- 1Clinical College of Anhui Medical University, Hefei, China
- 2School of Nursing, Anhui University of Chinese Medicine, Hefei, China
- 3School of Nursing, Anhui Medical University, Hefei, China
Background: Medical students suffer more pressure due to various reasons and their mental health problems get more attention. Resilience is a positive psychological perspective to explore the medical students’ mental health and coping style problems. This study focuses on the medical students in school and uses the method of latent category analysis (LCA) to analyze the classification characteristics of their resilience. Therefore, the study aims to help psychological educators in medical colleges to develop positive mental health education strategies for medical students.
Objective: To explore the potential categories of resilience of medical students and the relationship between these categories and mental health and coping style.
Methods: A total of 1,457 medical students from four medical colleges in Anhui Province were selected as the research subjects by a convenience sampling method. A general information questionnaire, the Connor-Davidson Resilience Scale (CD-RISC), Kessler 10 and the Simplified Coping Style Questionnaire (SCSQ) were used to investigate; SPSS 25.0 and Mplus 7 software were used for basic analysis and latent category exploration.
Expected results: The medical students were divided into three potential categories of mental resilience: the low resilience group, moderate resilience self-improvement group and high resilience tough group. The optimism dimension level of the three categories was low. There were statistically significant differences in the distribution of resilience among medical students, such as gender, source of students, and paternal and maternal education level. There were significant differences in the mental health, positive coping style and negative coping style scores among the three categories. Female medical students with low parental education levels have a lower level of resilience. Logistic regression analysis showed that a lower maternal education level was a risk factor for resilience level, and a high positive coping style score and gender were protective factors for resilience level.
Discussion: There are group differences in the resilience of medical students, which suggests that school health workers should formulate targeted intervention programs for different types of students to improve their resilience and mental health, and further more, this study reminds mental health workers in colleges and universities to pay more attention to the mental health status of female medical students whose parents are less educated.
Introduction
Medical students are an important part of the development of health services. Because of the strong professional content, various subjects, long academic cycle, postgraduate entrance examinations and employment problems, medical students are under increased pressure, and their mental health and stress coping have received more attention (Liu et al., 2020). At present, the global pandemic is still spreading, and the new coronavirus will coexist with us for a long time, which will significantly increase challenges for the mental health of the population, especially depression, anxiety and stress coping (Gianfredi et al., 2021). Studies have shown that obsessive symptoms, anxiety, terror and psychosis of medical students are higher than those of the national norms (Zhang et al., 2021). It has been well shown that students experience stress and anxiety due to the nature and rigor of medical school if protective factors, such as “Grit” and “Resilience,” aid some students’ ability to cope better than others (Haskett et al., 2022).
Psychological resilience has been widely studied as a top quality. Masten (2015) believed that resilience may be affected by a series of activities, such as receiving effective care since childhood, the development of intimate relationships with adults, and learning effective problem-solving skills, which can help adults achieve self-awareness and emotional control and participate in meaningful projects. Resilience can helps individuals recover from depression and disappointment, resist adverse environmental effects and make positive adjustments in adverse environments. It can help individuals obtain physical and mental balance energy, successfully adapt to challenging life pressures and improve their wellbeing (Tedeschi and Kilmer, 2005; Liz and Hasson, 2020). Ran et al. (2020) studies found that the higher the resilience score, the lower the anxiety and depression levels. And students with higher resilience scores were more optimistic about clinical education. Those with higher resilience scores were less likely to report anxiety, insomnia, and tiredness (Haskett et al., 2022). Therefore, it is imperative to determine factors associated with or influencing resilience in Chinese medical students. It is also important to consider separate component factors of resilience since resilience is multi-dimensional (Birhanu et al., 2017). For example, in the contemporary context, we need to understand the resilience of medical students and their general characteristics (Such as gender, age, major, grade, paternal and maternal education level and so on), coping style and other factors. Previous studies had shown that different studies had found differences in resilience of medical students in gender comparison. Some studies found there were significant differences between females and males in the dimension of interpersonal assistance of resilience, the interaction effect of resilience with emotional abuse on depressive symptoms was stronger in females compared to males (Ding et al., 2020; Wei et al., 2021). However, Miao et al. (2019) found that male medical students scored higher on resilience than female medical students (Peng et al., 2012). Except gender, there are few studies on the influence of parents’ education level, students’ major and other general characteristics on the resilience of medical students. Fletcher et al.’s (2020) study found that maternal education level affected college students’ mental health and learning behaviors in school and promoted college students’ interpersonal relationships and academic achievement.
Resilience can reduce the risk of individual psychological problems, and it is a protective factor to maintain and promote mental health. It is often regarded by researchers as a moderator of mental health (Efstathopoulou and Bungay, 2021). Coping style can affect people’s perceptions and management of stressful events. Some studies have shown that there is a certain correlation between psychological resilience and coping style. Improving the level of psychological resilience is conducive for individuals to adopt positive coping styles. Resilience seems to be a protective factor to reduce the impact of stressors (Connor et al., 2021). Therefore, from the perspective of positive psychology, exploring the psychological resilience of medical students to understand the mental health of medical students and how they cope with stress will open a new way of thinking.
Current research methods on resilience are mainly based on variable-centered ideas and methods, and different critical values are divided on the grounds of the scale scores to evaluate and determine the level of individual resilience (Wang et al., 2020). Miao analyzed related research on the resilience of medical students in China and found that the current studies on the psychological resilience of medical students has mainly focused on the relationship between the total resilience score and related variables (Miao et al., 2021). It is believed that the research method of the psychological resilience of medical students in China is still in its infancy, and further specific and systematic research is urgently needed. Due to the complexity of the resilience dimension, individuals in the total sample are often heterogeneous, the total score may conceal specific information, and there may be deficiencies in distinguishing different characteristics and qualitative differences between groups (Fang et al., 2017). Therefore, the evaluation and development of medical students’ resilience should be based on the individual-centered perspective to explore the category characteristics and mode transformation of individual or group resilience of medical students. The homogeneity of resilience of medical students was investigated by category analysis method, so as to realize the dynamic grasp of the transformation trend of individual resilience of medical students. At the same time, it also provided theoretical basis for developing individualized intervention plan of resilience for medical students and improving their mental health level.
