- Instituto Tecnológico de Informática, Valencia, Spain
Virtual and augmented reality have been used to diagnose and treat several mental health disorders for decades. Technological advances in these fields have facilitated the availability of commercial solutions for end customers and practitioners. However, there are still some barriers and limitations that prevent these technologies from being widely used by professionals on a daily basis. In addition, the COVID-19 pandemic has exposed a variety of new scenarios in which these technologies could play an essential role, like providing remote treatment. Disorders that traditionally had received less attention are also getting in the spotlight, such as depression or obsessive-compulsive disorder. Improvements in equipment and hardware, like Mixed Reality Head Mounted Displays, could help open new opportunities in the mental health field. Extended reality (XR) is an umbrella term meant to comprise Virtual reality (VR), mixed reality (MR), and augmented reality (AR). While XR applications are eminently visual, other senses are being explored in literature around multisensory interactions, such as auditory, olfactory, or haptic feedback. Applying such stimuli within XR experiences around mental disorders is still under-explored and could greatly enrich the therapeutic experience. This manuscript reviews recent research regarding the use of XR for mental health scenarios, highlighting trends, and potential applications as well as areas for improvement. It also discusses future challenges and research areas in upcoming topics such as the use of wearables, multisensory, and multimodal interaction. The main goal of this paper is to unpack how these technologies could be applied to XR scenarios for mental health to exploit their full potential and follow the path of other health technologies by promoting personalized medicine.
1. Introduction
In recent years, mental health is beginning to be acknowledged as an essential part of individual and global well-being. The World Health Organization has included it in the Sustainable Development Goals and estimates that about 25% of the world's population experiences a mental health problem at some point in their life (WHO et al., 2021). In addition, mental health conditions are among the leading causes of disabilities, comorbidity, and premature deaths1,2. The COVID-19 pandemic has also affected the global prevalence of disorders such as anxiety and depression by 25% worldwide 3.
Technology plays an essential role in supporting mental health, as it can be applied for screening, diagnosis, treatment of mental health conditions, and improving general well-being. Both commercial and research applications have used different types of technologies to address a diverse set of pathologies. The most common one has been the use of mobiles/tablets and e-Health applications, either for collecting data from the mobile device passively (e.g., GPS location, daily steps) or through daily questionnaires that the user has to fill in about how they are feeling (Wang et al., 2018; Habets et al., 2020). Gesture recognition devices such as LeapMotion have been used for games to improve cognitive and motor skills in people with attention deficit and hyperactivity disorder (ADHD) (Garcia-Zapirain et al., 2017), or autism spectrum disorder (ASD) (Cai et al., 2018). Body movement detection has also been used to detect anxiety or depression based on walking posture (Zhao et al., 2019), or stereotypies in ASD (Jazouli et al., 2019). Regarding eye-tracking technology, it has been helpful to observe differences in the patterns of users with or without ASD (Eraslan et al., 2019). Several studies have also been carried out with robots, which allow working on social or emotional aspects through conversation or care (Moyle et al., 2013; Yun et al., 2017; Choi et al., 2019).
One of the technologies that is gaining momentum is extended reality (XR). Extended reality (Chuah, 2018; Mann et al., 2018) encompasses virtual reality (VR), augmented reality (AR), and mixed reality (MR). Virtual reality makes reference to fully computer graphics (CG) generated environments, AR means overlaying CG elements on the real world, and MR is built on AR scheme but with VR interaction capabilities with synthetic assets. Each technology has different characteristics that could be explored to contribute to diverse mental health conditions, but, in general, they share some intrinsic immersive capabilities. Immersion represents the potential of technology to surround someone perceptually and to make them believe that the digital environment they are experiencing is “real” (Slater, 2018). Believe and real are words used here by simplification since users actually know that what is happening inside and XR experience is not real but, as it occurs in cinema and theater, they self-impose their cognition as a kind of temporary willing suspension of disbelief (Coleridge, 1984). Immersion generates the feeling of presence, which is a subjective construct that represents how much “real” a virtual experience might feel for a user immersed in an XR environment (Slater et al., 1994). Presence is commonly linked to the feeling of “being there,” where users experiment the virtual world more intensely than the actual world. Understanding immersion and presence in XR experiences is so relevant for researchers and practitioners. These concepts are key in enabling XR as one of the most promising technologies in supporting mental health applications and interventions in the upcoming years, since they are responsible for turning virtual worlds in believable and transferable scenarios.
2. Extended reality for mental health
Usually, XR experiences for mental health are based on Cognitive Behavioral Therapy (CBT, focuses on identifying and changing cognitive distortions) and exposure therapy (involves gradually exposing the patient to the discomfort source or its context) to make patients face an uncomfortable or fearful situation in a controlled scenario. Following the therapist's guidance, the patient works on understanding the cognitive biases and thoughts that trigger their well-being, such as increased anxiety or panic. Across the literature in XR for mental health, VR technology has received more attention than AR, being MR research almost non-existent. Related works have explored the use of VR for treating acrophobia (Donker et al., 2019; Bălan et al., 2020; Giraldy and Novaldo, 2022), agoraphobia in patients with panic attacks (Lundin et al., 2022) or psychosis (Freeman et al., 2022), social phobia (Wechsler et al., 2019), or obsessive-compulsive disorder (OCD) (Laforest et al., 2016; Francova et al., 2019; Miegel et al., 2022). These interventions are highly effective thanks to the sense of presence that VR environments allow. This is because users' psycho-cognitive reactions to XR exposure are entirely similar to those in the real world (Loomis et al., 1999) to the same stimuli even though they know that the environment is synthetically generated.
Comparative studies demonstrate that VR and AR exposure therapy are useful alternatives to traditional in-vivo treatments for small animal phobia (Suso-Ribera et al., 2019). For example, there are works exploring AR mobile apps for exposure therapy with cockroaches (Botella et al., 2010) or spiders (Zimmer et al., 2021), which obtained very positive results, and recent works have also combined tactile feedback in these experiences (Kurscheidt et al., 2019).
