- 1Department of Medical Education, College of Medicine, King Saud bin Abdulaziz University for Health Sciences, Riyadh, Saudi Arabia
- 2King Abdullah International Medical Research Center, Riyadh, Saudi Arabia
- 3College of Medicine, King Saud bin Abdulaziz University for Health Sciences, Riyadh, Saudi Arabia
Background: Globally, there is a rising interest in the concept of social accountability (SA). The literature evaluating SA of medical schools is limited; however, some international studies have revealed a lack of understanding of SA by medical students. This study evaluated the perception of SA among medical students at a governmental university in Saudi Arabia.
Method: A cross-sectional study with 336 currently enrolled medical students was conducted from September 2020 to May 2021. The data were collected using an electronic survey comprised of the THEnet questionnaire that included 12 items to assess the perception of SA and some demographic variables. The total score was categorized into four groups and compared with the demographic profile of students.
Results: Out of the 336 participants, the mean age was 21.26 ± 0.5 years, with most students in the 19–21 age group (n = 154, 46%), and 189 (56.3%) were males. In addition, preclinical and clinical students had similar representation: 170 (51%) and 166 (49%), respectively. Most participants (173, 52%) scored in the 18–36 range, reflecting good perceived SA. The demographic profile of students (i.e., age, GPA, and year of study) was significantly associated with perceived SA (p = 0.003, 0.002, and < 0.001, respectively).
Conclusion: The study concludes that most medical students had a good level of perceived SA about their institution. The preclinical year students exhibited a better perception of SA. The final-year students were more critical about the SA of the institution compared to other students.
Introduction
The concept of social accountability (SA) has attained a growing interest worldwide (Emadzadeh et al., 2016). SA includes citizen-led efforts to hold public officials, lawmakers, and service providers accountable for their acts and performance in providing services, enhancing people’s welfare, and preserving their rights (Beck et al., 2007). In 1995, the World Health Organization (WHO) adapted this concept in medical schools (Boelen et al., 1995). The WHO defines SA in the context of medical education as the responsibility to focus education, research, and service activities on tackling the most pressing health issues in the communities, regions, and countries they are intended to serve (Boelen et al., 1995). As SA is considered the foundation of both medical practice and medical schools, four values were introduced by WHO, namely, quality, equity, relevance, and cost-effectiveness, to evaluate the progress of medical schools in addressing SA (Boelen et al., 1995). This implies that SA should emphasize meeting professional standards and satisfying community expectations through providing equal opportunities for healthcare to everyone, addressing locally relevant problems, and ensuring the cost-effectiveness of healthcare service delivery.
The main challenge for medical schools in the twenty-first century resides in the responsibility for achieving community-based medical education that is relevant to the community health needs to produce competent graduates who can provide optimal healthcare status. With the global shift toward anticipating the individual and societal health needs and tailoring curriculum to best meet priority health concerns of a nation, SA was integrated into some medical schools’ educational programs (Boelen et al., 1995; GCSAMS, 2010). Canadian medical schools were the earliest schools that officially adapted the concept of SA to ensure a highly valued Canadian healthcare system (Social Accountability | The Association of Faculties of Medicine of Canada [AFMC], 2022). Furthermore, other countries like Sudan, Saudi Arabia, and Egypt have also taken initiatives toward achieving community-based, socially accountable medical education. A study that assessed the SA of the Faculty of Medicine at the University of Gezira (FMUG), Sudan, concluded their educational program as socially responsible and socially accountable only in certain aspects (Ahmed et al., 2020). Hosny et al. (2015) suggested using the conceptualization production usability (CPU) model to assess SA in medical institutions. The study emphasized compliance with parameters of CPU domains for an institution to be recognized as a proactive, socially accountable medical school (Hosny et al., 2015).
Furthermore, a recent study conducted in Saudi Arabia used the SA grid issued by the WHO as a basis for assessing SA. The study concluded that the educational aspect had the highest compliance for SA. Nevertheless, there is a need for more studies to explore how to achieve accountable social status (Alrebish et al., 2020). Some locally conducted studies in Saudi Arabia have focused on developing an integrated curriculum that is more community-orientated for a new medical college. It was noted that the traditional curriculum was insufficient to graduate doctors, consequently providing lower quality services to their community (El-Naggar et al., 2017). They started formulating the new curriculum by interviewing experts and doing a literature survey/search to gather the needed information (El-Naggar et al., 2017). The study ended up formulating a program that consists of three phases “pre-med (year 1), organ/system, and clinical clerkship to be followed by a year of internship.” The Jazan Faculty of Medicine has adopted this program to improve the outcomes of medical staff (El-Naggar et al., 2017). Both studies have locally provided evidence that some medical schools in Saudi Arabia are socially accountable, although the extent is unknown, and more studies are needed to evaluate SA in the other medical schools.
Although the importance of SA is widely agreed upon, the concept of SA is less familiar among the medical students who are the end product of a medical college. A study conducted at Makerere College of Health Sciences exploring the perceptions of senior medical educators and students discovered that SA was an unfamiliar concept to many of the respondents. Many students are not even aware of this term (Galukande et al., 2012). Another international study conducted in the United Kingdom to assess the concept of SA in a medical school illustrated that students could not express a well-understanding of SA meaning. However, they admitted that the curricula revealed a few core principles around SA (McCrea and Murdoch-Eaton, 2014). A study by Social Accountability in Health Professional Education (SAHPE) showed that the associated supervisors in the hospital rated SAHPE medical workforce higher overall than traditional medical school graduates in socially accountable competencies and the overall performance and clinical skills (Woolley et al., 2019).
The perception of SA among students varies among different institutions across the world. Due to the limited reports on SA in Saudi Arabia, the study aimed to assess the perceived SA of medical students currently studying at the governmental institution following problem-based learning. Also, we wanted to assess whether the concept of SA was clearer among students across different years in medical school.
Materials and Methods
Study Design and Setting
A cross-sectional questionnaire-based survey was conducted in Riyadh campus between September 2020 and May 2021 at King Saud bin Abdulaziz University for Health Sciences (KSAU-HS). KSAU-HS is a governmental university first established in Riyadh in 2005, making it the first specialized university in health sciences in Saudi Arabia and the whole region (College Of Medicine Riyadh-Home, 2022). Subsequently, other campuses were established later in Jeddah and Al-Ahsa. It has 14 colleges in various health-related specialties on all these three campuses. The College of Medicine (COM) only exists in Riyadh and Jeddah, graduating almost 500 doctors every year.
