
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Educ., 16 August 2022
Sec. Higher Education
Volume 7 - 2022 | https://doi.org/10.3389/feduc.2022.978796
This article is part of the Research TopicEducation and Innovative Perspectives in Higher EducationView all 24 articles
 Joana Berger-Estilita1,2*
Joana Berger-Estilita1,2* Sofia Merlo3
Sofia Merlo3 Sissel Guttormsen1
Sissel Guttormsen1 Alexander Fuchs4
Alexander Fuchs4 Robert Greif4,5†
Robert Greif4,5† Hsin Chiang4†
Hsin Chiang4†Background: The several definitions of Interprofessional Education (IPE) allow for different interpretations and interchangeable terms. This study aims to determine the characteristics and attributes of the definition of IPE.
Materials and methods: In November 2019, 31 medical students (64.5% female) from a single institution took part in nine semi-structured interviews. We created a deductive three-level code system followed by an inductive code system based on several known IPE definitions. We extracted the main entities of the concept of IPE according to both code systems to create a framework. We used MaxQDA software for qualitative analysis. Verification of codes and categories was attained through sequential peer-debrief.
Results: Participants correctly named the WHO’s definition of IPE, and outlined its four main dimensions according to the Interprofessional Education Collaborative report. We found new IPE attributes and demonstrated the weight of communication and role recognition. Two-thirds of medical students mentioned IPE activities that we classified as a contrary model (without collaboration or patient-centeredness) and a minimum weight was given to the importance of patient-centeredness.
Conclusion: Medical students’ understanding of the concept of IPE is coherent. We deepened the understanding of previously identified definitions of IPE, and we identified new attributes of the concept. Finally, we added “well-being” as a component of interprofessionality.
Clinical Trial Registration: [https://www.isrctn.com/], identifier [ISRCTN41715934].
Interprofessional Education (IPE) is fundamental to the excellent functioning of healthcare systems (Lapkin et al., 2013). It enhances attitudes toward collaboration and teamwork during medical formation, leading to improved attitudes toward interprofessionality upon graduation and better patient outcomes (Reeves et al., 2016). Its implementation in medical curricula is strongly recommended (Bandali et al., 2011).
Literature shows that medical students display very positive attitudes toward IPE (Ruebling et al., 2014; Chua et al., 2015; Luderer et al., 2017; Berger-Estilita et al., 2020a). Medical students in pre-clinical years have more positive attitudes, when compared to students in later stages of their training (Kozmenko et al., 2017; de Oliveira et al., 2018; Berger-Estilita et al., 2020a). Factors contributing to this decline in interprofessional attitudes include being more experienced in the healthcare field (McFadyen et al., 2010), previous IPE contact (Anderson and Thorpe, 2008), previous less positive experiences in IPE (Coster et al., 2008; Hudson et al., 2016; Visser et al., 2017) and having parents working in healthcare (Cooper et al., 2005).
The World Health Organization’s Framework for Action in Interprofessional Education and Collaborative Practice (WHO, 2010) defines IPE as an activity of “students from two or more professions learn about, from, and with each other to enable effective collaboration and improve the quality of care.” However, a closer look at the literature reveals several different interpretations and interchangeable terms (Olenick et al., 2010):
• According to the Centre for Advancement of Interprofessional Education (CAIPE, 2021), IPE involves “educators and learners from two or more health professions and their foundational disciplines, who jointly create and foster a collaborative learning environment.”
• The Interprofessional Education for Collaborative Patient-Centred Practice (Wener et al., 2009) defines IPE as “learning together to promote collaboration” and further depicts three components in IPE: socialising healthcare professionals working together, developing mutual understanding and respect for various disciplines and imparting collaborative practice competencies.
• The Canadian Interprofessional Health Collaborative (CIHC, 2010) defines IPE as “occurring when students learn with, from and about one another” adding that IPE takes place when “healthcare professionals learn collaboratively within and across disciplines to acquire knowledge, skills and values needed for working in teams” (CIHC, 2010).
In 2009, six health professions from educational associations (osteopathic and allopathic medicine, nursing, pharmacy dentistry, and public health) in the United States created a collaborative to promote IPE learning interventions and established a document disclosing the core competencies for collaborative practice. This document, known as the Interprofessional Education Collaborative (IPEC) report (IPEC, 2011, 2016), aims to prepare the future healthcare workforce for enhanced team-based patient care. Over time, the IPEC report has gained worldwide acceptance as a core document to guide curriculum design within healthcare teaching.
The IPEC report sets four different dimensions of expert panel recommendations on interprofessional core competencies, which are aligned with the WHO statements: (1) ethics and values, (2) roles and responsibilities, (3) interprofessional communication, and (4) teamwork. This report provides a framework for high-quality, integrated patient care within each country’s healthcare system.
Although the abovementioned definitions have overlapping terminologies and include aspects of interprofessionality, collaboration, shared values, and socialisation, an apparent uniformity of the definition of IPE is lacking, which might contribute to the misunderstanding of IPE. The correct understanding of the concept of IPE has implications for the adequate implementation of IPE activities in healthcare personnel formation curricula and may affect students’ attitudes toward collaborative practice (Khalili et al., 2013). Therefore, the determination of a clear operational definition of IPE is the base for developing a more effective IPE design, delivery, and measurement.
This study aims to determine the characteristics and attributes of the definition of IPE and to distinguish between the defining and incorrect attributes of IPE in a medical student population. Moreover, we aim to develop a conceptual framework of IPE in a microcontext and determine the weight of each component of the IPE definition.
The participants gave written informed consent to the interviews and the Bern Cantonal Ethics Committee (Req-2019-00743, 23.08.2019) waived the need for ethics approval. We used ID numbers to code students and requested no identifying data. All procedures from this investigation followed the Helsinki Declaration. This study was registered with the number ISRCTN41715934, first registration 12/12/2019.
The Medical Faculty of the University of Bern in Switzerland offers a 6-year curriculum of studying human medicine and features a 2-day optional rotation in interprofessional care. All medical students actively enrolled in the Faculty of Medicine of the University of Bern, Switzerland, during the academic year 2019/2020 were eligible for inclusion in the study (N = 2,089 students).
