- 1Department of Health Management and Policy, University of Michigan School of Public Health, Ann Arbor, MI, United States
- 2Department of Psychiatry, Michigan Medicine, Ann Arbor, MI, United States
- 3Department of Survey Research, University of Michigan Institute of Social Research, Ann Arbor, MI, United States
School closures due to COVID-19 left students in Michigan without physical access to school mental health professionals (SMHPs) and other supports typically available in schools. This report examines the needs of SMHPs across Michigan during the early months of the COVID-19 pandemic and how those needs informed programming and resources provided by a University of Michigan school mental health training and implementation program. In April 2020, a web-based survey asking about student and SMHP mental health was sent to 263 SMHPs who had previously participated in this program. 155 SMHPs (58.9%) responded. Nearly half of SMHPs reported their students’ most pressing needs were support for self-care, anxiety, depression, and traumatic stress. Some SMHPs also met screening criteria themselves for depression and/or anxiety. This survey provided an overview of SMHPs’ concerns early in the COVID-19 pandemic and drove development of new COVID-19-related resources designed to support SMHPs.
Introduction
High schools increasingly provide numerous services to students, including mental health support. Historically, the inclusion of general health care in the school setting (e.g., school nurses) began in the early 20th century and was increasingly common by the 1980s (Flaherty and Osher, 2003). From that point, the provision of comprehensive health services, including mental health services, in the school setting has gained attention, but has typically seen slower adoption and lower funding than other services (Flaherty and Osher, 2003; Weir, 2020). Despite challenges, school-based mental health care delivered by trained, mental health professionals has become an important resource for students facing anxiety, depression, and other mental health concerns.
School-based delivery of mental health services for students is particularly important in light of numerous barriers that preclude most young people from accessing needed clinic- or community-based mental health treatment (Brener et al., 2001; Burns et al., 1995; Schlitt et al., 2000). Barriers to care include logistical or practical challenges, such as insufficient numbers of qualified child and adolescent mental health providers, long wait lists, and inadequate insurance coverage; as well as more nuanced or societal challenges, such as social stigma, shame, or mistrust of the healthcare system (Brener et al., 2001). These barriers are often most pronounced in settings impacted by social determinants of health. For example, communities impacted by poverty and limited resources may also have higher rates of trauma exposure, family stress, and mental health concerns (Burns et al., 1995; Schlitt et al., 2000). Thus, embedding mental health services in schools provides a critical strategy for addressing significant inequities in health care access.
As mental health care has increasingly been provided in the school setting, the various models of service delivery have adapted based on funding, program creation, and students’ needs (Flaherty et al., 1996). Currently, school-based mental health delivery often involves first screening students to identify their needs (Fazel et al., 2014). Students with identified symptoms may be offered an intervention, typically provided by a school mental health professional (SMHP; school social workers, counselors, psychologists, etc.) (Whiston and Quinby, 2009). These interventions can be delivered individually or via structured group sessions (Whiston and Quinby, 2009). Research conducted prior to and during the COVID-19 pandemic shows that schools are the most frequent setting in which youth receive mental health care, including treatment for anxiety disorders (e.g., Social Anxiety Disorder), mood disorders (e.g., Major Depressive Disorder), and other mental health concerns (Costello et al., 2014; Duong et al., 2020).
Given this context, when Michigan Governor Gretchen Whitmer mandated closure of all K-12 school buildings across the state on March 16, 2020 (Whitmer-Executive Order, 2020-05; Whitmer-Executive Order, 2020-35), students were left without physical access to an important source of mental health care (Lee and Ward, 2020). At the same time, the COVID-19 pandemic brought about unparalleled shifts in social circumstances, such as social distancing and quarantine guidelines (CDC, 2020), that contributed to increased social isolation and decreased social support for students, further impacting mental health (Jones et al., 2021). These changes highlighted the important role that mental health care often plays in promoting learning, as seen through the development of school-based mental health in the 1990s, and renewed calls to prioritize mental health delivery in the school setting in response to its sudden in-person absence (Flaherty and Osher, 2003; Weir, 2020).
For educators and school staff, COVID-19 school closures produced a number of new challenges in the delivery of mental health support. For example, in a sample of 583 adolescents (80% female, 71% White) surveyed between April 27 and July 13, 2020, symptoms of depression were reported among 55%, anxiety among 48%, and Post-Traumatic Stress among 45% (Jones et al., 2021; Murata et al., 2021; Zhou S.-J. et al., 2020). These rates are higher than those observed prior to the COVID-19 pandemic. Further, circumstances have placed SMHPs at higher risks of anxiety, emotional exhaustion, and depressive symptoms than before the pandemic (Joshi and Sharma, 2020). Increased prevalence of anxiety and depression (Muller et al., 2020), as well as sleep disturbances and intense grief reactions (Murata et al., 2021), have been identified among health care workers who, much like SMHPs, have had their work significantly impacted by COVID-19 (Joshi and Sharma, 2020). COVID-19 school closures also resulted in new barriers to school-based mental health services, further magnifying the increased mental health needs of both students and SMHPs (Asarnow et al., 2005; Costello et al., 2014; Jones et al., 2021; Weist et al., 2007).