The KSAU-HS mission is to deliver high-quality medical education, medical research, and community services that enhance society’s health. To achieve that, KSAU-HS adapts a problem-based, community-based, student-centered, and outcome-oriented program for the specialty of medicine and surgery in collaboration with Sydney University, Australia (College Of Medicine Riyadh-Home, 2022). Given the sizeable global shift toward competency-based medical education and its dominance over traditional learning approaches, the spectrum of educational interventions, including learning resources allocation, educational methods, teaching faculty, and Students’ performance assessment, should be shaped to best meet priority healthy needs (GCSAMS, 2010). Therefore, the Saudi Medical Education Directives Framework (SaudiMEDs framework) competencies were integrated into the KSAU-HS curriculum (Tekian and Al Ahwal, 2015; Ten Cate, 2017). It was adopted to ensure the implementation of six key competencies, namely, scientific method in practice, patient-centered care, community-based practice, professionalism, research, and scholarship. This would ensure a more efficiently delivered educational infrastructure and facilitate the graduation of competent healthcare providers capable of providing optimal healthcare services (Tekian and Al Ahwal, 2015).
Study Participants
The target population was all medical students studying preclinical and clinical phases from 2020 to 2021 at the Riyadh campus. Including both male and female campuses, both stream I, students who recently graduated from high school, and stream II, students who already have a bachelor’s degree in science, applied medical science or pharmacy, and currently studying medicine as a second major, from third to the sixth year. However, we excluded pre-medical students since they were new to the college during the data collection. The final sample was 336 students currently enrolled at the college of medicine. The non-probability quota sampling was used to include proper representation across different years of students and gender and avoid under or overpresenting the student groups. The approximate number of male and female students in each batch was 300 and 150, respectively. Therefore, the sample was divided into 50 and 34 participants from each male and female batch.
Data Collection Tool and Process
A validated questionnaire created by a collaboration between the International Federation of Medical Students Association (IFMSA) and the Training for Health Equity Network (THEnet) (Dijk et al., 2017) was used and distributed among students as an electronic survey available on Google Docs online platform. The link of the survey was distributed with the help of focal person who were the batch leaders from preclinical and clinical years. No prior pretesting was done before the data collection, and the questionnaire was adopted in its original form. The survey was accessible only to the target population. Due to unforeseen COVID-19 restrictions, the teaching model was shifted to online. Therefore, the mode of data collection was changed from self-administered hardcopy to online survey. Students had the right not to participate; filling out the questionnaire and submitting it was considered consent for participation (see Supplementary Appendix 1).
The main sections of the questionnaire were adapted from the original created by IFMSA; therefore, no prior pilot testing was done before formal data collection (Dijk et al., 2017). The questionnaire consisted of three sections. The first part displayed an introductory paragraph of the study’s aims and participation request along with consent form. The second section included questions related to demographic profile, including current year of study, clinical phase, stream, educational level, whether any family member belongs to healthcare background, and campus. The third section included the IFMSA and THEnet 12-item questionnaire to evaluate the medical colleges’ SA based on Students’ perceptions. The items were assessed on a four-point Likert scale (no = 0, somewhat = 1, good = 2, excellent = 3), with the lowest and highest score of 0–36 for the 12 items, respectively.
Statistical Analysis
A Microsoft Excel sheet was initially used for data entry and coding. The data were checked for correctness and missing information. After data cleaning, it was transferred for statistical analysis to Statistical Package for the Social Sciences software version 24. The overall Cronbach’s alpha for the 12 items on SA was 0.80 showing good internal reliability of the questionnaire in our sample. The descriptive statistics were reported for all the variables, and the means standard deviations (SDs) were reported for 12 items and other numerical variables, while the categorical data were presented as percentages. The total score for the 12 items on SA was computed first and presented as mean ± SD for the individual item. The total score was later categorized into four groups, namely, weak foundation in SA (score: 0–8), some SA (score: 9–17), look for areas of improvement (score: 18–26), and strong foundation in SA (score: 27–36). The percentages for each of the SA categories were also presented. To assess the association of SA categories with the profile of the students, chi-square and Fisher’s exact tests were applied as applicable. Additionally, a new variable was computed using the scores of SA items, and the cutoff score for acceptable SA was ≥ 18, and low SA was ≤ 17. Statistical significance was set at p-values < 0.05 for all the tests applied.
Ethical approval was given by the Institutional Review Board of King Abdullah International Medical Research Center, with ref No. IRBC/1413/20. All collected data were coded and kept under lock and key. Confidentiality and anonymity were always maintained during all the stages of the research.
