- Department of Emergency Medicine, The First Affiliated Hospital of Guangxi Medical University, Nanning, China
Objective: This study aimed to evaluate the effectiveness of a virtual reality (VR)-based training program in improving emergency physicians’ ability to manage multi-casualty traffic injuries, compared to conventional training methods.
Methods: A randomized controlled trial was conducted with 76 emergency physicians from a single hospital. Participants were randomly assigned to either the VR group (n = 38) or the control group (n = 38). The VR group underwent immersive training using a VR simulation of multi-casualty traffic accidents, while the control group received traditional lectures and mannequin-based simulations. Primary outcomes included on-site assessment, triage accuracy, and decision-making in transportation, assessed immediately post-training. Secondary outcomes were participant satisfaction and confidence levels.
Results: The VR group performed significantly better in on-site assessments (P < 0.05), triage accuracy (P < 0.05), and transportation decision-making (P < 0.05) compared to the control group. The VR group also reported higher satisfaction and confidence in applying learned skills in real-world situations (P < 0.05).
Conclusion: VR-based training enhances emergency physicians’ performance in managing multi-casualty traffic accidents, demonstrating its potential as a scalable and effective educational tool for emergency medical training.
1 Introduction
Trauma constitutes a significant global cause of death, particularly affecting individuals in the young and middle-aged demographic. According to the World Health Organization’s latest report, more than 1.3 million people die each year from road traffic accidents, and millions more are left disabled, losing both their ability to work and live independently (Razzaghi et al., 2020). This places a substantial burden on society, families, economies, and healthcare systems. In the process of treating road traffic injuries, timely and effective early assessment and intervention are crucial for saving lives, reducing disability, and minimizing complications. In practice, managing victims at the scene of mass casualty incidents from road traffic accidents is often chaotic, requiring emergency physicians to make rapid decisions and respond swiftly to multiple complex injuries (Mohanty et al., 2022). This places increased demands on the routine training of emergency physicians.
Current training for road traffic injury treatment primarily relies on lectures, textbook knowledge, tabletop exercises, or limited mannequin-based simulations (Tune et al., 2023). While these methods are effective in conveying foundational information, traditional simulations are often inadequate in replicating the complexity of real-world environments and sudden, unexpected situations, leaving trainees with insufficient emergency response skills and limited psychological resilience. Additionally, most trainees are unable to play a key leadership role during the actual handling of road traffic injuries (Nelson et al., 2020). A major challenge remains how to improve their emergency management and decision-making abilities without compromising patient safety during the training process.
Virtual reality (VR) is a computer-generated immersive simulation environment that allows users to interact with virtual scenarios, providing a more realistic experience compared to traditional media (Bruno et al., 2022). VR technology has been widely employed across a variety of industries due to its high level of immersion and interactivity (Kanschik et al., 2023). In the field of medical education, VR enables healthcare providers to practice procedures and make decisions within virtual clinical scenarios (Kanschik et al., 2023; Chiang et al., 2022). VR offers several potential advantages: Realism and immersive learning: VR can simulate lifelike medical scenarios, allowing trainees to experience realistic emergencies or trauma situations outside of the classroom (Goel et al., 2023). Repetitive practice: VR environments allow trainees to repeatedly practice specific scenarios until proficiency is achieved, without consuming resources or risking real patients (Just et al., 2024). Personalized training: VR also supports gradually increasing the level of challenge based on a trainee’s initial skills and responses, tailoring learning pathways to match individual proficiency levels (Ramalho et al., 2024). VR technology has been shown to improve learning outcomes and practical skills in areas such as disaster response (Kman et al., 2023), cardiopulmonary resuscitation (CPR) training (Cerezo Espinosa et al., 2019), and surgical skills practice (Fahl et al., 2023). However, there remains limited application and research on the use of VR in complex, multi-casualty settings like road traffic accident emergency care. While traditional training methods can simulate common traffic accident scenarios, they often fall short in presenting the detailed, dynamic complexities of multiple trauma injuries and team-based responses. More academic research is needed to substantiate the effectiveness of VR in training healthcare providers in such high-risk environments.
Based on the aforementioned background information, existing literature indicates that virtual reality technology is paving new educational pathways across various fields, including healthcare (Wang et al., 2024). However, its application in the management of complex and sudden road traffic accident emergencies remains underexplored. To address this research gap, this study employs a randomized controlled trial design to investigate whether virtual reality-based emergency medical training can address the limitations of traditional training methods, and to explore new approaches for enhancing trainees’ emergency response and decision-making abilities.
