- 1Department of Neurology, Neuroscape, University of California San Francisco, San Francisco, CA, United States
- 2Centre for Psychedelic Research, Department of Brain Sciences, Faculty of Medicine, Imperial College London, London, United Kingdom
- 3aNUma, Inc., San Rafael, CA, United States
- 4Intangible Realities Laboratory, Centro Singular de Investigación en Tecnoloxías Intelixentes da USC, Universidade de Santiago de Compostela, Santiago de Compostela, Spain
- 5Numadelic Labs, El Cerrito, CA, United States
- 6Departments of Physiology and Psychiatry, University of California San Francisco, San Francisco, CA, United States
- 7Department of Psychology, University of Exeter, Exeter, United Kingdom
Introduction: Being diagnosed with a life-threatening illness (LTI) is often accompanied by feelings of fear, uncertainty, and loneliness that can severely impact mental health. Relatively few interventions are available to address the existential concerns of individuals facing LTI, while treatment of the underlying physical ailment typically remains the priority of the healthcare system. Research has shown that psychedelic-assisted psychotherapy (PAT) holds promise for supporting mental health in people with LTIs. However, PAT’s potential in this population remains curtailed by several limitations, including regulatory and accessibility issues. Novel approaches that could provide some of the benefits of psychedelic experiences, while avoiding associated challenges, would therefore be highly desirable for supporting the mental wellbeing of people with LTIs. Among such interventions, virtual reality (VR)-based experiences have been suggested as a promising candidate. We here evaluate a program that includes weakly representational, multi-user VR experiences based on a design aesthetic previously described as “numadelic,” which has been demonstrated to elicit self-transcendent experiences comparable to psychedelics.
Methods: A prospective cohort study design was used to assess the effects of “Clear Light” (CL), a group-based, 6-session multimedia program that included VR experiences, video calls, and text chats spanning 3 weeks. Participants were individuals suffering from LTIs that self-selected to participate in the CL program. A total of N = 15 participants were evaluated based on assessments 1 week before and after the program, using self-report measures of anxiety, depression, wellbeing, and secondary psychological outcomes.
Results: The intervention was well-tolerated among participants. Significant improvements with moderate effect sizes were observed on self-reported measures of anxiety, depression, and wellbeing. Secondary measures assessing demoralization, connectedness, and spiritual wellbeing also showed significant improvements.
Discussion: This observational study demonstrated the feasibility and potential benefits of a group-based VR program that can be delivered at-home to people suffering from LTIs. While conclusions are presently limited by the lack of randomization or a comparison group, our findings strongly suggest further research is warranted, including randomized controlled trials.
Introduction
Modern medicine has produced a wide range of approaches to treating the physical body of patients with life-threatening illnesses (LTIs), up to the moment of death. However, fewer resources are available to support patients in managing the fear, uncertainty, and loneliness that often accompany LTI diagnoses (Pitman et al., 2018; Ho et al., 2023). LTIs can exact a substantial psychosocial burden due to fear of death, reduced physical mobility and fatigue induced by illness or medications, increased time spent on procuring medical services, and associated social isolation (Rokach, 2003). Although up to 40% of cancer patients meet the criteria for mood disorders (Mitchell et al., 2011), evidence-based treatments for supporting mental health and wellbeing in patients with LTIs are limited and often difficult to access. Current treatments primarily include talk therapy and medications such as serotonin-selective reuptake inhibitors (SSRIs) or benzodiazepines (Grassi and Riba, 2014), which are however limited in their effectiveness for people with LTIs. For example, pharmacological depression treatments have been found to be less effective in the LTI population compared to adults suffering from non-LTI related depression (Ostuzzi et al., 2018). The development of novel and innovative treatment modalities to support mental health of people with LTIs is thus highly desirable, and there has been recent increased interest in developing new technologies, including VR experiences, to support this population (Carmont and McIlfatrick, 2022; Martin et al., 2022; Mo et al., 2022; Woo et al., 2024).
In recent years, there has been renewed interest in the use of psychedelic drugs, such as psilocybin, for people facing LTI (Grob et al., 2011; Griffiths et al., 2016; Ross et al., 2016; Anderson et al., 2020; Yu et al., 2021). Results indicate that these individuals can experience rapid and sustained reduction in symptoms of anxiety and depression following psychedelic-assisted psychotherapy (PAT) (Ross et al., 2016). While the mechanisms of action driving the benefits of PAT are a matter of continued research, there appears to be a strong relationship between the occurrence of psychedelic-induced self-transcendent experiences (STEs) and the mental health benefits reported by people with LTIs (Griffiths et al., 2016). This is consistent with research suggesting that the efficacy of psychedelics in therapeutic settings depends on the acute subjective experience during the session (Roseman et al., 2018; Roseman et al., 2019). One study has found similarities between the experience elicited by the psychedelic N,N-Dimethyltryptamine (DMT) and near-death experience (NDE) reports (Timmermann et al., 2018), which could be another explanation for the efficacy of psychedelics in LTI populations, considering that NDEs can lead to drastic reductions in fear of death (Pehlivanova et al., 2023). Unfortunately, PAT is challenging to implement on a broad scale in the LTI population, owing to legal restrictions, high cost of delivery, and side effects (Muttoni et al., 2019). Even as psychedelics become more widely available and socially acceptable, limitations to access will remain for many people with LTIs, including frailty or use of medications that render psychedelics contraindicated. Finally, many individuals may not feel comfortable taking psychedelics, considering their intense subjective effects and stigma surrounding their use. Thus, solutions that deliver some of the benefits of PAT in people with LTIs, without its limitations, would be highly desirable.
Recently, Glowacki and colleagues (2020, 2022) described the design of multi-user VR experiences using a so-called “numadelic aesthetic,” (from Greek pneuma: “breath,” “spirit,” or “soul,” and delein: “to reveal” or “to manifest”), a weakly representational visual approach inspired by near-death phenomenology (Glowacki, 2024). Whereas most VR applications aim for photorealistic fidelity, numadelic representations are intentionally abstract, dissolving conventional spatiotemporal distinctions between self and other to achieve a sense of connectedness and unity. Compared to typical metaverse avatars, which represent bodies as highly detailed, the numadelic aesthetic represents participants as luminous energetic essences with diffuse boundaries, as illustrated in Figures 2, 3 below. “Isness,” a guided multi-person VR experience designed within this numadelic aesthetic, was found to elicit self-transcendent experiences (STEs) comparable to those following a moderate dose of psilocybin (Glowacki et al., 2022), using a range of psychometric measures, including the Mystical Experiences Questionnaire (MEQ-30) (Griffiths et al., 2006; MacLean et al., 2012), Inclusion of Other in Self (IOS) Scale, Ego Dissolution Inventory (EDI) (Nour et al., 2016), and Communitas scale (Kettner et al., 2021).
Building on this work, we here test the feasibility and potential benefits of a multi-session, multimedia, group-based intervention of numadelic VR experiences, video calls, and group text chats, called “Clear Light” (CL), for reducing the psychosocial symptom burden in people with LTIs. Given the connection between the numadelic aesthetic and NDEs and STEs, we hypothesized that facilitated, group experiences designed to address existential concerns related to mortality presented in such an environment would be particularly well suited for individuals facing LTIs.
Group-based VR interventions have been shown to offer unique potential in addressing issues of loneliness and isolation in patient populations with limited mobility or ability to participate in social life, including individuals in residential care (Gaspar et al., 2018; Brimelow et al., 2022), aphasic stroke patients (Marshall et al., 2020), and those suffering from social anxiety (Anderson et al., 2013; Ngai et al., 2015; Anderson et al., 2017) or social phobia (Salehi et al., 2020). The need for novel interventions that include social support for people facing LTIs is further exacerbated by the fact that loneliness and social isolation do not only increase symptom burden (Abedini et al., 2020) and reduce quality of life (Hyland et al., 2019; Dahill et al., 2020), but are also associated with increased mortality following a diagnosis (Drageset et al., 2013). Although extended, interactive, group-based VR interventions therefore hold a unique potential for patients with restricted mobility, studies on the use of VR for the LTI population have thus far mostly employed solo experiences involving photorealistic or 3D content viewed in a single session (Carmont and McIlfatrick, 2022; Martin et al., 2022). The CL program presented here aims to overcome several of these limitations, as will be shown below.
