- 1Department of Psychology, “Sapienza University of Rome,” Rome, Italy
- 2Social Neuroscience Laboratory, IRCCS Fondazione Santa Lucia, Rome, Italy
Psoriasis is a chronic dermatological condition that is frequently associated with problematic patterns of emotional reactivity (the way in which patients react to stimuli), alexithymia (their ability to recognize and label the emotional reaction), and emotion regulation (the ability to enhance or reduce their own emotional reaction). A research in the peer-reviewed scientific literature was conducted in order to identify articles describing the association of psoriasis and affective problems. In particular, we first evaluate studies that have investigated abnormal emotional reactivity (in terms of duration, frequency, or type of the experienced emotions) and its impact on patients’ quality of life; next, we review the role of alexithymia and emotion regulation in modulating the relationship between emotional reactivity and quality of life in this population. From a critical analysis of the reviewed studies, we highlight that altered emotional processing might be particularly important in the characterization of this condition. In particular, we show that this condition is related to an emotional reactivity characterized by negative emotions that have a stronger impact on patients’ quality of life when emotion regulation abilities are weak, especially if patients have alexithymia. Finally, we present suggestions for future directions in both clinical and research fields.
Introduction
Psoriasis is a chronic inflammatory skin disease affecting approximately 2% of the population (Schmid-Ott et al., 2007) and characterized by cutaneous lesions that may appear on any part of the body. This condition can be very challenging and has such a strong impact on patients’ physical appearance in that embarrassment over appearance is rated as the most debilitating feature of the disease (Vardy et al., 2002). Psychological stress, in turn, has a negative impact on psoriasis symptoms leading to a self-perpetuating mechanism that might be difficult to interrupt (Basavaraj et al., 2011). In such a scenario, emotional reactivity (i.e., the emotional response provoked by the perception and the valuation of a given situation; Gross and Jazaieri, 2014) and emotion regulation (i.e., the ability to modify the perceived emotion in terms of its quality, intensity, or duration; Gross and Jazaieri, 2014) become particularly crucial. Importantly, the way in which we experience and regulate our emotions is strictly dependent on the ability to recognize and distinguish them from other bodily sensations (Chen et al., 2011), thus, deficit in such domain (i.e., alexithymia) can also worsen the affective experience of psoriasis patients.
In what follows, we provide a review of the literature tapping into emotional processing in psoriasis with the aim of characterizing it in terms of emotional reactivity, alexithymia, and emotion regulation. Even though these constructs can be correlated with each other, here, we highlight how their abnormal functioning is associated with different dermatological, psychological, or life quality outcomes. Finally, we discuss the implications for clinical practice and research.
Methods
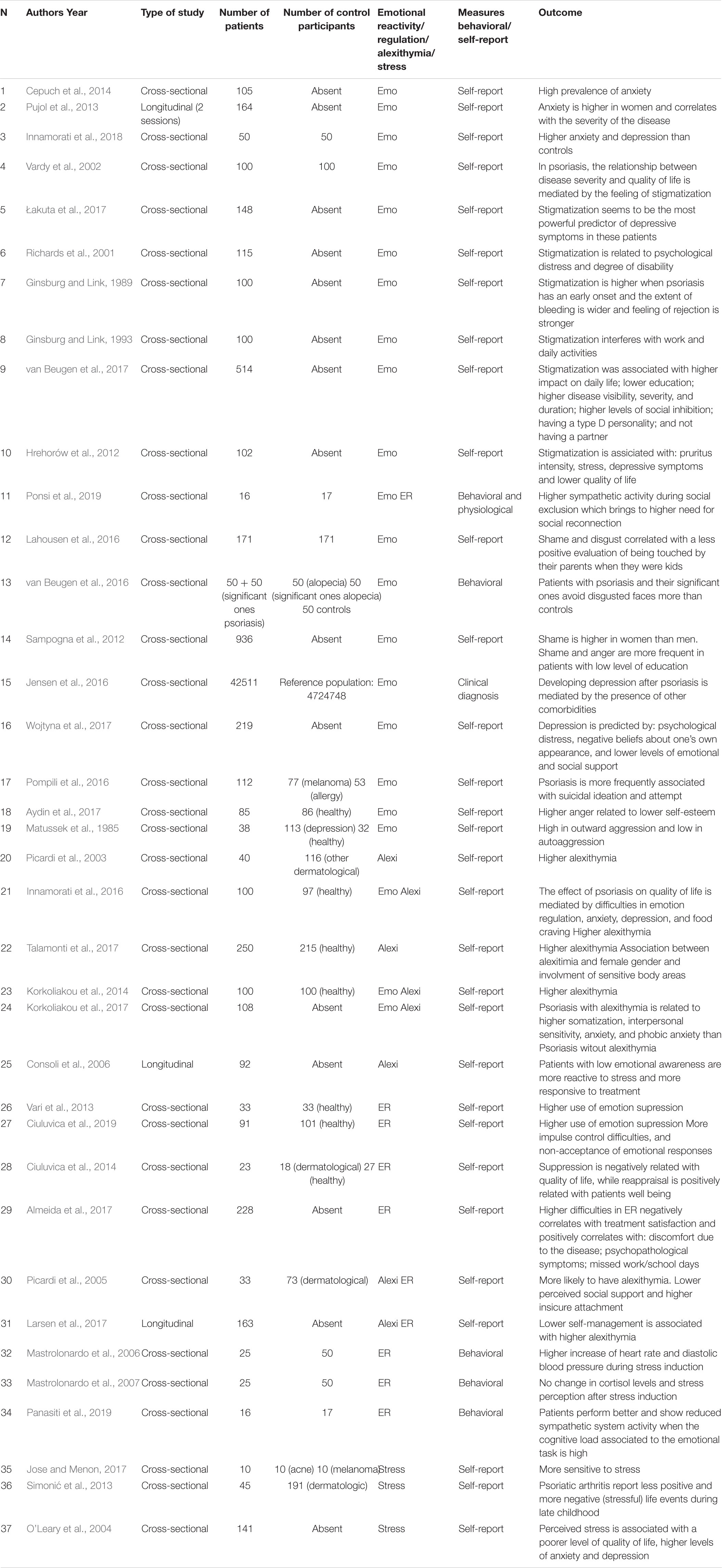
We conducted a search of PubMed’s database of articles containing the word “psoriasis” and one of the following terms: emotional reactivity, alexithymia, social exclusion, stigmatization, stress, anxiety, depression, and emotion regulation. Additional records were identified through manual searches of references of identified articles. Thirty-seven studies were selected (see Table 1).
