-specific Bridge program helped underrepresented students gain awareness, interest, and access to that field. Applying lessons from B2BB, we offered B2HI before the 14-month MSHI program.
2. Materials and methods
2.1. Program design and rationale
The B2HI summer program was designed to provide intensive training in technical knowledge, communication and research skills, and career readiness (Figure 1) with the convenience of being entirely online. The program commenced on Monday through Friday from 9:00 a.m. to 4:00 p.m. each day for 5 weeks. The curriculum was designed to engage participants in current issues, e.g., brainstorming solutions in teams to address health disparities during the COVID-19 pandemic or digital disparities in rural areas.
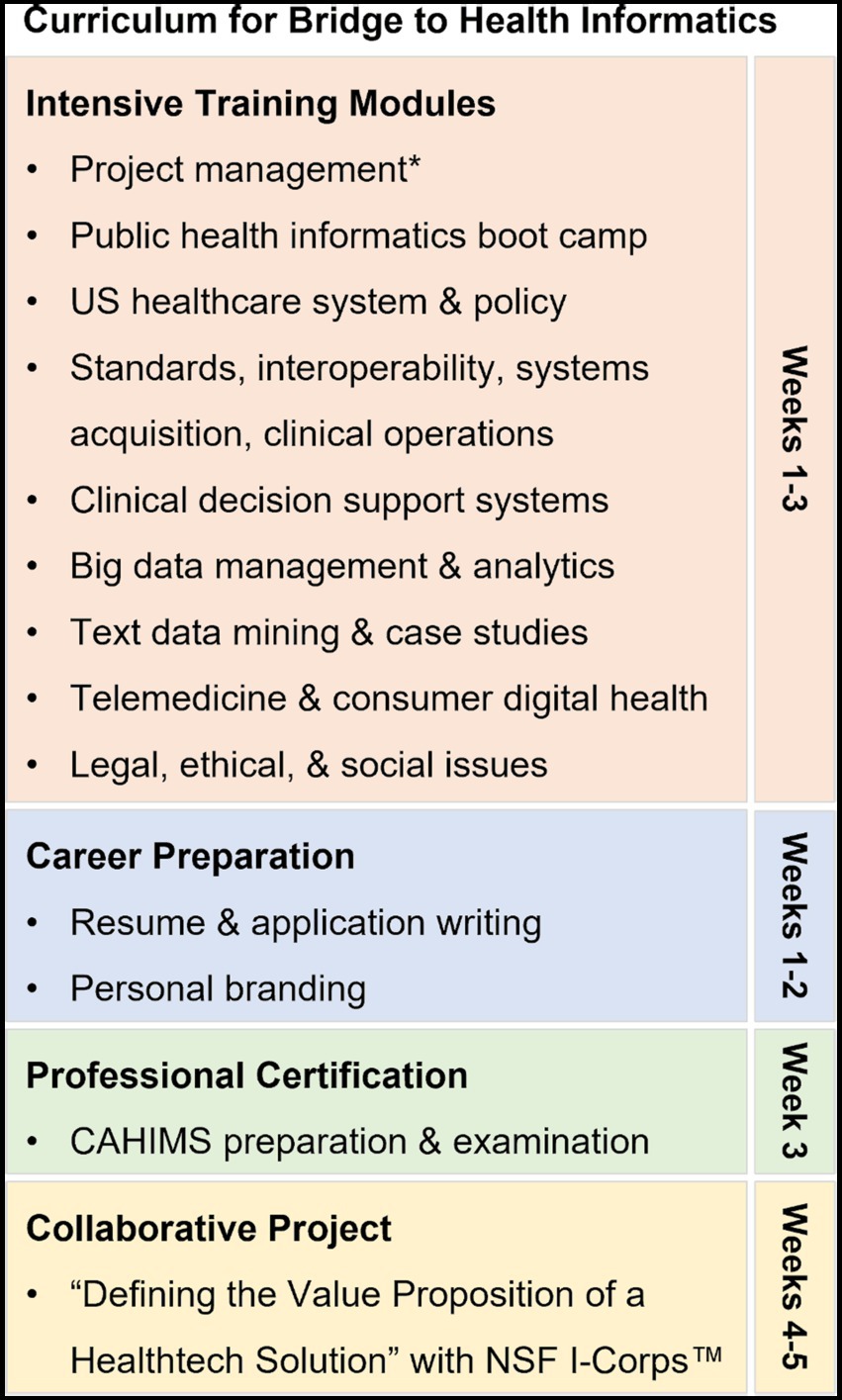
Figure 1. Online curriculum for Bridge to Health Informatics 2021. *Followed frameworks and best practices of the Project Management Institute.
Key to B2HI were partnerships with professional organizations, especially NSF I-Corps™ and Healthcare Information and Management Systems Society (HIMSS). The NSF I-Corps™ program provides experiential entrepreneurship training so that innovations can translate into market impacts (Bosman and Garcia-Bravo, 2021).1 DuringB2HI, participants completed a two-week intensive project in teams to develop a service or product toward commercialization. This immersive experience with mentorship from the I-Corps™ team involved identifying problems, design thinking, intellectual property, customer discovery, research, and interviewing thought leaders. The I-Corps™ team also provided expertise and logistics to execute this endeavor online.
Standing out from other summer programs known to date including those at MSM, B2HI provided the opportunity to obtain the Certified Associate in Healthcare Information and Management Systems (CAHIMS) credential through partnership with HIMSS, a non-profit national and global organization geared toward transforming the healthcare system.2 As an Approved Education Partner (AEP) with HIMSS, MSM was able to offer a CAHIMS review module and allow students to sit for this certification exam during B2HI and cover the exam fee.
Finally, key partnerships with the United Negro College Fund (UNCF) and the Atlanta University Data Science Initiative lowered barriers to participation by providing participants with a $500 stipend upon completing the program and a $1,000 scholarship for the 35-credit hour MSHI program, for which full tuition is $33,250.
2.2. Recruitment
The recruitment plan targeted individuals who were interested in advancing their careers in HI and would likely be interested in the MSM online Master’s of Science (MS) degree programs. We deployed several different strategies to recruit participants with the goal of recruiting at least 50 to 75 participants into the program. In these strategies, we communicated the potential impacts of the program, avenues for career development, and low barriers to participation through a variety of channels across the United States, as described in Figure 2. Our messaging highlighted the guaranteed acceptance into the online MS degree programs and other benefits of successfully completing the pipeline program. Social media was used to market the Summer Bridge Program and online MS Degree programs and outlined how they would collate with each other.
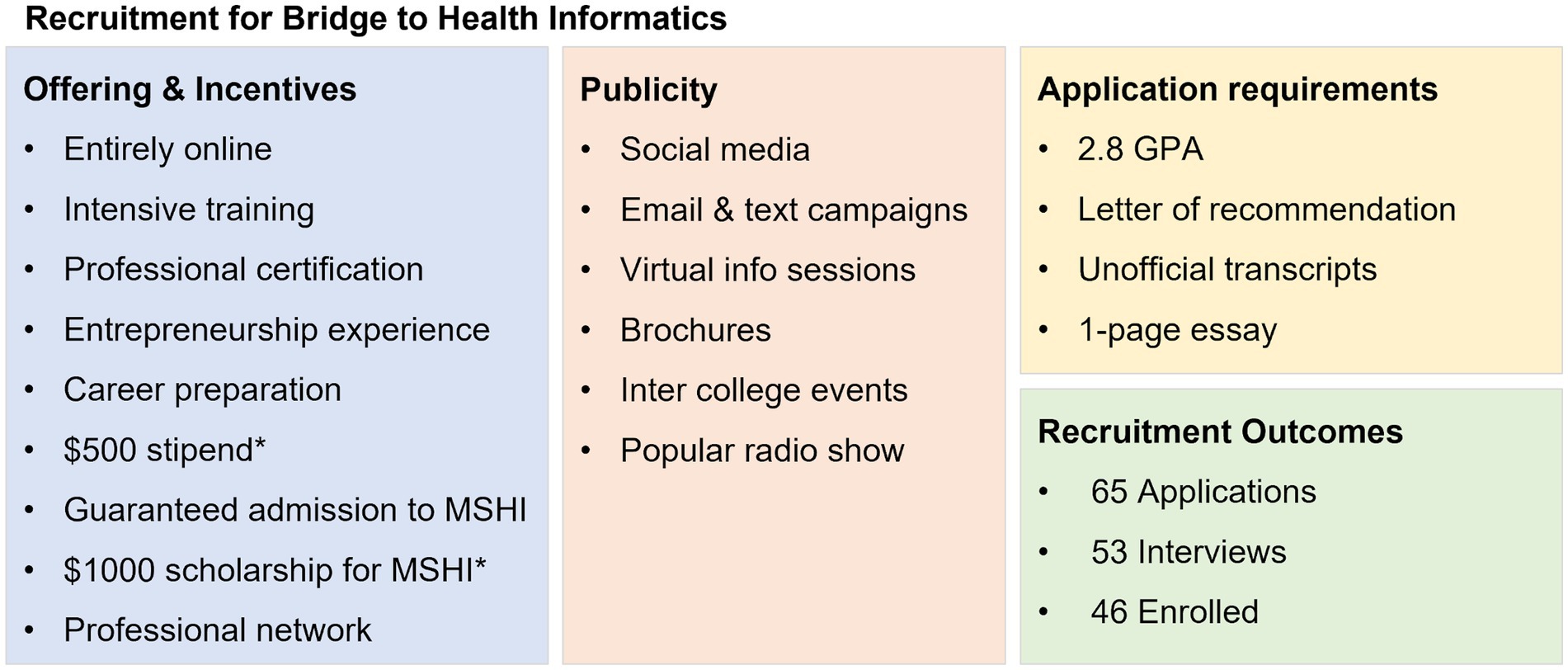
Figure 2. Recruitment strategy and outcome for Bridge to Health Informatics 2021. *Supported by the UNCF and Atlanta University Data Science Initiative.
