- 1School of Optometry, Université de Montréal, Montreal, QC, Canada
- 2CRIR/Institut Nazareth et Louis-Braille du CISSS de la Montérégie-Centre, Longueuil, QC, Canada
- 3Interdisciplinary School of Health Sciences, Faculty of Health Sciences, University of Ottawa, Ottawa, ON, Canada
- 4CRIR/Centre de réadaptation Lethbridge-Layton-Mackay du CIUSSS du Centre-Ouest-de-l’Île-de-Montréal, Montreal, QC, Canada
Introduction: The proportion of older adults with combined acquired vision and hearing impairments (referred to as Dual Sensory Impairment/DSI) is growing, and their unique care needs are beginning to receive increased attention. Considering the age-related demographic shift, one million older adults in Canada are expected to experience DSI by 2036, and evidence suggests that DSI is associated with communication difficulties, cognitive decline, depression, functional decline, and participation challenges. Given that the goal of sensory rehabilitation is to improve participation, the study explored perceived contextual barriers and facilitators of social participation among older adults with DSI to better understand their lived experience.
Methods: The International Classification of Functioning, Disability and Health (ICF) was used as a framework to identify and describe the contextual factors (environmental and personal) that influence the social participation of older adults with DSI. Sixteen older adults with DSI (mean age = 86 years, SD = 7; 9 female; registered with an urban sensory rehabilitation organization) were interviewed using a semi-structured qualitative interview guide. Interviews were audio-recorded, transcribed, and then analyzed using a content analysis approach.
Results: Environmental factors, such as societal attitudes toward disability, access to technology aids, and availability of transportation services emerged as the most important factors influencing participation. The onset and type of the impairments and attitude toward one’s disability were important personal factors affecting the participation. The availability of social support and the use of assistive devices (e.g., magnifiers, glasses, and hearing aids) were reported to be facilitators. In contrast, the inaccessibility of the built environment and the cost and limited availability of accessible transportation were key barriers to their social participation.
Discussion: Our study indicated that assistive devices facilitate older adults with DSI in their day-to-day functioning and improve social participation, while expensive and inadequate transportation services may deter their participation. For rehabilitation professionals working with older adults with DSI, it is crucial to consider the barriers to and facilitators of social participation when designing interventions. Future research is warranted to investigate the role of assistive devices and transportation in improving the social participation of older adults with DSI.
Introduction
The proportion of older adults with combined acquired vision and hearing impairments is growing, and their unique care needs are starting to receive increased attention (Schneider et al., 2011; Wittich et al., 2016a). Anywhere between 1.7 and 33% (Carabellese et al., 1993; Gopinath et al., 2013) of persons over the age of 50 have been reported to live with dual sensory impairment (DSI). The 5-year incidence is estimated at 1.6% for those with no impairment and 11.3% for persons with one existing sensory loss (Schneider et al., 2012). The effects of DSI spans widely, affecting all aspects of wellbeing, including increased depression and anxiety, as well as impaired communication (Heine and Browning, 2002; McDonnall and Capella-McDonnall, 2009; Cosh et al., 2018; Crowe et al., 2019), and participation challenges (For a comprehensive overview of the impact of DSI see Wittich and Simcock, 2019).
Loneliness, social isolation and reduced social participation have become an increasing concern for older adults in general (Holt-Lundstad, 2017), and in those with sensory loss in particular (Mick et al., 2018). However, the extent to which these restrictions in participation (at societal, community, and/or family levels) are affecting older adults with DSI remains relatively limited in the research literature (see Saunders and Echt, 2007; Viljanen et al., 2014). Previous work by members of our team has explored the concept of social participation in older adults’ with a single impairment (Fraser et al., 2019a). In addition, we have explored combined sensory loss with specific focus on the perspective of working-age adults (Jaiswal et al., 2018, 2019a,b); however, few studies have focused specifically on older adults with DSI in this context (McDonnall and Capella-McDonnall, 2009; McDonnall et al., 2016).
According to the World Health Organization (WHO)s’ International classification of functioning, disability and health (ICF), aspects of a persons’ level of functioning (i.e., activity and social participation) can be influenced by contextual factors (World Health Organization, 2001). These can be personal (e.g., age, gender, etc.) as well as environmental (e.g., use of assistive devices, social support, and negative attitudes; World Health Organization, 2013). Using the ICF model, qualitative research with working-aged adults with DSI has revealed that the onset and nature of impairment and proactive outreach to others emerged as important personal factors (Jaiswal et al., 2019b). The availability of services and policies specific to deafblindness; attitudes of others; presence of support and relationships (family, friends, and teachers); and access to assistive technology emerged as significant environmental factors affecting the participation of working-aged adults in society (Jaiswal et al., 2019b).
A cross-sectional study by Viljanen et al. (2014) in Europe found sensory difficulties to be associated with social inactivity and recommended qualitative enquiry to explore the perspective of older adults with sensory impairment on how to enhance their social participation (Viljanen et al., 2014). In addition, other work examining the limitations of older adults with DSI (McDonnall et al., 2016) has identified transportation, training in the use of assistive devices, help with daily tasks and problems with communication as the principal challenges experienced by their sample of older participants with DSI. They generally reported that persons in their environment (e.g., family members or health care professionals) could benefit from education and information about DSI. This would facilitate the social participation of older adults with DSI and reduce some of the challenges/barriers they face.
Using a qualitative approach, LeJeune’s (2010) findings also support the need for assistive devices information and training for older adults with DSI and many of their care providers. During interviews, the participants highlighted the psychological strain, depression and fear of being stigmatized, and marginalized. Similarly, communication, activities of daily living, and independence were central to the concerns of the older DSI participants interviewed by Fletcher and Guthrie (2013). When focusing on long-term care, Roets-Merken et al. (2017) mirror these findings, and highlight the desire of older adults with DSI to gain some aspects of control in their lives. They underscored the participation problems faced by residents with DSI under three categories: (1) lack of access to communication, information and mobility, (2) concerns of not belonging or not being able to connect with other people, and (3) the desire to be actively involved in care delivery. Given the goal of sensory rehabilitation to address these core concerns, the present study aims to shed light on the experience of social participation among older adults with acquired DSI that have accessed and undergone rehabilitation for their sensory impairments. We explored their perception of which contextual barriers or facilitators influenced their social participation in order to better understand and learn from their lived experience. This understanding will inform future service delivery and may be instrumental in designing rehabilitation interventions aimed at improving participation outcomes (Perenboom and Chorus, 2003; Hammel et al., 2008; Mallinson and Hammel, 2010; Eyssen et al., 2011; Jaiswal et al., 2018).