Research on individual orientation is helpful for analyzing the psychology and behavior of groups or individuals and has great breakthrough significance for further research on relationship (Gong et al., 2020). Individual-centered latent category analysis (LCA) has attracted increasing attention. LCA focuses on the relationship between variables, helps researchers understand the mixing of variables and the results of specific groups, determines different types of subgroups based on differences in the nature and degree of explicit variables, and captures population inequality, which cannot be observed in variable-centered research (Wang, 2018). At present, the research fields of potential models of resilience at home and abroad mainly involve young graduate students, children, police, empty-nest elderly individuals and cancer patients (Fang et al., 2017; Zhang et al., 2017; van der Meulen et al., 2019; Chen et al., 2022). This kind of research confirmed the difference in resilience of the research subjects and provided the corresponding objective description for the intragroup and intergroup differences in the psychological resilience of different groups. At present, studies on the latent category model of medical students include the stress perception (Liu et al., 2020) and suicide attempts of medical vocational students (Nan et al., 2022) but less frequently include resilience. This study focused on medical students. LCA was used to analyze the characteristics of the psychological resilience of medical students. The differences in the scores of mental health and coping styles among various potential categories were further explored. The effects of gender, major and grade on the potential classification of resilience were also discussed. The results provide the basis for the development of targeted intervention measures for positive mental health education for medical students.
Methods
Research subjects
Based on the principle of convenience sampling, this study selected undergraduate and specialized medical students from four medical colleges in Anhui Province. The purpose and precautions of the investigation were explained by on-site investigators. After informed consent was obtained, the two-dimensional code was scanned to complete the electronic questionnaire. After reviewing and eliminating invalid questionnaires, all survey content was kept strictly confidential. The inclusion criteria were students in medical school and those who provided informed consent. The exclusion criterion were students with mental illness and a previous history of mental illness. A total of 1,505 people met the criteria, and 1,457 responded, including 678 boys and 779 girls aged 20.21 ± 1.41 years. The effective response rate was 96.8%.
Research variables
Demographic indicators
The demographic data questionnaire was self-designed by the research group based on a literature review to collect the basic information about medical students, including 10 parameters such as gender, age, academic type, major, grade, paternal and maternal education level, source of students, etc.
Resilience
Connor-Davidson Resilience Scale (CD-RISC) was translated and revised by Yu (Yu and Zhang, 2005). The scale contained 25 items with three dimensions: optimism (e.g., No matter what happens I can cope with), self-improvement (e.g., I tend to recover quickly after a hard time or illness) and tenacity (e.g., I can make unusual or difficult decisions). Scores were calculated using a 5-point Likert scale from 0 (never like this) to 4 points (almost always). The total score ranged from 0∼100. The higher the score was, the better the resilience. The reliability and validity of the scale were good. Cronbach’s alpha for this scale is 0.95.
Mental health
The Kessler 10 scale was used for evaluating mental health, and included 10 items (e.g., Do you often feel restless?). A 5-point Likert scale ranging from 1 (almost never) ∼ 5 points (all the time) was used, and the total score ranges from 10 to 50 points. The higher the score, the worse the psychological status (Tran et al., 2019). The reliability and validity of the scale were good. Cronbach’s alpha for this scale is 0.96.
Coping style
Style Questionnaire (SCSQ) was used to assess the coping style of the research subjects (Xie, 1998). With 20 items in total, it is divided into two dimensions: positive coping (e.g., Try to look on the bright side) and negative coping (e.g., Accept it, because there is no other way). A 4-point scale, ranging from 0 (not used) to 3 (frequently used), is used. The scores of each dimension are obtained by adding the items. The reliability and validity of the questionnaire in different age groups were good (Fang et al., 2018). Cronbach’s alpha for this scale is 0.90.
Missing data
Data were collected by electronic questionnaire in this study. Before the formal investigation, the investigators of the research group and the assistance personnel of each school were trained. The investigators were responsible for explaining the investigation purpose and matters needing attention in filling out the questionnaire, answering relevant questions on site, and reviewing the questionnaire. Before data retrieval and entry, researchers conducted error checking, omission checking and logic checking on the questionnaire again, eliminated questionnaires with obvious logic errors, and adopted full information maximum likelihood processing for missing values, so as to effectively control the completion rate and efficiency of the questionnaire. Logic detection function is a special function in the design of electronic questionnaire, which can effectively reduce invalid questionnaires by setting option skip logic, topic association logic, option association logic and option reference logic. Missing data was estimated using the full information maximum likelihood (FIML) method. FIML was chosen due to its ability to retain cases with missing data, therefore avoiding potentially biased parameter estimates through pairwise and listwise deletion (Schafer and Graham, 2002).
