
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
MINI REVIEW article
Front. Comput. Sci. , 13 May 2021
Sec. Mobile and Ubiquitous Computing
Volume 3 - 2021 | https://doi.org/10.3389/fcomp.2021.661676
This article is part of the Research Topic 2021 Editor's Pick: Computer Science View all 11 articles
In this study, we review the role of wearable devices in tracking our daily locomotion. We discuss types of wearable devices that can be used, methods for gait analyses, and multiple healthcare-related applications aided by artificial intelligence. Impaired walking and locomotion are common resulting from injuries, degenerative pathologies, musculoskeletal disorders, and various neurological damages. Daily tracking and gait analysis are convenient and efficient approaches for monitoring human walking, where concreate and rich data can be obtained for examining our posture control mechanism during body movement and providing enhanced clinical pieces of evidence for diagnoses and treatments. Many sensors in wearable devices can help to record data of walking and running; spatiotemporal and kinematic variables can be further calculated in gait analysis. We report our previous works in gait analysis, discussing applications of wearable devices for detecting foot and ankle lesions, supporting surgeons in early diagnosis, and helping physicians with rehabilitation.
Walking is one of the most common activities we perform on daily basis. Normal human walking requires high a level of movement coordination between our extremities and the trunk. Constantly monitoring our walking pattern is a way to examine our health because the central nervous system is involved intensively to control the limb movements and the function of posture control while our body is moving. We believe wearable devices can play an important role in daily surveillance on our walking.
Impaired walking and locomotion are commonly seen worldwide resulting from injuries, degenerative pathologies, musculoskeletal disorders, and neurological damages. In traditional practice, physicians make diagnoses of these injuries base on physical and medical examinations. Complete gait analysis can only be performed in some tertiary hospitals on a small number of patients. Many scientists argued that gait analysis should be applied to all patients with degenerative diseases and those in need of long-term rehabilitation.
Gait analysis is systematic research involving sensor technology, anthropometry, and artificial intelligence. Wearable sensors and devices are widely applied to intelligent healthcare as the fast development in wireless communication, network technology, and micro-electronic technique. Unlike laboratory-based motion trackers, wearable devices are plausible for gait analysis. Technologies such as smartphones, sensors, and sensing fabric et al., are small, low-cost, and available for monitoring individuals’ activities.
Nowadays, wearable devices are increasingly used in biomechanical studies and sports medicine. As the development of the sensor technology, gait analysis is gradually employed in healthcare management including daily health monitoring, clinical diagnosis and rehabilitation assessment in surgery, elder’s fall risk detection et al. Several studies reported that gait analysis facilitated the whole process management of individuals and the decision-making of physicians in diagnosis and treatment.
The main purpose of this study is to review wearable devices for motion-tracking, gait analysis methods, and multiple healthcare-related applications in intelligent healthcare. To achieve the goal, we introduce common wearable motion-tracking devices including smartphones, wearable sensors, and sensing fabric; report our previous works in spatiotemporal gait analysis; discuss the application of gait analysis in daily health monitoring, sickness prevention, early diagnosis, and rehabilitation.
Wearable devices, such as smartphones, wearable sensors, and sensing fabrics, are widely applied to gait monitoring. The gait measures for different wearable devices are crucial for their application. We showed the pros and cons of different types of wearable devices (Table 1).
Each smartphone has various built-in sensors, such as GPS sensors, accelerometers, and gyroscopes. Therefore, variables for describing gaits, such as walking distance, frequency, and speed, etc. can be recorded by these sensors. We understand that the sensors can be secondarily developed by the application programming interfaces. Often the question for us is how to extract data from these sensors and how to develop a trusted methodology for reading these data and monitoring the abnormality in gait.
Yodpijit et al. used a smartphone as a wireless accelerometer to extract the gait parameters (stride time, stance time, swing time, and cadence). This study created a smartphone application for abnormal gait detection (Yodpijit et al., 2017). Reginya et al. applied a smartphone with accelerometers and gyroscopes to detect individuals with Parkinson’s disease (PD). They analyzed the amplitude and spectrum parameters from acceleration signal and rotation speed during a conventional neurologic walking test to find the difference between individuals with and without PD (Reginya et al., 2019). Kwon et al. proposed unsupervised learning algorithms using a smartphone to distinguish patient activities in the room. These approaches were based on clustering algorithms recognizing human activity, even when the number of activities was unknown (Kwon et al., 2014). Ahmed et al. recorded gait samples from 63 different subjects to predict the body mass index and age associated with high cholesterol, diabetes, cancer, and heart attack. Fourteen statistical features were extracted from each segment of the time-series including Jitter, mean crossing rate, autocorrelation mean/SD, autocovariance mean/SD, skewness, and kurtosis et al. (Ahmed et al., 2017).
