
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychol. , 23 September 2020
Sec. Psycho-Oncology
Volume 11 - 2020 | https://doi.org/10.3389/fpsyg.2020.564079
Objectives: While both patients and informal caregivers report high levels of cancer-related distress, supportive care needs of relatives are often not taken into account and little is known about mutual perception of distress within couples. Therefore, we aimed to investigate distress in female patients with breast cancer and their male partners as well as supportive care needs in partners.
Methods: In this cross-sectional study, we recruited women with breast cancer during primary cancer care and their male partners, obtained information on mental distress and supportive care needs through visual analog scales for four mood domains and the Short Form of Supportive Care Needs Survey (SCNS-SF34).
Results: Among 250 eligible patients with breast cancer, 102 patients (40.8%) and their male partners participated. Partners reported higher levels of distress (p = 0.02), whereas patients (self-assessment) indicated stronger needs for help (p < 0.001). Men with higher levels of distress were younger (p < 0.001), and reported a shorter relationship duration (p = 0.001) compared to partners with lower distress. Partners overestimated distress, anxiety, depression, and need for help in the patient. Patients overestimated partners need for help. The majority of partners (78%) reported at least one unmet need, most frequently related to the health system and information domain.
Conclusion: A systematic distress and needs assessment for women with breast cancer and their male partners is mandatory. The provision of optimal supportive care depends on protocols that include not only psychosocial care for patients but also procedures for managing distress and needs for partners including individual and couple-based interventions.
It is well-known that breast cancer and its treatment have a debilitating effect on patients suffering from health restrictions such as lymphedema, pain, early menopause, and sexual problems (Baucom et al., 2006), as well as from wide-ranging psychosocial consequences like anxiety, depression, and self-image concerns (Bloom, 2002; Mitchell et al., 2011; Ng et al., 2011). An extensive review on unmet needs of women with breast cancer concludes that the greatest need is in the area of health system/information and psychological topics (Fiszer et al., 2014).
Cancer and its treatments also have an impact on the family environment. Several studies yielded to examine this issue including mood disturbance and mental burden of family members (Pitceathly and Maguire, 2003; Drabe et al., 2013; Williams et al., 2013; Schrank et al., 2016). Kayser et al. (2007) postulated cancer as a “we-disease.” Patients and caregivers show clinically relevant cancer-related distress and sometimes caregivers report even higher levels of anxiety than patients (Northouse et al., 2012; Feiten et al., 2013; Gröpper et al., 2016). In contrast, another study found that 35.7% of patients with breast cancer and 16.1% of partners report moderate to severe distress (Dumitra et al., 2018). A comparison of spouses and other social network members of women with breast cancer and prostate cancer patients revealed high depression levels in spouses (Segrin and Badger, 2010). Studies on gender and role (patient vs. partner) in couples dealing with cancer show that women in both roles report higher burden than males and that women and male partners report lower quality of life compared to the general population (Bergelt et al., 2008; Drabe et al., 2016). Distress levels and quality of life do not differ between female patients and female partners, and both groups report higher distress and lower quality of life than unaffected controls, while male partners report higher distress levels than male patients (Hagedoorn et al., 2000).
The majority (60%) of women with breast cancer regards their partner as their main source of emotional support (Sandgren et al., 2004). However, patients with breast cancer frequently report that they do not talk about their feelings with the family (Faller, 1998). Insufficient communication about perceived distress, anxiety and related issues can lead to misperception of burden in both partners, which can affect the couple’s relationship and further adaptive coping efforts. In palliative situations, family caregivers overestimate symptoms in patients (Oechsle et al., 2013b) and increased anxiety in family caregivers is associated with a discrepancy in the patients’ symptom evaluation in terminally ill patients (Oechsle et al., 2013a).
Both patients and partners are facing major challenges in diagnosis and treatment. Dyadic coping is characterized by interaction between stress signals in one partner and the coping response of the other. According to Bodenmann’s systemic-transactional theory (Bodenmann, 1997) coping is a stress management process in which one partner either ignores or reacts to the other partner’s stress signals in order to maintain a level of stability at the individual level on one hand and at the dyadic level on the other hand. Couples react as an emotional system and not as individuals (Hagedoorn et al., 2008). The partners’ distress is significantly related to lower relationship satisfaction (Pankrath et al., 2018). Higher distress in partners might adversely influence dyadic coping processes and have a negative impact on patients’ and partners’ quality of life and the relationship quality (Segrin, 2005; Kayser et al., 2007; Brusilovskiy et al., 2009; Robbins et al., 2014). A study of 42 couples in whom the male partner suffer from prostate cancer highlighted the association between perception of negative coping in each other with a higher psychological burden (Regan et al., 2014). These results are complemented by a study in patients with metastatic breast cancer and their partners which has shown that positive joint coping strategies lead to lower stress levels and better adaptation to the situation for both partners (Badr et al., 2010). Open and constructive communication seems to improve dyadic coping (Brandão et al., 2017).
In Germany, according to guidelines of the German Cancer Society, the German Cancer Aid and the Working Groups of the Scientific Medical Societies for the treatment of breast cancer (2020) and also according to the guideline on psycho-oncological diagnostics and care of cancer patients (2014), a routine distress screening in patients is mandatory, which entails that psycho-oncological care often focuses on supporting the patient while distress in relatives might remain undetected.
