- 1Department of Midwifery, College of Health Sciences, Debre Berhan University, Debre Berhan, Ethiopia
- 2Department of Clinical Midwifery, School of Midwifery, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia
- 3Department of Midwifery, College of Medicine and Health Sciences, Debre Markos University, Debre Markos, Ethiopia
Background: The COVID-19 pandemic has had a profound effect on the general healthcare system and higher education worldwide. Adapting to the culture of “new normal,” an emerging response to COVID-19, is crucial for public health recovery and learning. This study investigated students' readiness and intention for adapting to the ‘‘new normal’’ COVID-19 prevention campaign during campus re-entry in Debre Berhan university in Ethiopia after the country eases lockdown restrictions.
Methods: A cross-sectional study was conducted from 20th to 30th January 2021, among graduate students in Debre Berhan university, Ethiopia. A simple random sampling technique was used to select 423 participants. A structured and pre-tested self-administered questionnaire was used to collect the data and bivariate and multivariable logistic regressions were fitted. Adjusted odds ratio (AOR) with a 95% confidence interval (CI) were used to interpret the strength of association and the statistical significance level was declared at a p-value of ≤0.05.
Result: In this study 423 participants were involved. The level of readiness and intention of adapting to the ‘‘new normal’’ prevention campaign were 49.4 and 54.8% respectively. Being a health science student (AOR = 1.82; 95% CI: 1.18, 2.81), being married (AOR = 2.10; 95% CI: 1.1, 4.05), having a smartphone (AOR = 1.84; 95% CI: 1.09, 3.12), and being knowledgeable towards COVID-19 (AOR = 1.56; 95% CI: 1.04, 2.34) were found to be significant factors associated with intention towards adapting to the ‘‘new normal’’ prevention practice. Also, the main reason why participants had no intention to carry out the ‘‘new normal’’ prevention campaign were a shortage of quality required preventive supplies (60%) and those who perceived themselves personally not at risk of COVID-19 (31.3%).
Conclusion: In this study, although information on the COVID-19 outbreak is continually evolving, readiness and intention for adapting to the ‘‘new normal’’ COVID-19 prevention campaign were insufficient. It is critical to improve readiness and intention through increasing knowledge and emphasizing the importance of new technologies and handy protective supplies that may encourage the sustainable practice of new norms post-pandemic.
Introduction
Coronavirus disease 2019 (COVID-19) is an infectious disease caused by Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2), imposing a huge toll on individuals, families, communities, and societies across the globe (Tadesse et al., 2020; Adane et al., 2021). It is considered to be the third pandemic within the 21st century (Stanley, 2020). The COVID-19 global health pandemic has a profound effect on the general healthcare system and Higher Education (HE) at the global level (Thompson, 2020). In December 2019, China’s center for disease control (CDC) reported a novel coronavirus as the causative agent of the COVID-19 outbreak (ECDC, 2020). The World Health Organization (WHO) also declared COVID-19 as a public health emergency of international concern on January 31, 2020 and declared it as a pandemic on March 11, 2020 (Cucinotta and Vanelli, 2020; WHO Director-General, 2020).
According to United Nations Educational, Scientific, and Cultural Organization (UNESCO), on April 1, 2020, schools and higher education institutions (HEIs) were closed in 185 countries, affecting 1,542,412,000 learners, which constitutes 89.4% of total enrolled learners across the world (Marinoni et al., 2020). At the same time, various universities and other higher education institutions had already anticipated the impacts of the move online or the influences of the economic crisis on national and international students and their families (IAEA COVID 19, 2021). Consequently, many universities in the world had moved to an emergency remote teaching via online platforms for about a year since the occurrence of COVID-19 (i.e., “lockdown”) (Ye et al., 2020). However, these measures can have a profound negative impact on individuals, communities, and societies from the poorest households and on those who require special needs (Ferri and PatriziaGrifoni, 2020; WHO, 2020; Greyling and Rossouw, 2021; Scroll and For, 2021).
The term “new normal” first appeared during the 2008 financial crisis to refer to the dramatic economic, cultural, and social transformations that caused precariousness and social turbulence, impacting collective perceptions and individual lifestyles (El-erian, 2010). This term has been used again during the COVID-19 pandemic to point out how it has changed essential aspects of human life (World Health Organization, 2021). Cultural philosophers argue that there is an interplay between culture and both personal feelings and information consumption during times of crisis (Alexander and Smith, 2020). Nevertheless, it is up to us to adapt to the challenges of the current pandemic and similar crises, and whether we respond positively or negatively can significantly affect our personal and social lives. Indeed, there are many lessons we can learn from this crisis that can be used in building a better society. How we respond to change will depend on our capacity to adapt, to manage resilience in the face of adversity, and our flexibility when forced to make changes. We may have to adjust to a new normal as people get back to work, school, and a more normal life. As such, “we have touched the end of the beginning. New conventions, rituals, images, and narratives will no doubt emerge, so there will be more work for cultural sociology before we get to the commencement of the end” (Biddlestone et al., 2020).
In early November 2020, Ethiopia partially emerged from the first wave of the COVID-19 pandemic and social activities gradually resumed. The higher education system in Ethiopia was planned to reopen after 8 months’ lockdown following permission from the Ethiopian Ministry of Health by considering an adaptation to the culture of ‘‘new normal’’ prevention response to COVID-19. ‘‘However ‘new normal’ is not normal,” it is a term resulting from the adaptation process while in the COVID-19 pandemic (CRISTOBAL et al., 2021). Countries worldwide are trying to adjust to the disruptions in the education landscape caused by the COVID-19 pandemic and will have new behaviors to prevent infection, captured in the acronym DReAM (World Health Organization (WHO), 2021; UNESCO, 2020). The acronym stands for: D–Distancing–maintain a physical distance of at least 1 m from others, avoid crowded places, close-contact settings, and confined and enclosed spaces; Re–Respiratory etiquette–cough/sneeze into your elbow and contact a doctor if you have suggestive signs/symptoms; A–Aseptic techniques–wash your hands frequently with soap and water for at least 20 s or use a hand sanitizer with at least 70% alcohol, avoid touching your eyes, nose, and mouth, and regularly disinfect frequently touched surfaces; and M–Mask–wear a face mask, ensuring you put on, take off, and store your mask properly at all times (Pragholapati; Pradipta et al., 2020). Practicing DReAM will control COVID-19 transmission and enable the continuation of economic and social activities such as reopening of schools. The Ethiopian government is preparing to reopen schools and the Ministry of Higher Education has issued guidelines to limit the number of students per classroom and dormitory and face-to-face class sessions (World Bank, 2020. Educat, 2020). Adaptation of such behaviors is an essential component in the battle against the pandemic (Roberts and David, 2021). Nevertheless, returning to universities during the COVID-19 pandemic may not feel normal, at least for a while (Edmunds, 2020; Mekonen and Mekuria, 2020). It is important to prepare for a safe return to campus for all, with millions of students around the world at risk of being left behind in COVID-19 education response plans. Moreover, following the government’s implementing strategies to re-open universities, understanding the necessity of students is a very cost-effective approach to scale up their compliance with ‘‘new normal’’ approaches during the post-pandemic period. This may enable HE stakeholders’ strategic readiness towards the projected healthcare costs for effective prevention and response to the COVID-19 pandemic (Jackson, 2020). What we are learning from COVID-19, similar to what we have seen in previous pandemics, is that readiness is crucial. So, it is important to enchance preparedness while schools reopen.
Ethiopia shares a major proportion of the global burden of this infectious disease (Mohammed et al., 2020; Musa et al., 2020). The pandemic still has the potential for greater loss of life in Ethiopia; more efforts are needed to increase prevention capacity and bring changes in behavioral intention (Dennis, 2020; Mohammed et al., 2020). As of August 17, 2021, in Ethiopia, COVID-19 had caused 290,818 confirmed cases, with 4,495 deaths and 265,663 recovered cases (MoH Ethiopia (2021). Hence, the Ethiopian Ministry of Health has taken immediate steps to achieve an overall decrease in COVID-19 spread through restricting mobility within and across borders, physical distancing, hand washing, and the use of personnel protective equipment (PPE) masks (Balachandar et al., 2020; Wang et al., 2020; Adane et al., 2021).