Virtual mental health care (i.e., telemedicine) in schools has quickly become one solution for reaching students (Liu et al., 2020; Sullivan et al., 2020; Zhou X. et al., 2020). However, many challenges to remote counseling and mental health service delivery exist. These include concerns about maintaining student privacy and confidentiality, technological difficulties, an inability of providers to observe important nonverbal cues, and difficulties in recognizing and acting on emergency situations (Stoll et al., 2020). Additional challenges include student skepticism toward virtual counseling (Li and Leung, 2020), difficulty scheduling appointments via email or text messaging, and variability in student internet access or technological availability (Hasking et al., 2021). In the context of the COVID-19 pandemic, the need for SMHPs to rapidly transition to virtual mental health care delivery, while also transitioning their other school duties, likely magnified these challenges and further complicated efforts to provide students with sufficient mental health care. In turn, this likely exacerbated the already significant risk of vicarious trauma and burnout that school staff face even under typical circumstances (Joshi and Sharma, 2020).
As COVID-19 school closures have persisted and many districts have employed virtual platforms for sustained use, increased emphasis has been placed on better accommodating student needs. This includes better avenues for determining specific student mental health needs (Jones et al., 2021) and for best supporting SMHPs in providing effective student mental health services (Olson et al., 2021). However, these changes also require development of resources and professional development opportunities for SMHPs to minimize mental health impacts of the pandemic on student populations and also encourage best practices for remote school-based mental health care delivery.
TRAILS (Transforming Research into Action to Improve the Lives of Students) is a University of Michigan (U-M) school mental health implementation program designed to improve youth access to evidence-based mental health services by training and supporting SMHPs in cognitive behavioral therapy (CBT) and mindfulness practices. To date, TRAILS has trained over 7,000 school staff and mental health care providers and partnered with over 350 schools across Michigan and several other U.S. states. When COVID-19 halted in-person programming offered by TRAILS, the program recognized a need to pivot to supporting virtual mental health care delivery by SMHPs. To inform this effort, TRAILS administered a brief 16-item web-based survey to SMHPs who had engaged with the program, seeking information about both student and SMHP needs with respect to mental health care and support for program delivery. This research brief describes the needs identified by SMHPs in this survey.
Methods
In April 2020, shortly following Michigan’s statewide school closures, TRAILS distributed a survey to 263 SMHPs that had participated in their programming to help TRAILS understand their present needs and inform programmatic next steps. Specifically, the survey was sent to a convenience sample that included all SMHPs that had completed TRAILS training at any point between 2013 (program inception) and December 2019. Qualtrics, an online data collection platform, was used to distribute the survey. SMHPs were invited to voluntarily complete the anonymous survey via email and were offered a $20 incentive for participating. The survey was open for one month (April 1–May 1, 2020). This study was approved by the Michigan Medicine Institutional Review Board (IRBMED).
Measures
SMHPs were asked the school district in which they were employed, their professional role, and regular caseload in the survey. Other measures were intended to assess SMHP needs and mental health. When validated measures for constructs of interest were available, they were used (e.g., Patient Health Questionnaire 2-item [PHQ-2] and the Generalized Anxiety Disorder 2-item [GAD-2] to assess SMHP depression and anxiety symptoms). Due to the novel situational circumstances created by COVID-19 and the speed at which student mental health care delivery drastically changed, the study team did not validate new measures. However, the questions comprising the survey were based on past evaluative work done by TRAILS. While more validated measures related to COVID-19 are available now (Cortez et al., 2020; Evren et al., 2020; Lee, 2020; Taylor et al., 2020; Zurlo et al., 2020), in April 2020 when the survey was distributed, few validated measures were available (Ahorsu et al., 2020).
Needs Assessment
In order to better inform the TRAILS programming needs during the pandemic, SMHPs were asked to report on their capability of contacting students, the mental health needs of their students, SMHPs’ own mental health and wellness (as described below), and resources and supports needed to promote student mental health and wellness. In addition, questions about students internet access and resource distribution were included in order to determine challenges to virtual delivery of mental health services. While the measures for the needs assessment have not been validated, the questions comprising them were based on past work done by TRAILS and were informed by TRAILS leadership, who have extensive experience working with SMHPs to improve student mental health care delivery in the school setting.