Results
Demographic Characteristics
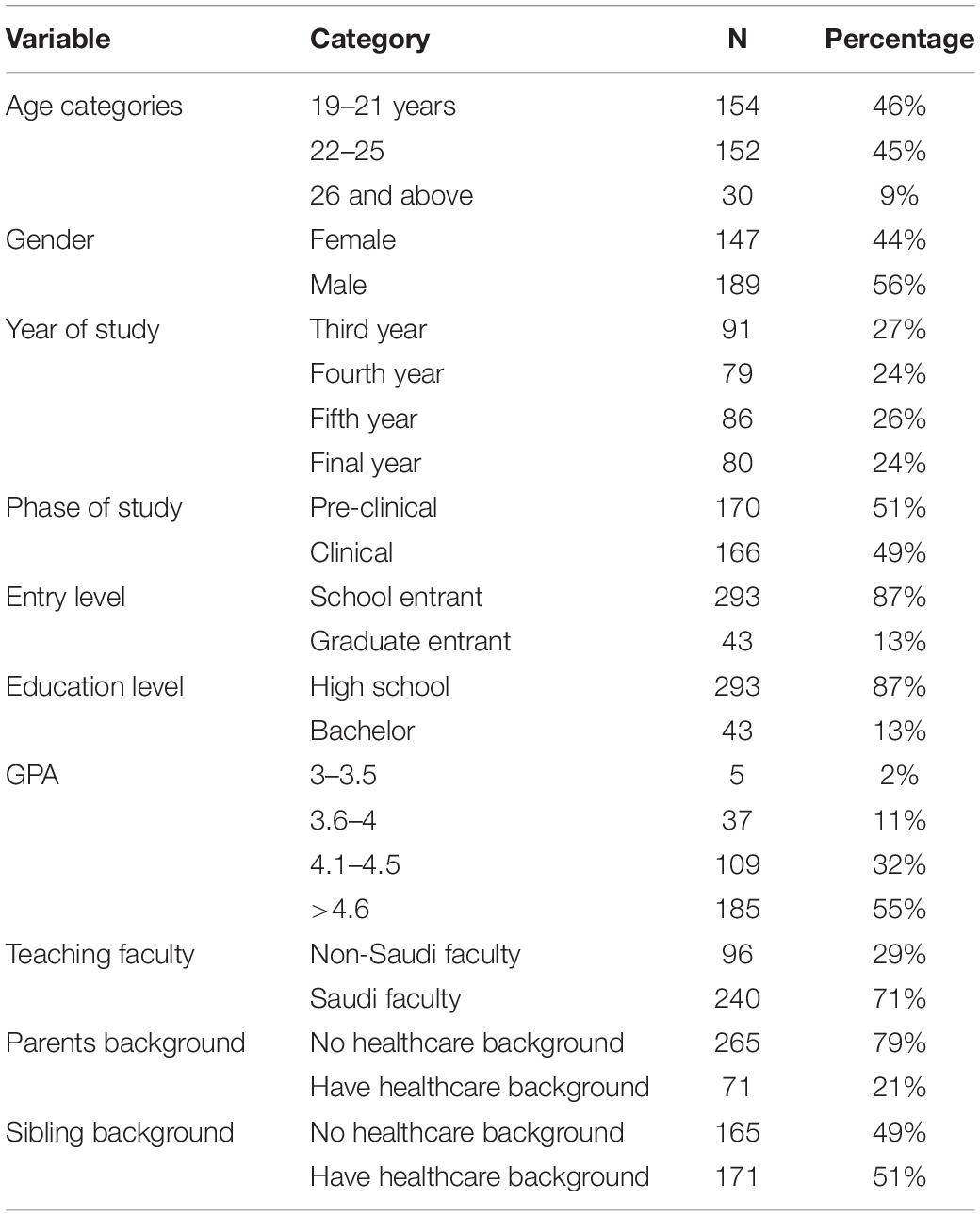
A total of 336 students with a mean age of 21.26 ± 0.5 years completed the survey distributed among medical students currently studying in KSAU-HS. Students aged < 25 years comprised the majority, with the 19–21-year-olds accounting for 46% (n = 154) of the students. Male participants represented 189 (56.3%) of the sample, with fourth-year students lowest in number 79 (24%). Similar percentages of medical students in their preclinical and clinical years were included in the study, 170 (51%) and 166 (49%), respectively. However, most enrolled students were school entrants, while only 43 (13%) were graduate entrants. On a GPA score of 5, the self-reported GPA for most students was >4.6. Furthermore, most students stated that they were taught by Saudi teaching faculty (Table 1).
Descriptive Summary of 12 Items Determining Social Accountability
Out of the 12 items determining the perceived SA, items 5 and 12 had the highest mean scores. Item 5, which evaluated the presence of the populations intended to be served by medical students at places where students are practicing medicine, had a mean of 2.08 ± 0.88. Furthermore, item 12 assessed the school’s positive impact on the community and had a mean of 2.07 ± 0.88. In addition, regarding the community-based research provided by the school, the mean score of item 10 was 1.9 ± 0.99, which was reasonable based on the scoring scale used in the study. Item 11, in contrast, assessed to what extent the school encouraged the students to undertake generalist specialties and had the least mean score of 1.18 ± 1.01. Items 6, 3, and 4 also had lower mean scores than the other items. Item 6 assessed if the community-based learning was one of the school’s learning objectives and had a mean score of 1.3 ± 1.04. Item 3 assessed whether the school’s curriculum considers other cultures and other social circumstances in a medical context, item 4, and had a mean of 1.39 ± 0.89. Items 1, 2, 7, 8, and 9 had an average assessment score between 1.6 ± 1.0 and 1.8 ± 0.87. Although the community’s needs are addressed by the school’s curriculum or not, which was evaluated by item 2, had a mean score of 1.87 ± 0.87. Furthermore, regarding the similarities of sociodemographic characteristics between the reference population and medical students, reference population, and teaching faculty, items 7 and 8 had mean scores of 1.71 ± 0.82 and 1.64 ± 0.88, respectively. Finally, item 9, which was related to the learning experience at the college allowing the students to play an active role in serving their community, had a mean score of 1.62 ± 1.00 (Table 2).
Social Accountability Status Based on Categorized Scores
Out of the 336 participants, 48 (14%) students perceived the SA of COM as very good and scored between 27 and 36, implying that the college has a strong foundation in SA and advocate for continued growth and leadership in SA. Whereas most of the students 173 (52%) scored between 18 and 26 and perceived that the school is doing well, there are weak areas and ways to improve SA. Furthermore, 98 (29%) students scored between 9 and 17 and perceived that the college has some SA strategies, and there is a need to build on these existing strategies. The rest of the students [17 (5%)] scored between 0 and 8, implying that the school has no SA and that there is a need to begin building up SA (Figure 1).
