- 1Department of Internal Medicine, Muhimbili University of Health and Allied Sciences, Dar es Salaam, Tanzania
- 2East African Centre of Excellence in Cardiovascular Sciences, Muhimbili University of Health and Allied Sciences, Dar es Salaam, Tanzania
- 3Department of Physiology, Muhimbili University of Health and Allied Sciences, Dar es Salaam, Tanzania
- 4Department of Epidemiology and Biostatistics, Muhimbili University of Health and Allied Sciences, Dar es Salaam, Tanzania
- 5Department of Clinical Pharmacy and Pharmacology, Muhimbili University of Health and Allied Sciences, Dar es Salaam, Tanzania
Introduction: Cardiovascular disease (CVD) contribute the largest mortality burden globally, with most of the deaths (80% of all deaths) occurring in low and middle-income countries (LMICs), including Tanzania. Despite the increasing burden, to date, CVD research output is still limited in Tanzania, as it is for many sub-Saharan Africa (SSA) countries. This trend hinders the establishment of locally informed CVD management and policy changes. Here, we aim to review the existing gaps while highlighting the available opportunities for a sustainable CVD research strategy in Tanzania.
Methods: A rapid review of available literature on CVD research in SSA was conducted, with emphasis on the contribution of Tanzania in the world literature of CVD. Through available literature, we identify strategic CVD research priorities in Tanzania and highlight challenges and opportunities for sustainable CVD research output.
Findings: Shortage of skilled researchers, inadequate research infrastructure, limited funding, and lack of organized research strategies at different levels (regional, country, and institutional) are among the existing key bottlenecks contributing to the low output of CVD research in Tanzania. There is generally strong global, regional and local political will to address the CVD epidemic. The establishment of the East African Centre of Excellence in Cardiovascular Sciences (EACoECVS) offers a unique opportunity for setting strategies and coordinating CVD research and training for Tanzania and the East African region.
Conclusion: There is a light of hope for long-term sustainable CVD research output from Tanzania, taking advantage of the ongoing activities and plans for the evolving EACoECVS. The Tanzanian experience can be taken as a lesson for other SSA countries.
Introduction
Cardiovascular disease (CVD) account for most non-communicable diseases (NCDs) deaths globally, an estimated 17 million people each year with 80% of these deaths occurring in low and middle-income countries (LMICs) (1). In sub-Saharan Africa (SSA) countries including Tanzania, cardiac diseases, chronic kidney disease, and stroke have been increasing rapidly (2) and now are important causes of morbidity, mortality and disability-adjusted life years (DALYs) lost among adults (1, 3). These three major CVD are driven by common risk factors –mainly hypertension, which occurs in one out of every four adults in Tanzania (4). Other important risk factors include diabetes mellitus, obesity, sedentary lifestyle, and cigarette smoking, all a result of an epidemiological transition that is currently taking place in the country (4, 5). Furthermore, in SSA there are still some CVD related to malnutrition, poverty and infections such as rheumatic heart disease, cardiomyopathies, untreated congenital heart diseases, as well as human immunodeficiency virus (HIV) and tuberculosis-related CVD (6). This results in a double burden of “old” and “new” lifestyle-related CVD. Africa has additional risks for CVD caused by inherently genetic diseases that are commonly found in this part of the world, like sickle cell anemia which causes systemic complications, including heart failure, kidney failure, pulmonary complications, and stroke (7).
When compared to Caucasians, CVD occur early among people of African origin, and with fast progression to end stage organ damage (6, 8). This causes major economic development challenges as well as direct or indirect hindrance to achieving sustainable millennium development goals one (no poverty), two (zero hunger), three (good health and well-being), four (quality education), eight (descent work and economic growth), and ten (reduced inequalities) (9). This is due to the economic drain brought about by loss of a productive work force, but also through high costs of treating the chronic conditions at individual, communities and national level.
Although not yet fully implemented, there is already some level of commitment to combat the increasing challenge of CVD both regionally and in Tanzania. NCDs including CVD have been recognized as one of the biggest threats to economic development that Africa is striving to achieve. At the continent level, African Ministers of Health have pledged their commitment to work together in fighting the diseases (10). In Tanzania, an NCDs special unit has been created at the Ministry of Health (11). This unit is dedicated to creating awareness and to oversee efforts to prevent NCDs and their associated risk factors. At the level of the East African Community, several initiatives including establishment of East African Centres of Excellences for NCDs including CVD, cancer and renal diseases are being implemented in different countries within the community (12). In this initiative, Tanzania has been given a task to develop an East African Centre of Excellence in Cardiovascular Sciences (EACoECVS). Fighting against CVD needs collective efforts. The Tanzanian Ministry of Health needs evidence-based research to inform the magnitude of the problem as well as findings from local communities in order to effectively implement preventive and control measures against CVD. However, until now there is limited research output from Tanzania addressing CVD, evidenced by the small contribution of scientific research articles emanating from Tanzania in the world literature (Figure 1). Additionally, even with the available research, there is lack of streamlined and focused research that addresses a common goal. Being the foremost health university in Tanzania and the host of the evolving EACoECVS, Muhimbili University of Health and Allied Sciences (MUHAS) is positioned to play a central role in conducting CVD research as well as train a critical mass of researchers to conduct CVD research. This will help to address two important gaps in CVD research in Tanzania, namely limited research output and shortage of researchers in CVD.
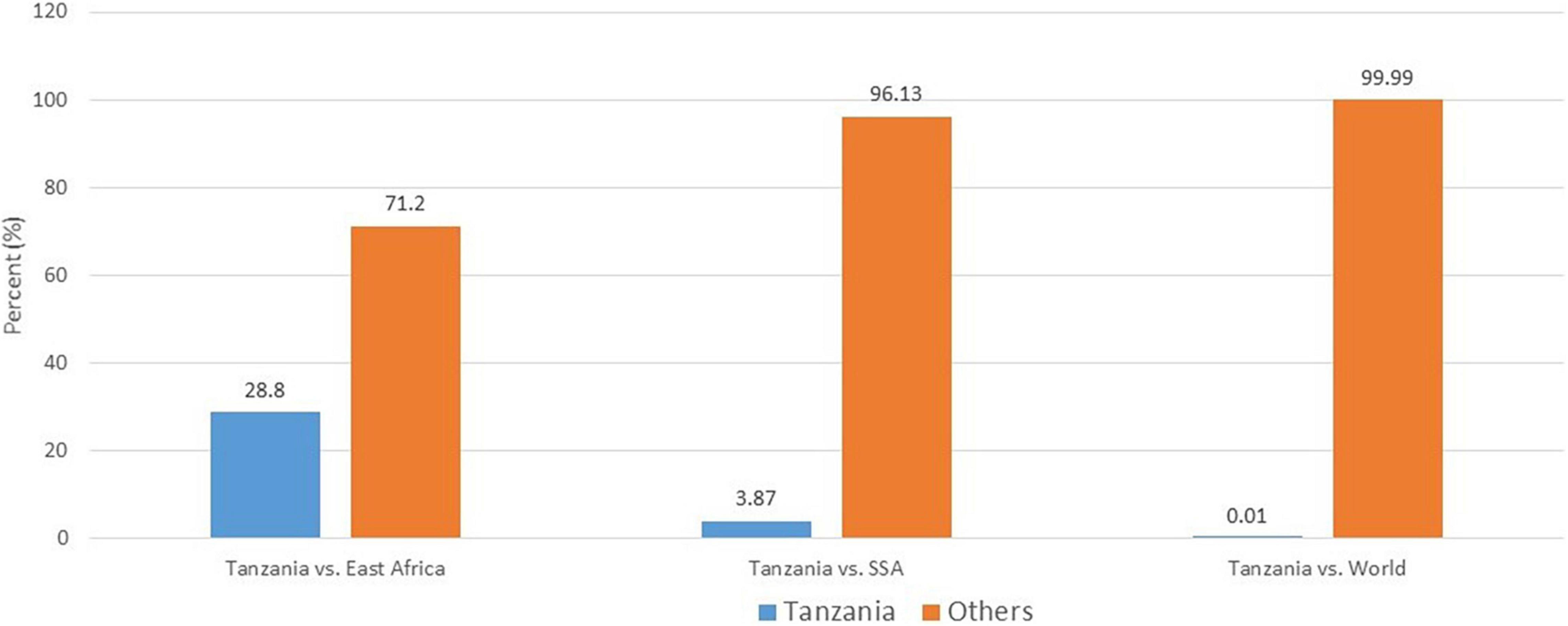
Figure 1. Cardiovascular disease research output from Tanzania compared to East Africa, sub-Saharan Africa, and World (PubMed search 2000–2021). Number of articles extracted: Tanzania, 196; East Africa, 681; sub-Saharan Africa, 142,395; World, 1,355,322.