Materials and Methods
Study Design and Sample
The ICF was used as a framework to identify and describe the contextual factors (environmental and personal) that influence the functioning of older adults with DSI (World Health Organization, 2007). The project was approved by the Ethics committee of the Center for Interdisciplinary Research in Rehabilitation of Greater Montreal (CRIR #938–0314). This qualitative study was based on semi-structured interviews with 7 men and 9 women living with DSI over 65 years of age (Mean = 86 years, SD = 7). They were registered with the CRIR/Centre de réadaptation Lethbridge-Layton-Mackay du CIUSSS du Centre-Ouest-de-l’Île-de-Montréal, an urban rehabilitation organization in Montreal, QC, Canada (Wittich et al., 2014). The clients were eligible for both vision and hearing rehabilitation services according to the criteria laid out by the Quebec Health Insurance system (Regie de l’assurance maladie du QUEBEC/RAMQ, 2006a, b). These criteria for vision indicate that clients have a visual acuity less than 20/70 (6/21) or a visual field of less than 60° in the better eye with best standard correction, or hemianopia (loss of half the visual field due to stroke or nerve/brain damage); and for hearing indicate an unaided average pure-tone threshold hearing level (HL) of >26 decibel (dB) across four frequencies (0.5, 1, 2, and 4 kHz) in the better ear. All participants lived independently in the community, wore at least one hearing aid, and had accessed both vision and hearing rehabilitation services at some point in the past. These services included but were not limited to free loans of assistive hearing and vision devices, training in compensatory strategies (e.g., speech reading), and environmental adjustments (e.g., lighting assessment at home).
We used purposive sampling to recruit individuals with DSI (Sandelowski, 1995; Patton and Cochran, 2002) from a day center program (Wittich et al., 2014). Potential participants were initially identified through the day center personnel. They were then approached by a research assistant, given a brief oral presentation of the project, and asked if they would be interested in participating. If so, written informed consent was obtained. Once recruited, a convenient time and place was arranged for an interview. The research was carried out with all participants who could be identified and recruited within a 10-month period (Sept 2014–June 2015). All of the participants had some residual hearing and visual ability, allowing them to communicate with the interviewer verbally.
Data Collection
Qualitative interviewing is used to collect data to obtain information about people’s perceptions, thoughts, and feelings (Creswell, 2013). Participants were interviewed using a qualitative semi-structured interview schedule (Creswell, 2013) that included open-ended questions about the participants’ living situation, changes in hearing and vision and the resulting effects on their life, and factors influencing their social participation. Participants were asked about activities in as well as outside the home. Information about use of the assistive devices often emerged spontaneously in response to the questions. Six interviews took place in participants’ homes, the remaining interviews took place in a quiet office in the same building as the day center. Interviews were typically an hour in duration. Interviews were conducted until data saturation was achieved (Fusch and Ness, 2015; Saunders et al., 2018).
Data Analysis
Interviews were audio-recorded, transcribed, and then managed using Atlas.ti 7 software. Qualitative content analysis was chosen as appropriate when there is limited knowledge about a research topic (Hsieh and Shannon, 2005). We used directed content analysis of transcripts as it involves a deductive approach where coding, analysis and interpretation of the participants’ responses are based on the predetermined theory, or guiding framework (Hsieh and Shannon, 2005). In this study, the ICF was the guiding framework for analysis and we coded transcripts specific to personal and environmental factors as predetermined codes. Drawing from the ICF framework, codes relating to environmental factors were organized according to the ICF environmental descriptions. For example, quotes related to attitudes used by participants were coded under the ICF’s environmental factors “attitudes” chapter.
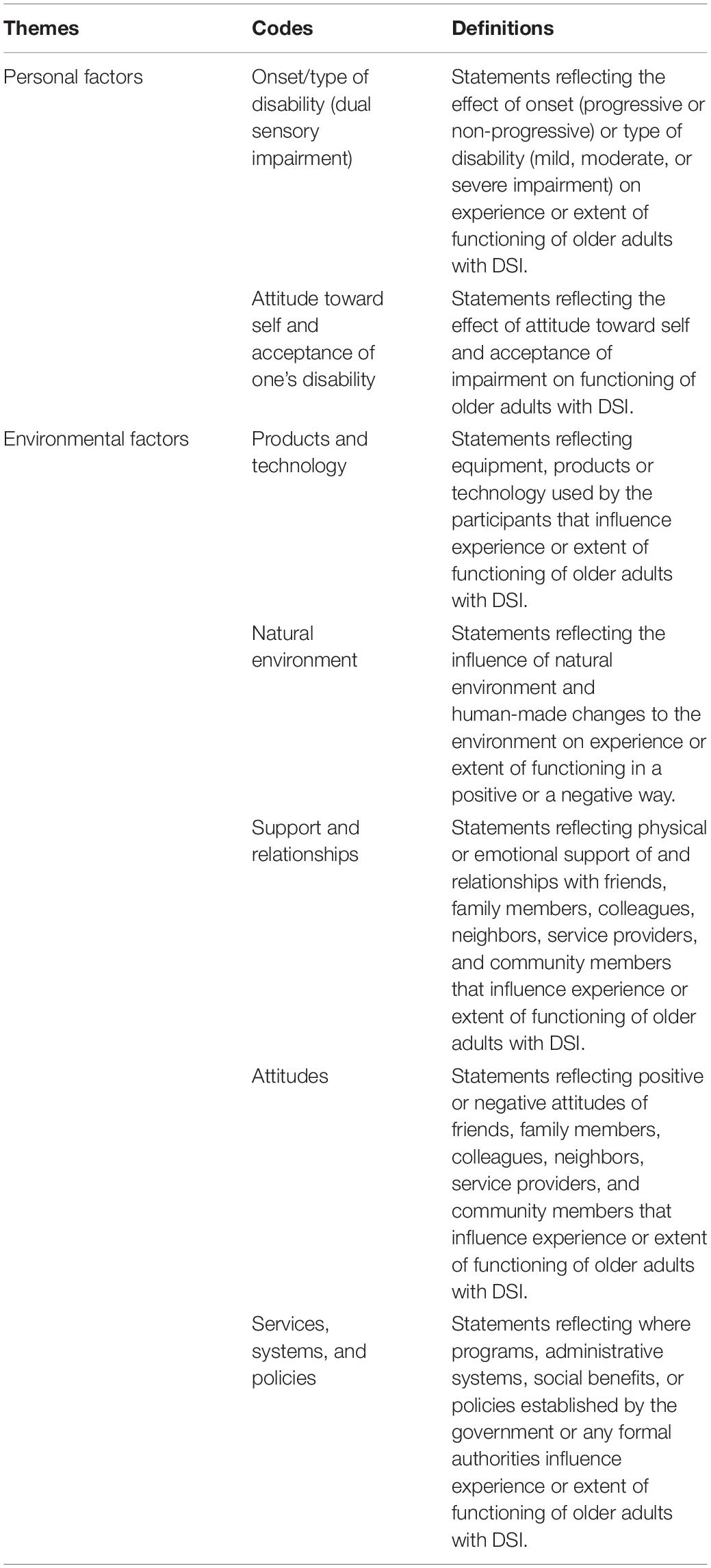
The first author developed a code book based on five randomly selected interviews (see Table 1. for codebook highlighting themes, codes and guiding definitions). Each transcript was read and re-read by the team and coded using the predetermined codes. Codes were then organized into personal and environmental factors. Codes were assigned to segments of text, using Atlas.ti 7, and segments of text could be assigned more than one code. To maximize rigor, each member of the research team (AJ, WW, and SF) coded the same two transcripts independently using the coding framework, then compared results. Differences in coding were discussed and consensus reached (Krefting, 1991; Gale et al., 2013). Intercoder reliability based on segments coded in the same way from the coding framework was calculated and found to be 0.75.
Periodic checks were conducted with the research team to discuss emerging categories and themes and any discrepancies were resolved by discussion in the team. In the final stages of content analysis, we selected direct quotes from transcripts as representative quotes of the different contextual factors perceived as influencing functioning of older people with DSI.