However, other mechanisms and procedures within CBT allow working on reducing cognitive biases and negative thoughts without relying on direct exposure to scenarios that elicit anxiety or fear. For example, compassion-focused therapy (CFT, encouraging people in treatment to be compassionate toward themselves and other people) have been shown to be effective in increasing cognitive empathy and compassion, and reducing stress, anxiety, and depression. Falconer et al. (2016) developed a VR experience to practice self-compassion in patients with depression, in which they delivered compassion in one virtual body and then received it in another one. Cebolla et al. (2019) designed a multi-sensory VR experience to induce a body swap illusion, in which participants saw themselves from a third perspective and had the illusion of touching themselves from outside. Recent works have studied different ways of managing mental health conditions with technological interventions other than XR experiences. For example, by personalizing and then destroying avatars that represent a patient's anxiety or fear (Pimentel and Kalyanaraman, 2020), or using games to manage anxiety (Schoneveld et al., 2016) and depression (Fleming et al., 2019).
Extended reality scenarios have also been applied for clinical assessment of specific treats of a disorder such as ASD (Alcañiz et al., 2022) or ADHD (Goharinejad et al., 2022), as well as to help those individuals to practice skills such as attention (Vahabzadeh et al., 2018), social, and communicative behaviors (Mesa-Gresa et al., 2018; Thai and Nathan-Roberts, 2018; Marto and Almeida, 2019).
In addition, there are mental disorders that historically have received more attention and effort from a technological point of view, such as ASD or depression (Riva et al., 2015). However, other mental health conditions such as schizophrenia (Bisso et al., 2020), OCD (van Loenen et al., 2022), borderline personality disorder, or anxiety have been less explored, especially within XR scenarios.
Age is also an essential factor to consider in designing proper XR interventions. So far, research has been mainly oriented toward adults. Extended reality for elders, especially VR, has shown good usability and acceptance (Tuena et al., 2020), and has primarily focused on dementia and its derived consequences on well-being and cognition (D'Cunha et al., 2019; Lee et al., 2019). Extended reality experiences for children have mainly focused on neurodevelopmental disorders such as ASD or ADHD. However, recent reports show a rapid increase in anxiety and depression disorders in children and teenagers, especially after COVID'19 pandemics (Hafstad et al., 2020; Zhang et al., 2020; Pizarro-Ruiz and Ordóñez-Camblor, 2021; Bera et al., 2022). Technological XR interventions could play an essential role in supporting not only mental health conditions but also emotional management (Colombo et al., 2019; Macey et al., 2022) and self-compassion in these age ranges (Ventura et al., 2018; Baghaei et al., 2019).
In this regard, ludic experiences can be better suited to appeal to children and teenagers. Recent works explore how VR and AR games can help children with ADHD improve their attention (Davis et al., 2018). Montaner-Marco et al. (2021) propose a mobile AR application allowing the customization of gamified tasks aimed to facilitate everyday activities for families and children with ASD.
Given the wide range of existing scenarios, technologies, and mental health conditions, there are still many challenges and opportunities to unravel regarding the use of XR technologies to improve mental health conditions. The following sections will review several aspects to be considered by researchers working in this area, defining promising lines of work to advance the field.
3. Challenges
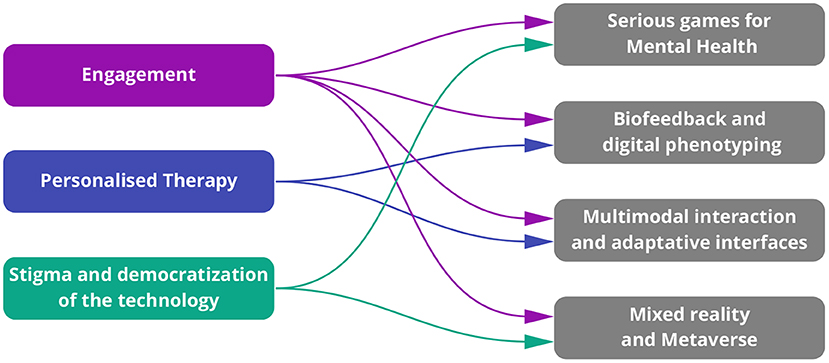
This section will discuss the three key challenges that XR needs to address to maximize its potential in the mental health field. These challenges are also shown on the left side in Figure 1.
3.1. Engagement
One of the main issues with current e-Health applications and technological interventions is the lack of motivation for patients to maintain a sustained and periodic use of the technology (Yang et al., 2022). Among the factors that cause this lack of interest are not perceiving the usefulness of the intervention and poor adaptation to the users' level of expertise with the technology leading to frustration (Donkin and Glozier, 2012; Nickbakht et al., 2020). Mobile apps that require the user to update their status periodically, feelings, or thoughts can be tedious to use on a daily basis, and users frequently stop providing updates to the app over time (Rickard et al., 2016). On the other side, there are applications and platforms that gather information from the user's patterns in the background without actively trying to engage the user in any kind of interaction. Active participation of patients in their therapeutic activities is essential to improve the impact that technological advances might have on these interventions (Yang et al., 2022). Extended reality scenarios offer an auspicious opportunity in this regard: the user has to participate in the activities actively, but the application can extract information from their performance transparently and unobtrusively.
Extended reality applications provide a novel and motivating way for patients to perform their therapeutic activities. However, the novelty effect might deteriorate as the user explores the application. Interventions that always propose the same activities without adaptation or professional supervision tend to result in treatment dropout (Donkin et al., 2011). It is, therefore, vital to find a balance between the learning curve and the novelty factor to create a suitable and engaging patient experience to facilitate treatment adherence.
However, while mobile apps, websites, and games have a wide historical background in user experience research, XR scenarios are still in their infancy regarding heuristics and UX standards. Hence, when developing mental health experiences for XR, it is essential to understand how to correctly map the specific use cases to a good UX design in the selected XR platform.
