- Department of Life Science, Health Science Research Centre, University of Roehampton, London, United Kingdom
“Quisquis amat valeat; pereat qui non-scit amare; bis tanti pereat, quisquis amare vetat”—(Whoever loves, may he be well; may he perish who does not know how to love; may he perish twice as much whoever forbids loving). This graffiti was found in the old city of Pompei. The author is unknown. Possibly a poet but quite possibly an ordinary citizen who in the spur of their passion wanted to share with everyone a pearl of wisdom. Amare in Latin is “to love” and, as in English, it is not just about sex or romance, but also about passion for a cause or an ideal. The Latins knew that to be in love, to have a passion, is to be healthy in the body and as well as in the mind. In this article, I hypothesize that the lack of passion and love in life is one of the main causes of modern diseases and specifically immune/inflammatory diseases. I will explore in layman terms the limitations of specifically focusing on controlling bodily functions without considering the social and emotional dimensions of one's life. Lastly, I will highlight the importance of cooperative research, engagement with the public and education as the way forward for a more effective and democratic model for new socially inclusive therapies.
Philosophy and Immunology: Similarities and Overlaps
Immunology is a relatively new biomedical discipline that has expanded exponentially in the last decades (Cohn, 2017). Even in popular science, the immune system has become a major driver of the quality of our daily living and directly connected to our well-being. Looking at social and daily media we learn that stress is “bad for the immune system” (about 144,000,000 results when typed in Google)—or that an incredibly vast variety of minerals and nutrients are needed “to keep the immune system strong” (about 96,500,000 results when typed in Google)—and, based on very recent evidence, even falling in love has been proposed to be an “immunological process” (Murray et al., 2018).
The reason behind this popularity should not be surprising. Indeed, few people realize that we project onto Immunology the same functions that our pre-decessors gave to Philosophy. Indeed, Immunology and Philosophy are greatly similar and have been proposed to be interconnected (Tauber, 1994; Pradeu, 2010, 2019; Pradeu et al., 2013; Anderson, 2014). Philosophy is a creation of the mind that we use as “a way of thinking about the world, the universe, and society.” Philosophy is what we have used every day to cope with the challenges of daily living and to understand better who we are.
Similarly, Immunology is the “language” our physical body uses to relate to the outside world and to adjust to it. Thanks to the immune system we can deal with a myriad of pathogens that are invisible to the naked eye. Both Philosophy and Immunology are concerned with “the inside and outside realities.” Both Philosophy and Immunology are concerned with the Self (Grabar, 1974; Vaz and Varela, 1978; Howes, 1998; Ohashi, 2002), i.e., “the conditions of identity that make one subject of experience distinct from all the other.”
Why has this switch from Philosophy to Immunology happened? And most importantly, how has this impacted the way we look at well-being? To answer these questions, it might be essential to take a few steps back in human history. The rise of specialized and reductionist research of the twentieth century has rendered speculative disciplines like Philosophy vague and unreliable. The main pre-occupation of a philosophical enquiry is the search and understanding of one's philosophical Self, i.e., one's personality, lifestyle and social conditions and emotional intelligence. This journey of self-discovery (know thyself; cit. Socrates) and management of one's well-being was often very painful and uncertain. There was no system of reference, and it required a very high degree of self-reliance. Instead, we have opted for more measurable and “numerical” disciplines like Immunology as these give objective measures about ourselves with minimum effort on our behalf. When we measure bodily functions, we rely on numbers produced by a machine rather than human participation. Through these numbers we ascertain if we are happy or sad, in need of some rest, fit or overweight.
The increased popularity of Genomics (Wall and Tonellato, 2012) is probably one of the best by-products of this new outlook to life. Many scientists are busy searching for a cure for defective genes responsible for obesity (Clément, 2006; Apalasamy and Mohamed, 2015) but few reflect on the fact that these genes do create a problem only when the subject carrying them is following an unhealthy lifestyle or an over caloric diet (Barrès and Zierath, 2016; Wang et al., 2018). As in the case of the search for a stronger and better immune system, we seek outside for something that is missing or malfunctioning inside. We do not take responsibility for what is happening to us or try to understand why we are having these health problems.
To make the problem worse, we have adopted a “Frankenstein” view of our living. The body is just a patchwork of tissues and organs glued together. One is obese because a metabolic gene is not expressed at the required physiological level (Skrypnik et al., 2017; Thaker, 2017)—obesity-associated depression comes from an imbalance of mediators in the brain (Pereira-Miranda et al., 2017)—obesity-driven activation of the immune inflammatory system is the primary determinant of the undesirable appearance of cellulite (de la Casa Almeida et al., 2013). Everything is compartmentalized, and for every single problem there is a prescribed best solution. God forbid thinking there are possible connections between these different issues.
Put together, the compartmentalization of problems and the release from any responsibility for one's health and well-being, has created our current twentieth century crisis in both body and mind well-being. This crisis has been experienced by all including the police (Winters et al., 2015; Chidgey et al., 2018). We keep moving from one solution to another hoping that the “new research” will get it right this time. We have become like a car (all with the same engine and body parts) that one needs to take care of by adding the right lubricants, petrol, and tires. Similar to a car, we can measure what is missing and top it up to bring everything back to “normal” with a single action and solution.