2 Materials and methods
2.1 Study design, setting, and ethics
This was a randomized, controlled trial of an educational intervention (VR simulation-based training). This study was conducted in the Emergency Department of Guangxi Zhuang Autonomous Region People’s Hospital from February 2024 to August 2024. All participants expressed interest in the study and provided informed consent, and underwent corresponding tests after a 3-h course. The course consisted of lectures, VR simulation training, scenario case analysis, and tabletop exercises.
The study was approved by the Ethics Committee of Guangxi Zhuang Autonomous Region People’s Hospital (KY-SY-2023–014). Informed consent was obtained from each participant, who signed the consent form prior to participation in the study.
2.2 Participants
This study recruited emergency physicians and resident trainees working in emergency department. Participants were selected based on the following inclusion and exclusion criteria. Inclusion criteria: Physicians with at least 1 year of experience in emergency medicine, willingness to participate and provide informed consent. Exclusion criteria were refusal to the study, having previously received VR-based emergency medical training before, diagnosed with cognitive or psychiatric conditions that may interfere with training comprehension, and were unable to complete the full course and tests duration of the study.
The participants were randomized into the control and VR groups in a 1:1 ratio using Excel software. Excel offered various functions that can generate random numbers, thereby facilitating random assignment. Specifically, random numbers were generated for each participant using Excel’s RAND function, and group assignment was based on the generated values. After randomization, baseline characteristics of the two groups, including age, gender, years of experience, and previous training, were compared to ensure balance between the groups.
2.3 Intervention
Participants in the VR group underwent a comprehensive, interactive training program designed specifically for emergency trauma treatment in road traffic accident scenarios, lasting a total of 180 min across two afternoons. The virtual reality scenario presented various complex trauma cases, including multi-casualty incidents, with realistic simulations of injuries commonly seen in road traffic accidents (e.g., Severe traumatic brain injury, aerothorax, multiple fractures, abdominal injuries). During the training process, the HTC VIVE VR device (Road Traffic Injury VR Software 1.0, developed by the Emergency Department of Guangxi Zhuang Autonomous Region People’s Hospital) was utilized. Each participant was required to practice emergency response, on-site assessment, triage, injury assessment and initial handling, transportation and evacuation during the VR training process. VR participants will had 10 min to familiarize themselves with the equipment as a group, included in the total training time.
To ensure consistency with the VR group, the control group also had 10 min allocated for familiarization with the training props used in the tabletop exercises. This time is included within the overall 180-min training duration. The control group’s training consists of lectures covering basic theoretical knowledge, followed by tabletop exercises where participants simulate road traffic accident scenes and discuss injury cases such as severe traumatic brain injuries and multiple fractures. These scenarios, focusing on injury assessment, triage, and emergency management, were designed to align closely with those in the VR training. Both groups engaged with similar content, ensuring that the control group’s learning experience was comparable.
2.4 Outcome measures
The primary and secondary outcome measures in this randomized controlled trial were designed to evaluate the effectiveness. These measures encompassed both objective performance metrics and subjective assessments from participants. The objective effectiveness of VR simulation was measured using three different aspects. Firstly, the on-site assessment process included preliminary investigation of the traffic accident site, analysis of injury mechanisms, assessment of safety hazards of the accident vehicle, and liaison with other departments. Secondly, Triage accuracy assessed the precision of participants in categorizing victims of varying injury severities using standardized triage models (START). Correct triage decisions were crucial for managing mass casualty incidents. The third aspect was the evaluation of the decision-making time and transportation decisions made by participants throughout the entire process. All primary outcome measures were evaluated using a standardized 4-point Likert scale, where 1 represents poor performance (inadequate or incorrect actions) and 4 represents excellent performance (timely and accurate execution of tasks as per clinical guidelines).
The secondary outcomes included participant satisfaction and user experience with the VR training. Training satisfaction was assessed using a post-training questionnaire, rated on a 5-point Likert scale, evaluating overall satisfaction, perceived relevance to clinical practice, and confidence in applying learned skills. This questionnaire was adapted from standardized measures based on previous studies (Just et al., 2024; Fahl et al., 2023; Kaim et al., 2024; Kman et al., 2023), ensuring its relevance and validity. VR user experience (specific to the VR group) was assessed via a custom questionnaire measuring the realism of the simulation, ease of use, engagement, and physical comfort, also using a 5-point Likert scale. Descriptive statistics will be calculated for these outcomes, and comparisons between groups were made using independent t-tests or Mann-Whitney U-tests. Additionally, thematic analysis will was performed on qualitative open-ended feedback for further insights.
