- 1Department of Personality, Assessment and Psychological Treatments, Faculty of Psychology, University of Valencia, Valencia, Spain
- 2Department of Methodology of the Social Sciences, Faculty of Psychology, University of Valencia, Valencia, Spain
Background: Patients at the end of life and their families experience a strong emotional impact. The well-being of these patients and that of their family caregiver are related.
Aim: To study the variables related with the emotional well-being of patients with and without cognitive impairment at the end of life and that of their primary family caregivers.
Design: Cross- sectional study.
Participants: Data was collected from 202 patients at the end of life with different diagnosis (COPD, cancer, and frail elderly) as well as from their respective 202 primary family caregivers.
Results: Structural equation models indicated that the emotional state of the patients was best predicted by their functional independence and the burden of their family caregivers. In addition, the emotional state of the primary family caregiver was predicted by their burden and not by the cognitive state or the functional independence of the patient. Nevertheless, the burden of the family caregiver, which is the only variable predicting both the emotional state of the patient and that of the caregiver, was directly related with the functional independence of the patient and indirectly with the patient’s cognitive state.
Conclusion: The family caregiver’s burden is an important factor to take into consideration when aiming to reduce the emotional distress of patients at the end of life with different diagnosis -whether or not they present significant cognitive impairment- and that of their family caregivers.
Introduction
The World Health Organization defines palliative care as “an approach that improves the quality of life of patients and their families facing the problem associated with life-threatening illness, through the prevention and relief of suffering by means of early identification and impeccable assessment and treatment of pain and other problems, physical, psychosocial, and spiritual” (Who, 2005).
The physical aspects of discomfort and suffering have been extensively studied in the context of palliative care (Cherny et al., 2015). In this context, it has also been highlighted the importance of the psychological and social aspects of suffering, when aiming to reduce the distress of these patients and that of their families (Cassell, 1998; Callahan, 2000; Who, 2005; Bennett and Shepherd, 2013; Grassi et al., 2015; Cipolletta et al., 2016, 2017; Fu et al., 2017).
The accurate assessment of needs is of capital importance in order to fulfill one of the main objectives of palliative care: the reduction of suffering of patients and their families (Sepúlveda et al., 2002). These needs have been considerably studied in the last 20 years, and based on these studies specific assessment instruments have been developed (Davis et al., 2016; Soto-Rubio A.L. et al., 2017). Nevertheless, the assessment of needs can be particularly challenging when the patient is no longer able to communicate (Sampson et al., 2006, 2015). Often, in end-of-life situations, the patient is unable to communicate because of fatigue, weakness, and a reduced level of awareness due to drugs to alleviate pain (Herr et al., 2006). At the same time, the advanced stage of some pathologies is associated to cognitive impairment (Liszewski et al., 2004; Cysique et al., 2006; Green, 2006; Pandharipande et al., 2013; Cosgrove and Alty, 2018). The severe physical and cognitive impairment of many patients hampers the assessment and treatment of their psychological needs (Sampson et al., 2006; Davis et al., 2016), especially those related to their emotional well-being.
Despite the obstacles to communication that may arise in end-of-life situations, the emotional well-being of the patients must be safeguarded (Oczkowski et al., 2016). In cases where the patient presents difficulties communicating verbally, there are behavioral parameters that can be observed and registered in order to assess the patient’s level of comfort/discomfort, such as facial expressions and posture and body language (Soto-Rubio A.L. et al., 2017). The European Association for Palliative Care recommends for these cases the use of observational scales (Sampson et al., 2015).
The strong emotional impact experienced by patients at the end of life and their families has been widely described in previous research (Baum et al., 2001; Pessin et al., 2002; Barreto and Martínez, 2003; Krikorian et al., 2012). Several studies address the needs of these families: social, physical, spiritual, emotional, and financial (Given et al., 2012; Chochinov et al., 2016; Fombuena et al., 2016). The emotional distress of the family caregivers in this context is characterized by symptoms of anxiety and depression (Toseland et al., 1995; Raveis et al., 1998, 2000; Sherwood et al., 2005; Northouse et al., 2012).
Also, the caring tasks and the restrictions that come with them usually cause discomfort in the caregiver (Buhse, 2008), which can lead to caregiver burden: a multidimensional response to psychological, physical, social, and financial stressors related to the caregiving experience (Zarit et al., 1980).
Previous research in the context of palliative care has provided evidence supporting a relationship between the patient’s emotional state and that of their family caregiver (Hodges et al., 2005; Bishop et al., 2007; Segrin et al., 2007; Hagedoorn et al., 2008). For this reason, it is of great importance to study the specific way in which the emotional state of these patients and that of their family caregivers are related, taking into consideration the possible influence that the cognitive state of the patient may be having. Moreover, this relationship should be taken into consideration in the design and implementation of interventions that aim to reduce the suffering of patients and families in the end-of-life context.
The present study aims to study the variables related with the emotional well-being of patients with and without cognitive impairment at the end of life and that of their primary family caregivers. More specifically, it analyses the relationships among the cognitive state, functional independence and emotional state of the patient, and the burden and emotional state of the primary family caregiver.