The Expansion of Immunology
Substituting the holistic view of well-being offered by Philosophy with the numbers and measures of reductionist science has not always gone too far. Few non-narrow-minded scientists have started to realize that the problem of well-being needs to be seen in a “transversal way.” A phase of zooming out instead of the reductionist zooming in has been set in motion. System biology, i.e., the holistic view of the functioning of different cells and tissues as part of something bigger, has gradually become popular. In Immunology, new areas of research have emerged such as Behavioral Immunology (Hucklebridge, 2002; Larson, 2002; Gassen et al., 2018) or Eco-Immunology (Ottaviani et al., 2008; Downs et al., 2014; Bowden et al., 2017). In both these cases, researchers have been trying to investigate how the Immune System of a single individual is influenced by the person's specific behavior and by their external environment. As I have already mentioned in my previous writings on this topic (Brod et al., 2014; D'Acquisto et al., 2014; D'Acquisto, 2017), there is now compelling evidence that the immune system is very “plastic” (Perobelli et al., 2015; Gronke et al., 2016; Laurent et al., 2017; Smith et al., 2017) and continually adjusting to whatever we are experiencing at the moment (Dhabhar, 1998, 2003, 2014). This includes a state of anxiety and fear (Salim et al., 2012; Ray et al., 2017) or happiness (Barak, 2006) and laughter (Yim, 2016).
Interestingly, we have just started to appreciate that well-being and living conditions are not only important and relevant to human beings but also other living creatures. Plants can suffer from social isolation (Gagliano et al., 2012; Gagliano and Renton, 2013), trees can talk to each other (Gorzelak et al., 2015), fish can be depressed (Brennan, 2011) or suffer from addictions (Ninkovic and Bally-Cuif, 2006; Klee et al., 2011; Mathur et al., 2011) and rats can be “pro-social” and help other rats in difficulties despite having different fur color (Ben-Ami Bartal et al., 2014).
Current Challenges in the Management of Well-Being
We live in a world where we are constantly told what to do and what we need to achieve. If we were to follow “what is recommended” in everything we do from the food that we eat, a healthy number of hours of sleep, amount of physical exercise and “mental activities” we would be occupied 24 h a day 7 days a week. There would be no time or space to make a single and simple decision because experts who “know better” has already decided on our behalf.
The irony of this situation is that these experts have never met us in person and do not seem to be in touch with reality. They might not know that eating just three of the recommended five-a-day (https://www.nhs.uk/live-well/eat-well/5-a-day-what-counts/) will cost a fortune in certain parts of the world. Instead, one can opt for a much more filling (and cheaper) meal with bad proteins, bad fat and 100% artificially flavored drinks. Equally the experts seem to ignore that mineral water costs substantially more than addictive drinks and that the recommended 30 min of daily exercise or 10,000 steps per day (Tudor-Locke et al., 2011) in a heavily polluted city is more likely to cause lung cancer (Fashi et al., 2015; Guillerm and Cesari, 2015; Kantipudi et al., 2016; Bhopal et al., 2019) (https://www.theguardian.com/cities/2017/feb/13/tipping-point-cities-exercise-more-harm-than-good) than generate a better control of blood glucose. In simple terms, this costly research that is made behind the four closed walls of a lab carries the risk of being utterly irrelevant to the individual (Lowenstein and Castro, 2009; Hwang et al., 2016; Fogel, 2018) that is genuinely trying to improve his/her life and well-being.
This division and lack of communication between the experts and society is also evident in a clinical setting. Compliance and adherence to pharmacological therapies are the most difficult challenges for the health system. Patient distrust in the medical sector as well as in research has never been this high (Schenker et al., 2012; Shoff and Yang, 2012; Grande et al., 2013). From the patient's perspective, it has become almost normal to be told one thing on a Monday and the polar opposite on Friday. And even when the therapies are followed, there are aspects of the disease that are either not considered at all or simply disregarded. This is especially true if those aspects cannot be measured. The best example of this is in the context of immune diseases is fatigue. Rheumatoid arthritis or multiple sclerosis patients (both diseases seriously impair one's overall mobility) can gain enormous benefits from current therapies. However, one common unsolved problem is fatigue or severe depression. Even more aggravating, these patients often refrain from reporting these problems (see for instance this very poignant video titled “Behind the smile” by the National Rheumatoid Arthritis Society https://www.facebook.com/nationalrheumatoidarthritissociety/videos/10154652264647300/) afraid to be perceived as being never satisfied although they “look just fine.”
Another example of incomplete understanding of patient's perspective is a study I have conducted on dream in patients suffering from autoimmune diseases (www.dreamingautoimmunity.com). The sufferers of these conditions experience very vivid dreams that they would reluctantly share with their GP or consultant amid their fear of been referred to a psychiatrist. The simple sharing of these experiences provides them with an enormous emotional and sometimes physical relief (F. D'Acquisto, unpublished data) at no cost or impact on standard pharmacological therapies.
These extreme cases pose the question of what should be really considered as well-being and what can be done in maintaining it. Thus far, I have highlighted that people want to actively control their life, and that when they are not allowed to, they lose interest (and passion)—they become completely disengaged from science and research.
Education and the Immune System
For the non-biomedical readers of this article, it might come as a surprise that immune cells are educated—and that this has a pivotal role in well-being. Evolved and complex species such as humans have a specific type of immune cell called “adaptive.” The name comes from the fact that these cells can adjust themselves and become specialized to respond to a wide range of problems (from viral infection to bacteria and worms). How do they do this? How do they know how to behave best when facing an immense diversity of potential threats that the outside world poses?
