- 1Department of Pathology, St. Matthew’s University, Grand Cayman, Cayman Islands
- 2Department of Psychology, University of Leicester, Leicester, United Kingdom
- 3Department of Student Affairs, St. Matthew's University, Grand Cayman, Cayman Islands
- 4Department of Clinical Medicine, St. Matthew's University, Grand Cayman, Cayman Islands
Background: Community service learning seems to positively impact undergraduate medical students’ practical procedural and communications skills. Events like health fairs also strengthen the bond between healthcare providers and the wider community. Recognizing this mutually beneficial situation, national accreditation agencies and medical boards have recommended incorporating community-based learning in the core undergraduate curriculum. Our university is the first to probe medical students’ perceptions of community service in our region to the best of our knowledge.
Objectives: We sought to analyze the experience of our students to improve the practical value of the curriculum.
Methods: This was a qualitative survey interviewing medical students volunteering at a health fair in a Caribbean Island aimed to screen gross cardio-vascular and metabolic abnormalities in the native adult population. The focus group interviews were processed, transcribed and coded for thematic analyses by independent observers.
Results: Overall, the students perceived CS as an opportunity to improve their clinical procedural and communications skills and to apply theoretical medical knowledge in practice to detect undiagnosed conditions like diabetes mellitus, hypertension and nutritional imbalance.
Pedagogical implications: We have increased practical laboratory sessions by 15% in the new semester to improve our students’ practical skills.
Conclusions: This is the first study that describes how community service may influence the individual learning curve of undergraduate medical students and may serve as a quality improvement tool to guide amendments to the curriculum. We opine that inter-agency, community-focused service promotes social, peer and active learning amongst undergraduate medical students.
Introduction
Community Service-learning (CSL) facilitates not only the implementation of theoretical knowledge in practice with the real-world demonstration of skills and boosts student learning outcomes (Buckner et al., 2010; Hunt et al., 2011; Claramita et al., 2019). It can take many forms that provide a rich learning experience to students that they may not encounter during their clinical rotations. Inter-agency events involving medical schools and community healthcare establishments have increasingly become an integral part of undergraduate medical education (Playford et al., 2017; Cohen et al., 2019; Sin et al., 2019), a concept also strongly recommended by Element 6.6 of the Liaison Committee on Medical Education (2021). Integrated CSL events address pragmatic public health concerns while helping students meet particular learning objectives so benefitting the community and individual (Long et al., 2011; Vyas et al., 2011; Lee et al., 2016; Tanna et al., 2020).
One of the prominent theories of learning by John Dewey describes the concept of an active connection between knowledge and experience by engagement with the real world outside of the classroom (Dewey et al., 1996; You and Rud, 2010). According to him, reflection is paramount in the process of learning. It involves recollection of the occurrence and exploring through questioning the reason of happenings and also thinking as to what actions could have led to a different conclusion (Dewey, 1998). Based on Dewey’s work, various models have been proposed, including reflection as a salient component. One of the dominant models of experiential learning given by David Kolb (1984) incorporated the reflection process into his learning cycle. It includes- “reflection on concrete experience, thoughtful observations, abstract conceptualization, and active experimentation leads to the inclusion of reflective activities before, during and after service as a part of service-learning assignments” (Sugarman and Kolb, 1987).
CSL has been recognized as an essential aspect of medical education (Dornan et al., 2007; Kandiah, 2017; Wang et al., 2020). Students can relate what they learn in the classroom to real-life situations and engage in self-reflection (Celio et al., 2011; Warren, 2012). Also, it can help to appreciate community-based problems and identify community resources for patients (Warren, 2012; Yorio and Ye, 2012). Despite promising evidence, however, most medical schools have not incorporated it formally into their curriculum. Some have started to revise the curriculum by including service-learning as an integral part others made it elective (Brush et al., 2006; Elam et al., 2003). Lack of standardized definitions and outcome measuring outcomes, the benefit of such a program in undergraduate medical education is mainly unknown (Dharamsi et al., 2010; Mc Menamin et al., 2014; Stewart and Wubbena, 2015).
At St. Matthews University, we integrated elective (non-graded) CSL opportunities into the basic sciences curriculum. Ours is a structured, competency-based medical education system that includes six core competencies-practice-based learning and improvement, patient care and procedural skills, systems-based practice, medical knowledge, interpersonal and communication skills, and professionalism. With a qualitative survey, we aimed to contribute to the existing evidence on CSL and used the collected data to drive a Quality Improvement Project to better our curriculum. Unfortunately, to the best of our knowledge, there have been no similar projects in the Caribbean.
Methods
Study Design, Participants and Procedure
It is a descriptive and interpretive qualitative study of thematic analysis of the student perceptions per (Kiger and Varpio, 2020). The students were in their first and second year of a 4-yr undergraduate medical degree. We have chosen this method because it best reflects Kolb’s learning cycle theory to underpin such qualitative research. Figure 1 illustrates the application of the learning cycle and the steps of our research.
All students from semester two to four were invited to take part in the project. Semester one students were excluded as not having sufficient clinical backgrounds to undertake nursing assistant tasks. Information letter was sent to all students via email. Participants were made aware of the research and were mandated to a signed informed consent, which could have been revoked at any time point. Participation was voluntary (unincentivized) basis and 15 students agreed to visit the health fair. A 2-day health fair was organized in conjunction with the local healthcare authority. A convenience sampling technique was used to divide participants into two groups (n = 7 and n = 8) by the faculty for visit on separate days.
