
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Virtual Real. , 14 November 2023
Sec. Virtual Reality in Medicine
Volume 4 - 2023 | https://doi.org/10.3389/frvir.2023.1294482
Objectives: Our study is a follow-up of a previous research study that was carried out in physiotherapy. The present study aims to evaluate the effectiveness of virtual reality (VR) as a tool to support emotional management during the acute phase of breast cancer treatment (chemotherapy session).
Materials and methods: A quasi-experimental protocol was implemented in an oncology department with 120 patients randomly assigned to one of four conditions that were being compared. During the first 10 minutes of a chemotherapy session, patients could either be exposed to a participatory immersion in a natural environment; or be placed in a contemplative immersion condition in the same environment; or listen to classical music; or receive no distraction. The involvement of the patients in the virtual environment and the relevance of the immersive modalities were measured through the evaluation of sense of presence. Particular interest was given to the evaluation of anxiety level and the emotional state of the patients.
Results: VR during chemotherapy reduces anxiety and calms emotional tension. The multi-sensory nature of this emotional regulation support tool was more effective than music in inducing positive emotion, and this benefit was the most salient when immersion was offered in an interactive format.
Conclusion: The relevance of providing support through VR in oncology is confirmed in this study. This tool can compensate for the fluctuating availability of caregivers by offering patients the possibility of shaping their own relaxing worlds and could help preserve the patient-caregiver relationship.
Virtual reality (VR) has been used during oncological care as a distractive strategy, capable of regulating the emotional response of patients undergoing stressful treatments by diverting their attention towards more pleasant stimuli (Chirico et al., 2019; Rutkowski, et al., 2021; Buche et al., 2022). For example, a study carried out during post-mastectomy scar massage sessions showed the relevance of using virtual reality by comparing two immersive modalities (i.e., participative vs contemplative) to a situation of listening to classical music or to a traditional treatment situation in the presence of the practitioner (Buche et al., 2021). The proposed immersions were distinguished according to the degree of attention solicited: either in participative immersion through an interaction with the virtual environment actively involving the patients, or in so-called contemplative immersion which passively redirects the patients’ attention (Buche et al., 2022). In this clinical rehabilitation context, distraction through VR was associated with better emotional comfort for the patients, which was also reflected by an underestimation of the duration of the treatment session. However, listening to classical music and the proximity of the practitioner as well as his/her interactions with the patient provided a context that was equally conducive to anxiety reduction and emotional regulation.
In line with these results, the present study aims to explore the benefits of VR in a more critical phase of care (i.e., chemotherapy) where the management of emotions proves to be crucial for patients, a context in which the nursing staff lacks, through no fault of their own, the availability to accompany them (Lerebours et al., 2015). While promising effects of VR have been observed on patients’ emotional state, particularly during physical therapy (Buche et al., 2021), the management of emotional states during other critical phases such as chemotherapy is probably more delicate. It has been reported that the psychological distress, which has been observed in one-third of breast cancer patients, tends to worsen during chemotherapy (Zielińska-Więczkowska and Betłakowski, 2010; Tsaras et al., 2018). Because of the frequency of chemotherapy, patients regularly go to the oncology department where the medical context is often stressful and time-consuming (more than 3 hours in outpatient hospitalization, including more than 50 minutes spent waiting) (Lerebours et al., 2015). Furthermore, nurses in oncology departments do not have the opportunity to develop a real empathic care relationship likely to optimize emotional management (Hjeij et al., 2022) and lack time, making them less likely to meet patients’ needs for support despite their efforts to do so (Coppée, 2022). However, numerous studies have shown that the relational dimension is an essential variable in guaranteeing patient satisfaction during treatment (Street et al., 2009) 20, Prip et al., 2018), as the richness of this relationship plays a primordial role in compliance with treatment, particularly during chemotherapy (Prip et al., 2018). Given this reality in the field, new technological tools such as VR, especially when offered by the nursing staff, could make up for their lack of availability.