Materials and Methods
Sample
All data was collected between September 2015 and September 2016. Cross- sectional data was collected from 202 patients at the end of life as well as from their respective 202 primary family caregivers. The age of the patients ranged from 43 to 99 years (M = 76.46 years; SD = 9.850), and 68.8% were men. The age of the family caregivers ranged from 22 to 92 years (M = 61.46 years; SD = 13.521), and 22.8% were men.
All patients were being attended in a Palliative Care Unit at the moment of assessment. The patients’ inclusion criteria were:
- Being judged by the medical team to be in an end-of-life situation, in accordance with the criteria established by the Spanish Society of Palliative Care (Sociedad Española de Cuidados Paliativos [SECPAL], 2018).
- The main diagnosis included at least one of the following: chronic obstructive pulmonary disease (COPD), cancer or frail elderly.
The family caregivers’ inclusion criterion was:
- To be the primary family caregiver of a patient participating in the study. In the present study, family caregiver is defined as “the member of the family that assume the main tasks of caregiving, and take care of the patient most of time, or during a longer time than other members of the family.”
The exclusion criterion for the family caregivers was to present cognitive decline.
Data was collected through an interview that took place the first week of admission in the palliative care unit of one of the hospitals participating in the study. All participants from the study signed an informed consent, in accordance with the Declaration of Helsinki. In the cases where the patients presented cognitive impairment, it was their legal tutor who signed an informed consent. The assessment protocol was approved by the Ethics Committee of the University of Valencia (H1385291905651).
Measures
Data about socio-demographic features from patients and family caregivers (e.g., age, gender, marital status, education, kinship between patient, and family caregiver) was registered. Also, information on the following aspects was collected.
Functional Independence of the Patient
This variable was assessed using the Barthel’s scale (Mahoney and Barthel, 1965), adapted to Spanish population (Baztán et al., 1993). The scores for this scale range from 0 to 100 (0 to 90 in case of wheelchair bound people), providing five levels of dependency (Mahoney and Barthel, 1965).
Cognitive State of the Patient
To assess this variable, it was used the Short Portable Mental Status Questionnaire (SPMSQ) (Pfeiffer, 1975) validated for Spanish population (Martínez et al., 2001). It is a 10 items questionnaire. Its total score range from 0 to 10. In the present study, a score ≤ 5 is rated as “non-significant cognitive impairment,” and a score > 5 is rated as “significant cognitive impairment” (the cut-off point is 6 instead of 5 for people with no elementary studies).
Emotional State of the Patient (ESP)
In order to assess the emotional state of the patient, the following tools were used: Hospital Anxiety and Depression Scale (HADS) (Zigmond and Snaith, 1983) adapted to Spanish population (Tejero et al., 1986): this questionnaire was used in patients without significant cognitive impairment to assess their emotional state (ESP). It includes 14 items that assess the main emotional and cognitive indicators of anxiety and depression. The total score ranges from 0 to 42. It provides two categories of global emotional state: <21 = absence of clinically significant emotional distress, >20 = presence of clinically significant emotional distress. In this study we will refer to this variable as ESP-HADS.
Discomfort Observation Scale (DOS) (Soto-Rubio A.L. et al., 2017): this scale was used to assess the emotional state (ESP) in patients with significant cognitive impairment. It presents nine items, each one describing a behavioral indicator whether of distress or of well-being. The scale is filled by a member of the medical staff of the palliative care unit, marking the presence or absence of each behavioral indicator. It offers scores from 0 to 9, higher scores meaning higher levels of discomfort. A score lower than 5 rates as a low level of discomfort, whereas a score equal or higher than 5 rates as a high level of discomfort. In this study we will refer to this variable as ESP-DOS.
Emotional State of the Primary Family Caregiver (ESF)
To assess this variable, it was used the HADS already described in this article. We will refer to this variable as ESF-HADS.
Burden of the Primary Family Caregiver
The Caregiver’s Burden Scale (Zarit et al., 1980): this scale contains 22 items rated on a five-point Likert scale, from 0 (“never”) to 4 (“nearly always”). It offers scores from 22 to 110, higher scores reflecting greater burden, and it is suitable for different populations (Hébert et al., 2000). It offers three levels of burden taking into account the total score: 22–46 = no burden, 47–55 = light burden, 56–110 = intense burden.
Statistical Analyses
Zero-order correlations have been calculated in SPSS 24. Correlation comparisons were also calculated between the two samples. Several structural equation models have been estimated and tested in Mplus 7.0 (Muthén and Muthén, 1998–2011). The structural model has been tested simultaneously in a multigroup routine in patients with and without significant cognitive impairment. The measurement invariance models are nested and their relative plausibility (fit) must be assessed. The plausibility of the structural models was assessed using: (a) the chi-square statistic (Kline, 2015); (b) the comparative fit index (CFI) of more than 0.90 (Bentler, 1990) (and, ideally, greater than 0.95) (Hu and Bentler, 1999); (c) Akaike Information Criterion (AIC) to compare models, with lower values indicating better fit; and (d) the root-mean-squared error of approximation (RMSEA) of 0.08 or less (and, ideally less, than 0.05) (Hu and Bentler, 1999). Nested models, as the ones in the invariance routine, can be compared with two rationales (Little, 1997): the statistical and the modeling one. The statistical rationale compares the chi-squares of the alternative models, with non-significant values suggesting multi-group equivalence or invariance. However, this statistical approach has been usually combined with the comparison of fit indices (Cheung and Rensvold, 2002). This practical or modeling approach, advocated among others by Little (1997), states that if a parsimonious model (such as the ones that posit invariance) evinces adequate levels of practical fit, then the sets of equivalences are considered a reasonable approximation to the data. Practical fit is usually determined with CFI differences. CFI differences lower than 0.01 (Cheung and Rensvold, 2002) or 0.05 (Little, 1997) are usually employed as cut-off criteria.