Statistical methods
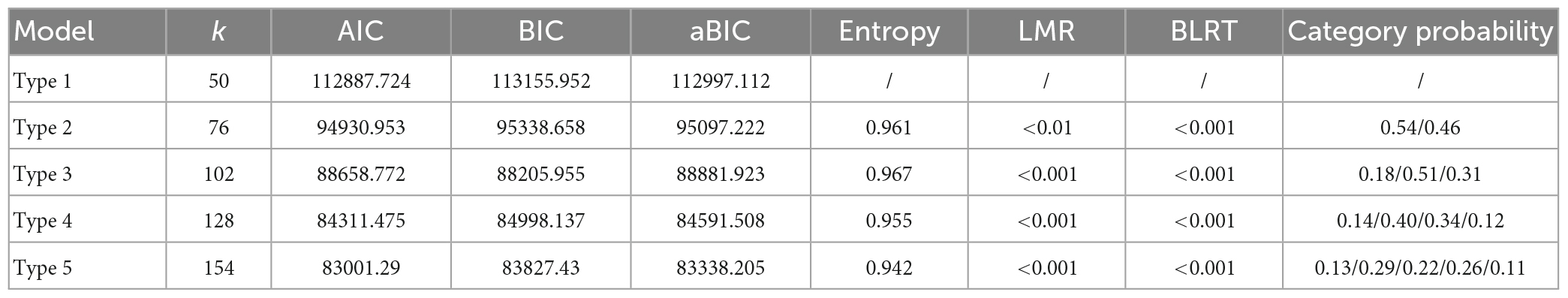
Based on the scores of each item of resilience, this study used Mplus 8.2 software to conduct latent profile analysis (LPA), fitting 1∼5 potential profile models using the Akaike information criterion (AIC), Bayesian information criterion (BIC), adjusted BIC (aBIC) and average information volume (entropy). The lower the AIC, BIC and aBIC, the higher the entropy (≥0.8 indicates that at least 90% of the individuals were correctly classified), and the higher the fitting degree of the model (Wang et al., 2020). The P-values of the LMR and blrt reached a significant level, which indicated that the K classification model had a better fitting effect than the k-1 model (Yang et al., 2021). On this basis, SPSS 25.0 was used to analyze the distribution differences of psychological resilience in the demographic variables of the medical students. The χ2 relationship between psychological resilience and related variables was analyzed by a multiple logistic regression model. The inspection level was set at α = 0.05.
Results
Potential profile analysis of medical students’ resilience
Taking the score of 25 items of resilience as the explicit variable, 1–5 potential profile models were established to estimate the model fitting of the pre-profile analysis of the characteristics of medical students’ resilience. With the increase in the number of classifications, the AIC, BIC, and aBIC decreased continuously, while the AIC, BIC, and aBIC decreased slightly when the number of categories was three. This showed that the optimization degree of potential profile model fitting decreased with the increase in the number of categories. Comparing the significance levels of the 3–5 category models, the P-values of the LMR and blrt were less than 0.001, both reaching a significant level. However, when psychological resilience was divided into three categories, entropy had the highest classification accuracy. Considering the above indicators, the simplicity of the model and the readability of the results, medical students’ resilience was divided into three types as the optimal classification results, as shown in Table 1.
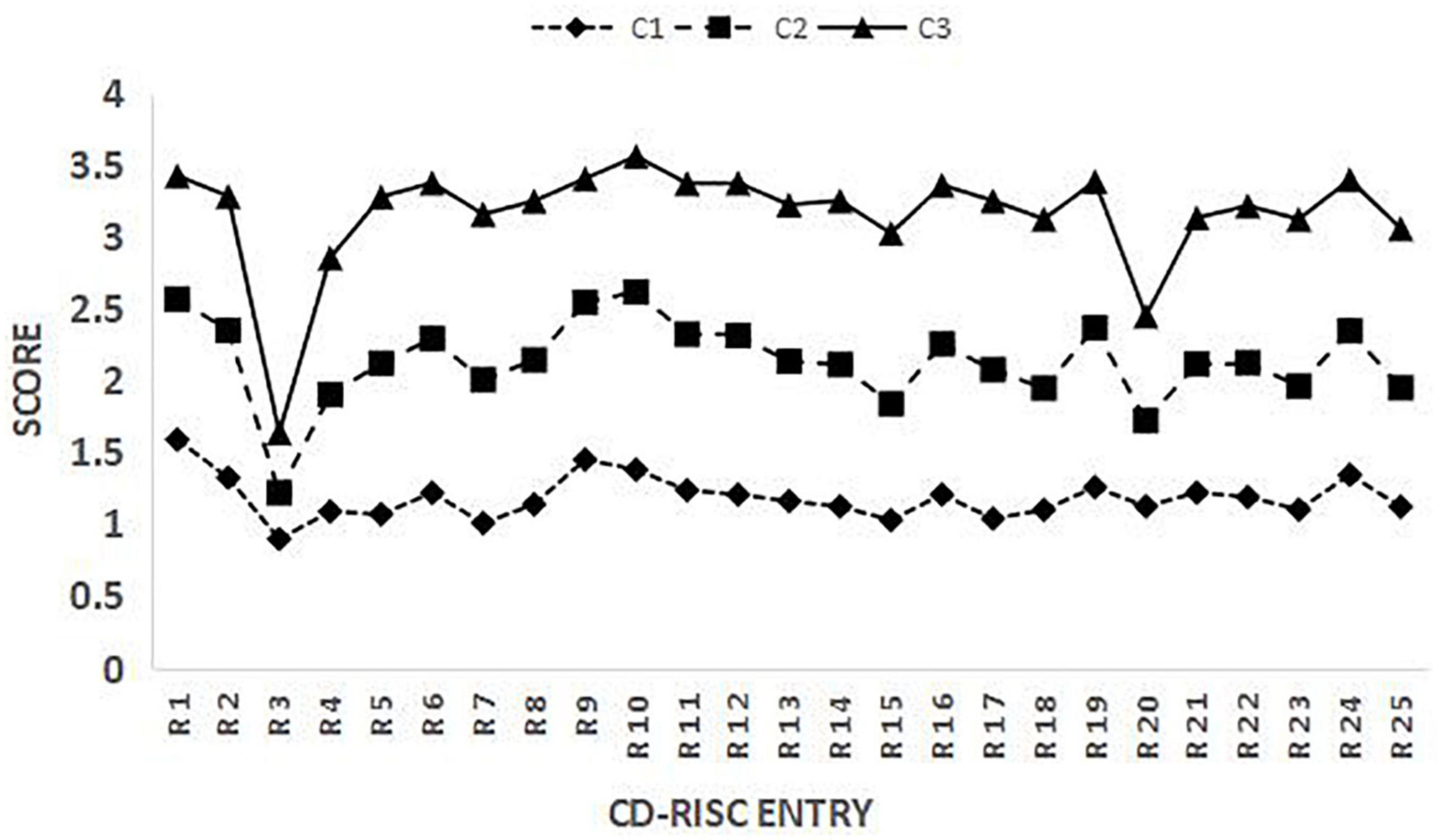
Characteristics and nomenclature of potential categories of medical students’ resilience
The scores of each potential category for 25 items are shown in Figure 1. The resilience scores of medical students in Category 1 (C1), Category 2 (C2), and Category 3 (C3) increased in turn. In this study, it was found that there was obvious group heterogeneity in the resilience of school medical students, which had obvious classification characteristics. There were 258 medical students included in Category 1 named “low resilience group,” accounting for 17.7% of the total sample. Students with the lowest total resilience scores and scores of each dimension were included in the “low resilience group.” There were 743 medical students included in Category 2 named “moderate resilience self-improvement group,” accounting for 51.0% of the total sample. Their resilience was generally at the medium level, and the score of the self-improvement dimension was higher. There were 456 medical students included in Category 3, accounting for 31.3% of the total sample. The overall level of resilience was the highest for these students. Among these students, the score of the tenacity dimension was higher; therefore, this group was named the “high resilience tenacity group,” as shown in Figure 1.