Emotional Reactivity
Emotional reactivity is the constellation of behavioral and physiological changes triggered by the evaluation of a given situation in relation to one’s own active goals (Gross and Jazaieri, 2014). It can assume the form of a discrete emotion (i.e., an intense and short-lived response; Sander, 2013) or a feeling (i.e., the conscious experience of the emotion state; Tsuchiya and Adolphs, 2007), or it can be chronically altered in affective clinical disorders (i.e., fear in anxiety or sadness in depression). Pathological forms of emotional reactivity are typically characterized in terms of emotion intensity (e.g., emotional hyporeactivity), emotion duration (e.g., prolonged negative emotions), emotion frequency (e.g., frequent aggressive episodes), or emotion type (e.g., displaying inappropriate emotions) (Gross and Jazaieri, 2014). Psoriasis patients tend to experience a wide range of negative emotions that can be altered in several of these qualities (Sampogna et al., 2012). Below, we provide a detailed review of emotions (anger, disgust, and shame), feelings (stigmatization and social exclusion), and affective clinical disorders (anxiety and depression) that have been studied in relation to psoriasis.
Anxiety
Psoriasis is characterized by anxiety (i.e., the feeling of apprehension, uncertainty, and fear) as showed by the high prevalence of anxiety disorders (13.1%; Lamb et al., 2017) diagnosed in these patients (Cepuch et al., 2014; Fleming et al., 2017). Self-reported anxiety seems to be higher in women with psoriasis with respect to men and is positively correlated with the severity of the disease (Pujol et al., 2013). Recently, higher level of anxiety and depression has been found in these patients, even in a sample of psoriasis patients with cognitive deficits (Innamorati et al., 2018).
Stigmatization, Shame, and Disgust
Given its impact on patients’ physical appearance, psoriasis is often associated with a feeling of stigmatization, especially when it appears early in patients’ life (Schmid-Ott et al., 2007). Stigmatization is higher when the disease has an early onset and when the extent of bleeding and feeling of rejection are greater (Ginsburg and Link, 1989). It has been shown that high levels of stigmatization are caused by disease’s severity and, in turn, provoke a significant decrement of quality of life (Vardy et al., 2002). Moreover, stigmatization seems to (i) be the most powerful predictor of depressive symptoms in these patients (Hrehorów et al., 2012; Łakuta et al., 2017); (ii) be significantly related to psychological distress and degree of disability (Richards et al., 2001); and (iii) interfere with work and daily activities (Ginsburg and Link, 1993). Patients suffering from stigmatization tend not to have a partner, to have lower education, to have a higher level of social inhibition, to show a type D personality (van Beugen et al., 2017), to have higher stress and pruritus intensity, and to have lower quality of life (Hrehorów et al., 2012). In a recent study (Ponsi et al., 2019), we showed that in patients with psoriasis with respect to controls, higher sympathetic system activation during an experimental paradigm designed to induce the feeling of social exclusion (i.e., cyberball paradigm) was related to a higher need for social reconnection (i.e., the need to invest in new social interactions).
When chronic stigmatization is associated with an anxious ambivalent attachment style, dermatological patients’ view of themselves can be severely influenced, and they can manifest negative feelings of self-disgust (Jafferany and Patel, 2019). Psoriasis patients show higher sense of skin-related shame and disgust, which correlates with a less positive evaluation of being touched by their parents when they were kids (Lahousen et al., 2016). Interestingly, it has been shown that not only psoriasis patients but also their significant ones tend to avoid disgusted faces more than do controls (van Beugen et al., 2016). Shame—which is associated with the severity of psoriasis symptoms and also with depression and anxiety—seems to be higher in women than men, and it is more frequent in patients with a low level of education (Sampogna et al., 2012).
Depression
It has been shown that the risk of developing depression in psoriasis patients (prevalence of 9.9% of Major Depressive Disorder; Lamb et al., 2017) seems to be mediated by the presence of other comorbidities, except in younger patients with severe psoriasis where the presence of the disease directly predicts the onset of depression (Jensen et al., 2016). Psychological distress, negative beliefs about one’s own appearance, and lower levels of emotional and social support are factors that predispose to the development of depression in psoriasis (Wojtyna et al., 2017). Also, compared with patients with other dermatological conditions such as acne or alopecia areata, psoriasis patients show higher scores of depression, and suicidal ideation (Pompili et al., 2016).