Digital brochures and program flyers outlining the specifics and benefits of engaging in B2BB and B2HI were developed and distributed. Virtual information sessions were first conducted with schools already partnered with MSM; additional virtual sessions were opened to members of other HBCUs and institutions interested in learning more about HI. We invited students of all majors including natural science, computer science, liberal arts and performing arts to attend the sessions and apply to the pipeline program. Email, text, and other digital marketing campaigns were used to reach prospective participants. One of the main recruitment strategies to promote the MS degree programs was through a popular local radio show with a web presence and > 3 million listeners nationwide. Radio interviews with the program director aired regularly beginning when applications opened in January and ended in early April of 2021.
One incentive to complete B2HI at MSM was guaranteed acceptance into the 14-month online MSHI program. The eligibility criteria for B2HI were the same as those for the MSHI. At the time of application, students were required to have a grade point average of 2.8, one letter of recommendation, unofficial transcripts (official transcripts were required when applying to MSBT or MSHI), and a one-page essay stating why they were interested in B2BB or B2HI. The program was open to undergraduate juniors, seniors, and post-baccalaureates. International applicants applied from Canada, Finland, and Pakistan.
For the summer 2021 cohort, we received 65 applications. We interviewed 53 applicants for B2HI and enrolled 46 participants. The interview panel consisted of one program coordinator, three program managers, the assistant dean of online education, and the admissions recruiter. Interviews lasted 10 min and included a series of questions along the following themes:
1. Share what you are currently doing related to work or school, and how will the Bridge to Health Informatics summer program help you with your long-term goals?
2. What skills do you expect to gain from this program that will prepare you for your future career?
3. Are you planning to apply for the MSHI 14-month program for Fall 2021, Spring 22, or uncertain at this time?
4. Due to the high volume of applicants with limited spots available due to funding, if you are not accepted into the summer program, are you still planning to apply for the Master of Science in Health Informatics.?
5. How did you hear about the summer program?
The interview panelists scored applicants on a 5-point Likert scale based on their responses during the interview and prioritized those who were interested in joining the MSHI program after participating in B2HI. Once the admissions team reviewed the applicants’ scores, acceptance or denial letters were sent out to all interviewees. Accepted scholars then needed to fill out the Summer Pipeline Acceptance Form to secure their spot by the deadline, in which they agreed to complete the weekly assignments, miss no more than two sessions, complete all pre- and post-surveys, be available during the given dates and times of the program, and would receive a certificate of completion only upon fulfilling these requirements.
2.3. Program curriculum
The curriculum of B2HI was intentionally developed to be broad in scope to expose potential students to a variety of content. The goal was to provide conceptual knowledge that could be transferable for further training and potential career pathways and to give students a taste of what the MSHI program offers. This was done to prepare and inform students about the next steps to pursue a chosen career path. Below, we describe the content and rationale. A week-by-week presentation of the curriculum is available in Table S1 of the Supplementary file.
Throughout B2HI, participants took part in training and knowledge sharing sessions and completed numerous individual and group projects. Lectures were delivered by professors from prominent institutions nationwide. Participants experienced training in project management, healthcare systems, interoperability, information systems acquisition, telemedicine, data analytics and more. Project assignments included interviewing healthcare workers, project implementation of a medical device/service that would benefit the healthcare field while increasing efficiency and in turn bettering patient outcomes, working in group settings to brainstorm issues relating to COVID and the disparities it illuminated, etc. We also carved out time during the B2HI program to allow participants to apply to the online MS Degree programs. Although graduates of B2HI were guaranteed admissions into the MSHI, they were still required to apply officially.
Week 1 in 2021, the two Bridge programs, B2HI and B2BB, ran concurrently starting with a half day of orientation. Orientation for the B2HI program included online etiquette, an overview of the B2HI program, a session on applying to the new MSHI program at MSM, and an overview of the culminating team project with NSF I-Corps™, “Defining the Value Proposition of a Healthtech Solution.” During the remainder of the first week, the participants of the two programs completed modules on project management; career readiness and resume writing; and a public health informatics boot camp.
The project management module and HI bootcamp were carried forward from the 2020 session of B2BB at MSM (Howard et al., 2021). They were led by the same facilitators and conducted in a similar format. The project management module occurred over 3 days and immersed participants in project management frameworks and best practices as classified by the Project Management Institute. Participants also learned the soft skills for engaging with stakeholders with different backgrounds and interests. The public health informatics boot camp gave participants hands-on training with informatics tools to work with massive amounts of data available via the worldwide web. Beginning with the language of the internet, participants learned to differentiate between data, meta data, and scripting and text analysis tools and where they are applied in the medical field at large and in specific career paths.
Following the first week, the two programs ran concurrently but separately except for singular sessions shared by the biotechnology and HI sectors including, graduate admissions and applications, personal branding, and legal, ethical, and social issues.
Week 2 began with an introduction to the US Healthcare System, covering how healthcare is delivered in the US, a conceptual framework for the medical model of healthcare delivery, health determinants, and theories of market and social justice. This module included a suite of required readings and videos from leaders in research, thought, policy, and media including John Oliver and Barack Obama (Obama, 2016). Some of this content scrutinized the state of American healthcare, such as the segment produced by the Public Broadcast Service “Is U.S. health care the best or ‘least effective’ system in the modern world?”3 and/or pinpointed historical and current instances of bias in medicine, as in “Bias in Medicine” an episode of Last Week Tonight with John Oliver.4 These media shine spotlights on systemic problems of effectiveness and equity in the US healthcare system. This segment of B2HI set the stage to define health informatics and how the field can mitigate these problems.
The remainder of week 2 consisted of intensive modules on different and current aspects of health informatics: HI Technology Standards and Interoperability, Telemedicine in COVID-19, Information Systems Acquisition, Consumer Digital Health, Clinical Operations, Clinical and Evidence Based Decision Making, and Text Data Mining. The program gave dedicated attention to the topic of telemedicine during the COVID-19 pandemic. Students were introduced to data points that highlighted the increasing presence of telemedicine and how it would have a lasting impact on healthcare delivery. As an exercise, participants worked in small breakout groups to analyze data and to brainstorm resolutions for the digital disparities that occurred in a small town in Georgia which had limited access to technology. Increasing digital access would give residents in this town and towns like it access to telemedicine. Groups devised ideas ranging from creating a space for digital access in common places such as libraries to addressing the job scarcities in rural/sparsely populated areas.
Week 3 encompassed modules on Big Data management and analytics followed by preparing for and taking the CAHIMS exam. Participants came away from the Big Data modules equipped with not technology skills and the analytical skills to ask questions and tell stories using statistics correctly, and how to observe incorrect uses of statistics in the world around them. For hands-on experience, participants learned the basics of data warehouses and coding with Python and used them to manipulate large datasets. These skills are transferable across numerous areas in health technology - including genomics, predicting adverse drug reactions, and health decision making, in addition to pressing societal problems. The third week culminated with preparation and sitting for the CAHIMS examination.
For weeks 4 and 5, the final 2 weeks, participants dove deep into the HI I-Corps program, conducted in collaboration with the NSF I-Corps team. During these 2 weeks, participants took part in expert-led workshops on the path to commercialization, identifying problems, design thinking, intellectual property, customer discovery, research and interviewing. Participants were assigned teams at the beginning of the I-Corps component and met in these teams between workshops to synthesize their learning and apply it to defining a value proposition. During the final week of the program, each team identified at least 15 experts and potential customers through LinkedIn and conducted interviews with them. The program culminated in an event where each team presented their ‘lean startup’ plan to the combined Bridges community of over 100 participants and instructors.
2.4. Data collection and analysis
To understand who the program attracted, we collected data on the demographics of the applicants, including gender, race/ethnicity, and age group were queried in the application itself. These data informed program managers as to who they were attracting to apply to the program and include responses from the entire applicant pool, regardless of whether they were accepted into the program.
Individuals accepted the program were asked to sign an agreement to participate in anonymous pre- and post-program surveys if they were to enroll in the program. Pre-program surveys were then emailed to participants several days before the program start and inquired their areas of interest in health informatics. After each module, participants received a link in Canvas to the post-module survey and daily reminders to complete them. During the final week of B2HI, the post-program survey was emailed to all participants for their feedback after the entire program. This survey contained multiple choice and open-ended response questions.