2.5 VR training experience (VR group only)
Participants in the VR group received an immersive virtual reality training experience, focused on simulating real-world trauma management scenarios. Each participant engaged in 3D interactive simulations that replicated emergency response situations in a traffic accident context. The VR system provided real-time feedback on performance, allowing participants to adjust their operational actions during the simulation under the guidance of the instructor to enhance learning, ensuring they became familiar with the VR system’s interface and controls. Following the training session, participants completed a survey to evaluate their experience based on realism, ease of use, immersion, and physical comfort, using a 5-point Likert scale.
2.6 Statistical analysis
Statistical analyses were performed using SPSS version 25. Descriptive statistics were presented as means ± standard deviations for continuous variables and percentages for categorical variables. Before conducting group comparisons, the normality of continuous variables was assessed using the Shapiro-Wilk test. For normally distributed continuous outcomes, independent t-tests will be used. If the data were not normally distributed, non-parametric tests, such as Mann-Whitney U-tests, were applied. For categorical variables, Chi-square tests or Fisher’s exact tests will be used, depending on the expected frequency of the categories. For secondary outcomes, satisfaction and user experience scores were compared using t-tests. Pearson’s or Spearman’s correlation coefficient will be used to assess relationships between subjective and objective outcomes, depending on the normality of the data. Statistical significance was set at P < 0.05.
3 Result
3.1 Sample characteristics
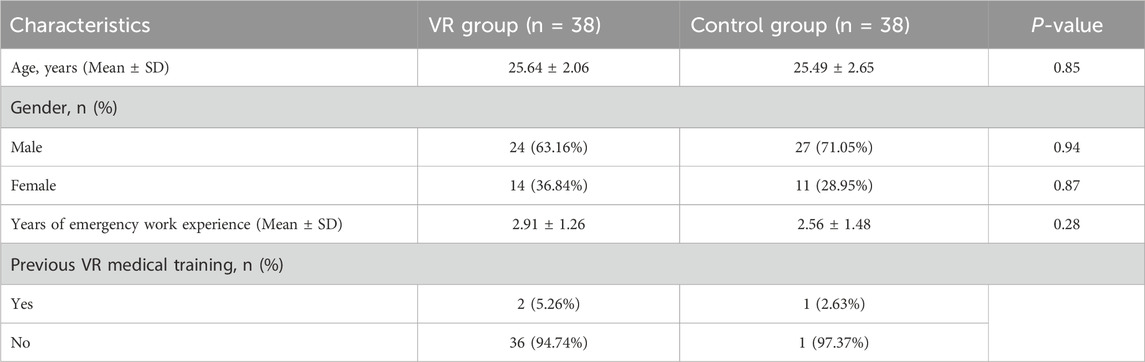
A total of 76 participants were enrolled in the study and randomly assigned in a 1:1 ratio to either the virtual reality (VR) group (n = 38) or the control group (n = 38) (Figures 1, 2). No participants were excluded after randomization, and all completed the study. Table 1 summarizes the baseline characteristics for both groups. The two groups were comparable in terms of age, gender distribution, years of experience in emergency medicine, and previous VR Medical Training. The mean age of participants in the VR group was 25.64 years (SD = 2.06), while in the control group, the mean age was 25.49 years (SD = 2.65) (P = 0.85). The percentage of male participants was 63.16% in the VR group and 71.05% in the control group ((P = 0.94). The mean number of years of experience in emergency care was 2.91 years (SD = 1.26) in the VR group, compared to 2.56 years (SD = 1.48) in the control group (P = 0.28). There were no significant differences between the groups in any of the baseline characteristics, indicating that randomization successfully balanced the two groups.