Univariate analysis of potential categories of medical students’ resilience
The differences in the latent category distribution of the resilience of medical students with different genders, majors, academic types, grades, origins, and paternal and maternal education levels were compared. There were statistically significant differences in gender, source of the students, and paternal and maternal education level (P < 0.05), as shown in Table 2.
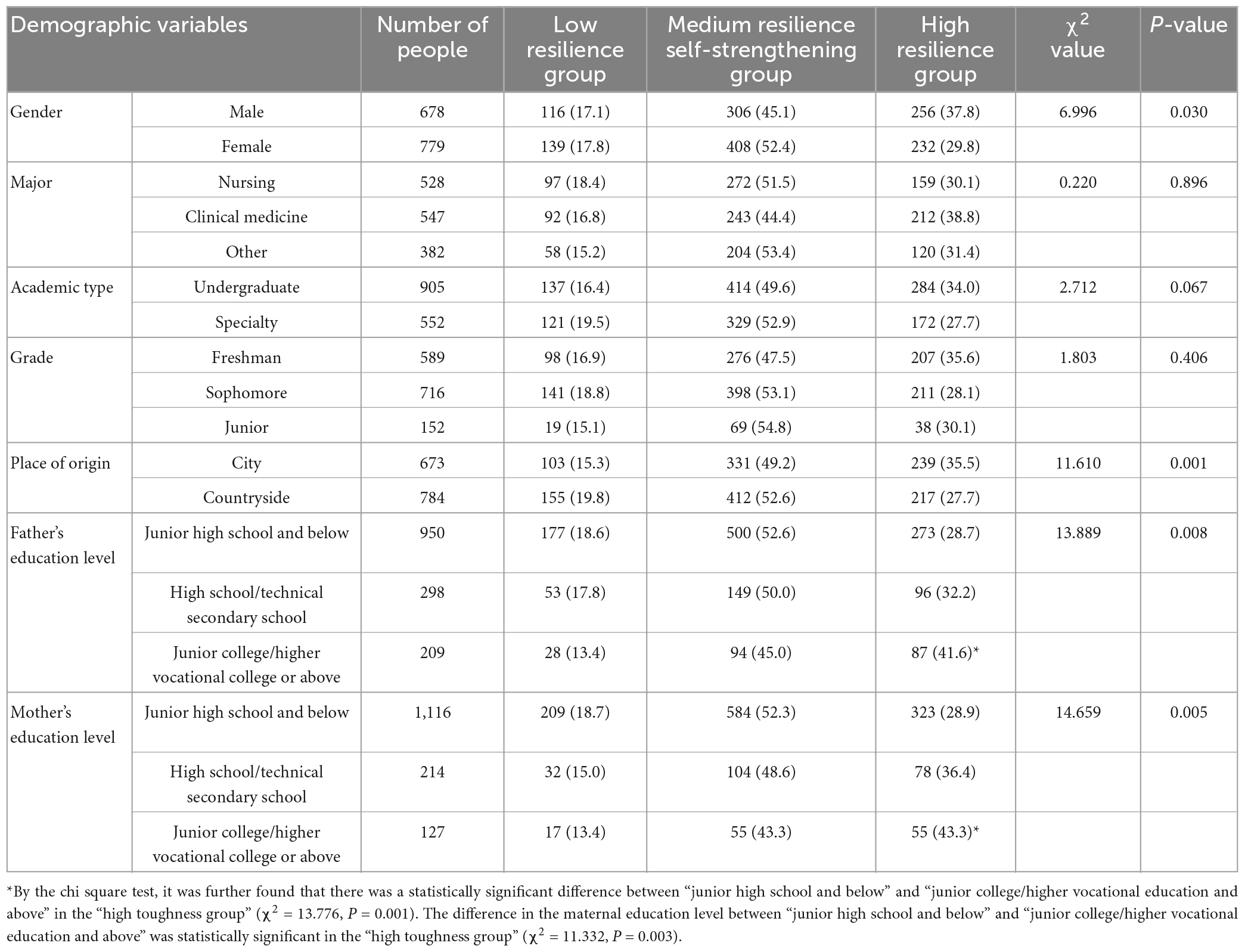
Table 2. Comparison of potential categories of the resilience of medical students with different demographic characteristics.
The scores of medical coping style and the mental resilience of students were compared. There were significant differences in the mental health scores and coping styles among students with different types of resilience, and there were statistically significant differences between the total mental health score and the coping style scores (P < 0.001), as shown in Table 3.
