- 1Ashiya Municipal Hospital, Department of Pharmacy, Ashiya, Hyogo, Japan
- 2Osaka University Graduate School of Pharmaceutical Sciences, Osaka, Japan
- 3Ashiya Municipal Hospital, Department of Nursing, Ashiya, Hyogo, Japan
Objective: Even if hospitalized terminal cancer patients wish to go out, it is sometimes difficult for them to realize this because of various symptoms. We have been providing a virtual outing experience using virtual reality (VR) for terminal cancer patients who have difficulty going out, and have often received requests to “talk with people in the virtual outing,” but there is a problem that a large time lag occurs in conversation in a VR space under the general Internet environment. However, with the advent of systems that enable high-speed, low-latency communications, real-time communication is now possible even in VR spaces. Thus, we aimed to explore the feasibility of implementing the real-time virtual outing.
Methods: The patient’s preferred virtual outing was to his daughter’s new home. The study operator used a 360° video real-time sharing system to broadcast the view of the daughter’s home. The patient experienced the images using a VR head-mounted display in his room. The patient’s wife, son, daughter, and grandson participated in this delivery using a laptop computer from a dayroom in the hospital, and his daughter’s husband participated using the 360° video real-time sharing system from the daughter’s home with the researcher. Before and after the virtual outing, changes in symptoms and emotions were assessed using the Edmonton Symptom Assessment System Revised Japanese version and the Numerical Rating Scale for headache, dizziness, pleasure, and satisfaction. In addition, we collected the patients’ impressions of the virtual outing.
Results: The patient was a male in his early 70s. After approximately 30 min of real-time virtual outings, “tiredness, drowsiness, depression, and wellbeing” were improved and “pleasure, and satisfaction” were increased, while no side effects or worsening of symptoms were observed. In addition, it was observed from the patient’s comments that he felt a sense of presence, as if he were her home.
Discussion: The patient and his family could enjoy smooth conversation without time lag even in the VR space. Therefore, it was suggested that real-time virtual outings using VR could help realize the wishes of hospitalized terminal cancer patients who have difficulty going out as a new approach.
1 Introduction
Terminally ill cancer patients may wish to go out. However, even if a hospitalized terminal cancer patient wishes to go out, it may be difficult to achieve due to the decline in physical functions and various symptoms, especially due to restrictions on visits and outings still remain in some hospitals, although many countries have eased restrictions due to coronavirus disease 2019 (COVID-19). Failure to fulfill the wish to go out may have various negative consequences. Specifically, there is a possibility that social interaction and social activities with friends and family will be restricted, resulting in feelings of loneliness, isolation, agitation, and anxiety (Lee et al., 2020; Murayama et al., 2021; van Tilburg et al., 2021).
Therefore, we turned our attention to virtual reality (VR) as a means of fulfilling patients’ desires to go out. Since 2017, we have been providing a virtual outing experience using Google Earth VR to hospitalized terminal cancer patients who have difficulty going outside. Then, we found that virtual outing using VR temporarily improved many of the patients’ physical and mental symptoms of “pain,” “fatigue,” " drowsiness,” “shortness of breath,” “depression,” “anxiety,” and “wellbeing” and did not cause serious side effects (Niki et al., 2019). Since this report, we have been conducting VR outing as a routine part of our care. For photos of the interior of patients’ homes that cannot be viewed on Google Earth, we have asked patients’ family members and others to take photos using 360° cameras and have patients view them as VR images in their hospital rooms to achieve virtual outings. Another report besides ours examined the impact of VR experiences with realistic 360° images on patients receiving palliative care. Austin et al. (2022) reported improved “pain,” “fatigue,” “drowsiness,” “shortness of breath,” “depression,” “anxiety,” and “wellbeing” after viewing VR images of nature. However, as far as we could find, we did not find any case in which a patient went on a VR outing according to his or her preferred location and examined the effects of the VR outing. During our own efforts, we have received requests from several people who have experienced VR outing that they would like to have conversations with people in the VR space, but there is a problem that a large time lag occurs in conversations in a VR space under the general Internet environment.