In those people who do not carry a smartphone, wearable sensors, such as accelerometers, force sensors, extensometers, gyroscopic sensors, and goniometers et al., are available for collecting gait data. The sensors can be attached to the limbs and the trunk by wearing special apparel, socks, and shoes. Foot pressure is generally regarded as a gold standard for gait detection. The inertial measurement unit (IMU) is increasingly used for motion tracking in recent years.
Samberg et al. designed a GaitShoe wearable system to detect heel-strike and toe-off, as well as estimate foot orientation and position. The GaitShoe could discriminate between healthy gait pattern and PD from mean foot pitch extrema and stride time (Bamberg et al., 2008). Calliess et al. used a mobile gait analysis system with three IMUs to measure the outcomes after knee arthroplasty. Their main parameters included knee flexion profile, velocity, and knee stability (Calliess et al., 2014). Zexia He et al. designed a wearable sensing and training system using a motion sensor and six pressure-sensitive electric conductive rubber sensors. This system helped the elder with knee osteoarthritis to estimate their adduction moment for rehabilitation assessment (He et al., 2019). Schlachetzki et al. developed a wearable sensors-based gait analysis system with a high biomechanical resolution for gait impairment in PD. The measures were spatiotemporal parameters including stride length/time, stance time, inter-stride variation et al. The system is feasible for large-scale clinical studies and individual patient care (Schlachetzki et al., 2017).
The wearable sensors support current applications for daily motion tracking and also need to reduce the measurement errors keeping up with the “gold-standard” optical motion capture system. Dahl et al. validated an IMU system against an optical motion capture system during common sports movements. Compared to the optical motion capture system, the IMU system reported a larger angle in the horizontal and forward plane, smaller angle in the sagittal plane (Dahl et al., 2020). Leandro Donisi et al. indicated that the Opal and G-Walk systems (two wearable IMU systems for gait analysis) have good repeatability, but their agreement is not perfect (Donisi et al., 2019). Current wearable sensors are appropriate for daily health monitoring not requiring very accurate and precise measurements. In the future, wearable sensors will improve their reliability to support clinical diagnosis (Chen et al., 2016).
If a person refuses to wear sensors, we can use the Microsoft Kinect device to capture the movement of the limbs and create an alternative but reliable gait analysis approach to them (Taborri et al., 2016). Kinect was able to track skeletal joints in 3-dimensional (3D) space and calculate spatiotemporal gait variables and gait kinematics for the health assessment (Springer and Seligmann, 2016). The 3D-skeleton-based gait database established by the Kinect allows us to extract the static and dynamic features during walking. The feature fusion in 3D space improved the recognition rate on walking detection (Wang et al., 2016).
Sensing fabrics can also be used for measuring physical variables. Early sensing fabrics are electronic components attached to the surface of fabrics. With the development of smart fabrics, sensing fabrics are woven fabrics consisting of polyester and electrically conductive filaments now. The sensing fabrics are able to measure various activities of human bodies by capacitive, resistive, or bio-impedance mode and sense physical quantities (e.g., conductivity, temperature, and elongation et al.).
Preliminary works demonstrated that sensing fabric-based wearable devices can record gait abnormalities during daily walking for posture reconstruction (Lorussi et al., 2004; Amitrano et al., 2020). Shu et al. presented a fabric sensor-based in-shoe plantar pressure measure and analysis system to evaluate spatial and temporal plantar pressure distributions for gait analysis and balance control. The performance of fabric-based wearable devices was robust in both static and dynamic measures (Shu et al., 2010). Changming Yang et al. provided a gait analysis system using fabric sensors in pants and socks to monitor the movement of walking forward and backward or going upstairs and downstairs (Yang et al., 2015). Tirosh et al. developed a pair of socks from sensing fabrics to measure foot plantar pressure and gait temporal parameters (e.g., stride and stance duration) during long-term outdoor walking. Data collected from the socks were able to accurately predict gaits patterns that were performed by patients with diabetes, stroke, PD, and calculating the risk for falls (Tirosh et al., 2013).
Gait kinetics studies the forces and moments resulting in locomotion of lower extremities during the gait cycle including plantar pressure distribution, ground reaction force (GRF), joint torque, and muscle activity, et al. (Tahir et al., 2020). The magnitude and distribution of plantar pressure directly reflect the function and posture control in the lower extremity. Foot scanning and in-shoe plantar pressure systems measure how their feet are functioning from heel contact to toe-off. Using plantar pressure analysis, we can measure multi-plantar pressure profiles; monitor the improvements in balance, strength, and weight-bearing; identify asymmetries during the stance phase. Gait kinetics plays a major role in the prevention, identification, and treatment of gait impaired. Recently, GRF were used to recognize Parkinson’s patients (Ren et al., 2017), identify the gender of participants (Soubra et al., 2016), and distinguish the normal gait pattern in autism spectrum disorder (ASD) (Hasan et al., 2018) and diabetes (Du et al., 2015).