We performed a qualitative methodology approach to promote the comprehensiveness, understanding and validity of a proposed framework on the concept of IPE (Figure 1). Our framework was developed using the conceptual framework analysis technique from Miles et al. (2014). He defined a conceptual framework as “a visual or written product that explains, either graphically or in narrative form, the main objectives to be studied and the presumed relationships among them” (Miles et al., 2014). At the heart of this methodology lies an interpretative approach to social reality, offering understanding of the concept, instead of establishing causal relationships intended to provide outcomes.
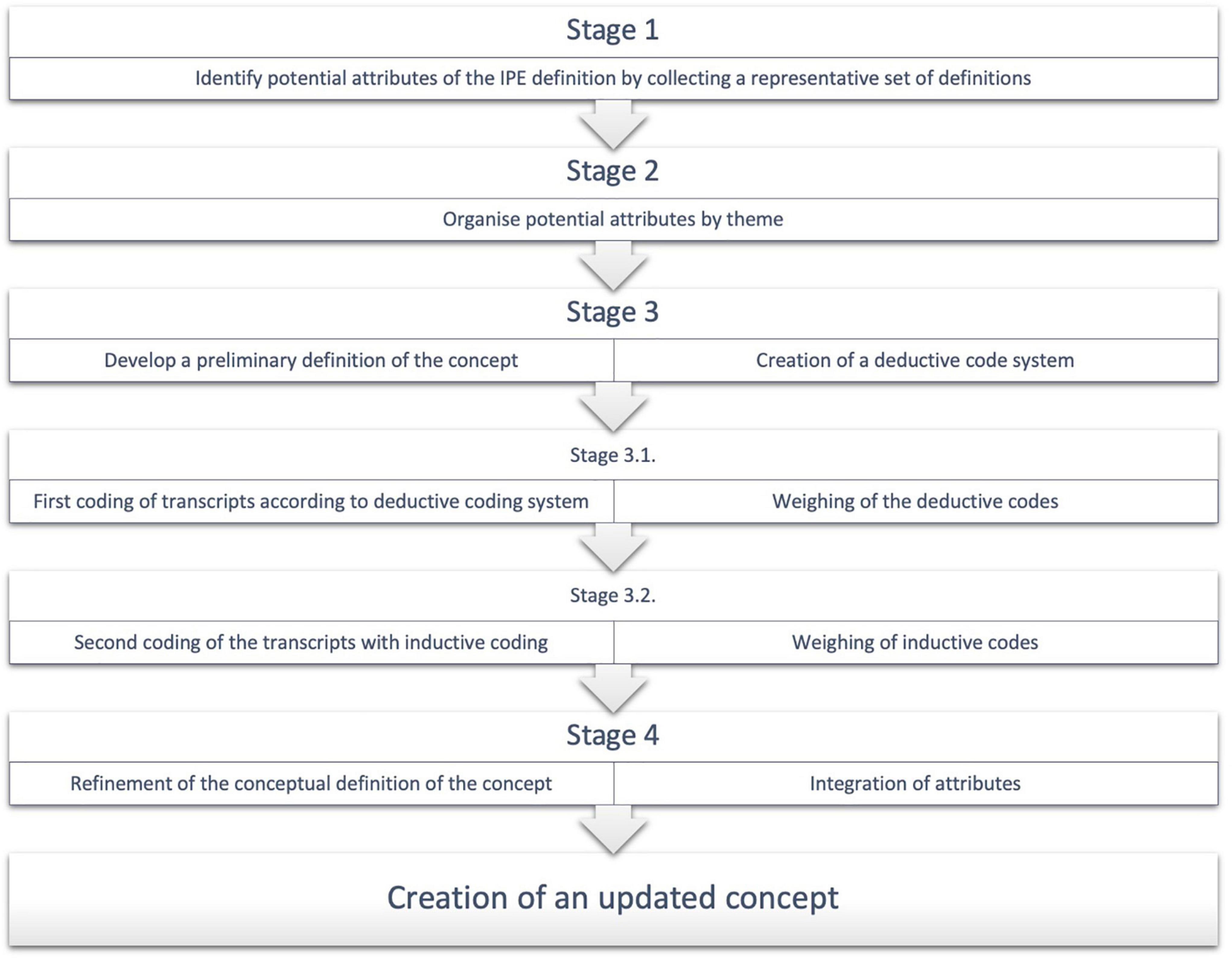
Figure 1. Study flowchart. Stepwise approach to the creation of an updated concept. IPE, interprofessional education.
This is a secondary qualitative analysis of a mixed-methods quantitative-qualitative design study based on a sequential explanatory model (Berger-Estilita et al., 2020a). Six hundred and eighty-three medical students from all 6 years of medical studies at the University of Bern, Switzerland replied to an online survey about attitudes toward interprofessional learning using a validated interprofessional attitudes scale (Pedersen et al., 2020). After completion of the online survey, students could tick a box signalling their availability to participate in semi-structured group interviews. Agreeing students were contacted to take part in nine semi-structured 1-h interviews, according to their availability. Thirty-one medical students took part, which focussed on their experience in interprofessional learning and the possible impact such learning might have on their own professional development. Students were asked about their characteristics (e.g., age, year of studies) and their understanding of IPE, according to a previously defined interview guide. The sessions were audio-recorded. HC transcribed it in intelligent verbatim format, and JB-E verified the transcripts’ accuracy. The summaries of each interview were sent to all participants for content verification and approval (member-checking) (Morse, 2015). Further details of the methodology can be found elsewhere (Berger-Estilita et al., 2020a).
We used data from the semi-structured interviews to investigate medical students’ perceptions of the definition of IPE. The interviewers (JB-E and HC) acted solely as facilitators, encouraging contributions from all participants and validating different views. The study was conducted in German. The analysis presented in this paper is an independent, post-hoc sub-study of the published group interview dataset (Berger-Estilita et al., 2020a).
All interviews took place at the Department of Anaesthesiology and Pain Therapy, Inselspital, Bern, Switzerland in November 2019.
We used a known protocol (Castillo-Montoya, 2016) to develop a semi-structured interview guide (Supplementary Data Sheet 1). We first ensured that interview questions were aligned with our research questions; we then constructed an inquiry-based conversation; we asked for external feedback on interview protocols; and we piloted the interview guide amongst peers. The question route was developed to explore in-depth knowledge of the concept of IPE, its advantages and disadvantages, and the optimal time for introducing IPE in the medical curriculum.
