- 1Department of Health Management and Policy, School of Public Health, University of Michigan, Ann Arbor, MI, United States
- 2Department of Psychiatry, School of Medicine, Michigan Medicine, University of Michigan, Ann Arbor, MI, United States
- 3Department of Health Policy and Management, Fielding School of Public Health, University of California, Los Angeles, Los Angeles, CA, United States
- 4School of Social Work, University of Michigan, Ann Arbor, MI, United States
- 5Department of Psychiatry, Columbia University Irving Medical Center/New York State Psychiatric Institute, New York, NY, United States
- 6Department of Learning Health Sciences, School of Medicine, University of Michigan, Ann Arbor, MI, United States
- 7Quality Enhancement Research Initiative (QUERI), United States Department of Veterans Affairs, Washington, DC, United States
School professionals (SPs) are increasingly tasked with providing mental health treatment for students. Successful implementation of school-based mental health evidence-based practices (EBPs) can reduce students’ depression and anxiety, but requires identification of appropriate students to benefit from these interventions. We examined the ability of SPs to identify students appropriate for cognitive behavioral therapy (CBT), using baseline data collected from a large-scale implementation trial. One hundred sixty-nine SPs from 94 Michigan high schools were asked to identify up to 10 students whom they believed could benefit from CBT. Identified students were asked to complete a baseline survey. We examined the proportion of consented students who screened positive for depression or anxiety, based on the Patient Health Questionnaire modified for teens and the Generalized Anxiety Disorder questionnaire, overall and by key school- and SP-level factors. Of the 1,347 students identified by 149 SPs, 899 students completed the survey. Of those students, 87% exhibited any depression or anxiety symptoms (score of five or higher) and 66% showed moderate/severe symptoms (score of ten or higher). Per SP, the proportion of consented students who screened positive for any depression or anxiety symptoms was, on average, 0.88. The effectiveness of SPs’ student identification did not vary significantly by school-specific role, prior CBT training, or geography. Results suggest that SPs can effectively identify students appropriate for CBT given minimal training and resources, an important first step in increasing student access to school-based mental healthcare.
Highlights
- School professionals (SPs) have the potential to play a crucial role in expanding adolescent access to evidence-based mental health treatment, but little is known about their ability to identify students who may be in need of clinical intervention.
- After receiving web-based toolkits and attending a 1-day training in CBT, SPs identified a diverse array of students (65% female, 28% non-White) whom they believed could benefit from CBT; nearly 90% of identified students screened positive for clinically significant depression or anxiety.
- Successful SP identification of students appropriate for CBT did not differ significantly by SP role, prior training in CBT, or school geography.
Introduction
Schools provide promising venues for increasing adolescents’ access to evidence-based practices (EBPs) for mental health disorders (Stephan et al., 2007; Beidas et al., 2012; Lyon et al., 2013; Sanchez et al., 2018; Koschmann et al., 2019). At least one in five adolescents experience mental health disorders, including depression and anxiety (Kessler et al., 2001; Merikangas et al., 2010), and mental health challenges among children and adolescents have further increased as a result of the COVID-19 pandemic (American Academy of Pediatrics, 2021; Racine et al., 2021). Depression and anxiety in youth can impair both academic and social functioning, and lead to increased substance abuse, hindering both students’ short-term academic success and their long-term quality of life (Pine et al., 1998; Comeau et al., 2001; Kessler et al., 2001). However, youth access to effective and evidence-based mental healthcare remains low, especially when accessed in settings outside of school, due to various barriers including stigma, cost, inconvenience, transportation, and time/cost intensive systems for identifying and referring students to treatment (Kataoka et al., 2002; Merikangas et al., 2011; Reardon et al., 2017; Kilbourne et al., 2018; Radez et al., 2021). School-based mental healthcare provides an encouraging option, as schools alleviate many of these barriers to accessing care (Kern et al., 2017; Ali et al., 2019). While less than 20% of youth have access to mental healthcare, 35–50% of adolescents receiving help do so within the school setting (Weist et al., 2007; Green et al., 2013; Duong et al., 2020), indicating that increasing school-based mental health access holds promise for reaching students in need of care.
Despite the increasingly important role of school-based mental healthcare, it is not yet widespread and schools still often struggle to provide adequate and timely mental health services to students (Stephan et al., 2007; Bruns et al., 2016). Cognitive Behavioral Therapy (CBT), an evidence-based, effective treatment for prominent student mental health concerns including anxiety and depression, is one example of a mental health EBP appropriate for delivery in a school setting (Spirito et al., 2011; Higa-McMillan et al., 2016; Haugland et al., 2020). However, numerous barriers and challenges have limited the implementation of EBPs such as CBT in schools (Rones and Hoagwood, 2000; Forman et al., 2008; Beidas et al., 2012), including a lack of administrative support and a lack of resources and/or trainings in EBPs that are affordable and easily available for school professionals (SPs) to access (Evans et al., 2005; Bruns et al., 2016; Kern et al., 2017). Difficulties accurately detecting and reaching students who would most benefit from EBPs are other challenges facing EBP delivery in schools (Masia Warner and Fox, 2012; Koschmann et al., 2019). For effective school-based delivery of EBPs like CBT, the identification of appropriate students for an intervention is required. Efforts have increasingly been made to train SPs and implement mental health EBPs like CBTs in schools (Beidas et al., 2012; Masia Warner et al., 2016; Kilbourne et al., 2018), but little is known regarding SPs’ effectiveness in identifying and reaching students with mental disorders (Scott et al., 2009; Cunningham and Suldo, 2014).
Early identification of youth mental health challenges, such as anxiety and depression, can be crucial in the prevention and early treatment of these illnesses—helping to alter the course of these mental health disorders and to lessen their burden over time (Stiffler and Dever, 2015). Given the high prevalence of anxiety and depression in adolescents, and the barriers to accessing care in other settings, schools have been identified as one ideal location for early identification (Stiffler and Dever, 2015; Humphrey and Wigelsworth, 2016; Burns and Rapee, 2021). Early identification efforts within the school setting can take on different forms and may range from administering universal screening measures to all students, to having teachers refer students to school mental health professionals for care (Stiffler and Dever, 2015; Burns and Rapee, 2021). Each of these procedures has advantages and disadvantages, with proponents of universal screening noting the reduction in racial and gender bias in referrals, as well as reduced reliance on observations of externalizing behavior to identify appropriate students. However, early identification efforts can be daunting to students and the system (Stiffler and Dever, 2015). For example, even when schools have developed protocols for student referrals to mental health services, they often do not have streamlined procedures in place for identifying students who need mental healthcare and/or can benefit from early intervention (Evans et al., 2005; Allison et al., 2014; Husabo et al., 2020). Moreover, common providers of mental healthcare in schools, including school counselors, school social workers, school psychologists, or school nurses, are often constrained by limited time to work with mental health issues due to many other competing responsibilities, as well as a large number of students assigned to their caseloads due to the shortage of SPs across schools (Flaherty et al., 1998; Evans et al., 2005; Langley et al., 2010; Lambie et al., 2019). Many SPs also lack specialized training or access to resources, including appropriate screening tools, to identify the students who could benefit most from mental health EBPs (Weist et al., 2007; Burns and Rapee, 2021).