During the analysis of the post-program survey data, we discovered that 54 responses were received while 38 individuals completed the program. This was due to an oversight in systems management that failed to bar participants from submitting more than one survey form. With the data being collected anonymously, no unique personal identifiers were requested nor assigned digitally, so we were unable to discern who submitted more than one response. Due to the delay between the program end date and this discovery, we deemed that resending the surveys would not yield feedback that represented participants’ impressions when they completed the program. Furthermore, gathering additional data could introduce additional bias to account for in the analysis.
We chose to proceed with making the most meaningful analysis possible by following published rationale to reduce possible duplicated and incomplete responses (Kang, 2013; Arevalo et al., 2022; Griffin et al., 2022), by applying rigorous inclusion and exclusion criteria to the data set. Briefly, missing data were treated as “missing at random,” as the discarded data points did not depend on the specific value expected to be obtained (Kang, 2013). To prevent bias, we applied listwise deletion to remove errant data fields (all answers from one response field were deleted). We removed responses submitted after the program end date and responses submitted before the deadline where participants did not complete the free response questions. Of the remaining responses, potential duplicates were flagged by evaluating similarities in the free response questions, such as those related to participants’ occupations prior to the program, how they heard about the program, and additional comments. After this work, we were left with 31 responses to analyze.
We then summarized the outcomes through descriptive statistics, using Python 3 (Jupyter Notebook 6.4.5), i.e., average values, standard deviations, minimum and maximum values (Van Rossum and Drake, 2009). For this purpose, data from fixed multiple-choice questions were first converted from verbal to numerical scales. For example, the options “strongly agree,” “agree,” “neutral,” “disagree,” and “strongly disagree” were converted to 5, 4, 3, 2, and 1, respectively. For questions with six answer choices, the responses were converted to a 6-point scale.
When we compared the reduced to the original dataset, we observed little change in the proportions of responses for each question. This error in impact measurement therefore did not detract from the value experienced by the participants or their likelihood to persist.
The original and reduced data sets are available in Tables S2-S4 in the Supplementary File. To protect the privacy of individuals and enterprises, we have de-identified any names in the participants’ answers to free response questions. Specifically, names of individuals and the radio show have been de-identified to protect their privacy. Names have been replaced with the role of the individual or radio program.
3. Results
Of the 46 participants who enrolled in B2HI, 38, or 82.6%, completed the program. Participation dropout was due to family issues, mismatched expectations about taking on the synchronous program simultaneously with regular work and life obligations, and not meeting the attendance policy, which stipulated that participants could not complete this session of the program if they missed more than 2 days.
Since B2HI completed, 13 individuals (33.3%) who completed B2HI in 2021 enrolled in the first ever offerings of MSHI beginning in either Fall 2021 or Spring 2022. These enrollments in the first two cohorts of MSHI nearly double the enrollment in the first two cohorts of the MSBT degree, which occurred before MSM created any bridge program. This outcome is consistent with the intention of the Bridge program raising students’ awareness and readiness for graduate training and connecting students who are ready with an advanced degree program.
Our recruitment strategy attracted participants from underrepresented backgrounds interested in Health IT from locations across the United States. Among the 65 applicants, 91% self-identified as African American in race or ethnicity. Among the remaining applicants, 3% identified as Latino, 3% as Asian, 1.5% as Native America, and 1.5% as Caucasian, as seen in Figure 3A.
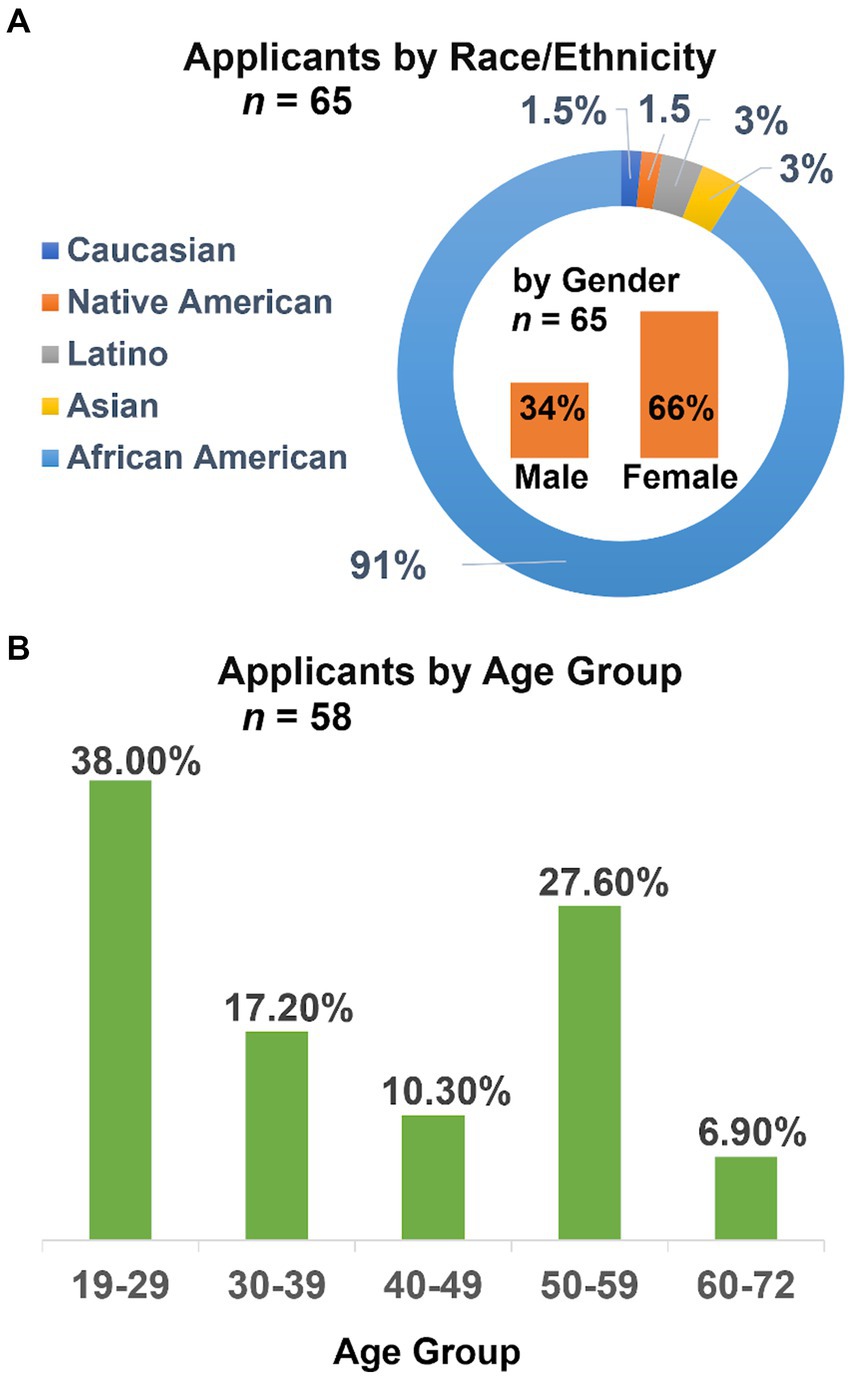
Figure 3. Demographics among the 65 applicants, by race or ethnicity and gender (A) and by age group (B).
The program also attracted adults from diverse phases of their professional and personal development, as applicants represented the full spectrum of age ranges from age 19 to 72. The 19–29 age group, while being the most represented age group, represented only 38% of the 58 respondents to the question, suggesting that most applicants were beyond their undergraduate degree years. The next most represented age group was 50–59 at 27.6% of responses, followed by 30–39 and 40–49. The eldest age group, 60–72, was least represented at 6.9% of respondents, as seen in Figure 3B. The majority were post-baccalaureate working adults.
As shown in Figure 4, we surveyed the interests of accepted applicants so that we might further tailor the program to their interests. Accepted applicants expressed most interest toward public health and clinical among domains, healthcare information systems among techniques, and health systems economic applications.