Two focus groups were held on separate days with 15 (n = 7 and n = 8) with students completing 4 h of service as nurse assistants on the health fair. Personal data was managed per the principles of the GDPR and the local regulations.
Ethical approval- The research was conducted after ethical approval from the SMU University ethics review committee (SMU- 1552).
Settings: The annual health fair is a free weekend event for adult residents of the Cayman Islands, offering non-fasting glucose testing (Roche XXX), recording height, weight and taking the vital signs, including blood pressure measurement (Omron XX). Both residents and the attending staff spoke English. The medical students (semesters two, three and four) assisted the nurses in all procedures. Before the event, all medical students received the same standardized training and were signed off for competency by two faculty of the university.
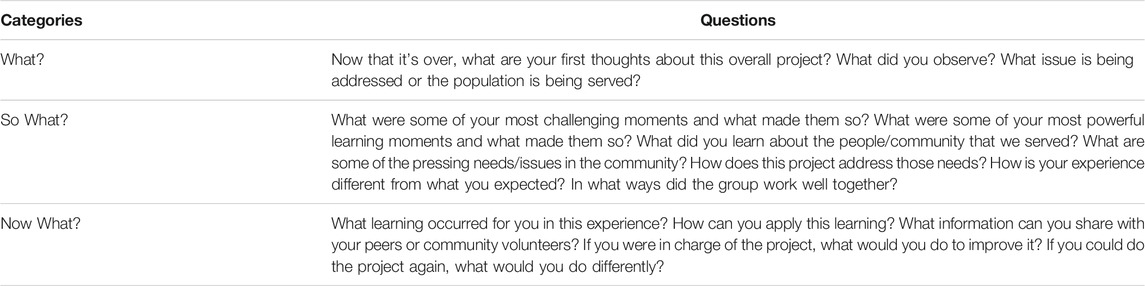
Data collection: To avoid recollection bias, focus group discussions (50 min) were held for each group of students on a prearranged and mutually agreed day in the week following the CSL event. Discussions were conducted on different days using a prospectively developed questionnaire (a similar questionnaire was validated by Simons and Cleary (2006) (SeeTable 1). Where appropriate, the interviewer faculty prompted participants to expand on their responses. The same faculty interviewed all students. Additional 10 min were given to each student to reflect on and document their experiences.
Data analyses: The process of data analysis was inductive and performed until no new codes or concepts emerged. In line with previous literature, an audit trail was developed to ensure rigor, including ongoing notes of all activities, discussions, and decisions made to enable others to judge the trustworthiness and dependability of the findings and interpretation (Nowell et al., 2017). Firstly, the interview was transcribed in the NVivo software (NVIVO, 2021, RRID:SCR_014802 version 2021). Further, two authors read it many times (SN/AB) before coding, also known as “Familiarization.” Next, the coding process started with a detailed, “line-by-line” coding of the focus group transcripts. As traditionally, line-by-line did involve, as the name suggests, coding each line of the transcript. In the second stage of analysis, these codes were scrutinized, and the authors reviewed transcripts and re-read them several times (SN/ID/AB). This procedure ensured that the created codes accurately described the original data and that there were no duplicates (codes covering the same content but of different wording). The descriptive codes were organized into a parent-child relationship (hierarchical organization). Subsequently, after duplicates were eliminated, themes were generated, combining several codes into a single theme. Finally, too vague or irrelevant themes were discarded. Eventually, to ensure the validity of themes, they were independently reviewed by a researcher (SN).
Results
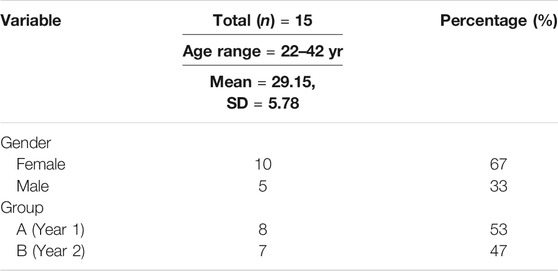
A total of 15 students in two groups participated in this program as shown in Table 2.