Universities are places where students live and study near each other. Nowadays, the foundations of this unique ecosystem have been impacted significantly by the rapid spread of the COVID-19 outbreak, creating uncertainty regarding the implications for higher education. University students are recognized as a vulnerable population, suffering from the pandemic due to a multitude of factors: communal residency in on-campus and off-campus housing, sharing cafeteria, and having dynamic social groups with strong mobility and socialization during the COVID-19 pandemic (Browning et al., 2021; Holzer et al., 2021; Ihm et al., 2021). One study in Ethiopia reported 47, 54, and 42.8% of the higher institution students had good knowledge, a positive attitude, and good prevention practices towards COVID-19, respectively (Angelo et al., 2020).
Although Ethiopia has achieved a certain success in the fight against the COVID-19 pandemic, the potential risk of new epidemic waves requires the readiness of the entire healthcare workforce, including university students. However, although there has been a surge of articles on knowledge towards COVID-19 and its prevention measures, the level of readiness and intention in carrying out the ‘‘new normal’’ practices are unknown. Further, there is a scarcity of evidence on the intention and restraining cognitive impairments of university students to adapt ‘‘new normal’’ practices endorsed by WHO and/or national public health institutes, particularly during campus re-entry. Therefore, this study was intended to assess 1) student’s levels of readiness and intention to adapt the ‘‘new normal’’ COVID-19 prevention campaign, and 2) to evaluate potential factors associated with intention of adapting to COVID-19 prevention and perceived barriers among university students in Ethiopia.
Methods and Materials
Study Design, Period, and Setting
An institution-based cross-sectional study was conducted from 20th to January 30, 2021, at Debre Berhan University, northeast Ethiopia. Debre Berhan University is one of thirteen new governmental universities founded in 2007. It is located in the Amhara regional state, in the town of Debre Berhan, which is the capital of the North-Shewa Zone, around 130 km far from Addis Ababa (the capital city of Ethiopia). The university had ten colleges and fifty departments. Currently, the university has a total number of 27,371 students: 17,397 males and 9,974 females. Of these, 11,573 are regular undergraduate and postgraduate students. Overall, the university has approximately 3,300 graduating class students who attend regular programs at different programs and years of study. During the design of this study, graduating class students were the first candidates for the re-admission program after the COVID-19 “lockdown.”
Source and Study Population
All graduating class students of Debre Berhan University were the source population, while graduate students in the selected departments during the data collection period in the university were the study population.
Inclusion and Exclusion Criteria
All graduating class students of Debre Berhan University during the data collection period were included. This is because they were the first candidates during school reopening after the COVID-19 ‘‘lockdown’’ as our focus during the design of this study. However, students with active SARS-CoV-2 infection were excluded.
Sample Size Determination
The sample size for this study was determined by using a single proportion formula depending on the following assumptions: 50% proportion of students’ intention towards COVID-19 prevention practice, 95% level of confidence, and 5% margin of error.
Where n = required sample sizes, α = level of significance, z = standard normal distribution curve value for 95% confidence level = 1.96, p = proportion of intention for adapting to the “new normal” COVID-19 prevention practice, and d = margin of error. By considering a 10% non-response rate, the final sample size was 423.
Sampling Technique and Procedure
Study participants were selected from all regular graduating class students using a simple random sampling technique. Nineteen representative departments were selected from all colleges. Each of the selected departments was selected using lottery method. A sampling frame was prepared by acquiring the list of students from the registrar’s office. Then, in the selected departments, the required sample size was proportionally allocated to the total number of students. From all students of the selected departments, a simple random sampling technique was used to pick the required sample size using a pre-determined sampling frame of all departments.
Precautions: Face masks were worn by the data collectors who were distributing the questionnaire as per the guidelines for the prevention of COVID-19. To minimize further risks of COVID-19 transmission, participants’ hands were sanitized before and after the questionnaire. Face masks were also provided to students who were not wearing one with the collaboration of the COVID-19 prevention task force and the recommended social distance was observed between the study staff and participants.
Measurements and Operational Definitions
The dependent variable in this study was the university students’ intention for adapting to the “new normal” COVID-19 prevention campaign endorsed by WHO. The participants were asked four questions to assess “new normal” practices, relating to wearing a mask, engaging in social distancing, handwashing with soap and water, and routine sanitizing of hands with sanitizer for sustainable response. The response options for each question were “Never,” “Occasionally,” or “Always’.” Thus, based on the summative scores designed to assess intention for adapting to the “new normal” WHO COVID-19 prevention practice, respondents answer above the mean score was considered as favorable intention of adapting to the “new normal” prevention campaign and those who scored below the mean value were considered as having Unfavorable intention. The higher values indicate higher intention (Andarge et al., 2020a; Dires et al., 2021).
Readiness: A total of 10 questions were prepared to determine readiness towards COVID-19 prevention. Each item has a “Yes” or “No” response giving a score of one and zero (i.e., a score of 1 was given for “Yes” and a score of 0 was given for “No”). The higher values indicate higher readiness to adapt to COVID-19 prevention. Depending on the mean score of readiness assessment questions, respondents who scored above the mean score were considered as having “Good readiness” and those who scored mean or below were considered as having “Poor readiness”. Likewise, the participants’ readiness was coded as “1” for Good readiness and ‘‘0″ for Poor readiness (Lazarus et al., 2021).
Knowledgeable towards COVID-19: Participants’ knowledge was determined by asking the eleven “Yes” or “No” knowledge assessment questions. Respondents who scored above the mean were categorized as knowledgeable (W/Mariam TGAyanaw et al., 2020) and vice versa.
Data Collection Tool and Quality Assurance
The data were collected using a pre-tested, self-administered, and structured questionnaire. The tool was developed from different literature (Andarge et al., 2020b; Iyengar et al., 2020; Mulu et al., 2020; Pradipta et al., 2020; Desalegn et al., 2021; He et al., 2021; Lazarus et al., 2021; Mekonnen et al., 2021; Sazali et al., 2021) following the COVID-19 Community Guidelines by CDC and the WHO and validated to fit the research objectives. To assess the study objectives, the questionnaire comprises four parts: 11 socio-demographic characteristics, 11 knowledge assessments, 10 readiness questions, and five for intention to adapt “new normal” practice assessment questions. The face and content validity of the questionnaire was checked by public health experts. The questions prepared in English were first translated into Amharic (local language) and then back into English to ensure consistency. A pre-test was conducted on 5% of the samples size at Debre Berhan Health science college. The language clarity and validity of the tool were checked and required amendments were made after the result of the pre-test. Thus, the internal consistency of each item scale was checked and Cronbach’s alpha coefficients for intention, readiness, and knowledge were 0.88, 0.78, and 0.69 respectively; this was verified as an acceptable range. Further, two BSc degree and two MSc holder midwives gathered the data and supervised the process. Before the actual work, data collectors and supervisors had received training on the purpose of the study, collection procedures, and confidentiality assurance.
Data Management and Analysis
Data were checked, coded, and entered into Epi Data version 4.6, and were exported to SPSS version 25 for analysis. Data cleaning was carried out before statistical analysis and descriptive statistics were used to present the participants’ characteristics. Both binary and multivariable logistic regression was fitted to identify statistically significant independent variables and the level of significance was determined at a p-value of ≤0.05. The model fitness of the multivariable logistic regression analysis was assessed using the Hosmer-Lemeshow goodness-of-fit test. Finally, the strength of association was interpreted using the Adjusted Odds ratio (AOR) with its 95% confidence interval and its p-value of ≤0.05.
Ethical Considerations
The study was conducted following the approval of the Debre Berhan University Institutional Review Committee (protocol number: P006/20). The study was conducted following the Ethiopian Health Research Ethics Guideline and the declaration of Helsinki. A formal letter of administrative approval was obtained from each college. Anonymous written consent was obtained from each study participant following a clear explanation of the goal of the study.