Addressing these barriers is an important step toward increasing student access to mental healthcare. The present study sets out to understand the feasibility of increasing student access to EBPs in the school setting through proper identification of students by SPs. Using a subset of baseline data collected from a large-scale implementation trial of school-based CBT, we explored how effective SPs were at identifying students with depression and anxiety. Objectives of this study are:
• To understand whether SPs were able to appropriately identify students for CBT; and
• To examine whether SPs’ student identification success differed by SP- or school-level characteristics.
This examination of SPs’ effectiveness in identifying appropriate students for CBT will further our understanding on one of the first steps for implementing high quality mental health interventions in school settings.
Methods
We explored SPs’ identification of students with depression and anxiety in the context of a state-wide implementation trial—the Adaptive School-based Implementation of CBT (ASIC) Study. A detailed study description and data collection processes can be found elsewhere (Kilbourne et al., 2018). In brief, ASIC compares the effectiveness of different implementation strategies on SP-delivered CBT in Michigan high schools and downstream student mental health outcomes. The study was approved by the University of Michigan Institutional Review Board.
Between May and November 2018, SPs at Michigan high schools were recruited to participate in ASIC and asked to complete a baseline survey which included questions about their professional role and prior CBT experience. Prior to trial initiation, SPs were required to attend a 1-day didactic CBT training in January 2019, provided by an established school-focused training program, Transforming Research into Action to Improve the Lives of Students (TRAILS).1 TRAILS training was offered at several locations across Michigan and covered various strategies for identifying students who would benefit from CBT, CBT core components, and theoretical underpinnings. SPs were provided with a packet including information about CBT delivery, as well as detailed guidelines regarding best practices for identifying and recruiting students for CBT groups and standard screening tools for depression and anxiety. Specifically, SPs were given access to a document with information about student characteristics that might be a good fit for CBT groups (e.g., students who are engaged, who are likely to attend, who do not have significant cognitive delays, who can engage prosocially with peers, who would allow them to practice the new skills, etc.). SPs were also presented with the Patient Health Questionnaire-9, modified for teens (PHQ-9T) (Richardson et al., 2010) and the Generalized Anxiety Disorder-7 (GAD-7) (Spitzer et al., 2006), which they could choose to use or not, depending on their preference, when identifying students.
SPs participating in ASIC were asked to identify up to 10 students whom they believed might benefit from CBT using various strategies provided at training and to list them on the study’s data collection dashboard. As the ASIC study was carried out over two academic years, SPs were asked not to include seniors who would be graduating during the study in their lists. Identified students were given the opportunity to consent to ASIC participation. Students were informed that their participation was voluntary and their consent or refusal to participate would have no bearing on their ability to participate in SP-provided counseling. One week after the training, SPs finalized their list of students and helped administer a baseline student survey on behalf of the study. The student survey included questions about their access to mental health services, if any, and brief screening tools for depression and anxiety, the PHQ-9T and GAD-7.
Using both SP and student baseline survey data, we assessed SPs’ effectiveness in identifying students appropriate for CBT based on students’ responses to the PHQ-9T and GAD-7. The PHQ-9T is a self-administered 9-item depression screener modified for teens, which was originally developed for adults (Kroenke et al., 2001) and psychometrically validated among adolescents (Richardson et al., 2010; Allgaier et al., 2012). The GAD-7 is a self-reported 7-item screener for generalized anxiety symptoms, which was developed for adults in the primary care setting and validated among youth (Spitzer et al., 2006; Mossman et al., 2017). The continuous scores from the PHQ-9T and GAD-7 can be used for defining symptom severity (Spitzer et al., 2006; Guidelines for Adolescent Depression in Primary Care, Version 2, 2010). Successful identification of an “appropriate” student was defined and analyzed in this study in two ways: (a) screening for more conventional cutoffs identifying moderate to severe cases, or those who scored between 10 and 27 on PHQ-9T or between 10 and 21 on GAD-7 (Spitzer et al., 2006; Richardson et al., 2010) and (b) screening for any level of symptom severity, or those who scored five or more on PHQ-9T or on GAD-7, as CBT is considered appropriate for mild cases of depression and anxiety (Flynn and Warren, 2014; Gautam et al., 2020). For each SP, we computed their effectiveness in student identification, which was the proportion of the students who screened positive for depression and/or anxiety at baseline using PHQ-9T and GAD-7 scores, among the students identified and consented to the study. Further, bivariate tests of association, including a two-sample’s t-test and a one-way analysis of variance (ANOVA) with a post-hoc pairwise comparison using the Tukey’s-Kramer solution, were used to examine whether SPs’ identification of appropriate students differed by professional role (school counselors, school social workers, or other), prior CBT training [formal training (e.g., a graduate course), informal training (e.g., continuing education), or none], or school geography (rural vs. urban). P-values of 0.05 were used for significance testing and all analyses were conducted in Stata version 16.
Results
A total of 169 SPs at 94 schools (among 227 SPs at 115 schools who agreed to participate) attended a TRAILS 1-day training and were included in the study. Of 169 ASIC-participating SPs, 163 SPs (96%) completed the SP baseline survey; about half of SPs were from rural schools (49%), most of them had a graduate degree (93%), 38% reported no prior CBT experience, and SPs had been in their position for 8 years, on average (Standard deviation, SD = 7.8) (Table 1). A majority of SPs were school counselors (59%), followed by school social workers (24%), and other positions (17%) including school psychologist, behavioral intervention specialist, teachers, and other staff.
School professionals identified 1,347 students whom they believed might benefit from CBT, or 8 students each, on average. Twenty SPs (12%) failed to identify any students. Failure to identify any students was not associated with SPs’ professional role (X2 = 2.72, p = 0.26), prior experience with CBT (X2 = 2.47, p = 0.29), or school geography (X2 = 1.08, p = 0.30).