In this review, we put forward the centre’s CVD research agenda and we describe how to utilize the existing opportunities for sustainable research output, while addressing the challenges in terms of academia, research training, research infrastructure and funding faced by many SSA countries, taking Tanzania as an example.
Methods
A rapid review of literature was conducted on the topic of CVD research in SSA. Search databases used were PubMed, African Journals Online and Google Scholar. Firstly, the PubMed database was used to assess the contribution of Tanzania in CVD research output in comparison to East Africa, SSA and globally. The PubMed search terms used were “cardiovascular diseases [MeSH Terms],” “Africa, sub Saharan [MeSH Terms],” “((((Kenya [MeSH Terms]) OR (Rwanda [MeSH Terms])) OR (Burundi [MeSH Terms])) OR (Uganda [MeSH Terms])) OR (Tanzania [MeSH Terms]),” and “united republic of Tanzania [MeSH Terms].” Filters were added to confine the PubMed search from 2000 to 2021 (Supplementary File 1). Search terms in African Journals Online and Google Scholar were: “cardiovascular diseases,” “cardiovascular research” “sub Saharan Africa,” “Tanzania,” “research training,” and “research strategy.” The literature obtained from PubMed and other databases searched were then critically examined to summarize information on CVD research priorities in Tanzania, as well as challenges and opportunities for CVD research in SSA, including Tanzania. All literature including original papers, perspectives, topic reviews, and conferences proceedings that focused on SSA CVD research were examined.
As part of the activities of the evolving EACoECVS, information on research priorities, action points for implementation, available opportunities as well as current challenges and their possible mitigations was obtained from several internal and external meetings/workshops with stakeholders of CVD in Tanzania and East Africa, including meetings of the East African Community Sectoral Council of Ministers of Health.
Defining the Research Agenda for the East African Centre of Excellence in Cardiovascular Sciences
Goal and Objectives
The overall goal of the centre’s research agenda is to contribute toward prevention and control of CVD in Tanzania and the East African region and eventually decrease morbidity and mortality resulting from these diseases. The immediate main objective is to train a critical mass of researchers to lead research in key strategic areas in order to identify and propose solutions to reduce the CVD burden in Tanzania and the East African region.
Research Priorities
Cardiovascular disease cover a broad range of conditions affecting the heart and blood vessels. In Tanzania, hospital data show that highly prevalent CVD include hypertensive heart disease leading to heart failure, hypertensive kidney disease leading to end stage renal failure as well as cerebrovascular diseases presenting as stroke (13–15). Other important CVD include rheumatic heart disease, cardiomyopathies – particularly dilated cardiomyopathy, untreated congenital heart diseases, endomyocardial fibrosis, and cardiovascular complications of sickle cell anemia, tuberculosis and HIV disease (7, 16–18). Although not yet ranking highest in Tanzania, ischemic heart disease is on the increase (19). With time, ischemic heart disease is likely to consume a significant amount of the already inadequate budget on health (20).
Here we define specific CVD research areas that despite existing efforts are still facing significant unmet needs. Epidemiological and scientific knowledge coupled with translation into policy and clinical implementation will have major impact on the society and individual well-being of many Tanzanians. The research priority areas are explained below:
Research Priority 1: Determine Cardiovascular Disease Burden Data
One of the major problems with research in SSA has been lack of even basic data on disease burden (21, 22). This reality has led to most of estimated global burden of disease (GBD) data to utilize structural modeled estimates as a result of extremely limited information from some regions of the world, including SSA (22, 23). In Tanzania, the prevalence of most risk factors for CVD are known; namely hypertension (25.9%), diabetes (9.1%), elevated cholesterol (26%) as well as lifestyle conditions like overweight and obesity (26%) and cigarette smoking (15.9%) (4). However, there is still limited data on the community disease burden of specific CVD like heart failure, stroke, renal diseases, rheumatic heart disease, atrial fibrillation, cardiomyopathies, and others. Furthermore, disease trends including incidence, survival, and long-term outcome of CVD are unknown. Community burden of disease is important in order to plan for prioritization as well as targeted community interventions. Implementing this agenda will also facilitate reliable data to be used in the GBD studies related to CVD, which is important to place the country’s CVD burden into the global perspective. The plan is to prioritize community surveys of specific CVD in order to fill in the missing numbers of disease burden.
Action Points
• List and prioritize unmet needs for community CVD burden, especially those included in the GBD study
• Liaise with different stakeholders, including global funding agencies for collaboration and funding of research
• Create new, and organize existing population-based community cohorts on CVD to capture disease incidence and trends
• Conduct community surveys on CVD, prevalence, incidence and outcomes.
Research Priority 2: Conduct Cardiovascular Disease Prevention and Public Health Promotion Research
For most CVD, many important biological risk factors such as age, blood pressure, cholesterol levels and the significant influence of lifestyle and other environmental factors are well known, due to the seminal work from large follow-up cohort studies such as the Framingham Heart Study (24). However, efforts to reduce CVD risk by improving lifestyle are not working well enough in many countries (25) including Tanzania (4). Furthermore, even the knowledge of common risk factors is not universally understood among people in our communities (26, 27). There is therefore a knowledge gap in Tanzania in this area. This calls for rigorous multi-disciplinary CVD prevention research, involving social scientists, policy makers, and importantly involvement of the general Tanzanian population from the outset. As a starting point, there is a need for up-to-date and detailed data on population knowledge, current practice and health seeking behaviors toward CVD, as well as understanding of the best strategies (i.e., what works and what does not) to be used for an effective behavioral change toward CVD.
Action Points
• Define areas of community awareness needs
• Involve multi-stakeholders’ team on prevention research
• Conduct Knowledge, Attitude and Practice (KAP) studies on CVD
• Conduct implementation research on best strategies to attain behavior change toward CVD prevention.
Research Priority 3: Research on Early Detection and Management of Cardiovascular Disease
Most lifestyle-related CVD take long before they manifest with symptoms, making it possible for effective early interventions (28). However, early detection of CVD has been a challenge in most SSA countries (6). In Tanzania, most patients with CVD present late, often with acute events (29) or end organ damage when they first show up at healthcare facilities (30, 31). Tanzania, and other SSA countries can learn from developed countries, where improvement on early detection of CVD and their risk factors have made possible for many people to be on treatment or on the watch-list to prevent future cardiovascular events (32). This has been found to be more cost-effective in dealing with CVD as opposed to treating acute events and their complications (33, 34). A significant area of unmet need in the Tanzanian context is therefore to detect signs of CVD risk earlier enough, and to adapt the health system to be able to manage the populations at risk more effectively.
Research in this agenda will focus on investigating the applicability and cost-effectiveness of active early detection of CVD and their risk factors as well as studies on unique approaches to treatment of early disease including use of primary health facilities to treat CVD risk factors like hypertension, diabetes, and obesity. Also important in Tanzania, is early detection of acute rheumatic fever and rheumatic heart disease, as well as recognition of cardiac manifestations of tuberculosis, HIV and sickle cell anemia, among others.
Action Points
• Define list of important signs of early CVD
• Liaise with policy makers on referral of patients with early CVD
• Involve multi-disciplinary team of researchers to conduct research on early CVD
• Conduct implementation and cost-effectiveness research on early detection of CVD.
Research Priority 4: Establishing Disease Specific Registries for Cardiovascular Disease
Disease registries are a collection of patients’ secondary data, usually for a specific disease. The importance of disease registries cannot be overstated. In the GBD outcome data on CVD, SSA did not perform well and mortality projections using structural models were used instead of real mortality data due to limited or unreliable mortality data from the region (1). In developed countries, disease registries have brought in a wealth of information of specific disease trajectory, risk factors for complications including areas for individualized treatment (35). Furthermore, many research questions can be answered through accumulated data, answering questions on the course of disease, understanding variations in treatment and outcomes, examining factors that influence prognosis, as well as assessing the quality of life and care patterns among patients (36). Through functionalities such as feedback of data, registries are also increasingly been used to study quality improvement (37).
In SSA, disease registries have recently been developed and are increasing in number. They include single-country (38, 39) as well as an increasing number of regional registries (40, 41). However, funding to maintain and produce the required reliable data may be an issue, especially if it is not constant, as previously reported (42). In Tanzania, there are currently no formal systematic specific disease registries for CVD, although small short registries have been conducted mainly as single-center research (13). This research agenda will align existing CVD registries (in-country, regional), but more important will seek to create sustainable systems and infrastructure to create CVD registries of importance in Tanzania.