Results
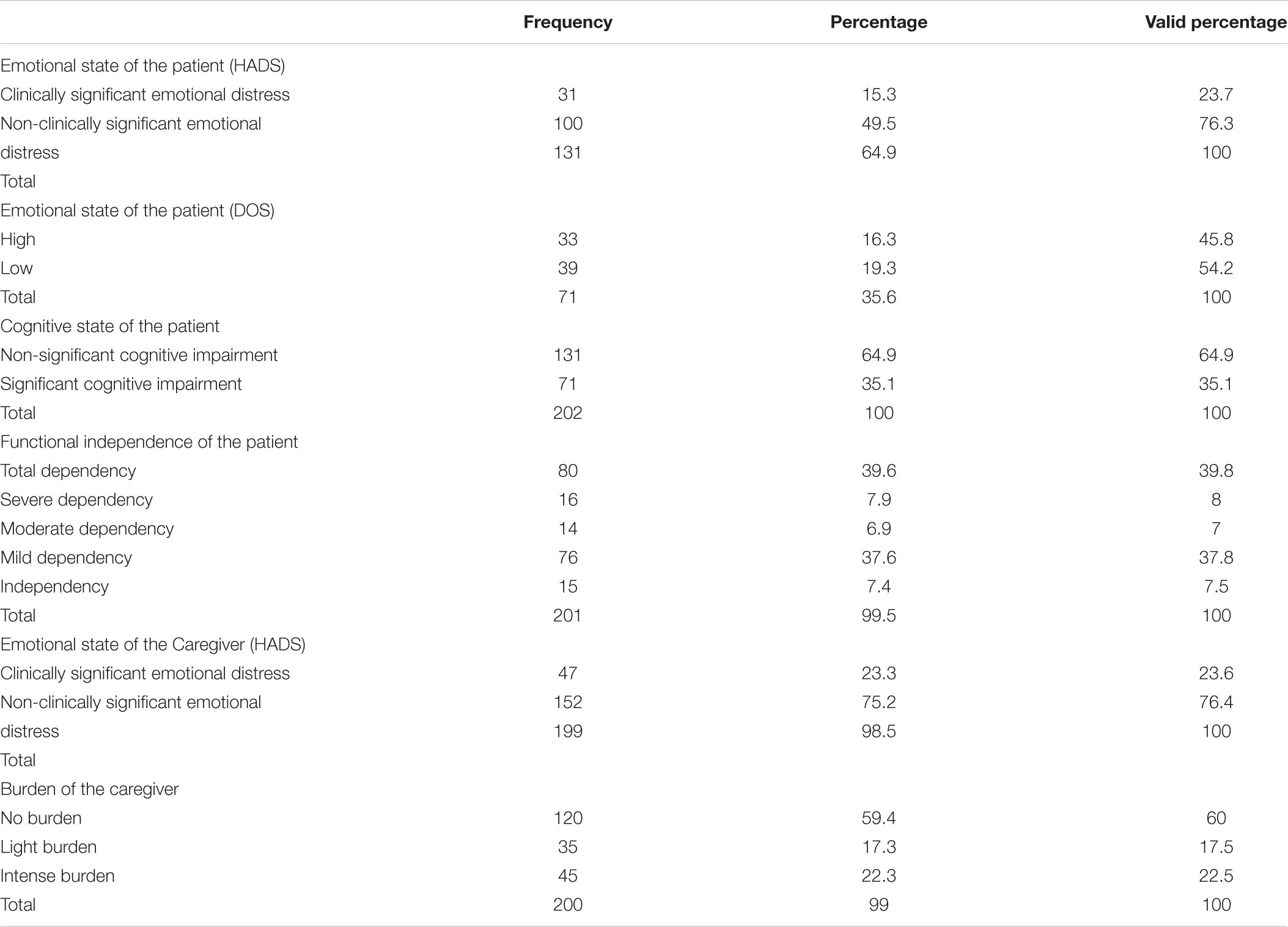
Descriptive statistics for variables of cognitive state, functional independence, and emotional state of the patient, as well as burden and emotional state of the primary family caregiver are presented in Table 1.
Correlations
We undertook preliminary correlational analyses to test if the correlation between the burden of the primary family caregiver and the emotional state of the patient was of the same direction and magnitude when estimated in patients with and without significant cognitive impairment. That is, the zero-order correlation between the emotional state of the patient and the burden of the family caregiver was estimated for patients without cognitive impairment (r = 0.23, p = 0.007), and for patients with cognitive impairment (r = 0.29, p = 0.005), and both correlations were statistically significant and positive. Then, both correlations were compared to test the null hypothesis of equal correlation, and this analysis was not statistically significant (z = -0.41, p > 0.05). Therefore, there is no evidence that the positive relationship between the emotional state of patient and the burden of the caregiver is different due to the change in the instrument used to measure patients’ emotional state.