Results
This section presents the findings identified in this study related to the ICF personal and environmental factors (World Health Organization, 2013). Quotations are followed by fictitious initials in order to separate and identify the individual viewpoints of participants.
Personal Factors
Onset/Type of Disability and Its Related Effects
The first personal factor that emerged as affecting participation of our sample was the onset/type of disability caused by DSI and its related effects. Many of our participants highlighted the disability caused by gradual decline of the hearing and vision senses and its impact on their day-to-day functioning. Firstly, they spoke about their reduced participation in activities that they were important to them such as reading a book or a newspaper, watching Television, knitting, cooking, going out for groceries, attending concerts, driving, and many others, due to the combined vision, and hearing loss. When asked about the changes over time, one participant reflected on giving up many activities due to his sensory impairments, in particular his role in the workforce: “Work, I can’t work, I’m blind, deaf, and cripple… it’s very hard to participate. I used to but one by one I gave everything up… because of the loss of my hearing and the loss of my eyesight” [ZH].
Apart from the activity restrictions, many of our participants shared their perceptions about the impact of sensory impairments on other cognitive functions and other downstream consequences. For example, they highlighted how their sensory impairments have led to social isolation, dependency, frustration, and decline in memory.
I talk to my neighbors, but I don’t have many friends because I don’t feel very well. I stay on my own a lot and it’s hard to create friendships when you don’t participate. I don’t participate in activities, you know, because I don’t feel well enough. [AB]
Attitude Toward Self and Acceptance of One’s Disability
The other personal factors that older adults with DSI described as affecting their social participation were their attitude toward self and acceptance of their own disability. These factors emerged both as a facilitator and a barrier to participation for our participants. For example, for some of the participants, reduced social participation was considered a normal part of aging, while for others it had a significant impact on their functional and psycho-emotional well-being. For the people that described themselves as having adapted to their condition, the use of their residual abilities was crucial, and was a way of and to life for them. One of these individuals, mentioned:
You don’t talk much, that much I got, but it’s like you’re living in a fog, like you’re living underwater. That’s your life now and you have to tolerate it because you don’t have a choice and if your attitude is not completely negative, you’ll survive, you’ll get along. You’ll do. I go to museums, I go to theater, I go to movies. I can’t see who is on the screen but I hear it. You know? So you can make something of your life. [PI]
For individuals who described negative experiences, dependency on others was an area of concern. They felt that they may become dependent with time due to the progressive loss of their sensory functions, which was hard to accept, as illustrated by this quote:
Being independent before that, that I could just get into the car, drive off and do whatever I want to, I find it sometimes hard because you have to depend on other people it makes it almost like a necessity that you have to depend on other people. Not only family but other people. I find it sometimes frustrating but the adaptations I have no other choice. So you do what you need to do and you work with what you have. [KW]
Another participant with a different perspective mentioned:
I’ve learned now that you can’t have it. Well… I’m giving up on the hearing now. Before I wanted to know every word that came out. And now I get used to the idea that I don’t hear every word just like I can’t see everything, I get used to it.
Environmental Factors
Products and Technology
Assistive aids and devices emerged as one of the most critical factors that the participants described as affecting their social participation and independence. Most of them used hearing aids, eyeglasses, magnifiers, tablets, large screens, CCTVs, computers, reading machines, a braille device, and/or white identification or long canes. These devices facilitated engagement and participation in activities that were otherwise becoming challenging, as illustrated by this quote: “with the hearing aids I hear very well. I go out or I go downstairs if I go shopping or whatever, yes I wear them” [AB]. Another participant who had an accessibility software in his computer quoted: “I read in the computer and this computer zoom desk 10. Zoom desk 10 makes it bigger and it say the 2 times. I make it 21/2 time as much as I want” [YS].
Participants felt that assistive devices helped them to remain independent and allowed them to maintain social relationships:
…they [magnifiers] are [helpful]. I don’t think that I can read a whole page of something because it runs together after a while but if I need to read my mail, I can make out a check, I can write a greeting card and that’s about it. I tried to be very independent, as much as I can [LG]
What I’m wearing now is distance glasses so I can see the outline of your face. I can’t see your face. I don’t see anybody’s face unless you’re this close…Then I can see and if the light is proper. Then I can see the face. Otherwise, I don’t see anybody’s face.
However, participants also spoke about the maintenance, costs, and training, or adaptation issues associated with using assistive devices. For instance, for a few, the hearing aids were described as not very helpful. A participant who tried to obtain a hearing aid mentioned:
Little by little it was getting harder and harder when you don’t hear, and I got hearing aids until about a year ago. One of them I bought for $2500. The other [pair] through Medicare. I couldn’t hear with any of them including the one I bought. [ZH]
Another participant shared: “It’s uncomfortable and it takes some getting used to, the fact that you hear a lot of extraneous noise more clearly too. Not more clearly, that’s the wrong choice of words, it’s more invasive” [MM].
Natural and Built Environment
Natural and built environment emerged as one of the minor themes in our analysis, wherein some of our participants spoke about how natural and built environments influenced their participation. For example, one of the participants mentioned the poorly maintained sidewalks and roads and how they were risky for her to go out, given her poor vision, and balance issues:
That’s another reason I don’t go anywhere. Just in case there’s cracks in the sidewalk, or there’s cracks in the road, or cracks in the street, or in the floor or whatever. I don’t go because I don’t necessarily see the cracks and if I would be pushing my walker and walking behind it and hitting one of the cracks, bad crack, I’d be on the floor because I would automatically fall down because of my balance [RG]
On the contrary, another participant appreciated her neighborhood in the city where parks were close and walkable for older adults with sensory impairments and enabled her to go out with her friends.
I, we go for the walks and we go in the park. We have a park near our condo. We have a park, we walk around the park, we enjoy the little babies and children on the playground and you know. [SW]
Support and Relationships
Support and relationships with friends and family emerged as one of the major factors that affected social participation of older adults with DSI. Our participants appreciated the support they received from their family or friends for essential daily activities and/or recreation and leisure activities, as highlighted by the quotes below:
I got a friend who told me, “call me you know if you want to go somewhere, call me and I’ll come with you. When she’s off she comes here. She helps me clean my place up and everything. Carry me out to shopping, do my little shopping and stuff. [CG]
Other participants mentioned:
They [family] are very cooperative especially my sister. She does everything, she calls often. She tells me that if I need something, she’ll be glad to do it for me. [JZ]
My daughter came last night although its tax season and she’s in accounting but she wanted to come see why I’m so weak so and why this. So, she stayed quite a while and she always does something that I need to be done, always. [AB]
In some cases where participants did not have a significant other- either a family member or friend to accompany or help, they spoke about how their participation was negatively affected. This is illustrated by the quote below:
I used to go to every concert… the ballet. They still call me from the [concert theater]. “Why aren’t you coming back Mrs. [name]?” “Because I can’t see.” And I don’t like going alone…. I haven’t done anything in my life for the last few years [SK]
It was interesting to note that while in some cases, participants were voluntarily offered such support by their friends or family, in others, the support was not always available, and they had to ask for it:
I would like to go to a movie. I would like to go to visit somebody sometimes at a hospital. Well that I did a few months ago. My son came into town and I insisted that he take me to the hospital to visit a cousin who was dying…[RG]
Attitudes
Other people’s attitudes directly or indirectly affected social participation of older adults with DSI. Most of the negative attitudes that were mentioned by the participants arose from the stigma attached to the use of hearing aids or other types of assistive devices. Some of the participants mentioned their positive interactions with the sighted community and how it helped them in their daily functioning, while others expressed their experience of negative attitudes in the same context. For example, participants who reported positive attitudes from others shared:
What I can’t find I ask somebody, either an employee, or another shopper. You won’t believe how kind people are! They are so kind, I’ve never been re-buffed, it’s been years and I can’t believe how kind they are, always! They’re wonderful. [AB]
The bus driver is very polite, same thing with the people, or if someone’s sitting in that seat that’s directly behind the bus driver, they’ll immediately get up and I’ll have that seat. Or something else and I’ll just tell him where I to get off and so he’ll stop there. [FW]
While another participant who had a negative experience shared:
You go into grocery store and I asked the guy that’s putting products on shelves: where would I find mustard? And he will say, look at the signs. and I’ll say, “If I could look at the signs would I ask you?” I go through this, not a lot, but infrequently yes. [PI]
Those who had a negative experience with others felt embarrassed for not being able to hear and see, needing to depend on others or assistive devices, thereby sometimes affecting their social participation. This is illustrated the following quote: “Sometimes it’s embarrassing. People look at you funny. “Oh, you have two of them [hearing aids]!” “Yes, I have two of them. I need them to hear.” You’d be surprised how weird people can be, how mean.” [SK].