Action Points
• Define priority diseases for registry
• Obtain legal framework for continuous data collection and use
• Obtain patient groups involvement in registry keeping
• Obtain government support to initiate and maintain disease registries
• Strengthen Information Technology (IT) infrastructure for continuous data capturing and storage.
Research Priority 5: Harnessing the Power of Big Data in Hospital Day to Day Records
Currently, the amount of electronic data generated in healthcare worldwide is immense. Already, in developed countries the concepts of Big Data and a learning health care system have been a fast-growing area of medicine (43). Big Data refers to large and diverse sets of patients’ clinical information that is dynamic, and encompasses volumes of information, velocity or speed at which they are generated and collected, as well as the variety or scope of the data collected (43). In developed countries, Big Data is already used to produce useful information including translational and precision medicine research (44). Due to its diverse nature, Big Data analyses could inform government policy and therefore bringing about efficient patient care.
In many SSA countries, the introduction of computer-based patient records is new, but has taken effect and more countries have started to use patient electronic health management information systems (HIMS) (45, 46). This creates a unique opportunity for continuous data capturing, which can be translated into research. In Tanzania, Information Communication and Technology (ICT) plays a major role in healthcare management services, and since 2003 the government of Tanzania introduced the use of HIMS in all tertiary healthcare facilities and plans are underway to make most facilities in Tanzania use HIMS (47, 48). Currently, the amount of data generated in healthcare in Tanzania is therefore already immense, but the data is still fragmented, unstructured, and difficult to access for analytic purposes (49). This results in a data-to-innovation gap in health research. This agenda plans to research on best strategies that will result in adaptation of the FAIR (Findable, Accessible, Interoperable, and Re-usable) CVD data collection principles in tertiary university teaching health facilities in Tanzania, which can in the future be rolled-out to other health facilities in the country.
Action Points
• Improve data entry by health personnel through education and implementation research
• Obtain legal framework for continuous data collection and use
• Obtain patient groups involvement in continuous data collection
• Obtain government support to strengthen IT infrastructure
• Conduct implementation research to demonstrate the feasibility and evaluating impact of Big Data collection including cost effectiveness studies.
Research Priority 6: Research on Genetics of Cardiovascular Disease
Knowledge regarding genetic contribution on disease has gained significant attention in the past decades, and is an area of active research (50). In CVD medicine, major advances including the complex interplay between genetics and environmental factors in CVD causation have been appreciated. Large scale genome wide studies (GWAS) have been successful in uncovering novel susceptibility loci for a wide range of complex human diseases including hypertension, diabetes, cardiomyopathies, coronary artery disease, congenital heart disease, dyslipidaemia, arrhythmias, and others (51, 52). These advances are paving way for future management, including the possibility of precision medicine and new treatment options. Much of research in genetics of CVD has however been done in High Income Countries (HICs) of North America and Europe (51, 52), although other emerging economies like China are increasing the output of genetic research in CVD (53).
For SSA, genetic research is still in its infancy, but efforts to contribute to the world genetic research are rising (54). Availability of genetic screening tools and application of precision medicine for people of SSA will need genetic studies from SSA. There is therefore a need for active participation in genetic research; as genetic findings from one ethnic group do not wholly translate to another ethnic group. In South Africa, for example, it was recently shown that a gene panel with a yield of >60% in a European population has a yield of only 18% in South Africans with hypertrophic cardiomyopathy (55). In Tanzania, much of the reports on genetic studies have been on sickle cell anemia and malaria (56, 57), as well as on-going research on rare disease conditions. This agenda will focus to put in place infrastructure in terms of resources and human capacity build-up to be able to host a wide range of genetic research on CVD.
Action Points
• Prepare legal framework for genetic research and data collection
• Prepare patients’ involvement groups on genetic research