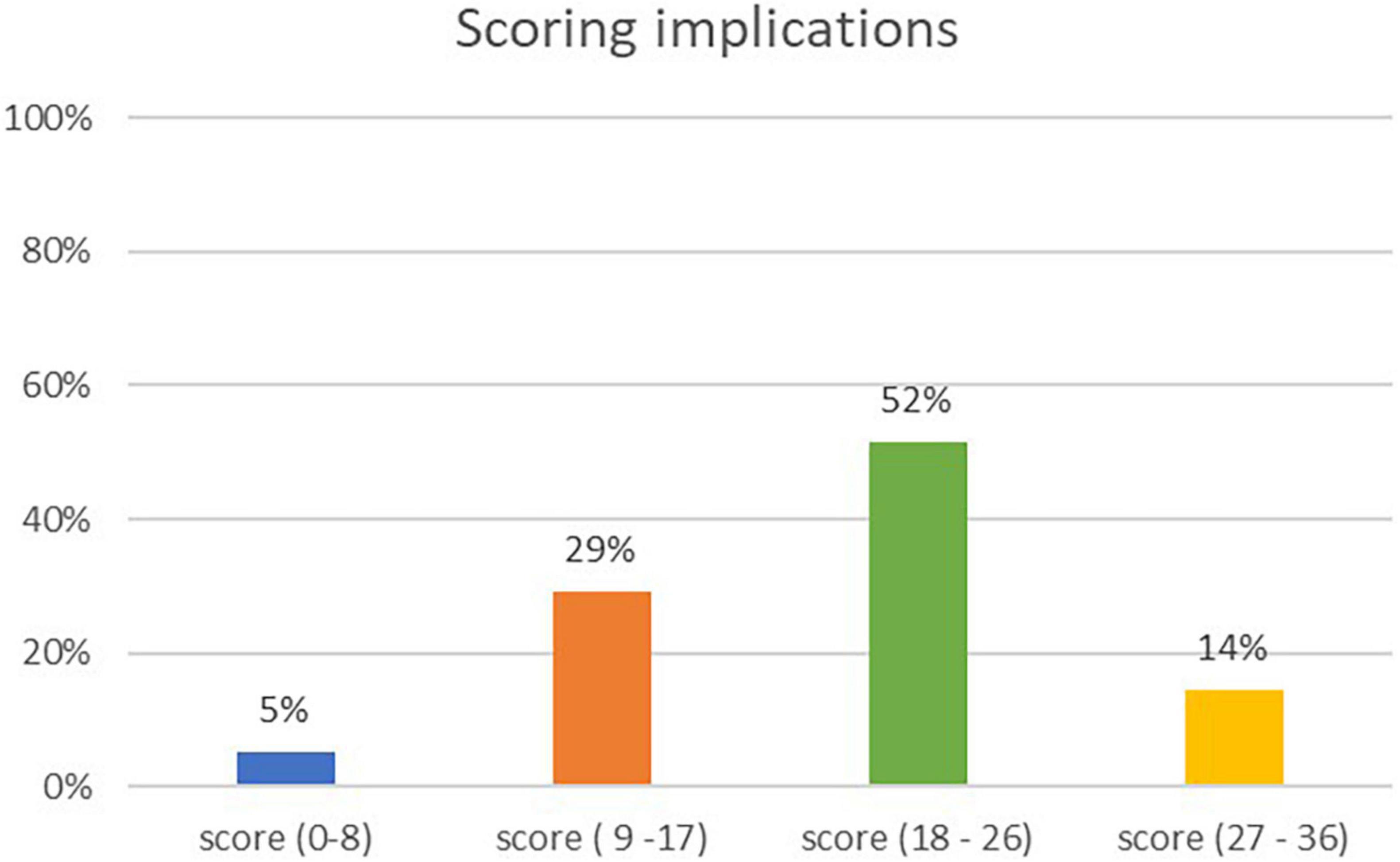
Figure 1. Social accountability status based on the categorized scores. (0–8) Start a conversation with your classmates and school to begin to build SA at your school (9–17), your school has some SA strategies, look for ways to advocate to build on these existing strategies (18–26), your school is doing well, look for areas of weakness and ways to advocate to improve SA (27–36), your school has a strong foundation in SA, advocate for continued growth and leadership in SA.
Association of Participants’ Profiles With Social Accountability
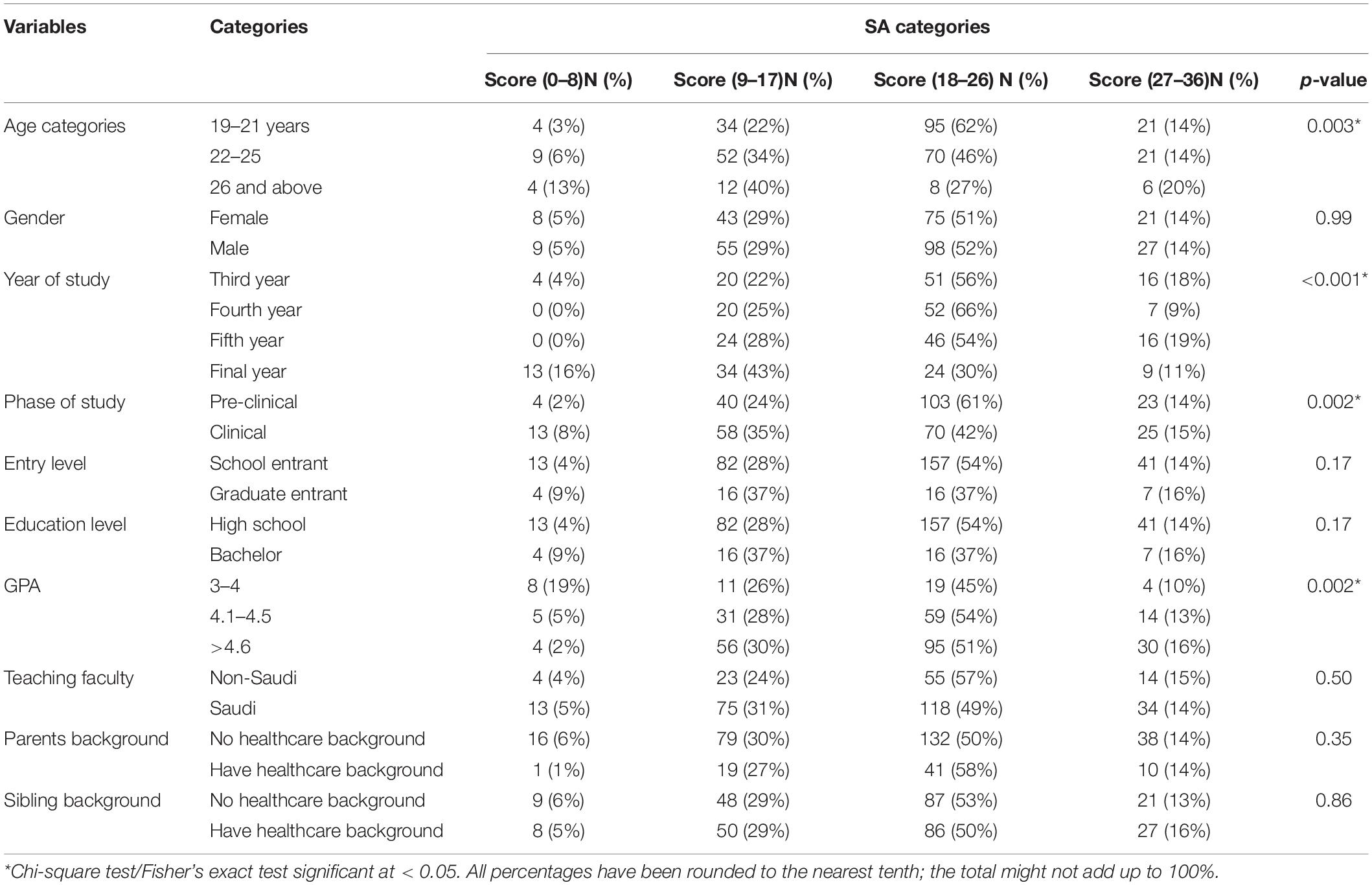
The demographic variables, age, year, phase of the study, and GPA were significantly associated with medical Students’ perception of SA. Most students scored highest in the 18–26 range, reflecting a good SA level. Within this scoring range, younger students were more likely to have better perception as the 19–21-year-old group had the highest score of 95 (62%), followed by the 22–25-year-old group (70, 46%) (χ2 = 19.6, p = 0.003). The preclinical year students (103, 61%), particularly fourth-year students [52 (66%)], were also significantly reporting the perceived SA within this range compared to clinical year students (χ2 = 40.4, p = 0.002) (χ2 = 49.8, p < 0.001), respectively. Moreover, 59 (54%) students who reported a GPA between 4.1 and 4.5 scored between 18 and 26 compared to other groups (χ2 = 22.1, p-value = 0.002). Other variables, including gender, education level, teaching faculty, and the presence of parents or sibling healthcare background, had no significant association with the perceived SA of medical students (Table 3).