Services, Systems, and Policies
The older adults with DSI in our sample described services, systems and policies as one of the critical factors that affected their participation. Within this theme, most of our participants shared their experiences with the transportation and healthcare system. With regards to transportation, many participants felt that it was either not available or not accessible or adapted to suit their needs, as shown here:
Oh it’s [transport services] horrible. Even getting to them [accessible transport services] on the phone. you’re not sure if you’ll get through and you could spend an entire day dialing and re-dialing and most of the [times] you get through but a lot of times you don’t. [PI]
In a few cases, participants felt that regular transportation was too expensive. This forced them to rely on accessible transport options thereby affecting their participation. This is illustrated by a quote below:
I have to go with adapté number one [accessible] bus transit… wait there for two hours to go home…. Regular taxi is too expensive. Costs me … about $50. No, I don’t want to go that badly and I’m not going to ask anybody to take me. [SK]
With regards to the healthcare system, a participant mentioned the lack of coordinated and systematic care for older adults with DSI, which severely affected his functioning and participation:
You know you have to be examined like twice a year when you wear contacts. Year after year he [doctor] would say: you see good enough. And you don’t argue with your doctor. But I believe that if I had been treated 40 years ago [by laser or injections that could have prevented the impairment or kept it at a lower level], I wouldn’t be in this situation [of almost not able to see at all] I am in now. [PI]
Participants discussed the lack of awareness and sensitivity of healthcare providers and other types of service providers (mostly public transit drivers) toward the needs of older adults with DSI. For example, a participant who wanted to get eyeglasses described:
So, when they called me for the glasses, I sit down there she put the glasses on, and she tell me- she gave me a book and I said, “I can’t see nothing!.” And that’s the pair of glasses there, I can’t see nothing there. And she said, “Well you’ll get accustomed to it, look in the bifocals.” I said, “I tell you, I can’t see nothing.” I had to pay, I don’t know much $200–300 or whatever for everything. But then I come home and it’s the same thing, I couldn’t see nothing at all! [CG]
Some of the participants also shared their positive experiences with some local public organizations that cater to the needs of people with sensory impairments, specifically related to the assistive devices. For example: “I found out there is an organization and I joined {name of the organization}. And they’re very nice over there. And they gave me their magnifier and I use it.” [ZH].
Similarly, another participant shared his positive experience with the hearing aids that were provided by the government:
…the government, I was ready to buy another one, but they gave it to me because I have vision problems. I’m due for two from the government the people who have no vision problems they only get one from the government. So I have two from the government and they are improved a lot since the first one, so I didn’t need to buy another expensive one because I am satisfied with the one that I have now. [LG]
Discussion
The present study explored which contextual barriers or facilitators influenced social participation from the perspective of older adults with DSI, in order to better understand and learn from their lived experience. Social isolation experienced by older adults is a public health concern (Holt-Lundstad, 2017; Fakoya et al., 2020). This is no less important for older adults with DSI who often experience participation restrictions due to challenges in communication, mobility, and access to information. To our knowledge, our study is the first of its kind and presents some salient findings on barriers, and facilitators that older adults with DSI perceive to influence their social participation. It is important to note here that an older adult with a single sensory impairment (vision or hearing impairment only) may compensate for the loss of uni-sensory information by using another sense (using vision cues in case of hearing loss and vice versa), but this might not be as simple for older adults with DSI, and challenges may be exacerbated due to multiplying effect of dual impairment (Wittich et al., 2013). Despite of varying degrees of hearing and vision challenges, participants in this study equivocally noted that social participation is important for them and they try to adapt to the changes in their functioning in order to continue to participate in society.
In general, previous studies on older adults and social participation, respectively, often omitted representing the voices of older adults with multi-sensory impairments (Hammel et al., 2008, 2015; Levasseur et al., 2010; Arnadottir et al., 2011; Alma et al., 2012; Meulenkamp et al., 2013; Laliberte Rudman et al., 2016; Martin Ginis et al., 2017; Tsai et al., 2017; Wong et al., 2017). Our study complements and advances the previous work on social participation and older adults by adding the perspectives of older adults with DSI on barriers to and facilitators of their social participation. Our findings resonate with the results of the studies conducted with older adults with DSI in countries other than Canada that have different health and social care arrangements for people with disabilities in Europe and the United States (Viljanen et al., 2014; McDonnall et al., 2016; Crowe et al., 2019). In line with their findings, our study participants reported that expensive and inadequate transportation services, negative stereotypes, and poorly maintained built environments, such as sidewalks and roads, were barriers to their outdoor mobility and social participation. Assistive devices and social support from family or friends for leisure and essential daily activities were considered important facilitators to their day-to- day functioning and maintained participation.
Previous work with older adults with DSI by McDonnall et al. (2016) indicated that this group is more interested in retaining or regaining use of their hearing and vision to the greatest extent possible, rather than learning alternative techniques (such as use of technology or alternative communication modalities). Our results suggest that, although participants felt that assistive devices helped them to remain independent and allowed them to maintain social relationships, they had challenges with cost, training in the use, maintenance, and adaptation of the device as per their individual specific need. This finding may be associated with the fact that assistive device interventions are effective (Binns et al., 2012) but complicated, in part because the characteristics, and needs are unique for every individual (Ripat and Strock, 2004). It is crucial to understand that there are factors that may continue to restrict the uptake of assistive devices by older adults, and challenges and preferences of older adults with age-related (later life) changes of DSI in relation to assistive technology interventions are somewhat distinct from those with early onset in life (Wittich et al., 2012, 2013, 2016b; Hersh, 2013; Jaiswal et al., 2018, 2019b; Wittich and Simcock, 2019).