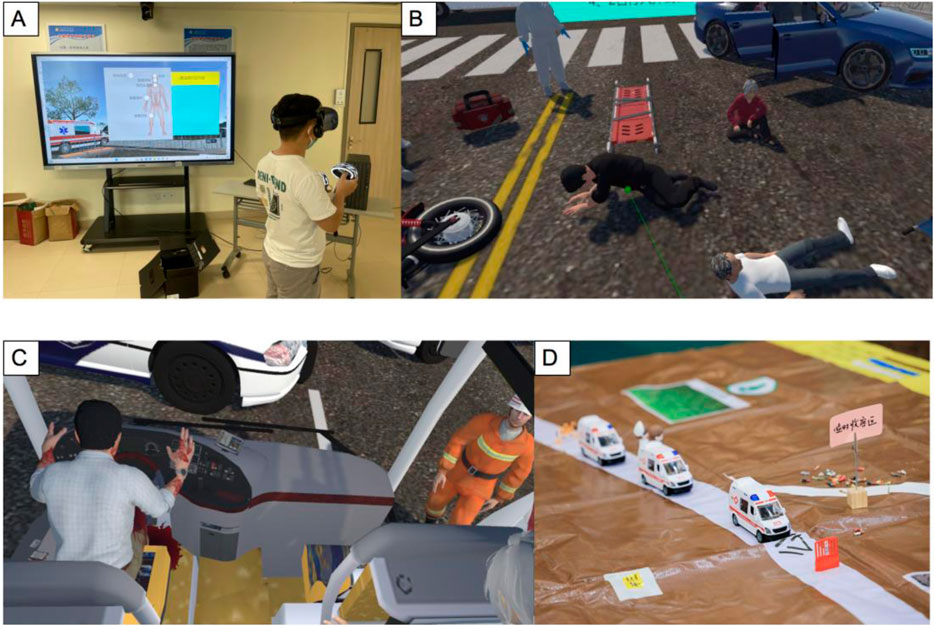
Figure 1. Overview of Training Methods and Group Activities: (A) Students are experiencing the scene of a car accident through VR immersive experiences. (B) In the VR perspective, the participant uses the controller to point to the injured person and proceeds with further actions. (C) The VR Group’s Perspective on Resource Allocation and Decision-Making in the Field. (D) Tabletop Exercise Props for the Control Group, Aligned with the VR Group Scenario.
3.2 Objective effectiveness
In terms of objective performance metrics, the VR group outperformed the control group across all evaluated aspects (Figure 3). The mean score for on-site assessment in the VR group was 2.83 ± 0.82, compared to 2.62 ± 0.88 in the control group (P < 0.05). For triage accuracy, the VR group scored 3.29 ± 0.73, while the control group scored 2.97 ± 0.75(P < 0.05). Similarly, the mean score for transportation decision-making was higher in the VR group (3.27 ± 0.86) compared to the control group (2.97 ± 0.91) (P < 0.05). These results indicate that VR-based training facilitated better overall performance in emergency management tasks than traditional training methods.
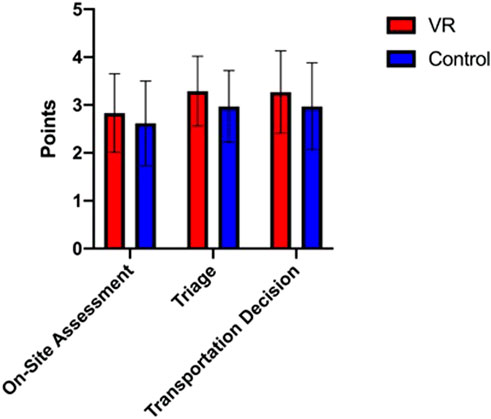
Figure 3. Comparison of VR and conventional training on key emergency management tasks (4-point likert scale).
3.3 Subjective effectiveness
As shown in Table 2, participants in the VR group generally reported higher levels of satisfaction and perceived improvements in various aspects of the training compared to the control group. Regarding understanding of emergency response to traffic accidents, 94.74% of the VR group rated the course positively (scores of 3–5), compared to 73.69% in the control group. Similarly, 50.00% of the VR group indicated significant improvement in practical skills (scores of 4–5), compared to 34.21% in the control group. In terms of applying theoretical knowledge to practical situations, 73.68% of the VR group gave high ratings (scores of 4–5) versus 57.89% in the control group. Both groups rated the course structure favorably, with 65.79% in the VR group and 68.42% in the control group assigning scores of 4–5. However, the VR group reported greater satisfaction with the tools and materials provided (63.16% vs. 39.47%). Additionally, the VR group found the content more comprehensive (78.95% vs. 57.89%) and reported that the course better met their expectations (68.42% vs. 55.26%). Confidence in applying learned skills in real-life emergency situations was also higher in the VR group (68.42% vs. 34.21%). Finally, the VR group reported better preparedness for dealing with traffic accident injuries (73.68% vs. 60.53%) and stronger confidence in executing emergency protocols (55.26% vs. 39.47%).