Using an open-label, observational cohort design, the present study prospectively assessed the effects of the CL program on a range of clinically relevant self-report measures, including depression, anxiety, and psychological wellbeing in LTI patients. It was hypothesized that participation in the CL program would lead to statistically significant reductions in symptoms of anxiety and depression, while improving mental wellbeing. Additionally, measures of demoralization, connectedness, spiritual wellbeing, and death acceptance were included as exploratory secondary outcomes.
Methods
Participants
Ethical approval for this study was granted by the Imperial College Joint Research Compliance Office (JRCO) and the Imperial College Research Ethics Committee. CL program organizers sent out a link to the study website to program participants. CL itself was advertised by word of mouth and via a website (https://anuma.com/clearlight). Additionally, several participants heard about CL from a podcast (Wyatt, 2023). Criteria for participating in the CL program included 1) self-reporting a LTI diagnosis; 2) speaking fluent English; 3) residing in the US, Canada, or UK; 4) being physically able to engage with the VR activities (e.g., being able to sit upright for approximately 1 hour and tolerating VR sufficiently well with no significant VR sickness); and, 5) being cognitively able to engage with the program activities (e.g., not suffering dementia).
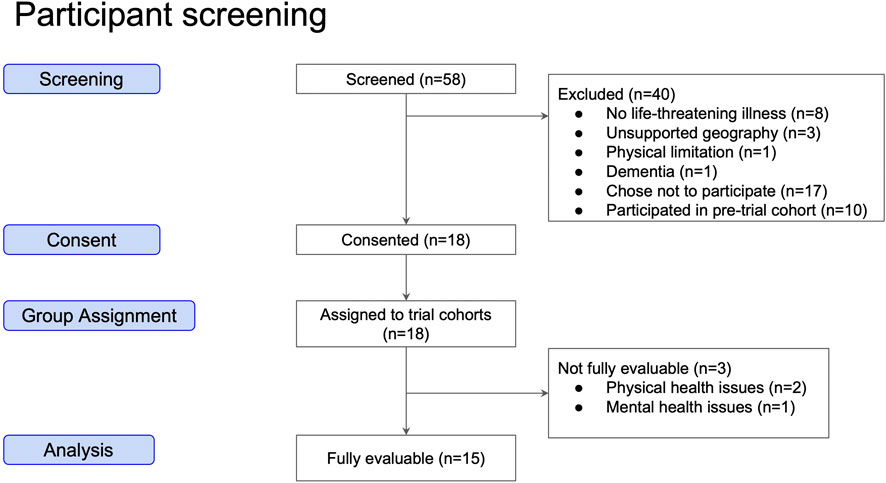
A total of 58 individuals filled out a web form indicating interest in participating in CL (Figure 1). Of those individuals, 13 were excluded due to not fulfilling one of the above criteria, 17 chose not to participate and 10 participated in pre-trial cohorts whose feedback was used to improve the CL experience. Of the 17 participants who were categorized as “Chose not to participate,” 6 indicated that none of the available times offered for sessions would work within their schedules. Seven participants stopped responding to communications (i.e., lost contact) prior to the consenting process. Four participants indicated they did not wish to participate for other personal reasons.
A total of 18 participants screened into the CL program gave consent to participate in the present observational study. Two participants were excluded from the analysis because they had dropped out prior to completing the program following hospitalization due to their illnesses. A third participant was excluded from the analysis because they reported a mental health emergency related to a psychedelic experience unrelated to the CL program or the present study, resulting in a total of 15 fully evaluable participants. Participants were divided into 3 cohorts of 6 participants, run sequentially between July and October 2023. There were 6, 5, and 4 fully evaluable participants in the first, second, and third cohorts, respectively.
The Clear Light experience
All cohorts were facilitated by the same facilitators, one male and one female. The CL program was composed of four distributed VR sessions, bookended by two video conference calls (Zoom Video Communications, Inc.) with asynchronous, encrypted group text chats (WhatsApp, Meta Platforms, Inc.) interspersed throughout. The CL environment was developed using the aNUmaXR experience creation platform (aNUma, Inc.) and delivered on Meta Quest 2 VR devices (Meta Platforms, Inc.). Primary funding for this study was provided by aNUma, the for-profit, public benefit corporation that provides CL (See Discussion and Conflict of Interest statement).
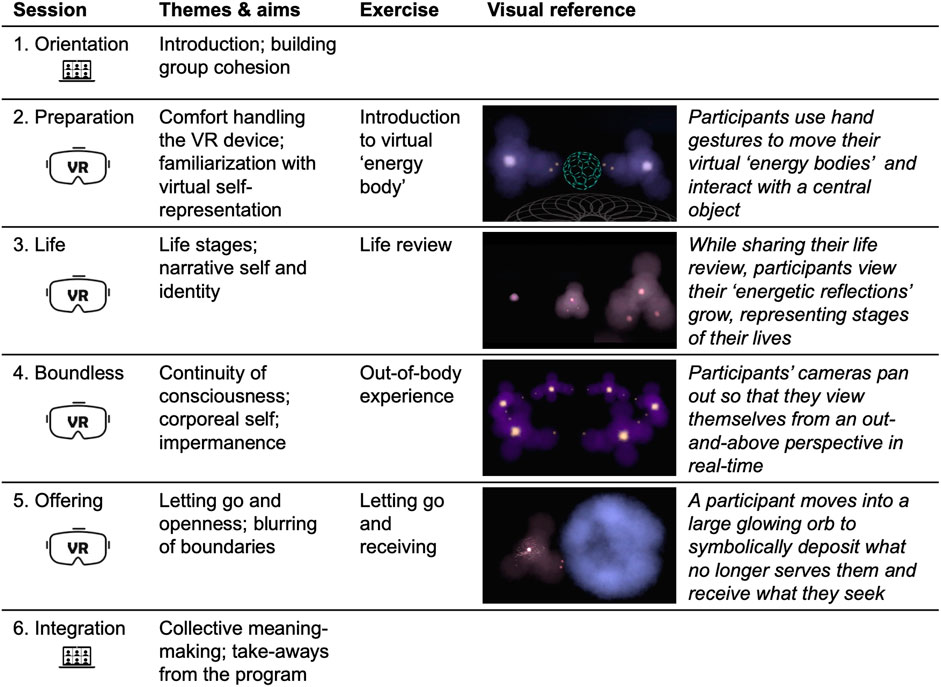
The content of each of the six sessions is presented below and in Figure 2.
1. Orientation (video conference, ∼90 min). The first session allowed participants to get to know each other and to meet the facilitators. Participants shared information about themselves, including how they were relating to their LTI, as well as their attitudes towards mortality. The facilitators explained the logistics and purpose of the program, and participants had an opportunity to ask any questions they had at that time.
2. Preparation (VR, 20–40 min). This session was a one-on-one session between each participant and a facilitator or other study staff in which participants were introduced to the VR hardware, including connecting the VR Head Mounted Display to WiFi, setting up a VR boundary, and starting the VR app (aNUmaXR). Once the participant launched the aNUmaXR app, they were met in the virtual environment by the facilitator or study staff. Participants then completed a short experience that included a guided meditation technique later used in the group sessions.
3. Life (VR, ∼60 min). The focus of the first group VR session was the life review, an evidence-based practice described first by Butler (1963), augmented by a VR visualization. Visualizations included a sequence in which the participants observed an abstracted version of themselves (“energetic reflection”) grow through life stages from infancy into adulthood, supported by an audio narrative.
4. Boundless (VR, ∼60 min). The fourth session was centered on an out-of-body experience in which participants’ points of view were moved from first person to a third person perspective, meaning they could observe themselves and their movements in real-time from further back and above. This was accompanied by a narrative that explored the relationship between consciousness and the corporeal body. Participants were told they would go on a short journey where they would extend their field of awareness beyond the boundary of their bodies. As their perspective shifted out of their avatars, they were asked how it feels to observe their body from afar and to imagine their conscious awareness merging into a broader field of awareness.