3.2. Personalized therapy
Personalized medicine has been identified as key in “achieving optimal individual health-care decisions”4. Artificial Intelligence has allowed us to apply personalized medicine to several fields within the health domain, such as image diagnostics or genomics (Schork, 2019). It is, therefore, time to boost personalized therapy in mental health applications.
From a psychological perspective, each mental health condition has a different kind of treatment and approach. Hence, technological solutions aimed toward a specific condition cannot usually be generalized to others. Moreover, patients diagnosed with the same disorder might present different symptoms, triggers, and experiences that can not be solved with a non-adaptive and rigid technological activity. Therapists and patients are likely to perceive those generic tech solutions as poor or inadequate for their interest if they fail to adapt to the vastly assorted cases they deal with on an everyday basis.
Technological solutions aimed at supporting professionals and patients with mental conditions should provide a certain degree of customization. This process needs to be also participatory involving all stakeholders: technology designers, researchers, and developers should collaborate closely with mental health professionals and end users in order to design and develop adequate and flexible technological solutions (Muller, 2002). Additionally, these customization features have to be easy to understand and learn so that they do not interfere with clinicians' regular practice or cause rejection in patients. Regarding XR setups, a significant challenge will be the development of such adaptive and customizable experiences that could adapt their interfaces and digital 3D content to the patient and context.
3.3. Stigma and democratization of the technology
There is still a significant stigma around people who go to therapy, and mental health disorders are yet misunderstood and poorly considered by society. People are less likely to report mental health issues compared to other health conditions (Bharadwaj et al., 2017). Mental health stigma might even be accentuated in specific communities and vulnerable groups (Egede et al., 2020). Social and self-stigma could lead to many consequences (Sickel et al., 2014), being under-diagnose as one of them. Technology could help a great deal in breaking these stereotypes: XR experiences can help people feel what other beings are feeling, for example, when they suffer from psychosis or a panic attack (Formosa et al., 2018). This exposure could help increase compassion toward individuals suffering from those conditions, creating more inclusive societies.
Another factor that could help break the stigma around mental health is democratizing access to healthcare resources. The WHO (2022) has emphasized the need for accessible community-based mental health services, stressed that the traditional business model for mental health is not enough, and steemed urgent the need for a wide-ranging transformation toward mental health.
The recent COVID pandemic has shifted the paradigm from traditional face-to-face therapy and popularized the possibility of online therapy in such a way that online therapy is still demanded in our post-pandemic society (Weinberg, 2020). These online opportunities could also help to lower the barrier of access to treatment for certain, especially vulnerable, demographics such as elders, people with limited mobility, or people living in rural areas far from access to specialized therapy. Extended reality technologies can also be regarded as online and remote therapies, with the added value that the patient can experience them both online at the same time with the therapist or offline to practice at their own pace. In both cases, therapists will need additional tools to manage the interventions and keep track of the patients' evolution.
Overall, digital and technology-driven interventions like those based on XR would help reduce the consequences of mental health stigma, reduce the barriers, and democratize access to mental health therapy.
4. Future trends and opportunities
This section will review how the aforementioned challenges can be addressed in XR scenarios by means of different technological opportunities. Figure 1 shows the relationship between the different challenges and opportunities presented.
4.1. Serious games for mental health
Over the last decade, serious games are increasingly gaining popularity as an alternative way of tackling different challenges on a wide range of topics. Even when there is no unique and standard definition of the serious games term, it exists some agreement between researchers and practitioners about their core conceptions: Serious games are games designed to have a main intended use apart from entertainment.
In the mental health domain, serious games have a significant positive impact on the effectiveness of certain therapies, as they are able to harness the appealing aesthetics, engaging interactions, and instantaneous feedback of video games for the benefit of individuals (Kato, 2010; Wattanasoontorn et al., 2014). Due to their ability to add interest to activities that may otherwise be boring or repetitive, serious games have the potential to overcome the engagement issues that conventional e-Health apps face.
As new research on the topic emerges, it is necessary to determine how much any link between using video games (serious games or commercial off-the-shelf) and training-related outcomes is mediated by adherence and whether this adherence is long-lasting (Primack et al., 2012).
Focusing on specific mental health therapies, there is also strong evidence about the positive effects of serious games on cognitive-behavioral treatments (Fleming et al., 2017). Moreover, even the United States Food and Drug Administration (FDA), has started to certify software as a drug and has implemented a Software Precertification Pilot Program version 1.0 Working Model (FDA, 2019) in order to clarify the risks/benefits balance of a therapeutic virtual experience. Serious games that have been approved by the FDA and other certification entities aim to tackle mental health conditions such as nightmare disorder or post-traumatic stress disorder5, insomnia6, and substance use disorder7. Additionally, FDA provides some mechanisms, like the De Novo request, to evaluate how appropriate an XR device is for its clinical utilization, attending to its potential hazards when used by patients (FDA, 2022).
4.2. Biofeedback and digital phenotyping
A common form of intervention in mental health is through the use of wearables and sensors that allow measuring a patient's physiological parameters, with recent trends on using heart-rate, respiration, and electrodermal activity (Alneyadi et al., 2021). Capturing biofeedback offers quantitative and objective information about the patient's state to the therapist. It also makes it possible to identify relevant patterns in the captured data for the prediction or diagnosis of pathologies such as depression (Tazawa et al., 2020) or ASD (Torrado et al., 2017). This moment-by-moment quantification of the user's data captured from digital devices is known as digital phenotype (Sequeira et al., 2019). It can be gathered passively from smartphones, wearables, or sensors, but it can also be collected within game-like experiences (Mandryk and Birk, 2019).
Combined with XR technology and XR serious games, biofeedback and digital phenotyping offer a mechanism to increase user engagement: an XR playful experience could gather data from different wearable sensors and IoT devices while the user is playing, identifying meaningful information that could be used to inform therapists. In addition, the data gathered from the patient could help adapt the interaction in real-time, personalizing the interventions, and keeping the user motivated. Adaptive interfaces could be envisioned, in which the experience could be tailored to the patient's current mental state. For example, the XR experience might offer different options depending on whether the user is feeling more or less stressed, happy, or anxious.