Gait kinematics helps clinicians to identify patients’ motion conditions and postulate the possible impaired neuromuscular control mechanism, which will facilitate early diagnosis and prompt treatment. Gait data collected by various sensors are the basis of gait kinematics. We need to build a trustable biomechanical model for gait analysis and require the application of artificial intelligence for data interpretation.
In recent years, several biomechanical models have been developed to measure foot and ankle motions. For example, the Oxford Foot Model (including the shank, hindfoot, forefoot, and hallux) has been used routinely in clinical practice to assess foot deformity and gait dysfunction, such as idiopathic clubfoot, foot arthritis, cerebral palsy, hemiplegia (Kostuj et al., 2018). The Milwaukee Foot Model, a four-segment model (tibia, hindfoot, forefoot, and hallux), has been applied to identify atypical segmental foot motion during ambulation and measure the intervention effectiveness after operations for the hallux valgus, hallux rigidus, posterior tibial tendon dysfunction, systemic rheumatoid arthritis and forefoot deformity (Canseco et al., 2012). The Istituti Ortopedici Rizzoli Foot model and three-dimensional (3D) foot model were developed to cover five-segment on the leg (shank, calcaneus, midfoot, metatarsals, and hallux) (Leardini et al., 2007). The Kinfoot model was a nine-segment model to cover the shank, hindfoot, two midfoot segments, two forefoot segments, two toe segments, and a hallux (MacWilliams et al., 2003).
In our recent study, we analyzed the motion of lower extremities in patients with lateral collateral ligament injuries of the ankle and synthesizing foot and ankle kinematic characteristics for adaptive injury detection (Liu et al., 2020). The Heidelberg Foot Measurement Model (HFMM) was used to examine foot and ankle kinematics in the entire gait cycle (Simon et al., 2006). The HFMM requires seventeen sensors to cover segments of the shank, the hindfoot, the midfoot, and the forefoot (both medial and lateral segments of the forefoot and hallux). The variables included tibiotalar flexion, forefoot/ankle abduction, medial arch angle, lateral arch angle, subtalar rotation, forefoot/ankle supination, MT I-V angle (Figure 1). These kinematic data enabled us quantitatively describe individuals’ behavior surrounding foot and ankle during walking and built up a foundation for us to run the deep learning-based algorithm to detect the nature of foot injuries. As shown in Figure 1, motion data recorded by these sensors were able to distinguish gait characteristics between normal and feet with lesions.
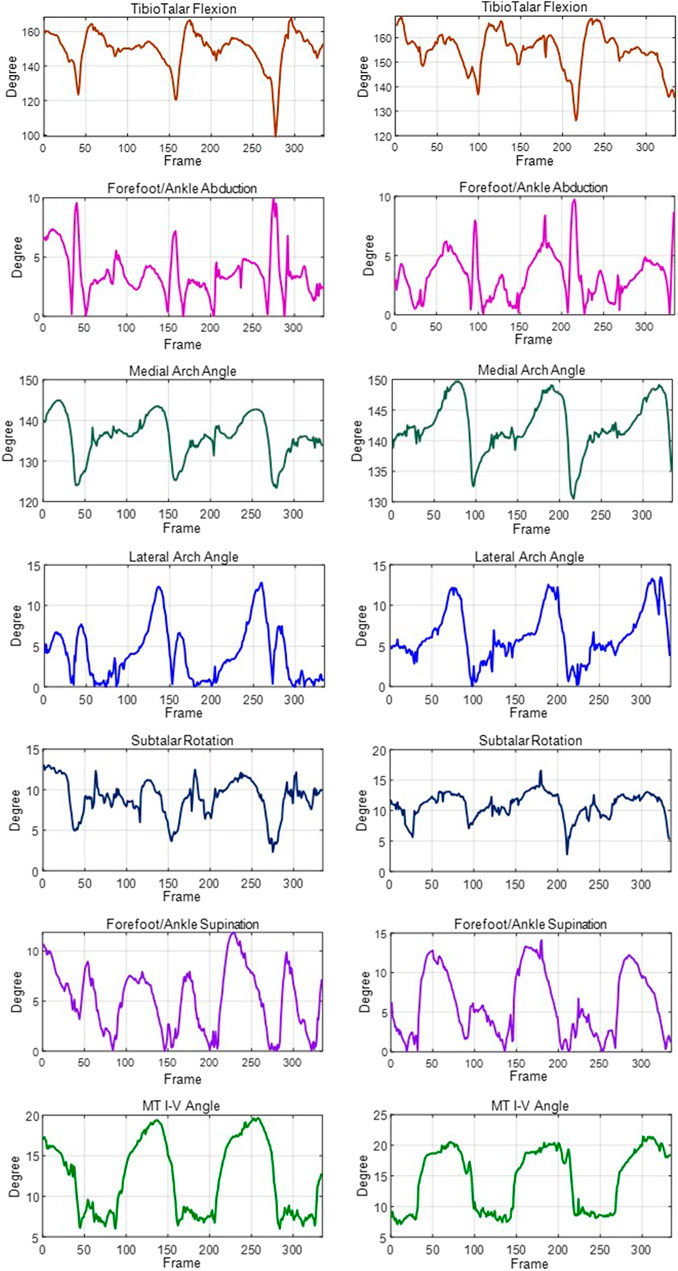
FIGURE 1. The gait kinematics variables (tibiotalar flexion, forefoot/ankle abduction, medial arch angle, lateral arch angle, subtalar rotation, forefoot/ankle supination, MT I-V angle) from a patient with lateral collateral ligament injuries of the ankle. Left: unaffected side; Right: affected side.
Motion data can be further used for calculating variables including gait speed, stride length, stride time, and force, pressure, etc. to describe spatiotemporal features of gaits accurately. Diliang Chen et al. calculated 26 gait parameters referring to basic gait parameters, gait variability, gait symmetry, and turning gait parameters for behavior recognition (sitting, standing, walking, running, up/down-stairs) to evaluate the performance of activities of daily living (Chen et al., 2020).