Result
Socio-Demographic Characteristics of Respondents
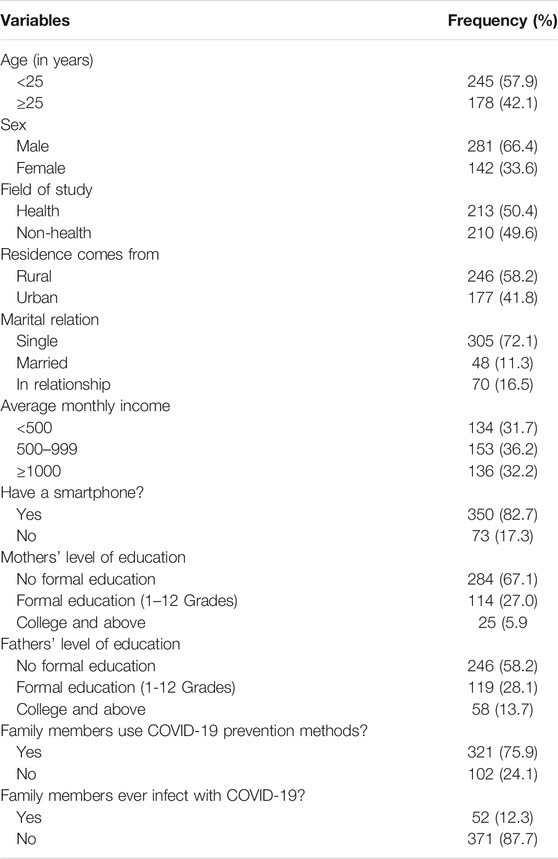
A total of 423 participants were involved in this study, giving a response rate of 100%. The mean age of study participants was 24.17 (SD ± 1.73). Of these, the majority were males (66.4%). Regarding marital status, most of the respondents (72.1%) were single. About three hundred and fifty (82.7%) of the study participants have a smartphone and three-fourths (75.9%) of the study participants’ family members have used COVID-19 prevention methods. Furthermore, half (50.4%) of the participants were Health Science students (Table1).
Knowledge Related Characteristics of Respondents
Overall, 63.1% 95% CI (59%, 68%) of university students were knowledgeable about COVID-19 and its prevention measures. The mean knowledge score of the respondents was 12.47 ± 2.1 (12.27–12.67). Of the 423 participants, a majority (95.3%) answered that they were aware of COVID-19 prevention measures. Most (95.5%) of the study participants knew the typical symptoms of COVID-19 (Table 2).
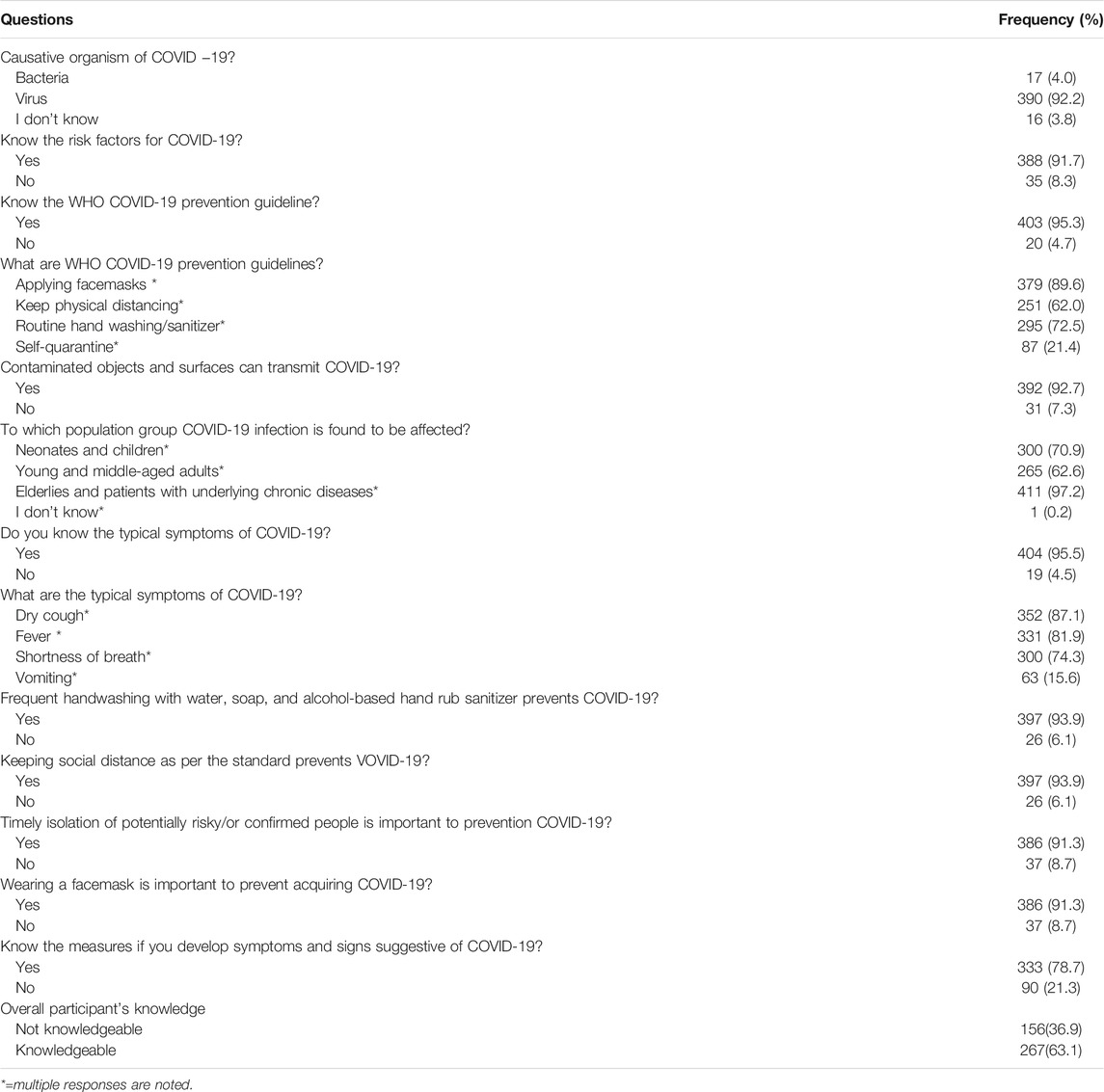
TABLE 2. Participants’ knowledge related characteristics about COVID-19 in Debre Berhan University, Northeast Ethiopia, 2021 (n= 423).
Readiness to Adapt New Normal COVID-19 Prevention Practice-Related Characteristics of Respondents
In this study, half (49.4%) 95% CI (45%, 54%) of the university students had a good readiness to prevent COVID-19. The average readiness score of the respondents was 7.18 ± 2.0 (6.99–7.37). Similarly, 294 (69.5%) of students would self-quarantine if they had developed signs and/or symptoms suggestive of COVID-19 infection and 265 (62.6%) understood they might transmit COVID-19 to their family members and classmates. Moreover, just a fourth of the participants declared they would not successfully control COVID-19 by adapting to the WHO prevention measures (Table 3).
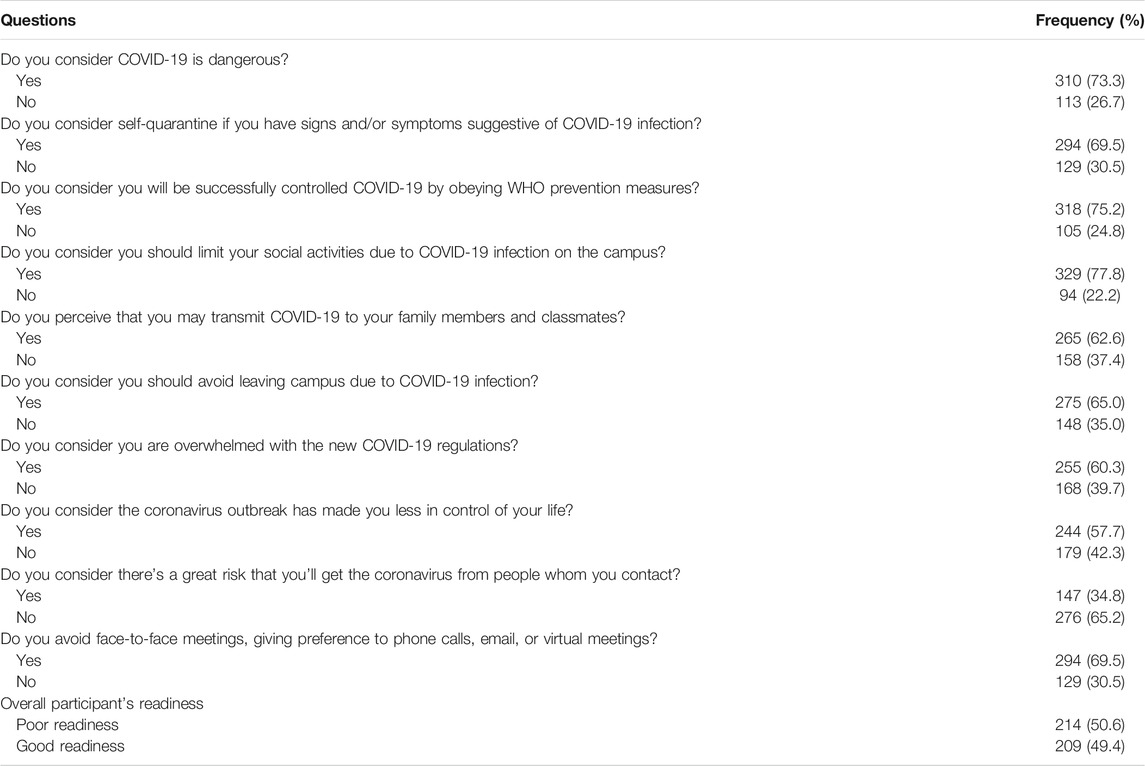
TABLE 3. Participants’ readiness-related characteristics about COVID-19 prevention campaign in Debre Berhan University, Northeast Ethiopia, 2021 (n= 423).