SMHPs Depression and Anxiety Symptoms
Validated, brief screening tools were included to measure SMHP symptoms of depression and anxiety during the beginning of the pandemic and concomitant school closures (i.e., in the 2 weeks prior to survey response). The PHQ-2 (Kroenke et al., 2003) was used to screen for symptoms of depression and the GAD-2 (Kroenke et al., 2007; Plummer et al., 2016) was used to screen for symptoms of anxiety. These brief, lower-burden two-item measures have similar sensitivity and specificity to their respective 9-item and 7-item measures (Kroenke et al., 2003; Plummer et al., 2016), and have been validated in a number of diverse patient populations, including adolescents (Richardson et al., 2010), young adults aged 14–26 with a substance use disorder diagnosis (Bentley et al., 2021), patients with migraines aged 16–65 (Seo and Park, 2015), and a sample of elderly persons aged 58–82 (Wild et al., 2014). The psychometrically validated measures have each demonstrated adequate internal consistency reliability (Cronbach’s alpha PHQ-2 α = 0.73–0.83 [Löwe et al., 2005; Zhang et al., 2013; Dadfar et al., 2019]; GAD-2 α = 0.77–0.81 [Hughes et al., 2018; Staples et al., 2019]). Both the PHQ-2 and the GAD-2 have score ranges of 0–6, with a score of three or higher indicating a positive screen.
Analysis
To better understand the needs of SMHPs and their students at the beginning of the pandemic and subsequently inform TRAILS programming, SMHP responses to the needs assessment questions were explored using univariate descriptive analyses. Frequencies and percentages for SMHPs’ responses to the needs assessment questions were examined. Findings were then summarized with respect to student mental health needs, current state of student contact, SMHP training needs, and SMHP mental health support needs. We also computed scores for the SMHP mental health screening and examined the distribution of PHQ-2 and GAD-2 total scores, namely examining the proportion of SMHPs that screened positive for depression or anxiety. Findings most relevant to informing TRAILS programming in response to COVID-19 are presented.
Results
Of the 263 SMHPs who were sent the survey, 155 completed the survey (58.9%). Respondents represented 68 of 544 Michigan school districts (Figure 1). Respondents were predominantly student support staff, including school social workers, counselors, psychologists, and nurses (n = 119, 76.8%). The remainder were instructional staff (n = 29, 18.7%), other school staff (n = 6, 3.9%), or school administrators (n = 1, 0.6%).
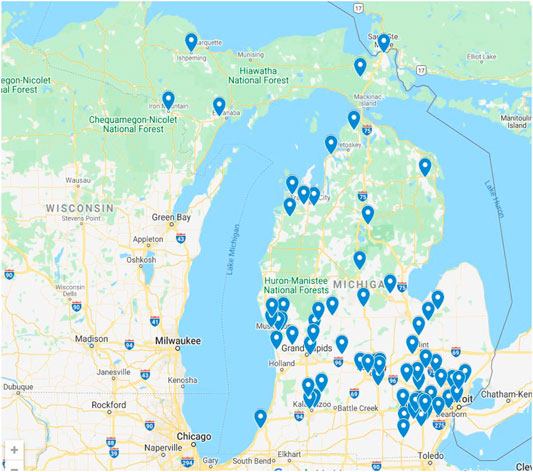
FIGURE 1. Michigan school districts employing survey respondents. Note: Survey question: “In what school district are you employed?”
Student Mental Health Needs
SMHPs were asked to rank the needs they felt were most pressing to their students. As shown in Figure 2, nearly half of SMHPs ranked general support for self-care and wellness as the most pressing student mental health need (n = 69, 44.5%). Support for coping with anxiety or depression was ranked as the second most common pressing need (n = 55, 35.5%), followed by support for coping with traumatic stress as the most common third most pressing need (n = 50, 32.3%), and support for coping with grief or loss as the fourth most common pressing need (n = 49, 31.6%). SMHPs believed that safety planning/crisis planning (due to neglect, risk of trauma exposure, or risk of suicide) were less pressing needs for students; only 5.8% (n = 9) ranked any of the safety planning needs as the most pressing need for their students.
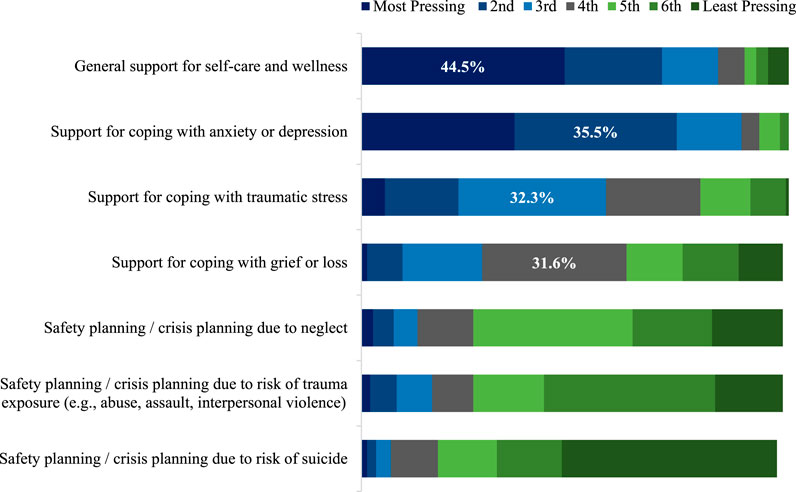
FIGURE 2. Students’ most pressing mental health needs as perceived by school mental health professionals. Note: Survey question: “What do you believe are the most pressing mental health needs of your students right now? [Drag and drop to rearrange the items below, placing them in order from: 1 = most pressing concern to 7 = least pressing concern]” N = 155; No responses = 10.