• Sensitize on volunteer programs for research
• Link–up with national, regional and international collaborators on CVD genetic research.
Strategies for Sustainable Cardiovascular Disease Research Output: Challenges and Opportunities
Strategy 1: Academia
Research undertaking requires human resources, in terms of number, expertise and dedication to lifelong research. In SSA, shortage of human resources for research is a well-recognized barrier to health research output from the region (58–61). The scarcity is in both the number of researchers, as well as the expertise (58, 59). Brain-drain, where young professionals emigrate to HICs for greener pastures (62) compounds the already scarce workforce in the region (63). Furthermore, while the culture of research is strongly embedded (64) and continuously been enhanced (65) in many developed countries, the same is not the case in SSA, where even the career path for a researcher is not well-defined (63). Competing interest with clinical work-load, engagement in private practice for economic reasons and un-interesting research questions (mainly conceived in Western countries), are some of the factors found to influence less interests in research among academic and non-academic health personnel in SSA (63, 66). However, with an increasing number of health care professionals reaching tertiary level education in the region (67), and increasing evidence that Africa-led research undertaking is possible (61) and an effective way to address local health challenges (68), this trend can be changed.
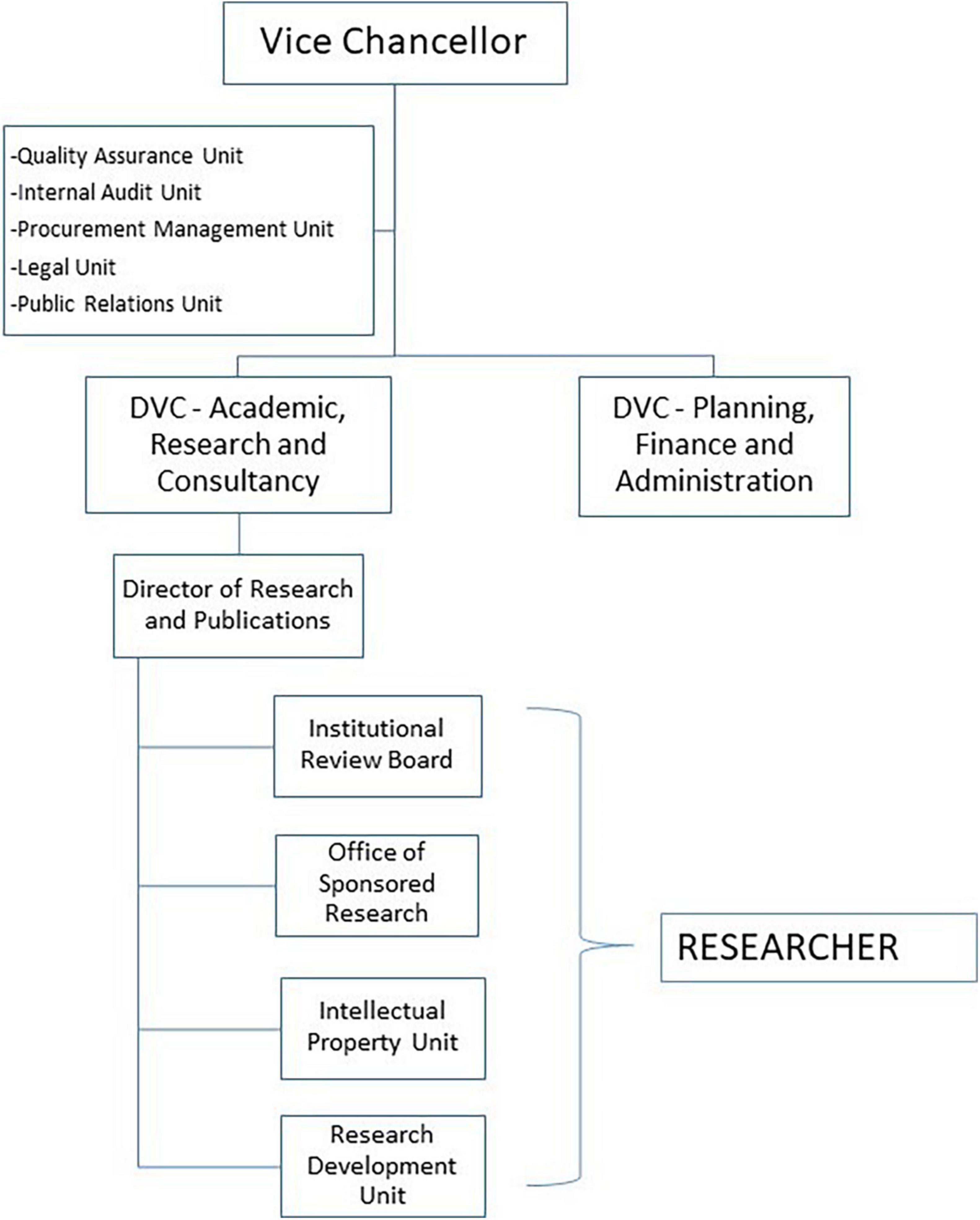
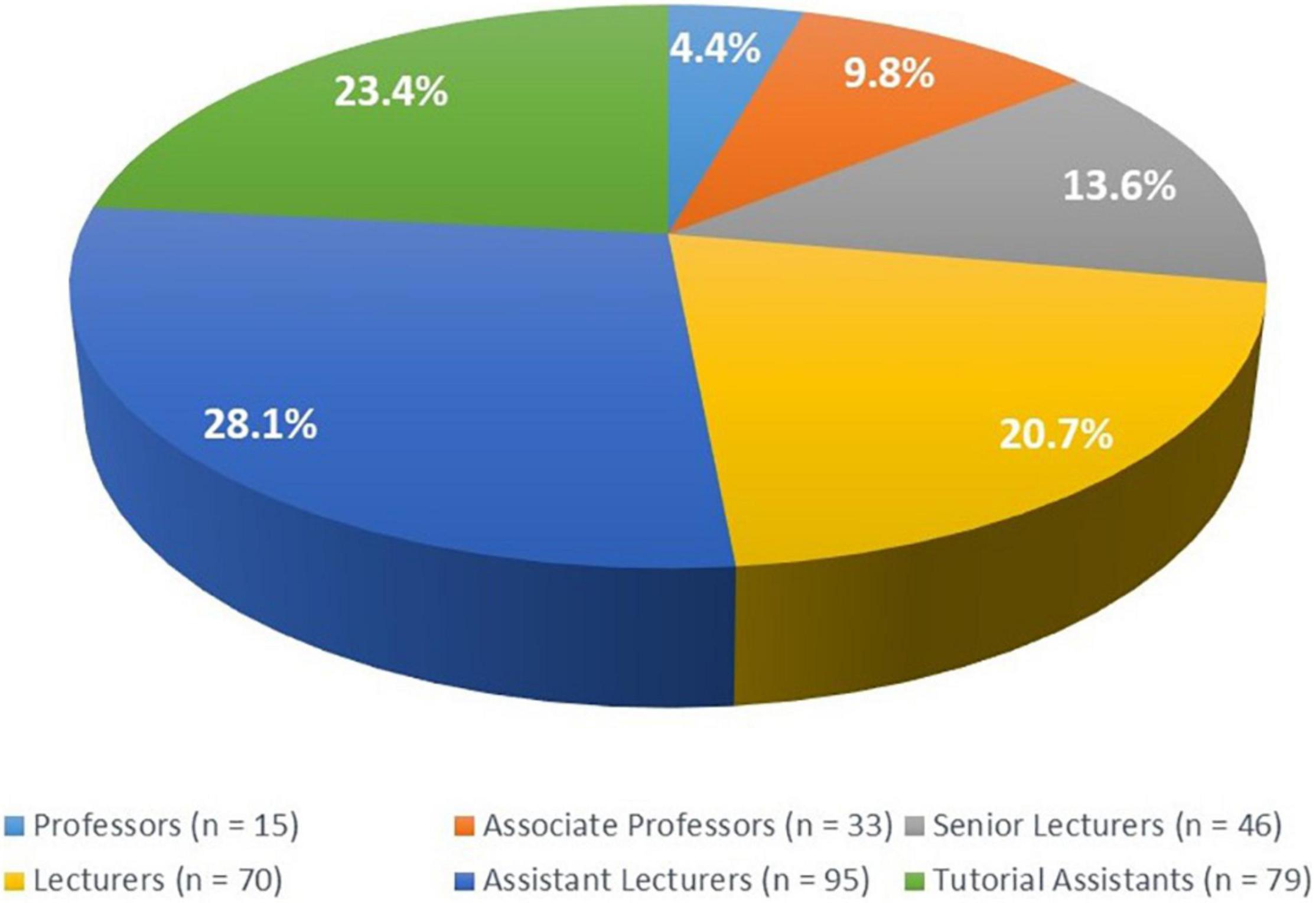
This research agenda will strategically be hosted, implemented, and managed through the existing MUHAS research management systems (Figure 2) and through MUHAS academic programs, its faculty and post-graduate trainees (69). Academic institutions worldwide have traditionally been in the forefront for research, utilizing the dynamic learning environment within them, and the prospect for continuity. The current MUHAS academic profile provides a strong base for current and future research undertakings, taking advantage of relatively many young faculty at the institution (Figure 3).
Furthermore, the scope of researchers for this agenda is not limited to MUHAS as more researchers through collaboration with MUHAS faculty are expected to form part. Here the strategy will be to utilize the existing network of regional and global collaborators in research and faculty/students exchange.
Opportunities
• Higher proportion of young faculty at MUHAS
• Existing programs for CVD specialties that require research (dissertation) in CVD
• Existing researchers in CVD
• Increased popularity of CVD research within MUHAS
• Increased inter-disciplinary research collaboration within MUHAS faculty
• Large network of regional and global collaborators.
Challenges
• There are no specific CVD research training programs at MUHAS
• Very few existing faculty with skills for some areas of CVD research like basic sciences and genetic studies.
Mitigations
• Through the EACoECVS, CVD research training programs will be developed in order to specifically train and create a cadre of researchers in cardiovascular sciences in Tanzania and the East African region.
• Purposely, young faculty will be mentored and trained to develop interest and skills for genetic studies, while taking advantage of knowledge and skills from external collaborators.
Strategy 2: Training
The low level of CVD research output from SSA is partly due to the low number of CVD researchers in the region (58, 59, 61, 63, 70). Furthermore, even with the available numbers, without proper research training, researchers from SSA lack expertise to conduct high caliber research. Proper research training is also a way of creating a culture of research, which has not been a well invested area in most SSA countries (61, 63, 71). Therefore, in order to increase the quantity and quality of research into CVD, there is a need in SSA, to urgently address two issues, i.e., increasing the number of researchers as well as improving their quality in order to produce researchers that will be professionals with in-depth scientific expertise and complementary leadership skills to enable them conduct independent, and internationally recognized CVD research.
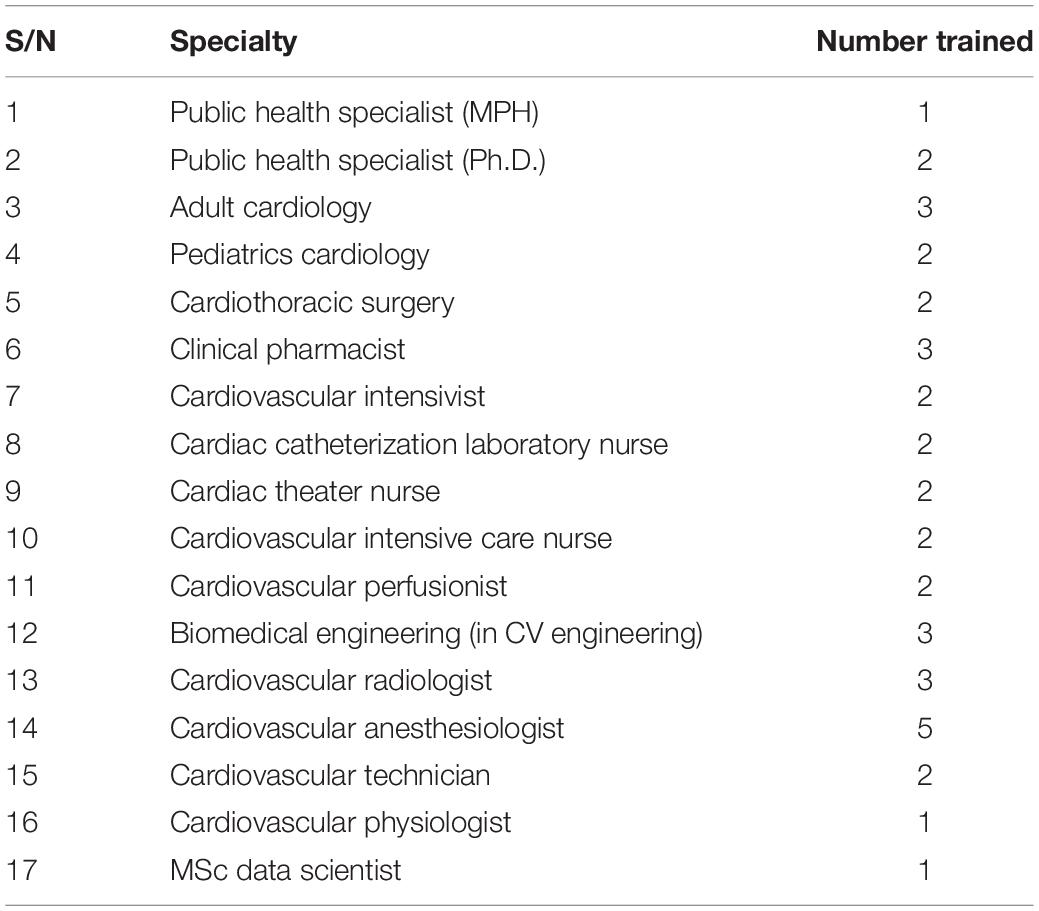
Until now MUHAS, through the EACoECVS has made significant progress in increasing CVD specialties’ training (Table 1). Most of the initial training took place abroad including India, South Africa, Germany, United Kingdom, and Ireland as well as locally in Tanzania. This group of specialists in different CVD fields forms a base for current and future CVD researchers for the center. The strategy is to align these future researchers with the planned research agenda for the center.
