- 1Department of Family Oral Health, Faculty of Dentistry, Universiti Kebangsaan Malaysia, Kuala Lumpur, Malaysia
- 2Nibong Tebal Dental Clinic, Penang State Health Department, Ministry of Health Malaysia, Penang, Malaysia
- 3Department of Restorative Dentistry, Faculty of Dentistry, Universiti Kebangsaan Malaysia, Kuala Lumpur, Malaysia
The COVID-19 pandemic has significantly affected the training of dental students and the impact can be felt not just by the students, but patients seen at dental school operated clinics. We used the modified-Delphi method to investigate the response from deans of all Malaysian dental schools on the impact of COVID-19, and to solicit their views on policy recommendations to sustain quality dental education during and beyond the infectious disease outbreak. Our analysis revealed that all dental deans are in agreement with strong consensus to 10 out of fifteen items listed to be the challenges they faced due to the COVID-19 pandemic particularly these three items: “Patients under care of students experienced interrupted dental treatment which increases their risk of having their dental and overall wellbeing affected”; “Increased clinical budget for daily operations of Students’ clinics to cater for extra PPE and related expenses,” and; “The Students’ ability to meet clinical requirements for safe and competent practice.” All deans agreed with a strong consensus to the policy statements formulated based on the WHO’s Six Building Blocks to sustain quality dental education. In view of the results, we further discussed the importance of acknowledging that university-led dental clinics as an important part of the national healthcare system. Hence, we proposed that dental education need to have clear policies on having adequate number of trained staff, sufficient funds, information, supplies, transport, communications and overall guidance, and direction to function. Having a National Dental Education Policy that addresses the unique challenges identified in this study will serve as a monumental cornerstone to sustain quality dental education during times of calamity.
Introduction
The COVID-19 pandemic, resulting from severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), has caused widespread infections with extreme consequences. The outbreak received global attention in December 2019 and was recognized as a pandemic of major public health concern by the World Health organization (WHO) on the 11th of March 2020 (WHO, 2020). Sadly, even after more than 2 years and despite the uptake of vaccination in most countries, the pandemic is not yet showing any sign of being contained soon. The appearance of new variants which cause the infected individuals to exhibit a spectrum of diverse reactions and symptoms severity adds to the challenge for policy-makers to optimize the use of resources in mitigating the disease (Boehm et al., 2021; Araf et al., 2022; Mistry et al., 2022).
The main transmission of SARS-CoV-2 virus among individuals is through respiratory droplet and direct contact with the individual with positive COVID-19. Social distancing is almost impossible in dentistry and with high amounts of aerosol generated during dental procedures, dental practitioners are at high risk of contracting or transmitting COVID-19 (Izzetti et al., 2020). There is a high COVID-19 inhalation transmission risk on execution of dental procedures with usage of handpieces, that causes aerosolization of the blood, saliva and bodily secretions (Meng et al., 2020).
Due to COVID-19, universities had adapted their curriculum delivery by moving teaching and learning activities to online platforms (Kerkstra et al., 2022). However, dental schools are not only educational and research institutions but also small hospitals and operational entities with high infrastructural and operational costs. They make an important contribution to the health and wellbeing of the population providing oral health care services. As such, unlike other courses, the dental curriculum requires students to undergo clinical training face to face, and this component of their teaching and learning had been interrupted during the early onset of the pandemic due to the high risk of virus transmission during clinical encounters. During the early phase, it should be noted that that the enhanced clinical protocol for cross infection control was not yet available, and neither was COVID-19 vaccination and self-test kits. Moreover, during the COVID-19 pandemic, series of Movement Control Orders (MCO) were imposed in Malaysia affecting parts or all of the country depending on the severity of the situation. These orders include instructions to close universities or only online teaching and learning were allowed, causing major disruptions to the clinical training (Ross, 2021).
For dental school administrators in Malaysia, it has been necessary to modify some aspects of the cross-infection control protocols and to make adaptations to the guidelines’ recommendations provided by the Ministry of Health (Oral Health Division Ministry of Health Malaysia, 2020a,b) for use at Students’ clinics. This is important so that clinical training of dental students may be resumed albeit conducted in the light of the “new norms.” New norms such as reduced hours each student spends in clinical sessions and low patient attendance due to enhanced clinical protocols, movement control order and fear of dental clinic exposure will have an impact on the clinical competency of graduating dentists because these students will see fewer patients. Many dental schools had to resort to delaying graduation by prolonging the academic semesters to ensure that students are safe and competent to practice. Studying the response of dental school administrators provides decision-makers with an insight on what are the challenges faced by dental schools to sustain quality dental education and to provide safe dental services for the public served by university dental clinics. The aim of this study was to investigate how the COVID-19 pandemic has impacted the Malaysian dental schools, and to solicit the views on policy recommendations to sustain quality dental education during and beyond the infectious disease outbreak from the leaders of the Malaysian dental schools.
Materials and methods
Study design
This is a nation-wide, cross-sectional study involving dental school deans which employed an online modified two-rounds Delphi survey method of data collection (Waggoner et al., 2016; Jünger et al., 2017). We modified the survey by asking the participants to rate their agreement on the pandemic-related issues impacting dental education synthesized from published literatures, instead of making the questions open-ended. We provided space for participants to state any other issues or comments if they had additional concerns.
Sample
There are thirteen dental schools in Malaysia comprising six from the public sector and seven from the private sector. In view of their capacity as leaders of dental schools, we invited all deans to participate in this study.