Intention for Adapting New Normal COVID-19 Prevention Practice-Related Characteristics of Respondents
The overall prevalence of students’ intention to adapt to “new normal” COVID-19 prevention was 54.8% (95% CI: 50%, 60%). The mean score of the intention of implementing the “new normal” mitigation measures among respondents was 4.65 ± 2.8 (4.38–4.92). Of the total study participants, 232 students have had favorable intentions for adapting to the “new normal” prevention measures during their campus re-entry. A few of the participants (22, or 5.2%) were not intending to comply with physical distancing as recommended by their campus (Table 4).
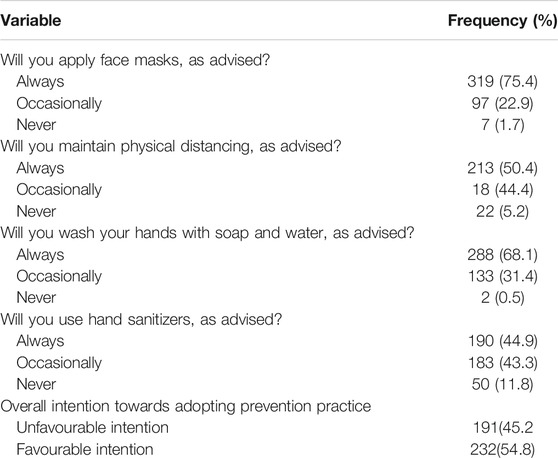
TABLE 4. Participants’ intention of adapting the ‘‘new normal’’ COVID-19 prevention practice-related characteristics of in Debre Berhan University, Northeast Ethiopia, 2021 (n= 423).
Perceived Barriers for Students Who did not Intend to Adapt the New Normal COVID-19 Prevention Practice
However, more than half of the study participants have a favorable intention to practice routine COVID-19 prevention measures, although there were multiple perceived barriers to a lack of intent to adapt. Thus, the top two perceived reasons for unfavorable intention by the study participants were the shortage of required preventive supplies (60%) and perceived considering not at risk of COVID-19 pandemic (31.3%) (Figure 1). Perhaps students leaving their campus (went crowded places) due to different reasons, such as purchasing necessities (42%), meeting their friends outside (21%), and having fun and leisure (20%) during the outbreak made it difficult to prevent the disease (Figure 2).
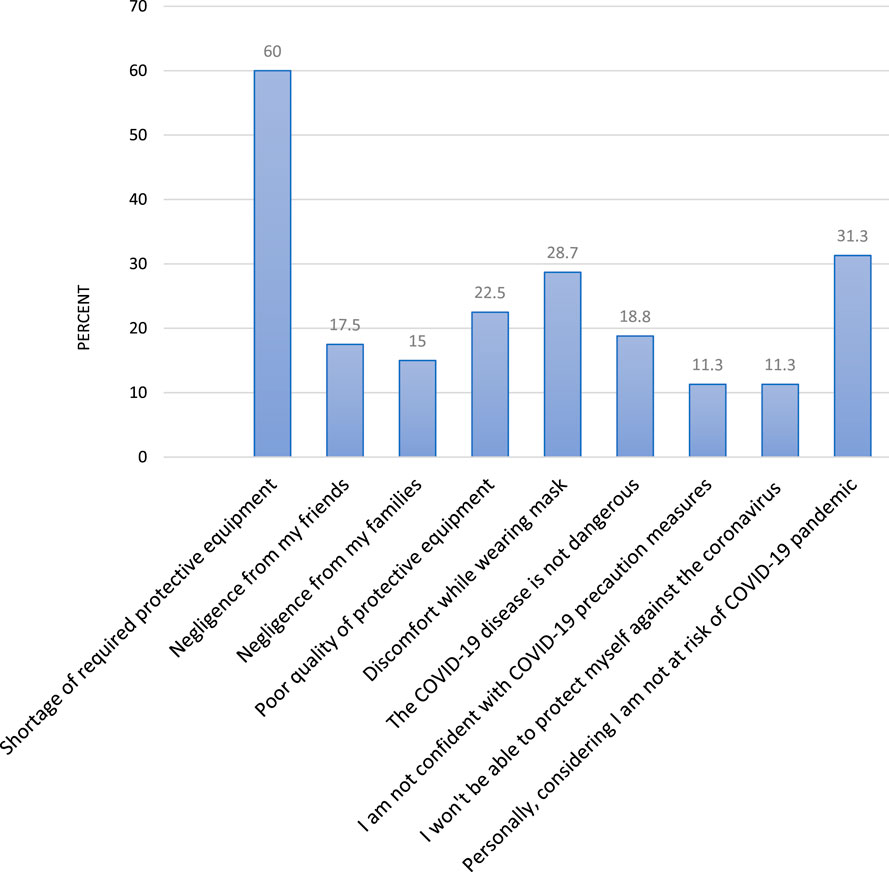
FIGURE 1. Destributions of reasons why not intend to carry COVID-19 WHO prevention measures among Debre Berhan University students, Northeast Ethiopia, 2021.
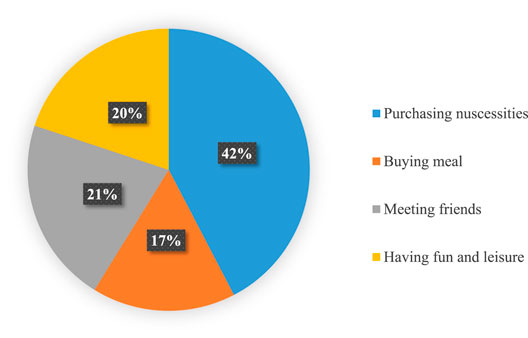
FIGURE 2. Main reasons for went outside university campus among Debre Berhan University students, Northeast Ethiopia, 2021.
Factors Associated With the Intention for Adapting the New Normal COVID-19 Prevention Practice
The association between covariates with response variables was estimated by the odds ratio using logistic regression analysis. Controlling the effect of confounding factors, being a health science student, married, knowledgeable, and having a smartphone had statistically significant associations with intention towards adapting to the “new normal” COVID-19 prevention measures during multivariable analysis.
This study revealed that students studying in the health science departments were 1.82 times more likely to have had a favorable intention than those who were in another department (AOR = 1.82,95% CI:1.18, 2.81). According to the results, married students had more favorable intentions than their single counterparts (AOR = 2.10, 95% CI: 1.1, 4.05). The odds of having favorable intentions among students with smartphones were 1.84 times higher compared to those who did not have a smartphone (AOR = 1.84, 95% CI: 1.09, 3.12). Likewise, the odds of having a favorable intention of adapting to the ‘‘new normal’’ prevention actions among knowledgeable respondents were 1.56 (AOR = 1.56, 95% CI: 1.04, 2.34) times higher as compared to their counterparts (Table 5).
