
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
BRIEF RESEARCH REPORT article
Front. Virtual Real., 20 March 2024
Sec. Virtual Reality in Medicine
Volume 5 - 2024 | https://doi.org/10.3389/frvir.2024.1369794
 Maximiliano Abundez Toledo1*†
Maximiliano Abundez Toledo1*† Ghadi Ghanem1†
Ghadi Ghanem1† Stuart Fine1†
Stuart Fine1† Daniel Weisman1,2
Daniel Weisman1,2 Yue Ming Huang2,3
Yue Ming Huang2,3 Amir A. Rouhani4
Amir A. Rouhani4Virtual reality (VR) has the potential to be used as a transformative tool in medical education - offering both interactive models and clinical simulations to enhance training. VR presents a space and cost-effective solution for remote education, combined with prospects of higher efficiency and interactivity than traditional training. This study aimed to explore the potential application and perception of VR in a focus group of medical students as an innovative tool for learning anatomy. Sixteen students underwent a structured VR lesson plan exploring concepts in anatomy. Pre- and post-surveys assessed participants’ exposure to VR, previous exposure to and preparedness in anatomy training, and attitudes toward VR. Results revealed that despite limited prior exposure to VR, participants found the technology both easy to navigate and comfortable to use. Notably, over 90% of students indicated that VR would enhance their anatomy learning experience and help them learn a topic better than traditional models. Furthermore, 94% of participants agreed that this learning modality should be offered to medical students, and if given access to this technology, most would utilize it for learning anatomy and potentially for other subjects as well. This study emphasizes VR’s potential to enhance medical education, particularly in anatomy instruction. VR’s adaptability, user-friendly interface, and positive student perceptions highlight its viability as a supplemental tool. Future research should explore specific anatomy applications, long-term impacts on knowledge retention, and the evolving role of VR in medical education.
Virtual reality (VR) is a novel learning tool that allows for the creation of interactive models and clinical simulations that can enhance undergraduate medical education. VR provides space and resource-effective education as it substitutes resource-intensive simulation technologies, such as high-fidelity computerized mannequin simulators, with a reusable head-mounted display (Erolin et al., 2019). This modality has been shown to also be cost-effective when compared to mannequin based methods, with a lower cost per point improvement in knowledge (Haerling, 2018). This immersive learning modality has been adopted in various fields such as neurosurgery, echocardiography, and orthopedics for resident training (O'Sullivan et al., 2021; Bernardo, 2017; Hall and Walmsley, 2022). VR’s expansion into graduate medical education has showcased it as superior or equal to traditional teaching modalities (Khatkar et al., 2022). Furthermore, students and trainees have expressed favorable impressions of this technology when compared to conventional methods (Kolla et al., 2020; Uruthiralingam and Rea, 2020; Hall and Walmsley, 2022; Khatkar et al., 2022).
The COVID-19 pandemic propelled telemedicine and remote learning modalities to the forefront of medical education. During this time, many interactive learning opportunities were removed from medical school curricula due to in-person restrictions and space limitations (Shahrvini et al., 2020). VR offers opportunities for remote learning in today’s dynamic medical environment, combined with low cost of maintenance, scalability, and real-time corrective feedback (Wickramasinghe et al., 2022). Studies have also highlighted the long-term economic benefits of investing in VR simulation to reduce the significant costs associated with books, classes, animals, and mannequins (Duarte et al., 2020). Therefore, VR technology has the potential to reduce disparities for trainees in remote or resource-limited settings by increasing access to standardized simulation-based learning (Pottle, 2019).
Despite its prospects, the implementation of VR in undergraduate medical education has been limited. In this study, we aimed to explore the potential application of VR in a focus group of current medical students as an innovative tool for learning anatomy.
We conducted a focus group at a traditional four-year medical school in the United States. Students were recruited from all years of medical training via email and social media postings. The only eligibility criteria was that students be currently enrolled in the medical school. This protocol was reviewed and approved by the institutional review board at UCLA (IRB #23-000163). All participants provided informed consent before participating in this study and did not receive financial compensation or undue influence throughout their participation.