4.3. Multimodal interaction and adaptive interfaces
Extended reality experiences are mostly visual, but designers and developers cannot forget about other senses and stimuli that will surely help to increase users' engagement. One of the recent trends in XR is exploring tangible and haptic feedback. There is evidence about how tangible pervasive tools can facilitate monitoring and sensing affect within mental health care (Guribye et al., 2016). Tangible interfaces offer a bridge between real and digital objects. In the context of XR, tangible interfaces have the potential to improve natural support for collaborative activities, physical interactions, and external representations and, also provide users with the feeling of directness.
In addition, multimodal interfaces for XR are still under-explored. Researching other modalities of interaction as well as multimodal XR experiences, could provide interesting opportunities to cater to different patients' needs and scenarios. Capitalizing on new advances in designing novel interfaces for XR such as olfactory (Wang et al., 2020), gustatory (Anbarasan et al., 2022), and haptic feedback could also provide options for building adaptive interfaces that provide a customized user experience in therapeutic applications. An ambitious but very promising opportunity lies in the development of XR serious games for mental health that allow for multimodal interactions while capturing the patients' biofeedback. These scenarios will allow the system to adapt intelligently to the patients' state and progress while offering suitable modes of interaction depending on the XR context and the patient's capabilities.
4.4. Mixed reality and metaverse
The increasing spread of XR technologies suggests a future in which MR becomes a ubiquitous component. Improvements in MR enabling technology have the opportunity to make it more accessible to the general public and to enable practitioners to build more immersive and multimodal experiences. Mixed reality technologies have the chance to enhance the way traditional therapies are made and facilitate easier access to such therapies, especially in a remote setting.
In the mental health field, therapists will be able to conduct more realistic MR therapeutic experiences that could be applied to more diverse demographics overcoming barriers present in other XR technologies such as VR: motion sickness (Chun et al., 2022), stress, or strain. Mixed reality also allows to create experiences in the real world instead of simulated environments, which could reduce the gap between exposure and in-vivo therapy.
Technological advancements will also bring the opportunity for creating collaborative experiences, both co-present and remote. Such experiences could give a chance to therapists and users to create interventions taking into consideration social aspects, lower the barrier for patients to practice social interventions in a controlled environment, and enable social therapeutic experiences such as group therapy.
The idea of metaverse represents a diffuse and variable concept that serves to identify a digital, persistent, multi-user world with high levels of interaction. This metaverse is shown as a scenario with great potential to host, in the not too distant future, collective environments for mental health work, where patients and therapists coexist and the interventions extend, physically and temporarily, beyond the consultation room.
5. Conclusion and future work
Universal and effective psychological treatment is a major challenge for clinical practitioners, governments, and society, even more so today, where mental health and well-being have become a priority for everyone. The use of XR experiences in the mental health domain represents an unstoppable trend supported by high-quality, affordable immersive technologies.
From early standard VR environments for exposure therapies to current studies on customized MR-based social treatments, the paradigm of technology mediated interventions has evolved to more customized, comfortable, democratized, and accessible approaches.
Future work opportunities on the field include transforming XR experiences into serious games by including game mechanics, interactive storytelling, and compelling aesthetics to increase patient engagement and the efficacy of treatments. Additionally, including biofeedback, multimodal, and adaptive experiences into XR serious games will help to create compelling and effective digital therapies. In this regard, MR experiences with such capabilities have the potential to be the medium to deliver engaging, personalized, and democratic mental health assistance in a global way. In order to support this approach, global efforts must be made to produce comfortable and affordable MR devices and creative and significant interactive therapeutic experiences. A whole new research topic has been unveiled where pervasive, multiuser, and multimodal XR environments have to be developed for supportive, accessible, and democratic mental health assistance. This new topic will require also new research methodologies such as remote XR experimentation (Ratcliffe et al., 2021).
Data availability statement
The original contributions presented in the study are included in the article, further inquiries can be directed to the corresponding author/s.
Author contributions
All authors made substantial contributions to the conception and development of the work.
Funding
This work has been funded by the Valencian Institute for the Enterprise Competitiveness (IVACE/FEDER) through the project ARCADIA (IMDEEA/2022/22).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Footnotes
1. ^https://www.mentalhealth.org.uk/explore-mental-health/statistics/uk-worldwide-statistics
2. ^https://www3.paho.org/hq/index.php?option=com_content&view=article&id=15481:mental-health-problems-are-the-leading-cause-of-disability-worldwide-say-experts-at-paho-directing-council-side-event&Itemid=72565&lang=en
3. ^https://www.who.int/news/item/02-03-2022-covid-19-pandemic-triggers-25-increase-in-prevalence-of-anxiety-and-depression-worldwide
4. ^http://www.engineeringchallenges.org/challenges/medicines.aspx
References
Alcañiz, M., Chicchi-Giglioli, I. A., Carrasco-Ribelles, L. A., Marín-Morales, J., Minissi, M. E., Teruel-García, G., et al. (2022). Eye gaze as a biomarker in the recognition of autism spectrum disorder using virtual reality and machine learning: a proof of concept for diagnosis. Autism Res. 15, 131–145. doi: 10.1002/aur.2636
Alneyadi, M., Drissi, N., Almeqbaali, M., and Ouhbi, S. (2021). Biofeedback-based connected mental health interventions for anxiety: systematic literature review. JMIR Mhealth Uhealth 9, e26038.doi: 10.2196/26038
Anbarasan, R., Gomez Carmona, D., and Mahendran, R. (2022). Human taste-perception: brain computer interface (BCI) and its application as an engineering tool for taste-driven sensory studies. Food Eng. Rev. 14, 408–434. doi: 10.1007/s12393-022-09308-0
Baghaei, N., Hach, S., Khaliq, I., Stemmet, L., Krishnan, J., Naslund, J., et al. (2019). “Increasing self-compassion in young people through virtual reality,” in 2019 IEEE International Symposium on Mixed and Augmented Reality Adjunct (ISMAR-Adjunct) (Beijing), 404–407. doi: 10.1109/ISMAR-Adjunct.2019.00042
Bălan, O., Cristea, T., Moise, G., Petrescu, L., Ivacu, S., Moldoveanu, A., et al. (2020). “eTher – an assistive virtual agent for acrophobia therapy in virtual reality,” in HCI International 2020 – Late Breaking Papers: Virtual and Augmented Reality, eds C. Stephanidis, J. Y. C. Chen, and G. Fragomeni (Cham: Springer International Publishing), 12–25.