According to the model of Buche et al. (2022), immersive VR is a powerful distractive technology that can visually and aurally isolate patients from the medical context to immerse themselves in a three-dimensional environment with positive stimuli, generated by a computer in real time (Chirico et al., 2016; 2019). Multisensory integration induces a sense of presence in the virtual Universe, producing a subjective impression of being in a different place than physical reality (Baus and Bouchard, 2014). The technological properties of VR have the advantage of offering several degrees of interaction, allowing patients to be active or passive within the virtual environment (Ahmadpour et al., 2020; Buche et al., 2021). The level of engagement and interactivity appear to be closely related to the sense of presence and increased attention allocated to distraction, reinforcing the positive effects of VR (Birnie et al., 2018; Indovina et al., 2018).
Furthermore, according to the theoretical conception of Frederickson. 2001; i.e., the broaden-and-build theory), promoting positive emotions could strengthen patients’ ability to overcome the ordeal of cancer. VR would thus offer many advantages in promoting emotional regulation (Macey et al., 2022). Emotionally supportive virtual environments are thought to lead to a sense of intense presence in a safe place, which in turn leads to more intensely felt positive emotions (Riva et al., 2007; Buche et al., 2021). Among the preferences declared by the patients, virtual environments including natural elements (e.g., mountains, forests, beaches, sounds of nature, etc.) are particularly popular for escaping from the stressful situation of oncology care (Michel et al., 2019). This spontaneous preference is even more interesting as natural environments intended to support emotional regulation have been found to have a greater restorative potential than other environments. The restorative effects of natural environments include increased relaxation, decreased anxiety and improved attention (Gamble et al., 2014; Valtchanov and Ellard, 2015; Navarro-Haro et al., 2017; Wilson and Scorsone, 2021).
Regarding the available scientific literature, the benefits of VR were first evaluated in 1999 with promising observations showing a considerable decrease in patients’ anxiety level. (Schneider and Workman, 1999; Oyama et al., 2000). According to the model of Schneider et al. (2011; the stimulation-cognitive accumulation model), VR appears to reduce patients’ attention to the time spent in treatment, leading to increased emotional comfort for patients with the subjective impression that the chemotherapy treatment passes more quickly when they are immersed in a virtual environment (see also Buche et al., 2021). Recent studies have confirmed the relevance of VR-delivered coaching to prevent and manage patient anxiety during chemotherapy administration and the symptoms of distress generated (e.g., nausea and vomiting) (Sakhri and Boulhart, 2021; Wilson and Scorsone, 2021; Wong et al., 2021; Ando et al., 2022; O'Gara et al., 2022). VR therapy administered over several sessions have been shown to consistently reduce anxiety levels and pain catastrophizing as well as improve feelings of self-efficacy (Sharifpour et al., 2020; Birkhoff et al., 2021). In addition to their emotional regulation benefits, current virtual devices are said to be innovative and particularly effective in distracting patients undergoing chemotherapy, breaking the monotony of treatment and providing additional support during sessions (Janssen et al., 2022). The implementation of such a procedure/device would increase patient engagement in their care pathway and the individualization of their treatment (Vincent et al., 2021).
Given the interest in the use of VR, it seems necessary to compare the contributions of VR to a more conventional emotional regulation technique in order to determine the relevance of using immersive VR during chemotherapy. Although listening to pleasant music may reduce anxiety levels by 30%–75% (Whitehead-Pleaux et al., 2007), immersive and interactive VR is more effective than music in reducing anxiety during chemotherapy (Chirico et al., 2019). However, the impact of patients’ level of involvement in the virtual world (i.e., Contemplative VR vs Participatory VR) has not yet been compared to listening to music during a chemotherapy session. The optimal conditions for the use of VR in chemotherapy therefore remain to be determined in order to present interfaces which are adapted to cancer patient care. Thus, the second objective of our study is to compare the effects of the two immersive modalities to a more conventional distractive technique, musical relaxation (i.e., Participatory VR vs Contemplative VR vs Music) in a health context where the nursing staff is not often available to patients. Like Chirico et al. (2019), we set up a protocol to make this comparison in the acute phase of cancer care, during a chemotherapy session. To identify the benefits of VR and music, a comparison was made with a control condition in which patients receive standard care (i.e., without distraction).