5. Offering (VR, ∼60 min). In the final group VR session, participants went through a series of sharing rounds that was more extended than in previous sessions. First, each participant described something that they would like to let go of and simultaneously “deposited” energy from their body into a central element. Later, each participant reentered the central element and “received” energy back into their avatar while sharing something that they felt they needed more of in their lives at that moment.
6. Integration (video conference, ∼90 min). The final session was a facilitated group conversation where participants could reflect on the experiences that they had together throughout the program. It was also an opportunity to discuss how to take what was learned and gained through the program into everyday life going forward.
In each VR session, participants appeared as diffuse and dynamic clouds of color (see Figures 2, 3), intending to substitute the physicality of embodiment with the impression of the body as energy. Participants’ hands were similarly figured as concentrated energetic luminosity, and simple environmental objects populated the space at various times. Each VR session included a curated soundtrack of ambient recorded music that was intended to match with the ongoing visual experience.
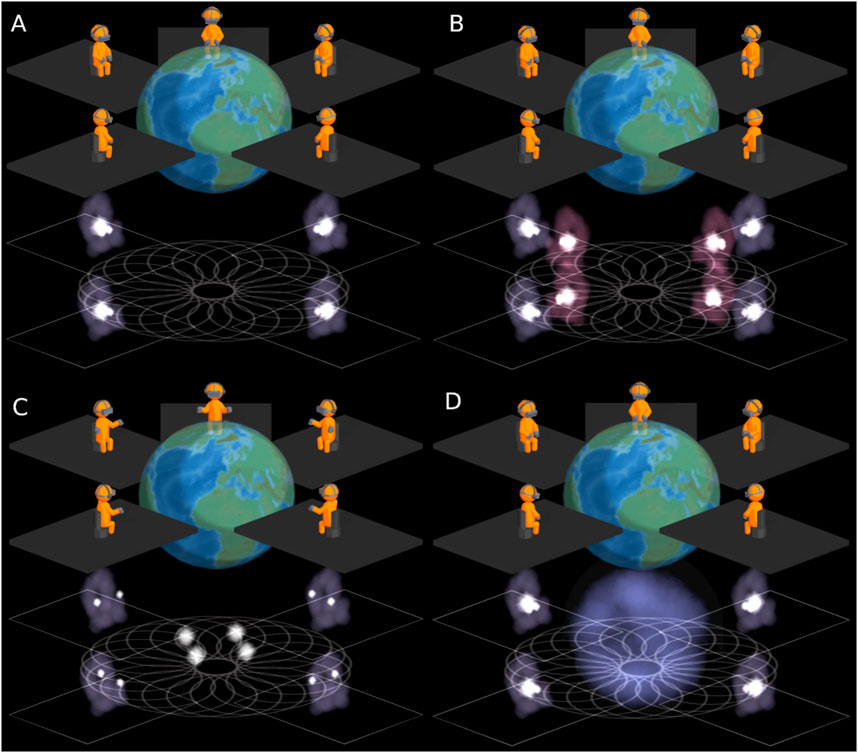
Figure 3. Schematic representation of the group “numadelic” VR setup. The top section of each panel represents individuals in physical space, seated with VR headsets and holding controllers. The lower section shows participants’ energy body avatars as purple clouds in the virtual environment. The large white light in the center of each avatar is located at and represents the avatar’s heart, while the two smaller lights follow the participant’s hand movements. Panel (A) represents the general setup, in this case showing four participants and one facilitator, with their hands in resting position. Panel (B) shows a schematic from Session #3 “Life” in which participants interact with their “energetic reflections” represented as maroon energy bodies. Panel (C) represents an exercise from Session #4 “Boundless” in which participants can share their heart lights into the center of the circle by spreading their arms. Panel (D) illustrates an exercise from Session #5 “Offering,” during which participants enter one-by-one into a large blue light sphere in the center of the circle in two distinct rounds. In the first round, they discuss something they would like to let go of and simultaneously “leave behind” the light energy from their body. Later, each participant reenters the light and “receives” energy back into their avatar while sharing something they feel they need more of in their lives now.
Each session also included guided meditations by facilitators and elements of embodiment practice. Most sessions included rounds of sharing in which participants respond to prompts (e.g., “What does ‘letting go’ mean to you?;” “How would you describe your process of releasing attachments or surrendering control?”). During sharing rounds, participants discussed how they were feeling regarding their LTI and were encouraged to engage in active listening with one another.
In addition to video calls and VR sessions, participants were able to communicate with other members of the cohort and facilitators asynchronously via WhatsApp. Facilitators provided prompts to generate contemplation and discussion within the group, which were designed to prepare participants for the upcoming sessions. For example, prior to the “Boundless” session, participants were prompted with the questions: “What negative thought, pattern, habit or tendency are you ready to release?” and “What qualities do you want to invite and cultivate more of?” These questions related to the activities of letting go and receiving that take place during that session. In response to these prompts, participants responded with answers about aspects of their mental life that they wanted to release, such as “guilt” or “shame” and aspects that they wanted to cultivate such as “love” or “forgiveness.” These asynchronous communications often built on themselves as participants reacted to what others in the group were saying.
Outcome measures
Participants were assessed within 1 week prior to the start of the program and again 1 week after it ended, a total of 5 weeks apart. Participants completed surveys on their personal computers or smartphones through a secure, encrypted interface (Alchemer, LLC).
The following primary outcomes were included:
• Hospital Anxiety and Depression Scale (HADS), assessing symptoms of anxiety and depression (Snaith, 2003). There are 7 questions each related to anxiety and depression. The minimum possible score is 0 (least anxious or depressed) and the maximum possible score is 21 (most anxious or depressed) for each subscale. Improvements correspond to lower scores.
• Short Warwick-Edinburgh Mental Well-Being Scale (sWEMWBS), a 7-item measure of psychological wellbeing (Shah et al., 2018). The minimum score is 7 (lowest mental wellbeing) and maximum score is 35 (highest mental wellbeing). Improvements correspond to higher scores.
Several measures were included as exploratory secondary outcomes:
• Demoralization Scale (DS-II) assessing hopelessness, helplessness and their impact on an individual’s overall wellbeing in the context of a serious illness (Kissane et al., 2004). Due to an oversight setting up the survey, 1 of the 16 items on the scale was never presented to participants. The minimum score is 0 (least demoralized) and the maximum score is 30 (most demoralized). Improvements correspond to lower scores.
• Watts Connectedness Scale (WCS). This scale was developed in the context of psychedelic research and measures an individual’s sense of connectedness to self, others, and the world (Watts et al., 2022). The minimum score is 0 (least connected) and the maximum score is 100 (most connected). Improvements correspond to higher scores.
• Functional Assessment of Chronic Illness Therapy - Spiritual Well-Being (FACIT-SP), assessing spiritual wellbeing in the context of chronic illness (Peterman et al., 2002). Due to a technical issue with the survey tool, only the first 10 items (of 12 total) were reliably delivered to participants. The sum of those 10 items were analyzed. The total scores range from a minimum of 0 (lowest spiritual wellbeing) to a maximum of 40 (highest spiritual wellbeing). Improvements correspond to higher scores.
• Death Attitude Profile-Revised (DAP-R), of which the Fear of Death and Death Avoidance subscales were used (Wong et al., 1994). The minimum score is 12 (least negative attitude), and the maximum is 84 (most negative attitude). Improvements correspond to lower scores.
As part of the post-program survey, participants were asked to rate on a scale of 0–10 whether they would recommend the experience to other individuals facing a LTI, referred to as Net Promoter Score (NPS) (Reichheld, 2003). Scores on the NPS range from −100 (all detractors) to +100 (all promoters). This measure served as an indicator of the acceptability of the program.