Study instrument
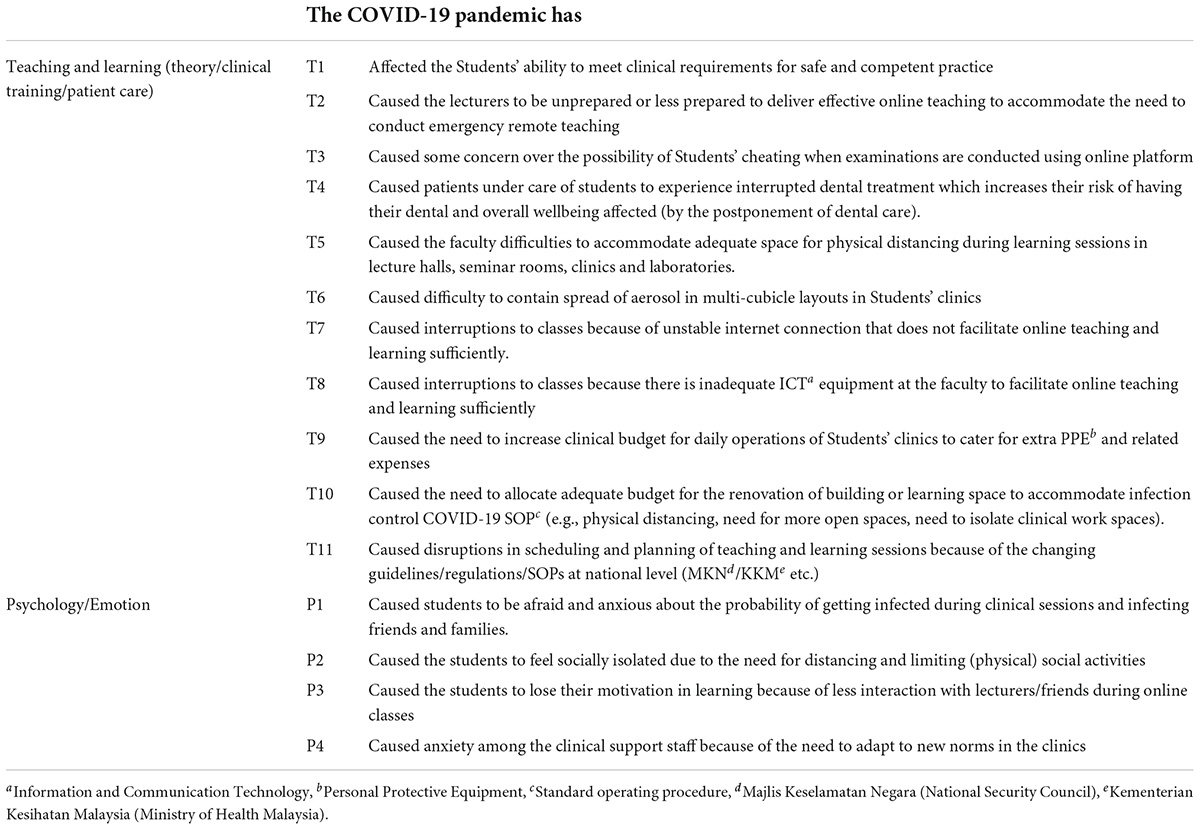
We developed the questionnaire consisting of two parts. Part A (Table 1) consists of statements related to the impacts of the COVID-10 pandemic on various aspects of dental schools. We started the literature search by searching Google Scholar and PubMed using the keywords “dental/dentistry,” “school/university/faculty/academia/students,” and “Corona- virus/Covid-19/Covid19/Sars-cov-2” for articles published up till 30th November 2020. A total of 143 articles was found. For each manuscript, preliminary relevance to the study scope was determined by its title. If the content seemed related to Covid-19 and dental education from the title, we obtained its full reference, including author, year, title, and abstract, for further evaluation.
After initial screening of the titles, a total of 47 studies were deemed relevant and we obtained the full-text article for quality assessment. We included studies that analyzed the impacts and challenges of Covid-19 to dental undergraduate educations. Whereas articles that were not original, study on other viruses or not related to dentistry were excluded. A total of seven studies were excluded after careful review: two were excluded because they did not focus on undergraduate education; three were excluded for the following reasons: not about dental education, a personal opinion and was not Covid-19 related. Overall, forty studies from the initial search were included for extraction of themes to be used in developing the questionnaire.
The final questionnaire used in Part A had a total of fifteen statements related to impacts of COVID-19 on dental education and training in the dental school’s environment. The respondents were required to rank the impact level of each statement based on their opinions on a 5-point Likert scale ranging from “minimal” to “severe.”
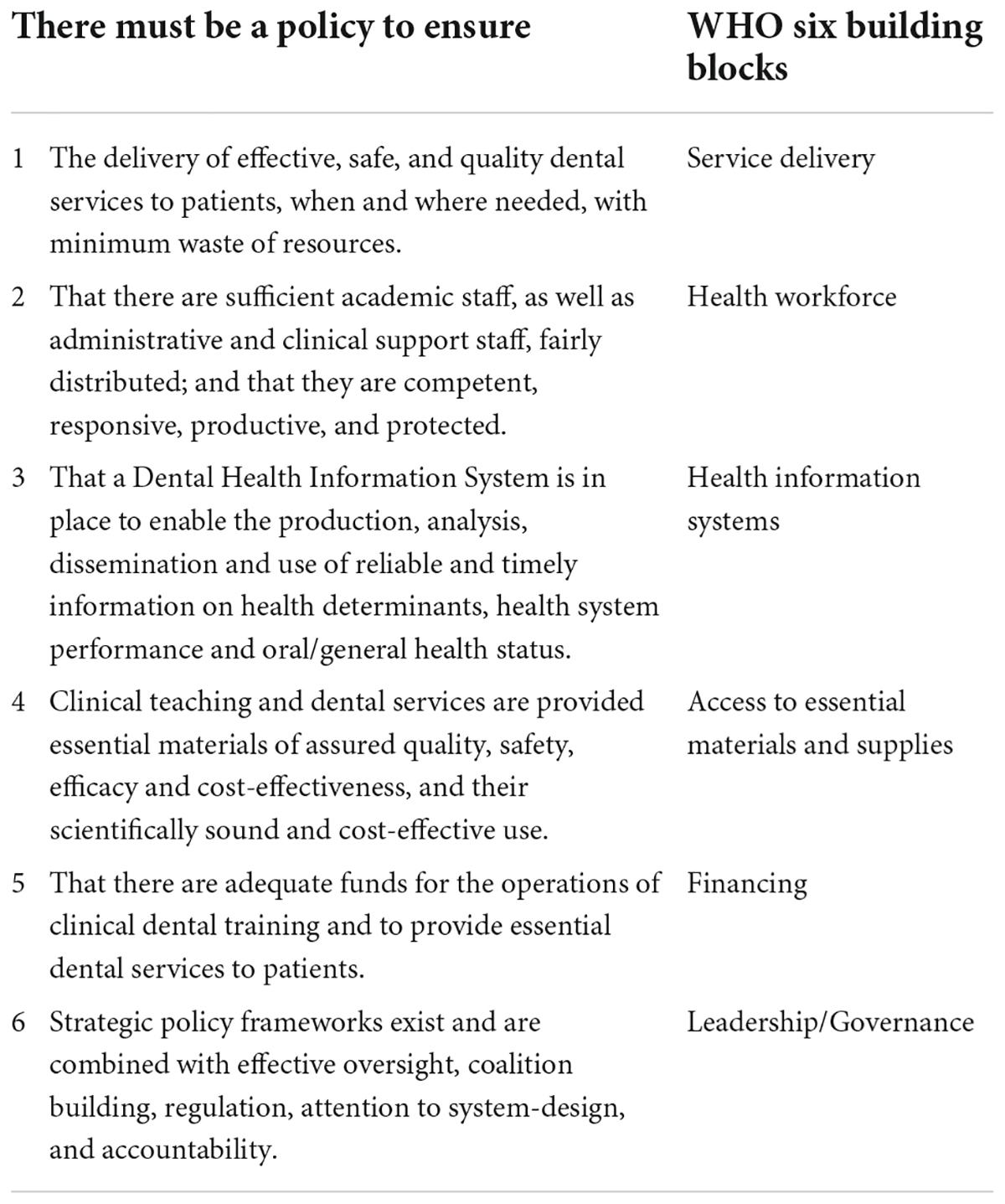
Part B (Table 2) consists of six policy recommendation statements based on the WHO Health Systems Framework: Six Building Blocks (WHO, 2007) where the respondents were required to rank their agreement on each statement on a 5-point Likert scale ranging from “strongly disagree” to “strongly agree.”