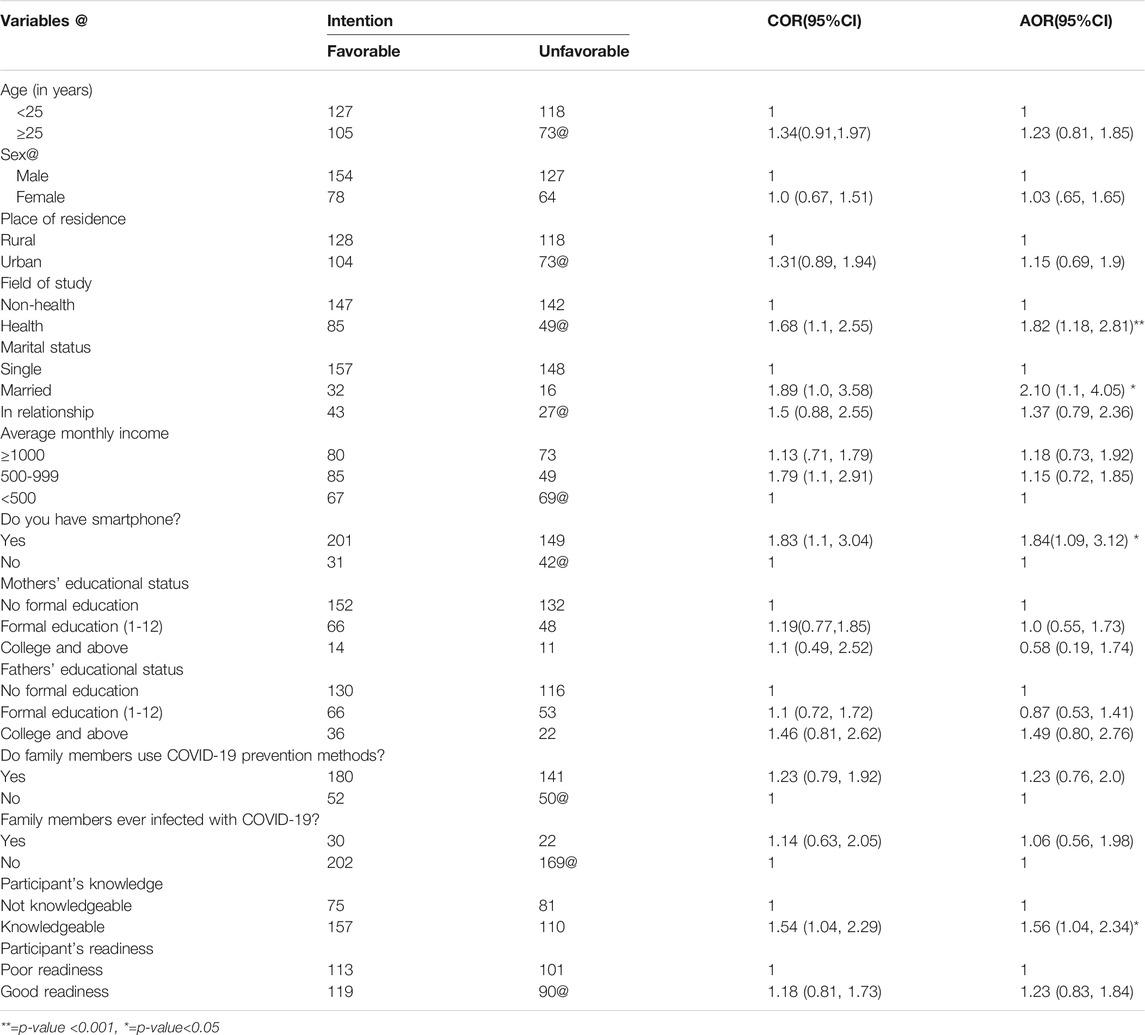
TABLE 5. Bivariable and multivariable analysis of variables on intention for adapting COVID-19 prevention campaign Debre Berhan University, Northeast Ethiopia, 2021 (n=423).
Discussion
Coronavirus disease 2019 is still a life-threatening infection worldwide and continues to be a public health concern in Ethiopia. Currently, as the disease has no cure, vaccine supplies dwindle in Africa, and the existence of new COVID-19 variants means prevention is a better available effective weapon to tackle the global consequences of the pandemic on students and learning. Hence, good intentions are an important starting point. Practice of COVID-19 prevention encapsulated in DReAM needs to have adequate readiness and intention. This study assessed Debre Berhan university students’ readiness and intention for adapting to “new normal” prevention endorsements and the factors that influence their intention and perceived barriers. Overall, half (49.4%) had good readiness and 54.8% of the respondents had a favorable intention for adapting to “new normal” mitigation measures. Moreover, student’s intention was influenced by the field of study, marital status, knowledge towards the pandemic, and having a smartphone.
The current study revealed that half (49.4%) 95% CI; 45%, 54%) of participants had good readiness to fight against the COVID-19 pandemic. In agreement with this finding, a study from Addis Ababa established healthcare professionals’ preparedness as 50% (Desalegn et al., 2021). The finding is higher as compared with other studies conducted in Ethiopia which shows Southwest Ethiopia at 25% (Mekonnen et al., 2021), Awi Zone at 20.2% (Adane et al., 2021), North Shewa Zone at 25.5% (Mulu et al., 2020), and Indonesia at 18.6% (Lazarus et al., 2021). This variation might be due to the difference in study setting (i.e. Ethiopia Vs Indonesia) and target population which greatly influence the awareness of the symptoms and the complications of COVID-19. Besides, the time gap among studies is a factor, since the COVID-19 outbreak is a global agenda and rapidly disseminated relevant information on the pandemic has led to unexpected changes in people’s daily lifestyles (Lin and Lin, 2021). Also due to poor healthcare, limited resources, low living standards, and environmental factors among prisoners (Mekonnen et al., 2021) as compared with the current study (i.e. readiness among prisoners 25% vs 49.4% in the current study). Thus, prisoners and detainees live in prison facilities close proximity with one another which likely increases the risk of person-to-person and droplet transmission of pathogens like COVID-19. In Indonesia, institutions have implemented a massive open online course, which may mitigate COVID-19 misinformation and help students in similar real-world circumstances (Lazarus et al., 2021). This implies that, when assessing management of COVID-19 risks, the local epidemiological situation of the destination country as well as its international and national strategy should be accounted for (Cauchemez and Kiem, 2021; Leung et al., 2021).
This study depicted that the overall participants’ intention for adapting to the “new normal” COVID-19 prevention campaign was 54.8% (95% CI: 50%, 60%). This is in line with another study from Ethiopia in which 52% of adults with chronic conditions were intending to engage with personal preventive practice (Andarge et al., 2020b). Unfortunately, due to the lack of similar literature to relate the changes in the intention of the “new normal” adaptation process during the pandemic, the appraisal and comparison were based on existing works. Thus, this finding was higher as compared to the previous study conducted among patients with chronic disease in Dessie Town, which was 28.3% (Dires et al., 2021). This variation might be due to the difference in study participants as this study employed university students who may have access to more information and tend to have good media exposure. Evidence has shown that regular exposure to media influences an individual’s preventive behavior and excessive preventive intention (Liu et al., 2020). On the other hand, a study from the American general population of 80% (Lennon et al., 2020) indicated a greater national intent to comply with WHO recommendations of COVID-19 prevention. This discrepancy might be due to the difference in the study population. The American study was conducted during the paradigm shift in the emergence of the pandemic (i.e., during the start of stay-at-home order) and would reflect people’s response to such an unprecedented crisis. In addition, as an online survey, they might not verify or describe the true prevalence, and response bias may have been introduced.
This study demonstrates that there was a positive statistical association between being in the health sciences field of study and the intention to adapt to the “new normal” COVID-19 prevention practice. This might be linked to adapting appropriate actions to limit the spread of the pandemic in the medical students (Sazali et al., 2021). This is because medical students have a better inclination and are readily accessible to accurate information that was obtained from their learning courses. Even though the current study did not explore the information source regarding COVID-19, it should be considered that the source of information from the mass media had a great influence on student’s intentions regarding the infectious disease.
Married participants also had higher odds of adapting to COVID-19 prevention practice than their counterparts. This study is supplemented with a study from the northwest part of Ethiopia which reported that the odds of good prevention practice in married study participants was 3.9-times higher than unmarried participants (Akalu et al., 2020). This could be because married people are responsible for taking care of their families and so have more positive protective attitudes and higher adherence rates to protective behaviors than single individuals (He et al., 2021). Moreover, married individuals may still have worried and decide to adapt to prevention practices against COVID-19 considering they are helping their families (Handebo et al., 2021). However, some studies reported that marital status does not affect the preventive measure rank (Yitayih et al., 2020; Birihane et al., 2020). This disagreement might be the difference in sample size, which was done only among 247 study participants in Jimma and 182 in Northern Ethiopia (Yitayih et al., 2020; Birihane et al., 2020) Another relevant finding from the study was that having a smartphone had a significant positive link to a higher intention of adapting to the “new normal” prevention campaign than those who have not. This is consistent with a review of articles as digital technologies are being harnessed to support the public-health response to COVID-19 worldwide (Sazali et al., 2021). A plausible explanation is that, since smartphones can be seen as an important source for regular updates and news related to COVID-19, these participants will have better information (Liu et al., 2020). Similarly, smartphones help in avoiding face-to-face contact (maintain social distancing and avoid virus transmission) (Iyengar et al., 2020).