On the other hand, the recent emergence of Internet systems that enable high-speed, low-latency communication has made real-time communication possible even in VR. In this report, we describe our experience of a real-time VR outing using such a system. The patient, a male in his early 70s, had gastric cancer of primary origin, esophageal invasion, pancreatic invasion, and liver metastasis. The purpose of admission was to receive his 10th course of chemotherapy for gastric cancer. After completing his 9th course, the patient was scheduled to be temporarily discharged from the hospital to visit his daughter’s home, but his deteriorating condition made it difficult for him to do so, and he requested a real-time VR outing. Performance status (PS) (Oken et al., 1982), which is a measure of general condition determined by Eastern Cooperative Oncology Group, and indicates the degree of a patient’s limitation in daily living on a scale of 0–4, as follows (0: fully active, able to carry on all pre-disease performance without restriction. 1: Restricted in physically strenuous activity but ambulatory and able to carry out work of a light or sedentary nature, e.g., light housework, office work. 2: Ambulatory and capable of all selfcare but unable to carry out any work activities. Up and about more than 50% of waking hours. 3: Capable of only limited selfcare, confined to bed or chair more than 50% of waking hours. 4: Completely disabled. Cannot carry on any selfcare. Totally confined to bed or chair.). The PS at the time of the VR outing was two.
2 Materials and methods
2.1 Ethical considerations
This study was approved by the Ethics Committee of Ashiya Municipal Hospital (approval number: 251).
2.2 Device and high-speed communication system and VR device
AVATOUR (NTT Communications Corporation, Tokyo, Japan) as the real-time 360° video delivery platform, Insta360 ONE R (Shenzhen Arashi Vision, Inc. Shenzhen, China) as the delivery camera, and Xperia 1 II SO-51A (NTT DOCOMO, Inc., Tokyo, Japan) as the delivery smartphone were used. AVATOUR is a solution that allows users to easily share 360° space in real time. The distributor can transmit live images using a 360° camera and smartphone application via a 5G connection or Wi-Fi, and participants can watch the transmission from a variety of devices with a 360° free viewpoint. Meta Quest2 (Meta Platforms, Inc., California, United States) was used as the head-mounted display for VR viewing.
2.3 Implementation of real-time VR outing
When the patient was asked about his preferred destination, it was a home recently purchased by his daughter. The home is 550 km away from the hospital, and it takes approximately 4.5 h by Shinkansen (Japanese bullet train) and local train. The researcher asked his daughter for her cooperation and received her permission. A schedule was then arranged for the implementation date, and KN visited the daughter’s home. In the researcher team, KN was responsible for video streaming, YO was responsible for patient support, and SE was responsible for patient family support. Specifically, using AVATOUR, a 360° video was streamed in real time from the daughter’s home for approximately 30 min. The patient, the patient’s wife, son, daughter and her husband, and grandchildren participated in this streaming. The patient participated by wearing Meta Quest2 in his hospital room. The operation of Meta Quest2 was supported by YO. The patient’s wife, son, daughter, and grandchildren participated from the hospital dayroom using a laptop computer because they were under visiting restrictions due to COVID-19. The laptop was operated with support from SE. The daughter’s husband participated from the daughter’s home with KN using AVATOUR and introduced the patient to the new home. We could not use a raw picture of the inside of the patient’s home due to privacy concerns, however, as shown in mosaiced Figure 1, the patient was wearing a VR headset and talked in the VR space, while the family members participated from the dayroom and talked on a laptop screen.
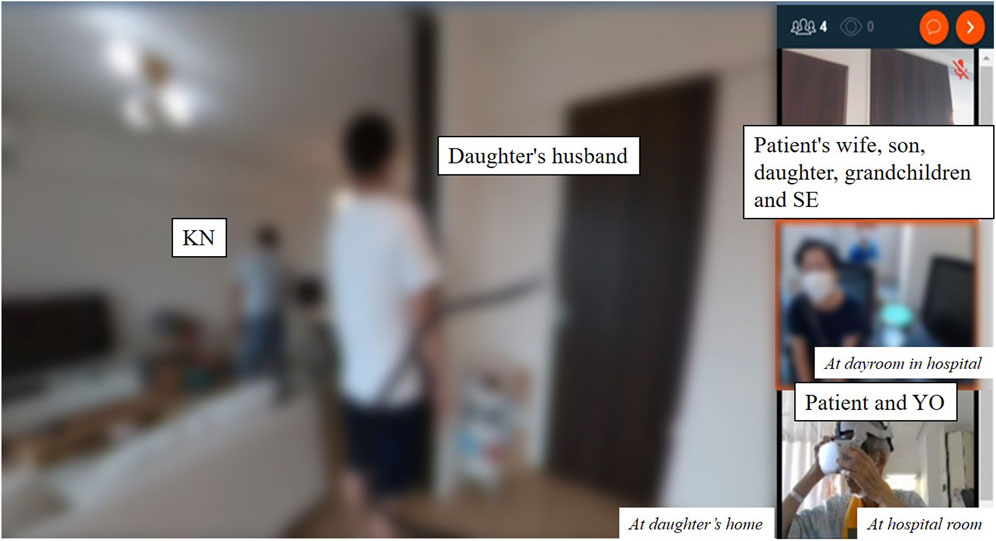
Figure 1. A scene from a real-time virtual outing viewed on a laptop. KN visited the daughter’s home. Then, using AVATOUR, a 360°video was streamed in real time from the daughter’s home. The patient participated by wearing Meta Quest2 in his hospital room. The operation of Meta Quest2 was supported by YO. The patient’s wife, son, daughter, and grandchildren participated from the hospital dayroom using a laptop computer because they were under visiting restrictions due to COVID-19. The laptop was operated with support from SE. The daughter’s husband participated from the daughter’s home with KN using AVATOUR and introduced the patient to the new home.