The benefits of VR distraction may be partly due to its multimodal and highly interactive nature which allows individuals to engage in the virtual world (Chirico et al., 2019; Buche et al., 2022). Modifying the appearance and adjusting the content of the virtual environment should increase the salience of sense of presence by keeping the user’s attention on the virtual experience (Bouvier, 2009; Maneuvrier, 2020). If patients’ presence and engagement in the immersive experience are reinforced under participatory VR, then we should observe a better quality of immersion in this more interactive modality, thus leading to a more marked benefit in terms of patients’ emotional state (Buche et al., 2021). As such, participatory immersion (involving the use of joysticks to perform actions in the virtual environment) should provide better support for emotional state regulation than a contemplative immersion during chemotherapy. According to Chirico et al. (2019), VR should be a more effective tool than music as the latter requires only passive attentional engagement from patients. VR could also provide effective support to patients by offering them the opportunity to be actors of their own wellbeing and preserve them from a negative perception of the patient/caregiver relationship.
The sample consisted of 120 breast cancer patients who were randomized to the different experimental conditions. These patients ranged in age from 29 to 87 years (mean age = 55.40 ± 12.09 years). The participants were recruited from the chemotherapy department at the Clémentville clinic in Montpellier, which specializes in breast cancer treatment in conjunction with the MIS (Montpellier Institut du Sein Montpellier Breast Institute). The inclusion criteria were: having breast cancer, being treated with chemotherapy, and being able to read and write in French. Patients with glasses were included in the study, as the VR headset had an adapter for this purpose. To prevent the risk of VR-related discomfort, patients with vestibular disorders or a reported history of motion sickness were excluded. The presence of seizure disorders, alcohol or drug addictions were also clinical exclusion factors for the study. All patients agreed to participate in this study by signing an informed consent form specifying the general context and the different stages of the research. Eighty-nine participants had corrected vision and four patients wore a hair loss cooling helmet during the immersion, which had no impact on the realization of the experiment.
This study is a continuation of an initial study (Buche et al., 2021) carried out during the physiotherapy rehabilitation phase with breast cancer patients who had undergone surgery. This first study aimed to compare the effectiveness of various distractive interventions (i.e., Music vs VR) as well as the impact of virtual stimuli of different natures (i.e., Participatory VR vs Contemplative VR). As an extension of that study, we will compare these two immersive modalities to music during a stage of treatment where health professionals are not systematically at the patient’s side during the entire course of care (i.e., chemotherapy).
According to the theory of Ulrich et al. (1991; i.e., psychophysiological stress recovery theory), a natural environment should promote anxiety reduction. Greener Gamer’s Nature Treks VR relaxation application (Carline and Carline, 2017) was reused in the present study. The application includes nine virtual relaxation environments (e.g., safari, beach, spring forest, winter forest, underwater.) to which relaxing sound stimuli were associated (i.e., nature sounds and relaxing music). The strength of the Nature Treks VR application lies in its two immersive modalities: one contemplative, the other participative. In the participatory version, in addition to contemplative exploration, patients have the possibility to shape their own environment (e.g., control the weather, plant trees or flowers, feed animals.).
For the music condition, “spring” from Vivaldi’s Four Seasons was again used, this music having been selected for its proven effectiveness in evoking positive emotions (Krumhansl, 1997).
An individual booklet was made up for each patient to facilitate the presentation of the questionnaires. As in our previous study (Buche et al., 2021), the booklets began with an introduction to the study, followed by the consent letter and a demographic questionnaire. They then included all the self-report questionnaires used at different stages of our study, presented to each patient according to the distraction condition to which they had been randomly assigned.
The measurement tools used in our previous study (Buche et al., 2021), were used in the same way in chemotherapy to assess patients’ emotional state, but also their anxiety level and to monitor any side effects that could be caused by the virtual device (e.g., nausea, headaches, dizziness, etc.). Concerning sense of presence, only two items were retained to measure spatial presence and patients’ engagement in the immersive task. All questionnaires that were used are listed in Table 1 below.
In addition, the Immersion Propensity Questionnaire (IPQ) from the Cyberpsychology Laboratory at UQO (2002), was added to the research protocol in order to measure the propensity to cut oneself off from external distractions during the performance of various daily activities. In other words, this measure provides an index of patients’ propensity to immerse themselves in the proposed virtual world. The IPQ consisted of 18 questions with a seven-point scale (1: never to 7: often) as a response modality, and provided a total score and four factors: focus, involvement, emotion and play.