Structural Models
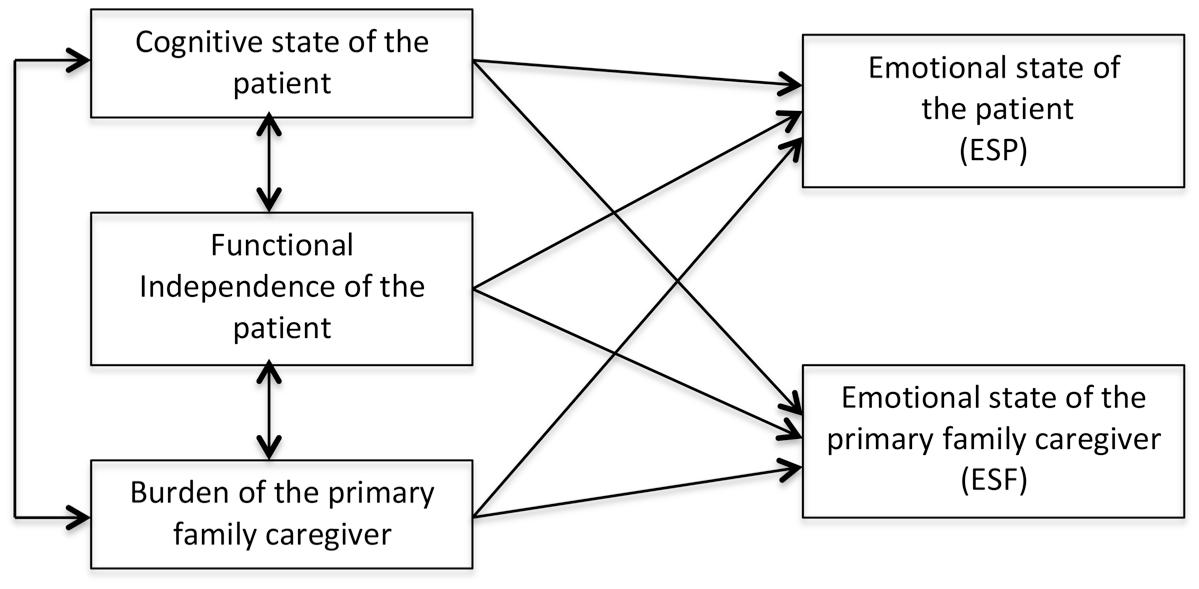
An a priori structural model was specified to relate the variables of interest (Figure 1). This model was tested in the sample of patients without cognitive impairment, the largest one, and fitted the data reasonably well [χ2(1) = 2.59, p = 0.10. CFI = 0.979, RMSEA = 0.112, 90% CI(0.000, -0.289), and AIC = 0.594]. However, this model is not parsimonious enough as the RMSEA shows and some relations were not statistically significant.
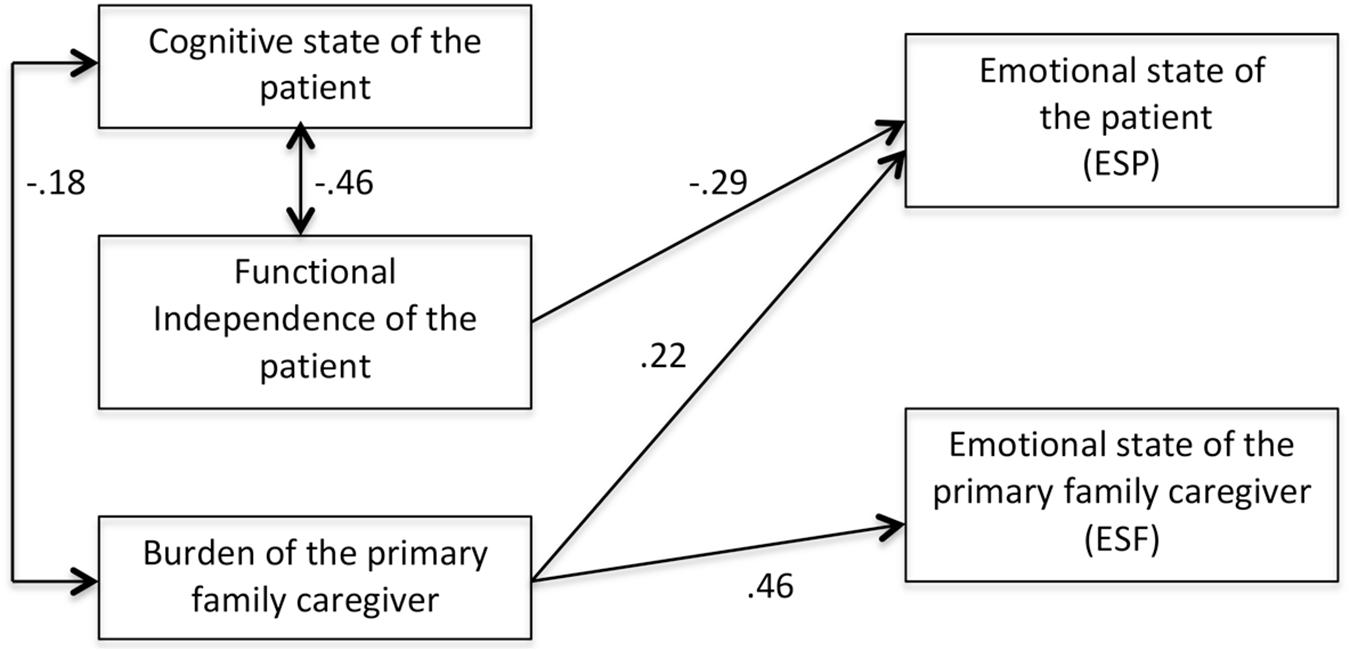
We removed the statistically non-significant relations and tested this new, more parsimonious, model. This model fitted the data very well: χ2(5) = 6.39, p = 0.26. CFI = 0.981, RMSEA = 0.047, 90% CI(0.000, -0.138), and AIC = -3.60. Moreover, a statistical comparison of both models showed no statistically significant differences [χ2(4) = 3.81, p = 0.43], the AIC for the more parsimonious model was lower than the AIC for the initial model and the CFI improved in the re-specified model. Accordingly, we decided to retain this model (Figure 2) as the best fitting model. This new, modified model, has then been analyzed with a multigroup routine. That is, the best-fitting model has been simultaneously tested in the samples of patients with and without cognitive impairment. This multigroup routine tries to test if the same relationships (and their magnitude) holds for both samples even tough the instrument of measurement for emotional state of the patients with and without cognitive impairment is not the same. The multigroup routine starts with a multisample model simultaneously tested in both samples with no constraints across groups being made. This unconstrained multisample model had a very good fit: χ2(10) = 13.63, p = 0.23. CFI = 0.969, RMSEA = 0.063, 90% CI(0.000, -0.158), and AIC = -6.36. Given that the model fitted the data well for both samples, a more parsimonious model, with the three relationships among the predictors and the criteria constrained to be equal was estimated. This constrained model tests for the hypothesis of same magnitude in the relationships among the constructs of interest in the samples of patients with and without cognitive impairment. If model fit does not deteriorate, and ideally it is not statistically different from the fit in the unconstrained model, then this is evidence of same relationships holding for both samples. This constrained model fitted the data well: χ2(13) = 14.69, p = 0.32. CFI = 0.986, RMSEA = 0.038, 90% CI(0.000, -0.158), and AIC = -11.30. Indeed, model fit did improve, as CFI is larger and RMSEA and AIC lower than in the unconstrained model. A robust chi-square difference test was not statistically significant [χ2(3) = 0.784, p = 0.85] reinforcing the evidence of equal relations in both samples. Therefore, the estimates in Figure 2 adequately represent both samples.
Discussion
The main contribution of this study is the empirical proposal of a model that reflects the main predictors of the patient’s emotional well-being at the end of life and that of their main family caregiver. We observed in the proposed structural equation model how the overburden of the family caregiver act as a predictor of the emotional state of both patient and family caregiver. In this model, the relevance of the level of burden of the family caregiver is pivotal, since it directly predicts the emotional discomfort