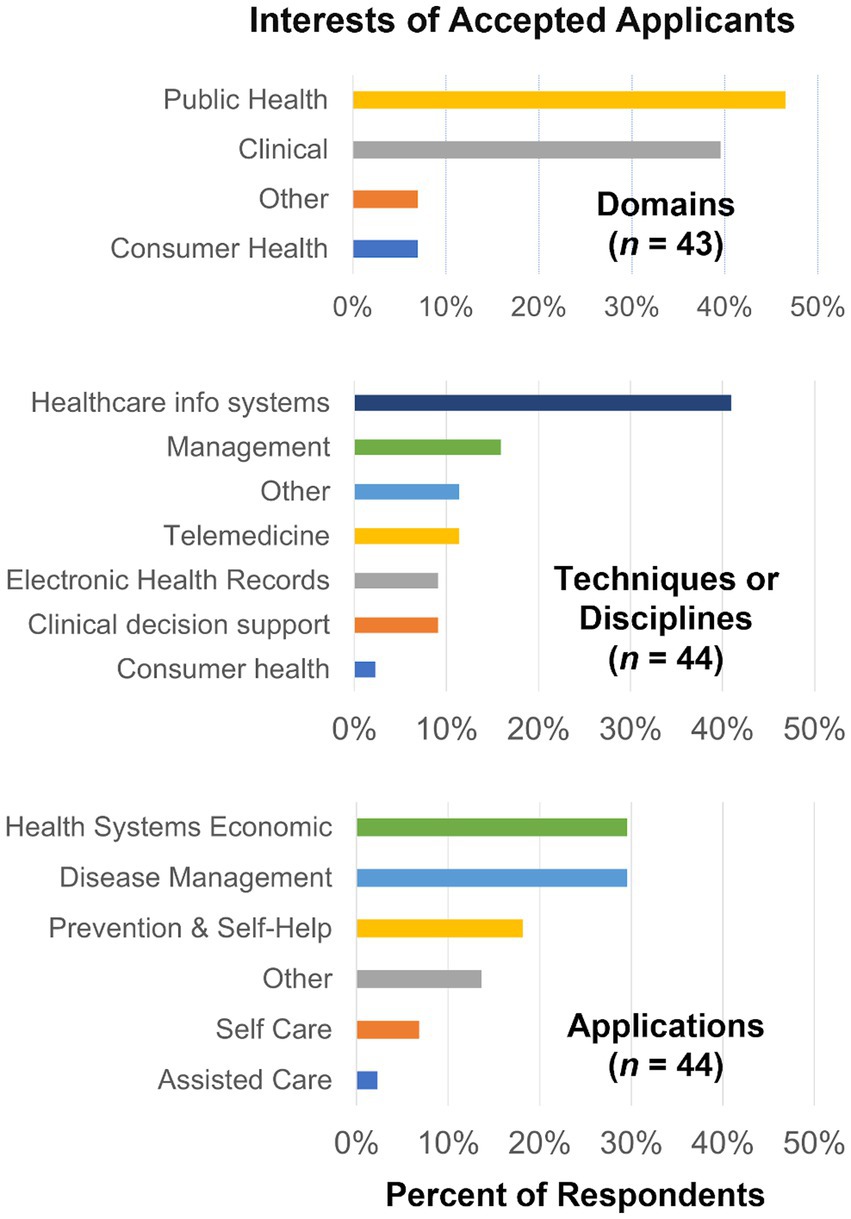
Figure 4. Interests among the 46 applicants accepted to the Bridge to Health Informatics 2021 session.
At the end of the program, participants were required to complete post-program surveys before they could download their certificates of completion. Our survey polled participants’ overall satisfaction with the program, individual aspects, and personal perceptions on the effects of the program. The full survey responses can be found in Tables S2-S4 in the Supplementary File, which includes both the original and final data sets. In Tables 1, 2, we summarize the participants’ post-program survey responses pertaining to their impressions of the program and perceptions of themselves in relationship to a career in HI, including the desire for further advanced training at MSM.
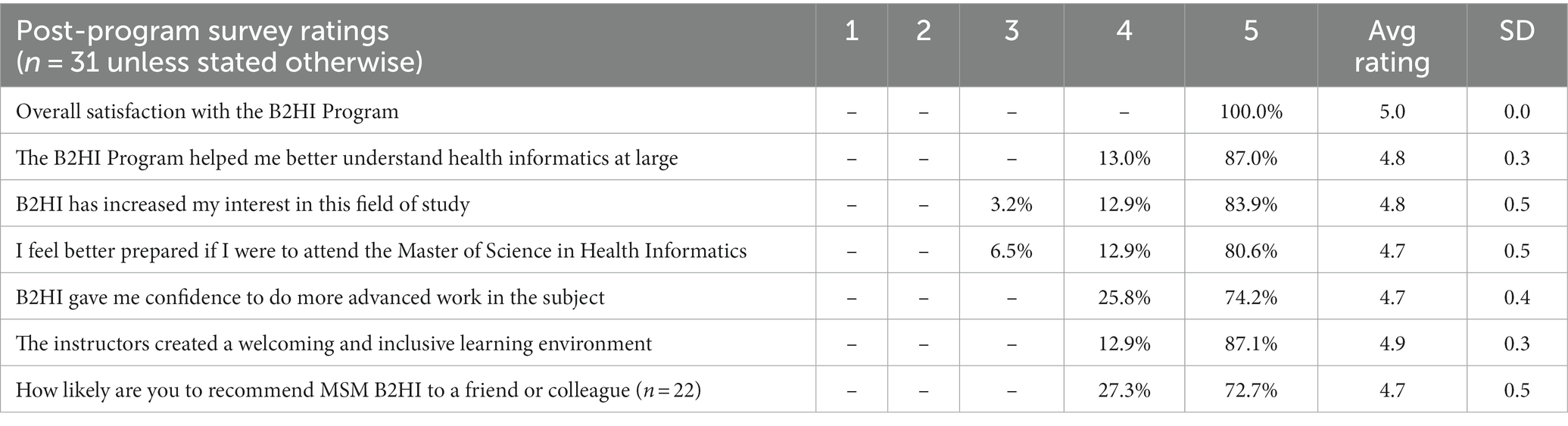
Table 1. Participants’ answers to post-program survey questions about their outlook and satisfaction with B2HI.
Among the 31 responses, 100% answered “Very Satisfied” (or 5 out of 5) for their overall satisfaction with the B2HI program. Such an outcome may seem extreme, however when looking at the ‘uncleaned’ pool of 54 responses, 51 (94.4%) of them were ‘Very satisfied’. The three entries with responses of “Neutral” or “Somewhat satisfied” for this question met the exclusion criteria along with 20 responses of “Very satisfied” and were therefore excluded from the pool of 31 responses further analyzed.
Over 70% of respondents gave the most positive answer, equivalent to 5 on a scale of 1–5 with 5 being most positive, for the remaining six (6) statements listed in Table 1, pertaining to increased understanding, preparation, interest, confidence, perceptions of the instructors, and their likelihood to recommend the program to others. The lowest rating given for any of these statements was equivalent to 3 on the 1–5 scale.
The responses were overwhelmingly positive for the instructors creating a welcoming and inclusive environment, with 87% of respondents strongly agreeing (or 5 out of 5) with this statement. Answers to other questions querying participants’ experience with the instructors about presenter selection and ability to have their questions answered (Supplementary File S1) were also overwhelmingly positive. In the answers to free response questions, many participants praised the instructors and program administrators by name, and some used labels such as mentors, guides, and examples (role model). When asked about their favorite modules project management was the most common answer, with some respondents commenting specifically on the professor’s delivery.
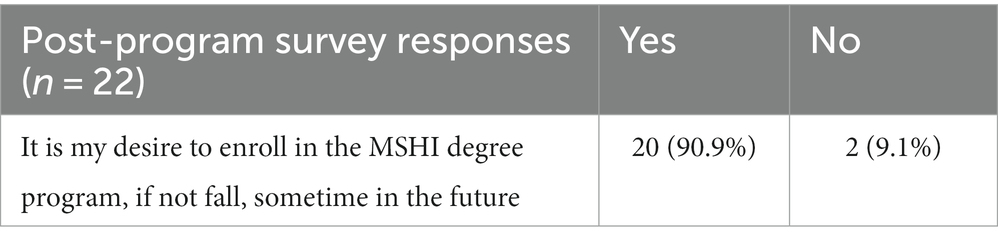
As seen in Table 2, 20 out of 22 respondents answered “yes” to the statement, “It is my desire to enroll in the MSBT program at some time in the future.”
Participants also rated aspects of the program related to its structure and execution on a 6-point scale with “very poor,” “poor,” “fair,” “good,” “very good,” and “excellent” as the options. The vast majority of the ratings were “excellent.” Areas that were assessed included the application process, accessibility to documents, content relevance, and accessing program facilitators/professors. We also asked participants’ perceptions of the course load, navigating through the course management system (Canvas), and getting questions answered in a timely way. We received one (1) rating of “poor” in just two areas, content relevance and Canvas, and no ratings of “very poor.”