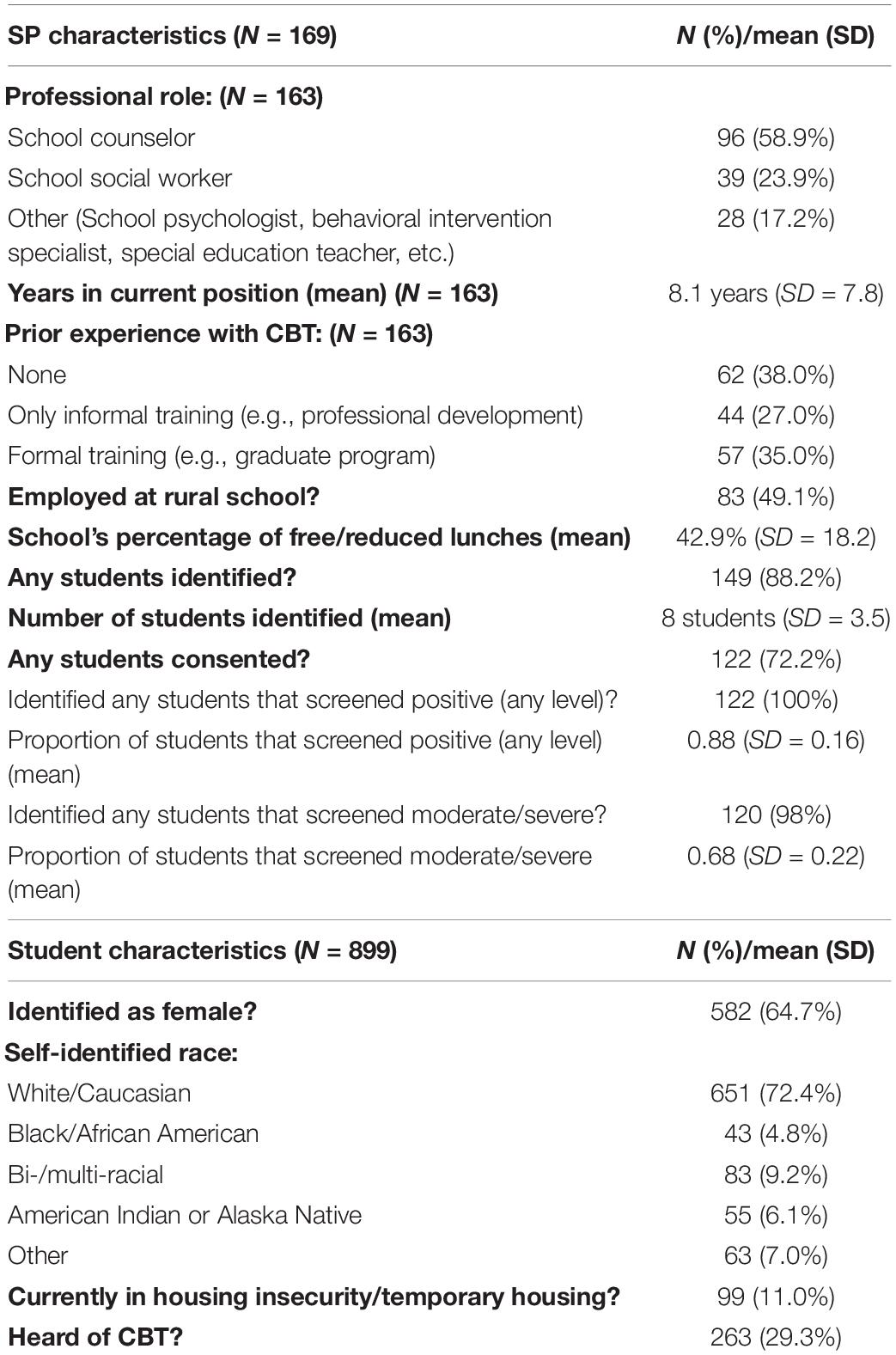
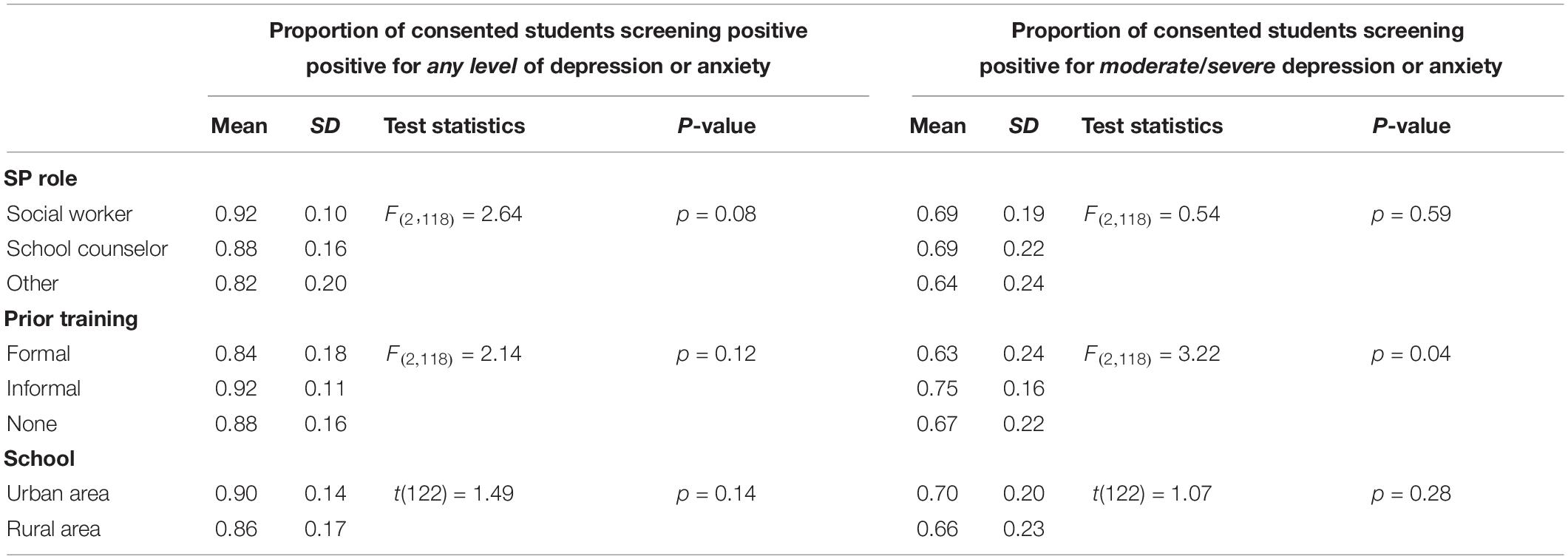
Of students identified by SPs, 899 students (67%) consented to participate in the study and completed the baseline surveys (Table 1). Those students were between 8th and 12th grade (8th grade: 2%, 9th: 25%, 10th: 40%, 11th: 33%, and 12th: 0.4%), 65% female, and 73% white. In terms of accessing mental healthcare resources over the past 6 months, 75% mentioned accessing school-based resources, 40% community-based resources and 28% healthcare-based resources. As shown in Figures 1 and 2, 87% of these students (N = 780) screened positive for any level of depression or anxiety, or scored five or more on the PHQ-9T and/or GAD-7, while 66% (N = 596) screened for moderate/severe depression or anxiety (scored ten or more) in these same measures.