Bera, L., Souchon, M., Ladsous, A., Colin, V., and Lopez-Castroman, J. (2022). Emotional and behavioral impact of the covid-19 epidemic in adolescents. Curr. Psychiatry Rep. 24, 37–46. doi: 10.1007/s11920-022-01313-8
Bharadwaj, P., Pai, M. M., and Suziedelyte, A. (2017). Mental health stigma. Econ. Lett. 159, 57–60. doi: 10.1016/j.econlet.2017.06.028
Bisso, E., Signorelli, M. S., Milazzo, M., Maglia, M., Polosa, R., Aguglia, E., et al. (2020). Immersive virtual reality applications in schizophrenia spectrum therapy: a systematic review. Int. J. Environ. Res. Public Health. 17, 6111. doi: 10.3390/ijerph17176111
Botella, C., Bretón-López, J., Quero, S., Baños, R., and García-Palacios, A. (2010). Treating cockroach phobia with augmented reality. Behav. Ther. 41, 401–413. doi: 10.1016/j.beth.2009.07.002
Cai, S., Zhu, G., Wu, Y. T., Liu, E., and Hu, X. (2018). A case study of gesture-based games in enhancing the fine motor skills and recognition of children with autism. Interact. Learn. Environ. 26, 1039–1052. doi: 10.1080/10494820.2018.1437048
Cebolla, A., Herrero, R., Ventura, S., Miragall, M., Bellosta-Batalla, M., Llorens, R., et al. (2019). Putting oneself in the body of others: a pilot study on the efficacy of an embodied virtual reality system to generate self-compassion. Front. Psychol. 10, 1521. doi: 10.3389/fpsyg.2019.01521
Choi, M.-T., Yeom, J., Shin, Y., and Park, I. (2019). Robot-assisted adhd screening in diagnostic process. J. Intell. Robot. Syst. 95, 351–363. doi: 10.1007/s10846-018-0890-9
Chuah, S. (2018). Why and who will adopt extended reality technology? Literature review, synthesis, and future research agenda. SSRN. 1–56. doi: 10.2139/ssrn.3300469
Chun, J. Y., Kim, H.-J., Hur, J.-W., Jung, D., Lee, H.-J., Pack, S. P., et al. (2022). Prediction of specific anxiety symptoms and virtual reality sickness using in situ autonomic physiological signals during virtual reality treatment in patients with social anxiety disorder: mixed methods study. JMIR Serious Games 10, e38284. doi: 10.2196/38284
Coleridge, S. T. (1984). Biographia Literaria, or, Biographical Sketches of my Literary Life and Opinions, Vol. 7. Princeton, NJ: Princeton University Press.
Colombo, D., Fernández-Álvarez, J., Garcia Palacios, A., Cipresso, P., Botella, C., and Riva, G. (2019). New technologies for the understanding, assessment, and intervention of emotion regulation. Front. Psychol. 10, 1261. doi: 10.3389/fpsyg.2019.01261
Davis, N. O., Bower, J., and Kollins, S. H. (2018). Proof-of-concept study of an at-home, engaging, digital intervention for pediatric ADHD. PLoS ONE 13, e0189749. doi: 10.1371/journal.pone.0189749
D'Cunha, N., Nguyen, D., Naumovski, N., McKune, A., Kellett, J., Georgousopoulou, E., et al. (2019). A mini-review of virtual reality-based interventions to promote well-being for people living with dementia and mild cognitive impairment. Gerontology 65, 430–440. doi: 10.1159/000500040
Donker, T., Cornelisz, I., van Klaveren, C., van Straten, A., Carlbring, P., Cuijpers, P., et al. (2019). Effectiveness of self-guided app-based virtual reality cognitive behavior therapy for acrophobia: a randomized clinical trial. JAMA Psychiatry. 76, 682–690. doi: 10.1001/jamapsychiatry.2019.0219
Donkin, L., Christensen, H., Naismith, S. L., Neal, B., Hickie, I. B., Glozier, N., et al. (2011). A systematic review of the impact of adherence on the effectiveness of e-therapies. J. Med. Internet Res. 13, e1772. doi: 10.2196/jmir.1772
Donkin, L., and Glozier, N. (2012). Motivators and motivations to persist with online psychological interventions: a qualitative study of treatment completers. J. Med. Internet Res. 14, e91. doi: 10.2196/jmir.2100
Egede, L. E., Ruggiero, K. J., and Frueh, B. C. (2020). Ensuring mental health access for vulnerable populations in covid era. J. Psychiatr Res. 129, 147–148. doi: 10.1016/j.jpsychires.2020.07.011
Eraslan, S., Yaneva, V., Yesilada, Y., and Harper, S. (2019). Web users with autism: eye tracking evidence for differences. Behav. Inform. Technol. 38, 678–700. doi: 10.1080/0144929X.2018.1551933
Falconer, C. J., Rovira, A., King, J. A., Gilbert, P., Antley, A., Fearon, P., et al. (2016). Embodying self-compassion within virtual reality and its effects on patients with depression. BJPsych. Open 2, 74–80. doi: 10.1192/bjpo.bp.115.002147
FDA (2019). Software Precertification Program: Working Model Version 1.0 January 2019. Technical Report. FDA.