Sixteen medical students completed the study at a California medical school in May of 2023. Each student was assigned a random study ID number and was informed that their responses to the surveys would be de-identified. Two fourth-year medical students with prior experience with VR and familiarity with the software served as peer instructors.
Upon enrollment, students were assigned to a focus group time by order of ranked preference, during which students underwent a confidence and experience pre-survey, a VR session, and an experience post-survey. Questions were scored on a 5-point Likert Scale with answers ranging from 1 (strongly disagree) to 5 (strongly agree). All surveys were created using Qualtrics (Seattle, WA, v6.21). All materials were originals created by the peer instructors and reviewed by faculty physicians.
The pre-survey consisted of six questions that focused on previous exposure to VR, anatomy proficiency, and technological literacy. The teaching demonstration took place in a multimedia room at the medical school. Participants were assigned to a station with an individual Oculus headset (Oculus Quest 2, version 55) and pre-mapped safety margin to avoid physically overlapping with other users. The demonstration was in collaboration with MAI, a VR technology company that provides BodyMap-an immersive anatomy education software-that was integral to this study. Students were then guided through a safety briefing for proper use of the equipment and asked to watch a 5-min demonstration of an instructor interacting with the hardware and software. This demonstration informed the students of how to navigate body and organ systems, as well as how to use virtual tools including zoom, slicer, pointer, rotation, labeling, quiz, and point-and-drag for manipulation and interaction with the display in front of them through handheld controllers and the headset.
The following six questions encompassed the Pre-VR questionnaire administered to the participants prior to the VR instruction:
1. I have had significant exposure to virtual reality in the past.
2. I consider myself proficient with technology/computers.
3. I have spent a significant amount of time in the anatomy lab.
4. I believe the current curriculum’s pre-anatomy lab modules and materials are sufficient for me to feel prepared before anatomy lab sessions.
5. I have had exposure to anatomy courses before medical school.
6. I am satisfied with the curriculum.
Participants then put on their headsets and were led through a structured lesson plan for basic anatomy over the course of 20 min. It took place in a multi-user VR setting in which groups of 3–5 participants joined the same virtual room and watched the instructor as they were guided on appropriate use of the software. This lesson plan began by providing an orientation of the visual space in front of the participants as well as the tools and menus available to each of them. Next, instructors proceeded with the identification and isolation of structures, spatial relationships, manipulation of anatomical landmarks, and plane dissection across body systems including cardiovascular, musculoskeletal, lymphatic, and nervous systems. Specifically, the lesson began with visualizing the skeletal system from head to toe with the freedom to walk around and view it from different angles as instructors pointed to, labeled, and manipulated individual bones such as the vertebrae and ribs. This was followed by the cardiovascular display where participants visualized the heart, main arteries and veins, and were led through a stepwise tracing of the aorta down through its bifurcation and similarly, the inferior vena cava and its tributaries into the heart. For the lymphatic and nervous systems, the participants saw a rendering of each where they got a sense of the vast connections throughout the body as instructors highlighted and manipulated the cervical lymph nodes, inguinal lymph nodes, vagus, and sciatic nerves. Participants were led through different activities and instructed to follow along with the instructors and replicate different maneuvers to obtain the same views and results, pausing for understanding and guidance as needed. Students were then allowed to freely interact with the software utilizing any of the available tools or body systems by using the skills they were previously taught by the instructors. This “free play” session lasted for 10 min for individual exploration with continued technical support and access to instructors for clarification. During this time, participants were able to go back to any portions of the lesson plan and manipulate structures covered in the lesson as well as any specific areas of interest. Instructors were on hand for directions on how to isolate, manipulate, and drag specific body parts at any level of magnification they desired.