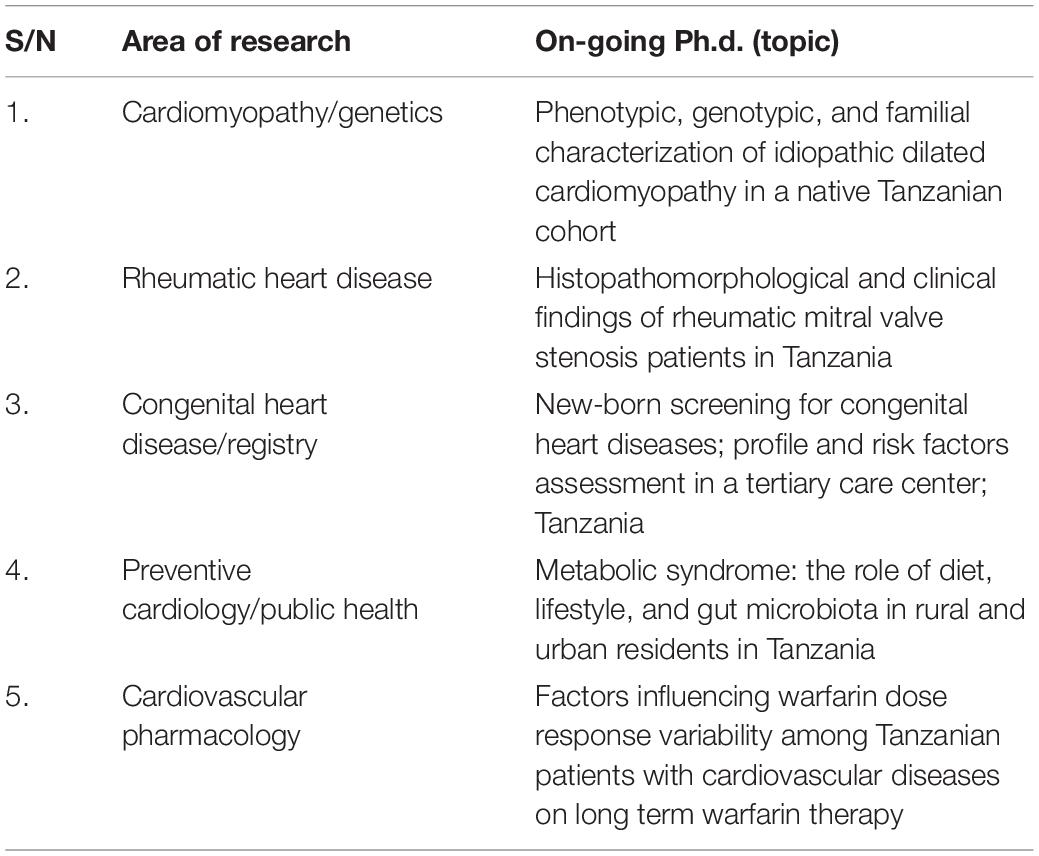
As part of research training at advanced levels, the EACoECVS has entered into memorandum of understanding with the University Medical Center Utrecht (UMCU) for tertiary CVD research training at the UMCU, through joint Ph.D. supervisions between UMCU and MUHAS. In this initiative, currently five Ph.D. fellows from MUHAS have already been registered with the Julius Global Health Ph.D. program and are doing their research in CVD (Table 2). Participants for this program receive all their formal research training in the Netherlands (both physically and through e-learning platforms), including research methods, epidemiology as well as scientific research writing. All research is done in Tanzania, following the research agenda highlighted.
Opportunities
• Presence of the EACoECVS
• Existing programs for CVD training at MUHAS
• Existing collaborators in CVD research
• Already there is a base of young researchers in CVD at MUHAS.
Challenges
• There are still few faculty to conduct CVD research training at MUHAS.
Mitigations
• Continue to work with outside collaborators in CVD research training.
Strategy 3: Infrastructure
Research infrastructure refers to facilities that provide resources, spaces and services for conducting research and foster innovation. In medicine these facilities include dedicated research laboratories, space for clinical trials, major scientific equipment, data repositories and archives, computing systems, and communication networks. Systems for supporting research management including quality assurance, monitoring and evaluation systems, financial systems, and physical space for researchers like faculty and scholars’ offices and lecture rooms are also part and parcel of a viable research environment. In SSA, both physical space and dedicated equipment for research have been in chronic shortage, and have been cited as major stumbling blocks for research undertaking in the region (63, 66, 68). This is further compounded by limited research organization at institutional, country or regional level (59). Over-reliance on infrastructure donation often brings lack of continuity when a certain project or research seizes to operate, leaving expensive machines unused.
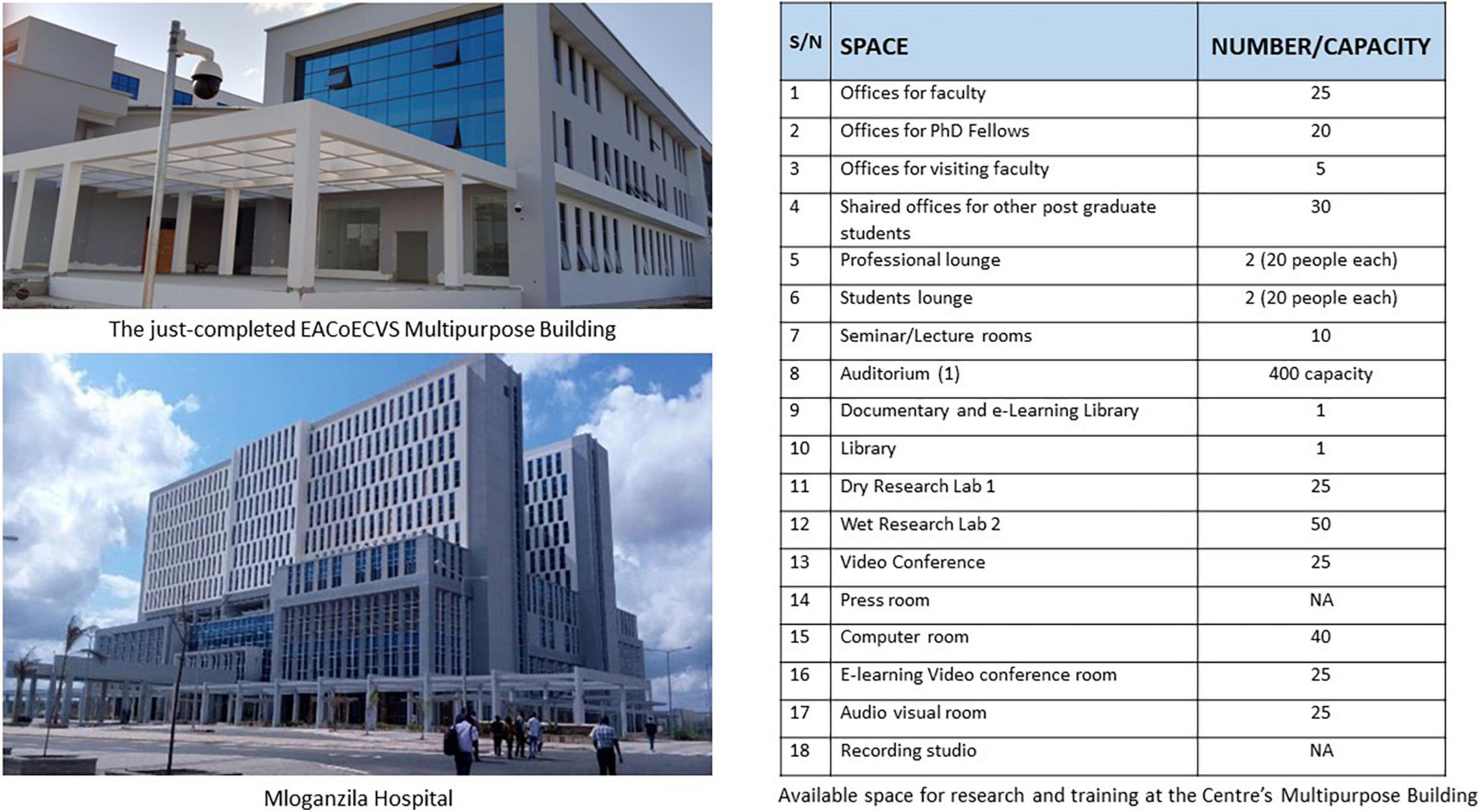
For this research agenda, most of the physical space will be through the deliberately built and strategically placed multipurpose building for the EACoECVS (Figure 4). This building is located at the new MUHAS Campus (approximately 3,800 acres about 25 km on the outskirts of Dar es Salaam city), and is close to the Mloganzila Hospital, a state-of-the art University teaching hospital for MUHAS. The construction of the multipurpose building for the EACoECVS was completed on 31 December 2021, and is expected to be fully functional in June 2022.