In order to minimize the risk of eye-motor disturbances and other side effects (e.g., nausea) that could be related to a lower quality technological device (Witmer Singer, 1998; Chirico et al., 2019), the Oculus Quest 2® headset was chosen to conduct this research in chemotherapy. Even more sophisticated than the one used in the previous study (Buche et al., 2021; Oculus GO®), its main advantage was to optimize the immersive quality, and thus to favor the study of VR contributions to ensure full patient satisfaction.
For the music condition, we used Beats by DR. DRE® SOLO PRO Hi-Fi headphones, a supra-aural model that includes two speakers in each earpiece. The headphones were connected wirelessly via Bluetooth to a SAMSUNG S21® smartphone.
The procedure from the study by Buche et al. (2021) was replicated and adapted to another stage of breast cancer management: chemotherapy (see Figure 1). To assess the benefits of the different distractions offered, patients were randomly assigned to one of four distraction conditions during a chemotherapy session (i.e., Participatory VR, Contemplative VR, Music and Control). Thus, the effects of music were compared with those of VR, and the immersion modalities (i.e., one purely contemplative and the other participatory) were also compared with each other. The sessions were all conducted in the chemotherapy department at the Clémentville Clinic in Montpellier. Patients were solicited on the recommendation of the nursing staff of the oncology department, and were informed beforehand about the possibility of participating in this study. They were given 1 week to consider their participation. Prior to participation, patients who volunteered were asked to sign the informed consent form. They were then asked to complete the demographic questionnaire. Once they were individually seated in their treatment room, patients were systematically informed about the proposed support (i.e., Participatory VR vs Contemplative VR vs Music vs Control) they would receive during chemotherapy care before completing the first set of questionnaires (i.e., SAM, STAI-YA). Data collection was conducted according to ethical guidelines to ensure patient anonymity. Patients were exposed to only one type of distraction during chemotherapy care (i.e., Participatory VR vs Contemplative VR vs Music vs control). Each individual session lasted approximately 25–45 min.
Patients were seated in a reclining treatment chair, in an individual room or cubicle. Nurses provided standard care and administered intravenous chemotherapy. On average, each chemotherapy treatment lasted between 45 and 90 min. The distraction session (i.e., Participatory VR, Contemplative VR, and Music) always took place following IV placement, after the patient had received instructions for the different distraction conditions, and had completed the first set of questionnaires.
For chemotherapy treatments with VR, the experimenter began by detailing the different environments available that each patient could select. The experimenter then demonstrated how to use the VR equipment according to the assigned distraction condition: participatory and contemplative immersions consisted of walking through the selected Universe without requiring physical movement. Exploration was performed using two joysticks that patients pointed in the desired direction. In addition to exploration, participatory immersion allowed patients to control weather and space-time (i.e., day vs night), plant trees or flowers to shape their own environment, and feed animals. The experimenter helped patients put on the VR headset and program the session to the desired environment for direct access to relaxation. During participatory immersion, the experimenter was able to simultaneously visualize the patients’ actions via a smartphone mirror screen application, so this monitoring ensured that they were performing the immersive task (i.e., shaping their natural relaxation environment through certain actions). During the contemplative immersion, the experimenter also monitored how the patients discovered their environment, knowing that all they could do was direct their observation of the natural 360° environment. As noted in a previous study (Buche et al., 2021), to prevent the risk of cybersickness associated with long-term immersion, patients were invited to use the equipment for 10 minutes only. This duration was considered beneficial for maintaining patients’ interest all along the immersive experience, while minimizing the appearance of cybersickness. At the end of the immersion, all participants were asked to complete the final set of questionnaires (i.e., SAM, STAI-YA, ITC-SOPI) and the control questionnaires (i.e., STAI-YB, QC, IPQ).
For the chemotherapy treatment in the music-listening condition, the experimenter prepared the music using a smartphone before helping patients put on the headphones. Patients listened to the music for 10 minutes, which was the same amount of distraction time as for the VR session. Once the music listening time was over, each patient was asked to complete the final set of questionnaires (i.e., SAM, STAI-YA).