We prepared the questionnaire form to be used as an online form and pre-tested it on eight senior clinical academics. The feedback from the pre-test was used to improve the clarity, ease of making responses, and the overall format of the questionnaire.
Data collection
We emailed the invitation to all deans of the thirteen dental schools across Malaysia. The invitation letter was accompanied by details of the study and an informed consent form for the deans to fill up if they agree to participate in the study. In the first round of the Delphi survey, participants would indicate their scores on each statement formulated for both Parts A and B, based on the Likert scales via the pre-tested online questionnaire. They submitted the answers within 4 weeks upon receiving the online questionnaire. Qualitative comments were collected for each statement and analysis of the comments was done by the research team. Any new issues suggested by the participants in Round One would be carried forward to Round Two. The researchers then summarized these scores and used them to formulate the second round of the Delphi survey.
In the second round, each participant was given the median group score of each of the statement which they had earlier ranked, alongside their own score. They were asked if they wished to change their score or keep their original score. The deans were also given the opportunity to add comments to their responses. The second round of the data collection was completed within 2 weeks.
The anonymity of the participants was maintained in both rounds. The participants involved only had the access to their own answers and the group’s median score from the first round. Only the researchers had the access to each participant’s answers and personal details.
Data analysis
Responses from the online form were exported to Microsoft Excel, and descriptive statistics were reported using the median Likert scores, and consensus score (%) for each item. The response for Likert Scale of 3–5 was counted as agreement to the statement and the percentage of agreement for each statement was calculated. Consensus was defined a priori as weak (less than 65% agreement), moderate (65–79% agreement), and strong (80% or more agreement) (Engelman et al., 2018).
Results
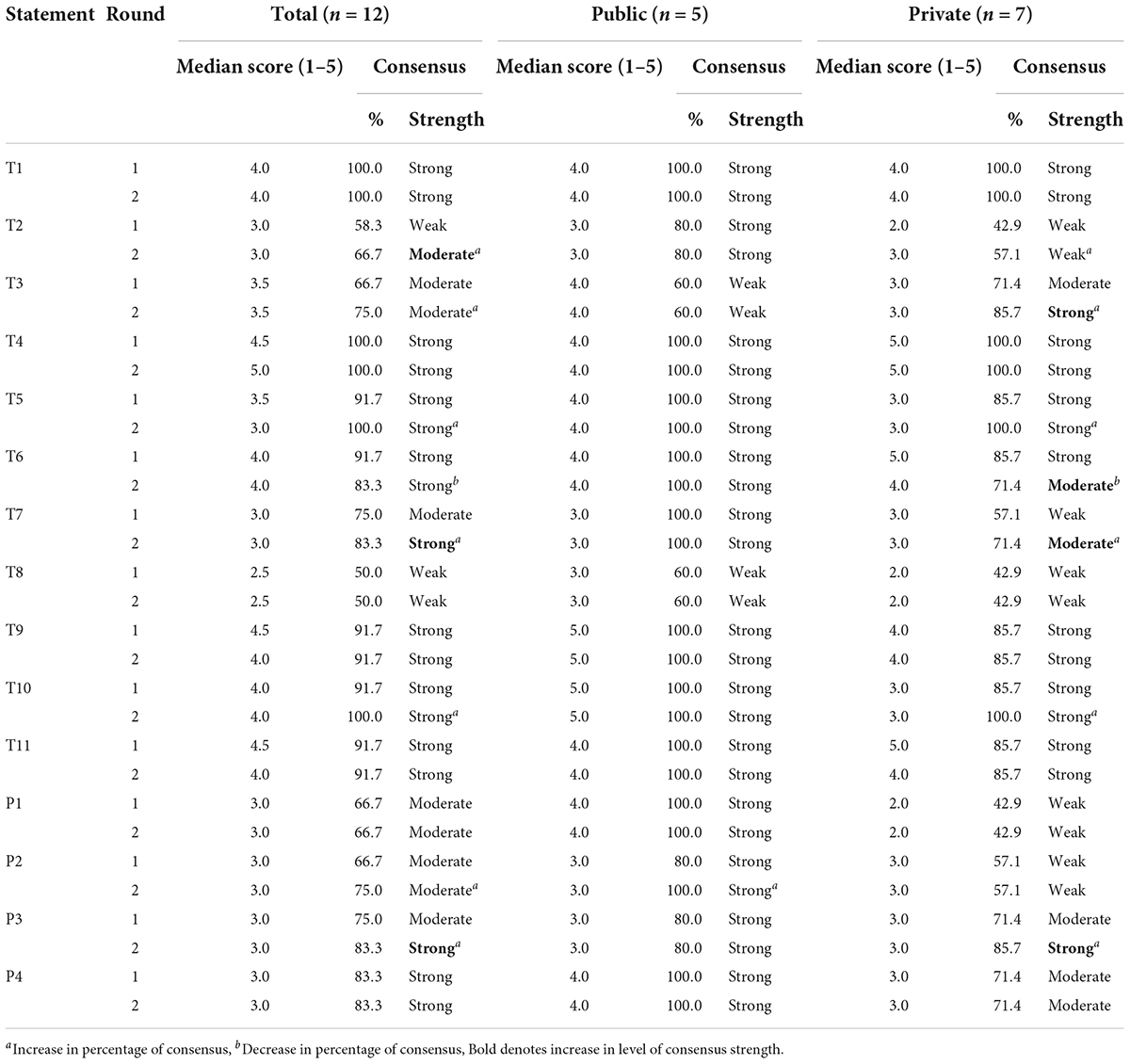
Twelve deans out of thirteen dental schools participated in both rounds of the modified Delphi survey (92.3% response rate), out of which five were public and seven were privately funded dental schools. Table 3 summarizes the round one and round two survey results of the deans’ consensus on the impact and challenges of the COVID-19 pandemic on dental education.