Student Contact
Nearly all SMHPs surveyed (n = 146, 94.2%) reported contacting one or more students in the month following COVID-19 school closures. Thirty-seven percent of SMHPs (n = 57) indicated they had been in contact with 1–10 students, while 19% (n = 30) had been in contact with more than 50 students.
SMHPs reported using various methods to contact their students. The most common form of communication reported was individual or small group email or text messages, with nearly three out of four SMHPs endorsing this method (n = 113, 72.9%). Two other popular methods were large-group/mass emails (n = 80, 51.6%) and posting information/resources on student-accessible websites (n = 76, 49.0%). Less frequently used forms of communication were individual or small group phone calls (n = 59, 38.1%) or individual or small group video chat (n = 44, 28.4%). A small number of SMHPs (n = 12, 7.7%) also mentioned that they had been in touch with students via other methods, including letters and forms sent to students by postal mail, interactions through platforms like Google Classroom and Instagram, and driving by students’ houses.
SMHP Training Needs
SMHPs were asked which types of training would be most helpful in navigating their new remote learning environment. Seventy percent (n = 109) indicated that professional training or consultation on best practices for remote delivery (i.e., phone, video, email) of mental health support services for youth would be most helpful. This was followed by endorsements of access to regular webinars on CBT and mindfulness techniques with students to support mental health during COVID-19 (n = 89, 57.4%) and training/consultation on best practices for delivering mental health support during public health emergencies (n = 80, 51.6%). About 20% of SMHPs indicated that access to group and individual consultations to think through difficult or high-risk student cases and plan service delivery options would also be helpful (n = 38 [24.5%] and n = 31 [20.0%], respectively).
SMHP Mental Health
Clinical measures indicated that 23.2% of SMHPs (n = 36) screened positive for anxiety disorders with a score of 3 or higher on the GAD-2; 7.7% (n = 12) scored 3 or higher on the PHQ-2, indicating likely major depressive disorder (Figure 3).
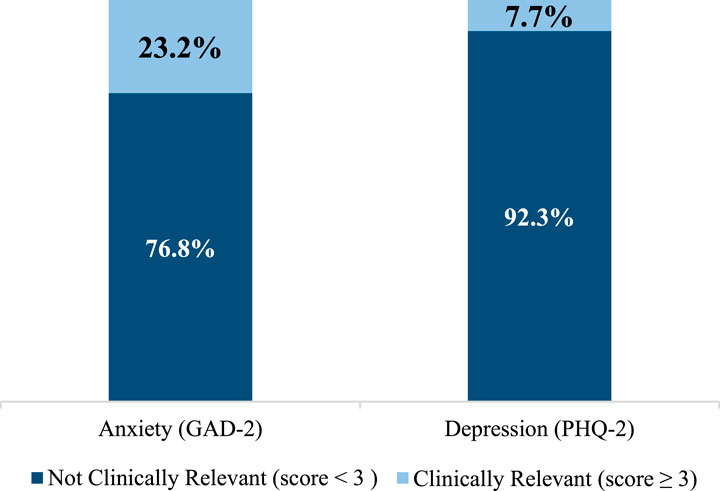
FIGURE 3. Anxiety and Depression in School Mental Health Professionals Based on GAD-2 and PHQ-2 Scores. Note: N = 155; No responses = 7. SMHPs screen for Generalized Anxiety Disorder if GAD-2 score is higher than or equal to 3 (Cronbach’s α = 0.80). SPs screen for Major Depressive Disorder if PHQ-2 score is higher than or equal to 3 (Cronbach’s α = 0.75).
Reflecting on their own needs for support to manage their personal mental health and wellness during the COVID-19 pandemic, more than half of SMHPs (n = 88, 56.8%) were interested in online self-care resources designed for mental health workers during a public health emergency. Other supports of interest included information about where to find urgent mental health support for education and healthcare workers (n = 33, 21.3%) and group or individual consultation/support to help prevent depression, burnout, and vicarious trauma (n = 36 [23.2%] and n = 35 [22.6%], respectively). Seventeen percent (n = 26) did not endorse any of the listed resources.
Discussion
The COVID-19 pandemic and resultant school closures changed the way that school professionals interacted with their students and required SMHPs to quickly reformat how they supported their students’ mental health, while also adding significant strain to their own mental health and wellness. The web-based survey described in this study, launched in April 2020 immediately following Michigan statewide school closures, examined the impact of the pandemic and school closures on mental health both for students and for SMHPs responsible for delivering mental health services in the school setting. Results helped the TRAILS implementation program determine the most pressing needs for supporting SMHP mental health care delivery in Michigan schools.