Anger
It has been shown that in dermatologic conditions, aggression is associated with anxiety, and with a lower level of optimism and social support (Coneo et al., 2017). In psoriasis, anger (subclinical condition) frequency correlates with severity and length of the disease, and it is higher in patients with a low level of education (Sampogna et al., 2012). Psoriasis patients are characterized by a higher level of trait anger respect to controls; moreover, when they have low self-esteem, they show more anger toward people or objects and have enhanced difficulties in anger control (Aydin et al., 2017); conversely, they score very low in autoaggression (Matussek et al., 1985). Notably, however, one study reported that psoriasis patients exhibited fewer verbal aggression responses after anger-inducing procedures (Niemeier et al., 1999).
Alexithymia
Alexithymia is a subclinical trait defined by difficulties in the following: (i) identifying, describing, and communicating one’s own feelings; (ii) differentiating them from emotionally unrelated bodily sensations; (iii) emotional awareness related to psychosomatic symptoms; and (iv) imagination, daydreaming, and introspection (Martin and Pihl, 1985; Taylor et al., 1991). Crucially, identifying emotions is believed to be related to the ability to regulate them (Chen et al., 2011).
Neuroscientific evidence links alexithymia to (i) aberrant emotion processing (i.e., decreased activation of limbic structures in response to negative emotional stimuli and angry vs. neutral faces; Kano et al., 2003; Van der Velde et al., 2013; (ii) reduced gray matter volume in emotional processing brain areas (Xu et al., 2018); and (iii) reduced connectivity within the default mode network (DMN), in brain areas involved in emotional awareness and increased connectivity of the DMN with areas involved in sensory input and emotion control (Liemburg et al., 2012).
The association between alexithymia and various medical disorders suggests that it may represent a risk factor for their development, probably because it enhances stress responses through autonomic dysregulation (i.e., the alexithymia–stress hypothesis; Martin and Pihl, 1985). In particular, alexithymic people seem not to cope effectively with stressors because of a stress response that is typically altered in its cognitive (i.e., lack of emotional awareness), behavioral (i.e., maladaptive coping and lack of emotional expression), and physiological (i.e., increased arousal) components (Martin and Pihl, 1985). This altered response to stress might prolong the exposure to stressors and, on the long run, exacerbate the somatovisceral response (Martin and Pihl, 1985).
Also, alexithymia presents hypo-reactive physiological responses rather than hyper-reactive ones (Van der Velde et al., 2013) and seems to be associated with poorer interoception and the tendency to misattribute bodily signals (Palser et al., 2018). Misinterpretation of bodily sensations associated with negative emotions might be another mechanism through which alexithymia worsens clinical conditions (Lumley et al., 1996; Tuzer et al., 2011).
Alexithymia is often associated with psoriasis (Picardi et al., 2003, 2005; Innamorati et al., 2016) (prevalence of 24.8%, Sampogna et al., 2017), especially in women and in cases in which the plaques extend to sensitive body areas (like the face, the hands, or the genitals) (Talamonti et al., 2017). These patients show a higher level of somatization, interpersonal sensitivity, anxiety, and phobic anxiety respect to non-alexithymic patients (Korkoliakou et al., 2014, 2017). Some researchers suggested that alexithymia might be a condition that patients acquired in order to avoid dealing with unwanted emotions (Panayiotou et al., 2015). Consistently with this point of view, emotional awareness, an emotional skill distinct but often correlated to alexithymia, consisting in the ability to integrate and differentiate emotions, predicts better response to treatment in psoriasis patients (Consoli et al., 2006). The reported studies measured alexithymia using the Toronto Alexithymia Scale (TAS−20; Bagby et al., 1994).
Emotion Regulation
Emotion regulation is a multi-componential process that comprehends the implicit and explicit strategies through which we act on the emotional experience in order to enhance or reduce it (Gross and John, 2003). Maladaptive emotion regulation is a component of many psychopathological diseases such as depression (Ehring et al., 2010) and post-traumatic stress disorder (McLean and Foa, 2017).
Compared with controls, patients with psoriasis are characterized by higher use of emotional suppression (Vari et al., 2013; Ciuluvica et al., 2014, 2019), an emotion regulation strategy considered rather primitive that consists in inhibiting the expression of the ongoing emotional response once it has been generated (Gross and John, 2003). Interestingly, this is the same strategy used by recovered-depressed patients (Ehring et al., 2010). Conversely, higher use of reappraisal (Ciuluvica et al., 2014), an emotion regulation strategy that is more adaptive than suppression and consists in re-thinking the situation to alter its meaning and emotional impact (Gross and John, 2003), has shown to be positively related with patients’ well-being (Ciuluvica et al., 2014). In patients with psoriasis, higher difficulty in emotion regulation, as measured by the difficulty in emotion regulation strategies (DERS) scale, negatively correlates with treatment satisfaction and positively correlates with (i) the discomfort due to the disease; (ii) the number of reported psychopathological symptoms; and (iii) the frequency of missed work/school days (Almeida et al., 2017). Moreover, subtypes of psoriasis patients also show different patterns of emotion regulation: early-diagnosed patients have higher difficulties in behaving according to their goals when distressed (Almeida et al., 2017); obese patients with psoriasis show higher difficulties respect to obese patients without psoriasis (Innamorati et al., 2016). It has also been shown that the ability of impulse control (subclinical condition) when experiencing negative emotions is lower in this condition (Innamorati et al., 2016). Two subscales of the DERS, namely, emotional clarity and emotion acceptance, which are believed to measure concepts that are very close to alexithymia, also show higher scores among these patients (Innamorati et al., 2016). In agreement, in two recent studies, we showed that psoriasis patients scored higher than controls in the “Lack of Emotional Clarity” subscale of the DERS, indicating that patients have more difficulties than controls in correctly identifying their own emotions (Panasiti et al., 2019; Ponsi et al., 2019).