Before transcript analysis, HC and JB-E deductively created a basic category system based on the existing definitions on IPE using the Podsakoff recommendations (Podsakoff et al., 2016). First, we identified all attributes from the abovementioned five representative definitions of IPE. Then, we organized those attributes by themes and sorted them in a hierarchy of increasingly complex attributes, where each attribute subsumes elements of the preceding lower level. Thus, conceptions in the category of attributes can include elements of the level below (Figure 2). We determined three levels, according to the increased complexity of the concept:
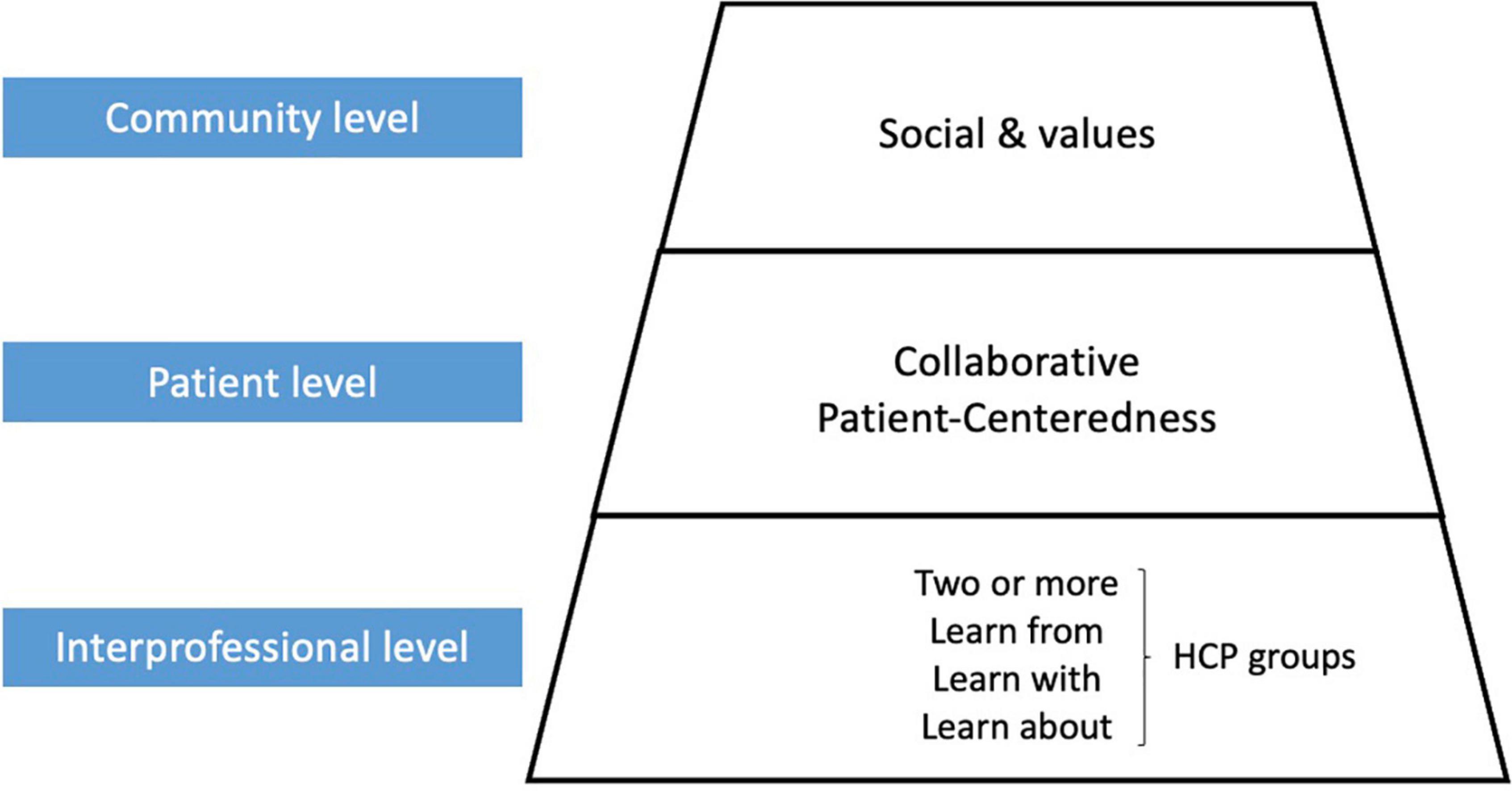
Figure 2. Three-level interprofessional education (IPE) framework. Deductively created three-level IPE framework, according to an increased concept complexity. HCP, healthcare professionals.
• Level One—“Interprofessional”: attributes related to work with individuals of other professions.
• Level Two—“Teamwork”: attributes related to knowledge of different roles, related to communication with patients, families and other health care professionals in a responsible manner, to attributes supporting a team approach and to building team dynamics, and related to patient-centred care.
• Level Three—“Societal”: attributes related to working to maintain a climate of mutual respect, shared values/ethics and social interactions.
Finally, we developed a preliminary version of the concept and used this category system to code all nine interviews with the MaxQDA2020 version 18.2.0 software (Verbi, Berlin, Germany).
Two different researchers (HC, JB-E) independently coded the interviews. Difficulties and inaccuracies were noted and were discussed in consensus before deciding on the final coding system. Ambiguities and redundancies were discussed and eliminated by consensus or by consulting a third author (RG). We updated this deductively created coding system with the notes and memos generated during the transcription process (parallel memoing). This process was performed in a phased fashion. After coding three interviews independently, HC and JB-E verified agreement of the coding distribution and checked for saturation, before proceeding with the following three interviews.