Our recent findings demonstrated that patients with lateral collateral ligament injuries of the ankle had shorter stride length, slower stride in the gait cycle, and more complex micro-adjustments in the 2nd rocker phase than in other rocker/swing phases during natural walking (Xin et al., 2021). Here, the five markers attached to TTU (tibia tuberosity), LML (lateral malleolus), CCL (dorsal calcaneus), DMT2 (distal 2nd metatarsal), and HLX (hallux) experience the change of velocity (speed up or slow down) during walking. Acceleration is the rate of change of the velocity for time. The moment when the acceleration was zero was considered to occur as a micro-adjustment.
These results revealed the motion compensatory mechanism in humans during walking. Patients with ligament injuries need more musculoskeletal adjustments to keeping body balance. Such micro-adjustment and compensation are difficult to be detected by physician’s eyes without using motion-tracking technology. Therefore, recording motion from gaits and precise descriptions of the kinematics is crucial for clinical assessment. Assessment results can guide surgeons to select appropriate treatment plans and examine operation outcomes after surgical management. Our results together with all other previous research in the field of gait analysis will provide a foundation for computer-aided diagnosis in the future.
Wearable devices can capture large-scale data. It is friendly to know the patient’s condition but unduly burden the clinicians. Computer-aided injuring detection will help clinicians analyze the complex relationships among the measures of gait kinetics, kinematics, and spatiotemporal features for pre-diagnosis (Saboor et al., 2020). Individuals can use their intelligent devices (i.e., smartphones) for auto-diagnosis at any time and anywhere. In recent studies, machine learning/deep learning has been used to analyze gait characteristics and recognize the impaired gait pattern. Mundt Marion et al. built a feedforward neural network to estimate the gait mechanics from the 3D joint angle and lower limb joint torque based on IMU data (Mundt et al., 2020). Wen Si et al. developed wearable sensing shoes to capture plantar pressure signals and used the support vector machine and fractal analysis for gait identification (standing, walking, and Jumping). Ravi Daniele et al. presented a deep learning method that combined IMU data with shallow features to enable real-time activity classification. They demonstrated that the proposed method is appropriated for smartphones and wearable sensor platforms (Ravi et al., 2017). In our current work, the Deep Convolutional Generation Adversarial Networks (DCGANs) were used to expand the spatiotemporal features during the gait cycle for training the detection model, and the Long Short-Term Memory (LSTM) networks were applied to detect ankle ligament injury patients (Liu et al., 2020). The artificial intelligent technique is promising for large-scale analytics, it can be used to analyze the large-scale wealthy information captured by wearable devices for health care.