Statistical analysis
We performed a Repeated Measures Multivariate Analysis of Variance (RM MANOVA) to test pre- to post-intervention changes across the 7 dependent variables. Multivariate significance is reported via the Wald-type statistic (WTS) (Randall et al., 1997) and modified ANOVA test statistic (MATS) (Friedrich and Pauly, 2018) which is robust against deviations from symmetry and heteroscedasticity. Levene’s test statistic was calculated for each outcome measure. To then examine univariate changes at the level of individual outcome measures, we ran two-tailed within-subjects t-tests as follow-up. For each outcome variable, Hedges g effect size was calculated and interpreted along the empirical guideline for social psychology of 0.15, 0.40 and 0.70 for small, medium, and large effects respectively (Lovakov and Agadullina, 2021). While uncorrected p-values are reported for follow-up tests, we report when secondary outcome measures would not survive Bonferroni correction.
Results
The mean age of the 15 fully evaluable participants was 66.7 (± 8.8 s.d.). All indicated their ethnicity as “White.” Thirteen participants were female and two were male. Thirteen of the participants were from the US, 1 was from the UK, and 1 was from Canada. Participants self-reported their diagnoses. All 15 participants indicated they had life-threatening illnesses. Diagnoses included advanced cases of cancer (n = 12), heart disease (n = 2), and lung disease (n = 1).
Levene’s test showed no deviations from homoscedasticity in any of the 7 analyzed outcome measures. RM MANOVA revealed significant multivariate differences between pre- and post-intervention scores (F (1, 28) = 13.16, p < 0 .001, WTS = 30.5, MATS = 13.2).
Follow-up t-tests showed that all three primary outcome measures were significantly improved at the post-intervention time point (Figure 4, Table 1). At baseline, considerable levels of anxiety and depression symptoms were reported by 60% (9/15) and 20% (3/15) of participants, respectively, based on the HADS (cutoff score >7, see Table 1). The mean pre-program HADS-A score was 8.73 (±0.97) and the post-program mean was 7.13 (±1.05), which was significantly lower (t (14) = 2.4, p = 0.030) with a moderate effect size (g = 0.40). The pre-program mean depression score (HADS-D) was 5.33 (±0.64), which fell to 3.80 (±0.58) post-program. This difference was significant (t (14) = 2.8, p = 0.015) at a medium-large effect size (g = 0.63). Wellbeing (sWEMWBS) scores increased from 24.33 (±0.91) to 26.53 (±0.99) post-program, which was also significant at a moderate effect size (t (14) = −3.8, p = 0.002, g = 0.58).
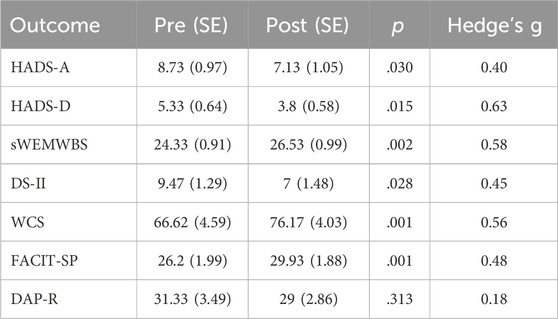
Table 1. Results from the prospective outcome measures. Mean scores (N = 15) measured 1 week before (Pre) and after (Post) participation in the Clear Light VR program are shown including standard error (SE). DAP-R: Death Attitude Profile-Revised; DS-II: Demoralization Scale II; FACIT-SP: Functional Assessment of Chronic Illness Therapy–Spiritual Well-Being; HADS-A/-D: Hospital Anxiety and Depression Scale, Anxiety and Depression Subscales; sWEMWBS: Short Warwick-Edinburgh Mental Well-Being Scale; WCS: Watts Connectedness Scale.
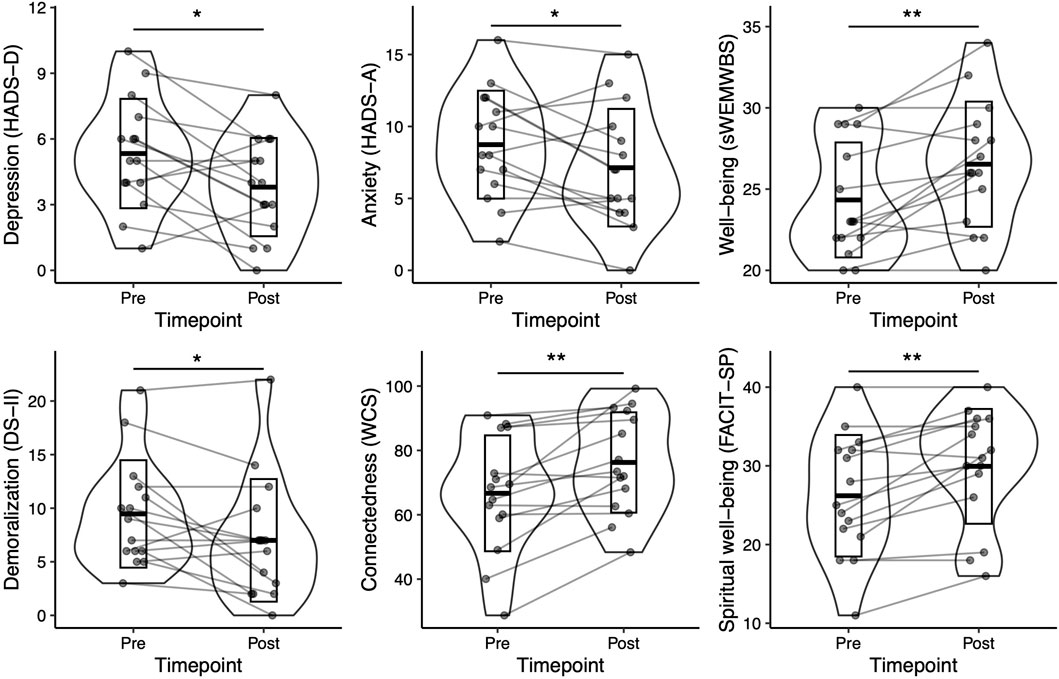
Figure 4. Statistically significant changes in primary and secondary outcomes. Mean scores measured 1 week before (Pre) and after (Post) participation in the Clear Light VR program are shown including standard deviation (SD) and individual participant data (N = 15). Significance indicated based on pairwise t-tests: *p <0 .05, **p <0 .01.
Among the secondary outcomes, significant improvements were detected among all measures except for death attitudes (DAP-R, t (14) = −1, p = 0.31). The greatest improvements were observed for connectedness (WCS), which significantly increased from 66.62 (±4.59) to 76.17 (±4.03) post-program (t (14) = −4.1, p = 0.001, g = 0.56). Demoralization (DS-II) was found to be reduced from 9.47 (±1.29) to 7.00 (±1.48), (t (14) = 2.5, p = 0.028, g = 0.45), although this effect would not have been significant at 7-fold Bonferroni-correction. Spiritual wellbeing (FACIT-SP) was increased from 26.20 (±1.99) to 29.93 (±1.88, t (14) = −4.0, p = 0.001, g = 0.48).
The mean score on the Net Promoter question was 8.93 (±0.27) out of a possible 10. The Net Promoter Score (NPS) was 60 (Reichheld, 2003), with six participants indicating a score of 10, and the lowest score being 7.
Discussion
This observational cohort study followed individuals facing a LTI from before to after their participation in a group-based multimedia (VR, video and text chat) program. We demonstrated the feasibility and potential benefits of the program, showing significant improvements in psychological and spiritual wellbeing, connectedness, anxiety, depression, and demoralization. A primary concern of this article is the feasibility of the CL program. Feasibility in this context includes interest in the program (will participants wish to participate?), successful delivery of the remote, multimedia intervention, compliance with and tolerance of the experience, and acceptability of the intervention. We conclude that the intervention is feasible. Fifty-eight participants expressed interest. It was successfully delivered to 15 fully evaluable participants in 3 different countries, with each participant connecting to the VR and Zoom sessions from home with equipment that was shipped to them. Participants found the intervention tolerable (i.e., were able to complete the sessions without significant complaints about VR sickness), and participants indicated that it was acceptable in that they would recommend the program to others with a similar condition (average rating of 8.93 out of 10). The present findings thereby add to the limited body of literature demonstrating the feasibility and beneficial effects of VR interventions for wellbeing (McGhee et al., 2024) and other secondary symptoms (Ioannou et al., 2020) in palliative care patients, while to our knowledge representing the first ever use of a group-based VR experience in LTI patients.