of the patient and the caregiver, even more than the level of functional independence of the patient or their level of cognitive impairment. These results suggest that reducing the family caregiver’s level of burden may contribute to the reduction of their own emotional distress and that of the patients they are taking care of. In this sense, our study provides useful data on the emotional well-being of the family system, specifically on the patient-caregiver dyad, highlighting the importance of the mutual influence between the well-being of the patient and that of the caregiver, as a starting point for the application of the model in future studies (Li and Loke, 2014).
An advantage of the model proposed in this study is that it predicts the emotional distress of the patient at the end of life and their main family caregiver whether the patient presents significant cognitive impairment or not. Therefore, we think our research provides new and useful knowledge in this sense.
Although the patient’s functional independence should be considered when promoting their own well-being and that of their families, our study suggest that the family caregiver’ burden might be equally important for this purpose. This is particularly interesting because there are effective interventions that might be implemented to reduce the overburden of the caregiver (Sörensen et al., 2002; Etters et al., 2008), whereas an intervention to reduce the patient’s functional dependence is not always feasible.
Data supporting the finding of the overburden of the family caregiver predicting the caregiver’s own emotional well-being and that of the patients has been found in previous research with patients at the end of life with a single specific diagnosis, like frail elderly (Soto-Rubio A. et al., 2017). The present study includes patients with different diagnosis (cancer, COPD, and frail elderly) while it takes into consideration their cognitive states, which makes our findings applicable to more diverse end-of-life settings.
One possible limitation of this study is that the patient’s emotional distress has been measured with two different instruments, depending on the cognitive status of the patients. However, both the correlation comparison analyzes and the comparison of the different structural equation models provide data in favor of the use of these two instruments in this context, since the observed relationships between the variables are the same.
Conclusion
This study suggests the need of implementing intervention programs in order to reduce the emotional distress of the patients at the end of life and their family caregivers, as well as to prevent the family caregivers’ overburden. Furthermore, the family caregiver’s overburden stands out as an important factor when aiming to reduce the emotional distress of patients at the end of life and their families, and this applies whereas the patient presents significant cognitive impairment or not. Our findings preliminarily suggest that reducing the family caregiver’s burden may also contribute to the reduction of the emotional distress of both patients and caregivers. In consequence, those interventions aimed to reduce the emotional distress of patients at the end of life and of their family caregivers should pay especial attention to indicators of overburden of the family caregiver, facilitating at the same time its prevention and reduction.