After the training, each student took a confidence post-test with questions pertaining to their overall experience with VR, and about how they envision it being integrated into the curriculum. The survey again used a 5-point Likert scale and was administered via a tablet device without the peer instructor present. A free response section (questions 13-15) was also added to the survey to elicit feedback on the session and other applications in which VR could be used in the medical curriculum. Lastly, questions 16 and 17 were used to assess the level of training and the perception for who this training would be most appropriate.
The following 17 questions encompassed the Post-VR questionnaire administered to the participants after the VR instruction:
1. Using VR helped me learn this topic better than a lecture would have.
2. The learning environment was safe and supportive.
3. The case facilitator helped me learn as much as possible from the simulation.
4. I felt comfortable using the VR headset.
5. The VR experience was easy to navigate.
6. I believe utilizing VR would help me to learn anatomy.
7. I believe VR could replace in-person anatomy training.
8. I feel that I retained information taught during the VR session more so than if it were taught using slides or lectures.
9. I believe medical schools should give students access to VR modules.
10. I believe utilizing VR would help me to learn subjects other than anatomy.
11. I would use VR in my medical training if it was available to me.
12. Using VR would be more efficient for my learning.
13. What would have made this session better?
14. What applications do you believe VR could have in your medical school training?
15. What problems do you foresee in utilizing VR as part of your learning?
16. Your Current Training level:
17. This case would be best for:
Participants had a wide array of background experiences relevant to the study. Most of the students (81%) denied having significant previous exposure to VR, and 56% of them answered neutral when asked if they considered themselves proficient with technology while 44% agreeing to being proficient.
The majority of students (11 out of 16 or 69%) had limited exposure to anatomy courses before medical school. Responses gauging whether participants had spent significant amounts of time in the anatomy lab were varied, with 10 out of 16 (63%) students reporting agreement or strong agreement. The majority (63%) of students answered neutrally when asked if they believed the current curriculum’s preparatory modules and materials for anatomy lab were sufficient to feel prepared before the lab session.
All learners strongly agreed that the learning environment felt safe and supportive throughout the session. 15 out of the 16 participants also strongly agreed that case facilitators helped them to learn as much as possible during the instructional component (Figure 1).
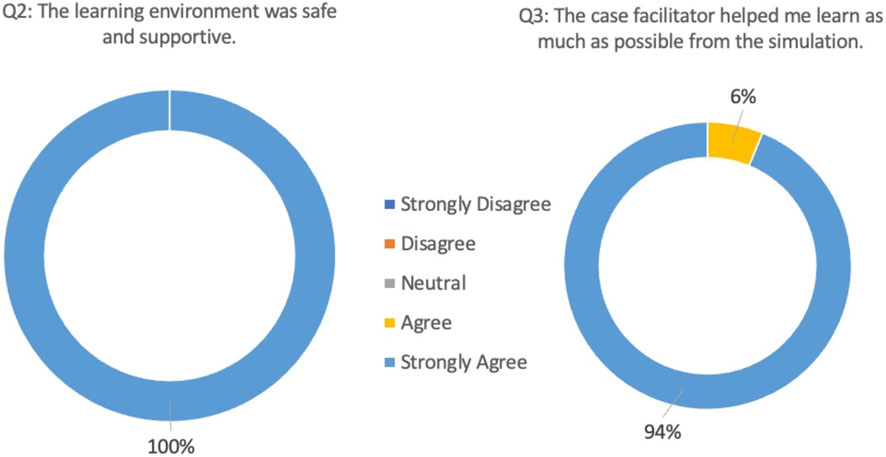
Figure 1. Post-VR training survey questions 2 and 3 pertaining to the learning environment and facilitator.
The majority of participants (14 out of 16) indicated that they felt comfortable using the VR headset, with 6 participants strongly agreeing and 8 participants agreeing with this statement. 15 out of 16 participants also indicated that they found the VR experience easy to navigate (Figure 2).
14 out of 16 participants agreed or strongly agreed that using VR helped them learn the subject matter better than a traditional lecture would have. Specifically, 13 out of 16 participants strongly agreed that utilizing VR would help them to learn anatomy. However, in assessing whether VR could entirely replace in-person anatomy training, the majority (7 out of 16) expressed neutrality and an additional 7 participants disagreed or strongly disagreed. Only 2 participants agreed to some extent.