Overall, SMHPs indicated that their students’ main mental health needs in response to COVID-19 were related to self-care, anxiety, and depression. SMHPs shared that they would be interested in materials and training to help them navigate virtual delivery of care to their students regarding these concerns. Additionally, SMHPs reported experiencing their own distress (i.e., depression and anxiety) and expressed interest in resources for managing their own mental health and wellness.
While SMHPs are frequently overburdened in their roles under normal circumstances (Joshi and Sharma, 2020), COVID-19 added significant challenges to SMHP delivery of mental health care to their students. TRAILS saw a need to provide better support for SMHPs and the web-based survey reported on here was used to help identify how to prioritize resource development to improve provision of school mental health given challenges and changes. In response to the needs SMHPs expressed, TRAILS developed a rapid response plan that included the following: 1) development of self-care materials and training for SMHPs, 2) adaptation of clinical and implementation supports for virtual delivery of student mental health care, and 3) the development of a 7-session youth CBT and mindfulness skill group called Coping with COVID-19 (CC-19) (Rodriguez-Quintana et al., in press). To date, a total of four CC-19 trainings have been offered since May 2020, reaching a total of 1,332 people. Since the implementation of these changes in the TRAILS program, the TRAILS website saw an increase in webpage views, from 160,778 between November 2019 and March 2020, to 565,621 between March 2020 and October 2020. Additionally, between April 20, 2020 and April 20, 2021, more than 73,000 people from over 120 different countries visited TRAILStoWellness.org, resulting in over one million page views in this time period.
Limitations
Given that this survey was developed as a first-line rapid assessment tool, the survey and our findings have several important limitations. First, SMHPs surveyed were from a select number of districts in Michigan and from a pool of SMHPs that were actively engaged with implementing mental health care in their schools via the TRAILS program. As such, they likely do not fully capture the experiences of all SMHPs in the state or nationwide. However, they do reflect perspectives of a number of SMHPs across Michigan that were actively invested in delivering mental health services to students prior to the pandemic. Second, the survey was conducted in the early weeks of the COVID-19 pandemic during a time of active transition for Michigan schools and the study did not address student and SMHP needs beyond the early months of COVID-19 school closures. The long-term needs of coping with COVID-19 for both students and SMHPs may have been different than those initially reported. To better understand and support the short- and long-term needs of SMHPs, especially if virtual learning options continue beyond COVID-19, further steps are needed, including conducting a more comprehensive needs assessment to inform implementation supports and reduce the burden on SMHPs. Fourth, as the study team tried to quickly gauge and respond to the pressing needs facing student and SMHP mental health in direct response to COVID-19, the survey questions were designed to explore the unprecedented situation. The novelty of the situation meant that validated instruments for assessing many key constructs of interest were not available; the urgency of the assessment meant that TRAILS opted to field the survey without extensive validation or pre-testing efforts. These limitations notwithstanding, however, this survey offered a unique glimpse into the early experiences of SMHPs responsible for delivering mental health support to students early in the COVID-19 pandemic.
Conclusion
The COVID-19 pandemic and associated school closures caused significant disruption to SMHPs’ typical interaction with students, requiring changes to how they delivered mental health support under uncertain and quickly changing circumstances. This survey, fielded in the 6 weeks immediately following initial COVID-19 school closures in Michigan, helped researchers and staff within this implementation program understand SMHP needs and inform program support for students and SMHPs. The survey informed TRAILS’ development of COVID-19-related materials/trainings and resulted in increased training participation and significantly increased web traffic. As COVID-19 school closures persist, or as hybrid models of school instruction are tested, new trainings and resources should be developed based on the needs of the communities for which they are meant to serve.
Data Availability Statement
The raw data supporting the conclusion of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by the University of Michigan Institutional Review Board. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author Contributions
EK and SS conceptualized the overarching research goals and aims. MS and EK developed the survey that informed this research and designed the methodology. AR, SC and AL wrote the preliminary manuscript. AR, NRQ, SC and MS performed the analyses and contributed to the results. AR created the data visualization for the figures. AR and NRQ carried out major revisions of the manuscript. AR, NRQ, SC, AL, MS, EK and SS edited and revised the manuscript. All authors approved of the final manuscript.