Although there was significant variability across the assessed outcomes, the observed improvements were moderate for all significant measures, being highest for depression, wellbeing, and connectedness, followed by spiritual wellbeing, demoralization and anxiety. With an average effect size of g = 0.52 for the statistically significant effects, the results were comparable to other psychosocial interventions for death anxiety (Menzies et al., 2018), following a similar pattern as found following psychotherapy in palliative care, insofar as depression and quality of life showed greater improvements than anxiety (Fulton et al., 2018). The magnitude of improvements was similar to those found for psilocybin treatment for end of life, although the three published clinical trials showed a great amount of variability in their effect sizes (Yu et al., 2021). Notably, significant effects could be detected in the present sample despite baseline depression and anxiety scores being on average within or close to the healthy normal (<8) range. Further research should thus examine the effects of the here-studied intervention in a selectively recruited sample consisting of more severely depressed or anxious patients.
While the present study was not aiming to explore the mechanisms underlying the intervention presented here, we hypothesize that a combination of intra- and inter-personal processes generated the observed mental health improvements. The numadelic representational aesthetic was designed to model aspects of self-transcendent and near-death experiences (STEs and NDEs, respectively), including an out-of-body sequence modelled on that described by Glowacki (Glowacki, 2024), and a sequence where each participant merged with a luminosity substantially larger than themselves. NDEs are sometimes able to dramatically diminish anxiety associated with death (Tassell-Matamua and Lindsay, 2016; Bianco et al., 2019), with the extent of death anxiety reduction seemingly correlated with NDE intensity (Greyson, 2015). Prior studies have shown that VR can effectively be used to generate NDE-like states (Barberia et al., 2018) and out of body experiences (Martial et al., 2023) which were able to attenuate fear of death in healthy participants (Bourdin et al., 2017). The CL program assessed in this study augmented similar STE and NDE-evoking elements with narrative support techniques shown to be effective in supporting the mental health and wellbeing of patients with LTIs (Rosenfeld et al., 2018).
This study did not find statistically significant improvements on the DAP-R (Fear of Death and Death Avoidance subscales). It is not possible to draw strong conclusions about this null result from the small sample observed in this study, and future research is warranted to determine why the hypothesized improvement was not found. If the failure to find such an effect is due to random variability in the sample or relatively low sensitivity of the DAP-R, then a statistically significant improvement may be observed in a larger sample. It is also possible that participants did not experience reduced fear of death or improvement in their death attitude. Such a conclusion would raise the intriguing possibility that the benefits of the program are mediated through a different (possibly more general) psychological mechanism than changing attitude toward death. Future research that utilizes larger sample sizes and additional measures of death attitude could tease apart these possibilities.
The fact that the above-described experiences took place in a group, rather than alone, with ample opportunity to discuss and reflect in sharing rounds mediated by trained facilitators, was hoped to further establish psychosocial resources known to greatly impact the quality of life in people suffering from LTIs. Several meta-analyses have shown the positive mental health effects of peer support groups for people with LTIs (Meyer and Mark, 1999; Rehse and Pukrop, 2003), including online-based support groups (Rains and Young, 2009; Ihrig et al., 2020), although recent studies have shown that face-to-face peer support is perceived as more beneficial (Huber et al., 2018) and more desirable (Boyes et al., 2018) than seeking support online. A VR experience similar to that used in the present intervention has previously been shown to elicit experiences of togetherness and shared humanity among participants on par with real-life group sessions (Glowacki et al., 2022). We therefore hope that this and similar VR interventions have the potential to leverage some of the advantages of embodied peer contact while remaining accessible to subjects with limited mobility, who would not otherwise be able to easily partake in face-to-face peer support.
Previous approaches using VR to support people with LTI differ from the strategies used in the CL program described here in several ways. Major differences include: 1) Previous studies typically involve one VR session, whereas CL is comprised of a series of modules that take place over several weeks. 2) Where previous studies have relied on solo VR experiences (Mo et al., 2022), the group aspect of CL allows participants to support and share with one another. 3) Most previous approaches have implemented 360-video as a passive viewing experience. Participants in the CL program can interact within the virtual world through speech and movements, meant to create a sense of embodied agency. 4) Most VR approaches rely on near-photorealistic content (e.g., 3D images and videos of nature scenes Niki et al., 2019; Ferguson et al., 2020; Johnson et al., 2020) and photo-realistic avatars (Dang M. et al., 2021), which can create an “uncanny valley” effect (Seyama and Nagayama, 2007). CL’s numadelic aesthetic uses a weakly representational approach, in which avatars appear as energy bodies with soft boundaries in a visually sparse environment that does not appear like anything encountered in the ‘real world.’ As such, CL attempts to stimulate endogenous meaning-making, inviting participants to project their own meaning into the visual content, comparable to how meaning is projected onto a Rorschach plot. 5) Finally, most VR studies have focused on a single technique, such as relaxation (Baños et al., 2013; Woo et al., 2024) or life review (Dang P. et al., 2021), in contrast to the multimodal approach implemented within CL.
Limitations
The observational design employed in the current study imposes several inherent limitations, including the lack of randomization, a control condition, or the targeted recruitment of a more ethnically or gender diverse, or more clinically defined study sample. In particular, this study lacked gender (mostly female) or ethnic (entirely “White”) diversity. Self-selection bias might have led to the inclusion of participants that had a particularly high potential to benefit from this intervention. Future study designs should incorporate a thorough inventory of any medications or other substances that participants are currently taking or plan to take. For example, knowing the chemotherapy regimen of cancer patients would be helpful for covariate analyses. These studies should also assess and preemptively exclude individuals who intend to use mind-altering substances that might interfere with the program during the study period.
Additionally, the design does not allow us to draw strong conclusions about the mechanisms of action of the intervention. The extent to which the VR sessions, or interactions with facilitators, or other participants during group calls may have contributed to improved mental health outcomes remains unclear based on the present results. In future studies, the specific impact of the different stages of the CL protocol could be elucidated through the inclusion of additional intermittent assessments and/or measures assessing potentially mechanistic variables pertaining to VR and group therapeutic experiences. For example, prior studies investigating a single-session, group, numadelic VR experience have demonstrated subjectively reported effects of ego attenuation, connectedness, and mystical-type experiences akin to psychedelic drug effects (Glowacki et al., 2020; Glowacki et al., 2022). Analysis of follow-up assessments will be required to draw any conclusions about sustained responses beyond the here-reported endpoints at 1-week post-intervention.
Several of the authors of this manuscript (DRG, JW, JLH, RLC-H) were affiliated with the for-profit, public benefit corporation that provides CL, which is a potential source of bias (See Conflict of Interest statement). In order to limit the potential for bias, CL was assessed here through an observational study designed and conducted in collaboration with authors not affiliated with the company (HK, LR; see Author Contributions). However, unintentional bias could still show up in a variety of ways, for example, in study design, participant recruitment, and in the interaction with participants. Set and setting are important components of self-transcendent experiences (Gukasyan and Nayak, 2022; Carhart-Harris et al., 2018). Therefore, the attitude and intention of the study staff, who were employed or contracted by the company, could have played an important role in participants’ experience. Further research where this intervention is applied by staff without such financial interest is therefore warranted. It is important to note that the success of such a program may depend on the intention and effort of the facilitators and other staff to provide a good experience, so quality control will be an important component of any future research.
