Introduction: Coronavirus disease 2019 (COVID-19) has caused more than 690 million deaths worldwide. Different results concerning the death rates of the Delta and Omicron variants have been recorded. We aimed to assess the secular trend of case fatality rate (CFR), identify risk factors associated with mortality following COVID-19 diagnosis, and investigate the risks of mortality and hospitalization during Delta and Omicron waves in the United States.
Methods: This study assessed 2,857,925 individuals diagnosed with COVID-19 in the United States from January 2020, to June 2022. The inclusion criterion was the presence of COVID-19 diagnostic codes in electronic medical record or a positive laboratory test of the SARS-CoV-2. Statistical analysis was bifurcated into two components, longitudinal analysis and comparative analysis. To assess the discrepancies in hospitalization and mortality rates for COVID-19, we identified the prevailing periods for the Delta and Omicron variants.
Results: Longitudinal analysis demonstrated four sharp surges in the number of deaths and CFR. The CFR was persistently higher in males and older age. The CFR of Black and White remained higher than Asians since January 2022. In comparative analysis, the adjusted hazard ratios for all-cause mortality and hospitalization were higher in Delta wave compared to the Omicron wave. Risk of all-cause mortality was found to be greater 14–30 days after a COVID-19 diagnosis, while the likelihood of hospitalization was higher in the first 14 days following a COVID-19 diagnosis in Delta wave compared with Omicron wave. Kaplan–Meier analysis revealed the cumulative probability of mortality was approximately 2-fold on day 30 in Delta than in Omicron cases (log-rank p < 0.001). The mortality risk ratio between the Delta and Omicron variants was 1.671 (95% Cl 1.615–1.729, log-rank p < 0.001). Delta also had a significantly increased mortality risk over Omicron in all age groups. The CFR of people aged above 80 years was extremely high as 17.33%.
Conclusion: Male sex and age seemed to be strong and independent risk factors of mortality in COVID-19. The Delta variant appears to cause more hospitalization and death than the Omicron variant.
Objectives: There is limited data regarding the prevalence of suicidal risk among physicians during COVID-19, and the risk factors relating to it. Dominant risk factors for suicide among physicians are depression and burnout. Maladaptive perfectionism may also serve as a profound risk factor for suicidality among physicians and may aggravate symptoms of distress under the challenges of COVID-19. This study aims to evaluate current suicidal risk, suicidal ideation, depression, and burnout before and during COVID-19 among physicians in Israel, and to identify the best sets of correlates between perfectionism and burnout, depression and suicidal ideation, during these time periods.
Methods: A sample of 246 Israeli physicians (160 before COVID-19 and 86 during COVID-19) completed online surveys assessing lifetime suicidal risk, suicidal ideation during the last year and current suicidal ideation, depression, burnout symptoms and maladaptive perfectionism.
Results: More than one-fifth of the sample (21.9%) reported high suicidal risk (Lifetime suicidal behaviors). More than one-fourth (27.2%) reported suicidal ideation during the last 12 months; and 13.4% reported suicidal ideation during the last 3 months. In addition, more than one-third (34.6%) exhibited moderate–severe levels of depressive symptoms and more than a half of the sample reported burnout symptoms. Maladaptive perfectionism was positively correlated with current suicidal ideation, burnout, and depression. Moderated serial mediation analysis demonstrated indirect effect of perfectionism on suicidal ideation by its impact on burnout and depression only during COVID-19. Before COVID-19, physicians were more likely to experience depressive symptoms.
Conclusion: Physicians in Israel are at increased risk for depression and suicidal ideation, regardless of the COVID-19 pandemic. Maladaptive perfectionism was found to be a risk factor for burnout, depression, and suicidal ideation. During the first waves of the pandemic, physicians were less likely to experience depressive symptoms. However, among physicians who were characterized with high maladaptive perfectionism, depression served as a significant risk factor for suicidal ideation during the pandemic, which places these individuals at increased risk for suicidality. These results highlight the importance of implementing intervention programs among physicians to reduce suicidal risk and to better identify rigid perfectionism and depressive symptoms.
Introduction: The COVID-19 pandemic continues to ravage the world, and mutations of the SARS-CoV-2 continues. The new strain has become more transmissible. The role of aerosol transmission in the pandemic deserves great attention.