Nevertheless, our study highlights that assistive technology can be effective to improve social participation as reported by others (Hersh, 2013; Eurpoean Parliamentary Research Services, 2015; Wittich et al., 2016b; Owuor et al., 2018; Perfect et al., 2018), but how much effort has been invested in research to develop assistive technologies catering to the unique needs of older adults with DSI remains a relevant question globally (Wittich et al., 2016a). Even the work of the World Health Organization on assistive technology misses to recognize the unique aspect of DSI and the need for a distinct set of assistive technologies for this subgroup of older adults with DSI (World Health Organization, 2010, 2016). Future research is warranted to better understand the challenges and preferences of older adults with DSI with respect to rehabilitation interventions and investigate the role of assistive devices and transportation in improving their functioning and social participation.
In terms of services, systems and policies, our participants highlighted the lack of awareness and sensitivity of healthcare providers and other types of service providers (mostly public transit drivers) toward the needs of older adults with DSI. This lack of awareness affects how older adults participate in various domains of community and civic life – be it access to healthcare or outdoor mobility in the community. In line with the study findings of Heine and Browning (2015), McDonnall et al. (2016), Crowe et al. (2019), our study also calls for education of service providers regarding the distinct needs and challenges of older adults with DSI and how to tailor services accordingly (McDonnall et al., 2016; Crowe et al., 2019). To improve rehabilitative outcomes for the older adults with DSI, it is imperative to educate and train healthcare and rehabilitation service providers on DSI (Heine and Browning, 2002, 2015; Saunders and Echt, 2007; McDonnall et al., 2016; Wittich et al., 2016a; Jaiswal et al., 2018; Fraser et al., 2019b). Given that most communication relies on both auditory and visual input in the form of verbal speech and non-verbal cues, enhancing patient-provider communication is highlighted as an important approach to accommodate the distinct sensory needs of older adults with DSI (Saunders and Echt, 2007; Fraser et al., 2019b).
Interestingly, this study on older adults with DSI very well complements the findings of our previous work where we understood the factors influencing social participation among working age adults with DSI in low and middle-income countries (LMICs) such as India (Jaiswal et al., 2019b). The study in India revealed that the individuals who could afford assistive technology, had social support, and were receiving DSI-specific services had more opportunities to participate. In the same study, lack of awareness on DSI among the general public, associated negative attitudes, limited access to resources, and inaccessible built environments were reported as barriers to their participation. It is worth to note that, despite the huge difference in economies in between the two countries (Canada and India), some of the challenges faced by both participant groups (working age adults versus older adults with DSI) remain alike where others are different. For instance, assistive technology, and social support could play a tremendous role in enabling participation of those with DSI, regardless of geographical location, the question is whether we can provide enabling, non-discriminating, and supportive environments and resources to help those with DSI to overcome participation challenges due to impairment and inherent disabling societal barriers.
In contrast, the culture of social support varies dramatically between the two countries. In Canada, caregiving of older adults with impairment relies heavily on formal health and social care system and services, while in India, caregiving for an older adult with impairment is often perceived as the responsibility of immediate family with the support of rehabilitation services. While affordability of assistive technology and access to rehabilitation services remain an important question for many with DSI in India due to limited resources and paying capacity (Jaiswal et al., 2019a, b), assistive technology and rehabilitation services are provided at no- or nominal cost to those with DSI in many parts of Canada, in particular in Quebec where our study was conducted (Wittich et al., 2012, 2014). Both scenarios present their own set of challenges, where in India access to technology or services remains a big challenge (Paul et al., 2016; World Health Organization, 2018; Jaiswal et al., in press), training in the use of assistive devices, and their abandonment remains a problem with service users in high-income countries such as Canada (Wittich et al., 2016b; Lorenzini and Wittich, 2019). It is interesting to note that across different settings and contexts there are common challenges throughout the world with regards to DSI and human rights (World Federation of the Deafblind, 2018; Simcock and Wittich, 2019).
In the quest of improving social participation of older adults with DSI, our study underscores the need to emphasize the person-environment fit to enable social participation where the environmental factors indicate how the environment/context influences participation and individual factors indicate how in-person factors shape participation experiences. Given the need to understand the effect and complex interplay of DSI and the environment on an individual, an interdisciplinary team of professionals from the disciplines of gerontology, vision, hearing, cognition, psychology, and rehabilitation are required to work together to conduct assessments and design interdisciplinary interventions to cater to the distinct needs of older adults with DSI and enhance their social participation (Heine and Browning, 2002, 2015; Saunders and Echt, 2007; McDonnall et al., 2016; Wittich et al., 2016a; Jaiswal et al., 2018; Heine et al., 2019; Fraser et al., 2019b). For professionals working with older adults with DSI, the key focus of interventions should be on the person-environment fit where the intervention goes beyond the older adults’ immediate environment and considers the influence of contextual factors (barriers and facilitators) at the micro, meso, and macro-level. Furthermore, longitudinal studies are needed to attain the person-environment fit across the lifespan, considering the changing health status, and needs of older adults.
From an ICF perspective, our study highlights how different participation domains of life (e.g., community, social, and civic life) are influenced by the interplay of individual factors (e.g., acceptance of one’s disability) and environmental factors (e.g., use of assistive technology). For instance, the stigma of using a hearing aid or another assistive device by an older adult with DSI in the community could be overcome by changing one’s attitude toward self, sensory loss, and assistive aids (at an individual level) and reducing the negative stereotypes that others may have about aging and disability (at an environmental level). Otherwise, this complex interplay of contextual factors may result in a barrier to social participation and lead to social exclusion and poor quality of life of older adults with DSI. This finding has been confirmed in other populations of older adults as well (Dionigi, 2015; Fraser et al., 2016).
Moreover, this study extends our knowledge of individual factors that may influence social participation such as (1) onset and type of impairment, and (2) attitude toward self and acceptance of one’s disability. It is noteworthy that the gradual onset of vision and hearing impairment caused participation challenges for older adults with DSI in activities of daily living important to them, such as reading a book or a newspaper, watching Television, knitting, cooking, going out for groceries, attending concerts, driving, and many others. This finding is very much aligned with previous work (Crews and Campbell, 2004; Brennan et al., 2005; Schneider et al., 2011; Cimarolli and Jopp, 2014; Guthrie et al., 2016). It is equally interesting to see how attitude toward self and acceptance toward one’s disability emerged as a strong individual factor influencing their participation. This finding is not surprising considering our participants because they are those who have lived the majority of their life without any impairment and now, they have to adapt to their age-related decline in vision and hearing. It is likely their attitude that will help them overcome their challenges and accept the condition, with the available and required adaptations, strategies and tools.
Very few studies have attempted to use the ICF in the context of DSI (Möller, 2003; Möller and Danermark, 2007; Jaiswal et al., 2019b, in press). This study contributes to the limited evidence by applying the ICF to exploring social participation in older adults with DSI and supports the use of the ICF as a guiding framework in research with individuals living with varying degrees of combined visual and hearing impairment. This study could potentially inform the development of ICF Core Sets for DSI to be used in clinical practice (Bickenbach et al., 2012).
Limitations
As indicated in the methodology section, our research participants were living autonomously in the community, were registered with a rehabilitation center, and participating in an adult day center. The support provided by the rehabilitation center likely contributed to their access and use of assistive devices. In terms of the potential limitations of this study, our participants were older adults who voluntarily participated in this study and who were optimally connected with services through organizations for people with DSI, have access to services, and were at an advantage compared to those who could not. Participants’ existing contact with a rehabilitation center could have influenced their responses, since individuals who have received services may have different experiences, and additional information or resources. Moreover, having perspectives from family members, friends, and DSI organization staff could have added a more comprehensive understanding of the contextual factors that influence social participation of older adults with DSI.