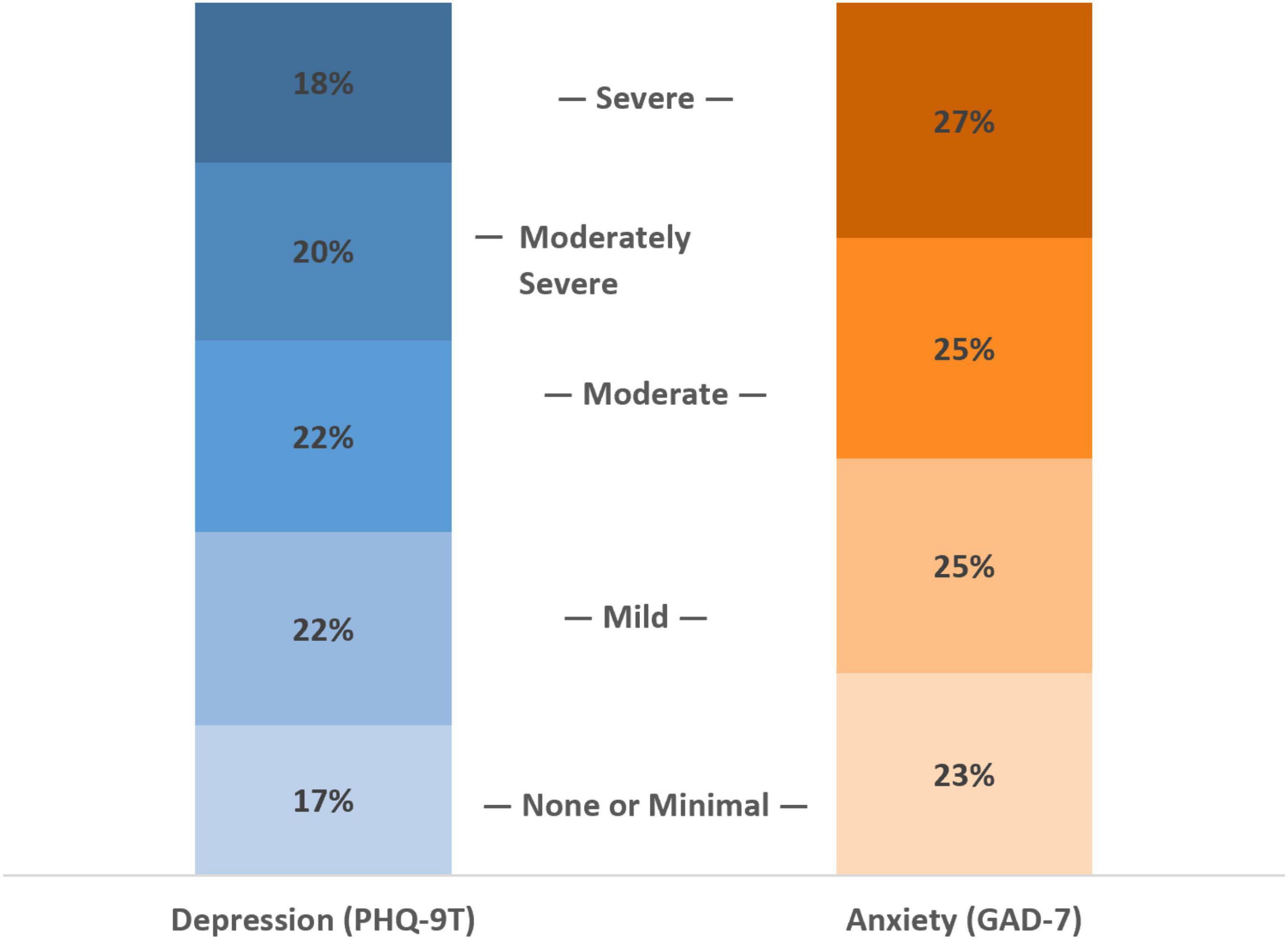
Figure 1. Prevalence of depression and anxiety among identified and consented students. Responses from student survey (N = 899). Depression symptoms were accessed using PHQ-9T, where the total score of 0–4 is considered no or minimal depression, 5–9 mild, 10–14 moderate, 15–19 moderately severe, and 20–27 severe depression. Anxiety symptoms were accessed using GAD-7, where the total score of 0–4 is considered as minimal anxiety, 5–9 mild, 10–14 moderate, and 15–21 severe anxiety.