It has been hypothesized that low abilities in emotion regulation in psoriasis patients might increase the impact of poor social support on the severity of the disease (Picardi et al., 2005). Moreover, lower self-management, a psychological construct composed of medical management, role management, and emotional management, is associated with higher alexithymia in patients with moderate to severe psoriasis (Larsen et al., 2017).
It has to be noticed that most of the studies present in the scientific literature, at least to our knowledge, employed self-report measures or questionnaires. The lack of behavioral and physiological evidence regarding emotion regulation deficits in this population is crucial. Two studies reported some indirect measure by submitting patients to a standardized stressful procedure (mental arithmetic and the Stroop Color-Word Naming Test). They found higher heart rate and diastolic blood pressure in psoriasis patients (Mastrolonardo et al., 2006), which, however, was not accompanied by differences in stress perception or salivary cortisol levels (Mastrolonardo et al., 2007). Importantly, we recently showed that when presented with a working memory task with emotional distractors (i.e., the Emotional N-Back), psoriasis patients perform better and show reduced sympathetic system activity when the cognitive load associated with the task is high versus low and thus found it easier not to pay attention to the emotional distractors (Panasiti et al., 2019).
To sum up, the impact of emotion regulation abilities on the course of psoriasis seems crucial: patients’ well-being is negatively associated with suppression and is positively associated with reappraisal. Suppression and rumination are indeed more strongly linked to psychopathological outcomes than reappraisal and acceptance strategies (Kobylińska and Kusev, 2019). To our knowledge, there are no studies exploring the employment of acceptance strategies in psoriasis.
Stress Managing
The experience of stress can impact each of the three aspects of emotional processing that we mentioned in this review (i.e., emotional reactivity, alexithymia, and emotion regulation): (i) exposure to stressors is correlated to higher experience of negative emotions (Feldman et al., 1999); (ii) higher basal cortisol level during stress anticipation is associated with higher alexithymia (de Timary et al., 2008); and (iii) acute stress impairs emotion regulation during fear conditioning (Raio et al., 2013).
Stress managing is pivotal in psoriasis patients because impaired emotional processing could affect not only the response to stressful events but also the quality of the general emotional response in psoriasis. Patients with psoriasis are more sensitive to stress with respect to other dermatological conditions such as acne or melanoma (Jose and Menon, 2017), and patients with psoriatic arthritis report less positive and more negative (stressful) life events during late childhood (Simonić et al., 2013). Stressful events are indeed very often reported by patients as the cause of the appearance or the exacerbation of the disease (Griffiths and Richards, 2001). Perceived stress in patients is significantly associated with a poorer level of quality of life and higher levels of depression and anxiety (O’Leary et al., 2004) and might be associated with dermatological worsening of the plaques (Basavaraj et al., 2011).
Conclusion and Future Directions
From our review, it is apparent that emotional reactivity, alexithymia, and emotion regulation have a profound impact on the management of psoriasis symptoms. On the one hand, emotional reactivity in patients with psoriasis seems to be characterized by negative emotions such as anger (Matussek et al., 1985; Sampogna et al., 2012; Aydin et al., 2017), shame (Sampogna et al., 2012; Shah and Bewley, 2014; Lahousen et al., 2016), disgust (Lahousen et al., 2016), and feelings like social exclusion (Vardy et al., 2002; Schmid-Ott et al., 2007; Lahousen et al., 2016; van Beugen et al., 2017; Łakuta et al., 2017) and also by psychopathological disorders such as anxiety (Pujol et al., 2013; Cepuch et al., 2014; Fleming et al., 2017) and depression (Jensen et al., 2016). This emotional pattern seems to affect slightly more women (Sampogna et al., 2012; Pujol et al., 2013; Talamonti et al., 2017) than men and to be a risk factor for a wide range of negative outcomes spanning from lower quality of life (Vardy et al., 2002; O’Leary et al., 2004; Vari et al., 2013) to suicide (Pompili et al., 2016).
On the other hand, the ability to regulate emotions seems to be a protective factor that improves quality of life (Vari et al., 2013), treatment satisfaction, and the impact of negative emotions (Almeida et al., 2017). This is especially true when patients do not suffer from alexithymia. The effect of presence of alexithymia or low emotional awareness in these patients is not completely clear: on the one hand, it seems to help them in ignoring unwanted emotions (Panayiotou et al., 2015) and improve the treatment outcome (Consoli et al., 2006); on the other hand, it seems to worsen the impact of emotions on quality of life (Picardi et al., 2005; Almeida et al., 2017). From this literature review, it appears clear that treatments for psoriasis should also include techniques that address emotional reactivity, alexithymia, and emotion regulation because affective symptoms, together with dermatological ones, play a fundamental role in the resolution of this condition. One promising candidate would be the emotion regulation therapy (ERT), which is a manualized intervention that aims at (i) increasing emotional and motivational awareness; (ii) developing emotion regulation abilities; and (iii) generating new learning experiences (Renna et al., 2017).