The fourth stage of the Podsakoff et al. (2016) recommendations included a refinement of the conceptual definition by adding attributes explored by inductive coding. To comply with this step, JB-E, HC, and SM re-analysed transcripts using inductive thematic coding, which involved iteratively reading and rereading the data, grouping extracts into common themes and naming concepts. This coding ensured that the data generated were grounded in, or emergent from, the narratives of the interview participants. Data was processed according to the Miles et al. (2014) framework for conceptual data analysis. This included first data reduction—including segmenting, editing and summarising the data—followed by data display, and finally conclusion verification. We also performed a qualitative “concept analysis” study according to Walker and Avant’s methodology (Walker and Avant, 2005). We first determined a “standard” and “contrary” model of IPE according to Olenick et al.’s (2010) concept. We defined “standard” IPE activities as those describing groups of different professions’ students participating in a learning activity where they collaborated in decision-making and developed plans of care, with a patient-centred focus. A “contrary” IPE activity would be any activity where, despite having participants from different professions, little or no evidence of collaboration or shared decision-making would be mentioned. We searched for examples of both models in the interviews. Additionally, we extracted code frequencies. During analysis, conceptual saturation was confirmed by the non-emergence of new codes or themes (Braun and Clarke, 2006). Relevant interview excerpts were selected to represent participants’ perceptions relevant to the themes and explanations being constructed. We used a functionalist approach of creating equivalent translation structures (Resch and Enzenhofer, 2018) to translate direct quotations from the interviews into English. HC and SM (German-speaking) translated the citations from German to English with Google Translate. SeM (English-native speaker) performed changes to ensure that the reader could understand the target text.
We interviewed students from all study years [Year 1: n = 5 (16%), Year 2: n = 8 (26%), Year 3: n = 2 (7%), Year 4: n = 8 (26%), Year 5: n = 7 (23%), Year 6: n = 1 (3%)]. There were 20 female students (64.5%). All 31 students mentioned previous interprofessional experiences (i.e., an IV cannulation workshop, a confidentiality seminar, nursing and clinical clerkships) during their studies, but only 6 (19%) took the optional 2-day rotation in interprofessional care.
Three main categories emerged from the semi-structured interviews: (1) attributes of IPE according to the three-level framework, (2) attributes of IPE according to the four dimensions of the IPEC report, (3) further attributes.
Students were aware of the intended meaning of IPE, as per WHO definition (2010). This description has been published elsewhere (Berger-Estilita et al., 2020a). The frequency and coverage of deductive codes according to the three-level framework is summarized in Table 1. Results stratified by year of studies can be found in Supplementary Table 1.
After being questioned, students could spontaneously give attributes of IPE concerning the four core competencies of the IPEC (2011) report.
Participants underlined that IPE promoted mutual understanding and shared mental models, facilitating future interprofessional relationships. IPE is able to break down barriers and reduce prejudices. When learning together, participants accept that other healthcare professionals perform some skills better, and this fosters mutual respect and trust. Students mentioned that IPE enhances patient-centred care: by leading to greater work efficiency and potentiating a more positive working environment, patients may feel that healthcare professionals listen more attentively and have a more accurate overview of their problems.
Students mentioned that IPE improves the extent of knowledge of other healthcare students’ roles, skills and abilities, and optimises cooperation while reducing misunderstandings. IPE makes one have a different perspective and be sensitive to how other healthcare professionals judge a situation. This clarifies the practical relevance of their work.
(…) one understands better what the different professional groups know and can do, which leads to fewer misunderstandings in everyday hospital life (Student 4, Interview 6).
Interprofessional education benefits communication between healthcare students regardless of the course content. Communication promotes shared mental models, and can facilitate future interprofessional relationships and a smoother settling into clinical practice. Good communication benefits collaboration and leads to better patient care. It also embodies a patient-centred approach, with multi-way communication between the patient, nurse and doctor. All this increases satisfaction in the workplace.
The tendency is that you gain more communicative skills and have a more respectful attitude [towards others] (Student 1, Interview 1).
Being conscious of what the other healthcare professions students learn leads to better cooperation and improves teamwork. IPE-experienced physicians will have a broader knowledge of available possibilities and delegate when appropriate, showing better attitudes toward collaboration. IPE reduces the effort to make teamwork efficient (facilitating interaction in hand-overs or rounds). This leads to easier integration in the workplace, enhances in-hospital social connections, and increases employee satisfaction.
[IPE leads to] efficiency. If you feel comfortable, the patients do too. It is also good that they see that working together works. Nothing is worse than everyone arguing around you (Student 4, Interview 3).
Interprofessional education can mimic a natural work environment, and students will learn clinically-relevant participants and problem-solving, making learning more motivating and purposeful. IPE also teaches how to behave in a professional context.
Cultivating interprofessionality leads to more organised and efficient teamwork and a better working atmosphere. This improves patient safety (teams make fewer mistakes) and employee well-being. More satisfied employees are less inclined to leave for other institutions. Students noted that this combination of a more stable workforce and increased productivity would lead to financial benefits (Table 2).
If nurses, doctors, physiotherapists and others involved in patient management (including secretaries) can work well together, there is a good working atmosphere. Therefore, people stay in the hospital. They are loyal to the employer (…). That saves money (Student 2, Interview 6).
We created 16 additional codes inductively, covering concepts not previously integrated into the definitions. Code frequency for the inductive codes is summarised in Table 3.
“Communication” was the most frequent inductive code, and students found it to have a central role in IPE. If health professionals are not forced to communicate, then they remain siloed. Communication between different health professionals is the starting point for exchanging ideas and coordinating teams. Many students argued that interprofessional learning should notably include communication skills. Students also related “communication” to higher attributes of IPE. They mentioned that improved communication between healthcare professionals might lead to more satisfied team members, working with less friction, and reducing the time and energy spent on overcoming issues arising from lack of communication.
“Role recognition” was the second most frequent inductive code. Students valued the understanding of different healthcare professionals’ competencies in interprofessional learning. Such role recognition facilitates task distribution by correctly assessing what each professional group can do and marks out the limits of each profession, suiting mutual expectations. Students mentioned that recognizing roles leads to the empowerment of each profession and enables better team performance and task completion.
We also frequently coded segments with “Preparation for practice.” Interprofessional learning seems more relevant for medical students in clinical settings, where role attribution is commonly applied. “Preparation for practice” was meant to promote early sensitisation to teamwork and facilitate future workplace interactions and skills, smoothing the transition into clinical practice. As higher interprofessional learning components, students mentioned the possibility of early networking, avoiding prejudices, and fostering horizontal leadership strategies.
Students gave 96 examples of IPE activities. Thirty-two examples (33%) corresponded to IPE model cases (i.e., including patient-centeredness and collaboration) and 64 (67%) to contrary cases.
A conceptual framework for IPE definition derived from the above results is presented in Figure 3.