10 participants supported the statement that they would retain more information if it were taught using VR versus traditional teaching with slides or lectures. Only one individual disagreed with this statement, while 5 remained neutral (Figure 3).
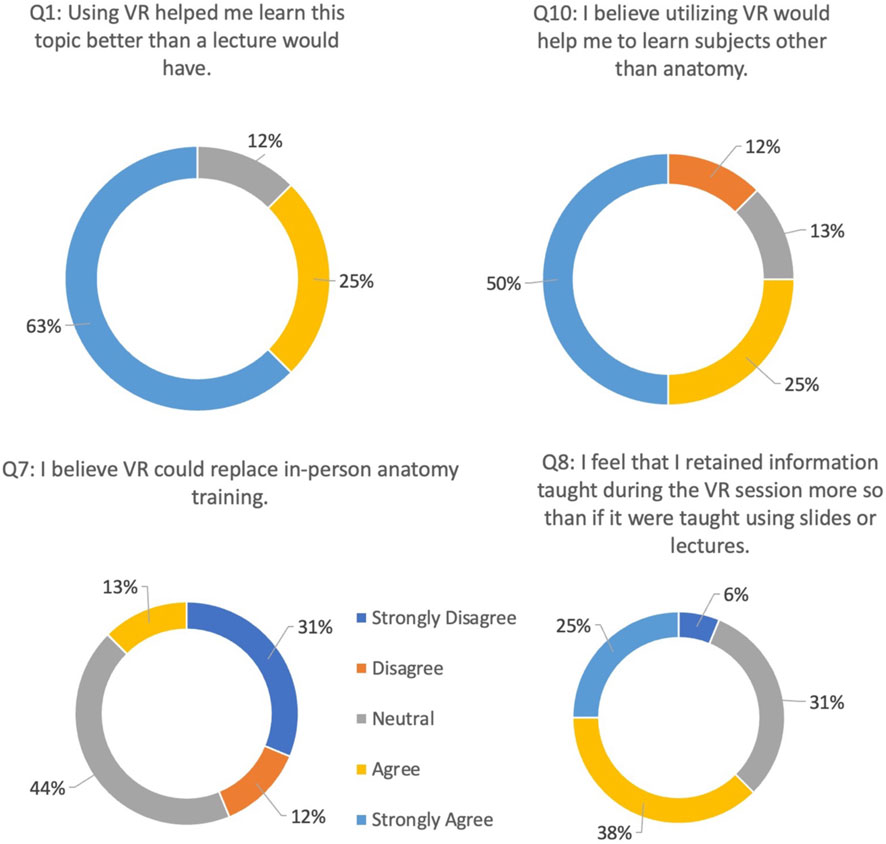
Figure 3. Post-VR training survey questions 1, 7, 8, and 10 pertaining to the comparison between Virtual Reality and traditional modalities.
75% (12 of 16 students) of participants agreed that utilizing VR would help learners with subjects other than anatomy. 15 of the participants agreed that medical schools should give students access to VR modules, 14 of whom stated that they would use the VR software if it was available to them. The majority of participants (13 out of 16) also expressed that VR would be efficient for their learning of materials (Figure 4).