The percentage of consensus for seven items increased while one item saw a slight decrease in the percentage of consensus at the second round of the survey. Overall, the deans agreed with strong consensus to 10 out of fifteen items listed to be the challenges they faced due to the COVID-19 pandemic. The only item that had a median score of less than 3 denoting disagreement of the item being a challenge was regarding COVID-19 causing interruptions to classes due to inadequate ICT equipment at the faculty to facilitate online teaching and learning sufficiently. However, the consensus among the deans was weak for this item (50.0%).
There is also a notable difference in the strength of consensus for the items listed between public and private dental school deans where the public dental school deans reached strong consensus for thirteen items compared to eight items among the private dental school deans. Nevertheless, all deans unanimously agreed with high median scores for these three statements: (T4) The COVID-19 pandemic has caused the patients under care of students to experience interrupted dental treatment which increases their risk of having their dental and overall wellbeing affected (by the postponement of dental care); (T10) The COVID-19 pandemic has caused the need to increase clinical budget for daily operations of Students’ clinics to cater for extra PPE and related expenses, and; (T1) The COVID-19 pandemic has affected the students’ ability to meet clinical requirements for safe and competent practice.
Table 4 summarizes the deans’ agreement on items related to policies needed for dental education for round one and round two of the survey. The median score for all statements was between 4.5 and 5 with strong level of consensus. No change of opinion was noted between round two and round one for this section.
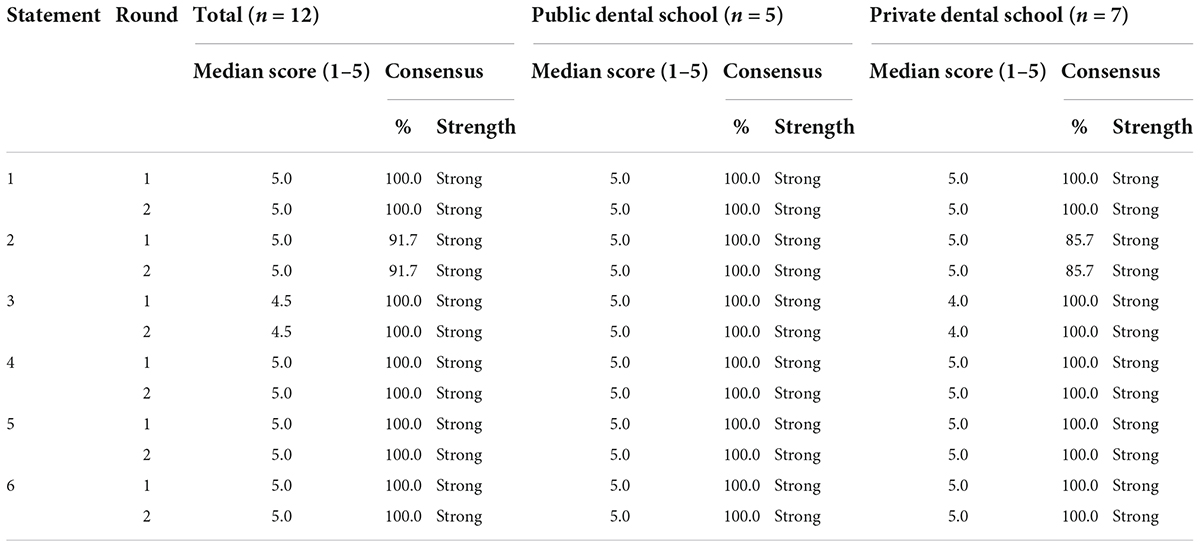
Table 4. Consensus on dental education policy statements to sustain safe and effective delivery of the curriculum based on the WHO Six Building Blocks.
Some deans also took the opportunity to add comments with regards to the challenges faced and policies needed to counter the impact brought by COVID-19 on the country’s dental education. All comments provided by the deans were scrutinized and found to be emphasizing the existing statements and so they were not added as new issues in the second round of the survey.
“Emotional support for the students and staff during this challenging time.” Dean-2
“Policy on the need for all dental clinics including private to employ officially trained clinical support staffs.” Dean-5
“The decision to close down operations of colleges and universities should be done with pragmatic approach, keeping a distinction between health professional institution and other programs. The actual impact of this year’s policy of MCO (Movement Control Order) will be borne by the future cohorts of students who are in their junior years and have not had the required clinical exposure thus leading to extension of their training. Also, a more flexi policy in terms of staff numbers, SLT management, regulating MCE/ECE (Minimum Clinical Exposure/Expected Clinical Exposure) etc. should be allowed for dental institutions for the next 2–3 years because the covid-19 pandemic impact has manifold ramification in the years ahead. This should be borne in mind especially when accreditation assessment.” Dean-6
“Relook into the Malaysian: expatriate staff ratio as it is very challenging to get clinicians in few regions of the country.” Dean-9
“In making demands to ensure quality and quantity, any policy created should be an equitable and fair one able to be met by both public and private universities. It is unfair to expect every single equipment in a private university must equate to public universities more so if the university is still young and groping. However, academic staff’s quality should not be compromised but again a fairer system should be discussed. Imposition of policies based on a so-called benchmark university will not help a young and new institution.” Dean-11
“Additionally, the uncontrolled increase in the price of these PPE, availability and excessive use and additionally PPE required due to enhanced infection control protocol, made the budgeting very challenging.” Dean-9
Discussion
Our study employed the modified Delphi method which is in line with the recommendations of past studies (Waggoner et al., 2016; Jünger et al., 2017). The Delphi technique was developed in the 1950s by The Rand Corporation scientists and has become increasingly used as a method for developing consensual guidance on best practice. Instead of starting the round with an open-ended questionnaire, our first round was modified by asking the participants to rank items synthesized from published literature. This modification was implemented to ensure a solid grounding in the existing evidence regarding the issue discussed. Additionally, the strength of the modified Delphi technique used lies in the anonymity of the participants as well as controlled feedback that is believed to reduce the effect of bias due to group interaction (Custer et al., 1999).