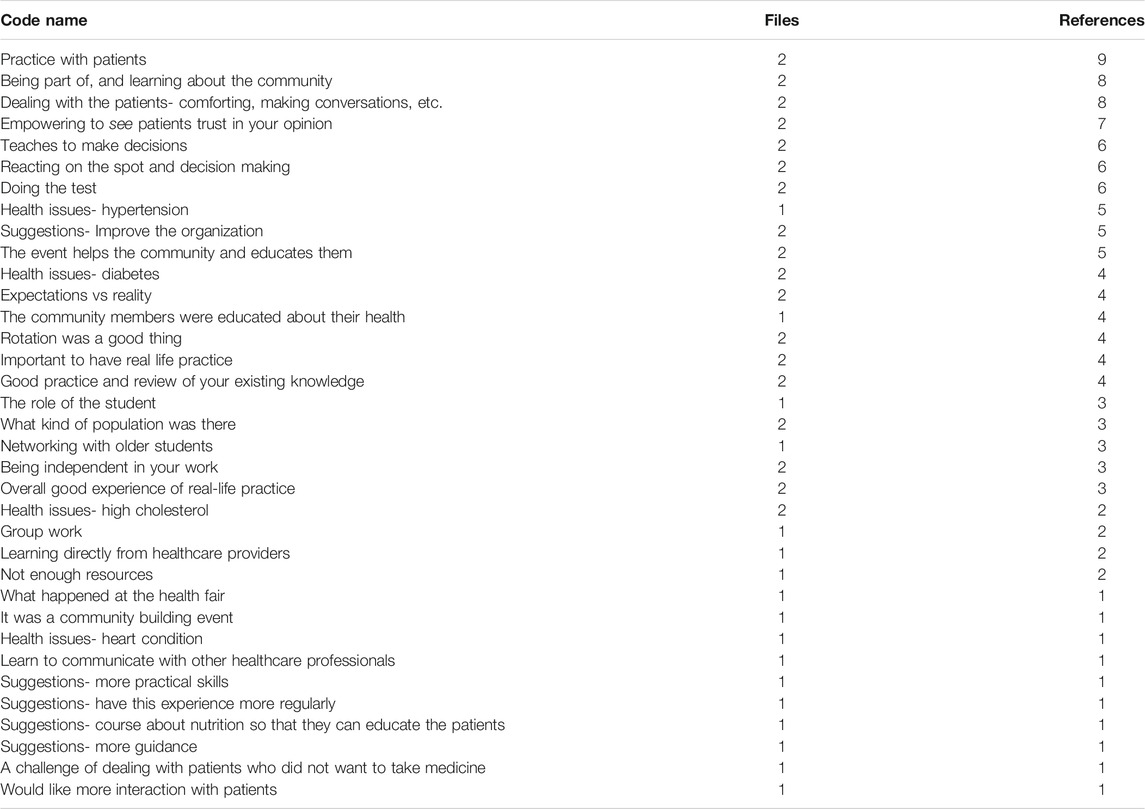
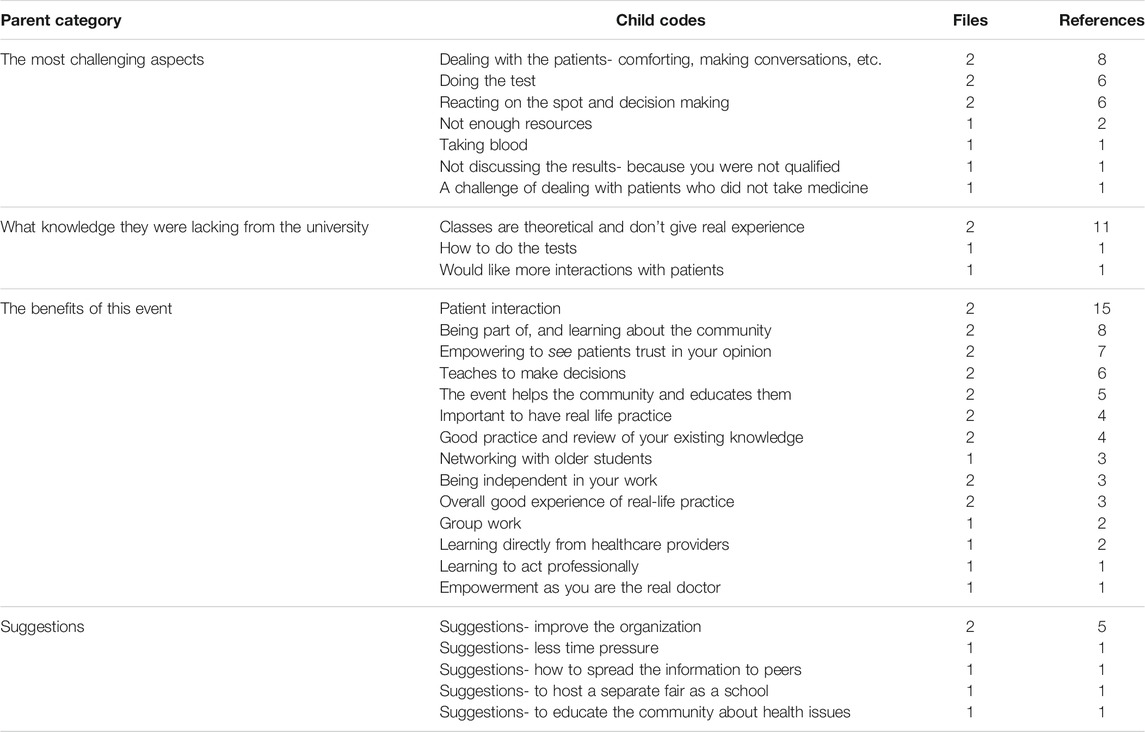
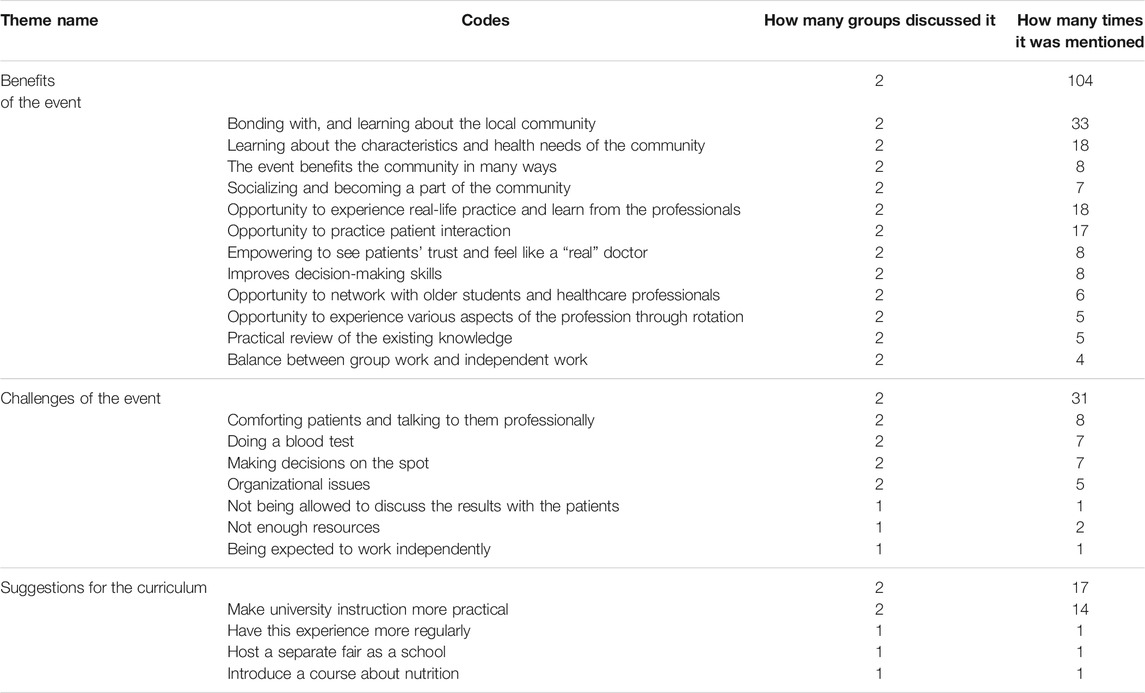
During line-by-line coding, 48 codes were recognized as shown in Table 3. Four main themes were generated from these codes (Table 4). These included:
A. The most challenging aspect
B. The knowledge they were lacking from the university
C. The benefits of this event
D. Suggestions
Subsequently, the themes were reviewed and the final three themes were generated (Table 5).
Benefits of the Event
The most discussed theme in the benefits was bonding with and learning about the local community (coded 33 times) (seeTable 4). It involved learning about the: Characteristics and health needs of the community (coded 18 times).
Female student one (group one): “They were healthy from what I saw. Not terrible, but I think they went there for a part of the health fair because it was offered to them for free.”
Female student three (group one): “For me, it became pretty clear that we have served an underserved community. Some of these patients do not go to see doctors. They wait for the health fairs because they know they can get free screening and see a physician afterward.”
Learning that the event benefits the community in many ways (coded eight times).
Female student three (group one): “What they were able to do is get a full screening, a meeting with health staff and the physician, and essentially, further planning for free.”
Socializing and becoming a part of the community (coded seven times).
Female student six (group one): “It was like a community-building event, and we were also part of that.”
Another benefit of the health fair discussed was “opportunity to experience real-life practice and learn from the professionals.
Male student two (group two): who had “never really had the chance to volunteer to events like these,” felt that he “definitely learned a lot,” including “how to take blood pressure, BMI and especially the blood glucose.”
Male student four (group one): “Like nothing can prepare you until you do it, and it is literally through mistakes that you learn the best ways.”
This led to another discussed benefit of the event: a “practical review of the existing knowledge” (coded five times).Female student four (group two): “We did a class last week taking patients’ history. That was useful because that was the first station I was on. I know that in our lecture, they were talking about the importance of making the patient feel comfortable.”