FDA. (2022). “Augmented reality and virtual reality medical devices,” in Executive Summary for the Patient Engagement Advisory Committee Meeting (FDA).
Fleming, T. M., Bavin, L., Stasiak, K., Hermansson-Webb, E., Merry, S. N., Cheek, C., et al. (2017). Serious games and gamification for mental health: current status and promising directions. Front. Psychiatry 7, 215. doi: 10.3389/fpsyt.2016.00215
Fleming, T. M., Gillham, B., Bavin, L. M., Stasiak, K., Lewycka, S., Moore, J., et al. (2019). SPARX-R computerized therapy among adolescents in youth offenders' program: Step-wise cohort study. Internet Intervent. 18, 100287. doi: 10.1016/j.invent.2019.100287
Formosa, N. J., Morrison, B. W., Hill, G., and Stone, D. (2018). Testing the efficacy of a virtual reality-based simulation in enhancing users' knowledge, attitudes, and empathy relating to psychosis. Austral. J. Psychol. 70, 57–65. doi: 10.1111/ajpy.12167
Francova, A., Darmova, B., Stopkova, P., Kosova, J., and Fajnerova, I. (2019). “Virtual reality exposure therapy in patients with obsessive-compulsive disorder,” in 2019 International Conference on Virtual Rehabilitation (ICVR) (Tel Aviv). doi: 10.1109/ICVR46560.2019.8994404
Freeman, D., Lambe, S., Kabir, T., Petit, A., Rosebrock, L., Yu, L., et al. (2022). Automated virtual reality therapy to treat agoraphobic avoidance and distress in patients with psychosis (gameChange): a multicentre, parallel-group, single-blind, randomised, controlled trial in England with mediation and moderation analyses. Lancet Psychiatry 9, 375–388. doi: 10.1016/S2215-0366(22)00060-8
Garcia-Zapirain, B., de la Torre Díez, I., and López-Coronado, M. (2017). Dual system for enhancing cognitive abilities of children with ADHD using leap motion and eye-tracking technologies. J. Med. Syst. 41, 111. doi: 10.1007/s10916-017-0757-9
Giraldy, D. J., and Novaldo, W. (2022). A systematic literature review: acrophobia treatment with virtual reality. Eng. Math. Comput. Sci. J. 4, 33–38. doi: 10.21512/emacsjournal.v4i1.8077
Goharinejad, S., Goharinejad, S., Hajesmaeel-Gohari, S., and Bahaadinbeigy, K. (2022). The usefulness of virtual, augmented, and mixed reality technologies in the diagnosis and treatment of attention deficit hyperactivity disorder in children: an overview of relevant studies. BMC Psychiatry 22, 4. doi: 10.1186/s12888-021-03632-1
Guribye, F., Gjøsæter, T., and Bjartli, C. (2016). “Designing for tangible affective interaction,” in Proceedings of the 9th Nordic Conference on Human-Computer Interaction, NordiCHI '16 (New York, NY: Association for Computing Machinery). doi: 10.1145/2971485.2971547
Habets, J., Heijmans, M., Herff, C., Simons, C., Leentjens, A. F., Temel, Y., et al. (2020). Mobile health daily life monitoring for Parkinson disease: development and validation of ecological momentary assessments. JMIR mHealth uHealth 8, e15628. doi: 10.2196/15628
Hafstad, G. S., Sætren, S. S., Wentzel-Larsen, T., and Augusti, E.-M. (2020). Longitudinal change in adolescent mental health during the covid-19 outbreak – a prospective population-based study of teenagers in Norway. SSRN. doi: 10.2139/ssrn.3727297
Jazouli, M., Majda, A., Merad, D., Aalouane, R., and Zarghili, A. (2019). Automatic detection of stereotyped movements in autistic children using the Kinect sensor. Int. J. Biomed. Eng. Technol. 29, 201–220. doi: 10.1504/IJBET.2019.097621
Kato, P. M. (2010). Video games in health care: closing the gap. Rev. Gen. Psychol. 14, 113–121. doi: 10.1037/a0019441
Kurscheidt, M., Ostapchuck, V., Sottek, F., Rauh, S. F., and Meixner, G. (2019). “Augmented reality exposure therapy with tactile feedback for small animal phobia : hardware concept and user study design,” in 2019 IEEE International Conference on Healthcare Informatics (ICHI) (Xi'an), 1–7. doi: 10.1109/ICHI.2019.8904800
Laforest, M., Bouchard, S., Crétu, A. M., and Mesly, O. (2016). Inducing an anxiety response using a contaminated virtual environment: validation of a therapeutic tool for obsessive-compulsive disorder. Front. ICT 3, 18. doi: 10.3389/fict.2016.00018
Lee, L. N., Kim, M. J., and Hwang, W. J. (2019). Potential of augmented reality and virtual reality technologies to promote wellbeing in older adults. Appl. Sci. 9, 3556. doi: 10.3390/app9173556
Loomis, J. M., Blascovich, J. J., and Beall, A. C. (1999). Immersive virtual environment technology as a basic research tool in psychology. Behav. Res. Methods Instrum. Comput. 31, 557–564. doi: 10.3758/BF03200735
Lundin, J., Lundstrm, A., Gulliksen, J., Blendulf, J., Ejeby, K., Nyman, H., et al. (2022). Using 360-degree videos for virtual reality exposure in CBT for panic disorder with agoraphobia: a feasibility study. Behav. Cognit. Psychother. 50, 158–170. doi: 10.1017/S1352465821000473
Macey, A.-L., Macey, J., and Hamari, J. (2022). “Virtual reality in emotion regulation: a scoping review,” 6th International GamiFIN Conference (Tampere).