The main issue with dental education and training is that university-led dental clinics are rarely seen as core to the national healthcare system because of the widespread perception that universities are for teaching and research only. Unless one has received treatment at a university dental clinic, most people are unaware that the bulk of the dental services at these clinics are provided by dental students. These existing shortcomings are further magnified by the restrictions imposed because of the pandemic. In dental school settings, dental faculty administrators have opted to make adaptations to the COVID-19 guidelines recommendation that were originally developed by the Ministry of Health for use at the various public and private sector dental clinics during and potentially beyond the pandemic.
Due to the different physical set-up of dental school clinics and the nature of patient flow in the clinical training environment, some of the measures in the original guidelines are not implementable. Furthermore, these adaptations would vary according to the unique dental school settings and geographical locations that may be affected by local authorities standard operating procedures. The adaptations of the original guidelines and ongoing uncertainties about the containment of the COVID-19 pandemic raises a concern whether dental students are able to continue their training to be safe and competent dentists. Subsequently, will universities be able to provide adequate resources to sustain safe and quality dental education and training amidst the uncertainties of this malicious disease outbreak?
Challenges and impact of COVID-19 on dental education
COVID-19 pandemic in Malaysia has caused interruptions to higher education from the first MCO issued. This had resulted in disruptions to teaching and learning activities of dental students as agreed unanimously by the deans of Malaysian dental school from this study and confirms that Malaysian dental schools experienced similar challenges reported worldwide (Gurgel et al., 2020; Peres et al., 2020; Quinn et al., 2020; Wang et al., 2021) such as limitation of face-to-face teaching and learning activities, and disrupted clinical training. Due to the limitation of face-to-face classes, all universities have adapted to the emergency remote teaching. However, not all components could be delivered via this method (Elangovan et al., 2020; Saeed et al., 2020).
In Malaysia, dental graduates are deemed as competent to fully register and serve as dentists with the Ministry of Health upon graduation as opposed to their medical counterpart who need to undergo houseman-ship for a minimum of 2 years. It is therefore imperative for all dental schools to ensure their graduating students have achieved the required competencies to serve as dentists independently. And this requires face to face clinical training. Another problem with remote teaching is it deepens the issue with inequalities where students from the lower socio-economic background were reported to have difficulties accessing remote lessons (Hill and Lawton, 2018; Zilka et al., 2021).
It is clear from our findings that the COVID-19 has impacted the training of dental students in Malaysia. Other surveys addressing the Malaysian dental students also reported similar sentiments (Lestari et al., 2022; Pandarathodiyil et al., 2022). Disrupted clinical training leads not just the difficulty in ensuring graduate competencies, it also affects the psychological and emotional state of the students, and leads to another major concern which was the disruption of continuity of care that would be detrimental for the oral health of their patients (Al-Omiri et al., 2021; Nguyen et al., 2021). Untreated oral diseases, resulting in preventable pain, infection and reduced quality of life, can lead to productivity losses such as missed schooling or work.
The clinical training of dental students in Malaysia was suspended intermittently for almost a year since 2020. These missed clinical sessions, if not replaced, will mean that students risk not getting the training and competencies required to graduate. The decision to suspend operations of colleges and universities should therefore be done with pragmatic approach, keeping a distinction between health professional institution and other programs. The dental faculty fraternity are at a higher risk to be infested with any blood-borne or fluid-borne (droplets and splatters) infectious disease due to close patient contact in the clinic environment. With a specific policy, concerns for their health and safety can be made a priority with regards to sufficient protective measures like personal protective equipment (PPE) and vaccination, as well as effective work from home measures to reduce unnecessary crowding at the workplace. Support for mental and emotional health of the dental faculty fraternity must also be in place because fear, anxiety and burnout are rife during these difficult times (Shacham et al., 2020; Uhlen et al., 2021). These policies will give autonomy to faculty administrators to make quick decisions regarding these matters and not strictly bounded by blanket practices in other faculties.
Recommendation for sustaining quality dental education
Acknowledging the challenges brought forth by the COVID-19 pandemic, current research proposed six policy statements based on the World Health Organization (WHO) Six Building Blocks of Health System Framework (WHO, 2007) to cover the areas needed for dental schools to sustain quality dental education even in the midst of infectious disease outbreaks or other situations of national crisis. The Six Building Blocks of Health Systems Framework describes health systems in terms of six building blocks namely service delivery, health workforce, health system information, essential materials and supplies, health financing, and leadership/governance. Each block holds equal importance in ensuring smooth running of a healthcare system.
Service delivery
When university-led dental clinics are not considered as core to the national healthcare system (Ahmad et al., 2020), they risk being under-funded when the given operating budget does not match the needs to run not only a teaching and research institution, but clinics providing treatment for real patients. Sustainable policies to help maneuver challenges faced in running dental schools not just based on their existence as training institutions but as part of the healthcare system are needed now more than ever.
Health workforce
In Malaysia, there is an apparent imbalance in the number of local against international academic manpower between public and private dental schools. Supported by the government fundings, public dental schools manage to implement recommended strategies (Corbet et al., 2008) such as competitive pay scale and better career advancement prospect; opportunities for sponsored postgraduate studies; and the chance to opt for an attractive retirement scheme. However, private dental schools are not able to offer similar benefits making it difficult for them to recruit local academics as commented by one of the dental deans. This discrepancy in human resource policy is an added challenge to the private institutions in recruiting and retaining clinical dental educators.
The ability of a dental faculty to meet its training, research and service goals depends largely on the knowledge, skills, motivation, and deployment of the people responsible for organizing and executing these tasks. Difficulty in securing a good number of human resources needed to deliver essential tasks including health services could be due to a number of reasons, for example location of the university or the inability to recruit qualified personnel (Godwin et al., 2014).