The answer is their education. Both T and B cells (two types of adaptive immune cells) undergo an elaborate programme of selection called positive and negative selection whereby they learn one fundamental lesson: to recognize what is “good” and what is “bad” (Santori, 2015; Takaba and Takayanagi, 2017). What is “good” is the cells and tissues of our own body (the immunological Self) and what is “bad” is everything else we consider as non-belonging to us, e.g., bacteria, viruses, and similar. This process of knowing and experiencing what is good or bad for the immune system has been slowly disappearing from our daily life as we have become more and more “clean” and dependent on what the above-mentioned experts sanctioned as “good.”
The lack of contact with the “dirt” (physical and emotional) of the outside world has been deleterious for our well-being and immune system as highlighted by the “hygiene hypothesis” (Stiemsma et al., 2015; Leong et al., 2016; Ege, 2017; Alexandre-Silva et al., 2018). According to this theory, “the decreasing incidence of infections in western countries and more recently in developing countries is at the origin of the increasing incidence of both autoimmune and allergic diseases” (Okada et al., 2010). In layman terms, the reduced chances of the immune system to be educated to fighting infections (or difficult life experiences) have made it unable to distinguish the Self from non-Self. As a consequence of this, there has been an increase of autoimmune diseases, i.e., pathologies where immune cells start to attack self-tissues and self-organs. Many of my colleagues in the immunology field have invested a great deal of their research time in assessing the impact of the hygiene hypothesis in a variety of immune disorders, but very few have tried to understand the psychosocial origin of this phenomenon.
If Aristotle were still with us, he would suggest that we have completely misunderstood his teaching and have confused being “clean and tidy” as being virtuous. Fearful of the possible disastrous consequences of being infected, we carry with us sanitizing gels for our hands 24/7. The market for hand sanitizers has increased from $28 million in 2002 to $402 million in 2015 (https://www.theguardian.com/society/2012/may/13/do-we-really-need-hand-sanitisers). Another classic example of this change of attitude is the “5 s rule” (https://www.independent.co.uk/news/science/five-second-rule-food-dropped-floor-germs-scientists-professor-anthony-hilton-aston-university-a7629391.html) according to which “if food is removed from a contaminated surface quickly enough, the microorganisms on the surface won't have time to transfer, or jump, onto the food.”
This closing up to experiencing the external world together with a lack of being in touch with ourselves has negatively impacted on both our immune systems and on our minds. As I mentioned before, well-being has become something we have no control over. It has become a prescription that even when followed does not hold the promise we have been given. How is this relevant to education and how can educators apply this scientific perspective to the context of learning? Rather than relying on pre-set answers and prescribed truths, students need to engage with dialogues and processes that can be challenging, dangerous and difficult. They need to understand that education is about developing their own truth rather than conforming to what has been prescribed, exactly as the immune system develops in a unique way in response to challenges in life. As educators, how do we foster this process of self-discovery? The answer might be to encourage students to be passionate about challenges in learning as this could be pivotal for their well-being.
Passion, Well-Being, and the Immune System
The idea that passion is good for someone's health and well-being is not new (St-Louis et al., 2016; Lalande et al., 2017). History has shown that passionate people are resilient in body and mind and deal with problems (emotional and physical) in a much better and constructive way compared to those that lack motivation. This is of course also very true in the context of the immune response. According to several studies of Steven Cole—eudaimonic people (Fredrickson et al., 2013, 2015; Cole et al., 2015; Davis et al., 2015) respond better to infections compared to hedonic.
The argument that eudaimonia—i.e., one's fulfillment and a meaningful life—is the future cure for the weakening of the immune system and today's poor well-being is not far-fetched and not just a thought-construction that I am trying to make here. The critical point is that eudaimonia supports the concept of personal fulfillment. It recognizes that we are all different and that we are in the first place responsible for keeping our body healthy. This is hugely relevant in the context of an immune response. As I have mentioned before we are all immunologically different and the very same seasonal flu can affect some people and not others, and it can be very harmful to some or very mild for others. When one starts to look at all these individuals not as bodies but in their fullness, i.e., their social connections, economic status, personality type and overall attitude to life, patterns emerge. Those who are “full of life” make their own choices, have a pursuit in life and actively engage with their surroundings by adjusting to it, are much better off at maintaining a status of well-being (Zozulya et al., 2008; OŽura et al., 2012; Mirnics et al., 2013; Jandackova et al., 2017; Masafi et al., 2018).
The immune system is one of the sensor organs of well-being. As I stated in my previous work (D'Acquisto, 2017), the immune response is the mirror of our emotional state and lifestyle. One best example that supports this statement is that short bouts of stress cause the immediate mobilization of immune cells in blood as a way to get us ready to “fight the danger” (causing our stress) (Dhabhar et al., 2012). A sustained level of continuous stress leads to a state of immunosuppression that ultimately creates many problems from flu to recurrent infection and pre-mature aging (Dohms and Metz, 1991; Cannizzo et al., 2011; Adamo, 2017; Sharif et al., 2018; Sun and Zhou, 2018). An individual with a eudaimonic approach to life would not engage in activities that cause long-term stress and would most certainly address the causes of their stress rather than counting calories, walking endlessly, or looking at the colors of vegetables.