Opportunities
• Availability of adequate physical space within the newly built EACoECVS multipurpose building
• Huge space for expansion to include other research facilities
• Existing and functional infrastructure for research within MUHAS
• Existence of functioning/running research laboratories at MUHAS
• Existence of memoranda of understanding for research and clinical services with major public referral hospitals in Tanzania, including the Jakaya Kikwete Cardiac Institute, Muhimbili National Hospital, and Muhimbili – Mloganzila Hospital.
Challenges
• Still, there is insufficient collaboration in CVD research within universities/research organizations within Tanzania and East Africa.
Mitigations
• As custodian for CVD research and training for East Africa, the EACoECVS will organize collaborations between all existing CVD research centers within East Africa as mandated by the wider East African Centres of Excellences for Biomedical Sciences Project.
Strategy 4: Funding
Funding is the backbone of any research endeavor. In developed countries, funding for research is a common practice and has been the driver for major breakthrough in health sciences (72). However, for many SSA countries the culture to fund research is lacking and brings about major challenges (63, 66, 71). Low social economic status of many SSA with competing budget priorities is undeniably the most important factor for poor research funding. However, other factors cited include lack of good governance, corruption and mismanagement of public funds at the higher levels (71). A review of research funding shows many researchers in SSA either self-fund their research or utilize post graduate small-scale dissertation funds to conduct research (63). Recently however, different initiatives have been implemented to facilitate SSA to access global health research funds, mainly by partnering with researchers from developed countries (73). Furthermore, access to other international funders like Bill and Melinda Gates Foundation, the Wellcome Trust, HIV Research Trust, The U.S. President’s Emergency Plan for AIDS Relief (PEPFAR), and others have been instrumental to funding research in SSA, mostly in infectious diseases (74). Only recently, funding for NCDs have emerged, although still very insufficient and with stiff competition (75).
This research agenda will not be practical without funding. As custodian of cardiovascular research in Tanzania, efforts to access cardiovascular research funds will be upgraded by equipping current and future generation researchers with skills to write competitive research grants. In publishing this agenda, potential collaborators for research from around the globe are being reached out, for the purpose of forming collaborations regionally and worldwide in order to attain sharing of research resources for a common goal. Locally, efforts to solicit research funding and support from government and non-governmental organizations will continue. This strategy will also involve reaching out to private partners, local philanthropists, businessmen and women as well as industries interested in cardiovascular research.
Opportunities
• Availability of competitive international funding organs for CVD research
• Increased global awareness of CVD as important developmental challenge.
Challenges
• Lack of research funding from national budget
• Less competitive advantages in proposal writing due to limited skills/expertise
• Expensive research undertakings
• Normally, donor-driven research questions
• Post-donor funded project discontinuation.
Mitigations
• Enforce efforts to solicit research funds through training, lobbying and involvement of the private sector.
Conclusion
Despite many challenges, there are opportunities that can be taken advantage of, for a sustainable CVD research in Tanzania; the greatest opportunity being the evolving EACoECVS. Training of current and future faculty to take lead in CVD research will have a lasting legacy in this area, and will help to address the existing gap in establishment of locally informed CVD management and policy changes.
The high-level commitment in addressing the CVD burden shown by the Tanzanian Government can be taken as a lesson to other SSA countries that are yet to take decisive actions. In setting this research agenda we believe the research community from other SSA countries will learn and benchmark from it in prioritizing research areas, mobilizing resources and training of CVD researchers in the region.
Author Contributions
PC, FM, and GK conceptualized the idea. PC performed literature search and wrote the first draft of the manuscript. FM, GK, PR, and AK critically reviewed the manuscript. All authors contributed to the manuscript and approved the final version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We acknowledge the administrative support given by MUHAS during the preparation of this manuscript. We also acknowledge Dr. Lulu Fundikira for her assistance in literature search for use in this review.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcvm.2022.849007/full#supplementary-material
References
1. GBD 2017 Causes of Death Collaborators. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980-2017: a systematic analysis for the global burden of disease study 2017. Lancet. (2018) 392:1736–88. doi: 10.1016/S0140-6736(18)32203-7
2. Cappuccio FP, Miller MA. Cardiovascular disease and hypertension in sub-Saharan Africa: burden, risk and interventions. Intern Emerg Med. (2016) 11:299–305. doi: 10.1007/s11739-016-1423-9
3. Gbd 2017 DALYs and Hale Collaborators. Global, regional, and national disability-adjusted life-years (DALYs) for 359 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990-2017: a systematic analysis for the global burden of disease study 2017. Lancet. (2018) 392:1859–922. doi: 10.1016/S0140-6736(18)32335-3
4. Mayige M, Kagaruki G. Tanzania STEPS Survey Report. (2013). Available online at : wwwwhoint/ncds/surveillance/steps/UR_Tanzania_2012_STEPS_Reportpdf.2013 (accessed October 7, 2020).
5. Roman WPMHD, Sauli E. Cardiovascular diseases in Tanzania: the burden of modifiable and intermediate risk factors. J Xiangya Med. (2019) 4:33.
6. Keates AK, Mocumbi AO, Ntsekhe M, Sliwa K, Stewart S. Cardiovascular disease in Africa: epidemiological profile and challenges. Nat Rev Cardiol. (2017) 14:273–93. doi: 10.1038/nrcardio.2017.19
7. Saidi H, Smart LR, Kamugisha E, Ambrose EE, Soka D, Peck RN, et al. Complications of sickle cell anaemia in children in Northwestern Tanzania. Hematology. (2016) 21:248–56. doi: 10.1080/10245332.2015.1101976
8. Jamerson KA. The disproportionate impact of hypertensive cardiovascular disease in African Americans: getting to the heart of the issue. J Clin Hypertens (Greenwich). (2004) 6:4–10. doi: 10.1111/j.1524-6175.2004.03563.x
9. UNDP.Sustainable Development Goals | United Nations Development Programme. (2022). Available online at: https://www.undp.org/sustainable-development-goals (accessed February 12, 2022)
10. Regional Committee for Africa.Accelerating The Response To Noncommunicable Diseases in the African Region in Line with the Political Declaration of the High-Level Meeting of the General Assembly on the Prevention and Control of NCDS: Report of the Secretariat. (2020). Available online at: https://apps.who.int/iris/handle/10665/331542 (accessed October 7, 2020).
11. Moh.go.tz.Strategic and Action Plan for the Prevention and Control of Non Communicable Diseases in Tanzania 2016 – 2020. (2022). Available online at: https://www.moh.go.tz/en/strategic-plans?download=196:strategic-and-action-plan-for-the-prevention-and-control-of-non-communicable-diseases-in-tanzania-2016-%E2%80%93-2020 (accessed February 12, 2022)
12. University World News.Four East Africa Medical Centres of Excellence Underway. (2012). Available online at: https://www.universityworldnews.com/post.php?story=20151009080919608 (accessed October 7, 2020)
13. Makubi A, Hage C, Lwakatare J, Kisenge P, Makani J, Ryden L, et al. Contemporary aetiology, clinical characteristics and prognosis of adults with heart failure observed in a tertiary hospital in Tanzania: the prospective Tanzania heart failure (TaHeF) study. Heart. (2014) 100:1235–41. doi: 10.1136/heartjnl-2014-305599
14. Furia FF, Shoo J, Ruggajo PJ, Kilonzo K, Basu G, Yeates K, et al. Developing nephrology services in low income countries: a case of Tanzania. BMC Nephrol. (2019) 20:378. doi: 10.1186/s12882-019-1568-7
15. Walker R, Whiting D, Unwin N, Mugusi F, Swai M, Aris E, et al. Stroke incidence in rural and urban Tanzania: a prospective, community-based study. Lancet Neurol. (2010) 9:786–92. doi: 10.1016/S1474-4422(10)70144-7
16. Raphael DM, Roos L, Myovela V, McHomvu E, Namamba J, Kilindimo S, et al. Heart diseases and echocardiography in rural Tanzania: occurrence, characteristics, and etiologies of underappreciated cardiac pathologies. PLoS One. (2018) 13:e0208931. doi: 10.1371/journal.pone.0208931
17. Chillo P, Bakari M, Lwakatare J. Echocardiographic diagnoses in HIV-infected patients presenting with cardiac symptoms at Muhimbili National hospital in Dar es Salaam, Tanzania. Cardiovasc J Afr. (2012) 23:90–7.