Conclusion
The existential and psychological implications of mortality are rarely discussed in secular modern societies (Hvidt and Assing Hvidt, 2019), although research indicates that structured engagement with one’s own mortality can improve quality of life and psychological wellbeing at the end of life (LeMay and Wilson, 2008). People with LTIs often encounter additional challenges when trying to access peer support, or any of the limited set of treatments available to support their mental health and wellbeing. We presented an observational cohort study of a novel group-based VR intervention, demonstrating its feasibility and potential benefits in improving symptoms of depression and anxiety in patients with a LTI diagnosis, while enhancing psychological and spiritual wellbeing and connectedness. These preliminary findings strongly warrant future independent, randomized, controlled studies, especially considering the scarcity of existing treatment options that can provide psychosocially supportive experiences to individuals who suffer from mobility-impairing serious illnesses.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by the Imperial College Research Ethics Committee, Imperial College London. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
HK: Data curation, Formal Analysis, Investigation, Methodology, Visualization, Writing–original draft, Writing–review and editing. DRG: Methodology, Resources, Software, Visualization, Writing–review and editing. JW: Investigation, Writing–review and editing. RLC-H: Conceptualization, Methodology, Supervision, Writing–review and editing. LR: Conceptualization, Methodology, Writing–review and editing. JLH: Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Project administration, Software, Writing–review and editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. Funding for the project was provided by aNUma, Inc. DRG recognizes support from Axencia Galega de Innovacion through the Oportunius Program, the Xunta de Galicia (Centro de investigación de Galicia accreditation 2019–2022, ED431G-2019/04), the European Union (European Regional Development Fund), and also the ArtSci International non-profit. JW was supported in part by funding from CiTIUS through the Xunta de Galicia (Centro de investigación de Galicia accreditation 2019–2022, ED431G-2019/04).
Acknowledgments
We would like to acknowledge the efforts of all the people who made this project possible. First, we would like to thank the participants who volunteered their time at this sensitive moment in their lives. We thank Anat Geiger, whose experience of numadelic VR and subsequent encouragement, in the days prior to her passing, helped motivate aspects of this work. We thank Summer Athena Fae for assisting in facilitating and supporting the cohorts. We would also like to thank Sergey Grishaev, Gregory Roufa, Rhos Roebuck Williams, Mike Chatziapostolou, Mark Wonnacott, Anne-Marie Keppel, Jamie Pike, and Tiu de Hann for developing and supporting the platform and program used in this study.
Conflict of interest
Author DRG is a co-founder of and shareholder in aNUma, Inc., the makers of the Clear Light program used in this study. Author JLH is a co-founder of and shareholder in aNUma, Inc. Author JW is a contractor for and a shareholder in aNUma, Inc. Author RLC-H is a shareholder in aNUma, Inc.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Abedini, N. C., Choi, H., Wei, M. Y., Langa, K. M., and Chopra, V. (2020). The relationship of loneliness to end-of-life experience in older Americans: a cohort study. J. Am. Geriatrics Soc. 68 (5), 1064–1071. doi:10.1111/jgs.16354
Anderson, B. T., Danforth, A., Daroff, P. R., Stauffer, C., Ekman, E., Agin-Liebes, G., et al. (2020). Psilocybin-assisted group therapy for demoralized older long-term AIDS survivor men: an open-label safety and feasibility pilot study. EClinicalMedicine 27, 100538. doi:10.1016/j.eclinm.2020.100538
Anderson, P. L., Edwards, S. M., and Goodnight, J. R. (2017). Virtual reality and exposure group therapy for social anxiety disorder: results from a 4–6 year follow-up. Cognitive Ther. Res. 41, 230–236. doi:10.1007/s10608-016-9820-y
Anderson, P. L., Price, M., Edwards, S. M., Obasaju, M. A., Schmertz, S. K., Zimand, E., et al. (2013). Virtual reality exposure therapy for social anxiety disorder: a randomized controlled trial. J. Consult. Clin. Psychol. 81 (5), 751–760. doi:10.1037/a0033559
Baños, R. M., Espinoza, M., García-Palacios, A., Cervera, J. M., Esquerdo, G., Barrajón, E., et al. (2013). A positive psychological intervention using virtual reality for patients with advanced cancer in a hospital setting: a pilot study to assess feasibility. Support. Care Cancer 21, 263–270. doi:10.1007/s00520-012-1520-x
Barberia, I., Oliva, R., Bourdin, P., and Slater, M. (2018). Virtual mortality and near-death experience after a prolonged exposure in a shared virtual reality may lead to positive life-attitude changes. PloS one 13 (11), e0203358. doi:10.1371/journal.pone.0203358
Bianco, S., Testoni, I., Palmieri, A., and Solomon, S. (2019). The psychological correlates of decreased death anxiety after a near-death experience: the role of self-esteem, mindfulness, and death representations. J. Humanist. Psychol., 0022167819892107. doi:10.1177/0022167819892107
Bourdin, P., Barberia, I., Oliva, R., and Slater, M. (2017). A virtual out-of-body experience reduces fear of death. PloS one 12 (1), e0169343. doi:10.1371/journal.pone.0169343
Boyes, A., Turon, H., Hall, A., Watson, R., Proietto, A., and Sanson-Fisher, R. (2018). Preferences for models of peer support in the digital era: a cross-sectional survey of people with cancer. Psycho-oncology 27 (9), 2148–2154. doi:10.1002/pon.4781
Brimelow, R. E., Thangavelu, K., Beattie, R., and Dissanayaka, N. N. (2022). Feasibility of group-based multiple virtual reality sessions to reduce behavioral and psychological symptoms in persons living in residential aged care. J. Am. Med. Dir. Assoc. 23 (5), 831–837.e2. doi:10.1016/j.jamda.2021.07.026
Butler, R. N. (1963). The life review: an interpretation of reminiscence in the aged. Psychiatry 26 (1), 65–76. doi:10.1080/00332747.1963.11023339
Carhart-Harris, R. L., Roseman, L., Haijen, E., Erritzoe, D., Watts, R., Branchi, I., et al. (2018). Psychedelics and the essential importance of context. J. Psychopharmacol. 32 (7), 725–731. doi:10.1177/0269881118754710
Carmont, H., and McIlfatrick, S. (2022). Using virtual reality in palliative care: a systematic integrative review. Int. J. Palliat. Nurs. 28 (3), 132–144. doi:10.12968/ijpn.2022.28.3.132
Dahill, A., Al-Nakishbandi, H., Cunningham, K., Humphris, G., Lowe, D., and Rogers, S. (2020). Loneliness and quality of life after head and neck cancer. Br. J. Oral Maxillofac. Surg. 58 (8), 959–965. doi:10.1016/j.bjoms.2020.04.041
Dang, M., Noreika, D., Ryu, S., Sima, A., Ashton, H., Ondris, B., et al. (2021a). Feasibility of delivering an avatar-facilitated life review intervention for patients with cancer. J. Palliat. Med. 24 (4), 520–526. doi:10.1089/jpm.2020.0020
Dang, P., Zhu, J., Pirasteh, S., Li, W., You, J., Xu, B., et al. (2021b). A chain navigation grid based on cellular automata for large-scale crowd evacuation in virtual reality. Int. J. Appl. Earth Observation Geoinformation 103, 102507. doi:10.1016/j.jag.2021.102507
Drageset, J., Eide, G. E., Kirkevold, M., and Ranhoff, A. H. (2013). Emotional loneliness is associated with mortality among mentally intact nursing home residents with and without cancer: a five-year follow-up study. J. Clin. Nurs. 22 (1-2), 106–114. doi:10.1111/j.1365-2702.2012.04209.x
Ferguson, C., Shade, M. Y., Blaskewicz Boron, J., Lyden, E., and Manley, N. A. (2020). Virtual reality for therapeutic recreation in dementia hospice care: a feasibility study. Am. J. Hospice Palliat. Medicine® 37 (10), 809–815. doi:10.1177/1049909120901525
Friedrich, S., and Pauly, M. (2018). MATS: inference for potentially singular and heteroscedastic MANOVA. J. Multivar. Analysis 165, 166–179. doi:10.1016/j.jmva.2017.12.008
Fulton, J. J., Newins, A. R., Porter, L. S., and Ramos, K. (2018). Psychotherapy targeting depression and anxiety for use in palliative care: a meta-analysis. J. Palliat. Med. 21 (7), 1024–1037. doi:10.1089/jpm.2017.0576
Gaspar, P., Westberg, K., Baker, A., Dunlap, T., and Nordlinger, K. (2018). What are the QoL outcomes of a group virtual reality experience for assisted living and independent living residents? Innovation Aging 2 (Suppl. 1), 1016.