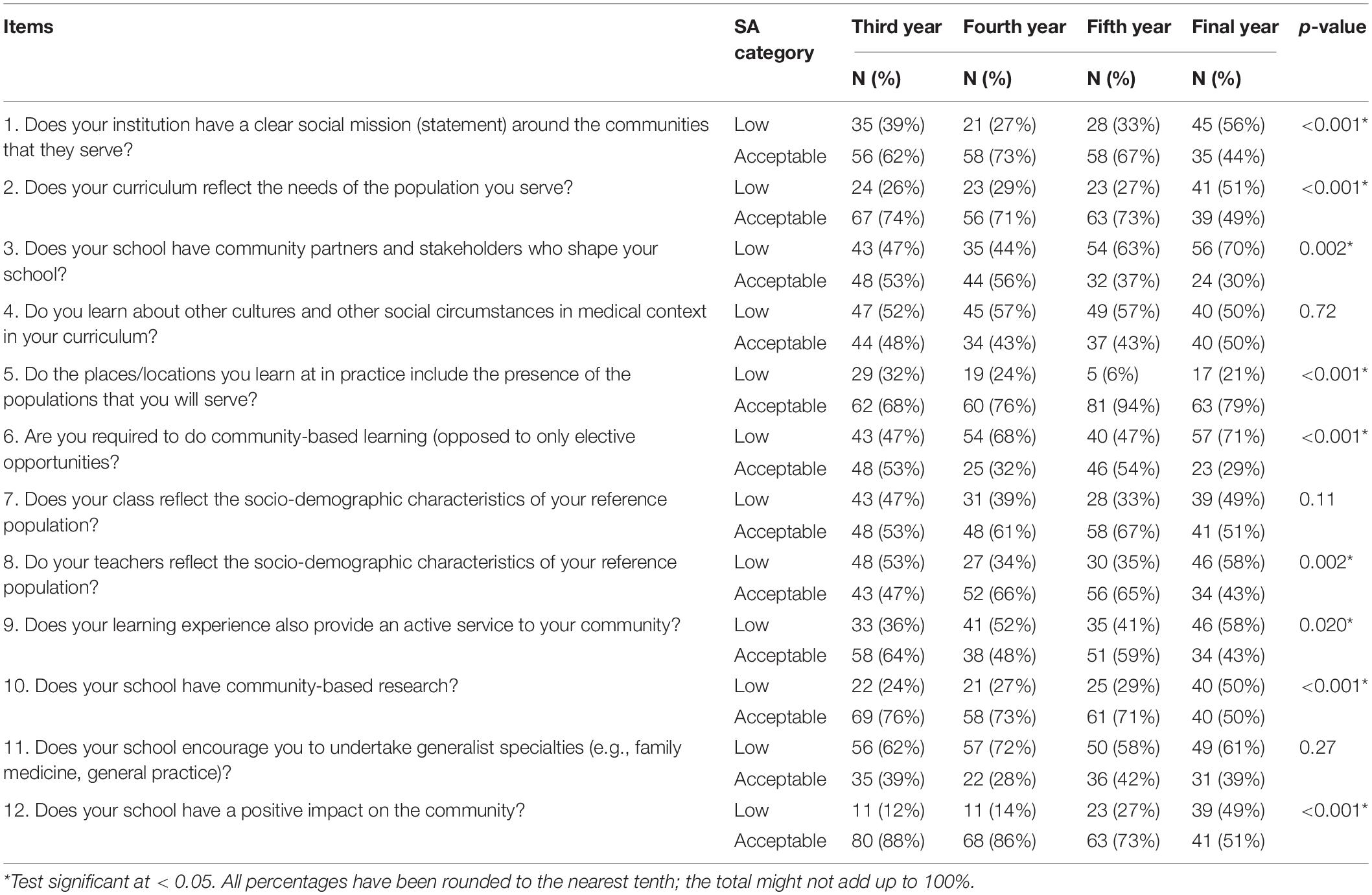
Each of the 12-item assessing SA was checked with the year of study to measure associations. It was found that 9 out of 12 items were significantly associated with the year of study. Item 5 had the highest reported good SA among year 5- and final-year students: 81 (94%) and 63 (79%) (χ2 = 18.9, p < 0.001). Moreover, item 9 revealed that third-year students scored the highest in the category of good SA [58 (64%)], whereas final-year students scored the lowest [34 (43%)] (χ2 = 9.8, p = 0.02). For item 10, students in their final year reported the lowest perceived SA (40, 50%), while the other years reported better perception of their school SA with a similar response rate (χ2 = 15.8, p < 0.001). Finally, item 12 showed that both third- and fourth-year students scored the highest in the good perception of the school SA [80 (88%) and 68 (86%)], respectively (χ2 = 37.4, p < 0.001) (Table 4).