Another widely discussed benefit of the event was the “opportunity to practice patient interaction” (coded 17 times). The participants felt that it was a “big learning point” to learn how to communicate with patients, adapt to their age and needs, and comfort them.
Female student four (group two): “Because there were so many different ages when I was talking to a child, I had to speak about different things and change my tone compared to when I was talking to a more mature individual.”
Related to the benefit of patient interaction, another benefit recognized by students was “empowering to see patients” trust and feel like a “real” doctor (coded eight times). For example, a student was impressed by “how the patients trusted our opinion so much, and they valued what we had to say about their results.” She described this sense as being “the most memorable thing” and an experience that reminded her that “you are becoming physicians for a good reason.”
Similarly, a student reflected on the experience, describing a shift in her self-positioning compared to being a student in a classroom.
Another benefit of the health fair was that it “improves decision-making skills” (coded eight times). As generally, “you get to see a better variety of patients” at such events, the participants were exposed to various uncommon situations. In some of these instances, they observed other health professionals making the decisions, and in others, they were the ones making them. A “challenging” patient who “was getting very apprehensive, but he wanted his test to be done.” The situation required the student to calm the patient down, and even though this experience was challenging, she seemed to appreciate it as a valuable one.
The participants also commented on the “opportunity to network with older students and healthcare professionals” (coded six times). As previously noted, they interacted with healthcare professionals, and not only did they learn a lot from them professionally, but they also appreciated the value of the interaction itself. In addition, they collaborated and interacted with older students, which contributed to their professional knowledge and potentially developing friendships.
Female student six (group one): “I enjoyed how we were at the afternoon shift, but people from the morning shift took their time to stay back and teach us how to do everything. Moreover, interactions with the fifth, fourth, third semesters opened up new friendships here. It was nice because I met a good number of students, and I was a first-semester.”