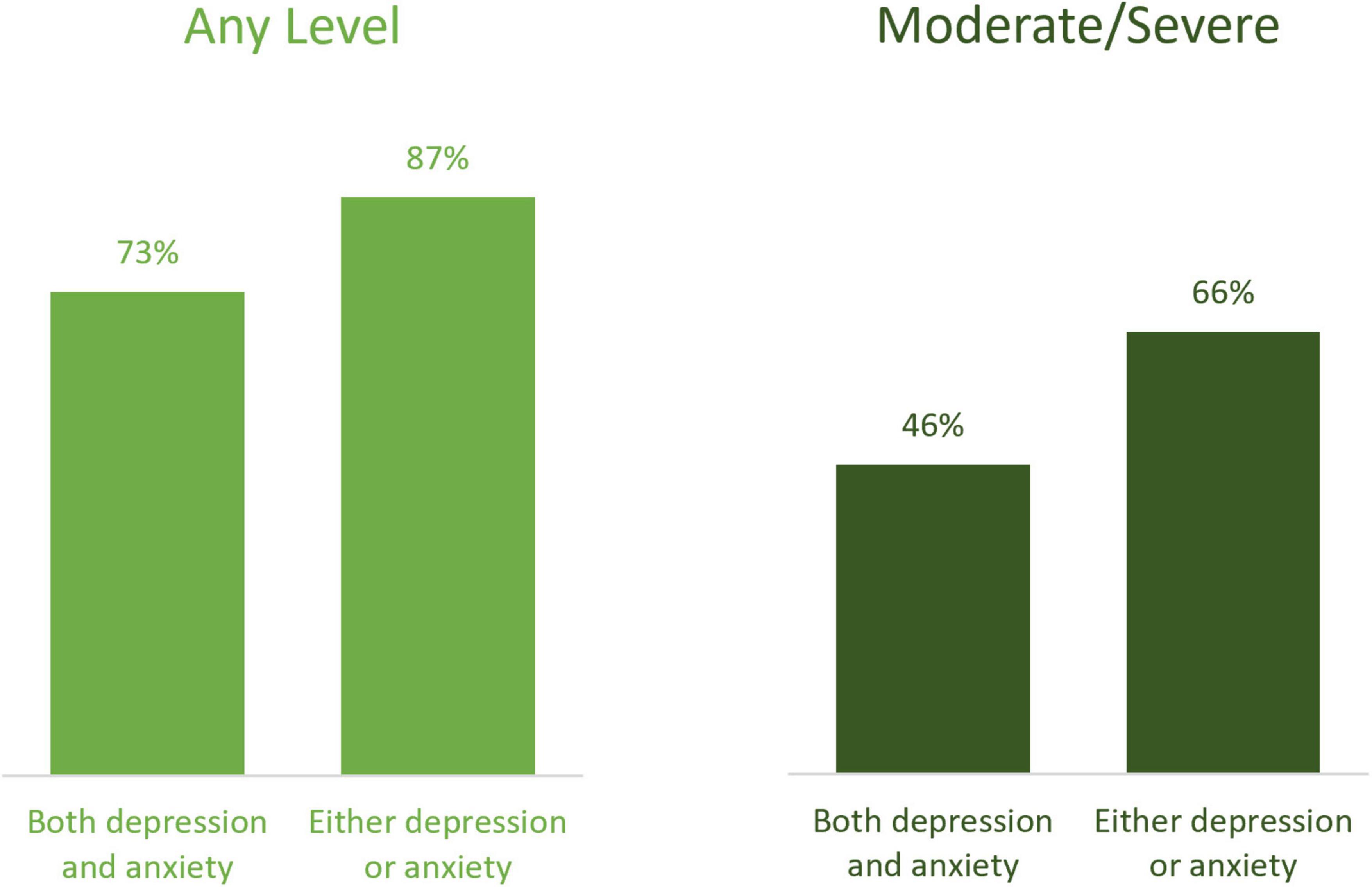
Figure 2. Depression and anxiety screening results among identified and consented students. Responses from student survey (N = 899). The left-side of the figure presents the percentage of students who exhibited any levels of symptoms, that is, mild/moderate/severe depression and/or anxiety symptoms (i.e., five or more total scores on PHQ-9T and/or GAD-7). On the right-side, it shows the percentages of students screened using conventional cutoffs, or those with moderate to severe symptoms (i.e., 10 or more total scores on PHQ-9T and/or GAD-7).
The 899 consented students were identified by 122 SPs at 71 schools. All 122 SPs identified at least one student with any level of depression or anxiety (scoring five or more on the PHQ-9T and/or GAD-7), and 120 SPs identified at least one student with moderate/severe symptoms. When the proportion of consented students who screened positive for any symptoms was computed for each of these 122 SPs, the average proportion was 0.88 (SD = 0.16); it was 0.68 (SD = 0.22) for moderate/severe symptoms (Table 1). That is, on average, 9 of 10 students identified by SPs were appropriate for CBT (screened for any level of symptoms); about 7 of 10 students identified by SPs showed moderate or severe symptoms. Of 122 SPs, 55 SPs (45%) had all consented students screen positive for any symptoms (i.e., the proportion of consented students who screened positive for any level equals one for 55 SPs), and 15 SPs (12%) had all students screen positive for moderate/severe symptoms.
We further examined if SPs’ effective identification of students varied by SP- or school-level characteristics. As summarized in Table 2, we found no evidence that identification of students with any symptoms varied by professional role, prior experience with CBT, or school location (rural vs. urban). For example, the proportion of identified students with mild or more symptoms per SP was not statistically different depending on school location [t(122) = 1.49, p = 0.14]. School social workers, compared to school counselors or other SPs, were slightly more likely to identify students with any level of symptoms (i.e., the mean proportion of students with any symptoms were 0.92, 0.88, and 0.82, respectively), but the difference was not statistically significant [F(2, 118) = 2.64, p = 0.08]. When it came to moderate/severe symptoms, the effectiveness of identification did also not vary by SPs’ professional role. Post-hoc pairwise comparisons found no statistically significant differences between SPs with different professional roles. However, SPs’ identification of students with moderate/severe symptoms did vary by SPs’ prior CBT experience: SPs with informal training had a slightly larger proportion of students with moderate/severe symptoms, compared to SPs with formal training or with no prior training (i.e., the average proportion of students with moderate/severe symptoms was 0.75 compared to 0.63 and 0.67, respectively, where F(2, 118) = 3.22, p < 0.05) (Table 2). Post-hoc pairwise comparisons found the difference between SPs with informal training and those with formal training statistically significant (95% CI = [0.02, 0.22], p = −0.015), while other two pairwise comparisons were not statistically significant.
Discussion
School-based delivery of EBPs may offer an efficient solution to meet mental health service needs created by high levels of depression and anxiety among youth facing numerous obstacles to treatment access. CBT offers a versatile treatment approach, as it is appropriate for both depression and anxiety (Chorpita et al., 2005; Chorpita and Daleiden, 2009), which are predominant among school age populations (Merikangas et al., 2010). To be effective in their service delivery, however, SPs need to first be able to accurately identify students with treatment needs and match them to the appropriate intervention. This study explored the identification of students by SPs who were offered information on how to screen students for depression or anxiety and a toolkit for helping SPs identify students appropriate for CBT at a 1-day training. The results suggest that SPs across a variety of training levels and experiences are capable of identifying appropriate students for a mental health EBP intervention when provided resources.
Following training, nearly 90% of SPs identified at least one student they felt appropriate for CBT and SPs were quite successful in detecting students with depression or anxiety. Among the students identified by SPs and that consented to the study, 66% screened positive for moderate to severe symptoms; 87% screened positive for some level of depression, anxiety, or both. Among students with some level of symptoms, the majority showed mild to moderate symptoms: 78% of students with some depression symptoms (579 out of 743 students) and 65% of students with some anxiety symptoms (447 out of 689 students) were in mild to moderate categories. This fits well with the treatment purview for SP-delivered CBT, which is flexible enough to address symptoms across a range of severity and presenting concerns, including both anxiety and depression (Spirito et al., 2011; Higa-McMillan et al., 2016; Haugland et al., 2020).