Discussion
The research was conducted to understand the SA from the Students’ perspective. Additionally, the association of gender and year of the study with the perceived SA was considered during the research. Results showed that the KSAU-HS medical students perceived their institution as a good, socially accountable institution. No statistically significant differences were noted among male and female students who study at two separate campuses within the same institution. The variation across different years of study with the acceptability of the institution’s SA was also noted.
In Saudi Arabia, almost all medical colleges have segregated male and female campuses. The teaching staff at male campuses is predominantly male and vice versa at the female campus. Yet, in our study, no such differences across gender were noted with the perceived SA. The role of the teaching staff is crucial in developing SA among students. The presence of socially responsible teaching faculty has a significant impact on medical programs progressing toward being fully socially accountable with community-oriented health services. This also ensures higher deployment and consistent retention of healthcare workers in rural or remote areas (Elsanousi et al., 2016). Similarly, the role of gender is also considered an important variable affecting the perception of SA (Alghamdi, 2014).
One of the notable findings of the study was the highest mean score associated with the item evaluating the location of the medical practice and the future posting preference of medical students. The result can be associated with the core of KSAU-HS mission, which is to graduate qualified physicians for community services and promote the concept of SA (Mission Vision and Strategic Goals, 2022). COM offers volunteering opportunities at multiple levels to meet this goal, such as volunteering in the Saudi red crescent authority, the Hajj volunteer program, and a mandatory summer elective course. Hence, allowing the students to be engaged and familiarized with the intended population and well-equipped for serving the community. Dharamsi et al. (2010) also support the effect of community placements in cultivating a sense of SA among students. A recent study conducted in Morocco showed similar results and reported that students who do social services perceived a better perception of SA (Sebbani et al., 2021). It is believed that engaging students in community-based learning sites representing the actual population ensure the acquisition of well-defined competencies for more efficient health service delivery and encourage medical students to feel their school impact on the community and, thereby, improve their perceived SA (Boelen, 2016; Clithero et al., 2017; Roughead et al., 2017; Woolley et al., 2019).
An interesting finding of the study was that students perceived the school did not promote general specialties, such as family medicine and general practice (GP). The finding was supported by another study conducted at KSAU-HS in which two-thirds of the medical students refrained from choosing a general specialty as a future career option (Alshammari et al., 2019). Unlike our study population, medical students from universities in the United Kingdom were more inclined toward opting for GP as a future specialty for practices (Alshammari et al., 2019; Henderson et al., 2020). The National Health System in the United Kingdom has integrated GP within the community at advanced levels, leading to higher earning potential and relatively easily manageable expertise compared to doctors working in other specialties (Henderson et al., 2020). The Saudi Commission for Health Specialties has urged medical colleges to align the curriculum with the newly implemented Saudi MED framework, focusing on the priority health needs of the Saudi population and society (Tekian and Al Ahwal, 2015). Therefore, similar strategic reforms to the United Kingdom may be instilled in Saudi medical colleges and healthcare setup to strengthen SA. Having said that, further research is required to understand the impact of other exogenous social factors such as lifestyle and luxuries on perceived SA among students. As the primary health setups are predominantly in the country’s rural areas, choosing a GP position in rural areas could be a hard decision for many young practitioners (Henderson et al., 2020). Individual motivation and commitment to service is considered as one of the factors that can increase SA among students (Mohammadi et al., 2020).
For the overall level of SA among our study, most participants scored within the range of 18–26 across all the survey questionnaires, indicating signs of weaknesses, despite the school’s improved efforts. The junior students revealed better and positive perceptions about school’s SA compared to final-year students. Similar findings were reported by a study at Qassim University. The higher rates of burnout syndrome and depression were associated with Students’ progression through the medical school, impacting the clinical phased Students’ perception of their school’s SA (Alkhamees et al., 2020). Besides a higher prevalence of burnout syndrome in senior students, depression can also affect their perception of the survey items (Pacheco et al., 2017).
For most items, the academic year of study was significantly associated with the level of Students’ perceptions of their school’s SA. An acceptable reason behind the senior Students’ high scores in the fifth item, which evaluates the presence of the targeted population to be served at Students’ practice sites, is that students start their hospital rotations during fourth and final academic years. In clinical years, learning becomes more patient-oriented, unlike third and fourth years, where most of the learning takes place in the college. Item 9, which assesses whether the learning experience is providing active service to the community, is evaluated through the availability of opportunities for students to create health promotion projects supported by the university faculty that target the community. One example is the “Yakfeek Sharraha” campaign conducted in 2019 by students with support from the university. This project aimed to raise community awareness about motor vehicle accidents and the role of different surgical specialties in saving lives (College Of Medicine Riyadh-Home, 2022). Another awareness campaign was educating the public and correcting the common misconceptions on what to do in emergencies. Thus, community-centered initiatives and the school’s contribution to the community it serves may play a pivotal role in promoting SA amongst medical students (Boelen, 2016; Boelen et al., 2016).
Item 10 of the SA questionnaire focused on evaluating the role of research in the university, whereas item 12 primarily evaluated university’s impact and engagement with the community. On the research front, medical research course is mandatory during the third and fourth academic years at COM. This ensures that students take initiative to conduct research in different priority areas set by the institution on yearly basis. As the medical research course is conducted during the preclinical years, this explains the significantly lower SA acceptance among the fourth- and final-year students in the research domain. Furthermore, the community engagement of the university was assessed through two parts, namely, first, the encouragement of scientific research through the number of publications and Students’ participation in conferences; and second, supporting students to adapt and engage in various community-based activities results in developing a positive landscape of the university among people. At KSAU-HS, the university Student’s club encourages students to engage in various activities to improve their skills and abilities, promote their social responsibility, and provide the maximum benefit to the community. Each college in the university has a student club, including a social team responsible for educating and raising the community’s health awareness through campaigns. Prioritizing the research based on the population’s needs is one of the ways that can successfully improve SA of an institution (Strasser et al., 2013; Ahmed et al., 2020).