In this sense, future research regarding the reduction of emotional distress in the end-of-life context should take into consideration the prevention and reduction of overburden in family caregivers.
Data Availability
The raw data supporting the conclusions of this manuscript will be made available by the authors, without undue reservation, to any qualified researcher.
Author Contributions
AS-R contributed to the writing of the article and collection of data. MP-M contributed to the writing of the article and supervision of the research. JT contributed to the writing of the article and methodological analysis. PB contributed to the writing of the article and supervision of the research.
Funding
This work was supported by the Ministry of Economy, Industry and Competitivity of Spain (PSI2014-51962-R) and the Generalitat Valenciana, Valencia, Spain (VALi + d grant, beneficiary: AS-R).
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We express our sincere thanks to the patients, the families and the clinicians who made this study possible.
References
Barreto, M., and Martínez, E. (2003). “Guía de tratamientos psicológicos eficaces en enfermos terminales,” in Guía de Tratamientos Psicológicos Eficaces II, eds M. Pérez, J. R. Fernández, C. Fernández, and I. Amigo (Madrid: Pirámide), 243–252.
Baum, A., Thompson, D., Stollings, S., Garofalo, J., and Redinbaugh, E. (2001). “Psychological and psychiatric practice in oncology populations,” in Psychology and Psychiatry: Integrating Medical Practice, eds J. Milgrom and G. D. Burrows (New York, NY: John Wiley and Sons),155–181.
Baztán, J., Pérez, J., Alarcón, T., San Cristóbal, E., Izquierdo, G., and Manzarbeitia, J. (1993). Indice de barthel: instrumento válido para la valoración funcional de pacientes con enfermedad cerebrovascular. Revista Española Geriatría Gerontología 28, 32–40.
Bennett, K. S., and Shepherd, J. M. (2013). Depression in Australian women: the varied roles of spirituality and social support. J. Health Psychol. 18, 429–438. doi: 10.1177/1359105312443400
Bentler, P. M. (1990). Comparative fit indices in structural models. Psychol. Bull. 107, 238–246. doi: 10.1037/0033-2909.107.2.238
Bishop, M. M., Beaumont, J. L., Hahn, E. A., Cella, D., Andrykowski, M. A., Brady, M. J., et al. (2007). Late effects of cancer and hematopoietic stem-cell transplantation on spouses or partners compared with survivors and survivor-matched controls. J. Clin. Oncol. 25, 1403–1411. doi: 10.1200/JCO.2006.07.5705
Buhse, M. (2008). Assessment of caregiver burden in families of persons with multiple sclerosis. J. Neurosci. Nurs. 40, 25–31.
Callahan, D. (2000). Death and the research imperative. N. Engl. J. Med. 342, 654–656. doi: 10.1056/NEJM200003023420910
Cassell, E. J. (1998). The nature of suffering and the goals of medicine. Loss Grief Care 8, 129–142. doi: 10.1188/08.ONF.241-247
Cherny, N., Fallon, M., Kaasa, S., Portenoy, R. K., and Currow, D. C. (eds) (2015). Oxford Textbook of Palliative Medicine, 5e. New York, NY: Oxford University Press.
Cheung, G. W., and Rensvold, R. B. (2002). Evaluating goodness-of-fit indexes for testing measurement invariance. Struct. Equ. Model. 9, 233–255. doi: 10.1207/S15328007SEM0902-5
Chochinov, H. M., Johnston, W., McClement, S., Hack, T. F., Dufault, B., Enns, M., et al. (2016). Dignity and distress towards the end of life across four non-cancer populations. PLoS One 11:e0147607. doi: 10.1371/journal.pone.0147607
Cipolletta, S., Gammino, G. R., and Palmieri, A. (2017). Illness trajectories in patients with amyotrophic lateral sclerosis: how illness progression is related to life narratives and interpersonal relationships. J. Clin. Nurs. 26, 5033–5043. doi: 10.1111/jocn.14003
Cipolletta, S., Pasi, M., and Avesani, R. (2016). Vita tua, mors mea: the experience of family caregivers of patients in a vegetative state. J. Health Psychol. 21, 1197–1206. doi: 10.1177/1359105314550348
Cosgrove, J., and Alty, J. E. (2018). Cognitive deficits in Parkinson’s disease: current perspectives. J. Parkinsonism Rest. Legs Syndr. 8, 1–11. doi: 10.2147/JPRLS.S125064
Cysique, L. A. J., Maruff, P., Darby, D., and Brew, B. J. (2006). The assessment of cognitive function in advanced HIV-1 infection and AIDS dementia complex using a new computerised cognitive test battery. Archives of Clinical Neuropsychology 21, 185–194. doi: 10.1016/j.acn.2005.07.011
Davis, J. C., Hsiung, G. Y., Bryan, S., Jacova, C., Jacova, P., Munkacsy, M., et al. (2016). Agreement between patient and proxy assessments of quality of life among older adults with vascular cognitive impairment using the EQ-5D-3L and ICECAP-O. PLoS One 11:e0153878. doi: 10.1371/journal.pone.0153878
Etters, L., Goodall, D., and Harrison, B. E. (2008). Caregiver burden among dementia patient caregivers: a review of the literature. J. Am. Acad. Nurse Pract. 20, 423–428. doi: 10.1111/j.1745-7599.2008.00342.x