Studies on the mutual assessments of distress in women with breast cancer and their male partners and the resulting supportive care needs are rare. The general aim of this study was to increase this knowledge in order to allow for the development of improved support strategies for patients and their partners.
Therefore, the study focused on the following objectives and hypotheses:
(1) How do female patients and their male partners evaluate their own distress levels (self-assessment)? We hypothesize that patients and partners do not differ significantly in this regard.
(2) How do male partners evaluate the distress level of female patients and vice versa (other reported assessment)? We hypothesize that partners overestimate the mental burden of the patients, and that the patients underestimate the mental burden of their partners.
(3) What supportive care needs do male partners of patients with breast cancer report?
In this cross-sectional study, we recruited women with breast cancer and their male partners over a 2-year period at the Breast Cancer Center, University Medical Center Hamburg, Germany. Patients were eligible if they were (i) diagnosed with a malignant tumor of the breast according to the medical record and/or their treating physician, (ii) 18 years or older, (iii) living in a heterosexual relationship, (iv) able to speak and read German and (v) able to give informed consent for study participation. Eligible patients were consecutively recruited by a trained study research assistant during outpatient chemotherapy treatment and were asked to complete a set of validated questionnaires. Each female patient asked her male partner if he was interested to participate in the study. Upon approval, the partner received a questionnaire in a closed envelope. Both patients and partners had to provide written informed consent and received prepaid envelopes to return the completed questionnaires. A color differentiation and unambiguous labeling ensured that the questionnaires were clearly assigned; (self-assessment vs. other reported assessment). The study participants filled out the questionnaire at home. Completing the questionnaires took about 20 min for each participant (patient and partner). A single reminder was sent out after 4 weeks.
The study was carried out in accordance with the Declaration of Helsinki and the data privacy protection laws and approved by the local ethics committee (Ethics Board Hamburg Number PV4560).
Medical data from the patients were obtained from the electronic hospital information system including location of the tumor, time of first diagnosis, time of current diagnosis (if recurrence or second tumor), TNM-classification, current treatment as well as relevant somatic comorbidities. Partners completed a questionnaire: items included age, relationship to the patient, number of children, level of education, employment status and monthly household income.
Patients were asked to assess how burdened they felt themselves due to their cancer (self-assessment). Furthermore, they were asked to estimate the level of burden in their partner (other reported assessment). Partners were asked to assess how burdened they felt because of the cancer (self-assessment) and how they assessed the burden of the patient (other reported assessment). Partners were also asked about their support needs.
To assess the mental burden we used the Emotion Thermometer (Mitchell et al., 2010). This visual analog scale covers for four mood domains: distress, anxiety, depression and anger. We additionally included need for help as a further domain. Participants were asked to rate every domain from 0 (“not at all or no help necessary”) to 10 (“extreme”). Following literature recommendations, we used a cut-off of 5 in the distress domain (Mehnert et al., 2006; Hinz et al., 2019).
The German version of the Supportive Care Needs Survey – Short Form 34 (SCNS-SF-34) measures participants’ perceived kind and level of need for support in five domains: health system and information, psychological, physical and daily living, patient care and support, and sexuality needs (Lehmann et al., 2012). If in need of support in a domain, they are asked to rate level of the need on a 5-point Likert scale (1 = no need, 2 = no need, satisfied, 3 = low need, 4 = moderate need, 5 = high need). For each scale, sum scores were calculated (between 0 and 100). High scores indicate high supportive care needs. Furthermore, the answers were dichotomized, i.e., answer alternatives 1 or 2 mean no need for support and answer alternatives 3–5 mean need for support. The reliability of the five scales is high with Cronbach’s alpha ranging from 0.82 to 0.95 (Nunnally, 1978).
Sociodemographic and medical characteristics of the samples were analyzed by descriptive statistics. Group differences regarding self-assessment and assessment of the partner for distress (other reported assessment) were analyzed by using t-test for independent samples. We analyzed associations between categorical variables using chi-square test. The association between the assessment of the partner’s burden and self-assessed mental burden was analyzed by Pearson’s correlation. Linear regression analyses were conducted to analyze association in mutual assessment. Therefore, we included age, marital status, children, school qualification, living together, and duration of relationship.
Supportive care needs were analyzed according to the manual of the SCNS-SF34 by calculating means and frequencies. The association between distress and other supportive care needs was analyzed by Pearson’s correlation. The level of significance for all tests was defined as p = 0.05. Statistical analyses were conducted using SPSS statistical software for windows version 25.
Out of 250 eligible female patients with breast cancer, 102 female patients (40.8%) and their male partners agreed to participate, and provided complete data (Figure 1). The reasons given for non-participation were excessive physical or mental burden, lack of interest, or the certainty that the partner would not participate. The mean age of the patients was 54 years (SD = 13.2; range 26–81) and of their partners 56 years (SD = 13.5; range 26–81).
Table 1 summarizes demography of the total sample as well as the medical characteristics of patients with breast cancer.