Conclusion
This study aimed to explore the barriers and facilitators that older adults with DSI perceive as influencing their social participation. To our knowledge, this was the first study to use the ICF to examine barriers to and facilitators of social participation among this population. We found that assistive technology and devices, accessible transportation, and support from friends or family were the main facilitators while negative attitudes and lack of awareness about DSI among service providers, and poorly maintained built environments were some of the major barriers, as identified by the participants. The findings of the study indicate that interventions to promote social participation among older adults with DSI should be multifaceted and integrate the person, built environment, and the health/social service system. Future studies should identify, develop and assess the effectiveness of such integrated interventions in improving social participation in older adults with DSI and their upstream effects on their overall quality of life. Because of the increasing numbers of older adults worldwide, the experience of social isolation is likely to increase with the rising number of older adults with DSI. More research on the role of environment modifications and the person-environment fit is needed to develop timely rehabilitation interventions aimed to promote social participation of older adults with DSI.
Data Availability Statement
The data transcripts of the interviews conducted for this study can be accessed through the corresponding author, pending the appropriate ethics approval.
Ethics Statement
The studies involving human participants were reviewed and approved by Ethics committee of the Center for Interdisciplinary Research in Rehabilitation of Greater Montreal (CRIR #938–0314). The patients/participants provided their written informed consent to participate in this study.
Author Contributions
SF and WW contributed to the conception and design of the study and completed data collection. AJ performed the data analysis and tested the code book with SF and WW. AJ wrote the first draft of the manuscript while SF and WW contributed to different sections of the manuscript. All authors contributed to manuscript revision, read, and approved the submitted version.
Funding
This study was supported by a grant from the Ministère de la Famille et des Aînés Program: Québec ami des aînés. AJ is a recipient of Health System Impact Postdoctoral fellowship from the Canadian Institutes of Health Research, the Fonds de Recherche du Queìbec – Santeì (FRQS), and the Institut Nazareth et Louis Braille du CISSS de la Monteìreìgie Center (INLB; Funding reference number: HI5 166371).
Conflict of Interest
WW serves as an invited Editor for a special issue in the journal.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The authors thank Kenneth Southall and Duncan Sanderson for their contribution toward the development of this study, especially in the data collection. The authors especially thank the participants for their time and generosity.
References
Alma, M. A., Van der Mei, S. F., Groothoff, J. W., and Suurmeijer, T. P. B. M. (2012). Determinants of social participation of visually impaired older adults. Qual. Life Res. 21, 87–97. doi: 10.1007/s11136-011-9931-6
Arnadottir, S. A., Gunnarsdottir, E. D., Stenlund, H., and Lundin-olsson, L. (2011). Participation frequency and perceived participation restrictions at older age: applying the International Classification of Functioning, Disability and Health (ICF) framework. Disabil. Rehabil. 33, 2208–2216. doi: 10.3109/09638288.2011.563818
Bickenbach, J. E., Cieza, A., Rauch, A., and Stucki, G. (2012). ICF CORE SETS - Manual for Clinical Pratice. Boston, MA: Hogrefe Publishing.
Binns, A. M., Bunce, C., Dickinson, C., Harper, R., Tudor-Edwards, R., Woodhouse, M., et al. (2012). How effective is low vision service provision? A systematic review. Surv. Ophthalmol. 57, 34–65. doi: 10.1016/j.survophthal.2011.06.006
Brennan, M., Horowitz, A., and Su, Y. P. (2005). Dual sensory loss and its impact on everyday competence. Gerontologist 45, 337–346. doi: 10.1093/geront/45.3.337
Carabellese, C., Appollonio, I., Rozzini, R., Bianchetti, A., Frisoni, G. B., Frattola, L., et al. (1993). Sensory impairment and quality of life in a community elderly population. J. Am. Geriatr. Soc. 41, 401–407. doi: 10.1111/j.1532-5415.1993.tb06948.x
Cimarolli, V. R., and Jopp, D. S. (2014). Sensory impairments and their associations with functional disability in a sample of the oldest-old. Qual. Life Res. 23, 1977–1984. doi: 10.1007/s11136-014-0657-0
Cosh, S., Von Hanno, T., Helmer, C., Bertelsen, G., Delcourt, C., and Schirmer, H. (2018). The association among visual, hearing and dual sensory loss with depression and anxiety over six years: the Tromsø Study. Int. J. Geriatr. Psychiatry 33, 598–605. doi: 10.1002/gps.4827
Creswell, J. W. (2013). Qualitative Inquiry and Research Design: Choosing Among Five Approaches (Third). Los Angeles: SAGE Publications Inc.
Crews, J. E., and Campbell, V. A. (2004). Vision impairment and hearing loss among community-dwelling older Americans: implications for health and functioning. Am. J. Public Health 94, 823–829. doi: 10.2105/ajph.94.5.823
Crowe, K., Hovaldt, H. B., and Dammeyer, J. (2019). Communication participation in older adults with dual sensory loss. Speech Lang. Hear. doi: 10.1080/2050571X.2019.1623457 [Epub ahead of print].
Dionigi, R. A. (2015). Stereotypes of aging: their effects on the health of older adults. J. Geriatr. 2015, 1–9. doi: 10.1155/2015/954027
Eurpoean Parliamentary Research Services (2015). Assistive Technologies to Support People with Disabilities. Available online at: http://www.europarl.europa.eu/EPRS/EPRS-Briefing-559513-Assistive-technologies-support-people-with-disabilities-FINAL.pdf (accessed December 28, 2018).
Eyssen, I. C., Steultjens, M. P., Dekker, J., and Terwee, C. B. (2011). A systematic review of instruments assessing participation: challenges in defining participation. Arch. Phys. Med. Rehabil. 92, 983–997. doi: 10.1016/j.apmr.2011.01.006
Fakoya, O. A., McCorry, N. K., and Donnelly, M. (2020). Loneliness and social isolation interventions for older adults: a scoping review of reviews. BMC Public Health 20:129. doi: 10.1186/s12889-020-8251-6
Fletcher, P., and Guthrie, D. M. (2013). The lived experiences of individuals with acquired deafblindness: challenges and the future. Int. J. Disabil. Commun. Rehabil. 12:44.
Fraser, S., Beeman, I., Southall, K., and Wittich, W. (2019a). Stereotyping as a barrier to the social participation of older adults with low vision: a qualitative focus group study. BMJ Open 9, 5–8. doi: 10.1136/bmjopen-2019-029940
Fraser, S., Kenyon, V., Lagacé, M., Wittich, W., and Southall, K. E. (2016). Stereotypes associated with age-related conditions and assistive device use in Canadian Media. Gerontologist 56, 1023–1032. doi: 10.1093/geront/gnv094
Fraser, S., Southall, K. E., and Wittich, W. (2019b). Exploring professionals’ experiences in the rehabilitation of older clients with dual-sensory impairment. Can. J. Aging 38, 481–492. doi: 10.1017/S0714980819000035
Fusch, P. I., and Ness, L. R. (2015). Are we there yet? Data saturation in qualitative research. Qual. Rep. 20, 1408–1416.