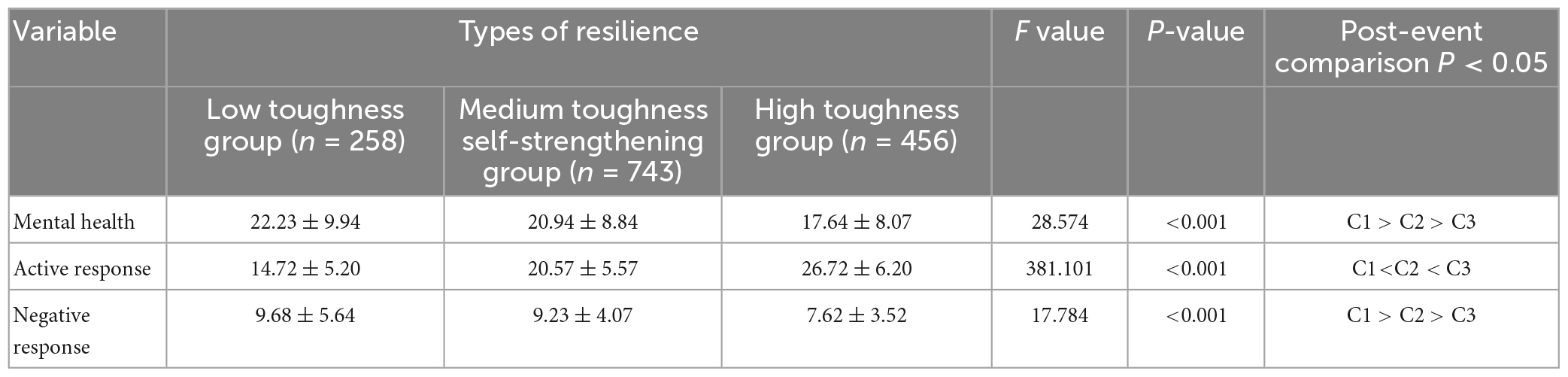
Table 3. Comparison of the mental health and coping style scores of medical students in potential categories of psychological resilience.
Multifactor analysis of potential categories of medical students’ resilience
Taking the three potential categories of psychological resilience as the dependent variables and Category 3 (high resilience group) as the reference category, the single factor was included in the ordered logistics regression analysis as an independent variable. The parallel line test showed a P < 0.05, so multiple logistic regression analysis was used. The results showed that compared with “high resilience,” a lower maternal education level was a risk factor for resilience level (P < 0.05), while a high score for positive coping style and male gender were protective factors for resilience level (P < 0.001), as shown in Table 4.
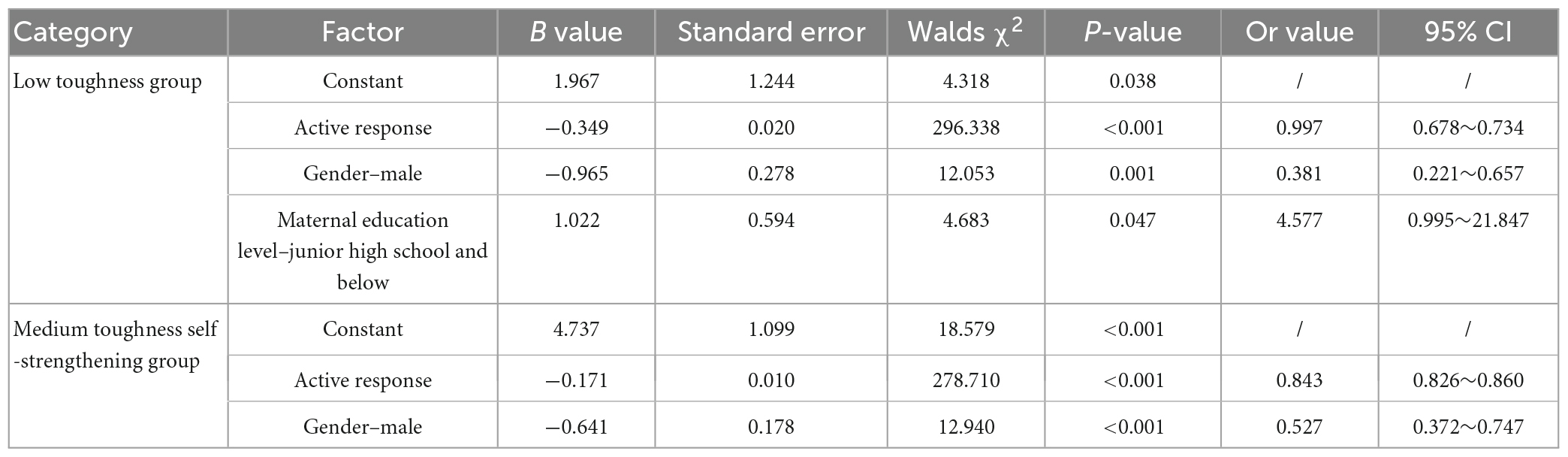
Table 4. Multiple logistic regression analysis of potential categories of psychological resilience of medical students.
Discussion
Because of the complexity of the resilience dimension, if previous studies used the total score of the scale to evaluate the level of resilience, the total score may be the same but the items and dimensions may be different. An LCA can distinguish medical students in different characteristic categories and the differences between students in different categories. The medical students in this group may lack tenacity and positive coping skills in the face of adversity and pressure, and they lack adaptability to life and learning and self-confidence in the challenges of adversity and stress. This group of students is the focus of attention of mental health workers in colleges and universities. The students in the “medium resilience self-improvement group” and “high resilience tenacity group” may have better cognitive flexibility, show better self-regulation and adaptability to maintain internal and external balance in the face of pressure, and may take positive actions toward positive goals when experiencing adversity, showing good self-esteem, self-reliance, and self-confidence.
Further analysis found that the three categories of medical students’ resilience in this study showed a low optimistic tendency. An individual’s way of guiding the future is deeply rooted in their cognition and even shapes how they perceive and respond to opportunities and threats at the unconscious level. The optimistic pessimistic tendency plays a very important role (Magee et al., 2022). Optimism is defined as a tendency to be less susceptible to a series of negative events, and an optimistic personality is more beneficial to mental health (Aue and Okon-Singer, 2020). The medical students in this study did not have an optimistic tendency, which may be related to the continuous pandemic situation. Studies have shown that during the pandemic prevention and control period, medical students generally had high loneliness, high learning burnout and other problems and were more likely to suffer from severe mental illness (Wu S. et al., 2020; Fan et al., 2021). Medical students are more likely to be exposed to the new coronavirus in later internships, which requires higher standards and requirements for medical students’ medical practice skills (Wu Y. et al., 2020). At the same time, the pandemic situation has a great impact on the recruitment market and the traditional recruitment mode, resulting in employment difficulties for medical students at different stages and in greater demand and competition among medical students for postgraduate entrance examinations. Therefore, during the pandemic period, medical students were not confident enough to face the above problems, so the overall level of optimism was low.