In the present study, we have also assessed the perceived barriers in participants who had no intention to carry out the “new normal” WHO prevention recommendations. Thus, shortage and poor quality of required preventive equipment/supplies was reported in 60%, perceiving themselves as personally not at risk of COVID-19 in 31.3%, and discomfort while wearing masks was reported in 28.7%. This finding is supported by other studies from Ethiopia and Indonesia (Lazarus et al., 2021)as there is a gap in necessary supplies (Dires et al., 2021; Mersha et al., 2021). In addition, 33.8% of participants described that they would go outside university campuses (crowded places) in order to purchase necessities 42%, meet friends 21%, and or for fun and leisure 20%. In this regard, the evidence from this finding calls upon policymakers and program managers to play a major role in implementing an integrated approach of health education and communication for a greater effect on negatively perceived barriers of COVID-19 prevention. University stakeholders should try their best to provide sufficient supplies of protective equipment that the student could use to take protective actions.
Knowledgeable respondents were more likely to intend to practice routine WHO COVID-19 mitigation measures than their counterparts. This agreement might be as stated in previous studies Ethiopia (Asemahagn, 2020), Ghana (Nkansah et al., 2020) and Saudi Arabia (Khan et al., 2014); it could be inferred that knowledge is a precondition for the formation and promotion of positive attitudes. This could also be explained by the awareness they access from different information sources, media, and experts which improves their level of practice (Nations et al., 2020), (Al-Mohaissen, 2017). Therefore, improving people’s knowledge and fostering positive intent to prevent outbreaks is critical to improving protective behaviors in the response to COVID-19 (Alves and Samorinha, 2020; Zhong et al., 2020). This is consistent with the findings of other recent studies in Ethiopia (Andarge et al., 2020a; Akalu et al., 2020). Furthermore, this finding indicates a need for targeted measures to improve protective behavior. There is still much to understand about COVID-19 and its impact in diverse contexts. Readiness and response movements towards the new normal COVID-19 prevention should continue to be motivated by rapidly accumulating scientific and public health knowledge.
The authors acknowledge this study has some limitations. First, as a cross-sectional study, we could not verify causal association. Second, the study answers reflect a single moment in time and may not be generalizable over time. Third, there is a lack of similar documentation to link respondent’s intent changes to the local context.
Conclusion
In this study, although information on the COVID-19 outbreak is continually evolving, the status of readiness and intention to adapt to the “new normal” COVID-19 prevention campaign was not sufficient enough. Poor readiness and unfavorable intention for adapting to the new normal COVID-19 prevention campaign was reported among students in the non-health sciences field of study, unmarried, not knowledgeable, and participants who did not have a smartphone. Multiple perceived barriers were the cause of a lack of intent of adapting routine prevention practices. Thus, the main reason why participants had no intention to carry out the “new normal” WHO prevention recommendations were shortage and poor quality of required preventive supplies (60%) and perceiving themselves as personally not at risk of COVID-19 (31.3%). This suggests that the policymakers and the health offices should consider these findings while developing strategies against COVID-19. Also, there is a need to focus on adapting new technologies and protective supplies, self-care practices, and appropriate capacity building through COVID-19 risk communication and public education.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics Statement
The studies involving human participants were reviewed and approved by Debre Berhan University institutional review board. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
BT had a major role in the conceptualization, data curation, develop the proposal, and data entry. All authors participate in formal analysis and writing the original draft. They equally participated in manuscript preparation, revision, and approved the manuscript to be considered for publication.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We would like to thank Debre Berhan University for its ethical authorization. Our compliment is also extended to study participants, data collectors, and supervisors for their friendly cooperation.
Abbreviations
CDC, center for disease control and prevention; COVID-19, coronavirus disease 2019; WHO, world health organization; HE, higher education; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2; DReAM, D-distancing, Re-respiratory etiquette, A-aseptic techniques and M-mask.
References
Adane, D., Yeshaneh, A., Wassihun, B., and Gasheneit, A. (2021). Level of Community Readiness for the Prevention of COVID-19 Pandemic and Associated Factors Among Residents of Awi Zone, Ethiopia: A Community-Based Cross-Sectional Study. Risk Manag. Healthc. Pol. 14, 1509–1524. doi:10.2147/RMHP.S302974
Akalu, Y., Ayelign, B., and Molla, M. D. (2020). Knowledge , Attitude and Practice towards COVID-19 Among Chronic Disease Patients at. Infect. Drug Resist. [Internet 13, 1949. doi:10.2147/IDR.S258736
Al-Mohaissen, M. (2017). Awareness Among a Saudi Arabian university Community of Middle East Respiratory Syndrome Coronavirus Following an Outbreak. East. Mediterr. Heal J. 23 (5), 351–360. doi:10.26719/2017.23.5.351
Alexander, J. C., and Smith, P. (2020). COVID - 19 and Symbolic Action : Global Pandemic as Code , Narrative , and Cultural Performance. Am. J. Cult. Sociol. [Internet] 8 (3), 263–269. doi:10.1057/s41290-020-00123-w
Alves, R. F., and Samorinha, C. (2020). Knowledge , Attitudes and Preventive Behaviors toward COVID-19 : a Study Among Higher Education Students in Portugal. J. Heal Res. [Internet, 0857–4421. doi:10.1108/JHR-07-2020-0254–
Andarge, E., Fikadu, T., Temesgen, R., Shegaze, M., Feleke, T., Haile, F., et al. (2020). Intention and Practice on Personal Preventive Measures against the Covid-19 Pandemic Among Adults with Chronic Conditions in Southern ethiopia: A Survey Using the Theory of Planned Behavior. J. Multidiscip Healthc. 13, 1863–1877. doi:10.2147/JMDH.S284707
Andarge, E., Fikadu, T., Temesgen, R., Shegaze, M., Feleke, T., Haile, F., et al. (2020). Intention and Practice on Personal Preventive Measures against the COVID-19 Pandemic Among Adults with Chronic Conditions in Southern Ethiopia : A Survey Using the Theory of Planned Behavior. J. Multidiscip Healthc. [Internet] 13, 1863–1877. doi:10.2147/JMDH.S284707
Angelo, A. T., Alemayehu, D. S., and Dacho, A. M. (2020). Knowledge, Attitudes, and Practices toward Covid-19 and Associated Factors Among university Students in Mizan Tepi university. Infect. Drug Resist. [Internet] 14, 349–360. Available from: 10.2147/IDR.S299576. doi:10.2147/IDR.S299576
Asemahagn, M. A. (2020). Factors Determining the Knowledge and Prevention Practice of Healthcare Workers towards COVID-19 in Amhara Region, Ethiopia: A Cross-Sectional Survey. Trop. Med. Health 48 (1). doi:10.1186/s41182-020-00254-3
Balachandar, V., Mahalaxmi, I., Kaavya, J., Vivekanandhan, G., Ajithkumar, S., Arul, N., et al. (2020). COVID-19: Emerging Protective Measures. Eur. Rev. Med. Pharmacol. Sci. [Internet] 24 (6), 3422–3425. doi:10.26355/eurrev_202003_20713
Biddlestone, M., Green, R., and Douglas, K. M. (2020). Cultural Orientation , Power , Belief in Conspiracy Theories , and Intentions to Reduce the Spread of. Br. J. Soc. Psychogy [Internet 59, 663–673. doi:10.1111/bjso.12397
Birihane, B. M., Bayih, W. A., Alemu, A. Y., and Belay, D. M. (2020). Perceived Barriers and Preventive Measures of COVID-19 Among Healthcare Providers in Debretabor, north central Ethiopia, 2020. Risk Manag. Healthc. Pol. 13, 2699–2706. doi:10.2147/RMHP.S287772
Browning, M. H. E. M., Larson, L. R., Sharaievska, I., Rigolon, A., McAnirlin, O., Mullenbach, L., et al. (2021). PLOS ONE Psychological Impacts from COVID-19 Among university Students : Risk Factors across Seven States in the United States. PLoS One [Internet] 16 (1), 1–27. doi:10.1371/journal.pone.0245327
Cauchemez, S., and Kiem, C. T. (2021). Managing COVID-19 Importation Risks in a Heterogeneous World. Lancet Public Heal [Internet] 2667 (21), 19–20. doi:10.1016/S2468-2667(21)00188-2
Cristobal, C. O. B. O., Alberto, M-N., and Inaki, S. C. (2021). Remote Learning during COVID-19 Pandemic: How Countries Have Faced the challenge of Implementing Multichannel Education Delivery Strategies. [Internet]. Washington, DC: Education for Global Development. Available at: https://blogs.worldbank.org/education/remote-learning-during-covid-19-pandemic-how-countries-have-faced-challenge-implementing (Accessed January 14, 2021).