Gale, N. K., Heath, G., Cameron, E., Rashid, S., and Redwood, S. (2013). Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med. Res. Methodol. 13:117. doi: 10.1186/1471-2288-13-117
Gopinath, B., Schneider, J. M., McMahon, C. M., Burlutsky, G., Leeder, S. R., and Mitchell, P. (2013). Dual sensory impairment in older adults increases the risk of mortality: a population-based study. PLoS One 8:e55054. doi: 10.1371/journal.pone.0055054
Guthrie, D. M., Declercq, A., Finne-Soveri, H., Fries, B. E., and Hirdes, J. (2016). The health and well-being of older adults with dual sensory impairment (DSI) in Four Countries. PLoS One 11:e0155073. doi: 10.1371/journal.pone.0155073
Hammel, J., Magasi, S., Heinemann, A., Gray, D. B., Stark, S., Kisala, P., et al. (2015). Environmental barriers and supports to everyday participation: a qualitative insider perspective from people with disabilities. Arch. Phys. Med. Rehabil. 96, 578–588. doi: 10.1016/j.apmr.2014.12.008
Hammel, J., Magasi, S., Heinemann, A., Whiteneck, G., Bogner, J., and Rodriguez, E. (2008). What does participation mean? An insider perspective from people with disabilities. Disabil. Rehabil. 30, 1445–1460. doi: 10.1080/09638280701625534
Heine, C., and Browning, C. (2015). Dual sensory loss in older adults: a systematic review. Gerontologist 55:gnv074. doi: 10.1093/geront/gnv074
Heine, C., and Browning, C. J. (2002). Communication and psychosocial consequences of sensory loss in older adults: overview and rehabilitation directions. Disabil. Rehabil. 24, 763–773. doi: 10.1080/09638280210129162
Heine, C., Gong, C. H., and Browning, C. (2019). Dual sensory loss, mental health, and wellbeing of older adults living in China. Front. Public Health 7:92. doi: 10.3389/fpubh.2019.00092
Hersh, M. A. (2013). Deafblind people, stigma and the use of communication and mobility assistive devices. Technol. Disabil. 25, 245–261. doi: 10.3233/TAD-130394
Holt-Lundstad, J. (2017). The potential public health relevance of social isolation and loneliness: prevalence, epidemiology, and risk factors. Public Policy Aging Rep. 27, 127–130. doi: 10.1093/ppar/prx030
Hsieh, H. F., and Shannon, S. E. (2005). Three approaches to qualitative content analysis. Qual. Health Res. 15, 1277–1288. doi: 10.1177/1049732305276687
Jaiswal, A., Aldersey, H., Wittich, W., Mirza, M., and Finlayson, M. (2018). Participation experiences of people with deafblindness or dual sensory loss: a scoping review of global deafblind literature. PLoS One 13:e0203772. doi: 10.1371/journal.pone.0203772
Jaiswal, A., Aldersey, H., Wittich, W., Mirza, M., and Finlayson, M. (in press). Factors that influence the participation of individuals with deafblindness: a qualitative study with rehabilitation service providers in India. Br. J. Vis. Impair.
Jaiswal, A., Aldersey, H. M., Wittich, W., Mirza, M., and Finlayson, M. (2019a). Meaning and experiences of participation: a phenomenological study with persons with deafblindness in India. Disabil. Rehabil. doi: 10.1080/09638288.2018.1564943 [Epub ahead of print].
Jaiswal, A., Aldersey, H. M., Wittich, W., Mirza, M., and Finlayson, M. (2019b). Using the ICF to identify contextual factors that influence participation of persons with deafblindness. Arch. Phys. Med. Rehabil. 100, 2324–2333. doi: 10.1016/j.apmr.2019.03.010
Krefting, L. (1991). Rigor in qualitative research: the assessment of trustworthiness. Am. J. Occup. Ther. 45, 214–222. doi: 10.5014/ajot.45.3.214
Laliberte Rudman, D., Gold, D., McGrath, C., Zuvela, B., Spafford, M. M., and Renwick, R. (2016). Why would i want to go out: age-related vision loss and social participation. Can. J. Aging 35, 465–478. doi: 10.1017/S0714980816000490
LeJeune, B. J. (2010). Aging with dual sensory loss: thoughts from consumer focus groups. AER J. 3, 146–152.
Levasseur, M., Desrosiers, J., and Whiteneck, G. (2010). Accomplishment level and satisfaction with social participation of older adults: association with quality of life and best correlates. Qual. Life Res. 19, 665–675. doi: 10.1007/s11136-010-9633-5
Lorenzini, M., and Wittich, W. (2019). Factors related to the use of magnifying low vision aids: A scoping review. Disabil. Rehabil. doi: 10.1080/09638288.2019.1593519 [Epub ahead of print].
Mallinson, T., and Hammel, J. (2010). Measurement of participation: intersecting person, task, and environment. Arch. Phys. Med. Rehabil. 91, S29–S33. doi: 10.1016/j.apmr.2010.04.027
Martin Ginis, K. A., Evans, M. B., Mortenson, W., and Ben Noreau, L. (2017). Broadening the conceptualization of participation of persons with physical disabilities: a configurative review and recommendations. Arch. Phys. Med. Rehabil. 98, 395–402. doi: 10.1016/j.apmr.2016.04.017
McDonnall, M. C., and Capella-McDonnall, M. E. (2009). The effects of developing a dual sensory loss on depression in older adults: a longitudinal study. J. Aging Health 21, 1179–1199. doi: 10.1177/0898264309350077
McDonnall, M. C., Crudden, A., Lejeune, B. J., Steverson, A., and Donnell, N. O. (2016). Needs and challenges of seniors with combined hearing and vision loss. J. Vis. Impair. Blind. 110, 399–411. doi: 10.1177/0145482X1611000603
Meulenkamp, T. M., Cardol, M., van der Hoek, L. S., Francke, A. L., and Rijken, M. (2013). Participation of people with physical disabilities: three-year trend and potential for improvement. Arch. Phys. Med. Rehabil. 94, 944–950. doi: 10.1016/j.apmr.2012.12.017
Mick, P., Parfyonov, M., Wittich, W., Phillips, N., and Pichora-Fuller, M. (2018). Associations between sensory loss and social networks, participation, support, and loneliness [Associations entre la perte sensorielle et les réseaux, la participation et le soutien sociaux ainsi que la solitude]. Can. Fam. Phys. 64, 33–41.
Möller, K. (2003). Deafblindness: a challenge for assessment–is the ICF a useful tool? Int. J. Audiol. 42, (Suppl. 1), S140–S142. doi: 10.3109/14992020309074635
Möller, K., and Danermark, B. (2007). Social recognition, participation, and the dynamic between the environment and personal factors of students with deafblindness. Am. Ann. Deaf 152, 42–55. doi: 10.1353/aad.2007.0012
Owuor, J., Larkan, F., Kayabu, B., Fitzgerald, G., Sheaf, G., Dinsmore, J., et al. (2018). Does assistive technology contribute to social inclusion for people with intellectual disability? A systematic review protocol. BMJ Open 8:e017533. doi: 10.1136/bmjopen-2017-017533
Patton, M. Q., and Cochran, M. (2002). A Guide to Using Qualitative Research Methodology. Médecins Sans Frontières, Paris. Available online at: https://evaluation.msf.org/sites/evaluation/files/a_guide_to_using_qualitative_research_methodology.pdf
Paul, A., Mathew, B., Kumar, U., Rizal, S., and Jaiswal, A. (2016). Early intervention (EI) for children with deafblindness in India: barriers and enablers. Disabil. Int. Dev. 1, 4–11.