2.4 Evaluation
Before and after the real-time VR outing, changes in symptoms and emotions were evaluated using the Edmonton Symptom Assessment System Revised Japanese version (ESAS-r-J) (Yokomichi et al., 2015). The ESAS is a self-report symptom measurement tool that includes nine common symptom-related items of advanced cancer (pain, tiredness, drowsiness, nausea, lack of appetite, shortness of breath, depression, anxiety, and wellbeing) in an 11-point Numerical Rating Scale (NRS), ranging from 0 (symptom absent or best) to 10 (worst possible). The NRS ranging from 0 (symptom absent or best) to 10 (worst possible) for the assessments of dizziness and headache, and an 11-point NRS ranging from 0 (none) to 10 (very much) for the assessments of pleasure and satisfaction. In addition, the patient’s impressions of the VR outing were collected in an open-ended format. The primary endpoint was the change in ESAS-r-J before and after the VR outing, and the secondary endpoints were the NRS on “dizziness, headache, pleasure, and satisfaction” and the comments from the patient and his family.
3 Results
In this real-time VR outing, other than the patient, five people participated with a laptop computer and one person streamed the video from his daughter’s home. Of these, only the patient was evaluated by ESAS-r-J and NRS, and a total of three people (patient, patient’s daughter, and daughter’s husband) were asked about their impressions after the real-time VR outing. After approximately 30 min of real-time VR outings, tiredness, drowsiness, depression, and wellbeing of the patient improved and pleasure and satisfaction increased, while no side effects or worsening of symptoms were observed (Table 1). In addition, the patient said “Wow, I felt like I was really in the living room. I was curious about the construction of my daughter’s new home, but it was good to be able to see what the pictures could not.” A patient’s daughter commented, “It was nice to be able to talk with my father and show him my home. I am glad he is happy.” The daughter’s husband said, “My father-in-law has been really good to me, and I’m sorry he will not be able to see my house for real, but I’m glad I was able to show him the inside of my house. With a cell phone camera, I have to check the image while I talk to him, but with the 360-degree camera, it is easy to just hold it and it delivers. I could concentrate on my conversation with him.” The researcher next to the patient observed that the patient was talking more animatedly and lively than usual, and he was sitting in a chair for 30 min during the real-time VR travel, even though he is usually supine.
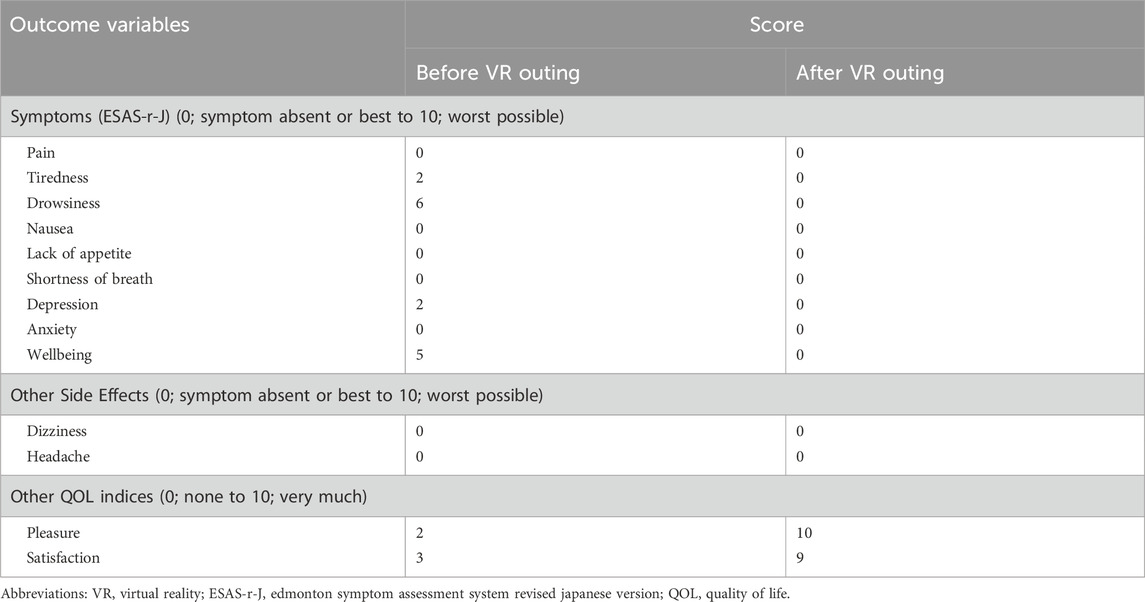
Table 1. Symptoms, other side effects, quality of life indices before and after real-time VR outing.