Mandryk, R. L., and Birk, M. V. (2019). The potential of game-based digital biomarkers for modeling mental health. JMIR. Ment. Health 6, e13485. doi: 10.2196/13485
Mann, S., Furness, T., Yuan, Y., Iorio, J., and Wang, Z. (2018). All reality: virtual, augmented, mixed (X), mediated (X, Y), and multimediated reality. CoRR. 1–14. doi: 10.48550/arXiv.1804.08386
Marto, A., and Almeida, H. A. (2019). “Using augmented reality in patients with autism: a systematic review,” in ECCOMAS Thematic Conference on Computational Vision and Medical Image Processing, VipIMAGE 2019. Lecture Notes in Computational Vision and Biomechanics, Vol. 34, eds J. Tavares and R. Natal Jorge (Cham: Springer), 454–463. doi: 10.1007/978-3-030-32040-9_46
Mesa-Gresa, P., Gil-Gómez, H., Lozano-Quilis, J. A., and Gil-Gómez, J. A. (2018). Effectiveness of virtual reality for children and adolescents with autism spectrum disorder: an evidence-based systematic review. Sensors (Basel) 18, 2486. doi: 10.3390/s18082486
Miegel, F., Bücker, L., Kühn, S., Mostajeran, F., Moritz, S., Baumeister, A., et al. (2022). Exposure and response prevention in virtual reality for patients with contamination-related obsessive compulsive disorder: a case series. Psychiatr. Q. 93, 861–882. doi: 10.1007/s11126-022-09992-5
Montaner-Marco, J., Jaen, J., and Pons, P. (2021). Designing a Mobile AR Application for Improving Pediatric Psychological Wellbeing. New York, NY: Association for Computing Machinery.
Moyle, W., Cooke, M., Beattie, E., Jones, C., Klein, B., Cook, G., et al. (2013). Exploring the effect of companion robots on emotional expression in older adults with dementia: a pilot randomized controlled trial. J. Gerontol. Nurs. 39, 46–53. doi: 10.3928/00989134-20130313-03
Muller, M. J. (2002). “Participatory design: the third space in HCI,” in The Human-Computer Interaction Handbook, Vol. 4235, ed M. J. Muller (Boca Raton, Fl: CRC Press), 1051–1068.
Nickbakht, M., Meyer, C., Scarinci, N., and Beswick, R. (2020). Exploring factors influencing the use of an ehealth intervention for families of children with hearing loss: an application of the COM-B model. Disabil. Health J. 13, 100921. doi: 10.1016/j.dhjo.2020.100921
Pimentel, D., and Kalyanaraman, S. (2020). Customizing your demons: anxiety reduction via anthropomorphizing and destroying an “anxiety avatar”. Front. Psychol. 11, 566682. doi: 10.3389/fpsyg.2020.566682
Pizarro-Ruiz, J. P., and Ordóñez-Camblor, N. (2021). Effects of covid-19 confinement on the mental health of children and adolescents in Spain. Sci. Rep. 11, 11713. doi: 10.1038/s41598-021-91299-9
Primack, B. A., Carroll, M. V., McNamara, M., Klem, M. L., King, B., Rich, M., et al. (2012). Role of video games in improving health-related outcomes: a systematic review. Am. J. Prev. Med. 42, 630–638. doi: 10.1016/j.amepre.2012.02.023
Ratcliffe, J., Soave, F., Bryan-Kinns, N., Tokarchuk, L., and Farkhatdinov, I. (2021). “Extended reality (XR) remote research: a survey of drawbacks and opportunities,” in Proceedings of the 2021 CHI Conference on Human Factors in Computing Systems (Yokohama), 1–13.
Rickard, N., Arjmand, H.-A., Bakker, D., and Seabrook, E. (2016). Development of a mobile phone app to support self-monitoring of emotional well-being: a mental health digital innovation. JMIR Ment. health 3, e49. doi: 10.2196/mental.6202
Riva, G., Calvo, R. A., and Lisetti, C. (2015). “Cyberpsychology and affective computing,” in The Oxford Handbook of Affective Computing, eds R. Calvo S. D'Mello, J. Gratch, and A. Kappas (Oxford: Oxford University Press), 547–558.
Schoneveld, E. A., Malmberg, M., Lichtwarck-Aschoff, A., Verheijen, G. P., Engels, R. C., and Granic, I. (2016). A neurofeedback video game (mindlight) to prevent anxiety in children: a randomized controlled trial. Comput. Hum. Behav. 63, 321–333. doi: 10.1016/j.chb.2016.05.005
Schork, N. J. (2019). Artificial intelligence and personalized medicine. Cancer Treat Res. 178, 265–283. doi: 10.1007/978-3-030-16391-411
Sequeira, L., Battaglia, M., Perrotta, S., Merikangas, K., and Strauss, J. (2019). Digital phenotyping with mobile and wearable devices: advanced symptom measurement in child and adolescent depression. J. Amer. Acad. Child Adoles. Psychiatry 58, 841–845. doi: 10.1016/j.jaac.2019.04.011
Sickel, A. E., Seacat, J. D., and Nabors, N. A. (2014). Mental health stigma update: a review of consequences. Adv. Ment. Health 12, 202–215. doi: 10.1080/18374905.2014.11081898
Slater, M. (2018). Immersion and the illusion of presence in virtual reality. Br. J. Psychol. 109, 431–433. doi: 10.1111/bjop.12305
Slater, M., Usoh, M., and Steed, A. (1994). Depth of presence in virtual environments. Pres. Teleoperat. Virt. Environ. 3, 130–144. doi: 10.1162/pres.1994.3.2.130
Suso-Ribera, C., Fernández-Álvarez, J., García-Palacios, A., Hoffman, H. G., Bretón-López, J., Baños, R. M., et al. (2019). Virtual reality, augmented reality, and in vivo exposure therapy: a preliminary comparison of treatment efficacy in small animal phobia. Cyberpsychol. Behav. Soc. Netw. 22, 31–38. doi: 10.1089/cyber.2017.0672
Tazawa, Y., Liang, K.-C., Yoshimura, M., Kitazawa, M., Kaise, Y., Takamiya, A., et al. (2020). Evaluating depression with multimodal wristband-type wearable device: screening and assessing patient severity utilizing machine-learning. Heliyon 6, e03274. doi: 10.1016/j.heliyon.2020.e03274