“Keep calm and carry on” is no-longer a reassuring motto and has now become the leading cause of suppressed frustrations and most likely one of the causes for the increase in allergies and immune disorders. Forcing people to fit into boxes created by bench-based research fosters these frustrations while luring people into thinking that their life might get better if they follow what they have been told. Not for a moment we are told to pay attention to what caused the flaring of symptoms and if there is anything that can be done about it.
This been said, the way we treat diseases is improving as we have started to consider all the unique elements of one's complex living conditions. Social prescribing is the best examples for these changes (Husk et al., 2016; Bickerdike et al., 2017) as it is based on using social interactions to treat diseases. According to the NHS, social prescribing is “helping patients to improve their health, well-being and social welfare by connecting them to community services which might be run by the council or a local charity” (https://www.england.nhs.uk/contact-us/privacy-notice/how-we-use-your-information/public-and-partners/social-prescribing/).
In my view, this is the most crucial aspect of management of well-being. Each individual should be educated to make a decision and take responsibility for it, listened to, and be supported in making their own decision in regards to treatment (Figure 1). Therapies should be participatory and be based on an active input on behalf of the individual. In a recent TV documentary on the mechanisms behind the effects of placebo (https://www.bbc.co.uk/news/health-45721670) it was shown that even when the people enrolled in the study were told that they had been given a placebo, they opted for continuing taking the “drug” as this was found very beneficial to treat their pain. This suggests that when we are actively involved in an activity we are passionate about it, something in our body changes.
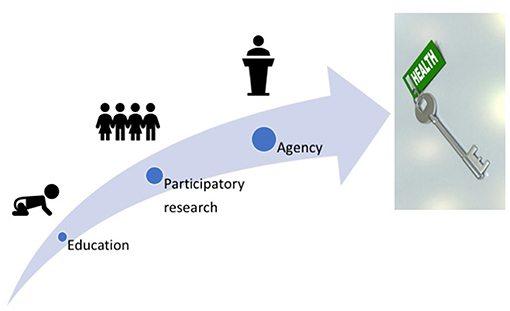
Figure 1. The future management of well-being. An effective system of management of well-being that can be applied to all human beings should be based on an effective system of education that empowers people to distinguish the good from the bad. Participatory research between the lay public and researchers in all fields of science should address health problems that are concerns for the whole society. Finally, the results of these studies should allow individuals to make conscious and independent choices of what needs to be done to keep a state of health and well-being that is unique as we all are.
If this holds true, what would be the implications for the future? I think that most of the health research on well-being we are currently doing should be participatory and more specifically driven by the public. Participatory research (Aungst et al., 2017; Salsberg et al., 2017; English et al., 2018; Kwon et al., 2018) is more informative, more accurate and of high translational value compared to lab-based research. Asking the lay public what they think would improve their health or what is missing in their life might provide us with an immense source of useful data that otherwise would never reach the bench in the lab. Going back to the hygiene hypothesis, in a recent study by Lorimer et al. (Hodgetts et al., 2018), a sample of families within a defined area around the University of Oxford were consulted to provide samples of surface swab from their kitchen choosing in particular areas they thought would be either very clean or very dirty. All the participating families attended group meetings to share the results and to maximize the impact of the findings. From the choice of the sampling method and the objects used for sampling to the motivations behind it this research project with few families has revealed much more information that a classical multicentric studies with thousands of participants around the world. If we were to find a new effective way to tackle the problems caused by the hygiene hypothesis or the ever-growing antibiotic resistance (e.g., the lack of effective antibiotics to treat infections) this would be the most likely to succeed.
Besides the strengths and limitation of participatory design (that will not be discussed here), the simple fact that people were willing to be involved in the research and were happy to lead on it should give us valuable insight in how to best tackle the issue of well-being. Being open to meet and work with the public also offer scientists to explain better and in a more pragmatic way the results of basic research. For my perspective as an immunologist, this type of research that includes an element of education would solve many pressing problems with the treatment of immune disorders. This includes the high risk of mental disorders in patients suffering from immune diseases and the role of emotions and living conditions in the fine-tuning of the inflammatory response.
I welcome and praise initiatives such as the current collection as a system to foster this culture of changes in the lay and scientific communities. It is indeed this kind of work that constitutes the stepping stone to the next level: governmental policy changes in the management of the health system. To achieve this goal, we need to capitalize and invest on education because as one of my colleagues (Prof. Jolanta Opacka-Juffry, University of Roehampton) often says: “there is no legislation without education”.
Author Contributions
The author confirms being the sole contributor of this work and has approved it for publication.