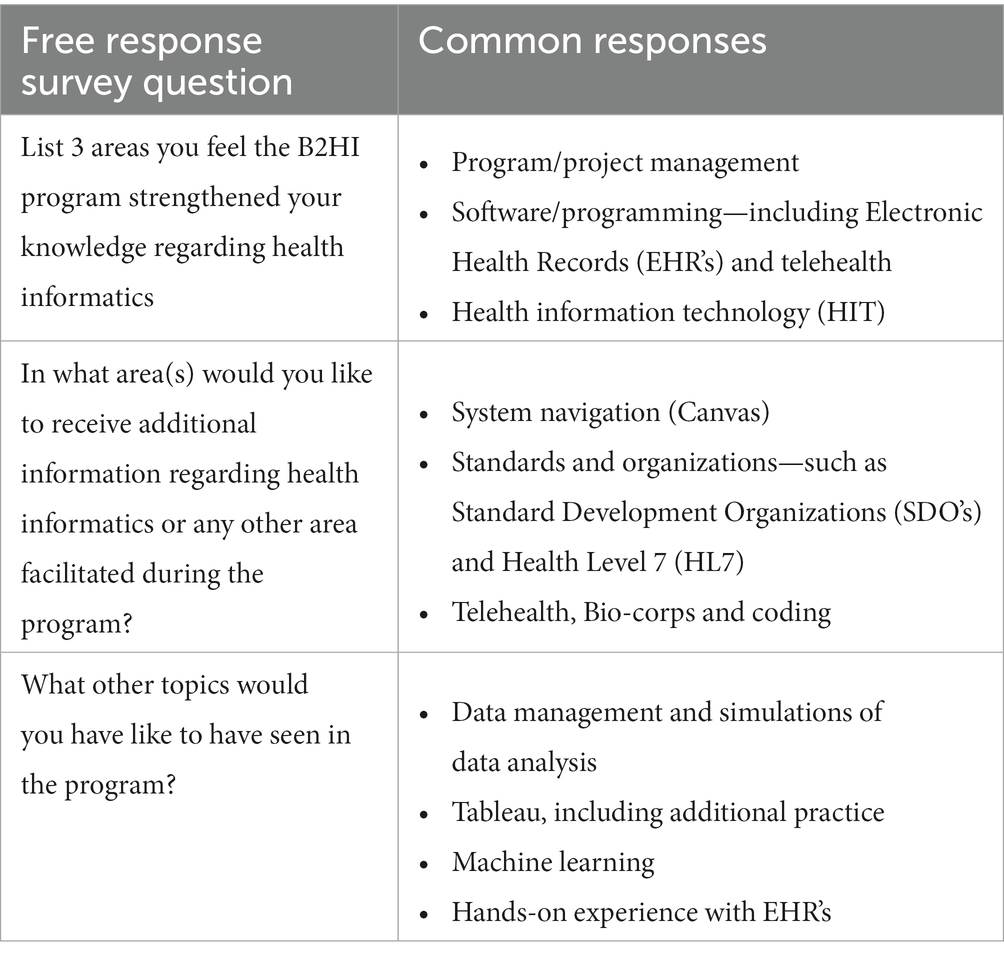
We also asked participants open-ended questions about the program and their outlooks. Table 3 provides common responses regarding areas that participants felt strengthened their knowledge, areas in which they would like additional information, and additional topics that could be added to the program.
Most constructive feedback related to the program’s schedule, which was 9:00 a.m. to 4:00 p.m. with a 1-h lunch break, Monday through Friday for 5 weeks. While some participants indicated feeling satisfied with the program’s schedule as is, the majority of participants took the time to write whether they preferred lectures only in the morning, afternoon, or evening, and how often. Suggestions included lectures in the mornings only followed by group work in the afternoons, more frequent or longer breaks, and having lectures several times a week instead of every day. Suggestions also included starting the morning session later, as 9 a.m. Eastern time is 6 a.m. Pacific Coast time, and the later session may increase geographic diversity among participants of the program, which is intended to serve participants anywhere in the United States. Overall, the abundance of positive and constructive feedback speaks to participants’ engagement with the mission of the program and content overall.
4. Discussion
4.1. Key findings and context
Key figures from enrollment and survey data indicate that B2HI met the intended outcomes of exposing students, to a broad overview of health informatics, thereby raising their awareness and interest to the field and its career pathways, and to connect those desiring further graduate with such an opportunity. Without B2HI, students might have remained unaware of the field and/or pathways to the rewarding and lucrative careers it offers.
Of the 46 participants individuals who enrolled in the program, 38 (82.6%) completed the program. Most respondents, 20 out of 22 (90.9%) expressed desire to enroll in the MSHI program, indicating high interest in pursuing graduate education after completing B2HI. Of these 20 students, a total of 13 (65%) enrolled in the MSHI program beginning in either the Fall 2021 or Spring 2022.
This premier session of B2HI attracted more applicants than spaces available from a huge diversity of backgrounds and geographic locations around the United States. Our pre-program and post-program data indicate that B2HI is addressing pain points that hinder diversity in health informatics and related fields. First, the program attracted members of underrepresented minority racial and ethnic groups. Among the 65 applicants, 91% self-identified as African American in race or ethnicity. The program also attracted adults from diverse phases of their professional and personal development, as applicants represented the full spectrum of age ranges from age 19 to 72, and diverse geographies across the US. For the applicants accepted into the B2HI program, healthcare and health systems were dominating themes for areas of interest according to the pre-program survey. Taken together, this recruitment strategy and curriculum successfully attracted adults from diverse background, career phases, and geographies who showed interest in furthering their careers in health informatics.
To give context, this enrollment outranks that of the first year of the sister program in biotechnology, the Master of Science in Biotechnology (MSBT) degree program, which enrolled only 7 individuals during its entire first year in 2019–2020, before any bridge program existed at MSM. We then created Bridges to Biotechnology and Bioentrepreneurship (B2BB) with the mission of exposing URMs and raising awareness of the opportunities. B2BB attracted more applicants than spaces available when it premiered in 2020, and participants reported increased awareness, interest, and confidence toward persisting in the field as well as perceptions of being part of the biotechnology community and able to contribute to addressing current problems in society. After the B2BB sessions in 2020 and 2021, participation in subsequent cohorts of the Master of Science in Biotechnology degree program at MSM multiplied, and graduates of MSBT have indicated strongly positive perceptions about their career path (Howard et al., 2023, Accepted manuscripts)5.
The B2HI program premiered in 2021 and is a success case in the generalizability of the bridge programs at MSM and the power of exposure and preparation as major influences in participation and persistence in the field. The B2HI program, which premiered in 2021, was specialized with content, partnerships, sponsorships, and opportunities unique to the HI field. Since B2HI premiered, bridge and master degree programs at MSM have expanded to include a concentration in medical cannabis and justice involved care. Each bridge program utilizes the 5-week intensive online structure, yet is customized with content and supported by facilitators and partner organizations specific to the program’s subject matter and career field. Our structure and strategy for the online Bridge programs at MSM are readily translatable to other institutions eager to expose minority scholars to training and opportunities in particular industries across diverse geographies.
These programs also demonstrate how an institution can extend service to underrepresented and underserved communities over diverse geographies. MSM is a historically Black medical school with a track record of serving members of underrepresented and underserved groups, especially African Americans. Recognizing the rigor of healthcare and health technology career opportunities, MSM’s master’s degree programs bridge professional training expectant of employers that require an advanced degree though not a traditional medical or nursing degree. Yet, prospective trainees are unlikely to invest in these degree programs without a concrete grasp of their value to their careers. B2HI fulfills that gap in a specialized way for health informatics through intensive training and first-hand exposure to real-life health disparity problems and health technology solutions.
Increasing diversity in the field, especially at advanced and leadership levels, hinges on the participation and persistence of members from backgrounds currently underrepresented in the field. All respondents represented in Table 1 indicated strong agreement with B2HI increasing their understanding and interest in health informatics, speaking to the program’s first mission of exposing students to opportunities they otherwise might not consider or even be aware enough to consider. The program also increased participants’ perceptions of confidence and preparation for more advanced work, as all respondents answered in agreement with the statement that B2HI gave them confidence to do more advanced work in the subject and over 90% answered in agreement with feeling better prepared if they were to attend the MSHI degree program. All respondents also agreed that the instructors created a warm and inclusive environment.
Research on racial diversity in health and STEM fields, including recent research of summer bridge programs targeted toward underrepresented racial groups in STEM, show that perceptions of self-efficacy and belonging are powerful predictors of persistence in STEM (Walton and Cohen, 2011; Barth et al., 2021; Fisk et al., 2021; McGee et al., 2021). Self-efficacy, the judgment of one’s own probability of success in an academic field or vocation, is critical in motivating individuals to continue on a path of learning or development in the face of challenge, as there is little incentive for people to take action without believing it will lead to success (MacPhee et al., 2013; Ware et al., 2019; Barth et al., 2021). While ability may be necessary to succeed, individuals of the similar ability who perceive that their ability is less than that of others are more likely to leave the field. This dynamic takes effect at early stages of school and pervades unless interventions change the dynamic (MacPhee et al., 2013; Hencke et al., 2022). Belonging describes the sense of fit, identity, and support in a chosen field and at an organization or place of work (Walton and Cohen, 2011). This construct has shaped the experience of individuals from underrepresented racial and ethnic groups in medical, health, and STEM fields in the US because historically, training programs were designed and populated by members of a privileged demographic and attracted members of similar demographics. Members of URM groups in these fields therefore experience socialization in these fields differently than members of dominant groups. Mentorship, professional community, and environmental support are even more critical to fostering feelings of inclusion and persistence among underrepresented minorities.
Participant feedback indicates that during B2HI, participants developed perceptions of self-efficacy and belonging, promising indicators that they will persist in this challenging yet exciting career field. The vast majority of participants self-report having confidence to pursue more advanced work in health informatics and feeling prepared if they were to enroll in the MSHI degree program at MSM, whether they do or not. Their free responses also convey sentiments of relating to their peers, the module instructors, the program director, and other key program personnel with whom they directly interacted. B2HI also builds community through the I-Corp segment of the program and by welcoming participants into professional communities. The I-Corp segment required participants to collaborate with their peers and to interact directly with health informatics professionals. In analyses of bridge programs for STEM undergraduates, direct interactions with individuals that students trust and can relate to affect their desire to persist (Benjamin et al., 2021). In addition, group work can both narrow performance gaps, build critical thinking skills, and strengthen feelings of being able to collaborate and contribute to a community (Miller-Cotto and Schunn, 2020).