Thai, E., and Nathan-Roberts, D. (2018). Social skill focuses of virtual reality systems for individuals diagnosed with autism spectrum disorder; a systematic review. Proc. Hum. Factors Ergon. Soc. Annu. Meet. 62, 1469–1473. doi: 10.1177/1541931218621333
Torrado, J. C., Gomez, J., and Montoro, G. (2017). Emotional self-regulation of individuals with autism spectrum disorders: smartwatches for monitoring and interaction. Sensors 17, 1359. doi: 10.3390/s17061359
Tuena, C., Pedroli, E., Trimarchi, P. D., Gallucci, A., Chiappini, M., Goulene, K., et al. (2020). Usability issues of clinical and research applications of virtual reality in older people: a systematic review. Front. Hum. Neurosci. 14, 93. doi: 10.3389/fnhum.2020.00093
Vahabzadeh, A., Keshav, N. U., Salisbury, J. P., and Sahin, N. T. (2018). Improvement of attention-deficit/hyperactivity disorder symptoms in school-aged children, adolescents, and young adults with autism via a digital smartglasses-based socioemotional coaching aid: short-term, uncontrolled pilot study. JMIR Ment. Health. 20, e25. doi: 10.2196/mental.9631
van Loenen, I., Scholten, W., Muntingh, A., Smit, J., and Batelaan, N. (2022). The effectiveness of virtual reality exposure–based cognitive behavioral therapy for severe anxiety disorders, obsessive-compulsive disorder, and posttraumatic stress disorder: meta-analysis. J. Med. Internet Res. 24, e26736. doi: 10.2196/26736
Ventura, S., Baños, R. M., Botella, C., and Mohamudally, N. (2018). “Virtual and augmented reality: New frontiers for clinical psychology,” in State of the Art Virtual Reality and Augmented Reality Knowhow, Vol. 10. ed N. Mohamudally (London: IntechOpen). doi: 10.5772/intechopen.74344
Wang, R., Wang, W., DaSilva, A., Huckins, J. F., Kelley, W. M., Heatherton, T. F., et al. (2018). Tracking depression dynamics in college students using mobile phone and wearable sensing. Proc. ACM Interact. Mob. Wear. Ubiquit. Technol. 2, 1–26. doi: 10.1145/3191775
Wang, Y., Amores, J., and Maes, P. (2020). “On-face olfactory interfaces,” in Proceedings of the 2020 CHI Conference on Human Factors in Computing Systems (Honolulu, HI), 1–9. doi: 10.1145/3313831.3376737
Wattanasoontorn, V., Hernández, R. J. G., and Sbert, M. (2014). “Serious games for e-health care,” in Simulations, Serious Games and Their Applications, eds Y. Cai and S. Goei (Singapore: Springer), 127–146.
Wechsler, T. F., Mühlberger, A., and Kümpers, F. (2019). Inferiority or even superiority of virtual reality exposure therapy in phobias? - A systematic review and quantitative meta-analysis on randomized controlled trials specifically comparing the efficacy of virtual reality exposure to gold standard in vivo exposure in Agoraphobia, Specific Phobia and Social Phobia. Front. Psychol. 10, 1758. doi: 10.3389/fpsyg.2019.01758
Weinberg, H. (2020). Online group psychotherapy: challenges and possibilities during covid-19 a practice review. Group Dyn. Theory Res. Pract. 24, 201–211. doi: 10.1037/gdn0000140
WHO, Mruckmayer, M., and Philips, W. (2021). Children and Mental Health : Preventive Approaches to Anxiety and Depression : European Platform for Investing in Children. European Commission and Directorate-General for Employment, Social Affairs and Inclusion. doi: 10.2767/730847
Yang, Y., Boulton, E., and Todd, C. (2022). Measurement of adherence to mHealth physical activity interventions and exploration of the factors that affect the adherence: scoping review and proposed framework. J. Med. Internet Res. 24, e30817. doi: 10.2196/30817
Yun, S.-S., Choi, J., Park, S.-K., Bong, G.-Y., and Yoo, H. (2017). Social skills training for children with autism spectrum disorder using a robotic behavioral intervention system. Autism Res. 10, 1306–1323. doi: 10.1002/aur.1778
Zhang, C., Ye, M., Fu, Y., Yang, M., Luo, F., Yuan, J., et al. (2020). The psychological impact of the covid-19 pandemic on teenagers in China. J. Adolesc. Health 67, 747–755. doi: 10.1016/j.jadohealth.2020.08.026
Zhao, N., Zhang, Z., Wang, Y., Wang, J., Li, B., Zhu, T., et al. (2019). See your mental state from your walk: recognizing anxiety and depression through Kinect-recorded gait data. PLoS ONE 14, e0216591. doi: 10.1371/journal.pone.0216591
Keywords: extended reality, mental health, serious games, multimodal interaction, biofeedback, mixed reality
Citation: Pons P, Navas-Medrano S and Soler-Dominguez JL (2022) Extended reality for mental health: Current trends and future challenges. Front. Comput. Sci. 4:1034307. doi: 10.3389/fcomp.2022.1034307
Received: 01 September 2022; Accepted: 24 October 2022;
Published: 18 November 2022.
Edited by:
Anton Nijholt, University of Twente, NetherlandsReviewed by:
Michele Scandola, University of Verona, ItalyMaryalice Jordan-Marsh, University of Southern California, United States
Antonio Giordano, Temple University, United States
Copyright © 2022 Pons, Navas-Medrano and Soler-Dominguez. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Patricia Pons, cHBvbnNAaXRpLmVz
 Patricia Pons
Patricia Pons Samuel Navas-Medrano
Samuel Navas-Medrano Jose L. Soler-Dominguez
Jose L. Soler-Dominguez