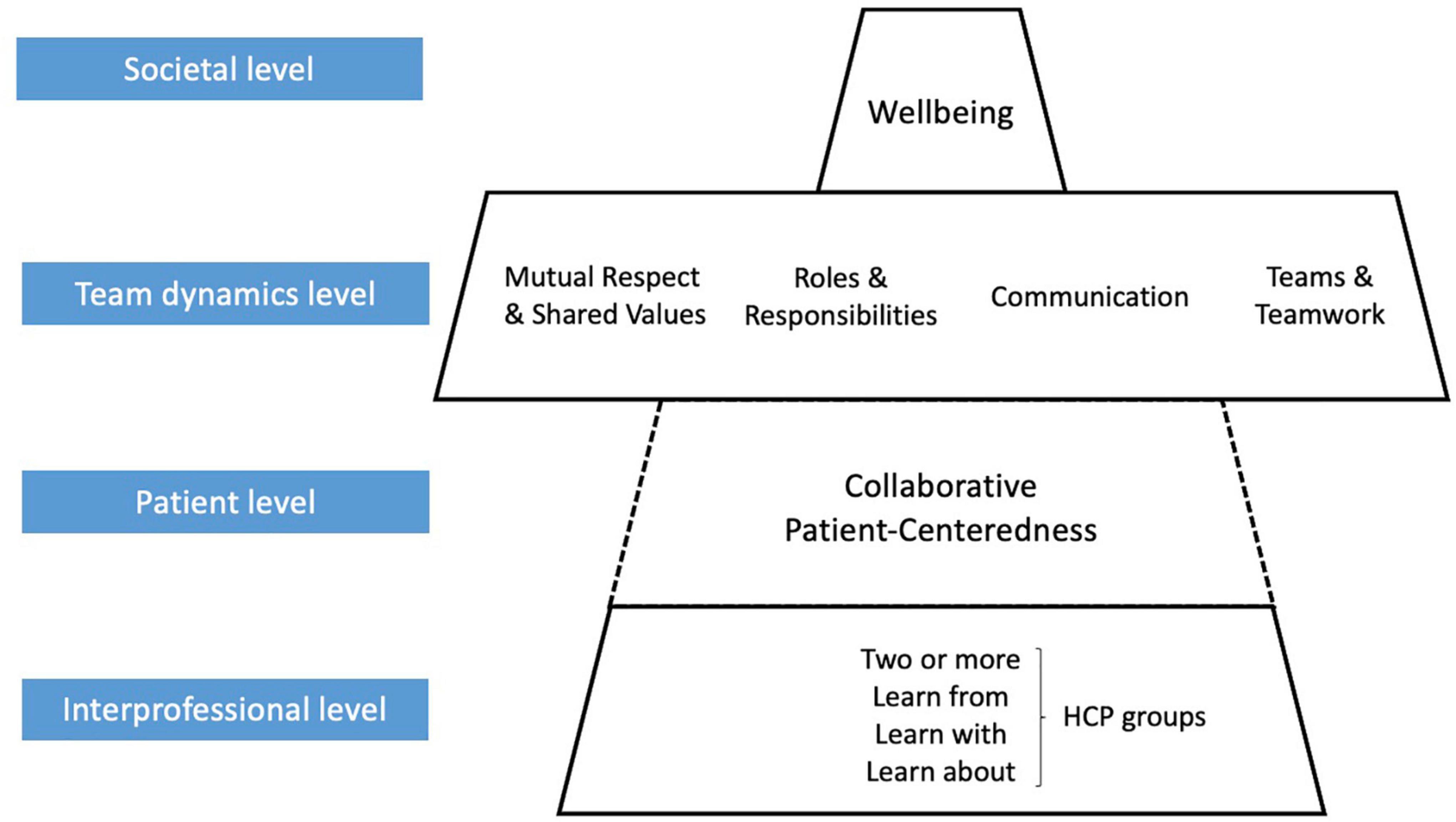
Figure 3. Final conceptual framework (“the IPE Pagoda”). Updated conceptual framework on IPE, “the IPE Pagoda.” HCP, healthcare professionals.
We determined four levels, according to the increased complexity of the concept:
• Level One—Interprofessional: as previously.
• Level Two—Patient: attributes related to role attribution of different team players, a collaboration between other healthcare professionals with the patient at the centre of care.
• Level Three—Team dynamics: attributes related to optimal teamwork, improved communication, work ethics and respectful interaction between team members (Weller et al., 2014; Rosen et al., 2018).
• Level Four—Societal (broader education outcomes): attributes related to relationships with other professions outside the work environment to improve well-being, patient care and advance learning.
• The framework structure loosely resembles a Japanese temple; therefore, it was called the “IPE pagoda.”
This qualitative study demonstrates that medical students at a university that offers one interprofessional internship could identify all the concepts present in international definitions of IPE. However, we verified that students gave different weights to different attributes. Additionally, two-thirds of medical students mentioned a “contrary” model (without collaboration or patient-centeredness) as IPE activities. These results both support and build on recent definitions of IPE. The additional themes identified in this study expand on previous literature on this topic (Wener et al., 2009; WHO, 2010; IPEC, 2011, 2016; CAIPE, 2021). This is important because it demonstrates that IPE plays a more expansive role in pre-licensure students’ medical education than previously thought (Hudson et al., 2016; Berger-Estilita et al., 2020b). Further, this is the first study in available IPE literature to confirm the four major principles of IPE as outlined by the IPEC report.
When asked, medical students could collectively name attributes of the IPEC dimensions and name other attributions outside the constructs above. We were positively surprised by these findings, as previous studies show that healthcare students may demonstrate professional socialisation (i.e., feeling and behaving like a member of that profession), which may lead to misconceptions and “tribalism” between professions (Beatie, 1995), leading to ineffective working and ultimately patient harm (Hawkes et al., 2013). We hypothesise that because medical students at Bern University have IPE in the first year of studies, they develop their professional identity parallel with other healthcare students. Such an early introduction of IPE may force medical students to contact and perceive other H as having the same basic knowledge, which will tackle lower levels of prejudice, permitting the development of better attitudes toward collaboration and mutual respect (Hawkes et al., 2013). Our findings corroborated this.