Conflict of Interest Statement
The author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
Adamo, S. A. (2017). The stress response and immune system share, borrow, and reconfigure their physiological network elements: evidence from the insects. Horm. Behav. 88, 25–30. doi: 10.1016/j.yhbeh.2016.10.003
Alexandre-Silva, G. M., Brito-Souza, P. A., Oliveira, A. C. S., Cerni, F. A., Zottich, U., and Pucca, M. B. (2018). The hygiene hypothesis at a glance: early exposures, immune mechanism and novel therapies. Acta Trop. 188, 16–26. doi: 10.1016/j.actatropica.2018.08.032
Anderson, W. (2014). Getting ahead of one's self? The common culture of immunology and philosophy. Isis 105, 606–616. doi: 10.1086/678176
Apalasamy, Y. D., and Mohamed, Z. (2015). Obesity and genomics: role of technology in unraveling the complex genetic architecture of obesity. Hum. Genet. 134, 361–374. doi: 10.1007/s00439-015-1533-x
Aungst, H., Fishman, J. R., and Mcgowan, M. L. (2017). Participatory genomic research: ethical issues from the bottom up to the top down. Annu. Rev. Genomics Hum. Genet. 18, 357–367. doi: 10.1146/annurev-genom-091416-035230
Barak, Y. (2006). The immune system and happiness. Autoimmun. Rev. 5, 523–527. doi: 10.1016/j.autrev.2006.02.010
Barrès, R., and Zierath, J. R. (2016). The role of diet and exercise in the transgenerational epigenetic landscape of T2DM. Nat. Rev. Endocrinol. 12, 441–451. doi: 10.1038/nrendo.2016.87
Ben-Ami Bartal, I., Rodgers, D. A., Bernardez Sarria, M. S., Decety, J., and Mason, P. (2014). Pro-social behavior in rats is modulated by social experience. Elife 3:e01385. doi: 10.7554/eLife.01385
Bhopal, A., Peake, M. D., Gilligan, D., and Cosford, P. (2019). Lung cancer in never-smokers: a hidden disease. J. R. Soc. Med. 1–3 doi: 10.1177/0141076819843654
Bickerdike, L., Booth, A., Wilson, P. M., Farley, K., and Wright, K. (2017). Social prescribing: less rhetoric and more reality. A systematic review of the evidence. BMJ Open 7:e013384. doi: 10.1136/bmjopen-2016-013384
Bowden, R. M., French, S. S., and Demas, G. E. (2017). Introduction to ecoimmunology: An integrative approach. J. Exp. Zool. A Ecol. Integr. Physiol. 327, 219–221. doi: 10.1002/jez.2114
Brennan, C. H. (2011). Zebrafish behavioural assays of translational relevance for the study of psychiatric disease. Rev. Neurosci. 22, 37–48. doi: 10.1515/rns.2011.006
Brod, S., Rattazzi, L., Piras, G., and D'Acquisto, F. (2014). 'As above, so below' examining the interplay between emotion and the immune system. Immunology 143, 311–318. doi: 10.1111/imm.12341
Cannizzo, E. S., Clement, C. C., Sahu, R., Follo, C., and Santambrogio, L. (2011). Oxidative stress, inflamm-aging and immunosenescence. J. Proteomics 74, 2313–2323. doi: 10.1016/j.jprot.2011.06.005
Chidgey, K., Procter, N., Baker, A., and Grech, C. (2018). Police response to individuals displaying suicidal or self-harming behaviours: an integrative review. Health Soc. Care Commun. 27, e112–24. doi: 10.1111/hsc.12668
Clément, K. (2006). Human obesity: toward functional genomics. J. Soc. Biol. 200, 17–28. doi: 10.1051/jbio:2006003
Cohn, M. (2017). Learning from a contemporary history of immunology. Immunol. Res. 65, 573–591. doi: 10.1007/s12026-017-8908-0
Cole, S. W., Levine, M. E., Arevalo, J. M., Ma, J., Weir, D. R., and Crimmins, E. M. (2015). Loneliness, eudaimonia, and the human conserved transcriptional response to adversity. Psychoneuroendocrinology 62, 11–17. doi: 10.1016/j.psyneuen.2015.07.001
D'Acquisto, F. (2017). Affective immunology: where emotions and the immune response converge. Dialogues Clin. Neurosci. 19, 9–19.
D'Acquisto, F., Rattazzi, L., and Piras, G. (2014). Smile–It's in your blood! Biochem. Pharmacol. 91, 287–292. doi: 10.1016/j.bcp.2014.07.016
Davis, L. Z., Slavich, G. M., Thaker, P. H., Goodheart, M. J., Bender, D. P., Dahmoush, L., et al. (2015). Eudaimonic well-being and tumor norepinephrine in patients with epithelial ovarian cancer. Cancer 121, 3543–3550. doi: 10.1002/cncr.29516
de la Casa Almeida, M., Suarez Serrano, C., Roldán Roldan, J., and Jiménez Rejano, J. J. (2013). Cellulite's aetiology: a review. J. Eur. Acad. Dermatol. Venereol. 27, 273–278. doi: 10.1111/j.1468-3083.2012.04622.x
Dhabhar, F. S. (1998). Stress-induced enhancement of cell-mediated immunity. Ann. N. Y. Acad. Sci. 840, 359–372. doi: 10.1111/j.1749-6632.1998.tb09575.x