Successful identification of students appropriate for CBT did not appear to differ significantly by SPs’ professional role or prior CBT experience, although school social workers identified a slightly larger proportion of students with any level of symptoms compared to school counselors or other roles (0.92 vs. 0.88 and 0.82, respectively) and SPs with informal CBT training did a slightly better job in identifying students with moderate/severe symptoms compared to those with formal or no training (0.75 vs. 0.63 and 0.67, respectively). Even SPs who had no prior exposure to CBT successfully identified students deemed appropriate for CBT.
This study had several important limitations. First, while our response rate was quite high, students who did not complete the baseline survey were not screened for depression or anxiety. It is possible that students who were less likely to screen positive were also less likely to consent to the study, in which case rates of SPs’ successful identification would be lower than reported here. However, students were offered an incentive to participate in the study, and no specific mental health pre-conditions were referenced in the survey consent. Second, this study was completed as part of the run-in phase of an implementation trial that SPs opted to participate in. As such, participating SPs were likely more invested in youth mental health, including awareness of depressive and anxiety symptoms, and may not accurately represent the broader SP populations’ accuracy in identifying students appropriate for CBT. Third, although our baseline survey asked about prior experience with CBT, we did not ask about prior experience in screening or identifying students with anxiety or depression; as such we are not able to discern whether prior levels or experience or expertise in identifying such students or whether the training and toolkit were related to the appropriate identification of students for CBT. We also did not verify that SPs used the provided screening tools in their student identification. Finally, as this study only examines baseline scores, we are not able to examine whether the students who were identified benefitted from, or even participated in, the recommended CBT intervention. This was beyond the scope of this study, but will be examined in the broader implementation trial. Despite these limitations, the current study does shed light on SPs’ overall ability to identify students with anxiety and depressive symptoms, who are likely very appropriate for CBT.
While this study assures that SPs are appropriate means for the provision of student mental healthcare and can appropriately identify students that can benefit from school-based mental health programming, more knowledge regarding student identification will allow SPs to more effectually serve students in need. Further studies could explore how other tools for student identification, including universal screening, familial input on student psychological distress, collaboration with community resources providing care, or other sources, could be combined with current practices to further improve identification of students in need. Future work could also explore the difference in student identification regarding SP background and training to better support professional development opportunities that could facilitate improved student identification.
Conclusion
Successful implementation of school-based mental health EBPs is essential to reduce the burden of depression and anxiety among students, and rests on appropriate identification of students with clinically significant symptoms. The findings showed that, after minimal support and training, SPs at a diverse set of Michigan high schools were generally able to identify students with symptoms of depression and/or anxiety who could likely benefit from CBT. These findings offer new evidence of the potential for SPs to play a significant role in increasing access to evidence-based mental health services among youth who may otherwise not receive care, and thereby improving mental health, wellness, educational, and other critical outcomes among the large proportion of students impacted by mental illness.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors upon request, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by the University of Michigan Institutional Review Board. Written informed consent from the participants’ legal guardian/next of kin was not required to participate in this study in accordance with the national legislation and the institutional requirements.
Author Contributions
SC and SS contributed to the study aims and conception of the methods, and analyses of the manuscript. SC performed the analyses and wrote the preliminary manuscript. AR and AL contributed to the background section. AR and SS contributed the discussion section. EK, JA, DE, JH, KF, CL, and AK contributed to overarching research aims and goals, and reviewed and revised the manuscript. SC, AR, SS, and EB carried out major revisions of the manuscript. All authors approved of the final manuscript.
Funding
This work was supported by the National Institute of Mental Health (R01MH114203). TRAILS was supported by funds from the Centers for Medicare and Medicaid Services through the Michigan Department of Health and Human Services, the Michigan Health Endowment Fund, the Ethel and James Flinn Foundation, and other Michigan-based foundations.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Footnotes
References
Ali, M. M., West, K., Teich, J. L., Lynch, S., Mutter, R., and Dubenitz, J. (2019). Utilization of mental health services in educational setting by adolescents in the United States. J. Sch. Health 89, 393–401. doi: 10.1111/josh.12753
Allgaier, A.-K., Pietsch, K., Frühe, B., Sigl-Glöckner, J., and Schulte-Körne, G. (2012). Screening for depression in adolescents: validity of the patient health questionnaire in pediatric care. Depress. Anxiety 29, 906–913.
Allison, V. L., Nativio, D. G., Mitchell, A. M., Ren, D., and Yuhasz, J. (2014). Identifying symptoms of depression and anxiety in students in the school setting. J. Sch. Nurs. 30, 165–172. doi: 10.1177/1059840513500076
American Academy of Pediatrics (2021). AAP-AACAP-CHA Declaration of a National Emergency in Child and Adolescent Mental Health. Available online at: http://www.aap.org/en/advocacy/child-and-adolescent-healthy-mental-development/aap-aacap-cha-declaration-of-a-national-emergency-in-child-and-adolescent-mental-health/ (accessed October 26, 2021).
Beidas, R. S., Mychailyszyn, M. P., Edmunds, J. M., Khanna, M. S., Downey, M. M., and Kendall, P. C. (2012). Training school mental health providers to deliver cognitive-behavioral therapy. Sch. Ment. Health 4, 197–206. doi: 10.1007/s12310-012-9074-0
Bruns, E. J., Duong, M. T., Lyon, A. R., Pullmann, M. D., Cook, C. R., Cheney, D., et al. (2016). Fostering SMART partnerships to develop an effective continuum of behavioral health services and supports in schools. Am. J. Orthopsychiatry 86, 156–170. doi: 10.1037/ort0000083
Burns, J. R., and Rapee, R. M. (2021). Barriers to universal mental health screening in schools: the perspective of school psychologists. J. Appl. Sch. Psychol. [Ahead of Print], 1–18. doi: 10.1080/15377903.2021.1941470
Chorpita, B. F., and Daleiden, E. L. (2009). Mapping evidence-based treatments for children and adolescents: application of the distillation and matching model to 615 treatments from 322 randomized trials. J. Consult. Clin. Psychol. 77, 566–579. doi: 10.1037/a0014565
Chorpita, B. F., Daleiden, E. L., and Weisz, J. R. (2005). Modularity in the design and application of therapeutic interventions. Appl. Prev. Psychol. 11, 141–156. doi: 10.1016/j.appsy.2005.05.002
Comeau, N., Stewart, S. H., and Loba, P. (2001). The relations of trait anxiety, anxiety sensitivity, and sensation seeking to adolescents’ motivations for alcohol, cigarette, and marijuana use. Addict. Behav. 26, 803–825. doi: 10.1016/S0306-4603(01)00238-6
Cunningham, J. M., and Suldo, S. M. (2014). Accuracy of teachers in identifying elementary school students who report at-risk levels of anxiety and depression. Sch. Ment. Health 6, 237–250. doi: 10.1007/s12310-014-9125-9
Duong, M. T., Bruns, E. J., Lee, K., Cox, S., Coifman, J., Mayworm, A., et al. (2020). Rates of mental health service utilization by children and adolescents in schools and other common service settings: a systematic review and meta-analysis. Adm. Policy Ment. Health Ment. Health Serv. Res. 48, 420–439. doi: 10.1007/s10488-020-01080-9
Evans, D. L., Foa, E. B., Gur, R. E., Hendin, H., O’Brien, C. P., and Seligman, M. E. P., (eds). et al. (2005). Treating and Preventing Adolescent Mental Health Disorders: What We Know and What We Don’t Know: A Research Agenda for Improving the Mental Health of Our Youth. New York, NY: Oxford University Press.