We were surprised to observe that “learning about” other HCP groups was more expressive than “learning from” or “learning with.” The emphasis on “learning about” likely reflects a lack of knowledge about other healthcare professions. This might be a consequence of the traditional “siloed” education of medical professions, which often leads to first exposure to IPE only in later stages of the training (Berger-Estilita et al., 2020a,b). Additionally, two-thirds of medical students mentioned a “contrary” model as IPE. While our sample stems from a medical programme with IPE already embedded in the curriculum, the current IPE offer might still be insufficient.
Patient-centeredness was mentioned in only one-fifth of the coded cites. Three core themes seem to emerge in different definitions of patient-centeredness (Hearn et al., 2019): patient participation and involvement, the relationship between the patient and the HCP, and the context in which health care is delivered. Patient-centredness is increasingly prioritised across medical schools and practice, but it is challenging to teach (Parent et al., 2016). Students expressed several concerns regarding this type of teaching, particularly knowing how to adequately present information to patients, being exposed to patients’ enquiries or “pimping” (Cox et al., 2011). IPE might still be underrepresented in the medical curriculum of the University of Bern, as most teaching is “disease-centred,” which reduces most probable awareness of the “patient-centred” style (Krupat et al., 1999). Our results suggest that medical students at the University of Bern have not yet fully evolved beyond the physician’s role as expert HCP and collaborator into more differentiated Canadian Medical Education Directives for Specialists (CanMEDS) competencies as advocate and manager (Frank et al., 2015). We hypothesise that as medical students become more comfortable with their role as medical experts, they can glean different impressions from clinical encounters and develop their other intrinsic functions, as recommended in the Principal Relevant Objectives and Framework for Integrative Learning and Education in Switzerland (Michaud and Jucker-Kupper, 2017). Alternatively, it may be that in their clinical training, they are forced to address the roles of other HCPs and thus broaden their view of interprofessionality. This is in alignment with other studies, that if students are allowed to work as part of a team, they can develop a more precise insight into a patient-centred approach (Scavenius et al., 2006). While such issues will need to be addressed in further studies, it seems reasonable to recommend that if medical students show little awareness of patient-centeredness, they should be more exposed to interprofessional activities during their training (Krupat et al., 1999).
The social component of IPE was often mentioned. Students considered networking beneficial, both inside and outside the workplace. By engaging in interprofessional relationships, students learn about each other’s curricula in informal settings and foster friendships. This aspect of IPE is not frequently explored in the literature. The social element repeatedly mentioned in the interviews mirrors the Social Learning Theory (Bandura, 1986). Learning is also a social and relational process, frequently occurring around authentic and meaningful patient treatment (Friman et al., 2017). These findings support that “formal” or planned educational IPE experiences also create “informal” opportunities to socialise and be acquainted on a personal level. Therefore, these “informal arenas can stimulate and set a solid basis for interprofessional collaboration” (Reeves, 2000).
Finally, we propose to add “well-being” as a possible dimension of IPE. Well-being is “a dynamic state that refers to individuals’ ability to develop their potential, work productively and creatively, build strong and positive relationships with others, and contribute to their community” (Beddington et al., 2008). This definition is deeply related to the previous concepts of interprofessionality. Interprofessional studies show that negative interprofessional interactions between nurses and physicians increase the likelihood of nurse burnout and may be a critical factor in decreasing nurse well-being, increasing turnover, and worsening patient outcomes (Sinclair et al., 2015; Dow et al., 2019). However, well-being research on physicians and medical students is less established. Dow et al. (2019) argued that using an interprofessional approach may aid in identifying factors and establishing interventions to support the well-being of different professions better. These recommendations closely align with our findings.
Our findings underline several considerations that educators may include when considering interprofessional activities, particularly the importance of considering all levels of interprofessionality and having clear objectives for each level. Our interprofessional learning framework brings oversight to what appears to be a longitudinal process underscored by its use to improve patient outcomes, team dynamics between professionals, and individual and collective well-being. More attention must be paid to the learning environment of IPE activities to facilitate open, frank, and effective interactions.
Our study has limitations. There was a potential for selection bias as students were recruited voluntarily. In addition, the basic themes for the construction of this framework were provided only by medical students. The authors are aware that the reported findings may not represent other cohorts of medical students in Switzerland or elsewhere, as well as students from other healthcare professions. Therefore, great care must be taken in generalisations. We acknowledge that our findings might have been richer if we had also included clinicians, educators or students of other healthcare professions. This can be taken up in future studies.
Moreover, group interviews may also have introduced social desirability bias and the potential for recall bias. Finally, from the methodological perspective, we used a modified version of the original model-contrary case concept proposed by Olenick et al. (2010). By only using the model and the contrary cases, we might have used very high standards to classify medical students’ experiences with IPE, leading to a high percentage of examples rated “contrary case.”
The impact of this study is two-fold. Firstly, we deepened the understanding of previously identified definitions of IPE, and we identified new attributes of the definition. Secondly, by considering “well-being” as a component of interprofessionality, curriculum planners may offer more objective and authentic interprofessional experiences.
The original contributions presented in this study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
The studies involving human participants were reviewed and approved by the Bern Cantonal Ethics Committee (Req-2019-00743, 23.08.2019). The patients/participants provided their written informed consent to participate in this study.
JB-E and RG contributed to the study design. HC, SM, and JB-E performed the quality analysis. RG, AF, and SG critically reviewed the manuscript. All authors contributed to interpretation of the results and important intellectual content to the manuscript and approved the final version.
This manuscript’s publication charges were supported by a grant from the Suzanne and Hans Biäsch Foundation for Applied Psychology (Nr. 2020-23). The funders had no role in study design, data collection and analysis, decision to publish, or manuscript preparation.
We thank the Dean’s office of the Medical Faculty of the University of Bern, particularly Peter Frey, MME, to facilitate students’ contacts at the University of Bern. We also thank all the medical faculty students who participated in this study. Finally, we thank Sean McAleer (SeM) for verifying the translations of the cites for readability.
JB-E was an associate editor for BMC Medical Education. RG was the Board Director of Guidelines and ILCOR of the European Resuscitation Council, the Task Force Chair Education, Implementation, and Team of ILCOR, and member of the direction of the MME Programme of the University of Bern. SG was also a member of the direction of the MME Programme of the University of Bern.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/feduc.2022.978796/full#supplementary-material
Supplementary Data Sheet 1 | Interview guide.