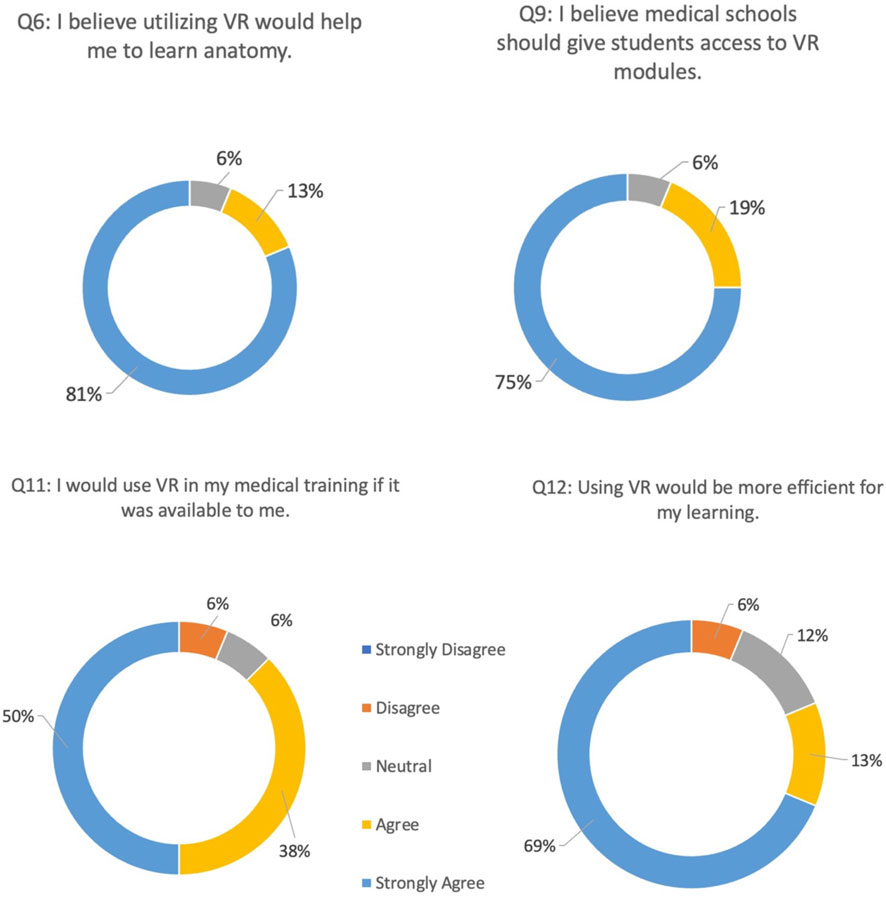
Figure 4. Post-VR training survey questions 6, 9, 11, and 12 pertaining to student’s perceptions of VR implementation in medical school.
Specific comments from participants included that they would want VR to be used as an adjunct to anatomy lab to get a closer review of structures that could not be seen in cadavers, or so that they may spend more time studying at home. Others suggested its utility as a preparatory material for anatomy lab, with an emphasis on pre-recorded VR lectures to enhance interactivity and retention of information. One participant noted its utility in remote learning during COVID-19 surges or similar stay-at-home situations; other applications suggested including pathology, simulation practice, surgical workshops, and peer anatomy tutoring.
Some reservations noted by the participants included a learning curve for use in first-time users, discomfort with prolonged operation of the headset, financial barriers to entry assuming that the headsets would be individually purchased by the students for their own learning and not by their school.
50% of our enrolled participants were first-year medical students, with another 25% being second-year students. Third- and fourth-year medical students comprised 6.25% and 12.5% of the study participants, respectively. Lastly, we had one MD PhD student participate.
When the participants were asked to indicate what level of training this session would be most appropriate for, the majority (67%) indicated that first year medical students would be the ideal. 27% indicated second year medical students, and the rest responded that “Everyone” could benefit from this.
The results of our study suggest that Virtual Reality (VR) is a promising tool for enhancing medical education, with anatomy being an ideal introduction to this technology. Despite most of our participants having limited previous exposure to VR, the vast majority found the technology easy to navigate and felt comfortable using the VR headset after just a brief presentation and a short amount of time interacting with the equipment. Our results show that with a supportive environment and facilitation, nearly all participants felt comfortable using the headset and found the overall experience to be easy to navigate. These findings are encouraging as they highlight the low barrier to entry for this technology even as a first-time experience for a lot of students. This information is critical in the evaluation of VR as a supplemental tool for anatomy instruction because it speaks to the user-friendly interface and quick adoption by students at different levels of familiarity.