Patients and partners reported similar levels of anxiety, depression and anger, while partners reported significantly higher distress levels than patients. In contrast, patients reported more need for help than partners (Table 2).
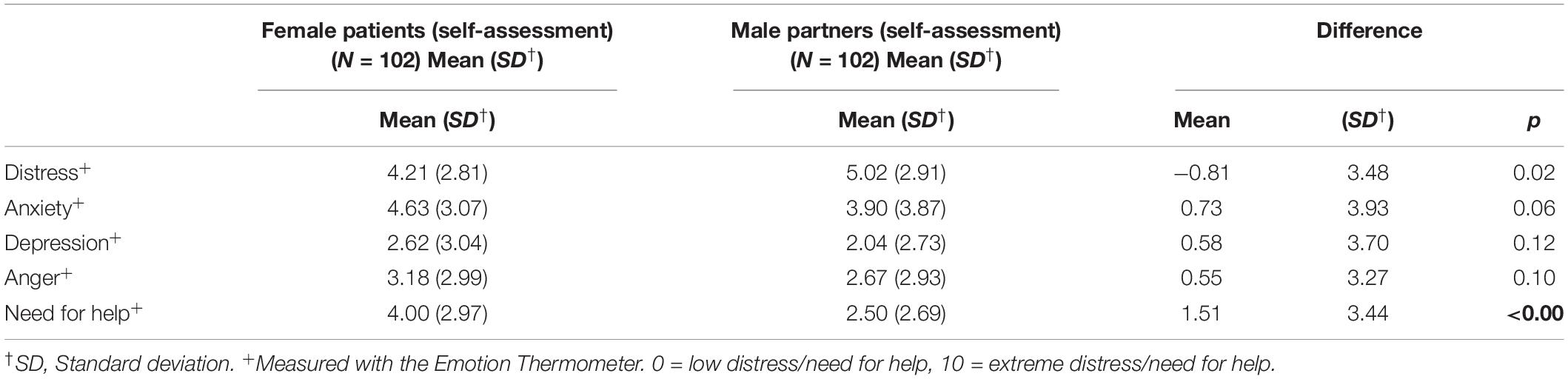
Table 2. Mental burden in female patients with breast cancer and their male partners (self-assessment).
47% of the patients and 62% of the partners reported clinically relevant distress levels above cut-off (p = 0.043). Highly distressed partners are significantly younger (51.2 years vs. 62.1 years; p < 0.001), and reported a shorter relationship duration (19.6 years vs. 31.5 years; p = 0.001) than less distressed partners, but do not differ to them with regard to having children (p = 0.14), school education (p = 0.25) or cohabitation (p = 0.35).
Male partners overestimated distress, anxiety, depression, and need for help in the patient, compared to the patients’ self-assessment, while anger was evaluated similarly to the patients’ report. The evaluation for the patient by her male partners (other reported assessment) was significantly associated to the self-perceived mental burden in the male partner (Table 3).
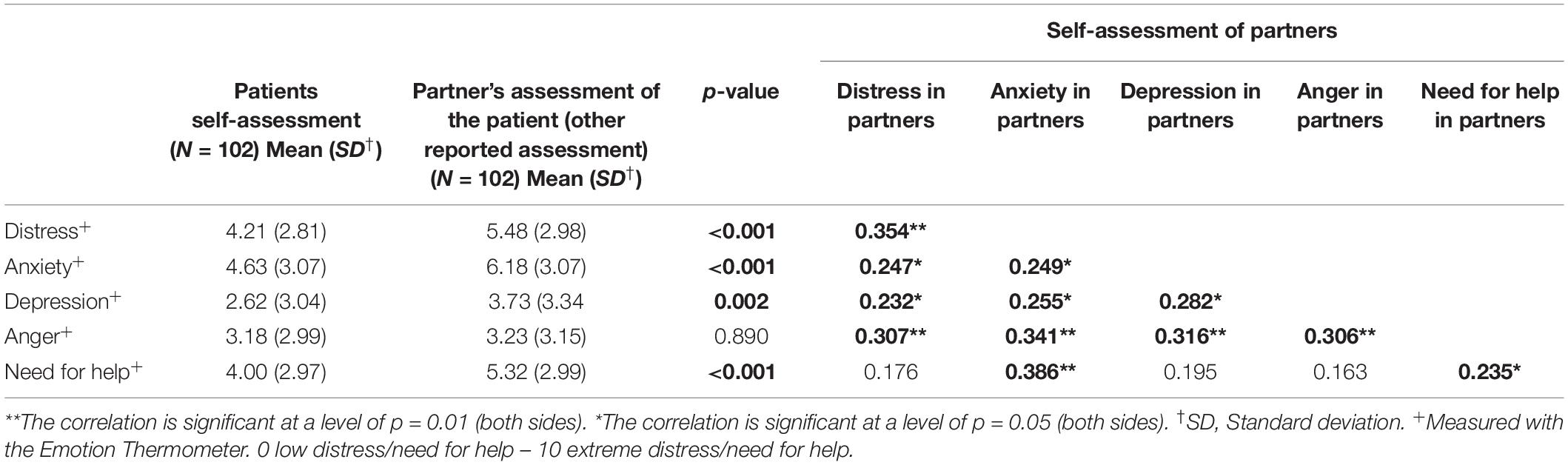
Table 3. Associations between male partners’ assessment of female patients’ mental burden (other reported assessment) and needs and patients self-assessment of mental burden and needs (Pearson’s correlation).