4 Discussion
In this case, the patient was able to fulfill his wish to visit his daughter’s new home, even pseudoactively, and smoothly enjoy a real-time conversation in the VR space without time lag and any side effects. As a result, the patient’s multiple physical and mental symptoms improved, and pleasure and satisfaction increased. In addition, the patient himself commented on the “realistic” effect of the VR space. The improvement in tiredness, drowsiness, depression, and wellbeing, which were observed in this case, were also significantly improved in our previous study, and the results were consistent with those of previous studies, including the absence of side effects (Niki et al., 2019). However, as far as we could find, we could not find any studies that directly compared the effects of real-time VR outings and non-real-time VR outings, so it would be desirable to examine the existence of an add-on effect of real-time outings from a scientific perspective in the future.
Currently, some travel agencies offer real-time virtual tour services, but most of them view2D images through PCs or smartphones. To realize real-time virtual travel in a VR space, fast and stable Internet connections and high-performance devices are required, therefore, the technology has not yet been widely adopted by the public. To the best of our knowledge, this is the first report in which hospitalized cancer patients went on a real-time virtual outing in a VR space.
In general, virtual outings have several advantages, such as saving money on transportation, lodging, and other expenses required for actual travel, saving time and effort for travel, and allowing patients to enjoy simulated travel in a safe environment without having to leave their hospital room or home. In addition to these advantages, real-time VR outings have the powerful advantage of allowing users to simultaneously enjoy conversations in a VR space. However, real-time VR outings have several disadvantages, such as the need for a high-speed communication system and high-performance devices, the inability to feel touch and smell, and the risk of eye fatigue and sickness if used for long periods of time. However, recent advances in technology are showing signs of overcoming these disadvantages. For example, the platform used in this case, which enables high-speed communication, is one such example, and devices that reproduce the senses of touch and smell are also being developed (Kaul and Rohs, 2017; Kon et al., 2017; Peiris et al., 2017; Wang et al., 2019; Tseng et al., 2020). Although the health concerns of prolonged use are a major issue regarding medical applications, a review compiled by D’Cunha et al. (2019) suggests that the VR experience should be no longer than 30 min, and our previous reports on patients admitted to palliative care units (Niki et al., 2019) and Ferguson et al. (2020) in dementia patients confirmed that viewing within 30 min did not cause any serious side effects. Therefore, it appears that health hazards can be minimized by limiting viewing time and avoiding use for those who are naturally susceptible to motion sickness. If the metaverse, which has been attracting attention recently, becomes more widespread, real-time VR outings may become common in the future, and it is expected that the cost issue will be overcome.