Male students were more likely to be included in the “medium resilience self-improvement group” and “high toughness group.” Regression analysis showed that being male was a protective factor for resilience level, which was consistent with relevant research (Erdogan et al., 2015). This may be affected by the traditional culture of society. Families, schools and society tend to cultivate boys’ to have a stronger ability to resist pressure. Boys show higher adaptability when encountering difficulties. Therefore, their self-confidence and tenacity may be higher than those of girls. The study found that a low maternal education level is a risk factor for psychological resilience, which is consistent with other studies. Studies had examined that higher maternal educational achievement might help buffer stress sensitivity associated with heightened threat-related amygdala activity for young adults (Swartz et al., 2018). Sun believed that in the aspect of suicide ideation and planning among medical college students, maternal education level affected college students’ mental health and learning behaviors, and mothers may be more protective than fathers (Sun et al., 2017). Due to the influence of social culture, mothers often take more responsibility in their children’s education. Higher mother’s education level was related to higher resilience in emotion regulation, family support, and interpersonal assistance (Xiao et al., 2019). Mothers with higher education pay more attention to their children’s physical and mental education and can sensitively identify their children’s problems and provide corresponding psychological support in a timely manner. Their children may face pressure and difficulties with a more confident and tough attitude and have a higher level of psychological resilience. In contrast, when a mother’s education level is low, their psychological resilience is higher, and the resilience of their children may be affected.
This study also confirmed that the mental health score of medical students in the “high toughness group” was significantly lower than those of the other two groups, indicating that the mental health level of this group was significantly higher than those of the other two groups. Previous studies have reported on the relationship between resilience and mental health. It shows that people with higher resilience experience less psychological stress and lower levels of anxiety and depression after facing adversity or trauma (Riehm et al., 2021; Taylor et al., 2022). Although study stress and the ongoing epidemic might have a potentially direct and continuously impact on the mental health of medical students, resilience as a protective factor which helps medical students adapt to adversity, buffers anxiety and depression, and helps medical students mobilize their mental resources to effectively reduce the risk of mental health.
The high positive coping style scores of medical students in the “high resilience group” indicates that medical students in different psychological resilience groups have different levels of perceived stress during school and have good discrimination, and a positive coping style is a protective factor of resilience levels, which was consistent with the research of Liu et al. (2020). Coping and resilience are interrelated but different concepts. Coping is an important part of resilience. As an influencing factor of individual resilience, a positive coping mechanism can improve individual resilience (Yesilot, 2021). Therefore, medical students with positive coping styles may adopt more effective ways to deal with stressful events in their studies and lives. As a protective factor, a positive coping style is more conducive to improving the psychological resilience of medical students.
Limitations and future directions
There are still some limitations in this study. First, this study is a cross-sectional survey, it is difficult to determine the causal relationship between resilience and related indicators. In the future, it is necessary to establish a cohort study among representative samples to further elaborate the relationship between the distribution characteristics of resilience and mental health and coping styles of medical students. Second, the survey was only conducted in Anhui Province, and the results were insufficient in generalization, so it is necessary to further expand the sample group and verify the analysis results in later studies.
Conclusion and implications
In summary, this study used the method of potential profile analysis to identify the types of psychological resilience among medical students, which can be divided into three potential categories: the low resilience group, medium resilience self-improvement group and high resilience tough group. Male medical students with high parental education levels have a higher level of resilience, and female medical students with low parental education levels have a lower level of resilience. The results show that there is a correlation between resilience and the mental health and coping style of medical students. Medical students with a high level of resilience are healthier. It was found that a positive coping style, as a protective factor, affects the level of resilience. Therefore, this study reminds mental health workers in colleges and universities to pay attention to the mental health status of female medical students whose parents are less educated. College education and mental health workers need to better understand the heterogeneity of resilience of medical students, so as to provide reference for the development of individualized psychological education intervention measures.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
This study was approved by the expert committee of Clinical College of Anhui Medical University. The patients/participants provided their written informed consent to participate in this study.
Author contributions
J-YS, Y-QG, and H-PL were involved in the conceptualization and design of the study, and the development of the study protocol. J-YS, Y-QG, S-ML, and YY were involved in participant recruitment and data collection. J-YS and Q-QB lead the data analyses with consultation from JG and J-XL. J-YS, Y-QG, and H-PL wrote the first draft of the manuscript, with all authors working on several edits of this manuscript. All authors contributed to the article and approved the final submitted version.