18. Cegielski JP, Lwakatare J, Dukes CS, Lema LE, Lallinger GJ, Kitinya J, et al. Tuberculous pericarditis in Tanzanian patients with and without HIV infection. Tuber Lung Dis. (1994) 75:429–34. doi: 10.1016/0962-8479(94)90116-3
19. WHO.Institute for Health Metrics and Evaluation. (2020). Available online at: http://www.healthdata.org/tanzania (accessed October 7, 2020).
20. The World Bank.Current Health Expenditure Per Capita (Current US$) – Tanzania | Data. (2020). Available online at: http://www.healthdata.org/tanzania (accessed October 10, 2020).
21. Mocumbi AO. Lack of focus on cardiovascular disease in sub-Saharan Africa. Cardiovasc Diagn Ther. (2012) 2:74–7. doi: 10.3978/j.issn.2223-3652.2012.01.03
22. Kariuki JK, Stuart-Shor EM, Leveille SG, Hayman LL. Methodological challenges in estimating trends and burden of cardiovascular disease in sub-Saharan Africa. Cardiol Res Pract. (2015) 2015:921021. doi: 10.1155/2015/921021
23. Roth GA, Johnson C, Abajobir A, Abd-Allah F, Abera SF, Abyu G, et al. Global, regional, and national burden of cardiovascular diseases for 10 causes, 1990 to 2015. J Am Coll Cardiol. (2017) 70:1–25. doi: 10.1016/j.jacc.2017.04.052
24. Hajar R. Framingham contribution to cardiovascular disease. Heart Views. (2016) 17:78–81. doi: 10.4103/1995-705X.185130
25. Rippe JM. Lifestyle strategies for risk factor reduction, prevention, and treatment of cardiovascular disease. Am J Lifestyle Med. (2019) 13:204–12. doi: 10.1177/1559827618812395
26. Boateng D, Wekesah F, Browne JL, Agyemang C, Agyei-Baffour P, Aikins AD, et al. Knowledge and awareness of and perception towards cardiovascular disease risk in sub-Saharan Africa: a systematic review. PLoS One. (2017) 12:e0189264. doi: 10.1371/journal.pone.0189264
27. Mosha NR, Mahande M, Juma A, Mboya I, Peck R, Urassa M, et al. Prevalence, awareness and factors associated with hypertension in North West Tanzania. Glob Health Action. (2017) 10:1321279. doi: 10.1080/16549716.2017.1321279
28. Chrysant SG. A new paradigm in the treatment of the cardiovascular disease continuum: focus on prevention. Hippokratia. (2011) 15:7–11.
29. Matuja SS, Munseri P, Khanbhai K. The burden and outcomes of stroke in young adults at a tertiary hospital in Tanzania: a comparison with older adults. BMC Neurol. (2020) 20:206. doi: 10.1186/s12883-020-01793-2
30. Chillo P, Lwakatare J, Rieck AE, Lutale J, Gerdts E. Prevalence and covariates of abnormal left ventricular geometry in never-treated hypertensive patients in Tanzania. Blood Press. (2014) 23:31–8. doi: 10.3109/08037051.2013.791415
31. Kilonzo S, Abdulraassul T, Bakshi D, Fatma A, Gunda DW. Renal dysfunction among adult patients in Mwanza, Tanzania: prevalence, outcomes and associated factors. Tanzan J Health Res. (2016) 18:1–18.
32. Virani SS, Alonso A, Benjamin EJ, Bittencourt MS, Callaway CW, Carson AP, et al. Heart disease and stroke statistics-2020 update: a report from the american heart association. Circulation. (2020) 141:e139–596.
33. Aminde LN, Takah NF, Zapata-Diomedi B, Veerman JL. Primary and secondary prevention interventions for cardiovascular disease in low-income and middle-income countries: a systematic review of economic evaluations. Cost Eff Resour Alloc. (2018) 16:22. doi: 10.1186/s12962-018-0108-9
34. Ngalesoni FN, Ruhago GM, Mori AT, Robberstad B, Norheim OF. Cost-effectiveness of medical primary prevention strategies to reduce absolute risk of cardiovascular disease in Tanzania: a Markov modelling study. BMC Health Serv Res. (2016) 16:185. doi: 10.1186/s12913-016-1409-3
35. Rossignol P, Lainscak M, Crespo-Leiro MG, Laroche C, Piepoli MF, Filippatos G, et al. Unravelling the interplay between hyperkalaemia, renin-angiotensin-aldosterone inhibitor use and clinical outcomes. Data from 9222 chronic heart failure patients of the ESC-HFA-EORP heart failure long-term registry. Eur J Heart Fail. (2020) 22:1378–89. doi: 10.1002/ejhf.1793
36. Gitt AK, Bueno H, Danchin N, Fox K, Hochadel M, Kearney P, et al. The role of cardiac registries in evidence-based medicine. Eur Heart J. (2010) 31:525–9. doi: 10.1093/eurheartj/ehp596
37. Gupta A, Yu Y, Tan Q, Liu S, Masoudi FA, Du X, et al. Quality of care for patients hospitalized for heart failure in China. JAMA Netw Open. (2020) 3:e1918619. doi: 10.1001/jamanetworkopen.2019.18619
38. Mandi DG, Bamouni J, Yameogo RA, Naibe DT, Kabore E, Kambire Y, et al. Spectrum of heart failure in sub-Saharan Africa: data from a tertiary hospital-based registry in the eastern center of Burkina Faso. Pan Afr Med J. (2020) 36:30. doi: 10.11604/pamj.2020.36.30.19321
39. Sliwa K, Wilkinson D, Hansen C, Ntyintyane L, Tibazarwa K, Becker A, et al. Spectrum of heart disease and risk factors in a black urban population in South Africa (the Heart of Soweto Study): a cohort study. Lancet. (2008) 371:915–22. doi: 10.1016/S0140-6736(08)60417-1
40. Karthikeyan G, Zuhlke L, Engel M, Rangarajan S, Yusuf S, Teo K, et al. Rationale and design of a global rheumatic heart disease registry: the REMEDY study. Am Heart J. (2012) 163:535–40.e1. doi: 10.1016/j.ahj.2012.01.003
41. Sani MU, Cotter G, Davison BA, Mayosi BM, Damasceno A, Edwards C, et al. Symptoms and signs of heart failure at admission and discharge and outcomes in the sub-saharan acute heart failure (THESUS-HF) registry. J Card Fail. (2017) 23:739–42. doi: 10.1016/j.cardfail.2016.09.016
42. Jandhyala R, Christopher S. Factors influencing the generation of evidence from simple data held in international rare disease patient registries. Pharmaceut Med. (2020) 34:31–8. doi: 10.1007/s40290-019-00316-w
43. Hemingway H, Asselbergs FW, Danesh J, Dobson R, Maniadakis N, Maggioni A, et al. Big data from electronic health records for early and late translational cardiovascular research: challenges and potential. Eur Heart J. (2018) 39:1481–95. doi: 10.1093/eurheartj/ehx487
44. Weintraub WS, Fahed AC, Rumsfeld JS. Translational medicine in the era of big data and machine learning. Circ Res. (2018) 123:1202–4.
45. Akanbi MO, Ocheke AN, Agaba PA, Daniyam CA, Agaba EI, Okeke EN, et al. Use of electronic health records in sub-Saharan Africa: progress and challenges. J Med Trop. (2012) 14:1–6.