The sample size for this study is too small to conclude on the feasibility and effectiveness of real-time VR outing. Therefore, although verification with additional cases, or scientific validation by comparison with 2D real-time virtual outings are desired, this case study suggests that real-time VR outings can be one approach to helping hospitalized patients fulfill their wishes to go out.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by the Ethics Committee of Ashiya Municipal Hospital. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
KN: Conceptualization, Funding acquisition, Investigation, Methodology, Project administration, Writing–original draft. SE: Investigation, Writing–review and editing. YO: Conceptualization, Investigation, Supervision, Writing–review and editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
We would like to thank the patient and his family for their cooperation in this study. We also appreciate Daikin Industries, Ltd. for loaning us the AVATOUR.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Austin, P. D., Siddall, P. J., and Lovell, M. R. (2022). Feasibility and acceptability of virtual reality for cancer pain in people receiving palliative care: a randomised cross-over study. Support Care Cancer 30, 3995–4005. doi:10.1007/s00520-022-06824-x
D'Cunha, N. M., Nguyen, D., Naumovski, N., McKune, A. J., Kellett, J., Georgousopoulou, E. N., et al. (2019). A mini-review of virtual reality-based interventions to promote well-being for people living with dementia and mild cognitive impairment. Gerontology 65, 430–440. doi:10.1159/000500040
Ferguson, C., Shade, M. Y., Blaskewicz Boron, J., Lyden, E., and Manley, N. A. (2020). Virtual reality for therapeutic recreation in dementia hospice care: a feasibility study. Am. J. Hosp. Palliat. Care 37, 809–815. doi:10.1177/1049909120901525
Kaul, O. B., and Rohs, M. (2017). “HapticHead: a spherical vibrotactile grid around the head for 3D guidance in virtual and augmented reality,” in In proceedings of the 2017 CHI conference on human factors in computing systems (New York, USA: CHI '17), 3729–3740. doi:10.1145/3025453.3025684
Kon, Y., Nakamura, T., and Kajimoto, H. (2017). “HangerOVER: HMD-embedded haptics display with hanger reflex,” in In proceedings of the ACM SIGGRAPH 2017 emerging Technologies (New York, USA: SIGGRAPH '17), 1–2. Article 11. doi:10.1145/3084822.3084842
Lee, C. M., Cadigan, J. M., and Rhew, I. C. (2020). Increases in loneliness among young adults during the COVID-19 pandemic and association with increases in mental health problems. J. Adolesc. Health 67, 714–717. doi:10.1016/j.jadohealth.2020.08.009
Murayama, H., Okubo, R., and Tabuchi, T. (2021). Increase in social isolation during the COVID-19 pandemic and its association with mental health: findings from the JACSIS 2020 study. Int. J. Environ. Res. Public Health 18 (16), 8238. doi:10.3390/ijerph18168238
Niki, K., Okamoto, Y., Maeda, I., Mori, I., Ishii, R., Matsuda, Y., et al. (2019). A novel palliative care approach using virtual reality for improving various symptoms of terminal cancer patients: a preliminary prospective, multicenter study. J. Palliat. Med. 22, 702–707. doi:10.1089/jpm.2018.0527
Oken, M. M., Creech, R. H., Tormey, D. C., Horton, J., Davis, T. E., McFadden, E. T., et al. (1982). Toxicity and response criteria of the eastern cooperative Oncology Group. Am. J. Clin. Oncol. 5 (6), 649–656. doi:10.1097/00000421-198212000-00014
Peiris, R. L., Peng, W., Chen, Z., Chan, L., and Minamizawa, K. (2017). “ThermoVR: exploring integrated thermal haptic feedback with head mounted displays,” in In proceedings of the 2017 CHI conference on human factors in computing systems (New York, USA: CHI '17), 5452–5456. doi:10.1145/3025453.3025824
Tseng, W.-J., Lee, Y.-C., Peiris, R. L., and Chan, L. (2020). “A skin-stroke display on the eye-ring through head-mounted displays,” in In proceedings of the 2020 CHI conference on human factors in computing systems (New York, USA: CHI '20), 1–13. doi:10.1145/3313831.3376700
Van Tilburg, T. G., Steinmetz, S., Stolte, E., van der Roest, H., and de Vries, D. H. (2021). Loneliness and mental health during the COVID-19 pandemic: a study among Dutch older adults. J. Gerontol. B Psychol. Sci. Soc. Sci. 76, e249–e255. doi:10.1093/geronb/gbaa111
Wang, C., Huang, D.-Y., Hsu, S.-W., Hou, C.-E., Chiu, Y.-L., Chang, R.-C., et al. (2019). “Masque: exploring lateral skin stretch feedback on the face with head-mounted displays,” in In proceedings of the 32nd annual ACM symposium on user interface software and technology (New York, USA: UIST '19), 439–451. doi:10.1145/3332165.3347898
Keywords: terminal cancer patient, real-time virtual outing, digital therapeutics, virtual reality-CSCI-ISED, palliative care
Citation: Niki K, Egashira S and Okamoto Y (2024) A real-time virtual outing using virtual reality for a hospitalized terminal cancer patient who has difficulty going out: a case report. Front. Virtual Real. 5:1269707. doi: 10.3389/frvir.2024.1269707
Received: 30 July 2023; Accepted: 25 April 2024;
Published: 09 May 2024.
Edited by:
Albert Rizzo, University of Southern California, United StatesReviewed by:
Ryan Kelly, The University of Melbourne, AustraliaFilipa Ferreira-Brito, Laboratório de Sistemas Informáticos de Grande Escala (LaSIGE), Portugal
Copyright © 2024 Niki, Egashira and Okamoto. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Kazuyuki Niki, a2F6dXl1a2kubmlraUBnbWFpbC5jb20=
 Kazuyuki Niki
Kazuyuki Niki Satomi Egashira3
Satomi Egashira3 Yoshiaki Okamoto
Yoshiaki Okamoto