Perenboom, R. J. M., and Chorus, A. M. J. (2003). Measuring participation according to the international classification of functioning, disability and health (ICF). Disabil. Rehabil. 25, 577–587. doi: 10.1080/0963828031000137081
Perfect, E., Jaiswal, A., and Davies, T. C. (2018). Systematic review: investigating the effectiveness of assistive technology to enable internet access for individuals with deafblindness. Assistive Technol. 31, 276–285. doi: 10.1080/10400435.2018.1445136
Regie de l’assurance maladie du QUEBEC/RAMQ (2006a). Services Covered in Quebec - Hearing Devices. Available online at: http://www.ramq.gouv.qc.ca/en/citizens/aid-programs/hearing-aids/Pages/hearing-aids.aspx (acccessed January 07, 2020).
Regie de l’assurance maladie du QUEBEC/RAMQ (2006b). Services Covered in Quebec - Visual Devices. Available online at: http://www.ramq.gouv.qc.ca/en/citizens/aid-programs/visual-aids/Pages/visual-aids.aspx (acccessed January 07, 2020).
Ripat, J., and Strock, A. (2004). Users’ perceptions of the impact of electronic aids to daily living throughout the acquisition process. Assist. Technol. 16, 63–72. doi: 10.1080/10400435.2004.10132075
Roets-Merken, L., Zuidema, S., Vernooij-Dassen, M., Dees, M., Hermsen, P., Kempen, G., et al. (2017). Problems identified by dual sensory impaired older adults in long-term care when using a self-management program: a qualitative study. PLoS One 12:0173601. doi: 10.1371/journal.pone.0173601
Sandelowski, M. (1995). Sample size in qualitative research. Res. Nurs. Health 18, 179–183. doi: 10.1002/nur.4770180211
Saunders, B., Sim, J., Kingstone, T., Baker, S., Waterfield, J., Bartlam, B., et al. (2018). Saturation in qualitative research: exploring its conceptualization and operationalization. Qual. Quant. 52, 1893–1907. doi: 10.1007/s11135-017-0574-8
Saunders, G., and Echt, K. V. (2007). An overview of dual sensory impairment in older adults: perspectives for rehabilitation. Trends Amplif. 11, 243–258. doi: 10.1177/1084713807308365
Schneider, J., Gopinath, B., McMahon, C., Leeder, S., Mitchell, P., and Wang, J. (2011). Dual sensory impairment in older age. J. Aging Health 23, 1309–1324. doi: 10.1177/0898264311408418
Schneider, J. M., Gopinath, B., McMahon, C., Teber, E., Leeder, S. S. R., Wang, J. J. J., et al. (2012). Prevalence and 5-year incidence of dual sensory impairment in an older Australian population. Ann. Epidemiol. 22, 295–301. doi: 10.1016/j.annepidem.2012.02.004
Simcock, P., and Wittich, W. (2019). Are older deafblind people being left behind? A narrative review of literature on deafblindness through the lens of the United Nations Principles for Older People. J. Soc. Welf. Fam. Law 41, 339–357. doi: 10.1080/09649069.2019.1627088
Tsai, I.-H., Graves, D. E., Chan, W., Darkoh, C., Lee, M.-S., and Pompeii, L. A. (2017). Environmental barriers and social participation in individuals with spinal cord injury. Rehabil. Psychol. 62, 36–44. doi: 10.1037/rep0000117
Viljanen, A., Törmäkangas, T., Vestergaard, S., and Andersen-Ranberg, K. (2014). Dual sensory loss and social participation in older Europeans. Eur. J. Ageing 11, 155–167. doi: 10.1007/s10433-013-0291-7
Wittich, W., Jarry, J., Groulx, G., Southall, K., and Gagné, J.-P. (2016a). Rehabilitation and research priorities in deafblindness for the next decade. J. Vis. Impair. Blind. 110, 219–231. doi: 10.1177/0145482x1611000402
Wittich, W., Murphy, C., and Mulrooney, D. (2014). An adapted adult day centre for older adults with sensory impairment. Br. J. Vis. Impair. 32, 249–262. doi: 10.1177/0264619614540162
Wittich, W., and Simcock, P. (2019). “Aging and combined vision and hearing loss,” in The Routledge Handbook of Visual Impairment, ed. J. Ravenscroft (New York: Routledge Taylor & Francis Group), 438–456. doi: 10.4324/9781315111353-27
Wittich, W., Southall, K., and Johnson, A. (2016b). Usability of assistive listening devices by older adults with low vision. Disabil. Rehabil. 11, 564–571. doi: 10.3109/17483107.2015.1042076
Wittich, W., Southall, K., Sikora, L., Watanabe, D., and Gagné, J.-P. (2013). What’s in a name: dual sensory impairment or deafblindness? Br. J. Vis. Impair. 31, 198–207. doi: 10.1177/0264619613490519
Wittich, W., Watanabe, D. H., and Gagné, J. P. (2012). Sensory and demographic characteristics of deafblindness rehabilitation clients in Montréal, Canada. Ophthalmic Physiol. Opt. 32, 242–251. doi: 10.1111/j.1475-1313.2012.00897.x
Wong, A. W. K., Ng, S., Dashner, J., Baum, M. C., Hammel, J., Magasi, S., et al. (2017). Relationships between environmental factors and participation in adults with traumatic brain injury, stroke, and spinal cord injury: a cross-sectional multi-center study. Qual. Life Res. 26, 2633–2645. doi: 10.1007/s11136-017-1586-5
World Federation of the Deafblind (2018). At Risk of Exclusion from CRPD and SDGs Implementation: Inequality and Persons with Deafblindness. Oslo: World Federation of the Deafblind.
World Health Organization (2001). International Classification of Functioning, Disability, and Health: ICF. Geneva: World Health Organization.
World Health Organization (2010). Medical Devices: Managing the Mismatch: An Outcome of the Priority Medical Devices Project. Geneva: World Health Organization.
World Health Organization (2013). How to use the ICF: A Practical Manual for using the International Classification of Functioning, Disability and Health (ICF). Geneva: World Health Organization.
World Health Organization (2016). Priority Assistive Products List. The GATE Initiative. Geneva: World Health Organization, 1–16.
Keywords: dual sensory impairment, functioning, older adults, barriers, facilitators, assistive technology, participation
Citation: Jaiswal A, Fraser S and Wittich W (2020) Barriers and Facilitators That Influence Social Participation in Older Adults With Dual Sensory Impairment. Front. Educ. 5:127. doi: 10.3389/feduc.2020.00127
Received: 12 April 2020; Accepted: 29 June 2020;
Published: 16 July 2020.
Edited by:
Douglas F. Kauffman, Medical University of the Americas, United StatesReviewed by:
Hu Jian, Jiangxi University of Finance and Economics, ChinaElisabetta Sagone, University of Catania, Italy
Copyright © 2020 Jaiswal, Fraser and Wittich. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Atul Jaiswal, YXR1bC5qYWlzd2FsQHVtb250cmVhbC5jYQ==
 Atul Jaiswal
Atul Jaiswal Sarah Fraser
Sarah Fraser Walter Wittich
Walter Wittich