In assessing the perceived effectiveness of VR as compared to traditional modalities, our results showed that over 90% of students believed that using VR would help them learn anatomy better than a lecture. This was further supported by the belief that this mode of teaching would help them retain the information learned better than traditional modalities. This data highlights the utility of VR within the scope of medical anatomy training as medical students at different levels of training expressed positive impressions of how this could benefit them in comparison to the ways in which they learned or are currently learning this complex material. The student perspective on this is invaluable and should be used as a guiding principle when assessing curriculum supplementation or restructuring to better cater to their needs and interests. However, it is important to note that our results also suggest that students do not yet believe that VR can replace in-person anatomy training (cadaver lab and physical models) entirely, but rather should act as a complement to in-person learning. Our initial exploratory study had a small sample size and selection bias may have contributed to the positive reactions. A wider scale VR integration will need to be examined to generalize to the entire student population.
Presumably, having access to this technology could improve the quality of preparation for anatomy lab and serve as an additional tool to yield better outcomes for students in basic anatomy courses. We propose that spending preparatory time with VR anatomy simulation may lead to students feeling better prepared for in-person cadaver laboratory by providing more concrete context and spatial understanding prior to coming into sessions. Most importantly, students in our study agreed that if this technology was available to them, they would utilize it for their medical training - both for anatomy and other different subjects. While learning outcomes were beyond the scope of our feasibility study, our findings align with previous studies that have highlighted the benefits of VR in medical education (Moro et al., 2017). For example, a meta-analysis conducted on the teaching of anatomy utilizing VR found a statistically significant pooled moderate enhancement in the standardized mean difference in test scores of VR learners in comparison with conventional teaching methods (Zhao et al., 2020). Our findings suggest that anatomy curricula using similar preparatory material for cadaver labs as the ones used by the medical school in this study- PowerPoint slides with sketches/drawings of anatomical landmarks-can be supplemented or replaced with VR lessons. These may come in the form of prerecorded walk throughs or individualized navigation of structures using the existing educational tools provided by the software such as labeling, highlighting, flashcard and quiz creation, and informational tags. However, given the importance of the interactive and tactile experiences provided by the in-person cadaver lab, especially for medical specialties requiring in depth understanding of anatomy and anatomical variations in patients such as surgery and emergency medicine, our study does not suggest that VR will or should replace cadaver labs themselves. We pose it as a supplementary preparatory tool with great promise to improve the experience of the students in the lab, allowing for more efficient and high-fidelity learning.
While the initial investment in VR equipment may seem substantial, the subsequent savings can help recuperate costs (Katz et al., 2020). Notably, utilization of VR can help replace the need for expensive anatomic models, specialized training facilities, simulation equipment, and specially prepared cadaveric models. In addition, the virtual environment allows for repeated practice without the consumption of physical resources, reducing the cost of consumables. VR can also significantly enhance efficiency and self-efficacy in the learning process (Chiang et al., 2022). Traditional medical education often relies on the rigid schedules of educators and the constraints of physical space. However, VR can provide workarounds for these limitations by providing a flexible, asynchronous, and on-demand learning environment - with the ability to pre-record interactive sessions. Learners can engage in anatomy modules and realistic medical simulations at their own pace, repeating lessons and scenarios as needed to reinforce understanding and skills - thereby helping to provide an individualized learning setting for each learner. This on-demand access to training materials reduces the time constraints associated with scheduling physical facilities, coordinating with instructors, and waiting for specific equipment availability. The time saved through VR learning can ultimately translate into accelerated competency development among medical students - a concept identified by students in our study who overwhelmingly agreed that VR would be more effective for their learning than traditional methods alone such as cadaver lab, 3D modeling, or anatomy PowerPoint slides. With current trends in medical education where students are expected to engage in more independent learning, VR can support optimize the time spent with clinical facilitators.