Flaherty, L. T., Garrison, E. G., Waxman, R., Uris, P. F., Keys, S. G., Glass-Siegel, M., et al. (1998). Optimizing the roles of school mental health professionals. J. Sch. Health 68, 420–424. doi: 10.1111/j.1746-1561.1998.tb06321.x
Flynn, H. A., and Warren, R. (2014). Using CBT effectively for treating depression and anxiety: modify the elements of CBT to address specific anxiety disorders, patient factors. Curr. Psychiatry 13, 45–52.
Forman, S. G., Olin, S. S., Hoagwood, K. E., Crowe, M., and Saka, N. (2008). Evidence-Based Interventions in Schools: Developers’ Views of Implementation Barriers and Facilitators. Sch. Ment. Health 1:26. doi: 10.1007/s12310-008-9002-5
Gautam, M., Tripathi, A., Deshmukh, D., and Gaur, M. (2020). Cognitive behavioral therapy for depression. Ind. J. Psychiatry 62(Suppl. 2), S223–S229. doi: 10.4103/psychiatry.IndianJPsychiatry_772_19
Green, J. G., McLaughlin, K. A., Alegría, M., Costello, E. J., Gruber, M. J., Hoagwood, K., et al. (2013). School mental health resources and adolescent mental health service use. J. Am. Acad. Child Adolesc. Psychiatry 52, 501–510. doi: 10.1016/j.jaac.2013.03.002
Guidelines for Adolescent Depression in Primary Care, Version 2 (2010). The REACH Institute. Available online at: https://staff.aacap.org/App_Themes/AACAP/docs/member_resources/toolbox_for_clinical_practice_and_outcomes/symptoms/GLAD-PC_PHQ-9.pdf (accessed May 5, 2018).
Haugland, B. S. M., Haaland, ÅT., Baste, V., Bjaastad, J. F., Hoffart, A., Rapee, R. M., et al. (2020). Effectiveness of brief and standard school-based cognitive-behavioral interventions for adolescents with anxiety: a randomized noninferiority study. J. Am. Acad. Child Adolesc. Psychiatry 59, 552–564e2. doi: 10.1016/j.jaac.2019.12.003
Higa-McMillan, C. K., Francis, S. E., Rith-Najarian, L., and Chorpita, B. F. (2016). Evidence base update: 50 years of research on treatment for child and adolescent anxiety. J. Clin. Child Adolesc. Psychol. 45, 91–113. doi: 10.1080/15374416.2015.1046177
Humphrey, N., and Wigelsworth, M. (2016). Making the case for universal school-based mental health screening. Emot. Behav. Diffic. 21, 22–42. doi: 10.1080/13632752.2015.1120051
Husabo, E., Haugland, B. S. M., McLeod, B. D., Ogden, T., Rapee, R. M., and Wergeland, G. J. (2020). Does school-based recruitment for anxiety interventions reach youth not otherwise identified? a comparison between a school-based sample and a clinical sample. Sch. Ment. Health 12, 366–377. doi: 10.1007/s12310-019-09357-7
Kataoka, S. H., Zhang, L., and Wells, K. B. (2002). Unmet need for mental health care among U.S. Children: variation by ethnicity and insurance status. Am. J. Psychiatry 159, 1548–1555. doi: 10.1176/appi.ajp.159.9.1548
Kern, L., Mathur, S. R., Albrecht, S. F., Poland, S., Rozalski, M., and Skiba, R. J. (2017). The Need for school-based mental health services and recommendations for implementation. Sch. Ment. Health 9, 205–217. doi: 10.1007/s12310-017-9216-5
Kessler, R. C., Avenevoli, S., and Ries Merikangas, K. (2001). Mood disorders in children and adolescents: an epidemiologic perspective. Biol. Psychiatry 49, 1002–1014. doi: 10.1016/S0006-3223(01)01129-5
Kilbourne, A. M., Smith, S. N., Choi, S. Y., Koschmann, E., Liebrecht, C., Rusch, A., et al. (2018). Adaptive School-based Implementation of CBT (ASIC): Clustered-SMART for building an optimized adaptive implementation intervention to improve uptake of mental health interventions in schools. Implement. Sci. 13:119. doi: 10.1186/s13012-018-0808-8
Koschmann, E., Abelson, J. L., Kilbourne, A. M., Smith, S. N., Fitzgerald, K., and Pasternak, A. (2019). Implementing evidence-based mental health practices in schools: feasibility of a coaching strategy. J. Ment. Health Train. Educ. Pract. 14, 212–231. doi: 10.1108/JMHTEP-05-2018-0028
Kroenke, K., Spitzer, R. L., and Williams, J. B. W. (2001). The PHQ-9. J. Gen. Intern. Med. 16, 606–613. doi: 10.1046/j.1525-1497.2001.016009606.x
Lambie, G. W., Stickl Haugen, J., Borland, J. R., and Campbell, L. O. (2019). Who Took “Counseling” out of the Role of professional school counselors in the United States? J. Sch. Based Couns. Policy Eval. 1, 51–61.