Dhabhar, F. S. (2003). Stress, leukocyte trafficking, and the augmentation of skin immune function. Ann. N. Y. Acad. Sci. 992, 205–217. doi: 10.1111/j.1749-6632.2003.tb03151.x
Dhabhar, F. S. (2014). Effects of stress on immune function: the good, the bad, and the beautiful. Immunol. Res. 58, 193–210. doi: 10.1007/s12026-014-8517-0
Dhabhar, F. S., Malarkey, W. B., Neri, E., and Mcewen, B. S. (2012). Stress-induced redistribution of immune cells–from barracks to boulevards to battlefields: a tale of three hormones–Curt Richter Award winner. Psychoneuroendocrinology 37, 1345–1368. doi: 10.1016/j.psyneuen.2012.05.008
Dohms, J. E., and Metz, A. (1991). Stress–mechanisms of immunosuppression. Vet. Immunol. Immunopathol. 30, 89–109. doi: 10.1016/0165-2427(91)90011-Z
Downs, C. J., Adelman, J. S., and Demas, G. E. (2014). Mechanisms and methods in ecoimmunology: integrating within-organism and between-organism processes. Integr. Comp. Biol. 54, 340–352. doi: 10.1093/icb/icu082
Ege, M. J. (2017). The Hygiene Hypothesis in the Age of the Microbiome. Ann. Am. Thorac. Soc. 14, S348–S353. doi: 10.1513/AnnalsATS.201702-139AW
English, P. B., Richardson, M. J., and Garzón-Galvis, C. (2018). From crowdsourcing to extreme citizen science: participatory research for environmental health. Annu. Rev. Public Health 39, 335–350. doi: 10.1146/annurev-publhealth-040617-013702
Fashi, M., Agha Alinejad, H., and Asilian Mahabadi, H. (2015). The effect of aerobic exercise in ambient particulate matter on lung tissue inflammation and lung cancer. Iran J Cancer Prev 8:e2333. doi: 10.17795/ijcp2333
Fogel, D. B. (2018). Factors associated with clinical trials that fail and opportunities for improving the likelihood of success: a review. Contemp. Clin. Trials Commun. 11, 156–164. doi: 10.1016/j.conctc.2018.08.001
Fredrickson, B. L., Grewen, K. M., Algoe, S. B., Firestine, A. M., Arevalo, J. M., Ma, J., et al. (2015). Psychological well-being and the human conserved transcriptional response to adversity. PLoS ONE 10:e0121839. doi: 10.1371/journal.pone.0121839
Fredrickson, B. L., Grewen, K. M., Coffey, K. A., Algoe, S. B., Firestine, A. M., Arevalo, J. M., et al. (2013). A functional genomic perspective on human well-being. Proc. Natl. Acad. Sci. U.S.A. 110, 13684–13689. doi: 10.1073/pnas.1305419110
Gagliano, M., and Renton, M. (2013). Love thy neighbour: facilitation through an alternative signalling modality in plants. BMC Ecol. 13:19. doi: 10.1186/1472-6785-13-19
Gagliano, M., Renton, M., Duvdevani, N., Timmins, M., and Mancuso, S. (2012). Out of sight but not out of mind: alternative means of communication in plants. PLoS ONE 7:e37382. doi: 10.1371/journal.pone.0037382
Gassen, J., Prokosch, M. L., Makhanova, A., Eimerbrink, M. J., White, J. D., Proffitt Leyva, R. P., et al. (2018). Behavioral immune system activity predicts downregulation of chronic basal inflammation. PLoS ONE 13:e0203961. doi: 10.1371/journal.pone.0203961
Gorzelak, M. A., Asay, A. K., Pickles, B. J., and Simard, S. W. (2015). Inter-plant communication through mycorrhizal networks mediates complex adaptive behaviour in plant communities. AoB Plants 7:plv050. doi: 10.1093/aobpla/plv050
Grabar, P. (1974). “Self”and “not-self” in immunology. Lancet 1, 1320–1322. doi: 10.1016/S0140-6736(74)90685-0
Grande, D., Shea, J. A., and Armstrong, K. (2013). Perceived community commitment of hospitals: an exploratory analysis of its potential influence on hospital choice and health care system distrust. Inquiry 50, 312–321. doi: 10.1177/0046958013516585
Gronke, K., Kofoed-Nielsen, M., and Diefenbach, A. (2016). Innate lymphoid cells, precursors and plasticity. Immunol. Lett. 179, 9–18. doi: 10.1016/j.imlet.2016.07.004
Guillerm, N., and Cesari, G. (2015). Fighting ambient air pollution and its impact on health: from human rights to the right to a clean environment. Int. J. Tuberc. Lung Dis. 19, 887–897. doi: 10.5588/ijtld.14.0660
Hodgetts, T., Grenyer, R., Greenhough, B., Mcleod, C., Dwyer, A., and Lorimer, J. (2018). The microbiome and its publics: a participatory approach for engaging publics with the microbiome and its implications for health and hygiene. EMBO Rep. 19:e45786. doi: 10.15252/embr.201845786
Howes, M. (1998). The self of philosophy and the self of immunology. Perspect. Biol. Med. 42, 118–130. doi: 10.1353/pbm.1998.0046