Funding
This research was supported by the Social Sciences and Humanities Research Foundation of the Education Department of Anhui Province of China (No. SK2021A0845). Funders were not be involved in the development of this research.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Aue, T., and Okon-Singer, H. (2020). Cognitive biases in health and psychiatric disorders. San Diego, CA: Elsevier Science & Technology. doi: 10.1016/B978-0-12-816660-4.10000-5
Birhanu, Z., Ambelu, A., Berhanu, N., Tesfaye, A., and Woldemichael, K. (2017). Understanding resilience dimensions and adaptive strategies to the impact of recurrent droughts in Borana zone, Oromia Region, Ethiopia: a grounded theory approach. Int. J. Environ. Res. Public Health 14:118. doi: 10.3390/ijerph14020118
Chen, S. S., He, Y., Xie, G. D., Chen, L. R., Zhang, T. T., Yuan, M. Y., et al. (2022). Relationships among adverse childhood experience patterns, psychological resilience, self-esteem and depressive symptoms in Chinese adolescents: a serial multiple mediation model. Prev. Med. 154:106902. doi: 10.1016/j.ypmed.2021.106902
Connor, M. O., Reilly, G. O., Murphy, E., Connaughton, L., Hoctor, E., and McHugh, L. (2021). Resilience mediates the cross-sectional relationship between mindfulness and positive mental health in early adolescence. J. Context. Behav. Sci. 21, 171–175. doi: 10.1016/j.jcbs.2021.07.003
Ding, Y., Ruan, Y., Tu, J. W., and He, Z. D. (2020). Psychological resilience of medical students during CoVID–1 9 epidemic. Chin. J. Health Psychol. 28, 1366–1368. doi: 10.13342/j.cnki.cjhp.2020.09.020
Efstathopoulou, L., and Bungay, H. (2021). Mental health and resilience: arts on Prescription for children and young people in a school setting. Public Health 198, 196–199. doi: 10.1016/j.puhe.2021.07.021
Erdogan, E., Ozdogan, O., and Erdogan, M. (2015). University students’ resilience level: the effect of gender and faculty. Proc. Soci. Behav. Sci. 186, 1262–1267. doi: 10.1016/j.sbspro.2015.04.047
Fan, P. Y., Shang, Y. H., Zhu, B., Wang, J., Guo, C. T., Jin, J. Y., et al. (2021). Investigation and analysis of loneliness, learning burnout and resilience of medical students under the normalization of novel coronavirus pneumonia. Chin. J. Health Psychol. 29, 1230–1235. doi: 10.13342/j.cnki.cjhp.2021.08.025
Fang, J., Wang, Y. T., Xiao, S. Y., Zhao, M., Jiang, H., and Hu, M. (2018). Reliability and validity of simplified coping style questionnaire among adolescents. Chin. J. Clin. Psychol. 26, 905–909. doi: 10.16128/j.cnki.1005-3611.2018.05.015
Fang, L. Y., Zhang, D. J., Wu, L. L., and Hu, T. Q. (2017). Latent class analysis of the secondary school students’ psychological Suzhi:a person-centered perspective. Stud. Psychol. Behav. 15, 20–25. doi: 10.3969/j.issn.1672-0628.2017.01.004
Fletcher, J. M., Ross, S. L., and Zhang, Y. X. (2020). The consequences of friendships: evidence on the effect of social relationships in school on academic achievement. J. Urban Econ. 116:103241. doi: 10.1016/j.jue.2020.103241
Gianfredi, V., Sandro, P., and Santangelo, O. E. (2021). What can internet users’ behaviours reveal about the mental health impacts of the COVID-19 pandemic? A systematic review. Public Health 198, 44–52. doi: 10.1016/j.puhe.2021.06.024
Gong, L., Hu, Y., and Gao, X. (2020). Latent classes of resilience and links to SCL-90 of the graduate students. Norm. J. Southwest China (Nat. Sci.) 45, 82–88. doi: 10.13718/j.cnki.xsxb.2020.10.013
Haskett, L. A., Doster, D. L., Athanasiadis, D. I., Anton, N. E., Huffman, E. K., Wallach, P., et al. (2022). Resilience matters: student perceptions of the impact of COVID-19 on medical education. Am. J. Surg. 224, 358–362. doi: 10.1016/j.amjsurg.2022.01.022
Liu, Z., Zhang, Y., Liu, R. X., Liang, L. J., Zhang, R., and Wang, F. (2020). Latent profile analysis of perceived stress in medical students. Chin. J. Health Stat. 37, 859–861. doi: 10.3969/j.issn.1002-3674.2020.06.015
Liz, S., and Hasson, F. (2020). Resilience, stress, and psychological well-being in nursing students: a systematic review. Nurse Educ. Today 90:104440. doi: 10.1016/j.nedt.2020.104440
Magee, W., Elliott, M. R., Sinkewicz, M., Finlay, J., and Clarke, P. (2022). Who looks on the bright side? Optimistic and pessimistic perceptual-response reflexes over American adulthood. Adv. Life Course Res. 51:100452. doi: 10.1016/j.alcr.2021.100452
Masten, A. S. (2015). Ordinary magic: resilience in development. New York, NY: The Guilford Press. doi: 10.1037//0003-066x.56.3.227
Miao, Y. X., Ning, N., and Qiao, H. (2021). Analysis of research hotspots and frontiers of medical students’resilience based on CiteSpace. J. Harbin Med. Univ. 55, 436–446. doi: 10.3969/j.issn.1000-1905.2021.04.025
Miao, Y. X., Ning, N., and Wang, L. (2019). Study on the relationship between resilience, social support and quality of life of medical students under the background of doctor-patient relationship cognition. Health Vocat. Ed. 37, 137–139.