Fombuena, M., Galiana, L., Barreto, P., Oliver, A., Pascual, A., and Soto-Rubio, A. (2016). Spirituality in patients with advanced illness: the role of symptom control, resilience and social network. J. Health Psychol. 21, 2765–2774. doi: 10.1177/1359105315586213
Fu, F., Zhao, H., Tong, F., and Chi, I. (2017). A systematic review of psychosocial interventions to cancer caregivers. Front. Psychol. 8:834. doi: 10.3389/fpsyg.2017.00834
Given, B. A., Given, C. W., and Sherwood, P. (2012). The challenge of quality cancer care for family caregivers. Semin. Oncol. Nurs. 28, 205–212. doi: 10.1016/j.soncn.2012.09.002
Grassi, L., Caruso, R., Sabato, S., Massarenti, S., and Nanni, M. G. (2015). Psychosocial screening and assessment in oncology and palliative care settings. Front. Psychol. 5:1485. doi: 10.3389/fpsyg.2014.01485
Green, M. F. (2006). Cognitive impairment and functional outcome in schizophrenia and bipolar disorder. J. Clin. Psychiatry 67, 3–8; discussion 36–42. doi: 10.4088/JCP.1006e12
Hagedoorn, M., Sanderman, R., Bolks, H. N., Tuinstra, J., and Coyne, J. C. (2008). Distress in couples coping with cancer: a meta-analysis and critical review of role and gender effects. Psychol. Bull. 134:1. doi: 10.1037/0033-2909.134.1.1
Hébert, R., Bravo, G., and Préville, M. (2000). Reliability, validity and reference values of the zarit burden interview for assessing informal caregivers of community-dwelling older persons with dementia. Can. J. Aging 19, 494–507. doi: 10.1017/S0714980800012484
Herr, K., Bjoro, K., and Decker, S. (2006). Tools for assessment of pain in nonverbal older adults with dementia: a state-of-the-science review. J. Pain Symptom. Manage. 31, 170–192. doi: 10.1016/j.jpainsymman.2005.07.001
Hodges, L. J., Humphris, G. M., and Macfarlane, G. (2005). A meta-analytic investigation of the relationship between the psychological distress of cancer patients and their carers. Soc. Sci. Med. 60, 1–12. doi: 10.1016/j.socscimed.2004.04.018
Hu, L. T., and Bentler, P. M. (1999). Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct. Equ. Model. 6, 1–55. doi: 10.1080/10705519909540118
Kline, R. B. (2015). Principles and Practice of Structural Equation Modelling. New York, NY: Guilford.
Krikorian, A., Limonero, J. T., and Maté, J. (2012). Suffering and distress at the end –of-life. Psychooncology 21, 799–808. doi: 10.1002/pon.2087
Li, Q., and Loke, A. Y. (2014). A literature review on the mutual impact of the spousal caregiver–cancer patients dyads:‘communication’,‘reciprocal influence’, and ‘caregiver–patient congruence’. Eur. J. Oncol. Nurs. 18, 58–65. doi: 10.1016/j.ejon.2013.09.003
Liszewski, C. M., O’Hearn, E., Leroi, I., Gourley, L., Ross, C. A., and Margolis, R. L. (2004). Cognitive impairment and psychiatric symptoms in 133 patients with diseases associated with cerebellar degeneration. J. Neuropsychiatry Clin. Neurosci. 16, 109–112.
Little, T. D. (1997). Mean and covariance structures (MACS) analyses of cross-cultural data: practical and theoretical issues. Multivariate Behavioral Research 32, 53–76. doi: 10.1207/s15327906mbr3201_3
Mahoney, F., and Barthel, D. (1965). Functional evaluation: the barthel index. Maryland State Med. J. 14, 61–65.
Martínez, J., Dueñas, R., Herrero, M., Onís, C., Aguado, C., Albert, C., et al. (2001). Adaptación y validación al castellano del cuestionario de Pfeiffer (SPMSQ) para detectar la existencia de deterioro cognitivo en personas mayores de 65 años. Med. Clín. 117, 129–134. doi: 10.1016/S0025-7753(01)72040-4
Muthén, L. K., and Muthén, B. O. (1998–2011). Mplus User’s Guide, Sixth Edn. Los Angeles, CA: Muthén Muthén.
Northouse, L. L., Katapodi, M. C., Schafenacker, A. M., and Weiss, D. (2012). The impact of caregiving on the psychological well-being of family caregivers and cancer patients. Semin. Oncol. Nurs. 28, 236–245. doi: 10.1016/j.soncn.2012.09.006
Oczkowski, S. J., Chung, H. O., Hanvey, L., Mbuagbaw, L., and You, J. J. (2016). Communication tools for end-of-life decision-making in ambulatory care settings: a systematic review and meta-analysis. PLoS One 11:e0150671. doi: 10.1371/journal.pone.0150671
Pandharipande, P. P., Girard, T. D., Jackson, J. C., Morandi, A., Thompson, J. L., Pun, B. T., et al. (2013). Long-term cognitive impairment after critical illness. N. Engl. J. Med. 369, 1306–1316. doi: 10.1056/NEJMoa1301372
Pessin, H., Rosenfeld, B., and Breitbart, W. (2002). Assessing psychological distress near the end of life. Am. Behav. Sci. 46, 357–372. doi: 10.1177/000276402237769
Pfeiffer, E. (1975). A short portable mental status questionnaire for assessment of organic brain deficit in elderly patients. J. Am. Geriatr. Soc. 23, 433–441. doi: 10.1111/j.1532-5415.1975.tb00927.x
Raveis, V. H., Karus, D., and Pretter, S. (2000). Correlates of anxiety among adult daughter caregivers to a parent with cancer. J. Psychosoc. Oncol. 17, 1–26. doi: 10.1300/J077v17n03-01
Raveis, V. H., Karus, D. G., and Siegel, K. (1998). Correlates of depressive symptomatology among adult daughter caregivers of a parent with cancer. Cancer 83, 1652–1663.