Seven out of 12 dental schools involved in this study are located in and around Kuala Lumpur, the capital city of Malaysia. For these schools, recruiting and retaining qualified personnel may not be as challenging as the schools located far away from the capital city. Dental education policies need to factor in the human resource challenges and relevant strategies such as more attractive renumeration to ensure core activities of the dental schools are not affected. The uniqueness of the dental school workforce should be given its due recognition because of the dual duties assumed in delivering training as well as dental services to the public.
Health information system
Sound information on the availability of human resource is needed to formulate a policy in pursuit of human resources to operate a dental school. Sound and reliable information also plays a vital role in making important decisions pertaining to health service delivery, research and training which are also the core components of a dental school. Hence, all dental schools should have a policy that supports the collection, analysis and management of health-related information in order to ensure successful monitoring and evaluation of training and service delivery.
It would be desirable that there is digital sharing of information between institutions to allow a larger pool of data to be generated and analyzed for better health and training needs decision-making, provided all precautionary measures are taken to ensure sensitive and personal data of patients and institutions are duly protected. This initiative would be in tandem with the aspirations of the Ministry of Health to achieve a seamless level of patient information services and systems and enhance the effectiveness of health services in terms of holistic patient care and management.
One of the major impacts of the COVID-19 pandemic of COVID-19 on the oral healthcare delivery is the reduced face-to-face consultation and the risk of infection during the delivery of aerosol generating procedure (AGP). Thus, it is worthwhile that investments in digital technology for tele-dentistry initiatives be considered, and this is in fact would be in line with the rise in patient expectation and consumerism (Loh et al., 2020; Patel and Wong, 2020; Menhadji et al., 2021).
Essential materials and supplies
The Malaysian dental deans also strongly agreed on the need for a policy guaranteed essential materials of assured quality, safety, efficacy, and cost-effectiveness, and their scientifically sound and cost-effective use for clinical teaching and dental services provided. One of the deans in the free comment section also noted that the prize of essential materials and supplies for clinical training and teaching need to be controlled. A well-functioning health system ensures equitable access to safe and effective materials and supplies essential for operation (WHO, 2010).
Just like other building blocks-related statements, the policy to monitor access to essential materials and supplies is closely intertwined with other building blocks. When essential materials and supplies are not secured, the service delivery will also be disrupted hence, weakening the health system. Therefore, essential materials and supplies for dental schools need to be made available within the context of functioning health systems at all times, in appropriate amount, with good quality, and at a controlled and affordable price.
Health system financing
Health financing is an essential part to maintain and improve health system. Without funds it is not possible to employ health workers nor procure essential materials and supplies as well as many other activities within the system. Malaysia was successful at achieving near-universal access to public sector healthcare at low cost with a huge portion of the healthcare financing absorbed by the government. The cost that needs to be absorbed by the government continues to increase and better health system financing has been discussed and proposed many times by experts from various backgrounds at national level. However, it is a challenge that need to be handled with care considering Malaysian policymakers feared for their political survival which made them refrain from implementing reforms to current policy especially when the Malaysian public is generally resistant to any change that might require them to pay even a small amount to contribute to the health financing mechanism (Croke et al., 2019).
COVID-19 has caused a significant impact on the financial aspects of the running of the dental schools. Dental schools in Malaysia belong to the Ministry of Higher Education and have limited autonomy in how they manage their funds. Proper consideration unique to dental schools is needed to maintain universal coverage that allows access to health services without the risk of a financial catastrophe to patients and the institution.
Leadership and governance
Governance in health is an integral part of the health system components and intimately connected with accountability. Leading and governing dental schools require great accountability to produce results from the fundings received. Accountability is therefore an important aspect of governance that concerns the management of health service delivery, training, and research activities in dental schools. Strong and effective leadership is a compulsory trait for dental academia leaders to succeed (Verma et al., 2019) amidst the challenges discussed in this paper.
There is currently no National Dental Education Policy, and hence there is no over-arching guidance document that unites the dental educators, and merges dental education and training with other dental agencies and stakeholders in achieving the overall quality of life direction for Malaysians. To be able to create a policy framework to address issues and challenges faced by the dental education sector is timely now as Malaysia aims to achieve the Sustainable Development Goals and specifically the National Oral Health Plan for Malaysia 2030 agenda in the era of post COVID-19 pandemic.
In view of the deans’ consensus on the impacts of COVID-19 and the policy statements for sustainable dental education, this study proposed that the policy on dental education should ensure that the following six deliverables are supported:
1. Delivery of effective, safe, and quality dental services to patients at the faculty clinics, when and where needed, with minimum waste of resources.
2. There are sufficient academic staff, as well as administrative and clinical support staff at the faculty, type and numbers fairly distributed across the departments; and that they are competent, responsive, productive, and protected.
3. A Dental Health Information System is in place to enable the production, analysis, dissemination, and use of reliable and timely information on health determinants, health system performance, and oral/general health status of the patients.
4. Clinical teaching and dental services are provided essential materials of assured quality, safety, efficacy, and cost-effectiveness, and their scientifically sound and cost-effective use.
5. Adequate funds for the operations of clinical dental training and to provide essential dental services to patients.
6. Strategic policy frameworks exist for teaching and learning activities for dental students, including dental services operations, and that these frameworks are combined with effective oversight of strong faculty leadership, coalition building with stakeholders (e.g., Ministry of Higher Education, Ministry of Health, Ministry of Defense), regulation, attention to system-design and accountability in decision-making.
Limitation of the study
Studies using the modified Delphi method may not achieve the same results as other methods to achieve consensus that employ face to face or online synchronous discussion. The lack of interactions between participants may have hampered the process of producing and assessing new ideas which was evident in the lack of new relevant issues provided by the participants in our study. Further, the statements used to achieve the consensus were synthesized from studies published during the early phase of the pandemic and may not reflect issues faced at a later phase. Nonetheless, the opportunity to add other statements had been given to the participants in the open-ended sections of the survey questionnaire.
Despite the absence of validated quality parameters to evaluate Delphi studies (Nasa et al., 2021) we took great care to ensure the methods used in our study observed the following recommendations: Experts recruited are defined and the method of recruitment is explained; Anonymity of participants are ensured; Iterative discussions with controlled feedback is employed; Consensus is defined; Statistical evaluation is described (Jünger et al., 2017; Engelman et al., 2018; Nasa et al., 2021).