Alternatively, similar forms of spatial rendering for anatomy education such as 3D anatomy applications on phones and tablets could provide a way for students to interact with anatomical structures. Some applications can render scans of real cadaver tissue which could also serve as a supplementary tool for medical students to better prepare for the visual components and natural variations encountered in the cadaver lab. While these tools could be helpful and potentially more economical, they may not fully replicate the immersive and three-dimensional experience of Virtual Reality that has been shown to enhance spatial understanding and memory retention. A separate study may assess the perception and effectiveness of these different technologies on cadaver lab preparation, performance, and retention.
In conclusion, our study underscores the potential of VR as an innovative tool in medical education. While it may not replace traditional teaching methods entirely, VR can certainly complement in-person anatomy instruction and offer unique learning opportunities. VR offers several advantages over traditional teaching methods, including immersion, interactivity, and visualization. As technology continues to evolve, we anticipate that VR will play an increasingly significant role in medical education. Future research should focus on exploring the specific areas where VR can be most beneficial and investigating the long-term impacts of VR-based learning on knowledge retention and clinical skills development.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving humans were approved by Institutional Review Board at the University of California Los Angeles (IRB #23-000163). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
MA: Writing–review and editing, Writing–original draft, Resources, Project administration, Methodology, Investigation, Formal Analysis, Data curation, Writing–review and editing, Writing–original draft, Resources, Project administration, Methodology, Investigation, Formal Analysis, Data curation, Writing–review and editing, Writing–original draft, Resources, Project administration, Methodology, Investigation, Formal Analysis, Data curation. GG: Writing–review and editing, Writing–original draft, Resources, Project administration, Methodology, Investigation, Formal Analysis, Data curation, Writing–review and editing, Writing–original draft, Resources, Project administration, Methodology, Investigation, Formal Analysis, Data curation, Writing–review and editing, Writing–original draft, Resources, Project administration, Methodology, Investigation, Formal Analysis, Data curation. SF: Writing–review and editing, Writing–original draft, Resources, Project administration, Methodology, Investigation, Formal Analysis, Data curation, Writing–review and editing, Writing–original draft, Resources, Project administration, Methodology, Investigation, Formal Analysis, Data curation, Writing–review and editing, Writing–original draft, Resources, Project administration, Methodology, Investigation, Formal Analysis, Data curation. DW: Writing–original draft, Resources, Methodology, Investigation, Writing–original draft, Resources, Methodology, Investigation, Writing–original draft, Resources, Methodology, Investigation. YH: Writing–review and editing, Resources, Writing–review and editing, Resources, Writing–review and editing, Resources, AR: Writing–review and editing, Writing–original draft, Visualization, Supervision, Project administration, Formal Analysis, Writing–review and editing, Writing–original draft, Visualization, Supervision, Project administration, Formal Analysis, Writing–review and editing, Writing–original draft, Visualization, Supervision, Project administration, Formal Analysis.