Age, marital status, children, school qualification, living together, and duration of relationship were not significantly associated with the partner’s overestimation of distress, anxiety, depression, and need for help in the patient (other reported assessment). There were no significant differences between patients’ assessment of the partner’s situation and partners self-assessment with regard of distress (5.05 vs. 5.02, p = 0.90), anxiety (4.00 vs. 3.90, p = 0.72), depression (1.78 vs. 2.04, p = 0.22) and anger (2.40 vs. 2.67, p = 0.35). Patients did, however, overestimate need for help in their partners (3.08 vs. 2.50; p = 0.03).
The majority of partners (78%) reported at least one unmet need (M = 14, SD = 11.6). All supportive care needs were significantly positively associated to higher levels of anxiety, depression and distress (see Table 4).
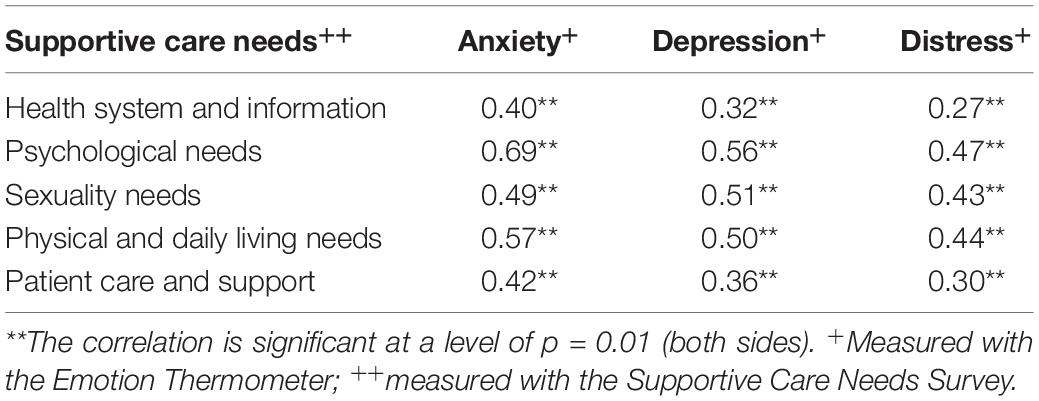
Table 4. Association of supportive care needs in male partners and mental burden in male partners (self-assessment) of female patients with breast cancer (Pearson’s correlation).
The highest rated needs according to the SCNS-SF-34 in male partners are in the domain health system and information (M = 38.9; SD = 34.9), followed by psychological needs (M = 34.7; SD = 31.7), sexuality needs (M = 29.7; SD = 32.1), physical and daily living needs (M = 23.5; SD = 22.4), and needs in patient care and support (M = 20.2; SD = 25.2).
This study examined psychosocial distress in women with breast cancer and their male partners and the impact on supportive care needs in partners. As hypothesized, we found that female patients and their male partners did not differ in self-assessment with regard to anxiety levels, depressive symptoms and anger. These findings support the results of other studies (Hodges et al., 2005; Rosenberger et al., 2012). The relatively high anxiety levels in this sample might be treatment-related, since most of the women (82%) were recruited during chemotherapy. A review of studies conducted between 1990 and 2010 also showed high anxiety levels in patients during chemotherapy (Lim et al., 2011). Interestingly, in our study partners reported higher distress than patients, which is in line with another study, were primary caregivers were more distressed than the respective patients (Sklenarova et al., 2015). Also previous studies found a higher global burden in spouses (Hasson-Ohayon et al., 2010; Segrin and Badger, 2010). Further, meta-analyses showed, that male partners have reported more distress when the women is the patient in the couple (Hagedoorn et al., 2008). However, some other studies also reported higher distress in women than in men regardless of their role as patient or caregiver (Hagedoorn et al., 2008). Our results do not necessarily contradict these findings. Our results rather indicate that the diagnosis and treatment of breast cancer in their wives are extremely burdening for male partners. A study on 96 dyads suggested that the within-dyad influence runs mostly from partners anxiety to the anxiety of women with breast cancer (Segrin et al., 2007).
Even though partners in our sample perceived higher distress levels than female patients, they reported fewer needs for help. This might possibly be explained by the treatment situation, in which women are physically impaired and therefore express more needs for help. Further, this finding could be gender-related: men might not perceive or admit supportive care needs due to their gender role perceptions. In the literature similar results are reported: women both reported more request for help (Merckaert et al., 2010) and accepted more help than men (Curry et al., 2002). Male partners also provide practical support for the patient and might thus neglect their own needs in this situation.