For chemotherapy treatment in the control condition (i.e., without distraction), patients completed the first set of questionnaires (i.e., SAM, STAI-YA) at the beginning of their session and the last set of questionnaires (i.e., SAM, STAI-YA) at the end of their session.
Of the 122 patients solicited, 120 participated in an experimental condition (i.e., Participatory VR vs Contemplative VR vs Music vs Control), in which 30 patients randomly assigned to each of the four conditions were compared to each other. Two patients did not continue the study, one due to a feeling of fatigue and weakness related to the chemotherapy components: the other due to difficulties after the first VR session (i.e., nausea). We therefore analyzed 98.36% of the baseline population. Seven patients declined to participate for various reasons such as fatigue or lack of interest in the device or the study. Ten patients removed the VR headset before the 10 minutes time limit because the environment lacked action or because they felt out of control. Of the 90 patients who experienced the virtual device, only seven had used VR before participating in the experiment. The socio-demographic characteristics of the patients are presented in Table 2.
Statistical analyses were performed using JASP software. On the emotional level, the following measures were taken into consideration: the emotional state (i.e., valence, intensity), and the anxiety level of the patients. Regarding the quality of immersion, the state of spatial presence and the level of engagement in the immersive task were analyzed. To test our hypotheses, ANOVAs were computed as in similar studies (Chirico et al., 2019). As with all work designed to evaluate the contribution of VR in oncology, independent Student's t-tests were performed to determine the presence of differences between the modalities. Two so-called control questionnaires (i.e., trait anxiety, immersion propensity) were compared to norms with a simple Student’s t-test. The significance level of 0.05 was adopted for all the statistical analyses carried out.
To measure patients’ emotional state before and after exposure to one of the four distraction conditions, mean valence and arousal scores (see Table 3) collected using the SAM scale were analyzed. Two repeated-measures ANOVA factorial designs were calculated: one on valence scores, the other on arousal scores, with time (before vs after) as a within-subjects factor, and distraction conditions (participatory VR vs contemplative VR vs Music vs Control) as a between-subjects factor.
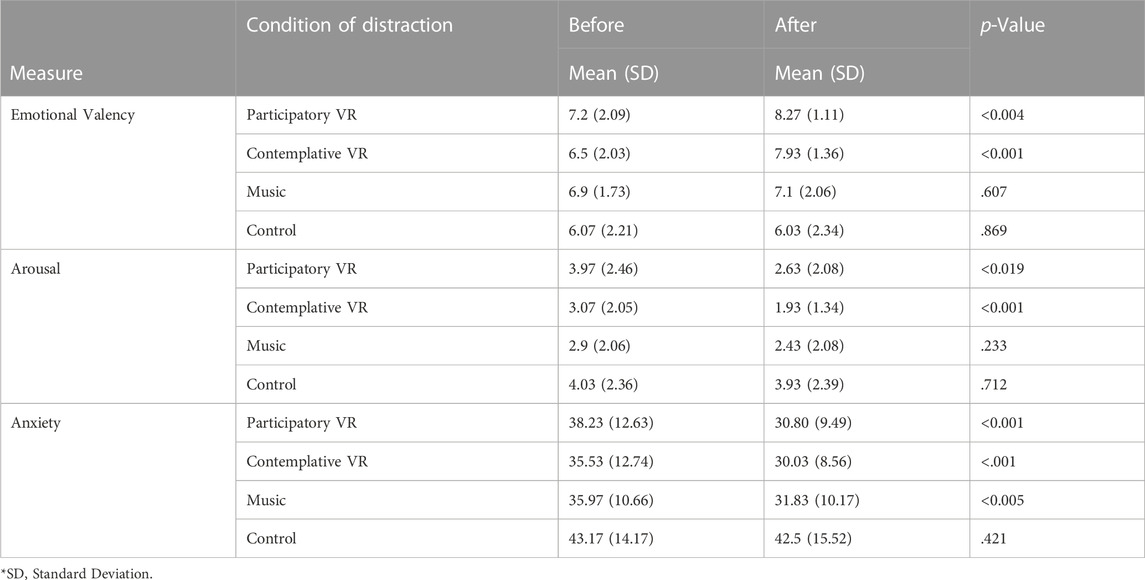
TABLE 3. Mean and standard deviation of emotional state and anxiety for each distraction condition as a function of measurement time, and significant differences by paired comparison.