3.4 Satisfaction with VR groups
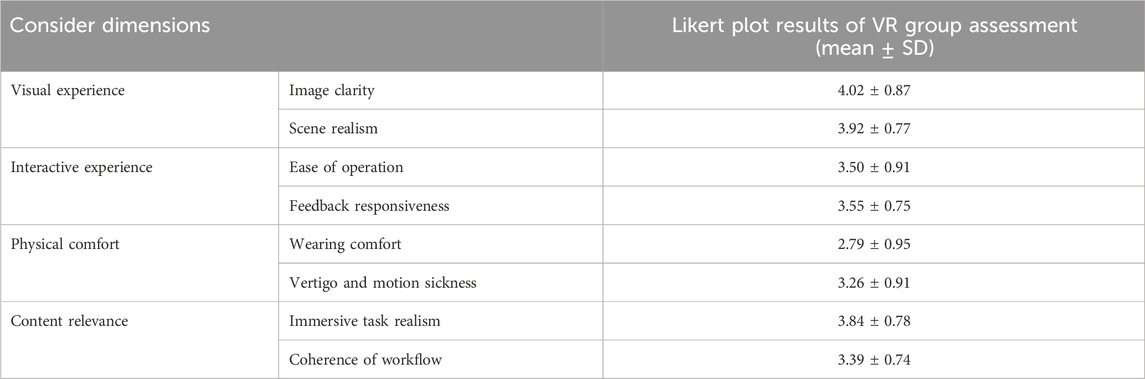
In the VR group, visual experience received generally positive ratings, with image clarity scoring 4.02 ± 0.87 and scene realism at 3.92 ± 0.77, indicating that participants found the visual components of the simulation sufficiently detailed and lifelike. However, the interactive experience was rated slightly lower, with ease of operation at 3.50 ± 0.91 and feedback responsiveness at 3.55 ± 0.75, suggesting that while functional, there may be room for improvement in the intuitiveness and responsiveness of the simulation. In terms of physical comfort, wearing comfort was rated modestly lower at 2.79 ± 0.95, potentially reflecting discomfort or difficulties associated with the VR hardware, although vertigo and motion sickness were moderate at 3.26 ± 0.91, indicating some tolerable levels of discomfort during use. Lastly, content relevance scored well, with immersive task realism rated 3.84 ± 0.78 and workflow coherence at 3.39 ± 0.74, showing that while the content was considered relevant and realistic, the logical progression of tasks could benefit from more streamlining (Table 3).
4 Discussion
In this randomized controlled trial, we demonstrated that virtual reality (VR)-based emergency medical training significantly enhanced participants’ performance in managing multi-casualty injuries resulting from traffic accidents compared with conventional training methods. Specifically, the VR group showed superior outcomes in terms of on-site assessment, triage accuracy, and transportation decision-making. These results suggest that VR offers a more immersive, interactive, and realistic training environment that better prepares emergency physicians for high-stress, real-world emergency scenarios. Furthermore, participants in the VR group reported higher satisfaction and confidence in applying acquired skills to clinical practice, indicating that VR training may also enhance psychological resilience and preparedness. These findings are consistent with previous studies demonstrating the benefits of VR in other areas of medical education, such as surgical training and disaster response (Kaim et al., 2024; Kman et al., 2023); however, our study extends these benefits to the complex and high-stakes setting of traffic accidents involving multiple victims. Overall, this study underscores the potential of VR technology as a superior educational tool for improving both cognitive and practical skills crucial to emergency medical care.
The results of this study align with recent literature demonstrating the effectiveness of VR in medical training across various domains (Yeung et al., 2021), yet our findings extend these benefits to the management of complex multi-casualty traffic accidents. VR training has been increasingly recognized for its ability to enhance the realism and interactivity of medical simulations (Chao et al., 2022), thereby improving skill retention and decision-making (Guo et al., 2021). For example, a 2021 study demonstrated that VR-based surgical training resulted in significantly higher accuracy and shorter procedure time in comparison to traditional methods (Bensky et al., 2021). Similarly, a randomized trial (Hollis et al., 2020) indicated that VR simulation enhanced both cognitive and procedural skills for emergency resuscitation, contributing to improved patient outcomes. These findings are consistent with our current study, where participants in the VR group exhibited superior triage accuracy and decision-making speed. However, while previous research largely focused on procedural skills in controlled environments (e.g., surgery and resuscitation), our study expands VR’s utility to the chaotic and unpredictable nature of trauma care during multi-casualty incidents. This is supported by recent work, such as that by Bensky et al. (2021), which emphasized the importance of immersive VR in improving real-time situational awareness and adaptive decision-making in emergency settings (Bensky et al., 2021). In our study, participants in the VR group demonstrated better handling of multiple trauma cases, indicating that VR may be particularly beneficial in preparing clinicians for dynamic and high-stress scenarios common in traffic accidents.