In our study, patients were asked, after having assessed their own burden (self-assessment), to assess their partner’s burden (other reported assessment) caused by their wives cancer disease. Accordingly, the partners were asked to assess their own burden first (self-assessment) and then the burden of the patient (other reported assessment). Our hypothesis that women overestimate mental burden distress in their partner (other reported assessment) was only confirmed with regard to need for help. Considering the sequence of questions, this might be an expression or projection for their own need and wish for help. This assumption matches and supports the clinical experience that women often wish for help for their partners. However, the mutual evaluation of female patients by male partners (other reported assessment) revealed an overestimation of distress, anxiety, and depression as well as for need for help. This was associated with high distress and mental burden in partners. These results are in the line with another study reporting that family caregivers of patients receiving chemotherapy typically overestimate cancer patients’ symptom burden and suffer from considerable mental burden themselves (Silveira et al., 2010). Our study also investigated supportive care needs in partners and has shown that partners of women with breast cancer report high levels of supportive care needs. The needs of partners are strongly related to their own distress, anxiety and depression. Most needs are health system and information needs as well as psychological needs. For example, “Having one member of hospital staff with whom you can talk to about all aspects of condition, treatment and follow up” is frequently mentioned (38.2%) as a health system need, as “Being informed as soon as possible about cancer which is under control or diminishing” (46.1%) in relation to information-related needs. This order seems to be the same for patients with breast cancer (Fiszer et al., 2014). A study in the outpatient setting reports similarly high needs in family caregivers of patients with different cancer diagnoses, but in reverse order (Rosenberger et al., 2012). In this study the relatives showed particularly high needs with regard to psychological needs followed by health system and information needs. It should also be noted that the relatives in this sample were predominantly female (67%), which could also be the reason for this order. These findings underline the high and so far often neglected, mental burden of partners.
Considering the interaction of the couple with regard to perceived burden and coping, the systemic-transactional theory model (Bodenmann, 1997), provides a useful framework for the interpretation of our results. Both partners are affected by the cancer diagnosis and its treatment. Partners include the stress of the partner in their own actions. For example, an overestimation of the partner’s need for support by the patient (other reported assessment) could be an expression of a desire to restore or maintain the dyadic system. This desire could be described as a supportive coping by the couple (Bodenmann, 2000). Alternatively, coping could take place by transferring the perceived burden. A recent study in Germany showed that couples in whom one partner had been diagnosed with cancer used similar coping strategies (Osin et al., 2018).
High levels of distress might indicate the need for specific psycho-oncological support for women with breast cancer as well as for male partners. Despite existing evidence that in couples with highly distressed patients with breast cancer and their partners demonstrated, that both patients and partners benefit from strengths-based interventions (Brandão et al., 2013; Bitz et al., 2015) partners are often not integrated in the health care system and available support offers according to their needs. A meta-analysis, which could include 10 randomized studies with psychotherapeutic couple-based interventions, showed significant improvements in mental stress (Faller et al., 2013).
However, there is also some evidence that especially in couples with a high relationship functioning at baseline, a psychological intervention does provide significant benefit (Traa et al., 2015). A study examined different aspects of couples with one of them suffering from cancer (Magsamen-Conrad et al., 2015). Here communication efficacy proved to be as an effective predictor for coping. An study on a dyadic coping (Saita et al., 2016) could demonstrate that patients who participated in a Cancer Dyads Group Intervention benefited regarding to the fighting spirit. One aim of the intervention was the improvement of patient engagement and the promotion of the relationship between patients and their informal caregivers. Individuals in the intervention group showed changes in all coping styles evaluated. As a further development of our results a group intervention for couples according to the Cancer Dyads Group Intervention would also be conceivable.
Our study has some limitations. First, study design was cross-sectional and thus cannot provide long-term data or give an indication on cause and effect. Second, while the response rate of 68% was relatively high, the completer rate was, however only 41%. There is a risk of a sample bias and we do not know, if couples with high relationship satisfaction or couples with high levels of distress are overrepresented in the sample. Previous research suggests that especially couples who are able to express their fears, feelings and needs in connection with cancer-specific issues report a higher level of relationship functioning (Traa et al., 2015). Perhaps these were the very couples who participated in our study. Furthermore, we have not measured communication efficacy, which may play a major role in managing cancer (Magsamen-Conrad et al., 2015). Thus, generalization of the results is limited. Hypotheses for further studies can be derived from this. For testing, patients with different tumor diagnoses and their partners should be selected. This could help to answer the question as to how far the sex of the patient and the type of oncological treatment plays a role in the management of the disease. It is important to measure dyadic coping, ideally over the course of the disease. For this purpose we suggest a mixed-method study design. For example, interviews with patients and partners could complement quantitative results with even deeper insights. Distress screening is nowadays state of the art in the interdisciplinary care for cancer patients, as mandated by current treatment guidelines (2020). However, our findings indicate that in addition to that a systematic distress and needs assessment for male partners of patients with breast cancer should be routinely implemented. According to the results of the screening and the preferences of patients and partners, psycho-oncological support services should offer both individual and couple-based interventions.
The datasets for this article are not publicly available because of data protection principles. Requests to access the datasets should be directed to UG,dXRlLmdvZXJsaW5nQGNoYXJpdGUuZGU=.
The studies involving human participants were reviewed and approved by the Ethics Board Hamburg. The patients/participants provided their written informed consent to participate in this study.
UG analyzed the data and wrote the manuscript. CB co-wrote the manuscript. AM-T and VM planned the study, analyzed, and co-wrote the manuscript. All authors contributed to the article and approved the submitted version.