Langley, A. K., Nadeem, E., Kataoka, S. H., Stein, B. D., and Jaycox, L. H. (2010). Evidence-based mental health programs in schools: barriers and facilitators of successful implementation. Sch. Ment. Health 2, 105–113. doi: 10.1007/s12310-010-9038-1
Lyon, A. R., Ludwig, K. A., Stoep, A. V., Gudmundsen, G., and McCauley, E. (2013). Patterns and predictors of mental healthcare utilization in schools and other service sectors among adolescents at risk for depression. Sch. Ment. Health 5, s12310–s12312. doi: 10.1007/s12310-012-9097-6
Masia Warner, C., Colognori, D., Brice, C., Herzig, K., Mufson, L., Lynch, C., et al. (2016). Can school counselors deliver cognitive-behavioral treatment for social anxiety effectively? A randomized controlled trial. J. Child Psychol. Psychiatry Allied Disciplines 57, 1229–1238. doi: 10.1111/jcpp.12550
Masia Warner, C., and Fox, J. K. (2012). Advances and challenges in school-based intervention for anxious and depressed youth: identifying and addressing issues of sustainability. Sch. Ment. Health 4, 193–196. doi: 10.1007/s12310-012-9087-8
Merikangas, K. R., He, J., Burstein, M., Swanson, S. A., Avenevoli, S., Cui, L., et al. (2010). Lifetime prevalence of mental disorders in U.S. Adolescents: results from the national comorbidity survey replication–adolescent supplement (NCS-A). J. Am. Acad. Child Adolesc. Psychiatry 49, 980–989. doi: 10.1016/j.jaac.2010.05.017
Merikangas, K. R., He, J., Burstein, M. E., Swendsen, J., Avenevoli, S., Case, B., et al. (2011). Service utilization for lifetime mental disorders in U.S. Adolescents: results of the national comorbidity survey adolescent supplement (NCS-A). J. Am. Acad. Child Adolesc. Psychiatry 50, 32–45. doi: 10.1016/j.jaac.2010.10.006
Mossman, S. A., Luft, M. J., Schroeder, H. K., Varney, S. T., Fleck, D. E., Barzman, D. H., et al. (2017). The generalized anxiety disorder 7-item (GAD-7) scale in adolescents with generalized anxiety disorder: signal detection and validation. Ann. Clin. Psychiatry 29, 227A–234A.
Pine, D. S., Cohen, P., Gurley, D., Brook, J., and Ma, Y. (1998). The risk for early-adulthood anxiety and depressive disorders in adolescents with anxiety and depressive disorders. Arch. Gen. Psychiatry 55:56. doi: 10.1001/archpsyc.55.1.56
Racine, N., McArthur, B. A., Cooke, J. E., Eirich, R., Zhu, J., and Madigan, S. (2021). Global prevalence of depressive and anxiety symptoms in children and adolescents During COVID-19: a meta-analysis. JAMA Pediatr. 175, 1142–1150. doi: 10.1001/jamapediatrics.2021.2482
Radez, J., Reardon, T., Creswell, C., Lawrence, P. J., Evdoka-Burton, G., and Waite, P. (2021). Why do children and adolescents (not) seek and access professional help for their mental health problems? A systematic review of quantitative and qualitative studies. Eur. Child Adolesc. Psychiatry 30, 183–211. doi: 10.1007/s00787-019-01469-4
Reardon, T., Harvey, K., Baranowska, M., O’Brien, D., Smith, L., and Creswell, C. (2017). What do parents perceive are the barriers and facilitators to accessing psychological treatment for mental health problems in children and adolescents? A systematic review of qualitative and quantitative studies. Eur. Child Adolesc. Psychiatry 26, 623–647. doi: 10.1007/s00787-016-0930-6
Richardson, L. P., McCauley, E., Grossman, D. C., McCarty, C. A., Richards, J., Russo, J. E., et al. (2010). Evaluation of the patient health questionnaire (PHQ-9) for detecting major depression among adolescents. Pediatrics 126, 1117–1123. doi: 10.1542/peds.2010-0852
Rones, M., and Hoagwood, K. (2000). School-based mental health services: a research review. Clin. Child Fam. Psychol. Rev. 3, 223–241.
Sanchez, A. L., Cornacchio, D., Poznanski, B., Golik, A. M., Chou, T., and Comer, J. S. (2018). The effectiveness of school-based mental health services for elementary-aged children: a meta-analysis. J. Am. Acad. Child Adolesc. Psychiatry 57, 153–165. doi: 10.1016/j.jaac.2017.11.022
Scott, M. A., Wilcox, H. C., Schonfeld, I. S., Davies, M., Hicks, R. C., Turner, J. B., et al. (2009). School-based screening to identify at-risk students not already known to school professionals: the Columbia suicide screen. Am. J. Public Health 99, 334–339. doi: 10.2105/AJPH.2007.127928
Spirito, A., Esposito-Smythers, C., Wolff, J., and Uhl, K. (2011). Cognitive-behavioral therapy for adolescent depression and suicidality. Child Adolesc. Psychiatr. Clin. North Am. 20, 191–204. doi: 10.1016/j.chc.2011.01.012
Spitzer, R. L., Kroenke, K., Williams, J. B. W., and Löwe, B. (2006). A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch. Intern. Med. 166:1092. doi: 10.1001/archinte.166.10.1092
Stephan, S. H., Weist, M., Kataoka, S., Adelsheim, S., and Mills, C. (2007). Transformation of Children’s mental health services: the role of school mental health. Psychiatr. Serv. 58:9. doi: 10.1176/ps.2007.58.10.1330
Stiffler, M. C., and Dever, B. V. (2015). Mental Health Screening at School: Instrumentation, Implementation, and Critical Issues. New York, NY: Springer International Publishing/Springer Nature, xv, 136. doi: 10.1007/978-3-319-19171-3
Keywords: school-based mental health, students, anxiety, depression, CBT, identification
Citation: Choi SY, Rusch A, Koschmann E, Bilek EL, Lane A, Abelson JL, Eisenberg D, Himle JA, Fitzgerald KD, Liebrecht C, Kilbourne AM and Smith SN (2022) How Effective Are School Professionals at Identifying Students Who Might Benefit From Cognitive Behavioral Therapy? Baseline Data From the Adaptive School-Based Implementation of Cognitive Behavioral Therapy Trial. Front. Educ. 7:814157. doi: 10.3389/feduc.2022.814157
Received: 12 November 2021; Accepted: 04 February 2022;
Published: 08 March 2022.
Edited by:
Herman Hay-ming Lo, Hong Kong Polytechnic University, Hong Kong SAR, ChinaReviewed by:
Jiwen Zhang, Hong Kong Polytechnic University, Hong Kong SAR, ChinaSamuel Shih-Chih Wang, University of Taipei, Taiwan
Copyright © 2022 Choi, Rusch, Koschmann, Bilek, Lane, Abelson, Eisenberg, Himle, Fitzgerald, Liebrecht, Kilbourne and Smith. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Seo Youn Choi, Y2hvaXNlb3lAdW1pY2guZWR1; Shawna N. Smith, c2hhd25hbmFAdW1pY2guZWR1
 Seo Youn Choi1*
Seo Youn Choi1* Amy Rusch
Amy Rusch Elizabeth Koschmann
Elizabeth Koschmann Annalise Lane
Annalise Lane James L. Abelson
James L. Abelson