Our review also highlights some limitations of the approaches that have been used so far for studying emotional processes in psoriasis. First of all, only few studies (Mastrolonardo et al., 2006, 2007; van Beugen et al., 2016; Panasiti et al., 2019; Ponsi et al., 2019) reported behavioral and physiological evidence. Although we acknowledge that self-report measures are important to understand the conscious evaluation that patients have of themselves, we also believe that implicit measures are crucial to understand what are the abilities that are truly compromised in these patients. Future studies should include these measurements and compare them with self-report measures in order to obtain a fine-grained picture of emotional processing in these patients. Second, many studies (15 of the 37 we reviewed) did not test a control group; this practice does not allow to disentangle whether what is observed is specific of this skin condition or is also true in the general population. Furthermore, very few studies tested a clinical control group with other dermatological conditions. Including such control groups would be very important to understand the altered psychological mechanisms behind psoriasis and to define efficient psychological treatments.
Author Contributions
All authors listed have made a substantial, direct and intellectual contribution to the work, and approved it for publication.
Funding
This study was supported by the BIAL Foundation Grant for Scientific Reserach (No. 276/18) awarded to GP.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
Almeida, V., Taveira, S., Teixeira, M., Almeida, I., Rocha, J., and Teixeira, A. (2017). Emotion regulation in patients with psoriasis: correlates of disability, clinical dimensions, and psychopathology symptoms. Int. J. Behav. Med. 24, 563–570. doi: 10.1007/s12529-016-9617-0
Aydin, E., Atis, G., Bolu, A., Aydin, C., Karabacak, E., Dogan, B., et al. (2017). Identification of anger and self-esteem in psoriasis patients in a consultation-liaison psychiatry setting: a case control study. Psychiatry Clin. Psychopharmacol. 27, 222–226. doi: 10.1080/24750573.2017.1326740
Bagby, R. M., Parker, J. D. A., and Taylor, G. J. (1994). The twenty-item toronto alexithymia scale–i: item selection and cross-validation of the factor structure. J. Psychosom. Res. 38, 23–32. doi: 10.1016/0022-3999(94)90005-1
Basavaraj, K. H., Navya, M. A., and Rashmi, R. (2011). Stress and quality of life in psoriasis: an update. Int. J. Dermatol. 50, 783–792. doi: 10.1111/j.1365-4632.2010.04844.x
Cepuch, G., Wojtas, K., Zych, B., and Matuszewska, B. (2014). Assessment of emotional state of psoriasis patients and the degree of acceptance of the disease. Fam. Med. Prim. Care Rev. 16, 85–87.
Chen, J., Xu, T., Jing, J., and Chan, R. C. (2011). Alexithymia and emotional regulation: a cluster analytical approach. BMC Psychiatry 11:33. doi: 10.1186/1471-244X-11-33
Ciuluvica, C., Amerio, P., and Fulcheri, M. (2014). Emotion regulation strategies and quality of life in dermatologic patients. Procedia Soc. Behav. Sci. 127, 661–665. doi: 10.1016/j.sbspro.2014.03.331
Ciuluvica, C., Fulcheri, M., and Amerio, P. (2019). Expressive suppression and negative affect, pathways of emotional dysregulation in psoriasis patients. Front. Psychol. 10:1970. doi: 10.3389/fpsyg.2019.01907
Coneo, A. M. C., Thompson, A. R., and Lavda, A. (2017). The influence of optimism, social support and anxiety on aggression in a sample of dermatology patients: an analysis of cross-sectional data. Br. J. Dermatol. 176, 1187–1194. doi: 10.1111/bjd.15115
Consoli, S. M., Rolhion, S., Martin, C., Ruel, K., Cambazard, F., Pellet, J., et al. (2006). Low levels of emotional awareness predict a better response to dermatological treatment in patients with psoriasis. Dermatology 212, 128–136. doi: 10.1159/000090653
de Timary, P., Roy, E., Luminet, O., Fillée, C., and Mikolajczak, M. (2008). Relationship between alexithymia, alexithymia factors and salivary cortisol in men exposed to a social stress test. Psychoneuroendocrinology 33, 1160–1164. doi: 10.1016/j.psyneuen.2008.06.005
Ehring, T., Tuschen-Caffier, B., Schnülle, J., Fischer, S., and Gross, J. J. (2010). Emotion regulation and vulnerability to depression: spontaneous versus instructed use of emotion suppression and reappraisal. Emotion 10, 563–572. doi: 10.1037/a0019010
Feldman, P. J., Cohen, S., Lepore, S. J., Matthews, K. A., Kamarck, T. W., and Marsland, A. L. (1999). Negative emotions and acute physiological responses to stress. Soc. Behav. Med. 21, 216–222. doi: 10.1007/BF02884836
Fleming, P., Bai, J. W., Pratt, M., Sibbald, C., Lynde, C., and Gulliver, W. P. (2017). The prevalence of anxiety in patients with psoriasis: a systematic review of observational studies and clinical trials. J. Eur. Acad. Dermatology Venereol. 31, 798–807. doi: 10.1111/jdv.13891
Ginsburg, I. H., and Link, B. G. (1989). Feelings of stigmatization in patients with psoriasis. J. Am. Acad. Dermatol. Acad. Dermatol. Venereol. 20, 53–62. doi: 10.1111/jdv.13748
Ginsburg, I. H., and Link, B. G. (1993). Psychosocial consequences of rejection and stigma feelings in psoriasis patients. Int. J. Dermatol. 32, 587–591. doi: 10.1111/j.1365-4362.1993.tb05031.x