The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the Susan G. Komen Germany r.a., association for cure in breast cancer (KOM12/12/2011).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
We thank Juliane Meise for assistance.
(2014). Leitlinienprogramm Onkologie (Deutsche Krebsgesellschaft, Deutsche Krebshilfe, AWMF): Psychoonkologische Diagnostik, Beratung und Behandlung von erwachsenen Krebspatienten, Langversion 1.1, AWMF-Registernummer: 032/051OL. Available at: http://leitlinienprogramm-onkologie.de/Leitlinien.7.0.html
(2020). Leitlinienprogramm Onkologie (Deutsche Krebsgesellschaft, Deutsche Krebshilfe, AWMF): S3-Leitlinie Früherkennung, Diagnose, Therapie und Nachsorge des Mammakarzinoms, Version 4.3, AWMF Registernummer: 032-045OL. Available at: http://www.leitlinienprogramm-onkologie.de/leitlinien/mammakarzinom/
Badr, H., Carmack, C. L., Kashy, D. A., Cristofanilli, M., and Revenson, T. A. (2010). Dyadic coping in metastatic breast cancer. Health Psychol. 29, 169–180. doi: 10.1037/a0018165
Baucom, D., Porta, L. S., Kirby, J. S., Gremore, T. M., and Keefe, F. J. (2006). Psychosocial issue confronting young women with breast cancer. Breast Dis. 23, 103–113. doi: 10.3233/BD-2006-23114
Bergelt, C., Koch, U., and Petersen, C. (2008). Quality of life in partners of patients with cancer. Qual. Life Res. 17, 653–663. doi: 10.1007/s11136-008-9349-y
Bitz, C., Clark, K., Vito, C., Kruper, L., Ituarte, P. H. G., and Loscalzo, M. (2015). Partners’ clinic: an innovative gender strengths-based intervention for breast cancer patients and their partners immediately prior to initiating care with their treating physician. Psycho Oncol. 24, 355–358. doi: 10.1002/pon.3604
Bodenmann, G. (1997). Dyadic coping: a systemic-transactional view of stress and coping among couples: theory and empirical findings. Eur. Rev. Appl. Psychol. 47, 137–140.
Brandão, T., Pedro, J., Nunes, N., Martins, M. V., Costa, M. E., and Matos, P. M. (2017). Marital adjustment in the context of female breast cancer: a systematic review. Psycho Oncol. 26, 2019–2029. doi: 10.1002/pon.4432
Brandão, T., Schulz, M. S., and Matos, P. M. (2013). Psychological intervention with couples coping with breast cancer: a systematic review. Psychol. Health 29, 491–516.
Brusilovskiy, E., Mitstifer, M., and Salzer, M. S. (2009). Perceived partner adaptation and psychosocial outcomes for newly diagnosed stage I and stage II breast cancer patients. J. Psychos. Oncol. 27, 42–58. doi: 10.1080/07347330802614774
Curry, C., Cossich, T., Matthews, J., Beresford, J., and McLachlan, S. (2002). Uptake of psychosocial referrals in an outpatient cancer setting: improving service accessibility via the referral process. Support. Care Cancer 10, 549–555. doi: 10.1007/s00520-002-0371-2
Drabe, N., Steinert, H., Moergeli, H., Weidt, S., Strobel, K., and Jenewein, J. (2016). Perception of treatment burden, psychological distress, and fatigue in thyroid cancer patients and their partners – effects of gender, role, and time since diagnosis. Psycho Oncol. 25, 203–209. doi: 10.1002/pon.3903
Drabe, N., Wittmann, L., Zwahlen, D., Büchi, S., and Jenewein, J. (2013). Changes in close relationships between cancer patients and their partners. Psycho Oncol. 22, 1344–1352. doi: 10.1002/pon.3144
Dumitra, S., Jones, V., Rodriguez, J., Bitz, C., Polamero, E., Loscalzo, M., et al. (2018). Disparities in managing emotions when facing a diagnosis of breast cancer: results of screening program of couples distress. Surgery [Epub ahead of print]. doi: 10.1016/j.surg.2017.11.022
Faller, H. (1998). Krankheitsverarbeitung bei Krebskranken. Göttingen: Verlag für Angewandte Psychologie.
Faller, H., Schuler, M., Richard, M., Heckl, U., Weis, J., and Küffner, R. (2013). Effects of psychooncological interventions on emotional distress and quality of life in adult cancer patients: systematic review andmeta-analysis. J. Clin. Oncol. 31, 782–793.