Moreover, the present study adds to the growing body of evidence advocating for the psychological resilience VR training provides in emergency care. A study noted that VR-based training significantly reduced trainee anxiety and enhanced confidence in coping with stressful medical situations, findings that are mirrored in our own data, with the VR group reporting higher self-confidence after training (Hollis et al., 2020). These benefits are likely attributable to VR’s immersive environment, which replicates real-world complexities more effectively than traditional simulations. Despite the promising results, there remains a need for more research on the long-term retention of skills learned through VR. Studies, such as the one conducted by Laing et al. (2023), highlight the potential for VR to improve long-term knowledge retention, though empirical validation in emergency medical contexts is still required (Laing et al., 2023). Future studies may need to focus on evaluating how VR can contribute to sustained proficiency in high-stakes medical scenarios over time.
The findings from this study highlight the potential of virtual reality (VR) training as an effective tool in emergency medical education, particularly for enhancing the management of multi-casualty traffic accidents. The VR group not only demonstrated improved performance in triage accuracy and decision-making speed, but also reported greater confidence in applying these skills in real-world scenarios. These improvements may directly contribute to better patient outcomes by enabling faster and more accurate decisions in high-pressure environments, which are critical for minimizing mortality in trauma care (Jones et al., 2021). Additionally, VR’s capacity to simulate dynamic and unpredictable scenarios provides trainees with a safe platform for repeated practice, honing their skills without risking patient safety (McGowan et al., 2022).
From an educational standpoint, VR offers substantial advantages in learner engagement and skill retention, which are increasingly recognized in medical training (Krämer et al., 2022). It provides a cost-effective and scalable solution to traditional resource-heavy simulations, reducing logistical constraints while maintaining a high-fidelity learning environment (Moreira et al., 2021). Given its ability to integrate immersive, hands-on experiences with immediate feedback, VR-based training could play a crucial role in preparing a highly qualified and agile emergency workforce capable of responding to crises efficiently (Silva et al., 2021). This positions VR as a powerful tool to supplement conventional training, offering new pathways for improving emergency medical education in both clinical efficacy and scalability.
Although this study provides valuable insights into the potential of virtual reality (VR)-based training in emergency medical education, several limitations must be acknowledged. Firstly, as the study was limited to a single hospital, its findings may not be easily generalized to other regions or institutions with diverse healthcare systems and technological resources. Furthermore, the relatively short duration of follow-up does not allow for the assessment of long-term skill retention, which is crucial for determining whether the benefits observed in VR training are sustained over time (Silva et al., 2021). Another limitation pertains to the physical discomfort reported by some participants, such as wearing the VR headset for extended periods, which could affect the overall engagement and effectiveness of the training (Tang and Chen, 2021). Lastly, the sample size, while adequate for detecting differences in performance outcomes, was modest for drawing broader conclusions about VR’s impact across different experience levels in emergency medicine.
Despite these limitations, the results offer a strong foundation for expanding research in this area. Future investigations should include multicenter trials to validate the findings across diverse healthcare environments using larger and more heterogeneous participant pools (Gerardi and Chung, 2020). Additional studies should also focus on optimizing the VR hardware to improve user comfort and reduce issues such as fatigue and motion sickness, which were noted in both our study and previous research (Zhang et al., 2022). Longitudinal assessments are needed to evaluate the long-term retention of skills learned through VR training, particularly in high-pressure scenarios specific to traffic accidents (Leung et al., 2023). Finally, further research should explore the integration of haptic feedback and advanced physiological simulations to enhance the realism of VR training and potentially extend its application to other areas of emergency care, such as mass casualty or disaster response (Alaraj et al., 2021).
5 Conclusion
In conclusion, this randomized controlled trial demonstrates that virtual reality (VR)-based emergency medical training offers significant advantages over traditional training methods in enhancing both the objective and subjective competencies of emergency physicians in managing complex multi-casualty traffic accidents. Participants trained using VR showed superior performance in triage accuracy, on-site assessment, and transportation decision-making, alongside higher levels of confidence and preparedness for real-world emergency scenarios. These findings support the broader adoption of VR as a valuable educational tool in emergency medicine, particularly in high-stakes environments where rapid decision-making is critical. Furthermore, the scalability and resource efficiency of VR suggest that it could become an integral part of routine emergency medical training, filling critical gaps in traditional methods without compromising patient safety.
Future studies should focus on assessing the long-term retention of skills acquired through VR, as well as exploring its potential for widespread use in other areas of trauma care and emergency medical education. By continuing to refine and integrate VR technology, we can significantly enhance the training and preparedness of healthcare providers, ultimately improving patient outcomes in emergency settings.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding authors.