Funding
This work is supported by the National Institute of Mental Health (R01MH114203) and by the Centers for Medicare and Medicaid Services through the Michigan Department of Health and Human Services.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
Ahorsu, D. K., Lin, C.-Y., Imani, V., Saffari, M., Griffiths, M. D., and Pakpour, A. H. (2020). The Fear of COVID-19 Scale: Development and Initial Validation. Int. J. Ment. Health Addict. 1-9. doi:10.1007/s11469-020-00270-8
Asarnow, J. R., Jaycox, L. H., Duan, N., LaBorde, A. P., Rea, M. M., Tang, L., et al. (2005). Depression and Role Impairment Among Adolescents in Primary Care Clinics. J. Adolesc. Health 37 (6), 477–483. doi:10.1016/j.jadohealth.2004.11.123
Bentley, K. H., Sakurai, H., Lowman, K. L., Rines-Toth, L., McKowen, J., Pedrelli, P., et al. (2021). Validation of Brief Screening Measures for Depression and Anxiety in Young People with Substance Use Disorders. J. Affective Disord. 282, 1021–1029. doi:10.1016/j.jad.2021.01.005
Brener, N. D., Martindale, J., and Weist, M. D. (2001). Mental Health and Social Services: Results from the School Health Policies and Programs Study 2000. J. Sch. Health 71 (7), 305–312. doi:10.1111/j.1746-1561.2001.tb03507.x
Burns, B. J., Costello, E. J., Angold, A., Tweed, D., Stangl, D., Farmer, E. M. Z., et al. (1995). Children’s Mental Health Service Use across Service Sectors. Health Aff. 14 (3), 147–159. doi:10.1377/hlthaff.14.3.147
CDC (2020). COVID-19 and Your Health. Centers for Disease Control and Prevention. Available at: https://www.cdc.gov/coronavirus/2019-ncov/if-you-are-sick/quarantine.html.
Cortez, P. A., Joseph, S. J., Das, N., Bhandari, S. S., and Shoib, S. (2020). Tools to Measure the Psychological Impact of the COVID-19 Pandemic: What Do We Have in the Platter? Asian J. Psychiatry 53, 102371. doi:10.1016/j.ajp.2020.102371
Costello, E. J., He, J.-p., Sampson, N. A., Kessler, R. C., and Merikangas, K. R. (2014). Services for Adolescents with Psychiatric Disorders: 12-Month Data from the National Comorbidity Survey-Adolescent. Ps 65 (3), 359–366. doi:10.1176/appi.ps.201100518
Dadfar, M., Salabifard, S., Dadfar, T., Roudbari, M., and Moneni Safarabad, N. (2019). Validation of the Patient Health Questionnaire-2 with Iranian Students. Ment. Health Religion Cult. 22 (10), 1048–1056. doi:10.1080/13674676.2019.1699042
Duong, M. T., Bruns, E. J., Lee, K., Cox, S., Coifman, J., Mayworm, A., et al. (2020). Rates of Mental Health Service Utilization by Children and Adolescents in Schools and Other Common Service Settings: A Systematic Review and Meta-Analysis. Adm. Pol. Ment Health 48, 420–439. doi:10.1007/s10488-020-01080-9
Evren, C., Evren, B., Dalbudak, E., Topcu, M., and Kutlu, N. (2020). Measuring Anxiety Related to COVID-19: A Turkish Validation Study of the Coronavirus Anxiety Scale. Death Stud. 0 (0), 1–7. doi:10.1080/07481187.2020.1774969
Fazel, M., Hoagwood, K., Stephan, S., and Ford, T. (2014). Mental Health Interventions in Schools in High-Income Countries. The Lancet Psychiatry 1 (5), 377–387. doi:10.1016/S2215-0366(14)70312-8
Flaherty, L. T., and Osher, D. (2003). “History of School-Based Mental Health Services in the United States,” in Handbook of School Mental Health Advancing Practice and Research. Editors M. D. Weist, S. W. Evans, and N. A. Lever (US: Springer), 11–22. doi:10.1007/978-0-387-73313-5_2
Flaherty, L. T., Weist, M. D., and Warner, B. S. (1996). School-based mental health services in the United States: history, current models and needs. Commun. Ment. Health J. 32 (4), 341–52. doi:10.1007/BF02249452
Hasking, P., Lewis, S. P., Bloom, E., Brausch, A., Kaess, M., and Robinson, K. (2021). Impact of the COVID-19 Pandemic on Students at Elevated Risk of Self-Injury: The Importance of Virtual and Online Resources. Sch. Psychol. Int. 42 (1), 57–78. doi:10.1177/0143034320974414
Hughes, A. J., Dunn, K. M., Chaffee, T., Bhattarai, J., and Beier, M. (2018). Diagnostic and Clinical Utility of the GAD-2 for Screening Anxiety Symptoms in Individuals with Multiple Sclerosis. Arch. Phys. Med. Rehabil. 99 (10), 2045–2049. doi:10.1016/j.apmr.2018.05.029
Jones, E. A. K., Mitra, A. K., and Bhuiyan, A. R. (2021). Impact of COVID-19 on Mental Health in Adolescents: A Systematic Review. Ijerph 18 (5), 2470. doi:10.3390/ijerph18052470
Joshi, G., and Sharma, G. (2020). Burnout: A Risk Factor Amongst Mental Health Professionals during COVID-19. Asian J. Psychiatry 54, 102300. doi:10.1016/j.ajp.2020.102300
Kroenke, K., Spitzer, R. L., Williams, J. B. W., Monahan, P. O., and Löwe, B. (2007). Anxiety Disorders in Primary Care: Prevalence, Impairment, Comorbidity, and Detection. Ann. Intern. Med. 146 (5), 317. doi:10.7326/0003-4819-146-5-200703060-00004
Kroenke, K., Spitzer, R. L., and Williams, J. B. W. (2003). The Patient Health Questionnaire-2: Validity of a Two-Item Depression. Screener 41 (11), 10. doi:10.1097/01.mlr.0000093487.78664.3c
Lee, S. A. (2020). Coronavirus Anxiety Scale: A Brief Mental Health Screener for COVID-19 Related Anxiety. Death Stud. 44 (7), 393–401. doi:10.1080/07481187.2020.1748481
Lee, S. J., and Ward, K. P. (2020). Mental Health, Relationships, and Coping during the Coronavirus Pandemic. Available at: https://www.parentingincontext.org/uploads/8/1/3/1/81318622/research_brief_mental_health_relationships_and_coping_during_the_coronavirus_pandemic_final.pdf.