The teamwork aspect evident in the above extract also leads to another advantage of the event: there seems to have been the right “balance between group work and independent work” (coded four times).
Female student two (group one): “When I had a problem, I told him that I need help, so he walked me through it, helped me, and confirmed that I could do it. So, it was beneficial. It made me feel better, made the patient feel better, it was calming in that stressful situation.”
Regarding the organization of the event and the students’ work, the final discussed benefit was that the event provided an “opportunity to experience various aspects of professional practice through rotation” (coded five times). The students “rotated around” (Male student one group one) various stations where they experienced various jobs and responsibilities, which gave them a feeling that “we had adequate training” and “we were all comfortable” (Female student three group one).
Challenges of the Event
Although, as previously noted, the participants generally praised the “opportunity to practice patient interaction, comforting patients and talking to them professionally” (coded eight times) was also mentioned as the most challenging aspect of the volunteering experience. For example, one student (female student group two) struggled with a patient who was afraid of needles and had to have the blood taken several times as “his blood was clotted.” As a result, the patient was “getting very apprehensive,” and “calming him down while trying to get enough blood from him was very difficult.” However, another student (female student group one), in turn, commented on the time when “the test takes a few minutes to run,” in which case “making conversation, finding that common ground, making the patients feel comfortable” was challenging.
The second most discussed challenge that partially emerged in the above discussion was the challenge of “doing the blood test” (coded seven times) “Making decisions on the spot” (coded seven times) was also difficult. However, as previously noted, the participants also recognized the value of learning to make difficult decisions. For example, a student (group two male) reported that some patients who had a heart condition “admitted to not taking medicine because they did not want to.” As a result, he was confused and admitted to not knowing “what do you even do at that point,” which he found to be an “issue.”
Another challenge was “organizational issues” (coded five times), which also related in some cases to the “lack of “(coded twice). For example, a student (female; group two) felt that, at times, “it was just very disorganized and not put together.” As she noted, “one of the nurses had to go to the GP office and take their glucometer because we did not have a working one.”
“Not being allowed to discuss the results with the patient” (coded once) was believed to be a challenge by a student from group one, who explained that “once I gave the patient the results,” “it was hard to not then discuss the results with them.”
Finally, although, as previously noted, the participants generally praised the opportunity to work independently, while a student from group two felt that expectation to work independently was challenging at times and stated, “They were instilling in confidence in us, and it was kind of nice that they trusted us, it is a little nerve-wracking at first to be working on your own.”
Quality Improvement Project based on Theme 3 (Suggestions for the curriculum)
Although the interview’s main focus was on the participants’ evaluation of the event, including its main benefits and challenges, several “suggestions for the curriculum” (coded 17 times) were openly made. The most common suggestion was to “make university instruction more practical” (coded 14 times). Several of these benefits are explicitly related to the opportunities to practice skills needed in the profession and implement the previously gained theoretical knowledge into practice. As previously noted, the participants made several comments in which they explained how vital practical skills are. Table 6 lists the medical school competencies addressed by the students in this research. According to the global medical education trend, most Caribbean universities have now incorporated CSL hours as a prerequisite for graduation. However, ours is the first project when credit hours were introduced into the curriculum for CSL, and student feedback actively shaped the following year’s curriculum. In the third semester, we increased simulation laboratory hours by 15 percent to enhance essential clinical skills.
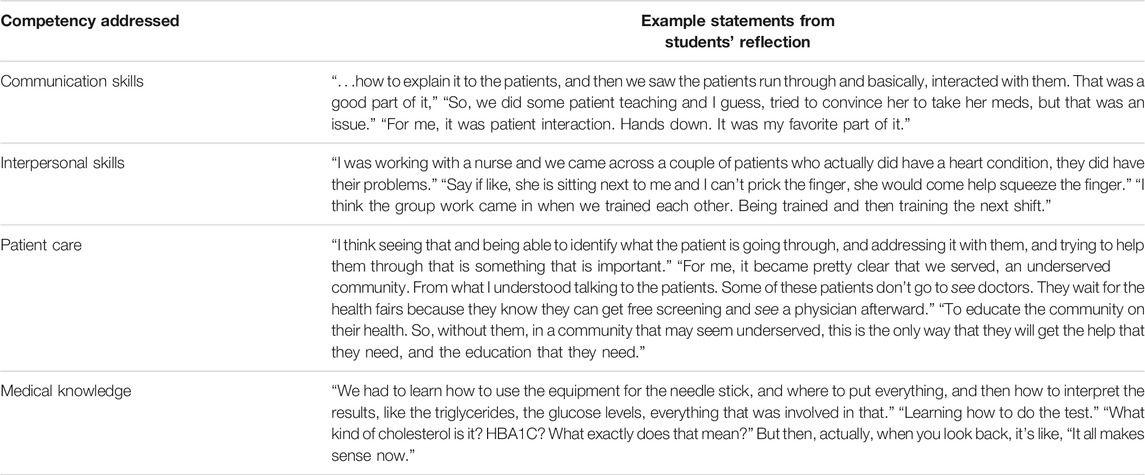
TABLE 6. Attainment of the competencies and learning objectives with quotes from student reflection.