Cucinotta, D., and Vanelli, M. (2020). WHO Declares COVID-19 a Pandemic. Acta Biomed. 91 (1), 157–160. doi:10.23750/abm.v91i1.9397
Dennis, M. J. (2020). Coronavirus Crisis and HE. Univ World News [Internet]. Available at: https://www.universityworldnews.com/page.php?page=Coronavirus_Hub (Accessed August 29, 2020).
Desalegn, Z., Deyessa, N., Teka, B., Shiferaw, W., Yohannes, M., Hailemariam, D., et al. (2021). Evaluation of COVID-19 Related Knowledge and Preparedness in Health Professionals at Selected Health Facilities in a Resource-Limited Setting in Addis Ababa , Ethiopia. PLoS One [Internet 16, 1–14. doi:10.1371/journal.pone.0244050
Dires, A., Gedamu, S., and Getachew, Y. (2021). Perception of COVID-19 Prevention Methods Efficacy and Intention to Use Among Patients with Chronic Disease in Dessie Town , Northeast Ethiopia : A Multicentered Cross-Sectional Study. J. Multidiscip Healthc. 14 (June), 1325–1339. doi:10.2147/JMDH.S313796
Edmunds, W. J. (2020). Comment Finding a Path to Reopen Schools during the COVID-19 Pandemic. Lancet Child. Adolesc. Heal [Internet] 4642 (20), 19–20. doi:10.1016/S2352-4642(20)30249-2
Ferri, F., and Patrizia Grifoni, T. G. (2020). Online Learning and Emergency Remote Teaching : Opportunities and Challenges in Emergency Situations. MDPI [Internet] 10 (86), 1–18. doi:10.3390/soc10040086
Greyling, T., and Rossouw, S. (2021). The Good , the Bad and the Ugly of Lockdowns during Covid-19. PLoS One [Internet] 16(1):1–18. doi:10.1371/journal.pone.0245546
Handebo, S., Adugna, A., Kassie, A., and Shitu, K. (2021). Determinants of COVID-19- Related Knowledge and Preventive Behaviours Among Students in Reopened Secondary Schools : Cross- Sectional Study. BMJ Open [Internet 11, 1–10. doi:10.1136/bmjopen-2021-050189
He, S., Chen, S., Kong, L., and Liu, W. (2021). Analysis of Risk Perceptions and Related Factors Concerning COVID-19 Epidemic in Chongqing, China. J. Community Health [Internet] 46 (2), 278–285. doi:10.1007/s10900-020-00870-4
Holzer, J., Pelikan, M., and Katariina Salmela-Aro, C. S. B. S. (2021). Higher Education in Times of COVID-19: University Students’ Basic Need Satisfaction, Self-Regulated Learning, and Well-Being, 7. Thousand Oaks, California: AERA Open volume, 1–13. doi:10.1177/23328584211003164
IAEA. COVID-19 (2021). Transitioning to a ’ New-Normal ’ when and How, Vol. 43.p. Available at: https://www.iaea.org/.
Yitayih, Y., Birhanu, Z., and Mekonen, S. (2020). Knowledge , Perceptions and Preventive Practices towards COVID-19 Early in the Outbreak Among Jimma university Medical center Visitors , Southwest Ethiopia. PLoS One [Internet 77 (May), 1–15. doi:10.1371/journal.pone.0233744
Ihm, L., Zhang, H., Vijfeijken, A. Van., and Waugh, M. G. (2021). Mpacts of the Covid ‐ 19 Pandemic on the Health of university Students. Int. J. Heal Plann. Mgmt 36, 618–627. doi:10.1002/hpm.3145
Iyengar, K., Upadhyaya, G. K., Vaishya, R., and Jain, V. (2020). COVID-19 and Applications of Smartphone Technology in the Current Pandemic. Diabetes Metab Syndr Clin Res Rev 14, 733–737. Available from. doi:10.1016/j.dsx.2020.05.033
Jackson, D. (2020). University Prep Academy COVID-19 Preparedness and Response Plan [Internet]. Available at: https://uprepschools.com/wp-content/uploads/2020/08/UPA-COVID-19-Preparedness-Response-Plan.pdf (Accessed August 29, 2020).
Khan, M. U., Shah, S., Ahmad, A., and Fatokun, O. (2014). Knowledge and Attitude of Healthcare Workers about Middle East Respiratory Syndrome in Multispecialty Hospitals of Qassim, Saudi Arabia. BMC Public Health 14 (1), 1–7. doi:10.1186/1471-2458-14-1281
Lazarus, G., Findyartini, A., Putera, A. M., Gamalliel, N., Nugraha, D., Adli, I., et al. (2021). Willingness to Volunteer and Readiness to Practice of Undergraduate Medical Students during the COVID-19 Pandemic : a Cross- Sectional Survey in Indonesia. BMC Med. Educ. [Internet 21, 1–12. doi:10.1186/s12909-021-02576-0
Lennon, R. P., Sakya, S. M., Miller, E. L., Snyder, B., Zgierska, A. E., Ruffin, M. T., et al. (2020). Public Intent to Comply with COVID-19 Public Health Recommendation. Heal Lit Res Pract 4, 160–165. doi:10.3928/24748307-20200708-01
Leung, K., Wu, J. T., and Leung, G. M. (2021). Effects of Adjusting Public Health, Travel, and Social Measures during the Roll-Out of COVID-19 Vaccination: a Modelling Study. Lancet Public Heal [Internet] 2667 (21), 1. doi:10.1016/S2468-2667(21)00167-5
Lin, X., and Lin, Y. (2021). Practice of New Normal Lifestyles , Economic and Social Disruption , and Level of Happiness Among General Public in China in the Post-COVID-19 Era. Risk Manag. Healthc. Pol. 14, 3383–3393. doi:10.2147/RMHP.S320448
Liu, L., Xie, J., Li, K., and Ji, S. (2020). Exploring How media Influence Preventive Behavior and Excessive Preventive Intention during the COVID-19 Pandemic in China. Int. J. Environ. Res. Public Health [Internet] 17 (21), 1–27. doi:10.3390/ijerph17217990
Marinoni, G., Land, H. Van., and Jensen, T. (2020). THE IMPACT of COVID-19 on HIGHER EDUCATION AROUND the WORLD IAU Global Survey Report.
Mekonen, N. S. A. M. A., and Mekuria, R. M. (2020).The Psychological Impacts of COVID-19 Pandemic Among University Students in Bench-Sheko Zone , South-West Ethiopia : A Community-Based Cross-Sectional Study. Psychol Res Behav Manag 13, 813–821. [Internet]Available from. doi:10.2147/PRBM.S275593
Mekonnen, B., Hailemariam, S., Ejigu, A., Shifera, N., and Simieneh, A. (2021). Preparedness and Readiness against COVID-19 Pandemic in Prison Institutions and Detention Centers in Southwest Ethiopia. Int. J. Gen. Med. [Internet 14, 37–46. Available from. doi:10.2147/IJGM.S287066
Mersha, A., Shibiru, S., Girma, M., Ayele, G., Bante, A., and Kassa, M. (2021). Perceived Barriers to the Practice of Preventive Measures for COVID-19 Pandemic Among Health Professionals in Public Health Facilities of the Gamo Zone , Southern Ethiopia : a Phenomenological Study. BMC Public Health [Internet 21, 1–10. doi:10.1186/s12889-021-10256-3
MoH Ethiopia (2021). Worldometer Report COVID-19 Cases in Ethiopia. Available at:https://www.worldometers.info/coronavirus/country/ethiopia/?lan=xzbfupgf (Accessed August 17, 2021).