Li, T. M. H., and Leung, C. S. Y. (2020). Exploring Student Mental Health and Intention to Use Online Counseling in Hong Kong during the COVID-19 Pandemic. Psychiatry Clin. Neurosci. 74 (10), 564–565. doi:10.1111/pcn.13117
Liu, S., Yang, L., Zhang, C., Xiang, Y.-T., Liu, Z., Hu, S., et al. (2020). Online Mental Health Services in China during the COVID-19 Outbreak. The Lancet Psychiatry 7 (4), e17–e18. doi:10.1016/S2215-0366(20)30077-8
Löwe, B., Kroenke, K., and Gräfe, K. (2005). Detecting and Monitoring Depression with a Two-Item Questionnaire (PHQ-2). J. Psychosomatic Res. 58 (2), 163–171. doi:10.1016/j.jpsychores.2004.09.006
Muller, A. E., Hafstad, E. V., Himmels, J. P. W., Smedslund, G., Flottorp, S., Stensland, S. Ø., et al. (2020). The Mental Health Impact of the Covid-19 Pandemic on Healthcare Workers, and Interventions to Help Them: A Rapid Systematic Review. Psychiatry Res. 293, 113441. doi:10.1016/j.psychres.2020.113441
Murata, S., Rezeppa, T., Thoma, B., Marengo, L., Krancevich, K., Chiyka, E., et al. (2021). The Psychiatric Sequelae of the COVID‐19 Pandemic in Adolescents, Adults, and Health Care Workers. Depress. Anxiety 38 (2), 233–246. doi:10.1002/da.23120
Olson, J. R., Lucy, M., Kellogg, M. A., Schmitz, K., Berntson, T., Stuber, J., et al. (2021). What Happens when Training Goes Virtual? Adapting Training and Technical Assistance for the School Mental Health Workforce in Response to COVID-19. Sch. Ment. Health 13 (1), 160–173. doi:10.1007/s12310-020-09401-x
Plummer, F., Manea, L., Trepel, D., and McMillan, D. (2016). Screening for Anxiety Disorders with the GAD-7 and GAD-2: A Systematic Review and Diagnostic Metaanalysis. Gen. Hosp. Psychiatry 39, 24–31. doi:10.1016/j.genhosppsych.2015.11.005
Richardson, L. P., Rockhill, C., Russo, J. E., Grossman, D. C., Richards, J., McCarty, C., et al. (2010). Evaluation of the PHQ-2 as a Brief Screen for Detecting Major Depression Among Adolescents. Pediatrics 125 (5), e1097–e1103. doi:10.1542/peds.2009-2712
Rodriguez-Quintana, N., Meyer, A. E., Bilek, E., Flumenbaum, R., Miner, K., Scoville, L., et al. (in press). Development of a Brief Group CBT Intervention to Reduce COVID-19 Related Distress Among School-Age Youth. Cogn. Behav. Pract., S1077722921000468. doi:10.1016/j.cbpra.2021.03.002
Schlitt, J., Santelli, J., Juszczak, L., Brindis, C., Nystrom, R., Klein, J., et al. (2000). Creating Access to Care: School-Based Health center Census 1998-99. Washington, DC: National Assembly on School-Based Heath Care.