Glowacki, D. R. (2024). VR models of death and psychedelics: an aesthetic paradigm for design beyond day-to-day phenomenology. Front. Virtual Real. 4, 1286950. doi:10.3389/frvir.2023.1286950
Glowacki, D. R., Williams, R. R., Wonnacott, M. D., Maynard, O. M., Freire, R., Pike, J. E., et al. (2022). Group VR experiences can produce ego attenuation and connectedness comparable to psychedelics. Sci. Rep. 12, 8995. doi:10.1038/s41598-022-12637-z
Glowacki, D. R., Wonnacott, M. D., Freire, R., and Glowacki, B. R. (2020). Isness: using multi-person VR to design peak mystical type experiences comparable to psychedelics. arxiv logo, 1–14. doi:10.1145/3313831.3376649
Grassi, L., and Riba, M. (2014). Psychopharmacology in oncology and palliative care: a practical manual. Springer.
Greyson, B. (2015). Reduced death threat in near-death experiencers. Death anxiety handbook: research, instrumentation, and application. New York: Taylor & Francis, 169–179.
Griffiths, R. R., Johnson, M. W., Carducci, M. A., Umbricht, A., Richards, W. A., Richards, B. D., et al. (2016). Psilocybin produces substantial and sustained decreases in depression and anxiety in patients with life-threatening cancer: a randomized double-blind trial. J. Psychopharmacol. 30 (12), 1181–1197. doi:10.1177/0269881116675513
Griffiths, R. R., Richards, W. A., McCann, U., and Jesse, R. (2006). Psilocybin can occasion mystical-type experiences having substantial and sustained personal meaning and spiritual significance. Psychopharmacology 187 (3), 268–283. doi:10.1007/s00213-006-0457-5
Grob, C. S., Danforth, A. L., Chopra, G. S., Hagerty, M., McKay, C. R., Halberstadt, A. L., et al. (2011). Pilot study of psilocybin treatment for anxiety in patients with advanced-stage cancer. Archives General Psychiatry 68 (1), 71–78. doi:10.1001/archgenpsychiatry.2010.116
Gukasyan, N., and Nayak, S. M. (2022). Psychedelics, placebo effects, and set and setting: insights from common factors theory of psychotherapy. Transcult. Psychiatry 59 (5), 652–664. doi:10.1177/1363461520983684
Ho, K. H. M., Yang, C., Ng, M. S. N., Tao, A., and Chan, H. Y. L. (2023). Loneliness at end-of-life: a scoping review. J. Clin. Nurs. 32 (17-18), 6179–6195. doi:10.1111/jocn.16748
Huber, J., Muck, T., Maatz, P., Keck, B., Enders, P., Maatouk, I., et al. (2018). Face-to-face vs. online peer support groups for prostate cancer: a cross-sectional comparison study. J. Cancer Surviv. 12, 1–9. doi:10.1007/s11764-017-0633-0
Hvidt, N. C., and Assing Hvidt, E. (2019). Religiousness, spirituality and health in secular society: need for spiritual care in health care? Spiritual. Religiousness Health Res. Clin. Pract., 133–152. doi:10.1007/978-3-030-21221-6_9
Hyland, K. A., Small, B. J., Gray, J. E., Chiappori, A., Creelan, B., Tanvetyanon, T., et al. (2019). Loneliness as a mediator of the relationship of social cognitive variables with depressive symptoms and quality of life in lung cancer patients beginning treatment. Psycho-oncology 28 (6), 1234–1242. doi:10.1002/pon.5072
Ihrig, A., Karschuck, P., Haun, M. W., Thomas, C., and Huber, J. (2020). Online peer-to-peer support for persons affected by prostate cancer: a systematic review. Patient Educ. Couns. 103 (10), 2107–2115. doi:10.1016/j.pec.2020.05.009
Ioannou, A., Papastavrou, E., Avraamides, M. N., and Charalambous, A. (2020). Virtual reality and symptoms management of anxiety, depression, fatigue, and pain: a systematic review. SAGE open Nurs. 6, 2377960820936163. doi:10.1177/2377960820936163
Johnson, T., Bauler, L., Vos, D., Hifko, A., Garg, P., Ahmed, M., et al. (2020). Virtual reality use for symptom management in palliative care: a pilot study to assess user perceptions. J. Palliat. Med. 23 (9), 1233–1238. doi:10.1089/jpm.2019.0411
Kettner, H., Rosas, F. E., Timmermann, C., Kärtner, L., Carhart-Harris, R. L., and Roseman, L. (2021). Psychedelic communitas: intersubjective experience during psychedelic group sessions predicts enduring changes in psychological wellbeing and social connectedness. Front. Pharmacol. 12, 234. doi:10.3389/fphar.2021.623985
Kissane, D. W., Wein, S., Love, A., Lee, X. Q., Kee, P. L., and Clarke, D. M. (2004). The Demoralization Scale: a report of its development and preliminary validation. J. Palliat. care 20 (4), 269–276. doi:10.1177/082585970402000402
LeMay, K., and Wilson, K. G. (2008). Treatment of existential distress in life threatening illness: a review of manualized interventions. Clin. Psychol. Rev. 28 (3), 472–493. doi:10.1016/j.cpr.2007.07.013
Lovakov, A., and Agadullina, E. R. (2021). Empirically derived guidelines for effect size interpretation in social psychology. Eur. J. Soc. Psychol. 51 (3), 485–504. doi:10.1002/ejsp.2752
MacLean, K. A., Leoutsakos, J. S., Johnson, M. W., and Griffiths, R. R. (2012). Factor analysis of the mystical experience questionnaire: a study of experiences occasioned by the hallucinogen psilocybin. J. Sci. study Relig. 51 (4), 721–737. doi:10.1111/j.1468-5906.2012.01685.x
Marshall, J., Devane, N., Talbot, R., Caute, A., Cruice, M., Hilari, K., et al. (2020). A randomised trial of social support group intervention for people with aphasia: a Novel application of virtual reality. PloS one 15 (9), e0239715. doi:10.1371/journal.pone.0239715
Martial, C., Cassol, H., Slater, M., Bourdin, P., Mensen, A., Oliva, R., et al. (2023). Electroencephalographic signature of out-of-body experiences induced by virtual reality: a novel methodological approach. J. Cognitive Neurosci. 35 (9), 1410–1422. doi:10.1162/jocn_a_02011
Martin, J. L., Saredakis, D., Hutchinson, A. D., Crawford, G. B., and Loetscher, T. (2022). Virtual reality in palliative care: a systematic review. Healthcare 10, 1222. doi:10.3390/healthcare10071222
McGhee, W. R., Doherty, C. J., Graham-Wisener, L., Fallis, R., Stone, C., Axiaq, A., et al. (2024). Immersive virtual reality and psychological well-being in adult chronic physical illness: systematic review. BMJ Support. & Palliat. Care 14 (1), 14–24. doi:10.1136/spcare-2023-004502
Menzies, R. E., Zuccala, M., Sharpe, L., and Dar-Nimrod, I. (2018). The effects of psychosocial interventions on death anxiety: a meta-analysis and systematic review of randomised controlled trials. J. anxiety Disord. 59, 64–73. doi:10.1016/j.janxdis.2018.09.004
Meyer, T. J., and Mark, M. M. (1999). “Effects of psychosocial interventions with adult cancer patients: a meta-analysis of randomized experiments.”