Feiten, S., Friesenhahn, V., Heymanns, J., Kleboth, K., Köppler, H., Mergenthaler, U., et al. (2013). Psychosocial distress in caregivers of patients with a metastatic solid tumor in routine care: a survey in a community based oncology group practice in Germany. Cancer Clin. Oncol. 2:v2n2p1. doi: 10.5539/cco.v2n2p1
Fiszer, C., Dolbeault, S., Sultan, S., and Brédart, A. (2014). Prevalence, intensity, and predictors of the supportive care needs of women diagnosed with breast cancer: a systematic review. Psychooncology 23, 361–374. doi: 10.1002/pon.3432
Gröpper, S., van der Meer, E., Landes, T., Bucher, H., Stickel, A., and Goerling, U. (2016). Assessing cancer-related distress in cancer patients and caregivers receiving outpatient psycho-oncological counseling. Support. Care Cancer 24, 2351–2357. doi: 10.1007/s00520-015-3042-9
Hagedoorn, M., Buunk, B. P., Kuijer, R. G., Wobbes, T., and Sanderman, R. (2000). Couples dealing with cancer: role and gender differences regarding psychological distress and quality of life. Psycho Oncol. 9, 232–242.
Hagedoorn, M., Sanderman, R., Bolks, H. N., Tuinstra, J., and Coyne, J. C. (2008). Distress in couples coping with cancer: a meta-analysis and critical review of role and gender effects. Psychol. Bull. 134, 1–30. doi: 10.1037/0033-2909
Hasson-Ohayon, I., Goldzweig, G., Braun, M., and Galinsky, D. (2010). Women with advanced breast cancer and their spouses: diversity of support and psychological distress. Psycho Oncol. 19, 1195–1204. doi: 10.1002/pon
Hinz, A., Mitchell, A. J., Dégi, C. L., and Mehnert-Theuerkauf, A. (2019). Normative values for the distress thermometer (DT) and the emotion thermometers (ET), derived from a German general population sample. Qual. Life Res. 28, 277–282. doi: 10.1007/s11136-018-2014-1
Hodges, L. J., Humphris, G. M., and Macfarlane, G. (2005). A meta-analytic investigati on of the relationship between the psychological distress of cancer patients and their carers. Soc. Sci. Med. 60, 1–12. doi: 10.1016/j.socscimed.2004.04.018
Kayser, K., Watson, L. E., and Andrade, J. T. (2007). Cancer as a “we-disease”: examining the process of coping from a relational perspective. Fam. Syst. Health 25, 404–418. doi: 10.1037/1091-7527.25.4.404
Lehmann, C., Koch, U., and Mehnert, A. (2012). Psychometric properties of the German version of the short-form supportive care needs survey questionnaire (SCNSSF34-G). Support. Care Cancer 20, 2415–2424. doi: 10.1007/s00520-011-1351-1
Lim, C. C., Devi, M. K., and Ang, E. (2011). Anxiety in women with breast cancer undergoing treatment: a systematic review. Int. J. Evid. Based Healthc. 9, 215–235. doi: 10.1111/j.1744-1609.2011.00221.x
Magsamen-Conrad, K., Checton, M. G., Venetis, M. K., and Greene, K. (2015). Communication efficacy and couples’ cancer management: applying a dyadic appraisal model. Commun. Monogr. 82, 179–200. doi: 10.1080/03637751.2014.971415
Mehnert, A., Müller, D., Lehmann, C., and Koch, U. (2006). Die deutsche version des NCCN distress-thermometers. Z. Psychiatr. Psychol. Psychother. 54, 213–223.
Merckaert, I., Libert, Y., Messin, S., Milani, M., Slachmuylder, J.-L., and Razavi, D. (2010). Cancer patients’ desire for psychological support: prevalence and implications for screening patients’ psychological needs. Psycho Oncol. 19, 141–149. doi: 10.1002/pon.1568
Mitchell, A. J., Baker-Glenn, E. A., Park, B., Granger, L., and Symonds, P. (2010). Can the distress thermometer be improved by additional mood domains? Part II. What is the optimal combination of emotion thermometers? Psychooncology 19, 134–140. doi: 10.1002/pon.1557
Mitchell, A. J., Chan, M., Bhatti, H., Halton, M., Grassi, L., Johansen, C., et al. (2011). Prevalence of depression, anxiety, and adjustment disorder in oncological, haematological, and palliative-care settings: a meta-analysis of 94 interview-based studies. Lancet Oncol. 12, 160–174. doi: 10.1016/S1470-2045(11)70002-X
Ng, C. G., Boks, M. P. M., Zainal, N. Z., and de Wit, N. J. (2011). The prevalence and pharmacotherapy of depression in cancer patients. J. Affect. Disord. 131, 1–7. doi: 10.1016/j.jad.2010.07.034
Northouse, L., Williams, A.-L., Given, B., and McCorkle, R. (2012). Psychosocial care for family caregivers of patients with cancer. J. Clin. Oncol. 30, 1227–1234. doi: 10.1200/jco.2011.39.5798
Oechsle, K., Goerth, K., Bokemeyer, C., and Mehnert, A. (2013a). Anxiety and depression in caregivers of terminally Ill cancer patients: impact on their perspective of the patients’ symptom burden. J. Palliative Med. 16, 1095–1101. doi: 10.1089/jpm.2013.0038
Oechsle, K., Goerth, K., Bokemeyer, C., and Mehnert, A. (2013b). Symptom burden in palliative care patients: perspectives of patients, their family caregivers, and their attending physicians. Support Care Cancer 21, 1955–1962. doi: 10.1007/s00520-013-1747-1