Despite the comprehensiveness of this research for capturing the perceptions around SA in medical universities in Saudi Arabia, there were certain limitations to the study approach. The mode of data collection was altered from a face-to-face self-administered approach to an Internet-based survey approach, which may have affected the study results. Additionally, the reporting bias may have affected the overall perception of the medical students. Single-institution-based survey can also limit the generalizability of the results to other medical colleges. Notwithstanding the limitations, efforts were made during the design phase to avoid the over- or underrepresentation of the participants through quota sampling, which is one of the strengths of this study. Our study participants represent the views of students studying in a public university. The private medical universities in Saudi Arabia are only a few; therefore, the results of the study can be generalized to most of the public medical universities.
Going forward, SA is a complex phenomenon and has different aspects that need more advanced understanding. One strategy for all the studying batches of students might not be applicable in medical colleges since each year has its own specific needs. Future research is required to further explore institutional-based evaluation models to identify well-defined indicators for improving SA among students. Additionally, a qualitative research study can also provide meaningful insight into understanding SA from a Student’s perspective. This may help identify the areas for improvement and reinforce the institutional strategy in meeting ideal SA principles.
To summarize, there is an urgent need to integrate SA approaches into healthcare delivery by medical schools and aid the establishment of a more relevant, equitable, high-quality, and cost-effective healthcare system at Saudi Arabia’s medical schools. Additionally, with the changing global dynamics of health as witnessed in the recent pandemic, medical schools must also be ready to adapt to the rapidly changing demand of their community (Minter et al., 2021; Papapanou et al., 2021). That might require more frequent changes to the existing modes of improving SA than expected as the students move along their growth trajectory.
Conclusion
The study concludes that one-third of the medical students had an overall low perceived SA. It was noted that the acceptability of SA varied across different years based on the individual items among preclinical and clinical year students. Therefore, the institution needs to focus its interventions based on the needs of preclinical and clinical year students accordingly. As final-year students were more critical, it is recommended that they require more attention to improve the acceptability of SA. The university should focus specifically on the needs of the graduating final-year students to meet the aim of socially accountable institutions meeting the need of their nation. It is recommended that the graduating students be provided sufficient exposure and spend an adequate length of time in community-based placements during clinical rotations. This can be an opportunity to enhance the overall perceived level of SA of medical institutions among the community and medical students.
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The data are not publicly available due to institutional policies of maintaining the confidentiality of the student data.
Ethics Statement
The studies involving human participants were reviewed and approved by the King Abdullah International Medical Research Centre, Riyadh, Saudi Arabia. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
NM contributed to conceptualization, proposal development, formal analysis and result interpretation, manuscript revision, and finalization for submission to the journal and general supervision as a senior member of the team. SA, OA, DAg, RA, and DAb contributed equally to proposal development and literature review, data acquisition, data cleaning and management, and manuscript writing and editing as junior research team members. SA-N contributed to study designing, data checking, result interpretation, manuscript editing, and technical revision and project management as a senior member. All authors have read and approved the final version of the manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We would like to thank all the participants who took out time and provided their valuable contributions to this project. We would also like to thank research unit faculty members for their support during the design and conception of this research.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/feduc.2022.868245/full#supplementary-material
References
Ahmed, M. H., Abdalla, M. E., and Taha, M. H. (2020). Why social accountability of medical schools in Sudan can lead to better primary healthcare and excellence in medical education? J. Fam. Med. Primary Care 9, 3820–3825. doi: 10.4103/jfmpc.jfmpc_498_20
Alghamdi, F. (2014). Saudisation and Women’s Empowerment Through Employment in the Health Care Sector, Master’s Thesis. Wellington: Victoria University of Wellington.
Alkhamees, A. A., Alaqil, N. S., Alsoghayer, A. S., and Alharbi, B. A. (2020). Prevalence and determinants of burnout syndrome and depression among medical students at Qassim University, Saudi Arabia. Saudi Med. J. 41, 1375–1380. doi: 10.15537/smj.2020.12.25427
Alrebish, S. A., Taha, M. H., Ahmed, M. H., and Abdalla, M. E. (2020). Commitment towards a better future for medical education in Saudi Arabia: the efforts of the college of medicine at Qassim University to become socially accountable. Med. Educ. Online 25:1710328. doi: 10.1080/10872981.2019.1710328
Alshammari, S. K., Altulaihi, B. A., Alghamdi, H. S., Alanazi, A. M., Alhazzaa, S. M., and Alanazi, R. K. (2019). Attitude of medical students at King Saud Bin Abdulaziz University for Health Sciences toward family medicine as a future specialty. J. Family Community Med. 26, 221–226. doi: 10.3389/fpubh.2017.00026
Beck, L., Mendel, T., and Thindwa, J. (2007). The Enabling Environment for Social Accountability in Mongolia. Washington, DC: The World Bank.
Boelen, C. (2016). Why should social accountability be a benchmark for excellence in medical education? Educ. Meìd. 17, 101–105. doi: 10.4103/jfmpc.jfmpc_498_20
Boelen, C., Heck, J. E., and World Health Organization (1995). Defining and Measuring the Social Accountability of Medical Schools (No. WHO/HRH/95.7). Geneva: World Health Organization.
Boelen, C., Pearson, D., Kaufman, A., Rourke, J., Woollard, R., Marsh, D. C., et al. (2016). Producing a socially accountable medical school: AMEE Guide No. 109. Med. Teach. 38, 1078–1091. doi: 10.1080/0142159X.2016.1219029
Clithero, A., Ross, S. J., Middleton, L., Reeve, C., and Neusy, A. (2017). Improving community health using an outcome-oriented CQI approach to community-engaged health professions education. Front. Public Health 5:26. doi: 10.3389/fpubh.2017.00026
College Of Medicine Riyadh-Home (2022). College of Medicine Riyadh - Home. Available online at: https://www.ksau-hs.edu.sa/English/Colleges/com/Riyadh (accessed January 7, 2022).
Dharamsi, S., Espinoza, N., Cramer, C., Amin, M., Bainbridge, L., and Poole, G. (2010). Nurturing social responsibility through community service-learning: lessons learned from a pilot project. Med. Teach. 32, 905–911. doi: 10.3109/01421590903434169
Dijk, S., Pálsdóttir, B., Ross, S. J., Bhiri, M., Ramalho, R., Glasner, J., et al. (2017). Students’ Toolkit on Social Accountability in Medical Schools. Amsterdam: IFMSA.