Graduates of B2HI join the academic and professional communities of MSM and HIMSS, providing intersectional support socially and professionally. The partnership with HIMSS allows MSM to participate as an organizational affiliate, allowing exchange in course content and access to resources toward further certifications and career development. By becoming members of both professional communities, participants expand their networks and pathways toward opportunities in health informatics that are well-paid, interesting, and satisfying.
In summary, the collective data of B2HI completion rate, subsequent enrollment in MSHI, and participants’ perceptions show that B2HI does address barriers that hinder participation and persistence among underrepresented groups in the HI field and increases participation in graduate training at MSM, the essential first step to increasing representation at advanced levels. The B2HI program contributes by uniquely attracting individuals ready for advanced training and career development in multiple facets within health informatics. The combination of intensive skills training, career preparation, group problem solving, and business training entirely online supported by a community of relatable mentors and role models is unprecedented.
4.2. Limitations and lessons learned
For this first session, we encountered setbacks in impact measurement, namely receiving more post-program survey submissions than program participants. As described in the methods, we established a robust data cleaning strategy that was unlikely to introduce bias into our interpretations (Kang, 2013; Arevalo et al., 2022).
Even so, some questions remained unanswered. Notably, students who did not respond to the survey question (“It is my desire to enroll in the MSHI degree program at MSM,…) also did not respond to the survey question (“How likely are you to recommend MSM B2HI program to a friend or colleague?”). Interestingly, if a student did respond to the survey question (“It is my desire to enroll in the MSHI degree program at MSM,…) they also responded to the survey question (“How likely are you to recommend MSM B2HI program to a friend or colleague?”). The lack of responses to these two survey questions (~30% did not respond) may be attributed to a lack of a desired response option, which could indicate that the students would have an increased response rate if an additional option were available.
To elaborate, for the survey question, “How likely are you to enroll in the MSHI degree program at MSM,…” the only options were “Yes” and “No.” For future surveys, additional options such as “Maybe” and “Possibly” might be needed to address students who have yet to decide. It may also be relevant to pose a follow-up question regarding their selection of “Yes,” “No,” or “Maybe,” to determine the driving force behind the decision, which could include financial considerations, time, workload, interest in the field, uncertainty about career prospects. For the survey question, “How likely are you to recommend MSM B2HI program to a friend or colleague?,” we acknowledge that having only “yes” or “no” options poses a risk of biasing the responses. Future surveys will use a numerical scale for this question.
For the survey question, “How likely are you to recommend the MSM B2HI program to a friend or colleague?”, the response selection ranged from “Very Likely,” “Likely,” “Neutral,” “Unlikely,” and “Very Unlikely.” Because the response rates of these two questions are correlated, it can be hypothesized that the response options may not have encompassed the student’s desired response option. For example, a student may not know of anyone who is interested in the field, and therefore would have no one to recommend the program to. A pre-question might be needed to identify if the student(s) knew of another individual who might be interested in the B2HI MSM program.
To ensure that our interpretation of these responses was not skewed by the data cleaning process, we compared the response rates to these questions among the original data set, the cleaned data set, and the data removed. In the original data, 11 out of 54 responses, approximately 20%, for these two questions were left unanswered. If one was left unanswered, both were left unanswered. The cleaned data represented 31 respondents, and 9 out of these 31 responses, approximately 29%, did not respond to either question. Of the 23 responses removed from the original data, 2 of the 23, approximately 8%, did not have a response to either of these questions.
From this analysis, we conclude that the selection criteria did not bias our interpretation in favor of respondents intending to enroll in the MSHI program or recommend the program to others. Note that the established selection criteria for cleaning the data were not based on the responses to either of these questions. Considering this condition and the above analysis, we conclude that, when participants did not respond to these questions, their lack of responses to these questions did not impact their responses to other multiple-choice questions or to free response questions.
Sharing these lessons learned is an opportunity to contribute transparency, ethics, and accountability to education research involving web-based surveys. Overall, the complications in our dataset presented valuable learning opportunities and did not detract from the positive impacts of the program for the participants and the health informatics field. Nonetheless they sounded a call to action to revise the data collection strategy to safeguard both the integrity of the data and participants’ privacy. Doing so essential to ensuring that the data reflects participants’ honest feedback about the program, their needs, and their interests.
Like other nascent programs, B2HI was not immune to the consequences of serving a large community with a new initiative on limited resources (Mendez et al., 2016; Bright et al., 2022). Web-based surveys confer huge advantages such as flexibility with geography and time, relatively low coordination costs, reduced collection time compare with other survey methods, and lack of social bias induced by the presence of an interviewer, nonetheless are vulnerable to many limitations when it comes to ensuring that the answers reflect genuine engagement of the participants with the questions (Sharma et al., 2021; Arevalo et al., 2022; Pew Research Center, n.d.). Recent reviews show that many studies do not describe their surveys fully and even fewer disclose their process for cleaning the data, if any (Eysenbach, 2004; Sharma et al., 2021). Transparency in reporting setbacks with data and sharing best practices as they evolve are paramount to protection the credibility of the impacts communicated from these programs and ultimately the integrity of education research using web-based tools.
Beginning in 2022, we have transitioned our surveys to a new platform and built in key elements to prevent repeating issues of the past and to safeguard privacy. Each participant now receives a personalized link that only they can access and allows for one submission. The platform keeps responses anonymous while informing the directors who has not completed the survey. The survey remains mandatory, and participants are instructed to upload a screenshot confirming that they completed the survey before they can access their certificates of completion. To avoid some of the challenges with interpreting incomplete surveys, all questions are now mandatory. Consistent with recommendations in the literature, we are testing systems thoroughly prior to administering the surveys with the participants. These guidelines frame best practices that protect the integrity of the data and privacy of the participants such that this work can proceed within compliance for studies exempt from Institutional Review Board oversight, which is favorable for expediency and affordability of performing these studies.
4.3. Future directions and broader impacts
Going forward, this research extends naturally in several directions. At the time of this research, the first session of B2HI had completed and the MSHI program had commenced, with a majority of MSHI students having completed B2HI—B2HI is NOT a prerequisite for MSHI. Our continued research investigates the extent to which B2HI helped MSHI students navigate the MSHI program. Over additional years of both B2HI and MSHI, we anticipate having sufficient data from which to infer statistically significant correlations between different aspects of the program and participants’ self-reported perceptions and intentions. Follow-up analysis with the second session of B2HI, completed in 2022, is ongoing as well as follow-up work with those participants who completed the B2HI in 2021 and enrolled in the MSHI program.
Additional follow-up will seek to understand the extent to which B2HI increases participation in the field and the underlying reasons. The program team stays connected with alumni of the program through follow-up surveys, LinkedIn connections, alumni groups, and regular emails with invitations to participate and engage with new opportunities and new students. Often the impacts of an intervention do not manifest immediately. Directors of one undergraduate enrichment program that included a summer bridge found it meaningful to look at graduation rates within 6 years of matriculating into the program in addition to the retention rate immediately following the bridge (Ghazzawi et al., 2021). They observed higher six-year graduation rates among participants of the program compared with non-participant peers at the same university, providing a more complete picture of the impacts of their program. Similarly, the full impacts of B2HI on participants may not be observable immediately.
The most complete multi-year follow-up available to us will be to observe the rates of matriculation and graduation of MSHI and the career trajectories of these graduates. The B2HI summer program prepares participants for graduate training in HI, whether it is through the MSHI program at MSM or elsewhere. We anticipate that increased awareness of HI and the rewarding career opportunities among B2HI graduates raises their likelihood of taking up advanced training and find the online MSHI opportunity an attractive option.
It would be meaningful to better understand the extent to which the cost of advanced education acts as a barrier to workforce diversity. While the tuition of USD $33,250 for the MSHI program at MSM is not small, it is less than the average tuition of USD $54,000 for a master of science degree program at a private institution (Best Online Master’s in Health Informatics Programs of 2023|BestColleges, n.d.) and the entirely online MSHI program incurs no expenses for location or travel.
The investment does open doors to many career paths that require an advanced degree and pay well. According to the database Payscale.com, graduates of master degree programs in health informatics in the US earned an average base salary of USD$72,000 per year (Master of Science, Health Informatics Salary|PayScale, n.d.). Salaries for health informatics specialist, which is just one of myriad roles in the field, range from approximately $59,000 to $97,000 per year. The Bureau of Labor Statistics predicts that overall employment in healthcare occupations will grow 13% from 2021 to 2031 (Healthcare Occupations: Occupational Outlook Handbook: U.S. Bureau of Labor Statistics, n.d.). Within these professions, employment health information technologists and medical registrars is predicted to grow 17% in this time frame, much faster than average for all occupations (Health Information Technologists and Medical Registrars: Occupational Outlook Handbook: U.S. Bureau of Labor Statistics, n.d.). According to a report by RBC Capital Markets and projections by International Data Corporation, 30% of the world’s data is generated by the healthcare industry and this share is projected to grow faster than manufacturing, financial services, and media & entertainment by 2025 (Reinsel et al., 2018; RBC Capital Markets|Navigating the Changing Face of Healthcare Episode, n.d.). These figures signal that advanced training in health informatics equips graduates with knowledge and connections that will help them stay current as the industry evolves.