Wearable sensors make it possible for motion tracking outside the laboratory. We can capture more spontaneous sports information using wearable devices for gait analysis in intelligent healthcare. In previous studies, the motion data captured by the smartphone were transformed to describe users’ daily exercise, to calculate the risk of fall, and to predict sports injuries using intelligent algorithms for improving individuals’ health management; smart insole was applied to measure step frequency, plantar pressure, and gait events for daily health monitoring; textile sensor arrays recognized motion behaviors in real-time (Chen et al., 2020).
Based on data collected from wearable devices, recent studies pay more attention to the measure of health status using intelligent mathematical models. For example, Joshua et al. developed GaitTrack software to detect health status via free-living walking patterns. The software using a linear regression algorithm evaluated the patients with chronic obstructive pulmonary disease and asthma (Juen et al., 2014). Raykov et al. proposed a structured probabilistic model to detect the disordered behaviors of individuals with Parkinson’s (Raykov et al., 2014). Several studies focused on pulmonary and cardiopulmonary function using gait patterns analysis (Cheng et al., 2016; Rasekaba et al., 2009). Moreover, some researchers analyzed gait based on wearable sensors for age and gender estimation (Ngo et al., 2019; Ahad et al., 2020). Daily health monitoring from wearable sensor-based gait analysis is becoming an indispensable way for healthcare in the future.
In the frontline of healthcare service, intelligent motion-tracking and analysis platforms are increasingly available, especially in rehabilitation and sports medicine (Merriaux et al., 2017). Multi-channels of 3D motion data captured by the Vicon motion capture systems and the computer-assisted rehabilitation environment (CAREN) system are analyzed by the biomechanical model for describing the kinematical features of gaits, posture control strategies, and energy expenditure. Clearly, Vicon and CAREN are laboratory-based devices and can only install in hospitals and rehabilitation centers, and applied to a small number of subjects. In the past decades, an increasing number of wearable devices is emerging (Flachenecker et al., 2020). Frequently recording of gaits of a wide range of people by wearable devices will open new opportunities for intelligent analysis. The wearable accelerometers and inertial measurement units can be attached to people in need outside healthcare institutes (Wang et al., 2021). These wearable devices provide long-term motion tracking during walking and allow for daily gait monitoring under different conditions. At present, wearable devices have been gradually used for physical rehabilitations on the treatment of neurodegenerative disease (e.g., Alzheimer’s disease, Parkinson’s disease), sports injury, bone malformation, and osteoarticular diseases (Sweeney et al., 2019). With assistance from wearable tracking devices on gaits, physical therapists can describe patients’ walking patterns, understand musculoskeletal disorders that constrain patients’ locomotion, and postulate the possible problems in the neural system that control patients’ movements (Hori et al., 2020). Data collected by wearable devices will help physical therapists to prescript the training protocol and make appropriate adjustments to improve therapy outcomes.
We review the application of wearable devices in motion-tracking, gait analysis, and its potentials for enhancing healthcare practices with the help of intelligent assisted data analysis. Various wearable devices and their research progress in motion tracking including smartphones, wearable sensors, and sensing fabrics are described. We briefly report our previous works on gait analysis using data collected from the foot and ankle ligament injuries patients. Daily monitoring of basic health data by wearable devices supports physicians to detect the health problem, make it possible for early diagnosis, and give them power for delivering appropriate treatment and rehabilitation to individuals in need. However, most current wearable sensors are not accurate enough for clinical evidence. We believe that wearable device should achieve equal or better outcome than motion-tracking platform (e.g., Vicon and CAREN) in the future.
Looking to the future, computer-assisted medicine based on data collected by wearable devices will attract an increasing amount of attention from researchers and clinicians. Intelligent analysis built on data collected by wearable devices will enhance clinical practice and biomechanical research.
XL: Data curation, formal analysis, writing-original draft preparation, visualization, funding acquisition. CZ: Resources, investigation. BZ: conceptualization, writing-original draft preparation, supervision. QG: Project administration, supervision. XD: Formal analysis. AW: Conceptualization. DZ: Project administration.