Mitchell, A. J., Chan, M., Bhatti, H., Halton, M., Grassi, L., Johansen, C., et al. (2011). Prevalence of depression, anxiety, and adjustment disorder in oncological, haematological, and palliative-care settings: a meta-analysis of 94 interview-based studies. lancet Oncol. 12 (2), 160–174. doi:10.1016/s1470-2045(11)70002-x
Mo, J., Vickerstaff, V., Minton, O., Tavabie, S., Taubert, M., Stone, P., et al. (2022). How effective is virtual reality technology in palliative care? A systematic review and meta-analysis. Palliat. Med. 36 (7), 1047–1058. doi:10.1177/02692163221099584
Muttoni, S., Ardissino, M., and John, C. (2019). Classical psychedelics for the treatment of depression and anxiety: a systematic review. J. Affect. Disord. 258, 11–24. doi:10.1016/j.jad.2019.07.076
Ngai, I., Tully, E. C., and Anderson, P. L. (2015). The course of the working alliance during virtual reality and exposure group therapy for social anxiety disorder. Behav. Cognitive Psychotherapy 43 (2), 167–181. doi:10.1017/s135246581300088x
Niki, K., Okamoto, Y., Maeda, I., Mori, I., Ishii, R., Matsuda, Y., et al. (2019). A novel palliative care approach using virtual reality for improving various symptoms of terminal cancer patients: a preliminary prospective, multicenter study. J. Palliat. Med. 22 (6), 702–707. doi:10.1089/jpm.2018.0527
Nour, M. M., Evans, L., Nutt, D., and Carhart-Harris, R. L. (2016). Ego-dissolution and psychedelics: validation of the ego-dissolution inventory (EDI). Front. Hum. Neurosci. 10, 269. doi:10.3389/fnhum.2016.00269
Ostuzzi, G., Matcham, F., Dauchy, S., Barbui, C., and Hotopf, M. (2018). Antidepressants for the treatment of depression in people with cancer. Cochrane Database Syst. Rev. 2018 (4). doi:10.1002/14651858.cd011006.pub3
Pehlivanova, M., Carroll, A., and Greyson, B. (2023). Which near-death experience features are associated with reduced fear of death? Mortality 28 (3), 493–509. doi:10.1080/13576275.2021.2017868
Peterman, A. H., Fitchett, G., Brady, M. J., Hernandez, L., and Cella, D. (2002). Measuring spiritual well-being in people with cancer: the functional assessment of chronic illness therapy—spiritual Well-being Scale (FACIT-Sp). Ann. Behav. Med. 24 (1), 49–58. doi:10.1207/s15324796abm2401_06
Pitman, A., Suleman, S., Hyde, N., and Hodgkiss, A. (2018). Depression and anxiety in patients with cancer. Bmj 361, k1415. doi:10.1136/bmj.k1415
Rains, S. A., and Young, V. (2009). A meta-analysis of research on formal computer-mediated support groups: examining group characteristics and health outcomes. Hum. Commun. Res. 35 (3), 309–336. doi:10.1111/j.1468-2958.2009.01353.x
Randall, R. L., Arthur Woodward, J., and Bonett, D. G. (1997). A wald test for the multivariate analysis of variance: small sample critical values. Commun. Statistics-Simulation Comput. 26 (4), 1275–1299. doi:10.1080/03610919708813440
Rehse, B., and Pukrop, R. (2003). Effects of psychosocial interventions on quality of life in adult cancer patients: meta analysis of 37 published controlled outcome studies. Patient Educ. Couns. 50 (2), 179–186. doi:10.1016/s0738-3991(02)00149-0
Rokach, A. (2003). Causes of loneliness of those afflicted with life-threatening illnesses. Soc. Behav. Personality Int. J. 31 (7), 663–674. doi:10.2224/sbp.2003.31.7.663
Roseman, L., Haijen, E., Idialu-Ikato, K., Kaelen, M., Watts, R., and Carhart-Harris, R. (2019). Emotional breakthrough and psychedelics: validation of the emotional breakthrough inventory. J. Psychopharmacol. 33 (9), 1076–1087. doi:10.1177/0269881119855974
Roseman, L., Nutt, D. J., and Carhart-Harris, R. L. (2018). Quality of acute psychedelic experience predicts therapeutic efficacy of psilocybin for treatment-resistant depression. Front. Pharmacol. 8, 974. doi:10.3389/fphar.2017.00974
Rosenfeld, D., Catalan, J., and Ridge, D. (2018). Strategies for improving mental health and wellbeing used by older people living with HIV: a qualitative investigation. AIDS Care 30 (Suppl. 2), 102–107. doi:10.1080/09540121.2018.1468016
Ross, S., Bossis, A., Guss, J., Agin-Liebes, G., Malone, T., Cohen, B., et al. (2016). Rapid and sustained symptom reduction following psilocybin treatment for anxiety and depression in patients with life-threatening cancer: a randomized controlled trial. J. Psychopharmacol. 30 (12), 1165–1180. doi:10.1177/0269881116675512
Salehi, E., Mehrabi, M., Fatehi, F., and Salehi, A. (2020) “Virtual reality therapy for social phobia: a scoping review,” in Medical informatics in europe conference (MIE) 2020. Amsterdam, Netherlands: IOS Press.
Seyama, J. i., and Nagayama, R. S. (2007). The uncanny valley: effect of realism on the impression of artificial human faces. Presence 16 (4), 337–351. doi:10.1162/pres.16.4.337
Shah, N., Cader, M., Andrews, W. P., Wijesekera, D., and Stewart-Brown, S. L. (2018). Responsiveness of the short Warwick Edinburgh mental well-being scale (SWEMWBS): evaluation a clinical sample. Health Qual. life Outcomes 16 (1), 239. doi:10.1186/s12955-018-1060-2
Snaith, R. P. (2003). The hospital anxiety and depression scale. Health Qual. life Outcomes 1, 1–4. doi:10.1186/1477-7525-1-29
Tassell-Matamua, N. A., and Lindsay, N. (2016). “I’m not afraid to die”: the loss of the fear of death after a near-death experience. Mortality 21 (1), 71–87. doi:10.1080/13576275.2015.1043252
Timmermann, C., Roseman, L., Williams, L., Erritzoe, D., Martial, C., Cassol, H., et al. (2018). DMT models the near-death experience. Front. Psychol. 9, 395026. doi:10.3389/fpsyg.2018.01424
Watts, R., Kettner, H., Geerts, D., Gandy, S., Kartner, L., Mertens, L., et al. (2022). The Watts Connectedness Scale: a new scale for measuring a sense of connectedness to self, others, and world. Psychopharmacology 239 (11), 3461–3483. doi:10.1007/s00213-022-06187-5
Wong, P. T., Reker, G. T., and Gesser, G. (1994). Death Attitude Profile-Revised: a multidimensional measure of attitudes toward death. Death anxiety Handb. Res. Instrum. Appl. 121, 121–148.
Woo, O. K., Lee, A. M., Ng, R., Eckhoff, D., Lo, R., and Cassinelli, A. (2024). Flourishing-Life-Of-Wish Virtual Reality Relaxation Therapy (FLOW-VRT-Relaxation) outperforms traditional relaxation therapy in palliative care: results from a randomized controlled trial. Front. Virtual Real. 4, 1304155. doi:10.3389/frvir.2023.1304155
Wyatt, K. (2023). “Virtual reality as a tool for end-of-life anxiety and pain with gregory roufa and lama karma,” in End-of-Life University Podcast. Available at: https://podcasts.apple.com/us/podcast/ep-389-virtual-reality-as-a-tool-for-end-of/id1033282990?i=1000598245311.
Keywords: virtual reality, life-threatening illness, wellbeing, anxiety, depression, psychosocial intervention, internet-based intervention, cohort study
Citation: Kettner H, Glowacki DR, Wall J, Carhart-Harris RL, Roseman L and Hardy JL (2025) Observational cohort study of a group-based VR program to improve mental health and wellbeing in people with life-threatening illnesses. Front. Virtual Real. 5:1466362. doi: 10.3389/frvir.2024.1466362
Received: 17 July 2024; Accepted: 03 December 2024;
Published: 07 January 2025.
Edited by:
Patrick K. A. Neff, University of Zurich, SwitzerlandReviewed by:
Katarzyna Wyka, City University of New York, United StatesLawrence Fischman, Tufts University, United States
Copyright © 2025 Kettner, Glowacki, Wall, Carhart-Harris, Roseman and Hardy. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Joseph L. Hardy, amxoYXJkeXBoZEBnbWFpbC5jb20=
 Hannes Kettner
Hannes Kettner David R. Glowacki
David R. Glowacki Justin Wall3,4,5
Justin Wall3,4,5 Robin L. Carhart-Harris
Robin L. Carhart-Harris Leor Roseman
Leor Roseman Joseph L. Hardy
Joseph L. Hardy