Osin, R., Pankrath, A.-L., Niederwieser, D., Döhner, H., Hönig, K., Vogelhuber, M., et al. (2018). Dyadisches Coping von hämatoonkologischen Patienten und ihren Partnern: Übereinstimmungsmaße und Zusammenhänge mit sozialer Unterstützung und psychischer Belastung. Psychother. Psychosom. Med. Psychol. 5, 55–65. doi: 10.1055/s-0043-110137
Pankrath, A.-L., Weißflog, G., Mehnert, A., Niederwieser, D., Döhner, H., Hönig, K., et al. (2018). The relation between dyadic coping and relationship satisfaction in couples dealing with haematological cancer. Eur. J. Cancer Care 27:e12595. doi: 10.1111/ecc.12595
Pitceathly, C., and Maguire, P. (2003). The psychological impact of cancer on patients’ partners and other key relatives: a review. Eur. J. Cancer 39, 1517–1524. doi: 10.1016/S0959-8049(03)00309-5
Regan, T. W., Lambert, S. D., Kelly, B., McElduff, P., Girgis, A., Kayser, K., et al. (2014). Cross-sectional relationships between dyadic coping and anxiety, depression, and relationship satisfaction for patients with prostate cancer and their spouses. Patient Educ. Couns. 96, 120–127. doi: 10.1016/j.pec.2014.04.010
Robbins, M. L., López, A. M., Weihs, K. L., and Mehl, M. R. (2014). Cancer conversations in context: naturalistic observation of couples coping with breast cancer. J. Fam. Psychol. 28, 380–390. doi: 10.1037/a0036458
Rosenberger, C., Höcker, A., Cartus, M., Schulz-Kindermann, F., Härter, M., and Mehnert, A. (2012). Angehörige und Patienten in der ambulanten psychoonkologischen Versorgung: zugangswege, psychische Belastungen und Unterstützungsbedürfnisse. Psychother. Psych. Med. 62, 185–194. doi: 10.1055/s-0032-1304994
Saita, E., Acquati, C., and Molgora, S. (2016). Promoting patient and caregiver engagement to care in cancer. Front. Psychol. 7:1660. doi: 10.3389/fpsyg.2016.01660
Sandgren, A. K., Mullens, A. B., Erickson, S. C., Romanek, K. M., and McCaul, K. D. (2004). Confidant and breast cancer patient reports of quality of life. Qual. Life Res. 13, 155–160. doi: 10.1023/b:qure.0000015287.90952.95
Schrank, B., Ebert-Vogel, A., Amering, M., Masel, E. K., Neubauer, M., Watzke, H., et al. (2016). Gender differences in caregiver burden and its determinants in family members of terminally ill cancer patients. Psycho Oncol. 25, 808–814. doi: 10.1002/pon.4005
Segrin, C. (2005). Dyadic interdependence on affect and quality-of-life trajectories among women with breast cancer and their partners. J. Soc. Pers. Relationsh. 22, 673–689. doi: 10.1177/0265407505056443
Segrin, C., and Badger, T. A. (2010). Psychological distress in different social network members of breast and prostate cancer survivors. Res. Nurs. Health 33, 450–464. doi: 10.1002/nur.20394
Segrin, C., Badger, T. A., Dorros, S. M., Meek, P., and Lopez, A. M. (2007). Interdependent anxiety and psychological distress in women with breast cancer and their partners. Psycho Oncol. 16, 634–643. doi: 10.1002/pon.1111
Silveira, M. J., Given, C. W., Given, B., Rosland, A. M., and Piette, J. D. (2010). Patient-caregiver concordance in symptom assessment and improvement in outcomes for patients undergoing cancer chemotherapy. Chron. Illn. 6, 46–56. doi: 10.1177/1742395309359208
Sklenarova, H., Krümpelmann, A., Haun, M. W., Friederich, H.-C., Huber, J., Thomas, M., et al. (2015). When do we need to care about the caregiver? Supportive care needs, anxiety, and depression among informal caregivers of patients with cancer and cancer survivors. Cancer 121, 1513–1519. doi: 10.1002/cncr.29223
Traa, M. J., De Vries, J., Bodenmann, G., and Den Oudsten, B. L. (2015). Dyadic coping and relationship functioning in couples coping with cancer: a systematic review. Br. J. Health Psychol. 20, 85–114. doi: 10.1111/bjhp.12094
Keywords: breast cancer, partner, distress, needs, psycho-oncology
Citation: Goerling U, Bergelt C, Müller V and Mehnert-Theuerkauf A (2020) Psychosocial Distress in Women With Breast Cancer and Their Partners and Its Impact on Supportive Care Needs in Partners. Front. Psychol. 11:564079. doi: 10.3389/fpsyg.2020.564079
Received: 20 May 2020; Accepted: 25 August 2020;
Published: 23 September 2020.
Edited by:
Chiara Acquati, University of Houston, United StatesReviewed by:
Emanuela Saita, Catholic University of the Sacred Heart, ItalyCopyright © 2020 Goerling, Bergelt, Müller and Mehnert-Theuerkauf. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Anja Mehnert-Theuerkauf, YW5qYS5tZWhuZXJ0QG1lZGl6aW4udW5pLWxlaXB6aWcuZGU=
†These authors have contributed equally to this work and share senior authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.