This work was supported by the National Natural Science Foundation of China (grant number 61801019); the Ministry of Science and Technology of the People’s Republic of China (grant number 2019ZX04003001-006); the China Scholarship Council (grant number 201906465021); the Beijing Association for Science and Technology (grant number 137862); and the Fundamental Research Funds for the Central Universities (grant number FRF-DF-20-04, FRF-BD-19-012A).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Ahad, M. a. R., Ngo, T. T., Antar, A. D., Ahmed, M., Hossain, T., Muramatsu, D., et al. (2020). Wearable Sensor-Based Gait Analysis for Age and Gender Estimation. Sensors 20 (8), 2424. doi:10.3390/s20082424
Ahmed, U., Ali, M. F., Javed, K., and Babri, H. A. (2017). “Predicting Physiological Developments from Human Gait Using Smartphone Sensor Data,” in Artificial Intelligence in Medicine. doi:10.1109/cybconf.2017.7985782
Amitrano, F., Coccia, A., Ricciardi, C., Donisi, L., Cesarelli, G., Capodaglio, E. M., et al. (2020). Design and Validation of an E-Textile-Based Wearable Sock for Remote Gait and Postural Assessment. Sensors 20 (22), 6691. doi:10.3390/s20226691
Bamberg, S., Benbasat, A. Y., Scarborough, D. M., Krebs, D. E., and Paradiso, J. A. (2008). Gait Analysis Using a Shoe-Integrated Wireless Sensor System. IEEE Trans. Inform. Technol. Biomed. 12 (4), 413–423. doi:10.1109/titb.2007.899493
Calliess, T., Bocklage, R., Karkosch, R., Marschollek, M., Windhagen, H., and Schulze, M. (2014). Clinical Evaluation of a Mobile Sensor-Based Gait Analysis Method for Outcome Measurement after Knee Arthroplasty. Sensors 14 (9), 15953–15964. doi:10.3390/s140915953
Canseco, K., Long, J., Smedberg, T., Tarima, S., Marks, R. M., and Harris, G. F. (2012). Multisegmental Foot and Ankle Motion Analysis after Hallux Valgus Surgery. Foot Ankle Int. 33 (2), 141–147. doi:10.3113/fai.2012.0141
Chen, D., Cai, Y., Qian, X., Ansari, R., Xu, W., Chu, K.-C., et al. (2020). Bring Gait Lab to Everyday Life: Gait Analysis in Terms of Activities of Daily Living. IEEE Internet Things J. 7 (2), 1298–1312. doi:10.1109/jiot.2019.2954387
Chen, S., Lach, J., Lo, B., and Yang, G.-Z. (2016). Toward Pervasive Gait Analysis with Wearable Sensors: A Systematic Review. IEEE J. Biomed. Health Inform. 20 (6), 1521–1537. doi:10.1109/jbhi.2016.2608720
Cheng, Q., Juen, J., Bellam, S., Fulara, N., Close, D., Silverstein, J. C., et al. (2016). Classification Models for Pulmonary Function Using Motion Analysis from Phone Sensors. AMIA Annu. Symp. Proc. 2016, 401–410.
Dahl, K. D., Dunford, K. M., Wilson, S. A., Turnbull, T. L., and Tashman, S. (2020). Wearable Sensor Validation of Sports-Related Movements for the Lower Extremity and Trunk. Med. Eng. Phys. 84, 144–150. doi:10.1016/j.medengphy.2020.08.001
Donisi, L., D’Addio, G., Pagano, G., Coccia, A., and Cesarelli, M. (2019). Study of Agreement between Two Wereable Inertial Systems for Gait Analysis Based on a Different Sensor Placement: G-Walk System and Opal System. Gait & Posture 74, 14. doi:10.1016/j.gaitpost.2019.07.462
Du, L., Zhu, X., and Zhe, J. (2015). An Inductive Sensor for Real-Time Measurement of Plantar Normal and Shear Forces Distribution. IEEE Trans. Biomed. Eng. 62 (5), 1316–1323. doi:10.1109/tbme.2014.2386136
Flachenecker, F., Gassner, H., Hannik, J., Lee, D., Flachenecker, P., Winkler, J., et al. (2020). Objective Sensor-Based Gait Measures Reflect Motor Impairment in Multiple Sclerosis Patients: Reliability and Clinical Validation of a Wearable Sensor Device. Mult. Scler. Relat. Disord. 39, 101903. doi:10.1016/j.msard.2019.101903
Hasan, C. Z. C., Jailani, R., and Tahir, N. M. (2018). “ANN and SVM Classifiers in Identifying Autism Spectrum Disorder Gait Based on Three-Dimensional Ground Reaction Forces,” in TENCON 2018 - 2018 IEEE Region 10 Conference, 2436–2440.