Discussion
The current study involved CSL as an active learning strategy framed by the experiential-learning theory inspired by Dewey and popularized by Kolb (1984). Our study explored medical student perceptions and expectations of a CSL experience and competencies attained. Overall, students reported positive perceptions of community service, including reports on characteristics and health needs of the society, enhancement relationship with seniors and others, and having higher levels of responsibility due to direct clinical “hands-on” experience compared to learning at medical school. In addition, this experiential learning pursued a framework to examine the correlation between classroom-acquired medical knowledge and its community healthcare application.
Various CSL models that researchers have proposed are targeted towards creating community-oriented healthcare professionals aligned with identification and addressing the health care needs of society. The true goal of medical education is to work in collaboration with society and strive to improve health systems and patient care (Davis and Gonzalo, 2019). This collaboration underpins the increasing need for medical students to learn the functioning of a physician in society (Asgary et al., 2016; Meili et al., 2011).
Another important finding of our study, peer learning and support, has also been described by researchers as enhancing medical knowledge, procedural skills, and the professional development of all students involved in such interactions (Held et al., 2019). While developing a culture of community outreach, CSL programs similar to ours have also shown improvement in student attitudes towards patients and the development of social accountability (Porter et al., 2015). However, more sophisticated and longitudinal research is required to know the long-term benefits of the community and academic partnerships.
Common challenges our students faced included comforting and communicating professionally, working independently, organizational issues, lack of resources and ethical issues. Similar to our findings, studies have listed CSL challenges, including language and cultural barriers or potentially harming the patient (Loh et al., 2015; Rovers et al., 2016). A similar potential adverse effect from the same study included creating dependencies of local communities on the local clinic or at the level of government policies and health insurance (Rovers et al., 2016). Funding has also been a crucial factor for the sustainability of such projects (Loh et al., 2015).
During the discussion, the students put many suggestions, which included the incorporation of more practical skills. Furthermore, students urged to have more opportunities like this by organizing a health fair by the university. Many students also suggested adding nutrition as a core module in their curriculum to help patients focus on disease prevention. Modern-day educational models now focus more than before and have increased teaching time for nutrition courses in medical school (Schoettler et al., 2015).
Another aim of the study was to see attained competencies during self-reflection. Communication and interpersonal skills, practice-based learning and improvement, patient care and procedural skills and medical knowledge were the top competencies discussed after the event. This result seems to be consistent with the previous research (Brown, 2017). These competencies help a medical student understand the functioning of a physician in society and aim for the true goal of medical education: to work in collaboration with society and strive to improve health systems and patient care.
Limitations
The limitation of the present study includes the limitation of the coding process and themes due to the exact wording and focus of the questions and by those not included. Another limitation was the small number of participants in this study; thus, the results cannot be generalized to the population. Also, the results are not transferable universally, as all students were from SMU, and the study was conducted in the same university. Finally, another limitation includes the influences by others’ comments and sentiments in focus groups versus private interviews and opinions. Despite the very robust methodology, group discussion might mitigate recall bias on the one hand; however, it could have potentially confounded the individual impressions or thoughts.
Conclusion
CSL program in medical school is a structured learning experience involving the active participation of medical students and faculty in coordination with physicians and community healthcare workers. Such programs are developed to align community-identified health concerns to the medical school curricular learning objectives. Most of the programs worldwide are structured to include the students’ learning experience with a community partner and include an orientation, service experience and post-experience reflection component.
This study aimed to explore students’ perceptions of CSL and identify attained competencies in basic sciences medical students. In addition, CSL presented the benefits of bonding with the community and enhancing student’s medical knowledge. Such events expose students to various people in the community, such as patients and healthcare professionals, which increases the competence of a medical student. Thus, medical educators should focus on creating such community programs that align medical education with public healthcare. In medical education, service-learning can strengthen medical school and community connections, benefit the lives of the underserved and educate future medical practitioners to address and prevent health problems and promote community health.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by St. Matthews University (SMU) School of Medicine Institutional Review Board. The patients/participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author Contributions
AB and SN conceived of the presented idea. ShN developed the theory and performed the data analyses. AB and ID verified the analytical methods. AB and ID supervised the findings of this work. GX reviewed and edited final versions. All authors discussed the results and contributed to the final manuscript.
Funding
The project was fully funded and supported by the St. Matthews University School of Medicine, Cayman Islands.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
This article was previously presented as a meeting abstract at the 2020 IAMSE Annual Meeting on June 15–18, 2020 and can be found at http://www.iamse.org/wp-content/uploads/2020/06/227-Nauhria.pdf. This article was also previously posted to the Research Square preprint server on December 16, 2020, and can be found at 10.21203/rs.3.rs-126072/v1.