One area worth further examining and highly relevant to career advancement is to foster professionalism in group work during the I-Corp segment of the program. Our observations as program leaders hinted at challenges of requiring individuals from diverse professional backgrounds to work together for equal credit. Our program attracted individuals from all age groups from 19 to 72 (Figure 3B), and with group members randomly assigned this time, individuals from vastly different stages of learning and professional development were grouped together. In our observations and in private conversations, individuals represented a range of maturity and senses of responsibility, and challenges arose around distribution of work and effective communication within the group and with limited accountability in the all-online format. With participants of two concurrent bridge programs, as B2HI ran concurrently with B2BB in 2021, split into more than 20 rooms, the program team was not able to monitor all teams.
The modern workplace naturally brings together professionals with diverse thinking styles, ages, stages of their professional path, and ways of working, especially with the rise of remote work. In these aspects, the I-Corps teams did not depart from reality, and like the modern workplace, group members should expect a degree of professionalism and personal accountability. Tragically, individuals who underinvest during this phase will likely leave the program least prepared for advanced studies and lack the personal accountability necessary for real-world collaborative problem solving. Therefore, we see opportunities to improve our program in this direction. One solution is to require groups to create a group contract that members adhere to maintain eligibility for completing the program. The contract would follow a rubric for engagement, which includes participation, collegiality, and punctuality, and require approval by the programming team. Oversight would be needed and if necessary, the director would exercise discretion in determining when an individual has breached the agreement and count it as a missed day of participation; participants can miss 2 days before losing eligibility to complete the program. Our admissions team will also look for indicators of applicants’ experience and attitudes toward teamwork in their applications and reference letters, as prevention is usually easier than mitigation. The impacts of these improvements can also be assessed by gathering participants’ feedback on the group work experience.
Ultimately, the broader impacts of B2HI and subsequent advanced training will be most felt when health disparities decrease, as health informatics reaches into all aspects of healthcare—from the clinic to research to nursing and business, and health technology provides the tools that measure, monitor, and mitigate health disparities. This would mean that more patients from underserved and marginalized groups receive equitable care as their counterparts from advantaged and majority groups. In the future, it may be possible for MSM to collect data that allows us to deduce the role of B2HI in the pathway toward work that influences health disparities positively. The subject matter in B2HI derives directly from real-life health equity problems with data provided by public databases such as the Georgia Department of Public Health, Johns Hopkins Data Science, and the US Centers for Disease Control, as well as statistics for treatments of cancer, diabetes, and other diseases that disproportionately afflict underserved communities. Following up with the job placements, internships, and subject matter of work that participants go into after leaving MSM will shed light on the extent to which B2HI shapes the health equity landscape.
In conclusion, this one-of-a-kind program provides the opportunity and the resources needed to help minority students increase their proficiency and confidence in informatics and business acumen, and as a result, the scope of their careers and financial opportunities. Programs like B2HI provide bridges necessary to increasing diversity and inclusion that is overdue in the US healthcare system and ultimately turning around health disparities.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
Ethical approval was not required for the studies involving humans because of local legislation and institutional requirements. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
AH conceptualized the project, designed the surveys, acquired the data, analyzed and interpreted the data, and supervised the preparation of the manuscript. LS interpreted the results, prepared the visuals, and supervised, prepared, and revised the manuscript. CS analyzed the data, wrote the code, prepared the visuals, interpreted the results, and wrote significant portions of the manuscript. RM analyzed the data, wrote the code, interpreted the results, and drafted portions of the manuscript. NK acquired the data, interpreted the data, and contributed to writing the manuscript. KB assisted with revisions of the manuscript and preparing the submission package. All authors reviewed and edited the manuscript.
Funding
Funding for Bridge to Health Informatics was provided by the Baxter International #670169, the United Negro College Fund #670182, and the Atlanta University Center Data Science Initiative #670180.
Acknowledgments
The authors express sincere thanks to Lanisha Howze for assistance with data collection. The authors also thank Joan Adebowale for helpful discussions.
Conflict of interest
LS was the sole director and employee of Clear Water Science Consulting Limited.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/feduc.2023.1194746/full#supplementary-material
Footnotes
1. ^https://beta.nsf.gov/funding/initiatives/i-corps
3. ^https://www.pbs.org/newshour/show/is-u-s-health-care-the-best-or-least-effective-system-in-the-modern-world
4. ^https://www.youtube.com/watch?v=TATSAHJKRd8
5. ^Howard, A. P., Slaughter, L. S., Adebowale, J., Bentley, K., and McPherson, R. (2023). Diversity in the biotechnology sector: a first look at the impact of a 5-week intensive program on graduate training and career outlook. [Accepted manuscript].
References
American Association of Colleges of Nursing (2022). Fact sheet: enhancing diversity in the nursing workforce. American Association of Colleges of nursing. Available at: https://www.aacnnursing.org/Portals/42/News/Factsheets/Enhancing-Diversity-Factsheet.pdf.
Arevalo, M., Brownstein, N. C., Whiting, J., Meade, C. D., Gwede, C. K., Vadaparampil, S. T., et al. (2022). Strategies and lessons learned during cleaning of data from research panel participants: cross-sectional web-based health behavior survey study. JMIR Format. Res. 6:e35797. doi: 10.2196/35797
Bailey, Z., Feldman, J., and Bassett, M. (2021). How structural racism works- racist policies as a root cause of U.S racial health inequities. N. Engl. J. Med. 384, 768–773. doi: 10.1056/NEJMms2025396
Bakken, S. (2020). Toward diversity, equity, and inclusion in informatics, healthcare and society. JAMIA 27, 1639–1640. doi: 10.1093/jamia/ocaa265
Barth, J. M., Dunlap, S. T., Bolland, A. C., McCallum, D. M., and Acoff, V. L. (2021). Variability in STEM summer bridge programs: associations with belonging and STEM self-efficacy. Front. Educ. 6:667589. doi: 10.3389/feduc.2021.667589
Benjamin, M. E., Yates, D., and Dupuis, S. (2021). LSAMP-NICE: expanding international STEM research for underrepresented minorities. Front. Educ. 6:668232. doi: 10.3389/feduc.2021.668232
Best Online Master’s in Health Informatics Programs of 2023|BestColleges (n.d.). Available at: https://www.bestcolleges.com/healthcare/masters/health-informatics/ (Accessed June 16, 2023).
Bosman, L., and Garcia-Bravo, J. (2021). Lessons learned: research benefits and beyond associated with participating in the NSF I-corps™ customer discovery program. Technol. Innov. 22, 41–54. doi: 10.21300/21.4.2021.5
Bright, T. J., Williams, K. S., Rajamani, S., Tiase, V. L., Senathirajah, Y., Hebert, C., et al. (2022). Making the case for workforce diversity in biomedical informatics to help achieve equity-centered care: a look at the AMIA first look program. J. Am. Med. Inform. Assoc. 29, 171–175. doi: 10.1093/jamia/ocab246
Eberly, L. A., Richterman, A., Beckett, A. G., Wispelwey, B., Marsh, R. H., Cleveland Manchanda, E. C., et al. (2019). Identification of racial inequities in access to specialized inpatient heart failure Care at an Academic Medical Center. Circ Heart Fail 12:e006214. doi: 10.1161/CIRCHEARTFAILURE.119.006214
Eysenbach, G. (2004). Improving the quality of web surveys: the checklist for reporting results of internet E-surveys (CHERRIES). J. Med. Internet Res. 6:e34. doi: 10.2196/jmir.6.3.e34
Fisk, S. R., Wingate, T., Battestilli, L., and Stolee, K. T. (2021). Increasing Women’s persistence in computer science by decreasing gendered self-assessments of computing ability. in Proceedings of the 26th ACM Conference on Innovation and Technology in Computer Science Education V. 1 ITiCSE ‘21. New York, NY: Association for Computing Machinery, 464–470.
Ghazzawi, D., Pattison, D., and Horn, C. (2021). Persistence of underrepresented minorities in STEM fields: are summer bridge programs sufficient? Front. Educ. 6:630529. doi: 10.3389/feduc.2021.630529
Gibbons, M. C. (2011). Use of health information technology among racial and ethnic underserved communities. Perspect. Health Inf. Manag. 8:1f.
Griffin, M., Martino, R. J., LoSchiavo, C., Comer-Carruthers, C., Krause, K. D., Stults, C. B., et al. (2022). Ensuring survey research data integrity in the era of internet bots. Qual. Quant. 56, 2841–2852. doi: 10.1007/s11135-021-01252-1
Hassan, G. (2019). Health care informatics. Int. J. Internet Educ. 18, 39–43. doi: 10.21608/ijie.2019.98636
Health Informatics Specialist Demographics and Statistics [2022]: Number of Health Informatics Specialists in the US (2021). Available at: https://www.zippia.com/health-informatics-specialist-jobs/demographics/ (Accessed November 9, 2022).