He, Z., Liu, T., and Yi, J. (2019). A Wearable Sensing and Training System: Towards Gait Rehabilitation for Elderly Patients with Knee Osteoarthritis. IEEE Sensors J. 19 (4), 5936–5945. doi:10.1109/jsen.2019.2908417
Hori, K., Mao, Y. F., Ono, Y., Ora, H., Hirobe, Y., Sawada, H., et al. (2020). Inertial Measurement Unit-Based Estimation of Foot Trajectory for Clinical Gait Analysis. Front. Physiol. 10, 1530. doi:10.3389/fphys.2019.01530
Juen, J., Cheng, Q., Prietocenturion, V., Krishnan, J. A., and Schatz, B. (2014). Health Monitors for Chronic Disease by Gait Analysis with Mobile Phones. Telemed. J. e-health : official J. Am. Telemed. Assoc. 20 (11), 1035–1041. doi:10.1089/tmj.2014.0025
Kostuj, T., Stief, F., Hartmann, K. A., Schaper, K., Arabmotlagh, M., Baums, M. H., et al. (2018). Using the Oxford Foot Model to Determine the Association between Objective Measures of Foot Function and Results of the AOFAS Ankle-Hindfoot Scale and the Foot Function Index: a Prospective Gait Analysis Study in Germany. Bmj Open 8 (4), e019872. doi:10.1136/bmjopen-2017-019872
Kwon, Y., Kang, K., and Bae, C. (2014). Unsupervised Learning for Human Activity Recognition Using Smartphone Sensors. Expert Syst. Appl. 41 (14), 6067–6074. doi:10.1016/j.eswa.2014.04.037
Leardini, A., Benedetti, M. G., Berti, L., Bettinelli, D., Nativo, R., and Giannini, S. (2007). Rear-foot, Mid-foot and Fore-Foot Motion during the Stance Phase of Gait. Gait & Posture 25 (3), 453–462. doi:10.1016/j.gaitpost.2006.05.017
Liu, X., Zhao, C., Zheng, B., Guo, Q., Zhang, Z., Wulamu, A., et al. (2020). Synthesizing Foot and Ankle Kinematic Characteristics for Lateral Collateral Ligament Injuries Detection. IEEE Access 8, 188429–188440. doi:10.1109/access.2020.3029616
Lorussi, F., Rocchia, W., Scilingo, E. P., Tognetti, A., and De Rossi, D. (2004). Wearable, Redundant Fabric-Based Sensor Arrays for Reconstruction of Body Segment Posture. IEEE Sensors J. 4, 807–818. doi:10.1109/jsen.2004.837498
Macwilliams, B. A., Cowley, M., and Nicholson, D. E. (2003). Foot Kinematics and Kinetics during Adolescent Gait. Gait & Posture 17, 214–224. doi:10.1016/s0966-6362(02)00103-0
Merriaux, P., Dupuis, Y., Boutteau, R., Vasseur, P., and Savatier, X. (2017). A Study of Vicon System Positioning Performance. Sensors 17 (7), 1591. doi:10.3390/s17071591
Mundt, M., Koeppe, A., David, S., Witter, T., Bamer, F., Potthast, W., et al. (2020). Estimation of Gait Mechanics Based on Simulated and Measured IMU Data Using an Artificial Neural Network. Front. Bioeng. Biotechnol. 8, 41. doi:10.3389/fbioe.2020.00041
Ngo, T. T., Ahad, M. a. R., Das Antar, A., Ahmed, M., Muramatsu, D., Makihara, Y., et al. (2019). “OU-ISIR Wearable Sensor-Based Gait Challenge: Age and Gender,” in 2019 International Conference on Biometrics (Icb).). doi:10.1109/icb45273.2019.8987235
Rasekaba, T., Lee, A. L., Naughton, M. T., Williams, T. J., and Holland, A. E. (2009). The Six-Minute Walk Test: a Useful Metric for the Cardiopulmonary Patient. Intern. Med. J. 39, 495–501. doi:10.1111/j.1445-5994.2008.01880.x
Ravi, D., Wong, C., Lo, B., and Yang, G.-Z. (2017). A Deep Learning Approach to On-Node Sensor Data Analytics for Mobile or Wearable Devices. IEEE J. Biomed. Health Inform. 21, 56–64. doi:10.1109/jbhi.2016.2633287
Raykov, Y. P., Boukouvalas, A., and Little, M. A. (2014). Simple Approximate MAP Inference for Dirichlet Processes Mixtures. Electron. J. Stat. 10 (2), 3548–3578. doi:10.1214/16-EJS1196
Reginya, S., Meigal, A. Y., Gerasimova-Meigal, L. I., Prokhorov, K., and Moschevikin, A. (2019). Using Smartphone Inertial Measurement Unit for Analysis of Human Gait. Int. J. Embedded Real-Time Commun. Syst. (Ijertcs) 10, 101–117. doi:10.4018/ijertcs.2019070107
Ren, P., Karahan, E., Chen, C., Luo, R., Geng, Y., Bosch Bayard, J. F., et al. (2017). Gait Influence Diagrams in Parkinson’s Disease. IEEE Trans. Neural Syst. Rehabil. Eng. 25, 1257–1267. doi:10.1109/tnsre.2016.2622285