Griffiths, C. E. M., and Richards, H. L. (2001). Psychological influences in psoriasis. Clin. Exp. Dermatol. 26, 338–342. doi: 10.1046/j.1365-2230.2001.00834.x
Gross, J. J., and Jazaieri, H. (2014). Emotion, emotion regulation, and psychopathology. Clin. Psychol. Sci. 2, 387–401. doi: 10.1177/2167702614536164
Gross, J. J., and John, O. P. (2003). Individual differences in two emotion regulation processes: implications for affect, relationships, and well-being. J. Pers. Soc. Psychol. 85, 348–362. doi: 10.1037/0022-3514.85.2.348
Hrehorów, E., Salomon, J., Matusiak, Ł, Reich, A., and Szepietowski, J. C. (2012). Patients with psoriasis feel stigmatized. Acta Derm. Venereol. 92, 67–72. doi: 10.2340/00015555-1193
Innamorati, M., Quinto, R. M., Imperatori, C., Lora, V., Graceffa, D., Fabbricatore, M., et al. (2016). Health-related quality of life and its association with alexithymia and difficulties in emotion regulation in patients with psoriasis. Compr. Psychiatry 70, 200–208. doi: 10.1016/j.comppsych.2016.08.001
Innamorati, M., Quinto, R. M., Lester, D., Iani, L., Graceffa, D., and Bonifati, C. (2018). Cognitive impairment in patients with psoriasis: a matched case-control study. J. Psychosom. Res. 105, 99–105. doi: 10.1016/j.jpsychores.2017.12.011
Jafferany, M., and Patel, A. (2019). Understanding psychocutaneous disease: psychosocial & psychoneuroimmunologic perspectives. Int. J. Dermatol 59, 8–15. doi: 10.1111/ijd.14629
Jensen, P., Ahlehoff, O., Egeberg, A., Gislason, G., Hansen, P. R., and Skov, L. (2016). Psoriasis and new-onset depression: a danish nationwide cohort study. Acta Derm. Venereol. 96, 39–42. doi: 10.2340/00015555-2183
Jose, M. R., and Menon, S. B. (2017). Cognitive emotional regulation, perceived stress and psychological general well-being in patients with skin diseases?: a comparative study. Int. J. Indian Psychol. 4, 5–19. doi: 10.25215/0404.002
Kano, M., Fukudo, S., Gyoba, J., Kamachi, M., Tagawa, M., Mochizuki, H., et al. (2003). Specific brain processing of facial expressions in people with alexithymia: an H215O-PET study. Brain 126, 1474–1484. doi: 10.1093/brain/awg131
Kobylińska, D., and Kusev, P. (2019). Flexible emotion regulation: how situational demands and individual differences influence the effectiveness of regulatory strategies. Front. Psychol. 10:72. doi: 10.3389/fpsyg.2019.00072
Korkoliakou, P., Christodoulou, C., Kouris, A., Porichi, E., Efstathiou, V., Kaloudi, E., et al. (2014). Alexithymia, anxiety and depression in patients with psoriasis: a case–control study. Ann. Gen. Psychiatry 13:38. doi: 10.1186/s12991-014-0038-7
Korkoliakou, P., Efstathiou, V., Giannopoulou, I., Christodoulou, C., Kouris, A., Rigopoulos, D., et al. (2017). Psychopathology and alexithymia in patients with psoriasis. An. Bras. Dermatol. 92, 510–515. doi: 10.1590/abd1806-4841.20175660
Lahousen, T., Kupfer, J., Gieler, U., Hofer, A., Linder, M. D., and Schut, C. (2016). Differences between psoriasis patients and skin-healthy controls concerning appraisal of touching, shame and disgust. Acta Derm. Venereol. 96, 78–82. doi: 10.2340/00015555-2373
Łakuta, P., Marcinkiewicz, K., Bergler-Czop, B., and Brzezinska-Wcisło, L. (2017). How does stigma affect people with psoriasis? Postep. Dermatol. Alergol. 34, 36–41. doi: 10.5114/pdia.2016.62286
Lamb, R. C., Matcham, F., Turner, M. A., Rayner, L., Simpson, A., Hotopf, M., et al. (2017). Screening for anxiety and depression in people with psoriasis: a cross-sectional study in a tertiary referral setting. Br. J. Dermatol. 176, 1028–1034. doi: 10.1111/bjd.14833
Larsen, M. H., Krogstad, A. L., and Wahl, A. K. (2017). Alexithymia, illness perception and self-management competency in psoriasis. Acta Derm. Venereol. 97, 934–940. doi: 10.2340/00015555-2707
Liemburg, E. J., Swart, M., Bruggeman, R., Kortekaas, R., Knegtering, H., Ćurèić-Blake, B., et al. (2012). Altered resting state connectivity of the default mode network in alexithymia. Soc. Cogn. Affect. Neurosci. 7, 660–666. doi: 10.1093/scan/nss048
Lumley, M. A., Stettner, L., and Wehmer, F. (1996). How are alexithymia and physical illness linked? A review and critique of pathways. J. Psychosom. Res. 41, 505–518. doi: 10.1016/S0022-3999(96)00222-X
Martin, J. B., and Pihl, R. O. (1985). The stress-alexithymia hypothesis: theorectical and empirical considerations. Psychother. Psychosom. 43, 169–176. doi: 10.1159/000287876
Mastrolonardo, M., Alicino, D., Zefferino, R., Pasquini, P., and Picardi, A. (2007). Effect of psychological stress on salivary interleukin-1 b in psoriasis. Arch. Med. Res. 38, 206–211. doi: 10.1016/j.arcmed.2006.09.009
Mastrolonardo, M., Picardi, A., Alicino, D., Bellomo, A., and Pasquini, P. (2006). Cardiovascular reactivity to experimental stress in psoriasis?: a controlled investigation. Acta Derm. Venereol. 86, 340–344. doi: 10.2340/00015555-0099
Matussek, P., Agerer, D., and Seibt, G. (1985). Aggression in depressives and psoriatics. Psychother. Psychosom. 43, 120–125. doi: 10.1159/000287868
McLean, C. P., and Foa, E. B. (2017). Emotions and emotion regulation in posttraumatic stress disorder. Curr. Opin. Psychol. 14, 72–77. doi: 10.1016/j.copsyc.2016.10.006
Niemeier, V., Fritz, J., Kupfer, J., and Gieler, U. (1999). Aggressive verbal behaviour as a function of experimentally induced anger in persons with psoriasis. Eur. J. Dermatol. 9, 555–558.