46. Mashoka RJ, Murray B, George U, Lobue N, Mfinanga J, Sawe H, et al. Implementation of electronic medical records at an Emergency Medicine Department in Tanzania: The information technology perspective. Afr J Emerg Med. (2019) 9:165–71. doi: 10.1016/j.afjem.2019.07.002
47. Health Informatics Association.Tanzania Digital Health Investment Road Map. (2017). Available online at: https://path.azureedge.net/media/documents/Tanzania_Digital_Health_Investment_Road_Map.2017_to_2023.pdf (accessed October 14, 2020).
48. Tzdpg.or.tz.Tanzania_Key_Health. (2020). Available online at: http://www.tzdpg.or.tz/fileadmin/documents/dpg_internal/dpg_working_groups_clusters/cluster_2/health/Key_Sector_Documents/Tanzania_Key_Health_Documents/Tz_eHealth_Strategy_Final.pdf (accessed October 14, 2020]
49. Maokola W, Willey BA, Shirima K, Chemba M, Armstrong Schellenberg JR, Mshinda H, et al. Enhancing the routine health information system in rural southern Tanzania: successes, challenges and lessons learned. Trop Med Int Health. (2011) 16:721–30. doi: 10.1111/j.1365-3156.2011.02751.x
50. Molster CM, Bowman FL, Bilkey GA, Cho AS, Burns BL, Nowak KJ, et al. The evolution of public health genomics: exploring its past, present, and future. Front Public Health. (2018) 6:247. doi: 10.3389/fpubh.2018.00247
51. Welter D, MacArthur J, Morales J, Burdett T, Hall P, Junkins H, et al. The NHGRI GWAS catalog, a curated resource of SNP-trait associations. Nucleic Acids Res. (2014) 42:D1001–6. doi: 10.1093/nar/gkt1229
52. International Consortium for Blood Pressure Genome-Wide Association Studies, Ehret GB, Munroe PB, Rice KM, Bochud M, Johnson AD, et al. Genetic variants in novel pathways influence blood pressure and cardiovascular disease risk. Nature. (2011) 478:103–9.
53. Li Y, Zhao Q, Liu XL, Wang LY, Lu XF, Li HF, et al. Relationship between cystathionine gamma-lyase gene polymorphism and essential hypertension in Northern Chinese han population. Chin Med J (Engl). (2008) 121:716–20.
54. Adebamowo SN, Tekola-Ayele F, Adeyemo AA, Rotimi CN. Genomics of cardiometabolic disorders in sub-Saharan Africa. Public Health Genomics. (2017) 20:9–26. doi: 10.1159/000468535
55. Ntusi NA, Shaboodien G, Badri M, Gumedze F, Mayosi BM. Clinical features, spectrum of causal genetic mutations and outcome of hypertrophic cardiomyopathy in South Africans. Cardiovasc J Afr. (2016) 27:152–8.
56. Nkya S, Mwita L, Mgaya J, Kumburu H, van Zwetselaar M, Menzel S, et al. Identifying genetic variants and pathways associated with extreme levels of fetal hemoglobin in sickle cell disease in Tanzania. BMC Med Genet. (2020) 21:125. doi: 10.1186/s12881-020-01059-1
57. Morgan AP, Brazeau NF, Ngasala B, Mhamilawa LE, Denton M, Msellem M, et al. Falciparum malaria from coastal Tanzania and Zanzibar remains highly connected despite effective control efforts on the archipelago. Malar J. (2020) 19:47. doi: 10.1186/s12936-020-3137-8
58. Volmink J, Dare L. Addressing inequalities in research capacity in Africa. BMJ. (2005) 331:705–6. doi: 10.1136/bmj.331.7519.705
59. Whitworth JA, Kokwaro G, Kinyanjui S, Snewin VA, Tanner M, Walport M, et al. Strengthening capacity for health research in Africa. Lancet. (2008) 372:1590–3. doi: 10.1016/S0140-6736(08)61660-8
60. Izugbara CO, Kabiru CW, Amendah D, Dimbuene ZT, Donfouet HPP, Atake EH, et al. “It takes more than a fellowship program”: reflections on capacity strengthening for health systems research in sub-Saharan Africa. BMC Health Serv Res. (2017) 17:696. doi: 10.1186/s12913-017-2638-9
61. Kasprowicz VO, Chopera D, Waddilove KD, Brockman MA, Gilmour J, Hunter E, et al. African-led health research and capacity building– is it working? BMC Public Health. (2020) 20:1104.
63. Kanmounye US, Jumbam DT, Endoma FT, Tochie JN, Mbonda AN, Ghomsi NC. Advancing medical research in sub-Saharan Africa: barriers, facilitators, and proposed solutions. Pan Afr Med J. (2020) 3:83.
64. Dimond EP, St Germain D, Nacpil LM, Zaren HA, Swanson SM, Minnick C, et al. Creating a “culture of research” in a community hospital: strategies and tools from the National cancer institute community cancer centers program. Clin Trials. (2015) 12:246–56. doi: 10.1177/1740774515571141
65. Slade SC, Philip K, Morris ME. Frameworks for embedding a research culture in allied health practice: a rapid review. Health Res Policy Syst. (2018) 16:29. doi: 10.1186/s12961-018-0304-2
66. Conradie A, Duys R, Forget P, Biccard BM. Barriers to clinical research in Africa: a quantitative and qualitative survey of clinical researchers in 27 African countries. Br J Anaesth. (2018) 121:813–21. doi: 10.1016/j.bja.2018.06.013
67. UNESCO.Trends In Tertiary Education:Sub-Saharan Africa. (2020). Available online at: <http://uis.unesco.org/sites/default/files/documents/fs10-trends-in-tertiary-education-sub-saharan-africa-2010-en.pdf> (accessed 14 November 2020).
68. Chu KM, Jayaraman S, Kyamanywa P, Ntakiyiruta G. Building research capacity in Africa: equity and global health collaborations. PLoS Med. (2014) 11:e1001612. doi: 10.1371/journal.pmed.1001612
69. MUHAS.Home | Muhimbili University of Health and Allied Sciences. (2020). Available online at: https://www.muhas.ac.tz/ (accessed 21 November 2020)
70. Kabiru CW, Izugbara CO, Wairimu J, Amendah D, Ezeh AC. Strengthening local health research capacity in Africa: the African Doctoral Dissertation research fellowship program. Pan Afr Med J. (2014) 17:1. doi: 10.11694/pamj.supp.2014.17.1.3729
71. Laabes EP, Desai R, Zawedde SM, Glew RH. How much longer will Africa have to depend on western nations for support of its capacity-building efforts for biomedical research? Trop Med Int Health. (2011) 16:258–62. doi: 10.1111/j.1365-3156.2010.02709.x
72. Fabbri A, Lai A, Grundy Q, Bero LA. The influence of industry sponsorship on the research agenda: a scoping review. Am J Public Health. (2018) 108:e9–16. doi: 10.2105/AJPH.2018.304677
73. Boum Ii Y, Burns BF, Siedner M, Mburu Y, Bukusi E, Haberer JE. Advancing equitable global health research partnerships in Africa. BMJ Glob Health. (2018) 3:e000868. doi: 10.1136/bmjgh-2018-000868
74. Viergever RF, Hendriks TC. The 10 largest public and philanthropic funders of health research in the world: what they fund and how they distribute their funds. Health Res Policy Syst. (2016) 14:12. doi: 10.1186/s12961-015-0074-z
Keywords: cardiovascular disease, cardiovascular research, Tanzania, research training, research strategy, sub-Saharan Africa, center of excellence
Citation: Chillo P, Mashili F, Kwesigabo G, Ruggajo P and Kamuhabwa A (2022) Developing a Sustainable Cardiovascular Disease Research Strategy in Tanzania Through Training: Leveraging From the East African Centre of Excellence in Cardiovascular Sciences Project. Front. Cardiovasc. Med. 9:849007. doi: 10.3389/fcvm.2022.849007
Received: 05 January 2022; Accepted: 01 March 2022;
Published: 25 March 2022.
Edited by:
Lebo F. Gafane-Matemane, North-West University, South AfricaReviewed by:
Daniel Boateng, University Medical Center Utrecht, NetherlandsJuliana Kagura, University of the Witwatersrand, South Africa
Copyright © 2022 Chillo, Mashili, Kwesigabo, Ruggajo and Kamuhabwa. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Pilly Chillo, cGNoaWxsb0BtdWhhcy5hYy50eg==; cGNoaWxsbzIwMDBAeWFob28uY28udWs=
 Pilly Chillo
Pilly Chillo Fredirick Mashili
Fredirick Mashili Gideon Kwesigabo
Gideon Kwesigabo Paschal Ruggajo
Paschal Ruggajo Appolinary Kamuhabwa
Appolinary Kamuhabwa