Sampson, E. L., Gould, V., Lee, D., and Blanchard, M. R. (2006). Differences in care received by patients with and without dementia who died during acute hospital admission: a retrospective case note study. Age Ageing 35, 187–189. doi: 10.1093/ageing/afj025
Sampson, E. L., van Der Steen, J. T., Pautex, S., Svartzman, P., Sacchi, V., Van den Block, L., et al. (2015). European palliative care guidelines: how well do they meet the needs of people with impaired cognition? BMJ Support. Palliat. Care 5, 301–305. doi: 10.1136/bmjspcare-2014-000813
Segrin, C., Badger, T., Dorros, S. M., Meek, P., and Lopez, A. M. (2007). Interdependent anxiety and psychological distress in women with breast cancer and their partners. Psychooncology 16, 634–643. doi: 10.1002/pon.1111
Sepúlveda, C., Marlin, A., Yoshida, T., and Ullrich, A. (2002). Palliative care: the World Health Organization’s global perspective. J. Pain Symptom. Manage. 24, 91–96. doi: 10.1016/S0885-3924(02)00440-2
Sherwood, P. R., Given, C. W., Given, B. A., and Von Eye, A. (2005). Caregiver burden and depressive symptoms analysis of common outcomes in caregivers of elderly patients. J. Aging Health 17, 125–147. doi: 10.1177/0898264304274179
Sociedad Española de Cuidados Paliativos [SECPAL] (2018). Definición de Enfermedad Terminal. Available at: http://www.secpal.com/biblioteca_guia-cuidados-paliativos_2-definicion-de-enfermedad-terminal [accessed Jun 15, 2018].
Sörensen, S., Pinquart, M., and Duberstein, P. (2002). How effective are interventions with caregivers? An updated meta-analysis. Gerontologist 42, 356–372. doi: 10.1093/geront/42.3.356
Soto-Rubio, A., Pérez-Marín, M. A., and Barreto, P. (2017). Frail elderly with and without cognitive impairment at the end of life: their emotional state and the wellbeing of their family caregivers. Arch. Gerontol. Geriatr. 73, 113–119. doi: 10.1016/j.archger.2017.07.024
Soto-Rubio, A. L., Tomás, J. M., Pérez-Marín, M., and Barreto, P. (2017). Patients with limited communication in end-of-life situations: initial psychometric properties of a discomfort observation scale. J. Health Psychol. doi: 10.1177/1359105317696139 [Epub ahead of print].
Tejero, A., Guimerá, E. M., Farré, J. M., and Peri, J. M. (1986). Uso clínico del HADS (Hospital Anxiety and Depression Scale) en población psiquiátrica: un estudio de su sensibilidad, fiabilidad y validez. Rev. Psiquiatr. Fac. Med. Barc. 13, 233–238.
Toseland, R. W., Blanchard, C. G., and McCallion, P. (1995). A problem solving intervention for caregivers of cancer patients. Soc. Sci. Med. 40, 517–528. doi: 10.1016/0277-9536(94)E0093-8
Who. (2005). World Health Assembly Resolution WHA58.22. Available at: http://www.who.int/ipcs/publications/wha/cancer_resolution.pdf [accessed Jun 15, 2018].
Zarit, S. H., Reever, K. E., and Back-Peterson, J. (1980). Relatives of the impaired elderly: correlates of feelings of burden. Gerontologist 20, 649–655. doi: 10.1093/geront/20.6.649
Keywords: burden, end-of-life, family caregiver, emotional well-being, cognitive impairment
Citation: Soto-Rubio A, Perez-Marin M, Tomas Miguel J and Barreto Martin P (2018) Emotional Distress of Patients at End-of-Life and Their Caregivers: Interrelation and Predictors. Front. Psychol. 9:2199. doi: 10.3389/fpsyg.2018.02199
Received: 02 August 2018; Accepted: 23 October 2018;
Published: 06 November 2018.
Edited by:
Changiz Mohiyeddini, Northeastern University, United StatesReviewed by:
Arianna Palmieri, Università degli Studi di Padova, ItalyEnrico Furlan, Università degli Studi di Padova, Italy
Copyright © 2018 Soto-Rubio, Perez-Marin, Tomas Miguel and Barreto Martin. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Marian Perez-Marin, bWFyaWFuLnBlcmV6QHV2LmVz
 Ana Soto-Rubio
Ana Soto-Rubio Marian Perez-Marin
Marian Perez-Marin Jose Tomas Miguel2
Jose Tomas Miguel2