Hucklebridge, F. (2002). Behavioral conditioning of the immune system. Int. Rev. Neurobiol. 52, 325–351. doi: 10.1016/S0074-7742(02)52015-8
Husk, K., Blockley, K., Lovell, R., Bethel, A., Bloomfield, D., Warber, S., et al. (2016). What approaches to social prescribing work, for whom, and in what circumstances? A protocol for a realist review. Syst. Rev. 5:93. doi: 10.1186/s13643-016-0269-6
Hwang, T. J., Carpenter, D., Lauffenburger, J. C., Wang, B., Franklin, J. M., and Kesselheim, A. S. (2016). Failure of investigational drugs in late-stage clinical development and publication of trial results. JAMA Intern. Med. 176, 1826–1833. doi: 10.1001/jamainternmed.2016.6008
Jandackova, V. K., Koenig, J., Jarczok, M. N., Fischer, J. E., and Thayer, J. F. (2017). Potential biological pathways linking Type-D personality and poor health: a cross-sectional investigation. PLoS ONE 12:e0176014. doi: 10.1371/journal.pone.0176014
Kantipudi, N., Patel, V., Jones, G., Kamath, M. V., and Upton, A. R. M. (2016). Air pollution's effects on the human respiratory system. Crit. Rev. Biomed. Eng. 44, 383–395. doi: 10.1615/CritRevBiomedEng.2017019757
Klee, E. W., Ebbert, J. O., Schneider, H., Hurt, R. D., and Ekker, S. C. (2011). Zebrafish for the study of the biological effects of nicotine. Nicotine Tob. Res. 13, 301–312. doi: 10.1093/ntr/ntr010
Kwon, S. C., Tandon, S. D., Islam, N., Riley, L., and Trinh-Shevrin, C. (2018). Applying a community-based participatory research framework to patient and family engagement in the development of patient-centered outcomes research and practice. Transl. Behav. Med. 8, 683–691. doi: 10.1093/tbm/ibx026
Lalande, D., Vallerand, R. J., Lafrenière, M. K., Verner-Filion, J., Laurent, F. A., Forest, J., et al. (2017). Obsessive passion: a compensatory response to unsatisfied needs. J. Pers. 85, 163–178. doi: 10.1111/jopy.12229
Larson, S. J. (2002). Behavioral and motivational effects of immune-system activation. J. Gen. Psychol. 129, 401–414. doi: 10.1080/00221300209602104
Laurent, P., Jolivel, V., Manicki, P., Chiu, L., Contin-Bordes, C., Truchetet, M. E., et al. (2017). Immune-mediated repair: a matter of plasticity. Front. Immunol. 8:454. doi: 10.3389/fimmu.2017.00454
Leong, R. W., Mitrev, N., and Ko, Y. (2016). Hygiene hypothesis: is the evidence the same all over the World? Dig. Dis. 34, 35–42. doi: 10.1159/000442922
Lowenstein, P. R., and Castro, M. G. (2009). Uncertainty in the translation of preclinical experiments to clinical trials. Why do most phase III clinical trials fail? Curr. Gene Ther. 9, 368–374. doi: 10.2174/156652309789753392
Masafi, S., Saadat, S. H., Tehranchi, K., Olya, R., Heidari, M., Malihialzackerini, S., et al. (2018). Effect of stress, depression and type D personality on immune system in the incidence of coronary artery disease. Open Access Maced. J. Med. Sci. 6, 1533–1544. doi: 10.3889/oamjms.2018.217
Mathur, P., Berberoglu, M. A., and Guo, S. (2011). Preference for ethanol in zebrafish following a single exposure. Behav. Brain Res. 217, 128–133. doi: 10.1016/j.bbr.2010.10.015
Mirnics, Z., Heincz, O., Bagdy, G., Surányi, Z., Gonda, X., Benko, A., et al. (2013). The relationship between the big five personality dimensions and acute psychopathology: mediating and moderating effects of coping strategies. Psychiatr. Danub. 25, 379–388.
Murray, D. R., Haselton, M. G., Fales, M., and Cole, S. W. (2018). Falling in love is associated with immune system gene regulation. Psychoneuroendocrinology 100, 120–126. doi: 10.1016/j.psyneuen.2018.09.043
Ninkovic, J., and Bally-Cuif, L. (2006). The zebrafish as a model system for assessing the reinforcing properties of drugs of abuse. Methods 39, 262–274. doi: 10.1016/j.ymeth.2005.12.007
Ohashi, P. S. (2002). Immunology. Exposing thy self. Science 298, 1348–1349. doi: 10.1126/science.1079323
Okada, H., Kuhn, C., Feillet, H., and Bach, J. F. (2010). The 'hygiene hypothesis' for autoimmune and allergic diseases: an update. Clin. Exp. Immunol. 160, 1–9. doi: 10.1111/j.1365-2249.2010.04139.x
Ottaviani, E., Malagoli, D., Capri, M., and Franceschi, C. (2008). Ecoimmunology: is there any room for the neuroendocrine system? Bioessays 30, 868–874. doi: 10.1002/bies.20801
OŽura, A., Ihan, A., and Musek, J. (2012). Can the big five factors of personality predict lymphocyte counts? Psychiatr. Danub. 24, 66–72.