Anderson, E. S., and Thorpe, L. N. (2008). Early interprofessional interactions: does student age matter? J. Interprof. Care 22, 263–282. doi: 10.1080/13561820802054689
Bandali, K., Niblett, B., Yeung, T. P., and Gamble, P. (2011). Beyond curriculum: embedding interprofessional collaboration into academic culture. J. Interprof. Care 25, 75–76. doi: 10.3109/13561820.2010.503948
Bandura, A. (1986). Social Foundations of Thought and Action: a Social Cognitive Theory. Englewood Cliffs, NJ: Prentice-Hall.
Beatie, A. (1995). “War and Peace among the Health Tribes,” in Interprofessional Relations in Health Care, eds K. Soothill, I. Mackay, and C. Webb (London: Edward Arnold), 11–30.
Beddington, J., Cooper, C. L., Field, J., Goswami, U., Huppert, F. A., Jenkins, R., et al. (2008). The mental wealth of nations. Nature 455, 1057–1060.
Berger-Estilita, J., Chiang, H., Stricker, D., Fuchs, A., Greif, R., and McAleer, S. (2020a). Attitudes of medical students towards interprofessional education: a mixed-methods study. PLoS One 15:e0240835. doi: 10.1371/journal.pone.0240835
Berger-Estilita, J., Fuchs, A., Hahn, M., Chiang, H., and Greif, R. (2020b). Attitudes towards Interprofessional education in the medical curriculum: a systematic review of the literature. BMC Med. Educ. 20:254. doi: 10.1186/s12909-020-02176-4
Braun, V., and Clarke, V. (2006). Using thematic analysis in psychology. Qual. Res. Psychol. 3, 77–101.
CAIPE (2021). The Centre for the Advancement of Interprofessional Education. Available online at: www.caipe.org.uk (accessed January 15, 2022).
Castillo-Montoya, M. (2016). Preparing for interview research: the interview protocol refinement framework. Qual. Rep. 21, 811–831.
Chua, A. Z., Lo, D. Y., Ho, W. H., Koh, Y. Q., Lim, D. S., Tam, J. K., et al. (2015). The effectiveness of a shared conference experience in improving undergraduate medical and nursing students’ attitudes towards inter-professional education in an Asian country: a before and after study. BMC Med. Educ. 15, 233–242. doi: 10.1186/s12909-015-0509-9
CIHC (2010). A national Interprofessional competency framework. Available online at: https://phabc.org/wpcontent/uploads/2015/07/CIHC-National-Interprofessional-Competency-Framework.pdf (accessed January 15, 2022).
Cooper, H., Spencer-Dawe, E., and McLean, E. (2005). Beginning the process of teamwork: design, implementation and evaluation of an inter-professional education intervention for first year undergraduate students. J. Interprof. Care 19, 492–508. doi: 10.1080/13561820500215160
Coster, S., Norman, I., Murrells, T., Kitchen, S., Meerabeau, E., Sooboodoo, E., et al. (2008). Interprofessional attitudes amongst undergraduate students in the health professions: a longitudinal questionnaire survey. Int. J. Nurs. Stud. 45, 1667–1681. doi: 10.1016/j.ijnurstu.2008.02.008
Cox, E. D., Schumacher, J. B., Young, H. N., Evans, M. D., Moreno, M. A., and Sigrest, T. D. (2011). Medical student outcomes after family-centered bedside rounds. Acad. Pediatr. 11, 403–408. doi: 10.1016/j.acap.2011.01.001
de Oliveira, V. F., Bittencourt, M. F., Navarro Pinto, ÍF., Lucchetti, A. L. G., and Lucchetti, G. (2018). Comparison of the Readiness for Interprofessional Learning and the rate of contact among students from nine different healthcare courses. Nurse Educ. Today 63, 64–68. doi: 10.1016/j.nedt.2018.01.013
Dow, A. W., Baernholdt, M., Santen, S. A., Baker, K., and Sessler, C. N. (2019). Practitioner wellbeing as an interprofessional imperative. J. Interprof. Care 33, 603–607. doi: 10.1080/13561820.2019.1673705
Frank, J. R., Snell, L., and Sherbino, J. (2015). CanMEDS 2015 Physician Competency Framework. Ottawa: Royal College of Physicians and Surgeons of Canada.
Friman, A., Wiegleb Edstrom, D., and Edelbring, S. (2017). Attitudes and perceptions from nursing and medical students towards the other profession in relation to wound care. J. Interprof. Care 31, 620–627. doi: 10.1080/13561820.2017.1336991
Hawkes, G., Nunney, I., and Lindqvist, S. (2013). Caring for attitudes as a means of caring for patients–improving medical, pharmacy and nursing students’ attitudes to each other’s professions by engaging them in interprofessional learning. Med. Teach. 35, e1302–e1308. doi: 10.3109/0142159X.2013.770129
Hearn, J., Dewji, M., Stocker, C., and Simons, G. (2019). Patient-centered medical education: A proposed definition. Med. Teach. 41, 934–938. doi: 10.1080/0142159X.2019.1597258
Hudson, J. N., Lethbridge, A., Vella, S., and Caputi, P. (2016). Decline in medical students’ attitudes to interprofessional learning and patient-centredness. Med. Educ. 50, 550–559. doi: 10.1111/medu.12958
IPEC (2011). Core Competencies for Interprofessional Education: Report of an Expert Panel. Washington, DC: IPE Collaborative.
IPEC (2016). Core competencies for interprofessional collaborative practice: 2016 update. Washington, DC: IPE Collaborative.
Khalili, H., Orchard, C., Laschinger, H. K., and Farah, R. (2013). An interprofessional socialization framework for developing an interprofessional identity among health professions students. J. Interprof. Care 27, 448–453. doi: 10.3109/13561820.2013.804042
Kozmenko, V., Bye, E. J., Simanton, E., Lindemann, J., and Schellpfeffer, S. E. (2017). The optimal time to institute interprofessional education in the Medical School Curriculum. Med. Sci. Educ. 27, 259–266.