O’Leary, C. J., Creamer, D., Higgins, E., and Weinman, J. (2004). Perceived stress, stress attributions and psychological distress in psoriasis. J. Psychosom. Res. 57, 465–471. doi: 10.1016/j.jpsychores.2004.03.012
Palser, E. R., Palmer, C. E., Galvez-Pol, A., Hannah, R., Fotopoulou, A., and Kilner, J. M. (2018). Alexithymia mediates the relationship between interoceptive sensibility and anxiety. PLoS One 13:e0203212. doi: 10.1371/journal.pone.0203212
Panasiti, M. S., Ponsi, G., Monachesi, B., Lorenzini, L., Panasiti, V., and Aglioti, S. M. (2019). Cognitive load and emotional processing in psoriasis: a thermal imaging study. Exp. Brain Res. 237, 211–222. doi: 10.1007/s00221-018-5416-y
Panayiotou, G., Leonidou, C., Constantinou, E., Hart, J., Rinehart, K. L., Sy, J. T., et al. (2015). Do alexithymic individuals avoid their feelings? Experiential avoidance mediates the association between alexithymia, psychosomatic, and depressive symptoms in a community and a clinical sample. Compr. Psychiatry 56, 206–216. doi: 10.1016/j.comppsych.2014.09.006
Picardi, A., Mazzotti, E., Gaetano, P., Cattaruzza, M. S., Baliva, G., Melchi, C. F., et al. (2005). Stress, social support, emotional regulation, and exacerbation of diffuse plaque psoriasis. Psychosomatics 46, 556–564. doi: 10.1176/appi.psy.46.6.556
Picardi, A., Pasquini, P., Sofia, M., Gaetano, P., Baliva, G., Franco, C., et al. (2003). Only limited support for a role of psychosomatic factors in psoriasis. Results from a case-control study. J. Psychosom. Res. 55, 189–196. doi: 10.1016/S0022-3999(02)00574-3
Pompili, M., Innamorati, M., Erbuto, D., and Costanzo, A. (2016). Psychiatric comorbidity and suicide risk in patients with psoriasis. Eur. Psychiatry 33, S395–S396. doi: 10.1016/j.eurpsy.2016.01.1421
Ponsi, G., Monachesi, B., Panasiti, V., Aglioti, S. M., and Panasiti, M. S. (2019). Physiological and behavioral reactivity to social exclusion: a functional infrared thermal imaging study in patients with psoriasis. J. Neurophysiol. 121, 38–49. doi: 10.1152/jn.00555.2018
Pujol, R. M., Puig, L., Daudén, E., Sánchez-Carazo, J. L., Toribio, J., Vanaclocha, F., et al. (2013). Mental health self-assessment in patients with moderate to severe psoriasis: an observational, multicenter study of 1164 patients in Spain (The VACAP study). Actas Dermosifiliogr 104, 897–903. doi: 10.1016/j.ad.2013.04.014
Raio, C. M., Orederu, T. A., Palazzolo, L., Shurick, A. A., and Phelps, E. A. (2013). Cognitive emotion regulation fails the stress test. Proc. Natl. Acad. Sci. U.S.A. 110, 15139–15144. doi: 10.1073/pnas.1305706110
Renna, M. E., Quintero, J. M., Fresco, D. M., and Mennin, D. S. (2017). Emotion regulation therapy: a mechanism-targeted treatment for disorders of distress. Front. Psychol. 8:98. doi: 10.3389/fpsyg.2017.00098
Richards, H. L., Fortune, D. G., Griffiths, C. E. M., and Main, C. J. (2001). The contribution of perceptions of psoriasis to disability in patients with psoriasis. J. Psychosom. Res. 50, 11–15. doi: 10.1348/014466502163949
Sampogna, F., Puig, L., Spuls, P., Girolomoni, G., Radtke, M. A., Kirby, B., et al. (2017). Prevalence of alexithymia in patients with psoriasis and its association with disease burden: a multicentre observational study. Br. J. Dermatol. 176, 1195–1203. doi: 10.1111/bjd.15243
Sampogna, F., Tabolli, S., and Abeni, D. (2012). Living with psoriasis: Prevalence of shame, anger, worry, and problems in daily activities and social life. Acta Derm. Venereol. 92, 299–303. doi: 10.2340/00015555-1273
Sander, D. (2013). “Models of emotion: the affective neuroscience approach,” in The Cambridge Handbook of Human Affective Neuroscience, eds J. Armony and P. Vuilleumier (Cambridge: Cambridge University Press), 5–53.