Saboor, A., Kask, T., Kuusik, A., Alam, M. M., Le Moullec, Y., Niazi, I. K., et al. (2020). Latest Research Trends in Gait Analysis Using Wearable Sensors and Machine Learning: A Systematic Review. IEEE Access 8, 167830–167864. doi:10.1109/access.2020.3022818
Schlachetzki, J. C. M., Barth, J., Marxreiter, F., Gossler, J., Kohl, Z., Reinfelder, S., et al. (2017). Wearable Sensors Objectively Measure Gait Parameters in Parkinson’s Disease. Plos One 12 (10), e0183989. doi:10.1371/journal.pone.0183989
Shu, L., Hua, T., Wang, Y. Y., Li, Q., and Tao, X. M. (2010). 111 Fabric Sensor Based In-Shoe Plantar Pressure Measurement System for Gait and Balance Analysis. Parkinsonism Relat. Disord. 16, S32. doi:10.1016/s1353-8020(10)70112-7
Simon, J., Doederlein, L., Mcintosh, A. S., Metaxiotis, D., Bock, H. G., and Wolf, S. I. (2006). The Heidelberg Foot Measurement Method: Development, Description and Assessment. Gait & Posture 23, 411–424. doi:10.1016/j.gaitpost.2005.07.003
Soubra, R., Diab, M. O., and Moslem, B. (2016). ““Identification of Parkinson’s Disease by Using Multichannel Vertical Ground Reaction Force Signals,” in 2016 International Conference on Bio-Engineering for Smart Technologies (BioSMART), 1–4. doi:10.1109/BIOSMART.2016.7835604
Springer, S., and Seligmann, G. Y. (2016). Validity of the Kinect for Gait Assessment: A Focused Review. Sensors 16 (2), 194. doi:10.3390/s16020194
Sweeney, D., Quinlan, L. R., Browne, P., Richardson, M., Meskell, P., and Olaighin, G. (2019). A Technological Review of Wearable Cueing Devices Addressing Freezing of Gait in Parkinson's Disease. Sensors 19 (6), 1277. doi:10.3390/s19061277
Taborri, J., Palermo, E., Rossi, S., and Cappa, P. (2016). Gait Partitioning Methods: A Systematic Review. Sensors 16 (1), 66. doi:10.3390/s16010066
Tahir, A. M., Chowdhury, M. E. H., Khandakar, A., Al-Hamouz, S., Abdalla, M., Awadallah, S., et al. (2020). A Systematic Approach to the Design and Characterization of a Smart Insole for Detecting Vertical Ground Reaction Force (vGRF) in Gait Analysis. Sensors 20 (4), 957. doi:10.3390/s20040957
Tirosh, O., Begg, R., Passmore, E., and Knopp-Steinberg, N. (2013). “Wearable Textile Sensor Sock for Gait Analysis,” in 2013 Seventh International Conference on Sensing Technology (Icst). doi:10.1109/icsenst.2013.6727727
Wang, F. C., Chen, S. F., Lin, C. H., Shih, C. J., Lin, A. C., Yuan, W., et al. (2021). Detection and Classification of Stroke Gaits by Deep Neural Networks Employing Inertial Measurement Units. Sensors 21 (5), 1864. doi:10.3390/s21051864
Wang, W., Sun, J. D., Li, J., and Zhao, D. (2016). “Gait Recognition Based on 3d Skeleton Joints Captured by Kinect,” in 2016 Ieee International Conference on Image Processing (Icip). doi:10.1109/icip.2016.7532940
Xin, L., Dezheng, Z., Bin, Z., Qinwei, G., and Zhongshi, Z. (2021). “Gait Kinematics of Patients with Lateral Collateral Ligament Injuries of Ankle,” in Research Square.
Yang, C. M., Yang, T. L., Yang, C. W., and Yang, H. (2015). System and Method for Analyzing Gait Using Fabric Sensors.
Keywords: gait analysis, motion-tracking, spatiotemporal variables, kinematics, application
Citation: Liu X, Zhao C, Zheng B, Guo Q, Duan X, Wulamu A and Zhang D (2021) Wearable Devices for Gait Analysis in Intelligent Healthcare. Front. Comput. Sci. 3:661676. doi: 10.3389/fcomp.2021.661676
Received: 31 January 2021; Accepted: 26 April 2021;
Published: 13 May 2021.
Edited by:
Ling Chen, Zhejiang University, ChinaReviewed by:
Haoru Su, Beijing University of Technology, ChinaCopyright © 2021 Liu, Zhao, Zheng, Guo, Duan, Wulamu and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Bin Zheng, YmluLnpoZW5nQHVhbGJlcnRhLmNh; Qinwei Guo, Z3VvcWlud2VpQHZpcC5zaW5hLmNvbQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.