Pereira-Miranda, E., Costa, P. R. F., Queiroz, V. A.O., Pereira-Santos, M., and Santana, M.L.P. (2017). Overweight and obesity associated with higher depression prevalence in adults: a systematic review and meta-analysis. J. Am. Coll. Nutr. 36, 223–233. doi: 10.1080/07315724.2016.1261053
Perobelli, S. M., Galvani, R. G., Gonçalves-Silva, T., Xavier, C. R., Nóbrega, A., and Bonomo, A. (2015). Plasticity of neutrophils reveals modulatory capacity. Braz. J. Med. Biol. Res. 48, 665–675. doi: 10.1590/1414-431x20154524
Pradeu, T. (2010). [What philosophy can say about immunogenicity]. Presse Med. 39, 747–752. doi: 10.1016/j.lpm.2010.03.012
Pradeu, T., Jaeger, S., and Vivier, E. (2013). The speed of change: towards a discontinuity theory of immunity? Nat. Rev. Immunol. 13, 764–769. doi: 10.1038/nri3521
Ray, A., Gulati, K., and Rai, N. (2017). Stress, anxiety, and immunomodulation: a pharmacological analysis. Vitam. Horm. 103, 1–25. doi: 10.1016/bs.vh.2016.09.007
Salim, S., Chugh, G., and Asghar, M. (2012). Inflammation in anxiety. Adv. Protein Chem. Struct. Biol. 88, 1–25. doi: 10.1016/B978-0-12-398314-5.00001-5
Salsberg, J., Macridis, S., Garcia Bengoechea, E., Macaulay, A. C., and Moore, S. (2017). The shifting dynamics of social roles and project ownership over the lifecycle of a community-based participatory research project. Fam. Pract. 34, 305–312. doi: 10.1093/fampra/cmx006
Santori, F. R. (2015). The immune system as a self-centered network of lymphocytes. Immunol. Lett. 166, 109–116. doi: 10.1016/j.imlet.2015.06.002
Schenker, Y., White, D. B., Asch, D. A., and Kahn, J. M. (2012). Health-care system distrust in the intensive care unit. J. Crit. Care 27, 3–10. doi: 10.1016/j.jcrc.2011.04.006
Sharif, K., Watad, A., Coplan, L., Lichtbroun, B., Krosser, A., Lichtbroun, M., et al. (2018). The role of stress in the mosaic of autoimmunity: an overlooked association. Autoimmun. Rev. 17, 967–983. doi: 10.1016/j.autrev.2018.04.005
Shoff, C., and Yang, T. C. (2012). Untangling the associations among distrust, race, and neighborhood social environment: a social disorganization perspective. Soc. Sci. Med. 74, 1342–1352. doi: 10.1016/j.socscimed.2012.01.012
Skrypnik, K., Suliburska, J., Skrypnik, D., Pilarski, Ł., Reguła, J., and Bogdanski, P. (2017). The genetic basis of obesity complications. Acta Sci. Pol. Technol. Aliment. 16, 83–91. doi: 10.17306/J.AFS.2017.0442
Smith, T. D., Nagalla, R. R., Chen, E. Y., and Liu, W. F. (2017). Harnessing macrophage plasticity for tissue regeneration. Adv. Drug Deliv. Rev. 114, 193–205. doi: 10.1016/j.addr.2017.04.012
Stiemsma, L. T., Reynolds, L. A., Turvey, S. E., and Finlay, B. B. (2015). The hygiene hypothesis: current perspectives and future therapies. Immunotargets Ther 4, 143–157. doi: 10.2147/ITT.S61528
St-Louis, A. C., Carbonneau, N., and Vallerand, R. J. (2016). Passion for a cause: how it affects health and subjective well-being. J. Pers. 84, 263–276. doi: 10.1111/jopy.12157
Sun, S., and Zhou, J. (2018). Molecular mechanisms underlying stress response and adaptation. Thorac. Cancer 9, 218–227. doi: 10.1111/1759-7714.12579
Takaba, H., and Takayanagi, H. (2017). The mechanisms of T cell selection in the thymus. Trends Immunol. 38, 805–816. doi: 10.1016/j.it.2017.07.010
Tauber, A. I. (1994). The immune self: theory or metaphor? Immunol. Today 15, 134–136. doi: 10.1016/0167-5699(94)90157-0
Thaker, V. V. (2017). Genetic and epigenetic causes of obesity. Adolesc. Med. State Art Rev. 28, 379–405.
Tudor-Locke, C., Craig, C. L., Brown, W. J., Clemes, S. A., De Cocker, K., Giles-Corti, B., et al. (2011). How many steps/day are enough? For adults. Int. J. Behav. Nutr. Phys. Act 8:79. doi: 10.1186/1479-5868-8-79
Vaz, N. M., and Varela, F. J. (1978). Self and non-sense: an organism-centered approach to immunology. Med. Hypotheses 4, 231–267. doi: 10.1016/0306-9877(78)90005-1
Wall, D. P., and Tonellato, P. J. (2012). The future of genomics in pathology. F1000 Med. Rep. 4:14. doi: 10.3410/M4-14
Wang, T., Xu, M., Bi, Y., and Ning, G. (2018). Interplay between diet and genetic susceptibility in obesity and related traits. Front. Med. 12, 601–607. doi: 10.1007/s11684-018-0648-6
Winters, S., Magalhaes, L., and Kinsella, E. A. (2015). Interprofessional collaboration in mental health crisis response systems: a scoping review. Disabil. Rehabil. 37, 2212–2224. doi: 10.3109/09638288.2014.1002576
Yim, J. (2016). Therapeutic benefits of laughter in mental health: a theoretical review. Tohoku J. Exp. Med. 239, 243–249. doi: 10.1620/tjem.239.243
Keywords: immune system, passion, love, well-being, psychoneuroimmunology
Citation: D'Acquisto F (2019) Quisquis Amat Valeat! (Whoever Loves, May He be Well) Why Love and Passion Are Important for the Well-Being of the Immune System. Front. Educ. 4:62. doi: 10.3389/feduc.2019.00062
Received: 16 January 2019; Accepted: 14 June 2019;
Published: 02 July 2019.
Edited by:
Gavin T. L. Brown, The University of Auckland, New ZealandReviewed by:
Tanja Sobko, The University of Hong Kong, Hong KongMargaret Grogan, Chapman University, United States
Copyright © 2019 D'Acquisto. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Fulvio D'Acquisto, RnVsdmlvLkRhY3F1aXN0b0Byb2VoYW1wdG9uLmFjLnVr
 Fulvio D'Acquisto
Fulvio D'Acquisto