References
Asgary, R., Naderi, R., Gaughran, M., and Sckell, B. (2016). A Collaborative Clinical and Population-Based Curriculum for Medical Students to Address Primary Care Needs of the Homeless in New York City Shelters : Teaching Homeless Healthcare to Medical Students. Perspect. Med. Educ. 5 (3), 154–162. doi:10.1007/s40037-016-0270-8
Brown, C. L. (2017). Linking Public Health Nursing Competencies and Service-Learning in a Global Setting. Public Health Nurs. 34 (5), 485–492. doi:10.1111/phn.12330
Brush, D. R., Markert, R. J., and Lazarus, C. J. (2006). The Relationship Between Service Learning and Medical Student Academic and Professional Outcomes. Teach. Learn. Med. 18 (1), 9–13. doi:10.1207/s15328015tlm1801_3
Buckner, A. V., Ndjakani, Y. D., Banks, B., and Blumenthal, D. S. (2010). Using Service-Learning to Teach Community Health: The Morehouse School of Medicine Community Health Course. Acad. Med. 85 (10), 1645–1651. doi:10.1097/acm.0b013e3181f08348
Celio, C. I., Durlak, J., and Dymnicki, A. (2011). A Meta-Analysis of the Impact of Service-Learning on Students. J. Experiential Educ. 34 (2), 164–181. doi:10.1177/10538259110340020510.5193/jee34.2.164
Claramita, M., Setiawati, E. P., Kristina, T. N., Emilia, O., and van der Vleuten, C. (2019). Community-based Educational Design for Undergraduate Medical Education: A Grounded Theory Study. BMC Med. Educ. 19 (1), 258. doi:10.1186/s12909-019-1643-6
Cohen, L., Leung, F.-H., Oriuwa, C., and Wright, R. (2019). Service-learning Curriculum Design and Implementation at the University of Toronto Faculty of Medicine. Mededpublish 8 (2), 17. doi:10.15694/mep.2019.000141.1
Davis, C. R., and Gonzalo, J. D. (2019). How Medical Schools Can Promote Community Collaboration Through Health Systems Science Education. AMA J. Ethics. 21 (3), E239–E247. doi:10.1001/amajethics.2019.239
Dewey, J., Boydston, J., and Hickman, L. (1996). The Collected Works of John Dewey, 1882-1953 (2nd Release). Electronic Edition. The Later Works of John Dewey, 1925-1953. Volume 3 : 1927-1928, Essays. Charlottesville, VA: InteLex Corporation.
Dewey, J. (1998). Experience and Education: The 60th Anniversary Edition. West Lafayette, IN: Kappa Delta Pi.
Dharamsi, S., Richards, M., Louie, D., Murray, D., Berland, A., Whitfield, M., et al. (2010). Enhancing Medical Students' Conceptions of the CanMEDS Health Advocate Role Through International Service-Learning and Critical Reflection: A Phenomenological Study. Med. Teach. 32 (12), 977–982. doi:10.3109/01421590903394579
Dornan, T., Boshuizen, H., King, N., and Scherpbier, A. (2007). Experience-based Learning: A Model Linking the Processes and Outcomes of Medical Students' Workplace Learning. Med. Educ. 41 (1), 84–91. doi:10.1111/j.1365-2929.2006.02652.x
Elam, C. L., Sauer, M. J., Stratton, T. D., Skelton, J., Crocker, D., and Musick, D. W. (2003). Service Learning in the Medical Curriculum: Developing and Evaluating an Elective Experience. Teach. Learn. Med. 15 (3), 194–203. doi:10.1207/s15328015tlm1503_08
Held, F. P., Roberts, C., Daly, M., and Brunero, C. (2019). Learning Relationships in Community-Based Service-Learning: A Social Network Analysis. BMC Med. Educ. 19 (1), 113. doi:10.1186/s12909-019-1522-1
Hunt, J. B., Bonham, C., and Jones, L. (2011). Understanding the Goals of Service Learning and Community-Based Medical Education: A Systematic Review. Acad. Med. 86 (2), 246–251. doi:10.1097/acm.0b013e3182046481
Kandiah, D. A. (2017). Perception of Educational Value in Clinical Rotations by Medical Students. Adv. Med. Educ. Pract. 8, 149–162. doi:10.2147/amep.s129183
Kiger, M. E., and Varpio, L. (2020). Thematic Analysis of Qualitative Data: AMEE Guide No. 131. Med. Teach. 42 (8), 846–854. doi:10.1080/0142159x.2020.1755030
Kolb, D. A. (1984). Experiential Learning: Experience as the Source of Learning and Development. Englewood Cliffs, NJ: Prentice-Hall.
Lee, W. K., Harris, C. C. D., Mortensen, K. A., Long, L. M., and Sugimoto-Matsuda, J. (2016). Enhancing Student Perspectives of Humanism in Medicine: Reflections from the Kalaupapa Service Learning Project. BMC Med. Educ. 16 (1), 137. doi:10.1186/s12909-016-0664-7
Liaison Committee on Medical Education (2021). Functions And Structure of a Medical School. Available at: https://lcme.org/publications (Accessed April 14, 2014).
Loh, A. Z., Tan, J. S., Lee, J. J., and Koh, G. C. (2015). Voluntary Community Service in Medical School: A Qualitative Study on Obstacles Faced by Student Leaders and Potential Solutions. Glob. Health Action. 8 (1), 27562. doi:10.3402/gha.v8.27562
Long, J. A., Lee, R. S., Federico, S., Battaglia, C., Wong, S., and Earnest, M. (2011). Developing Leadership and Advocacy Skills in Medical Students Through Service Learning. J. Public Health Manag. Pract. 17 (4), 369–372. doi:10.1097/phh.0b013e3182140c47
Mc Menamin, R., Mc Grath, M., Cantillon, P., and Mac Farlane, A. (2014). Training Socially Responsive Health Care Graduates: Is Service Learning an Effective Educational Approach? Med. Teach. 36 (4), 291–307. doi:10.3109/0142159x.2013.873118
Meili, R., Fuller, D., and Lydiate, J. (2011). Teaching Social Accountability by Making the Links: Qualitative Evaluation of Student Experiences in a Service-Learning Project. Med. Teach. 33 (8), 659–666. doi:10.3109/0142159x.2010.530308
Nowell, L. S., Norris, J. M., White, D. E., and Moules, N. J. (2017). Thematic Analysis. Int. J. Qual. Methods 16 (1), 1–13. doi:10.1177/1609406917733847
NVIVO (2021). QSR International. Version 2021. Available at: https://www.qsrinternational.com/nvivo-qualitative-data-analysis-software/home.