Krupat, E., Hiam, C. M., Fleming, M. Z., and Freeman, P. (1999). Patient-centeredness and its correlates among first year medical students. Int. J. Psychiatry Med. 29, 347–356. doi: 10.2190/DVCQ-4LC8-NT7H-KE0L
Lapkin, S., Levett-Jones, T., and Gilligan, C. (2013). A systematic review of the effectiveness of interprofessional education in health professional programs. Nurse Educ. Today 33, 90–102. doi: 10.1016/j.nedt.2011.11.006
Luderer, C., Donat, M., Baum, U., Kirsten, A., Jahn, P., and Stoevesandt, D. (2017). Measuring attitudes towards interprofessional learning. Testing two German versions of the tool “Readiness for Interprofessional Learning Scale” on interprofessional students of health and nursing sciences and of human medicine. GMS J. Med. Educ. 34, 33–46. doi: 10.3205/zma001110
McFadyen, A. K., Webster, V. S., Maclaren, W. M., and O’Neill, M. A. (2010). Interprofessional attitudes and perceptions: results from a longitudinal controlled trial of pre-registration health and social care students in Scotland. J. Interprof. Care 24, 549–564. doi: 10.3109/13561820903520369
Michaud, P., and Jucker-Kupper, P. (2017). PROFILES; principal objectives and framework for integrated learning and education in Switzerland. Bern: Joint Commission of the Swiss Medical Schools.
Miles, M., Huberman, A. M., and Saldana, J. (2014). Qualitative Data Analysis. Los Angeles, CA: SAGE.
Morse, J. M. (2015). Critical analysis of strategies for determining rigor in qualitative inquiry. Qual. Health Res. 25, 1212–1222. doi: 10.1177/1049732315588501
Olenick, M., Allen, L. R., and Smego, R. A. Jr. (2010). Interprofessional education: a concept analysis. Adv. Med. Educ. Pract. 1, 75–84. doi: 10.2147/AMEP.S13207
Parent, K., Jones, K., Phillips, L., Stojan, J. N., and House, J. B. (2016). Teaching patient- and family-centered care: integrating shared humanity into medical education curricula. AMA J. Ethics 18, 24–32. doi: 10.1001/journalofethics.2016.18.1.medu1-1601
Pedersen, T. H., Cignacco, E., Meuli, J., Habermann, F., Berger-Estilita, J., and Greif, R. (2020). The German interprofessional attitudes scale: translation, cultural adaptation, and validation. GMS J. Med. Educ. 37:Doc32. doi: 10.3205/zma001325
Podsakoff, P. M., MacKenzie, S. B., and Podsakoff, N. P. (2016). Recommendations for creating better concept definitions in the organizational, behavioral, and social sciences. Organ. Res. Methods 19, 159–203. doi: 10.1016/j.jsxm.2019.07.025
Reeves, S., Fletcher, S., Barr, H., Birch, I., Boet, S., Davies, N., et al. (2016). A BEME systematic review of the effects of interprofessional education: BEME Guide No. 39. Med. Teach. 38, 656–668. doi: 10.3109/0142159X.2016.1173663
Reeves, T. (2000). Alternative approaches for online learning environments in higher education. J. Educ. Comput. Res. 23, 101–111.
Resch, K., and Enzenhofer, E. (2018). The Sage handbook of qualitative data collection. Los Angeles, CA: SAGE.
Rosen, M. A., DiazGranados, D., Dietz, A. S., Benishek, L. E., Thompson, D., Pronovost, P. J., et al. (2018). Teamwork in healthcare: key discoveries enabling safer, high-quality care. Am. Psychol. 73:433. doi: 10.1037/amp0000298
Ruebling, I., Pole, D., Breitbach, A. P., Frager, A., Kettenbach, G., Westhus, N., et al. (2014). A comparison of student attitudes and perceptions before and after an introductory interprofessional education experience. J. Interprof. Care 28, 23–27. doi: 10.3109/13561820.2013.829421
Scavenius, M., Schmidt, S., and Klazinga, N. (2006). Genesis of the professional-patient relationship in early practical experience: qualitative and quantitative study. Med. Educ. 40, 1037–1044. doi: 10.1111/j.1365-2929.2006.02594.x
Sinclair, R. R., Sliter, M., Mohr, C. D., Sears, L. E., Deese, M. N., Wright, R. R., et al. (2015). Bad versus good, what matters more on the treatment floor? Relationships of positive and negative events with nurses’. burnout and engagement. Res. Nurs. Health 38, 475–491. doi: 10.1002/nur.21696
Visser, C. L. F., Ket, J. C. F., Croiset, G., and Kusurkar, R. A. (2017). Perceptions of residents, medical and nursing students about Interprofessional education: a systematic review of the quantitative and qualitative literature. BMC Med. Educ. 17:77–96. doi: 10.1186/s12909-017-0909-0
Walker, L. O., and Avant, K. C. (2005). Strategies for theory construction in nursing. Upper Saddle River, NJ: Pearson/Prentice Hall.
Weller, J., Boyd, M., and Cumin, D. (2014). Teams, tribes and patient safety: overcoming barriers to effective teamwork in healthcare. Postgrad. Med. J. 90, 149–154. doi: 10.1136/postgradmedj-2012-131168
Wener, P., Nelson, M., Fricke, M., MacDonald, L., Anderson, J. E., The Manitoba, et al. (2009). Contributing to the sustainability of Interprofessional Education for Collaborative Patient-Centred Practice (IECPCP): A teaching resource manual. J. Interprof. Care 23, 201–203. doi: 10.1080/13561820802293105
Keywords: interprofessional education, interprofessional learning, healthcare professionals, conceptual framework, qualitative methods
Citation: Berger-Estilita J, Merlo S, Guttormsen S, Fuchs A, Greif R and Chiang H (2022) Pre-licensure medical students’ knowledge and views on interprofessional learning: A qualitative concept analysis based on real-world data. Front. Educ. 7:978796. doi: 10.3389/feduc.2022.978796
Received: 26 June 2022; Accepted: 26 July 2022;
Published: 16 August 2022.
Edited by:
Ana Luísa Rodrigues, University of Lisbon, PortugalReviewed by:
Sebastian Bode, Ulm University Medical Center, GermanyCopyright © 2022 Berger-Estilita, Merlo, Guttormsen, Fuchs, Greif and Chiang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Joana Berger-Estilita, am9hbmFtYmVyZ2VyQGdtYWlsLmNvbQ==
†These authors share last authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.