Author contributions
ZL: Data curation, Formal Analysis, Methodology, Visualization, Writing–original draft, Writing–review and editing. WW: Formal Analysis, Funding acquisition, Supervision, Validation, Writing–original draft. Z-ZH: Investigation, Methodology, Writing–review and editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This research was supported by the Guangxi Medical and Health Appropriate Technology Development and Promotion Application Project (grant number: S2023013) and the Guangxi Natural Science Foundation (grant number: 2024GXNSFAA010071). The funding provided resources for experimental materials, data analysis software, and research assistant stipends.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that Generative AI was used in the creation of this manuscript. The use of Generative AI in this study is only for Language Refinement and Grammar Check.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Alaraj, A., Osman, K., and Toledo, M. (2021). Integration of haptic feedback in virtual reality surgical training: a closer approach to real-world settings. J. Surg. Simul. Train. 6 (3), 109–118.
Bensky, M., Carling, B., and Gray, W. (2021). Enhancing situational awareness in emergency response using immersive VR training. Prehosp Disaster Med. 36 (5), 563–571.
Bruno, R. R., Wolff, G., Wernly, B., Masyuk, M., Piayda, K., Leaver, S., et al. (2022). Virtual and augmented reality in critical care medicine: the patient's, clinician's, and researcher's perspective. Crit. Care 26 (1), 326. doi:10.1186/s13054-022-04202-x
Cerezo Espinosa, C., Segura Melgarejo, F., Melendreras Ruiz, R., García-Collado, Á. J., Nieto Caballero, S., Juguera Rodríguez, L., et al. (2019). Virtual reality in cardiopulmonary resuscitation training: a randomized trial. Emergencias 31 (1), 43–46.
Chao, R., Zhang, L., Chen, Y., and Wang, J. (2022). The impact of virtual reality on resuscitation training: a randomized controlled trial. Resuscitation 168, 166–172.
Chiang, D. H., Huang, C. C., Cheng, S. C., Cheng, J. C., Wu, C. H., Huang, S. S., et al. (2022). Immersive virtual reality (VR) training increases the self-efficacy of in-hospital healthcare providers and patient families regarding tracheostomy-related knowledge and care skills: a prospective pre-post study. Med. Baltim. 101 (2), e28570. doi:10.1097/md.0000000000028570
Fahl, J. T., Duvivier, R., Reinke, L., Pierie, J. E. N., and Schönrock-Adema, J. (2023). Towards best practice in developing motor skills: a systematic review on spacing in VR simulator-based psychomotor training for surgical novices. BMC Med. Educ. 23 (1), 154. doi:10.1186/s12909-023-04046-1
Gerardi, S., and Chung, R. (2020). Wearability challenges of virtual reality systems in healthcare training: user discomfort and its implications. J. Healthc. Eng. 2020, 9875123.
Goel, T., Sharma, N., Gehlot, A., and Srivastav, A. K. (2023). Effectiveness of immersive virtual reality training to improve sitting balance control among individuals with acute and sub-acute paraplegia: a randomized clinical trial. J. Spinal Cord. Med. 46 (6), 964–974. doi:10.1080/10790268.2021.2012053
Guo, Z., Li, S., and Liang, Y. (2021). Virtual reality training in surgical skills: a randomized controlled trial. J. Surg. Educ. 78 (4), e22–e28.
Hollis, N., Richard, P., and Turner, K. (2020). Reducing anxiety in medical trainees via immersive virtual reality environments. Med. Educ. 54 (9), 876–885.
Jones, M., Smith, R., and Cooper, M. (2021). Virtual reality for trauma management: enhancing real-world decision-making in multi-casualty incidents. J. Trauma Acute Care Surg. 91 (4), 690–696.
Just, S. A., Lütt, A., Siegle, P., and Döring-Brandl, E. J. (2024). Feasibility of using virtual reality in geriatric psychiatry. Int. J. Geriatr. Psychiatry 39 (1), e6060. doi:10.1002/gps.6060
Kaim, A., Milman, E., Zehavi, E., Harel, A., Mazor, I., Jaffe, E., et al. (2024). Augmented reality-virtual reality wartime training of reserve prehospital teams: a pilot study. Isr. J. Health Policy Res. 13 (1), 46. doi:10.1186/s13584-024-00634-8
Kanschik, D., Bruno, R. R., Wolff, G., Kelm, M., and Jung, C. (2023). Virtual and augmented reality in intensive care medicine: a systematic review. Ann. Intensive Care 13 (1), 81. doi:10.1186/s13613-023-01176-z
Kman, N. E., Price, A., Berezina-Blackburn, V., Patterson, J., Maicher, K., Way, D. P., et al. (2023). First Responder Virtual Reality Simulator to train and assess emergency personnel for mass casualty response. J. Am. Coll. Emerg. Physicians Open 4 (1), e12903. doi:10.1002/emp2.12903
Krämer, E., Artz, G., and Bühler, Y. (2022). Immersive learning in medical education: how virtual reality simulations elevate emergency response training. Med. Teach. 44 (5), 565–573.