Playford, D., Bailey, S., Fisher, C., Stasinska, A., Marshall, L., Gawlinski, M., et al. (2017). Twelve Tips for Implementing Effective Service Learning. Med. Teach. 41 (1), 24–27. doi:10.1080/0142159x.2017.1401217
Porter, J., Quinn, K., Kane, K., Stevermer, J., and Webb, W. (2015). How We Incorporated Service Learning into a Medical Student Rural Clinical Training Experience. Med. Teach. 38 (4), 353–357. doi:10.3109/0142159x.2015.1078889
Rovers, J., Japs, K., Truong, E., and Shah, Y. (2016). Motivations, Barriers and Ethical Understandings of Healthcare Student Volunteers on a Medical Service Trip: A Mixed Methods Study. BMC Med. Educ. 16 (1), 94. doi:10.1186/s12909-016-0618-0
Schoettler, C. L., Lee, J. N., Ireland, K. A., and Lenders, C. M. (2015). A Novel Method of Increasing Medical Student Nutrition Awareness and Education. J. Biomed. Educ. 2015, 1–8. doi:10.1155/2015/784042
Simons, L., and Cleary, B. (2006). The Influence of Service Learning on Students' Personal and Social Development. Coll. Teach. 54 (4), 307–319. doi:10.3200/ctch.54.4.307-319
Sin, D., Chew, T., Chia, T. K., Ser, J. S., Sayampanathan, A., and Koh, G. (2019). Evaluation of Constructing Care Collaboration - Nurturing Empathy and Peer-To-Peer Learning in Medical Students Who Participate in Voluntary Structured Service Learning Programmes for Migrant Workers. BMC Med. Educ. 19 (1), 304. doi:10.1186/s12909-019-1740-6
Stewart, T., and Wubbena, Z. C. (2015). A Systematic Review of Service-Learning in Medical Education: 1998-2012. Teach. Learn. Med. 27 (2), 115–122. doi:10.1080/10401334.2015.1011647
Sugarman, L. (1987). Experiential Learning: Experience as the Source of Learning and Development, David A. Kolb, Prentice-Hall International, Hemel Hempstead, Herts., 1984. No. Of Pages: Xiii + 256. J. Organiz. Behav. 8 (4), 359–360. doi:10.1002/job.4030080408
Tanna, S., Fyfe, M., and Kumar, S. (2020). Learning Through Service: A Qualitative Study of a Community-Based Placement in General Practice. Educ. Prim. Care. 31 (5), 305–310. doi:10.1080/14739879.2020.1759459
Vyas, R., Zachariah, A., Swamidasan, I., Doris, P., and Harris, I. (2011). Integration of Academic Learning and Service Development Through Guided Projects for Rural Practitioners in India. Med. Teach. 33 (7), e401. doi:10.3109/0142159x.2011.575900
Wang, J., Guo, J., Wang, Y., Yan, D., Liu, J., Zhang, Y., et al. (2020). Use of Profession-Role Exchange in an Interprofessional Student Team-Based Community Health Service-Learning Experience. BMC Med. Educ. 20 (1), 212. doi:10.1186/s12909-020-02127-z
Warren, J. L. (2012). Does Service-Learning Increase Student Learning? A Meta-Analysis. Mich. J. Community Serv. Learn. 18 (2), 56–61. Available at: https://files.eric.ed.gov/fulltext/EJ988320.pdf.
Yorio, P. L., and Ye, F. (2012). A Meta-Analysis on the Effects of Service-Learning on the Social, Personal, and Cognitive Outcomes of Learning. Amle 11 (1), 9–27. doi:10.5465/amle.2010.0072
You, Z., and Rud, A. G. (2010). A Model of Dewey's Moral Imagination for Service Learning: Theoretical Explorations and Implications for Practice in Higher Education. Educ. Cult. 26 (2), 36–51. Available at: https://docs.lib.purdue.edu/cgi/viewcontent.cgi?article=1245&context=eandc.
Keywords: service learning, medical students, undergraduate, social learning, community service
Citation: Nauhria S, Nauhria S, Derksen I, Basu A and Xantus G (2021) The Impact of Community Service Experience on the Undergraduate Students’ Learning Curve and Subsequent Changes of the Curriculum- A Quality Improvement Project at a Caribbean Medical University. Front. Educ. 6:709411. doi: 10.3389/feduc.2021.709411
Received: 13 May 2021; Accepted: 25 August 2021;
Published: 10 September 2021.
Edited by:
Ehsan Namaziandost, Islamic Azad University of Shahrekord, IranReviewed by:
Ansar Abbas, Airlangga University, IndonesiaReza Kafipour, Shiraz University of Medical Sciences, Iran
Copyright © 2021 Nauhria, Nauhria, Derksen, Basu and Xantus. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Samal Nauhria, c2FtYWxuYXVocmlhQGdtYWlsLmNvbQ==
 Samal Nauhria
Samal Nauhria Shreya Nauhria
Shreya Nauhria Irene Derksen3
Irene Derksen3