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
We would like to express our deepest gratitude to the members of the UCLA Simulation Center for their expertise and assistance with the logistics of this study. Their collaboration significantly contributed to the success of this project and enhanced the quality of our research. We particularly appreciate their technical support and willingness to lend us equipment and materials. Special thanks to Sarah Petro, Operations Director, whose support allowed us to bring this project to life.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Bernardo, A. (2017). Virtual reality and simulation in neurosurgical training. World Neurosurg. 106, 1015–1029. doi:10.1016/j.wneu.2017.06.140
Chiang, D. H., Huang, C. C., Cheng, S. C., Cheng, J. C., Wu, C. H., Huang, S. S., et al. (2022). Immersive virtual reality (VR) training increases the self-efficacy of in-hospital healthcare providers and patient families regarding tracheostomy-related knowledge and care skills: a prospective pre-post study. Med. Baltim. 101 (2), e28570. doi:10.1097/MD.0000000000028570
Duarte, M. L., Santos, L. R., Guimarães Júnior, J. B., and Peccin, M. S. (2020). Learning anatomy by virtual reality and augmented reality. A scope review. Morphologie 104 (347), 254–266. doi:10.1016/j.morpho.2020.08.004
Erolin, C., Reid, L., and McDougall, S. (2019). Using virtual reality to complement and enhance anatomy education. J. Vis. Commun. Med. 42 (3), 93–101. doi:10.1080/17453054.2019.1597626
Haerling, K. A. (2018). Cost-utility analysis of virtual and mannequin-based simulation. Simul. Healthc. J. Soc. Simul. Healthc. 1, 33–40. doi:10.1097/sih.0000000000000280
Hall, A. J., and Walmsley, P. (2022). Technology-enhanced learning in orthopaedics: virtual reality and multi-modality educational workshops may be effective in the training of surgeons and operating department staff. Surgeon 21, 217–224. S1479-666X(22)00077-4. doi:10.1016/j.surge.2022.04.009
Katz, D., Shah, R., Kim, E., Park, C., Shah, A., Levine, A., et al. (2020). Utilization of a voice-based virtual reality advanced cardiac life support team leader refresher: prospective observational study. J. Med. Internet Res. 22 (3), e17425. doi:10.2196/17425
Khatkar, H., Ferro, A., Kotecha, S., Prokopenko, M., Evans, A., Kyriakides, J., et al. (2022). Assessing the attitude of surgical trainees towards virtual reality simulation: a national cross-sectional questionnaire study. Scott Med. J. 67, 87–92. doi:10.1177/00369330221103279
Kolla, S., Elgawly, M., Gaughan, J. P., and Goldman, E. (2020). Medical student perception of a virtual reality training module for anatomy education. Med. Sci. Educ. 30 (3), 1201–1210. doi:10.1007/s40670-020-00993-2
Moro, C., Štromberga, Z., Raikos, A., and Stirling, A. (2017). The effectiveness of virtual and augmented reality in health sciences and medical anatomy. Anat. Sci. Educ. 10 (6), 549–559. doi:10.1002/ase.1696
O’Sullivan, D. M., Foley, R., Proctor, K., Gallagher, S., Deery, A., Eidem, B. W., et al. (2021). The use of virtual reality echocardiography in medical education. Pediatr. Cardiol. 42 (4), 723–726. doi:10.1007/s00246-021-02596-z
Pottle, J. (2019). Virtual reality and the transformation of medical education. Future Healthc. J. 6 (3), 181–185. doi:10.7861/fhj.2019-0036
Shahrvini, B., Baxter, S. L., Coffey, C. S., MacDonald, B. V., and Lander, L. (2020). Pre-clinical remote undergraduate medical education during the COVID-19 pandemic: a survey Study . Res. Sq. doi:10.21203/rs.3.rs-33870/v1
Uruthiralingam, U., and Rea, P. M. (2020). Augmented and virtual reality in anatomical education - a systematic review. Adv. Exp. Med. Biol. 1235, 89–101. doi:10.1007/978-3-030-37639-0_5
Wickramasinghe, N., Thompson, B. R., and Xiao, J. (2022). The opportunities and challenges of digital anatomy for medical sciences: narrative review. JMIR Med. Educ. 8 (2), e34687. doi:10.2196/34687
Keywords: virtual reality, anatomy, simulation, medical education, oculus, augmented reality, headset, meta
Citation: Abundez Toledo M, Ghanem G, Fine S, Weisman D, Huang YM and Rouhani AA (2024) Exploring the promise of virtual reality in enhancing anatomy education: a focus group study with medical students. Front. Virtual Real. 5:1369794. doi: 10.3389/frvir.2024.1369794
Received: 12 January 2024; Accepted: 06 March 2024;
Published: 20 March 2024.
Edited by:
Michael J. Roy, Uniformed Services University, United StatesReviewed by:
Athanasios Raikos, Bond University, AustraliaCopyright © 2024 Abundez Toledo, Ghanem, Fine, Weisman, Huang and Rouhani. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Maximiliano Abundez Toledo, bWF4YnJ1aW4xN0BnLnVjbGEuZWR1
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.