Conclusion
The COVID-19 pandemic has further magnified the existing shortcomings faced by the dental schools and is expected to have manifold ramification in the years ahead. Accepting that dental schools are part of the health system acknowledges their need to have clear policies on having adequate number of trained staff, sufficient funds, information, supplies, transport, communications, and overall guidance and direction to function. Having a National Dental Education Policy that addresses the unique challenges identified in this study will serve as a monumental cornerstone to sustain quality dental education during times of calamity.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
This study was reviewed and approved by the Research Ethics Committee of Universiti Kebangsaan Malaysia (UKM PPI/111/8/JEP-2020-690). The participants provided their written informed consent to participate in this study.
Author contributions
TM-D, KL, HR, and HY involved in the design of the study and contributed to the review of literature. KL collected the data. KL, TM-D, and HR conducted analyses. HR and TM-D wrote the first draft of the manuscript, after which KL and HY read and critically revised. All authors have made a substantial, direct, and intellectual contribution to the work, and approved it for publication.
Funding
This study was supported by the Ministry of Higher Education Special Post-Covid Grant (COVIDKPT-2020-001).
Acknowledgments
We thank the deans who participated in this study, and the following dental educators who helped extract the themes from the selected literature: Abishek Parolia; Budi Aslinie Md Sabri; Kranthi Raja Kacharaju; Niekla Andiesta, Nik Mohd Mazuan Nik Mohd Rosdy; and Rashidah Esa.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Ahmad, R., Zul, N. A., Mohtar, S. A., Tennant, M., and Mohd-Dom, T. N. (2020). Revisiting a funding model for university-led dental clinics: The case of complete denture fabrication. J. Dent. Indones. 27, 61–66. doi: 10.14693/jdi.v27i2.1136
Al-Omiri, M. K., Al-Shayyab, M. H., al Nazeh, A. A., Alraheam, I. A., Malkawi, Z. A., Alomiri, A. K., et al. (2021). COVID-19 and dentistry: An updated overview of dental perspectives and a recommended protocol for dental care and emergency dental treatment. J. Contemp. Dent. Pract. 22, 572–586. doi: 10.5005/jp-journals-10024-3076
Araf, Y., Akter, F., Tang, Y., Fatemi, R., Parvez, M. S. A., Zheng, C., et al. (2022). Omicron variant of SARS-CoV-2: Genomics, transmissibility, and responses to current COVID-19 vaccines. J. Med. Virol. 94, 1825–1832. doi: 10.1002/jmv.27588
Boehm, E., Kronig, I., Neher, R. A., Eckerle, I., Vetter, P., and Kaiser, L. (2021). Novel SARS-CoV-2 variants: The pandemics within the pandemic. Clin. Microbiol. Infect. 27, 1109–1117. doi: 10.1016/j.cmi.2021.05.022
Corbet, E., Akinwade, J., Duggal, R., Gebreegziabher, G., Hirvikangas, H., Hysi, D., et al. (2008). Staff recruitment, development and global mobility. Eur. J. Dent. Educ. 12, 149–160. doi: 10.1111/j.1600-0579.2007.00496.x
Croke, K., Mohd Yusoff, M., Abdullah, Z., Mohd hanafiah, A., Mokhtarudin, K., Ramli, E., et al. (2019). The political economy of health financing reform in Malaysia. Health Policy Plan 34, 732–739. doi: 10.1093/heapol/czz089
Custer, R., Scarcella, J., and Stewart, B. (1999). The modified Delphi technique-A rotational modification. J. Career Tech. Educ. 15, 50–58. doi: 10.21061/jcte.v15i2.702
Elangovan, S., Mahrous, A., and Marchini, L. (2020). Disruptions during a pandemic: Gaps identified and lessons learned. J. Dent. Educ. 84, 1270–1274. doi: 10.1002/jdd.12236
Engelman, D., Fuller, L. C., Steer, A. C., and International Alliance for the Control of Scabies Delphi panel (2018). Consensus criteria for the diagnosis of scabies: A Delphi study of international experts. PLoS Negl. Trop. Dis. 12:e0006549. doi: 10.1371/journal.pntd.0006549
Godwin, D., Hoang, H., Crocombe, L., and Bell, E. (2014). Dental practitioner rural work movements: A systematic review. Rural Remote Health 14:2825. doi: 10.22605/RRH2825
Gurgel, B. C., de, V., Borges, S. B., Borges, R. E. A., Calderon, P., and dos, S. (2020). COVID-19: Perspectives for the management of dental care and education. J. Appl. Oral Sci. 28:e20200358. doi: 10.1590/1678-7757-2020-0358
Hill, C., and Lawton, W. (2018). Universities, the digital divide and global inequality. J. High. Educ. Policy Manage. 40, 598–610. doi: 10.1080/1360080X.2018.1531211
Izzetti, R., Nisi, M., Gabriele, M., and Graziani, F. (2020). COVID-19 transmission in dental practice: Brief review of preventive measures in Italy. J. Dent. Res. 99, 1030–1038. doi: 10.1177/0022034520920580
Jünger, S., Payne, S. A., Brine, J., Radbruch, L., and Brearley, S. G. (2017). Guidance on Conducting and REporting DElphi Studies (CREDES) in palliative care: Recommendations based on a methodological systematic review. Palliat. Med. 31, 684–706. doi: 10.1177/0269216317690685
Kerkstra, R. L., Rustagi, K. A., Grimshaw, A. A., and Minges, K. E. (2022). Dental education practices during COVID-19: A scoping review. J. Dent. Educ. 86, 546–573. doi: 10.1002/jdd.12849
Lestari, W., Yazid, N. H., Azhar, Z. N., Ismail, A., and Sukotjo, C. (2022). Impact of COVID-19 on Malaysian dental students’ physical, mental, financial and academic concerns. BMC Oral Health 22:46. doi: 10.1186/s12903-022-02081-w
Loh, M., Loh, D., and Loh, W. Y. C. (2020). Global pandemic: Consulting strategies in managing dental patients. Clin. Dent. Rev. 4:19. doi: 10.1177/0022034521990314
Meng, L., Hua, F., and Bian, Z. (2020). Coronavirus disease 2019 (COVID-19): Emerging and future challenges for dental and oral medicine. J. Dent. Res. 99:1113. doi: 10.1177/0022034520932149
Menhadji, P., Patel, R., Asimakopoulou, K., Quinn, B., Khoshkhounejad, G., Pasha, P., et al. (2021). Patients’ and dentists’ perceptions of Tele-Dentistry at the time of COVID-19. A questionnaire-based study.: Tele-dentistry at the time of COVID-19. J. Dent. 113:103782. doi: 10.1016/j.jdent.2021.103782
Mistry, P., Barmania, F., Mellet, J., Peta, K., Strydom, A., Viljoen, I. M., et al. (2022). SARS-CoV-2 Variants, vaccines, and host immunity. Front. Immunol. 12:809244. doi: 10.3389/fimmu.2021.809244
Nasa, P., Jain, R., and Juneja, D. (2021). Delphi methodology in healthcare research: How to decide its appropriateness. World J. Methodol. 11, 116–129. doi: 10.5662/wjm.v11.i4.116
Nguyen, T. M., Tonmukayakul, U., and Calache, H. (2021). Dental restrictions to clinical practice during the COVID-19 Pandemic: An Australian perspective. JDR Clin. Trans. Res. 6, 291–294. doi: 10.1177/23800844211000341
Oral Health Division Ministry of Health Malaysia (2020a). Guidelines on issues related to COVID-19 infection at the dental clinics (in Malay). Putrajaya: Ministry of Health Malaysia.