Laing, S., Grewal, G., and O'Brien, C. (2023). Virtual reality learning for long-term skill retention in emergency scenarios: a systematic review. Simul. Healthc. 18 (2), 98–105.
Leung, W., MacFarlane, C., and Xenophon, J. (2023). Long-term impact of virtual reality-based emergency training: a longitudinal study. Simul. Healthc. 18 (1), 75–82.
McGowan, C., Kilgore, A., and Arnold, A. (2022). The role of virtual reality in reducing in-hospital adverse events through simulation-based training. Simul. Healthc. 17 (2), 150–158.
Mohanty, C. R., Radhakrishnan, R. V., Stephen, S., Jain, M., Shetty, A. P., Issac, A., et al. (2022). Epidemiology of mass casualty incidents in a tertiary care trauma center in eastern India: a retrospective observational study. Turk J. Emerg. Med. 22 (2), 96–103. doi:10.4103/2452-2473.342806
Moreira, T., Santos, P., and Almeida, F. (2021). Engaging medical students with virtual reality: impacts on psychological and procedural readiness for emergency scenarios. Adv. Med. Educ. Pract. 12, 567–575.
Nelson, J. G., Hevesi, S., Welborn, R., Carlson, K. R., Eide, B., Winkler, M., et al. (2020). Periodic refresher emails for emergency department mass casualty incident plans. J. Educ. Teach. Emerg. Med. 5 (3), C1–C81. doi:10.21980/J8C05W
Ramalho, A., Duarte-Mendes, P., Paulo, R., Serrano, J., and Petrica, J. (2024). Crossing the digital frontier: are older adults ready for virtual reality workouts? Front. Public Health 12, 1324004. doi:10.3389/fpubh.2024.1324004
Razzaghi, A., Soori, H., Abadi, A., and Khosravi, A. (2020). World Health Organization's estimates of death related to road traffic crashes and their discrepancy with other countries' national report. J. Inj. Violence Res. 12 (3), 39–44. doi:10.5249/jivr.v12i3.1425
Silva, D., Fonseca, L., and Marques, F. (2021). Cost-efficiency and scalability of virtual reality-based training: a review for wider adoption in medical education. J. Med. Internet Res. 23 (6), e24149.
Tang, X., and Chen, L. (2021). Long-term retention of skills post-virtual reality training: a systematic review. J. Med. Educ. Curric. Dev. 8, 238–245.
Tune, SNBK, Mehmood, A., Naher, N., Islam, B. Z., and Ahmed, S. M. (2023). A qualitative exploration of the facility-based trauma care for road traffic crash patients in Bangladesh: when only numbers do not tell the whole story. BMJ Open 13 (11), e072850. doi:10.1136/bmjopen-2023-072850
Wang, Y., Zhu, M., Chen, X., Liu, R., Ge, J., Song, Y., et al. (2024). The application of metaverse in healthcare. Front. Public Health 12, 1420367. doi:10.3389/fpubh.2024.1420367
Yeung, A. W. K., Tosevska, A., Klager, E., Eibensteiner, F., Laxar, D., Stoyanov, J., et al. (2021). Virtual and augmented reality applications in medicine: analysis of the scientific literature. J. Med. Internet Res. 23 (2), e25499. doi:10.2196/25499
Keywords: virtual reality, emergency medical training, traffic accidents, medical education, randomized controlled trial
Citation: Li Z, Wang W and Huang Z-Z (2025) Virtual reality for emergency medicine training on traffic accident injury treatment: a randomized controlled trial. Front. Virtual Real. 6:1518016. doi: 10.3389/frvir.2025.1518016
Received: 27 October 2024; Accepted: 05 February 2025;
Published: 26 February 2025.
Edited by:
Clint Bowers, University of Central Florida, United StatesReviewed by:
Giuseppe Caggianese, National Research Council (CNR), ItalyChristine Seaver, University of Central Florida, United States
Copyright © 2025 Li, Wang and Huang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zhe Li, bHpsemx6MTBAMTYzLmNvbQ==; Wei Wang, d2FuZ3dlaUBzdHUuZ3htdS5lZHUuY24=
 Zhe Li
Zhe Li Wei Wang*
Wei Wang*