Health Information Technologists and Medical Registrars: Occupational Outlook Handbook: U.S. Bureau of Labor Statistics (n.d.). Available at: https://www.bls.gov/ooh/healthcare/health-information-technologists-and-medical-registrars.htm (Accessed June 16, 2023).
Healthcare Occupations: Occupational Outlook Handbook: U.S. Bureau of Labor Statistics (n.d.). Available at: https://www.bls.gov/ooh/healthcare/home.htm (Accessed June 16, 2023).
Hencke, J., Eck, M., Sass, J., Hastedt, D., and Mejia-Rodriguez, A. M. (2022). April 2022: missing out on half of the world’s potential: fewer female than male top achievers in mathematics and science want a career in these fields|IEA.Nl. International Association for the Evaluation of Educational Achievement Available at: https://www.iea.nl/publications/series-journals/iea-compass-briefs-education-series/april-2022-missing-out-half-worlds.
Hoffman, H. K., Trawalter, S., Axt, J. R., and Oliver, M. N. (2016). Racial bias in pain assessment and treatment recommendations, and false beliefs about biological differences between blacks and whites. Proc. Natl. Acad. Sci. U. S. A. 113, 4296–4301. doi: 10.1073/pnas.1516047113
Howard, A. P., Slaughter, L. S., Carey, K. M., and Lillard, J. W. (2021). Bridges to biotechnology and bioentrepreneurship: improving diversity in the biotechnology sector. Nat. Biotechnol. 39, 1468–1474. doi: 10.1038/s41587-021-01110-3
Informatics: Research and Practice|AMIA - American Medical Informatics Association (n.d.). Available at: https://amia.org/about-amia/why-informatics/informatics-research-and-practice (Accessed June 9, 2023).
Johnson-Agbakwu, C. E., Ali, N. S., Oxford, C. M., Wingo, S., Manin, E., and Coonrod, D. V. (2020). Racism, COVID-19, and health inequity in the USA: a call to action. J. Racial Ethn. Health Disparities 9, 52–58. doi: 10.1007/s40615-020-00928-y
Kang, H. (2013). The prevention and handling of the missing data. Korean J. Anesthesiol. 64, 402–406. doi: 10.4097/kjae.2013.64.5.402
Ly, D. P. (2022). Historical trends in the representativeness and incomes of black physicians, 1900–2018. J. Gen. Intern. Med. 37, 1310–1312. doi: 10.1007/s11606-021-06745-1
MacPhee, D., Farro, S., and Canetto, S. S. (2013). Academic self-efficacy and performance of underrepresented STEM majors: gender, ethnic, and social class patterns. Anal. Soc. Issues Public Policy 13, 347–369. doi: 10.1111/asap.12033
Master of Science, Health Informatics Salary|PayScale (n.d.). Available at: https://www.payscale.com/research/US/Degree=Master_of_Science_(MS)%2C_Health_Informatics/Salary (Accessed June 16, 2023).
McGee, E., Fang, Y., Ni, Y., and Monroe-White, T. (2021). How an anti-science president and the COVID-19 pandemic altered the career trajectories of STEM PhD students of color. Aera Open 7:233285842110392. doi: 10.1177/23328584211039217
Mendez, R. G., Torres, J., Ishwad, P., Nicholas, H. B., and Ropelewski, A. (2016). Assisting bioinformatics programs at minority institutions: needs assessment, and lessons learned -- a look at an internship program. in Proceedings of the XSEDE16 Conference on Diversity, Big Data, and Science at Scale XSEDE16. New York, NY: Association for Computing Machinery), 1–8.
Miller-Cotto, D., and Schunn, C. (2020). Mind the gap: how a large-scale course re-design in economics reduced performance gaps. J. Exp. Educ. 90, 783–796. doi: 10.1080/00220973.2020.1805717
Moscato, J., Gopalkrishnan, V., Lotze, M., and Becich, M. (2014). Creating a pipeline of talent for informatics: STEM initiative for high school students in computer science. J. Pathol. Informatics 5:12. doi: 10.4103/2153-3539.129448
Nelson, R. (2019). Racism in science: the taint that lingers. Nature 570, 440–441. doi: 10.1038/d41586-019-01968-z
NORC at University of Chicago (2013). Understanding the impact of health IT in underserved communities and those with health disparities. Available at: https://www.healthit.gov/sites/default/files/hit_disparities_report_050713.pdf.
Pew Research Center (n.d.). Internet surveys. Collecting survey data. Available at: https://www.pewresearch.org/politics/methodology/collecting-survey-data/internet-surveys/ (Accessed February 23, 2023).
Phillips, N., Park, I.-W., Robinson, J. R., and Jones, H. P. (2020). The perfect storm: COVID-19 health disparities in US blacks. J. Racial Ethn. Health Disparities 8, 1153–1160. doi: 10.1007/s40615-020-00871-y
RBC Capital Markets|Navigating the Changing Face of Healthcare Episode (n.d.). Available at: https://www.rbccm.com/en/gib/healthcare/story.page (Accessed June 16, 2023).
Reinsel, D., Gantz, J., and Rydning, J. (2018). The digitization of the world - from edge to Core. Data age 2025: international data corporation Available at: https://www.seagate.com/files/www-content/our-story/trends/files/idc-seagate-dataage-whitepaper.pdf.
Rights (OCR) (2009). HITECH act enforcement interim final rule. Available at: https://www.hhs.gov/hipaa/for-professionals/special-topics/hitech-act-enforcement-interim-final-rule/index.htmlHHS.gov (Accessed June 12, 2023).
Scholarships for Disadvantaged Students|Benefits.gov (n.d.). Available at: https://www.benefits.gov/benefit/875 (Accessed October 25, 2022).
Sharma, R., Tikka, S. K., Bhute, A. R., and Bastia, B. K. (2021). Adherence of online surveys on mental health during the early part of the COVID-19 outbreak to standard reporting guidelines: a systematic review. Asian J. Psychiatr. 65:102799. doi: 10.1016/j.ajp.2021.102799
Southerland, W. M., Swamidass, S. J., Payne, P. R. O., Wiley, L., and Williams-DeVane, C. (2018). The diversity and disparity in biomedical informatics (DDBI) workshop. Pac. Symp. Biocomput. 23, 614–617. doi: 10.1142/9789813235533_0056
Togioka, B., Duvivier, D., and Young, E. (2022). Diversity and discrimination in healthcare. StatPearls. Available at: https://www.statpearls.com/ArticleLibrary/viewarticle/130469 (Accessed November 9, 2022).
US Census Bureau (2019). The black alone population in the United States: 2018.. Available at: https://www.census.gov/data/tables/2018/demo/race/ppl-ba18.htmlCensus.gov (Accessed March 8, 2023).
USF Health (2018). Does responsibility of building diversity in health informatics fall to universities? EOE Journal Available at: https://eoejournal.com/building-diversity-in-health-informatics/.
Veinot, T. C., Ancker, J. S., and Bakken, S. (2019). Health informatics and health equity: improving our reach and impact. J. Am. Med. Inform. Assoc. 26, 689–695. doi: 10.1093/jamia/ocz132
Vyas, D. A., Eisenstein, L. G., and Jones, D. S. (2020). Hidden in plain sight—reconsidering the use of race correction in clinical algorithms. N. Engl. J. Med. 383, 874–882. doi: 10.1056/NEJMms2004740
Walton, G. M., and Cohen, G. L. (2011). A brief social-belonging intervention improves academic and health outcomes of minority students. Science 331, 1447–1451. doi: 10.1126/science.1198364
Ware, A. D., Murdock, T., Voltaggio, L., Windon, A. L., Troncoso, J. C., Hruban, R. H., et al. (2019). The “race” toward diversity, inclusion, and equity in pathology: the Johns Hopkins experience. Acad. Pathol. 6:2374289519873104. doi: 10.1177/2374289519873104
Keywords: health informatics, diversity, equity, inclusion, health disparities, pipeline programs, underrepresented minorities
Citation: Howard AP, Slaughter LS, Simmonds C, McPherson R, Kennedy N and Bentley K (2023) Bridge to health informatics—a 5-week intensive online program to increase diversity in health informatics. Front. Educ. 8:1194746. doi: 10.3389/feduc.2023.1194746
Edited by:
Miriam Segura-Totten, University of North Georgia, United StatesReviewed by:
Veronica A. Segarra, Goucher College, United StatesAnthony Solomonides, NorthShore University HealthSystem, United States
Copyright © 2023 Howard, Slaughter, Simmonds, McPherson, Kennedy and Bentley. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Angelita P. Howard, YWhvd2FyZEBtc20uZWR1
 Angelita P. Howard
Angelita P. Howard Liane Siu Slaughter
Liane Siu Slaughter Consuela Simmonds
Consuela Simmonds Rebecca McPherson
Rebecca McPherson Nia Kennedy1
Nia Kennedy1 Keisha Bentley
Keisha Bentley