Seo, J.-G., and Park, S.-P. (2015). Validation of the Generalized Anxiety Disorder-7 (GAD-7) and GAD-2 in Patients with Migraine. J. Headache Pain 16 (1), 97. doi:10.1186/s10194-015-0583-8
Staples, L. G., Dear, B. F., Gandy, M., Fogliati, V., Fogliati, R., Karin, E., et al. (2019). Psychometric Properties and Clinical Utility of Brief Measures of Depression, Anxiety, and General Distress: The PHQ-2, GAD-2, and K-6. Gen. Hosp. Psychiatry 56, 13–18. doi:10.1016/j.genhosppsych.2018.11.003
Stoll, J., Müller, J. A., and Trachsel, M. (2020). Ethical Issues in Online Psychotherapy: A Narrative Review. Front. Psychiatry 10, 993. doi:10.3389/fpsyt.2019.00993
Sullivan, A. B., Kane, A., Roth, A. J., Davis, B. E., Drerup, M. L., and Heinberg, L. J. (2020). The COVID-19 Crisis: A Mental Health Perspective and Response Using Telemedicine. J. Patient Experience 7 (3), 295–301. doi:10.1177/2374373520922747
Taylor, S., Landry, C. A., Paluszek, M. M., Fergus, T. A., McKay, D., and Asmundson, G. J. G. (2020). Development and Initial Validation of the COVID Stress Scales. J. Anxiety Disord. 72, 102232. doi:10.1016/j.janxdis.2020.102232
Weir, K. (2020). Safeguarding Student Mental Health. Available at: https://www.apa.org. https://www.apa.org/monitor/2020/09/safeguarding-mental-health.
Weist, M. D., Rubin, M., Moore, E., Adelsheim, S., and Wrobel, G. (2007). Mental Health Screening in Schools. J. Sch. Health 77 (2), 53–58. doi:10.1111/j.1746-1561.2007.00167.x
Whiston, S. C., and Quinby, R. F. (2009). Review of School Counseling Outcome Research. Psychol. Schs. 46 (3), 267–272. doi:10.1002/pits.20372
Whitmer—Executive Order (2020-35). Provision of K-12 Education during the Remainder of the 2019-2020 School Year—RESCINDED. (2020). Available at: https://www.michigan.gov/whitmer/0,9309,7-387-90499_90705-524032--,00.html.
Whitmer—Executive Order (2020-05). Temporary Prohibition on Large Assemblages and Events, Temporary School Closures—RESCINDED. (2020). Available at: https://www.michigan.gov/whitmer/0,9309,7-387-90499_90705-521595--,00.html.
Wild, B., Eckl, A., Herzog, W., Niehoff, D., Lechner, S., Maatouk, I., et al. (2014). Assessing Generalized Anxiety Disorder in Elderly People Using the GAD-7 and GAD-2 Scales: Results of a Validation Study. Am. J. Geriatr. Psychiatry 22, 1029–1038. doi:10.1016/j.jagp.2013.01.076
Zhang, Y.-L., Liang, W., Chen, Z.-M., Zhang, H.-M., Zhang, J.-H., Weng, X.-Q., et al. (2013). Validity and Reliability of Patient Health Questionnaire-9 and Patient Health Questionnaire-2 to Screen for Depression Among College Students in China. Asia-Pacific Psychiatry 5 (4), 268–275. doi:10.1111/appy.12103
Zhou, S.-J., Zhang, L.-G., Wang, L.-L., Guo, Z.-C., Wang, J.-Q., Chen, J.-C., et al. (2020). Prevalence and Socio-Demographic Correlates of Psychological Health Problems in Chinese Adolescents during the Outbreak of COVID-19. Eur. Child. Adolesc. Psychiatry 29 (6), 749–758. doi:10.1007/s00787-020-01541-4
Zhou, X., Snoswell, C. L., Harding, L. E., Bambling, M., Edirippulige, S., Bai, X., et al. (2020). The Role of Telehealth in Reducing the Mental Health Burden from COVID-19. Telemed. E-Health 26 (4), 377–379. doi:10.1089/tmj.2020.0068
Keywords: COVID-19, public health, adolescent health, public health practice, mental health, school health
Citation: Rusch A, Rodriguez-Quintana N, Choi SY, Lane A, Smith M, Koschmann E and Smith SN (2021) School Professional Needs to Support Student Mental Health During the COVID-19 Pandemic. Front. Educ. 6:663871. doi: 10.3389/feduc.2021.663871
Received: 03 February 2021; Accepted: 11 May 2021;
Published: 18 June 2021.
Edited by:
Maria Anna Coniglio, University of Catania, ItalyReviewed by:
Mohamed A. Ali, Grand Canyon University, United StatesZia Ul Mustafa, Independent Researcher, Sahiwal, Pakistan
Copyright © 2021 Rusch, Rodriguez-Quintana, Choi, Lane, Smith, Koschmann and Smith. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Amy Rusch, YW15cnVzY2hAdW1pY2guZWR1
 Amy Rusch
Amy Rusch Natalie Rodriguez-Quintana
Natalie Rodriguez-Quintana Seo Youn Choi1
Seo Youn Choi1 Annalise Lane
Annalise Lane Maureen Smith
Maureen Smith Elizabeth Koschmann
Elizabeth Koschmann