Nan, J., Jiang, H. J., Lin, L. N., Zhu, H. Q., and Guan, B. Q. (2022). The latent class and related factors of suicide ideation in medical vocational college freshmen. Chin. J. Health Psychol. 30, 275–281. doi: 10.13342/j.cnki.cjhp.2022.02.024
Peng, L., Zhang, J. J., Li, M., Li, P. P., Zhang, Y., Zuo, X., et al. (2012). Negative life events and mental health of Chinese medical students: the effect of resilience, personality and social support. Psychiatry Res. 196, 138–141. doi: 10.1016/j.psychres.2011.12.006
Ran, L., Wang, W., Ai, M., Kong, Y. T., Chen, J. M., and Kuang, L. (2020). Psychological resilience, depression, anxiety, and somatization symptoms in response to COVID-19: a study of the general population in China at the peak of its epidemic. Soc. Sci. Med. 262:113261. doi: 10.1016/j.socscimed.2020.113261
Riehm, K. E., Brenneke, S. G., Adams, L. B., Gilan, D., Lieb, K., Kunzler, A. M., et al. (2021). Association between psychological resilience and changes in mental distress during the COVID-19 pandemic. J. Affect. Disord. 282, 381–385. doi: 10.1016/j.jad.2020.12.071
Schafer, J. L., and Graham, J. W. (2002). Missing data: Our view of the state of the art. Psychol. Methods. 7:147–177. doi: 10.1037//1082-989X.7.2.147
Sun, L., Zhou, C. C., Xu, L. Z., Li, S. X., Kong, F. L., and Chu, J. (2017). Suicidal ideation, plans and attempts among medical college students in china: the effect of their parental characteristics. Psychiatry Res. 247, 139–143. doi: 10.1016/j.psychres.2016.11.024
Swartz, J. R., Knodt, A. R., Radtke, S. R., and Hariri, A. R. (2018). Post-secondary maternal education buffers against neural risk for psychological vulnerability to future life stress. Neuropsychologia 109, 134–139. doi: 10.1016/j.neuropsychologia.2017.12.019
Taylor, S. C., Smernoff, Z. L., Rajan, M., Steeman, S., Gehringer, B. N., Dow, H. C., et al. (2022). Investigating the relationships between resilience, autism-related quantitative traits, and mental health outcomes among adults during the COVID-19 pandemic. J. Psychiatr. Res. 148, 250–257. doi: 10.1016/j.jpsychires.2022.01.046
Tedeschi, R. G., and Kilmer, R. P. (2005). Assessing strengths, resilience, and growth to guide clinical interventions. Prof. Psychol. Res. Pract. 36, 230–237. doi: 10.1037/0735-7028.36.3.230
Tran, T. D., Kaligis, F., Wiguna, T., Willenberg, L., Nguyen, H. T. M., Luchters, S., et al. (2019). Screening for depressive and anxiety disorders among adolescents in Indonesia: formal validation of the centre for epidemiologic studies depression scale-revised and the Kessler psychological distress scale. J. Affect. Disord. 246, 189–194. doi: 10.1016/j.jad.2018.12.042
van der Meulen, E., van der Velden Marc, J. P. M., and van der Velden, P. G. (2019). Stability of psychological resilience of police officers: a three-wave latent class analysis. Pers. Individ. Differ. 144, 120–124. doi: 10.1016/j.paid.2019.03.006
Wang, M. C. (2018). Latent variable modeling and Mplus application advanced article. Chongqing: Chongqing University Press.
Wang, Q. L., Li, H. P., Hu, S. H., Chen, J. J., Wang, Y. X., and Wu, D. Y. (2020). Relationship between resilience and subjective well-being in cancer patients: based on latent profile analysis. Chin. J. Health Psychol. 28, 1617–1623. doi: 10.13342/j.cnki.cjhp.2020.11.005
Wei, J. S., Gong, Y. S., Wang, X. M., Shi, J. X., Ding, H. S., Zhang, M. L., et al. (2021). Gender differences in the relationships between different types of childhood trauma and resilience on depressive symptoms among Chinese adolescents. Prev. Med. 148:106523. doi: 10.1016/j.ypmed.2021.106523
Wu, S., Li, Z., Li, Z., Xiang, W., Yuan, Y., Liu, Y., et al. (2020). The mental state and risk factors of Chinese medical staff and medical students in early stages of the COVID-19 epidemic. Compr. Psychiatry 102:152202. doi: 10.1016/j.comppsych.2020.152202
Wu, Y., Yu, Z. F., Cheng, L. W., and Feng, J. (2020). Strengthening the standardized training management of residents during the prevention and control of COVID-19. Shanghai Med. 41, 3–4, 12. doi: 10.3969/j.issn.1006-1533.2020.08.002
Xiao, Y. Y., Wang, Y. Y., Chang, W., Chen, Y., Yu, Z., and Risch, H. A. (2019). Factors associated with psychological resilience in left-behind children in southwest China. Asian J. Psychiatr. 46, 1–5. doi: 10.1016/j.ajp.2019.09.014
Xie, Y. N. (1998). A preliminary study on the reliability and validity of the simple coping style scale. Chin. J. Clin. Psychol. 6, 114–115.
Yang, Y. J., Xu, H. L., Wang, Y., Xie, Y., Zou, L. W., Li, T. T., et al. (2021). Latent classes of health risk behaviors in medical students and depressive symptom. Chin. J. Sch. Health 42, 583–592. doi: 10.16835/j.cnki.1000-9817.2021.04.024
Yesilot, S. B. (2021). Coping styles and resilience in women living in the same neighborhood with distinct cultures. Int. J. Intercult. Relat. 84, 200–209.
Yu, X. N., and Zhang, J. X. (2005). “Application of connor-davidson resilience scale (CD-RISC) in the mainland of China,” in Proceedings of the 10th national psychological conference, (Shanghai: East China Normal University), 7.
Zhang, D. F., Gao, X. M., and Lu, Y. (2021). Exploring the mechanism of negative life events on the mental health in medical students:the mediating role of mental resilience. J. Nanjing Univ. Trddit. Chin. Med. (Soc. Sci. Ed.) 22, 30–35.
Keywords: resilience, mental health, coping style, latent category analysis, medical students
Citation: Song J-Y, Gao Y-Q, Li H-P, Gao J, Li J-X, Bi Q-q, Li S-M and Ye Y (2023) The latent category of resilience and its relationship with the mental health and coping styles of medical students. Front. Educ. 8:1114352. doi: 10.3389/feduc.2023.1114352
Received: 02 December 2022; Accepted: 02 May 2023;
Published: 15 May 2023.
Edited by:
María Luisa Zagalaz-Sánchez, University of Jaén, SpainReviewed by:
Dewen Liu, Nanjing University of Posts and Telecommunications, ChinaWahyu Rahardjo, Gunadarma University, Indonesia
Copyright © 2023 Song, Gao, Li, Gao, Li, Bi, Li and Ye. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hui-Ping Li, bGlodWlwaW5nQGFobXUuZWR1LmNu
†These authors have contributed equally to this work and share first authorship
 Jiang-Yan Song
Jiang-Yan Song Ya-Qin Gao
Ya-Qin Gao Hui-Ping Li
Hui-Ping Li Jie Gao
Jie Gao Jia-Xin Li3
Jia-Xin Li3 Shu-Mei Li
Shu-Mei Li