Mohammed, H., Oljira, L., Roba, K. T., Yimer, G., Fekadu, A., and Manyazewal, T. (2020). Containment of COVID-19 in Ethiopia and Implications for Tuberculosis Care and Research. BMC Res. Notes [Internet 9, 1. doi:10.1186/s40249-020-00753-9
Mulu, G. B., Worku, S. A., Moges, Y., and Ayelign, B. (2020). Preparedness and Responses of Healthcare Providers to Combat the Spread of COVID-19 Among North Shewa Zone Hospitals , Amhara , Ethiopia. Infect. Drug Resist. [Internet] 13 (September), 71–78. doi:10.2147/IDR.S265829
Musa, S. S., Zhao, S., Wang, M. H., Habib, A. G., Mustapha, U. T., and He, D. (2020). Estimation of Exponential Growth Rate and Basic Reproduction Number of the Coronavirus Disease 2019 ( COVID-19 ) in Africa. BMC Res. Notes [Internet 9, 1. doi:10.1186/s40249-020-00718-y
Nations, U., Educational, S., and Coi for, E. P. (2020). Competency-based Approach to Technical and Vocational Education and Training in Africa Competency-Based Approach to Technical and Vocational Education. [Internet].
Nkansah, C., Serwaa, D., Adarkwah, L. A., Osei-Boakye, F., Mensah, K., Tetteh, P., et al. (2020). Novel Coronavirus Disease 2019: Knowledge, Practice and Preparedness: A Survey of Healthcare Workers in the Offinso-north District, Ghana. Pan Afr. Med. J. 35 (Suppl. 2), 1–6. doi:10.11604/pamj.supp.2020.35.2.23644
Pradipta, D. J., Pradnyana, I. N. P., and Raharjo, T. (2020). The New Normal Strategy for Project Management in Directorate General of Customs and Excise. 3rd International Conference on Computer and Informatics Engineering. New York, NY: IC2IE, 249–254. doi:10.1109/ic2ie50715.2020.9274568
Pragholapati, A. (). New Normal “Indonesia” after Covid-19 Pandemic, Vol. 20190. doi:10.31234/osf.io/7snqb
Roberts, J. A., and David, M. E. (2021). Improving Predictions of COVID-19 Preventive Behavior : Development of a Sequential Mediation Model Corresponding Author . J. Med. INTERNET Res. 23, 1–10. doi:10.2196/23218
Sazali, M. F., Sharizman, S., Abdul, S., Mohamed, M. H., Tze, N., Pang, P., et al. (2021). Knowledge , attitude and practice on COVID-19 among students during the early phase of pandemic in a university in Borneo , Malaysia on om m er ci al us e on ly on m er al. J. Public Health Res. 10, 22.
Scroll, P., and For, D. (2021). Challenges in Distance Education during the ( Covid- 19) Pandemic Period. PLoS One [Internet] 9, 328–360. doi:10.17583/qre.2020.5872
Stanley, P. (2020). Another Decade , Another Coronavirus. N. Engl. J. Med. [Internet] 38 (February), 760–762. doi:10.1056/NEJMe1917479
ECDC (2020). Coronavirus Disease 2019 (COVID-19) Pandemic: Increased Transmission in the EU/EEA and the UK – Seventh Update [Internet], Vol. 2019. European Center for Disease Prevention and Control, 31. Available from: https://www.ecdc.europa.eu/sites/default/files/documents/RRA-seventh-update-Outbreak-of-coronavirus-disease-COVID-19.pdf (Accessed March 25, 2020).
Tadesse, T., Alemu, T., Amogne, G., Endazenaw, G., and Mamo, E. (2020). Predictors of Coronavirus Disease 2019 (COVID-19) Prevention Practices Using Health Belief Model Among Employees in Addis Ababa, Ethiopia, 2020. Infect. Drug Resist. 13, 3751–3761. doi:10.2147/IDR.S275933
Thompson, R. (2020). Pandemic Potential of 2019-nCoV. Lancet Infect. Dis. 20 (20), 280. doi:10.1016/S1473-3099(20)30068-2
UNESCO. COVID-19 (/covid19) Adverse Consequences of School Closures [Internet]. Vol. 19. 2020. doi:10.1108/DPM-07-2017-0173/full/
W/Mariam Tg, , Ayanaw, B. K., Asratie, M. H., and Abate, A. T. (2020). The Effects of Fear and Knowledge of COVID-19 on Preventive Practice Among Pregnant Women Who Attend Antenatal Care in Northwest Ethiopia, 13. Newzealand: Institution-Based Cross-Sectional StudyDoc Guid [Internet, 95–100. doi:10.2147/IJWH.S286088
Wang, C. J., Ng, C. Y., and Brook, R. H. (2020). Response to COVID-19 in Taiwan: Big Data Analytics, New Technology, and Proactive Testing. JAMA - J. Am. Med. Assoc. [Internet] 323 (14), 1341–1342. Available at:. doi:10.1001/jama.2020.3151
Who Director-General, (2020). WHO Director-General’s Opening Remarks at the media Briefing on COVID-19 - 12 October 2020. World Heal Organ [Internet]. Available at: https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---12-october-2020 (Accessed December 27, 2020).
Who, (2020). COVID-19 STRATEGY UPDATE. Available at: www.who.int/emergencies/en.
World Health Organization (2021). From the “ New normal ” to a “ New Future ”: A Sustainable Response to COVID-19, 12–14. Available at: https://www.who.int/westernpacific/news/commentaries/detail-hq/from-the-new-normal-to-a-new-future-a-sustainable-response-to-covid-19 (Accessed October 13, 2020).
World Health Organization (Who) (2021). Towards A New New Normal : Nationwide COVID-19 Prevention Campaign, 2020–2022. Available at: https://www.who.int/srilanka/news/detail/06-10-2020-towards-a-new-new-normal-nationwide-covid-19-prevention-campaign (Accessed October 6, 2021).
Ye, Y., Wang, R., Feng, D., Wu, R., Li, Z., Long, C., et al. (2020). The Recommended and Excessive Preventive Behaviors during the COVID-19 Pandemic: A Community-Based Online Survey in China. Int. J. Environ. Res. Public Health 17 (19), 1–17. doi:10.3390/ijerph17196953
Zhong, B., Luo, W., Li, H., Zhang, Q., Liu, X., Li, W., et al. (2020). Knowledge, Attitudes , and Practices towards COVID-19 Among Chinese Residents during the Rapid Rise Period of the COVID-19 Outbreak : a Quick Online Cross-Sectional Survey. Int. J. Biol. Sci. [Internet] 16, 10. doi:10.7150/ijbs.45221
Keywords: adaptation, COVID-19 prevention campaign, intention, readiness, new normal
Citation: Taye BT, Mihret MS, Tiguh AE, Dinberu MT, Kitaw TM, Tessema SD, Zerihun MS, Haile AB, Worku SA, Amogne FK, Amare NS, Demisse TL, Ambaw YL, Dagnaw AM, Ferede AA, Wondie KY and Kebede AA (2021) Readiness and Intention for Adapting New Normal COVID-19 Prevention Campaign for Sustainable Response Among Debre Berhan University Student’s During Campus Re-Entry: A Cross-Sectional Study. Front. Educ. 6:762943. doi: 10.3389/feduc.2021.762943
Received: 23 August 2021; Accepted: 21 September 2021;
Published: 18 October 2021.
Edited by:
Adrian Castro-Lopez, University of Oviedo, SpainReviewed by:
Lakia Scott, Baylor University, United StatesMelaku Ashagrie Belete, Wollo University, Ethiopia
Copyright © 2021 Taye, Mihret, Tiguh, Dinberu, Kitaw, Tessema, Zerihun, Haile, Worku, Amogne, Amare, Demisse, Ambaw, Dagnaw, Ferede, Wondie and Kebede. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Birhan Tsegaw Taye, tsegawbirhan2@gmail.com
 Birhan Tsegaw Taye
Birhan Tsegaw Taye Muhabaw Shumye Mihret2
Muhabaw Shumye Mihret2 Mesfin Tadese Dinberu
Mesfin Tadese Dinberu Mulualem Silesh Zerihun
Mulualem Silesh Zerihun Fetene Kasahun Amogne
Fetene Kasahun Amogne Azmeraw Ambachew Kebede
Azmeraw Ambachew Kebede