Oral Health Division Ministry of Health Malaysia (2020b). Guidelines for Dental Services Post Movement Control Order due to COVID-19 (in Malay). Putrajaya: Ministry of Health Malaysia.
Pandarathodiyil, A. K., Mani, S. A., Ghani, W. M. N., Ramanathan, A., Talib, R., and Zamzuri, A. T. (2022). Preparedness of recent dental graduates and final-year undergraduate dental students for practice amidst the COVID-19 pandemic. Eur. J. Dent. Educ. [Epub ahead of print]. doi: 10.1111/eje.12779
Patel, T., and Wong, J. (2020). The role of real-time interactive video consultations in dental practice during the recovery and restoration phase of the COVID-19 outbreak. Br. Dent. J. 229, 196–200. doi: 10.1038/s41415-020-1918-7
Peres, K. G., Reher, P., Castro, R. D., de, and Vieira, A. R. (2020). COVID-19-related challenges in dental education: Experiences from Brazil, the USA, and Australia. Pesqui. Bras. Odontopediatr. Clín. Integr. 20, 1–10. doi: 10.1590/pboci.2020.130
Quinn, B., Field, J., Gorter, R., Akota, I., Manzanares, M.-C., Paganelli, C., et al. (2020). COVID-19: The immediate response of European academic dental institutions and future implications for dental education. Eur. J. Dent. Educ. 24, 811–814. doi: 10.1111/eje.12542
Ross, J. (2021). Universities shuttered across Malaysia as third Covid wave hits | Times Higher Education (THE) [WWW Document]. Times Higher Education. Available online at: https://www.timeshighereducation.com/news/universities-shuttered-across-malaysia (accessed September 09, 2021).
Saeed, S. G., Bain, J., Khoo, E., and Siqueira, W. L. (2020). COVID−19: Finding silver linings for dental education. J. Dent. Educ. 84, 1060–1063. doi: 10.1002/jdd.12234
Shacham, M., Hamama-Raz, Y., Kolerman, R., Mijiritsky, O., Ben-Ezra, M., and Mijiritsky, E. (2020). COVID-19 factors and psychological factors associated with elevated psychological distress among dentists and dental hygienists in Israel. Int. J. Environ. Res. Public Health 17:2900. doi: 10.3390/ijerph17082900
Uhlen, M. M., Ansteinsson, V. E., Stangvaltaite-Mouhat, L., Korzeniewska, L., Skudutyte-Rysstad, R., Shabestari, M., et al. (2021). Psychological impact of the COVID-19 pandemic on dental health personnel in Norway. BMC Health Serv. Res. 21:420. doi: 10.1186/s12913-021-06443-y
Verma, M., Wilson, N. H. F., Lynch, C. D., and Nanda, A. (2019). Leadership in academic dentistry. J. Dent. 87, 2–6. doi: 10.1016/j.jdent.2019.05.002
Waggoner, J., Carline, J. D., and Durning, S. J. (2016). Is there a consensus on consensus methodology? Descriptions and recommendations for future consensus research. Acad. Med. 91, 663–668. doi: 10.1097/ACM.0000000000001092
Wang, K., Zhang, L., and Ye, L. (2021). A nationwide survey of online teaching strategies in dental education in China. Journal of Dental Education 85, 128–134. doi: 10.1002/jdd.12413
WHO (2007). The WHO’s Health System Building Blocks Framework. World Health Organization. Everybody’s Business: Strengthening health systems to improve health outcomes—WHO’s Framework for Action. Geneva: WHO.
WHO (2020). Director-General’s opening remarks at the media briefing on COVID-19 - 11 March 2020 [WWW Document], 2020. Available online at: https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19—11-march-2020 (accessed September 9, 2021).
WHO (2010). Monitoring the building blocks of health systems?: A Handbook of Indicators and their measurement strategies. Geneva: WHO.
Keywords: COVID-19, dental education, modified-delphi technique, WHO’s Six Building Blocks, health care system
Citation: Mohd-Dom TN, Lim KX, Rani H and Yew HZ (2022) Malaysian dental deans’ consensus on impact of COVID-19 and recommendations for sustaining quality dental education. Front. Educ. 7:926376. doi: 10.3389/feduc.2022.926376
Received: 22 April 2022; Accepted: 10 August 2022;
Published: 29 August 2022.
Edited by:
Zahiruddin Fitri, University of Malaya, MalaysiaReviewed by:
Gudrun Edgren, Lund University, SwedenJuraifa Jais, Universiti Tenaga Nasional, Malaysia
Alexandre Rezende Vieira, University of Pittsburgh, United States
Copyright © 2022 Mohd-Dom, Lim, Rani and Yew. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Haslina Rani, aHJAdWttLmVkdS5teQ==
 Tuti Ningseh Mohd-Dom
Tuti Ningseh Mohd-Dom Kai Xin Lim
Kai Xin Lim Haslina Rani
Haslina Rani Hsu Zenn Yew
Hsu Zenn Yew