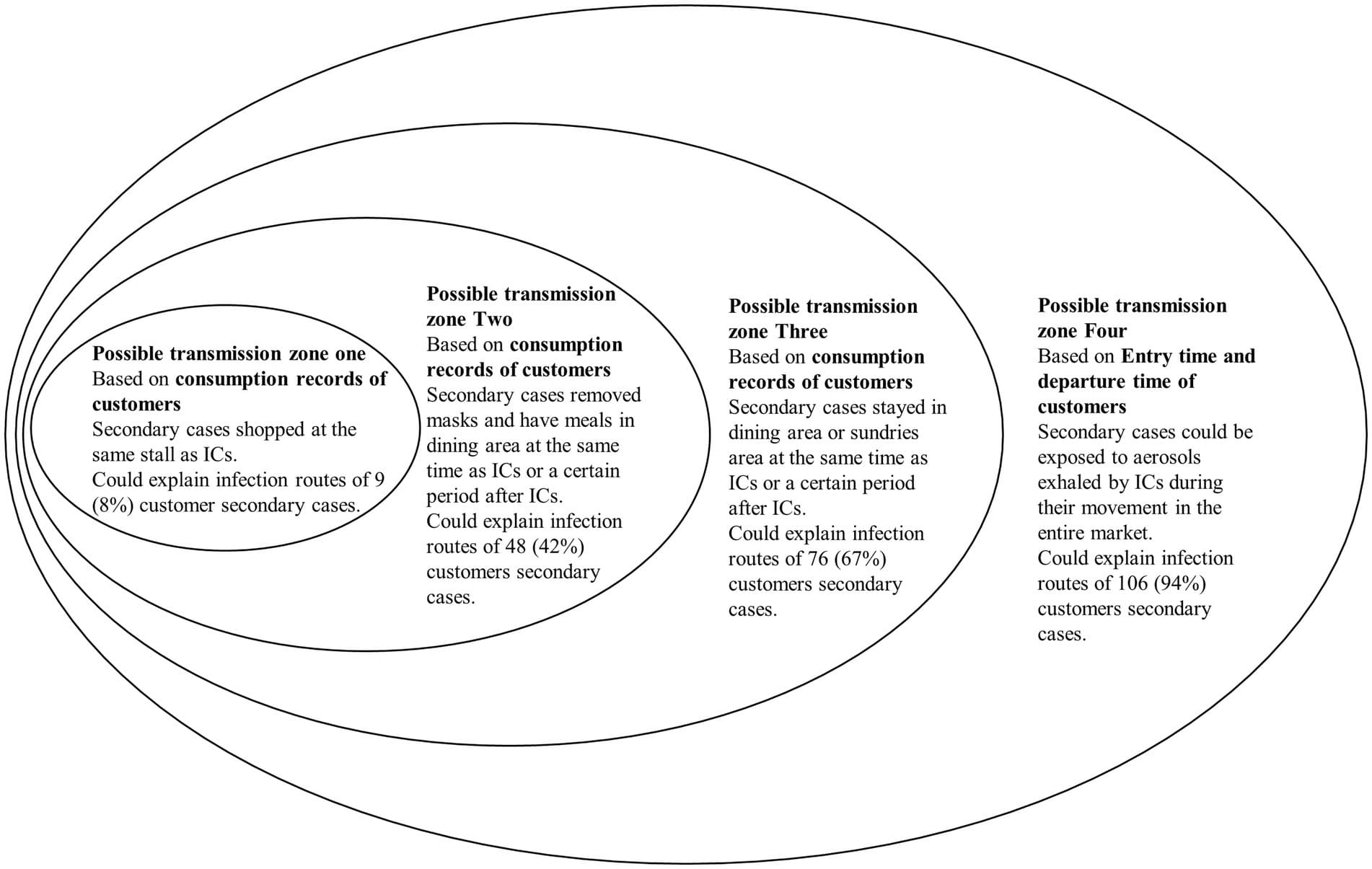
Methods: In this observational study, we collected data from market customers and stallholders who had been exposed to the virus in the Qingkou night market on July 31 and were subsequently infected. We analyzed the possible infection zones of secondary cases and aerosol suspension time in ambient air. We described and analyzed the characteristics of the secondary cases and the transmission routes for customers.
Results: The point source outbreak of COVID-19 in Qingkou night market contained a cluster of 131 secondary cases. In a less-enclosed place like the Qingkou night market, aerosols with BA.5.2 strain released by patients could suspend in ambient air up to 1 h 39 min and still be contagious.
Conclusion: Aerosols with viruses can spread over a relatively long distance and stay in ambient air for a long time in a less enclosed space, but shorter than that under experimental conditions. Therefore, the aerosol suspension time must be considered when identifying and tracing close contact in outbreak investigations.