El-Naggar, M. M., Ageely, H., Salih, M. A., Dawoud, H., and Milaat, W. A. (2017). Developing an integrated organ/system curriculum with community-orientation for a new medical college in Jazan, Saudi Arabia. J. Fam. Community Med. 14, 127–136.
Elsanousi, S., Elsanousi, M., Khalafallah, O., and Habour, A. (2016). Assessment of the social accountability of the faculty of medicine at University of Gezira, Sudan. East Mediterr. Health J. 22, 258–266. doi: 10.26719/2016.22.4.258
Emadzadeh, A., Moonaghi, H. K., Bazzaz, M. M., and Karimi, S. (2016). An investigation on social accountability of general medicine curriculum. Electron. Physician 8, 2663–2669. doi: 10.19082/2663
Galukande, M., Nakasujja, N., and Sewankambo, N. K. (2012). Social accountability: a survey of perceptions and evidence of its expression at a Sub Saharan African University. BMC Med. Educ. 12:96. doi: 10.1186/1472-6920-12-96
GCSAMS (2010). Global Consensus for Social Accountability of Medical Schools. Available online at: https://healthsocialaccountability.sites.olt.ubc.ca/files/2011/06/11-06-07-GCSA-English-pdf-style.pdf (accessedApril 18, 2022).
Henderson, E., Berlin, A., and Fuller, J. (2020). Attitude of medical students towards general practice and general practitioners. Br. J. Gen. Pract. 52, 359–363.
Hosny, S., Ghaly, M., and Boelen, C. (2015). Is our medical school socially accountable? The case of Faculty of Medicine, Suez Canal University. Med. Teach. 37, S47–S55. doi: 10.3109/0142159X.2015.1006600
McCrea, M. L., and Murdoch-Eaton, D. (2014). How do undergraduate medical students perceive social accountability? Med. Teach. 36, 867–875. doi: 10.3109/0142159X.2014.916784
Minter, D. J., Geha, R., Manesh, R., and Dhaliwal, G. (2021). The future comes early for medical educators. J. Gen. Intern. Med. 36, 1400–1403. doi: 10.1007/s11606-020-06128-y
Mission, Vision and Strategic Goals (2022). Mission, Vision & Strategic Goals. Available online at: https://com.ksau-hs.edu.sa/index.php/2015-10-29-08-06-32/2015-10-29-07-51-40 (accessed January 7, 2022).
Mohammadi, M., Bagheri, M., Jafari, P., and Bazrafkan, L. (2020). Motivating medical students for social accountability in medical schools. J. Adv. Med. Educ. Prof. 8, 90–99. doi: 10.30476/jamp.2020.84117.1128
Pacheco, J. P., Giacomin, H. T., Tam, W. W., Ribeiro, T. B., Arab, C., Bezerra, I. M., et al. (2017). Mental health problems among medical students in Brazil: a systematic review and meta-analysis. Braz. J. Psychiatry 39, 369–378. doi: 10.1590/1516-4446-2017-2223
Papapanou, M., Routsi, E., Tsamakis, K., Fotis, L., Marinos, G., Lidoriki, I., et al. (2021). Medical education challenges and innovations during COVID-19 pandemic. Postgrad. Med. J. 2021:140032. doi: 10.1136/postgradmedj-2021-140032
Roughead, T., Gill, H., Dewar, K., Kasteel, N., and Hamilton, K. (2017). The Need for social accountability in medical school education: a tale of five students’ integration into vancouver’s downtown eastside. Univ. Ottawa J. Med. 7, 1–3. doi: 10.18192/uojm.v7i1.1512
Sebbani, M., Adarmouch, L., Mansouri, A., and Amine, M. (2021). Social accountability: attitudes and awareness among undergraduate medical students in Morocco. J. Adv. Med. Educ. Prof. 9, 1–7. doi: 10.30476/jamp.2020.87197.1298
Strasser, R., Hogenbirk, J. C., Minore, B., Marsh, D. C., Berry, S., Mccready, W. G., et al. (2013). Transforming health professional education through social accountability: Canada’s Northern Ontario School of Medicine. Med. Teach. 35, 490–496. doi: 10.3109/0142159X.2013.774334
Tekian, A. S., and Al Ahwal, M. S. (2015). Aligning the SaudiMED framework with the National Commission for Academic Accreditation and Assessment domains. Saudi Med. J. 36, 1496–1497. doi: 10.15537/smj.2015.12.12916
Ten Cate, O. (2017). Competency-based postgraduate medical education: past, present and future. GMS J. Med. Educ. 34:Doc69. doi: 10.3205/zma001146
The Association of Faculties of Medicine of Canada [AFMC] (2022). Social Accountability | AFMC. Available online at: https://www.afmc.ca/en/priorities/social-accountability (accessed January 7, 2022).
Keywords: medical students, medical schools, social accountability, social responsibility, medical education
Citation: Masud N, Alenezi S, Alsayari O, Alghaith D, Alshehri R, Albarrak D and Al-Nasser S (2022) Social Accountability in Medical Education: Students’ Perspective. Front. Educ. 7:868245. doi: 10.3389/feduc.2022.868245
Received: 02 February 2022; Accepted: 29 April 2022;
Published: 09 June 2022.
Edited by:
Andres Eduardo Gutierrez Rodriguez, Monterrey Institute of Technology and Higher Education (ITESM), MexicoReviewed by:
Mohamed Hassan Taha, University of Sharjah, United Arab EmiratesAmmar Ahmed Siddiqui, University of Hail, Saudi Arabia
Copyright © 2022 Masud, Alenezi, Alsayari, Alghaith, Alshehri, Albarrak and Al-Nasser. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Nazish Masud, bmF6aXNobXNkQGdtYWlsLmNvbQ==; bWFzdWRuQGtzYXUtaHMuZWR1LnNh
 Nazish Masud
Nazish Masud Shahad Alenezi
Shahad Alenezi Ohoud Alsayari
Ohoud Alsayari Deemah Alghaith
Deemah Alghaith Rana Alshehri
Rana Alshehri Danah Albarrak
Danah Albarrak Sami Al-Nasser1,2
Sami Al-Nasser1,2