Schmid-Ott, G., Schallmayer, S., and Calliess, I. T. (2007). Quality of life in patients with psoriasis and psoriasis arthritis with a special focus on stigmatization experience. Clin. Dermatol. 25, 547–554. doi: 10.1016/j.clindermatol.2007.08.008
Shah, R., and Bewley, A. (2014). Psoriasis: “The badge of shame”. A case report of a psychological intervention to reduce and potentially clear chronic skin disease. Clin. Exp. Dermatol. 39, 600–603. doi: 10.1111/ced.12339
Simonić, E., Peternel, S., Stojnić-Soša, L., Ronèević-Gržeta, I., Prpić-Massari, L., Massari, D., et al. (2013). Negative and positive life experiences in patients with psoriatic arthritis. Rheumatol. Int. 33, 1587–1593. doi: 10.1007/s00296-012-2569-z
Talamonti, M., Galluzzo, M., Servoli, S., D’Adamio, S., and Bianchi, L. (2017). Alexithymia and plaque psoriasis: preliminary investigation in a clinical sample of 250 Patients. Dermatology 232, 648–654. doi: 10.1159/000453661
Taylor, G. J., Michael Bagby, R., and Parker, J. D. A. (1991). The alexithymia construct: a potential paradigm for psychosomatic medicine. Psychosomatics 32, 153–164. doi: 10.1016/S0033-3182(91)72086-0
Tsuchiya, N., and Adolphs, R. (2007). Emotion and consciousness. Trends Cogn. Sci. 11, 158–167. doi: 10.1016/j.tics.2007.01.005
Tuzer, V., Bulut, S. D., Bastug, B., Kayalar, G., GöKa, E., and BeStepe, E. (2011). Causal attributions and alexithymia in female patients with fibromyalgia or chronic low back pain. Nord. J. Psychiatry 65, 138–144. doi: 10.3109/08039488.2010.522596
van Beugen, S., Maas, J., van Laarhoven, A. I. M., Galesloot, T. E., Rinck, M., Becker, E. S., et al. (2016). Implicit stigmatization-related biases in individuals with skin conditions and their significant others. Heal. Psychol. 35, 861–865. doi: 10.1037/hea0000404.supp
van Beugen, S., van Middendorp, H., Ferwerda, M., Smit, J. V., Zeeuwen-Franssen, M. E. J., Kroft, E. B. M., et al. (2017). Predictors of perceived stigmatization in patients with psoriasis. Br. J. Dermatol. 176, 687–694. doi: 10.1111/bjd.14875
Van der Velde, J., Servaas, M. N., Goerlich, K. S., Bruggeman, R., Horton, P., Costafreda, S. G., et al. (2013). Neural correlates of alexithymia: a meta-analysis of emotion processing studies. Neurosci. Biobehav. Rev. 37, 1774–1785. doi: 10.1016/j.neubiorev.2013.07.008
Vardy, D., Besser, A., Amir, M., Gesthalter, B., Biton, A., and Buskila, D. (2002). Experiences of stigmatization play a role in mediating the impact of disease severity on quality of life in psoriasis patients. Br. J. Dermatol. 147, 736–742. doi: 10.1046/j.1365-2133.2002.04899.x
Vari, C., Velotti, P., Zavattini, G. C., Richetta, A. G., and Calvieri, S. (2013). Emotion regulation strategies in patients with psoriasis. J. Psychosom. Res. 74:560. doi: 10.1016/j.jpsychores.2013.03.084
Wojtyna, E., Łakuta, P., Marcinkiewicz, K., Bergler-Czop, B., and Brzezińska-Wcisło, L. (2017). Gender, body image and social support: biopsychosocial deter-minants of depression among patients with psoriasis. Acta Derm. Venereol. 97, 91–97. doi: 10.2340/00015555-2483
Keywords: psoriasis, emotional reactivity, alexithymia, emotion regulation, stress
Citation: Panasiti MS, Ponsi G and Violani C (2020) Emotions, Alexithymia, and Emotion Regulation in Patients With Psoriasis. Front. Psychol. 11:836. doi: 10.3389/fpsyg.2020.00836
Received: 11 January 2020; Accepted: 06 April 2020;
Published: 19 May 2020.
Edited by:
Nils Kohn, Radboud University Nijmegen, NetherlandsReviewed by:
Katharina Sophia Goerlich, University Medical Center Groningen, NetherlandsGeorgia Panayiotou, University of Cyprus, Cyprus
Copyright © 2020 Panasiti, Ponsi and Violani. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Maria Serena Panasiti, bWFyaWFzZXJlbmEucGFuYXNpdGlAdW5pcm9tYTEuaXQ=
 Maria Serena Panasiti
Maria Serena Panasiti Giorgia Ponsi
Giorgia Ponsi Cristiano Violani
Cristiano Violani