Regarding emotional valence, the ANOVA revealed a main effect of measurement time, F (1, 116) = 17.727, p < .001, η2p = 0.133. Emotional states were more positive (i.e., patients were in a more pleasant mood) after the experiment (M = 7.33, SD = 1) than before (M = 6.67, SD = 0.49). Analysis also revealed a main effect of the distraction condition, F (3, 116) = 5.136, p < .002, η2p = 0.117: emotional valence varied significantly by condition. Emotional state was more positive in patients in the distraction conditions including participatory VR (M = 7.73, SD = 0.75), contemplative VR (M = 7.22, SD = 1.01), or music (M = 7.1, SD = 0.14), compared with patients placed in the control condition (M = 6.05, SD = 0.02).
A significant interaction between measurement timing and distraction condition was also observed, F (3, 116) = 4.838, p < .003, η2p = 0.111. Distraction type did influence measurement timing for two conditions. The Student’s t-test indicated the presence of a significant difference between before and after each immersive modality. Patients who experienced participatory VR reported a more pleasant feeling after the virtual experience (M = 8.27, SD = 1.11) than before (M = 7.2, SD = 2.09), t (29) = −3.087, p < 0.004, Cohen’s d = 0.56, with a moderate effect size. Similarly, patients who experienced contemplative VR reported a more pleasant feeling after the virtual experience (M = 7.93, SD = 1.36) than before (M = 6.5, SD = 2.03), t (29) = −4.687, p < 0.001, with a strong Cohen’s d = 0.86. In contrast, there was no significant difference between before (M = 6.9, SD = 1.73) and after (M = 7.1, SD = 2.06) listening to music, t (29) = −0.520, p = 0.607, nor between before (M = 6.07, SD = 2.21) and after (M = 6.03, SD = 2.34) chemotherapy session without distraction, t (29) = −0.166, p = 0.869. Thus, the induction of a more pleasant emotional state after the experiment is obtained only in patients who benefited from VR.
Regarding the measure of arousal level, the ANOVA reveals a main effect of measurement timing F (1, 116) = 15.385, p < .001, η2p = .0.117 with lower emotional intensity after the experiment (M = 2.73, SD = 0.85) than before (M = 3.49, SD = 0.59). Because the SAM scale associates the highest value with the adjective “excited” and the lowest with the adjective “calm,” these results seem to reflect the appearance of a calming effect.
The analysis also shows a main effect of distraction type F (3, 116) = 4.024, p < .009, η2p = 0.094. The level of arousal was significantly lower in patients who received contemplative immersion (M = 2.5, SD = 0.8) or listened to music (M = 2.67, SD = 0.33) than in patients who received participatory immersion (M = 3.3, SD = 0.94) and/or no distraction (M = 3.98, SD = 0.07).
Regarding the interaction between measurement time and distraction condition, F (3, 116) = 2.207, p = 0.091, η2p = 0.013, it is close to the significance level. The Student’s t-test demonstrates the presence of a significant difference between before and after for both distraction conditions under VR. Patients who experienced participatory VR felt calmer after the virtual experience (M = 2.63, SD = 2.08) than before (M = 3.97, SD = 2.46), t (29) = 2.494, p < 0.019, Cohen’s d = 0.46, with a moderate effect size. Patients who experienced contemplative VR also felt calmer after the virtual experience (M = 1.93, SD = 1.34) than before (M = 3.07, SD = 2.05), t (29) = 3.704, p < 0.001, Cohen’s d = 0.68, with a moderate effect size. No significant difference was observed between before (M = 2.9, SD = 2.06) and after (M = 2.43, SD = 2.08) in the music condition t (29) = 1.219, p = 0.233, nor between before (M = 4.03, SD = 2.36) and after (M = 3.93, SD = 2.39) in the control condition, t (29) = 0.372, p = 0.712. Thus, patients felt calmer only after the VR immersion, whether participatory or contemplative in nature.
Surprisingly, no significant difference was observed between participatory VR (M = 2.63, SD = 2.08) and contemplative VR (M = 1.93, SD = 1.34), t (58) = 1.553, p = 0.126 on patient-reported arousal state, nor between participatory VR (M = 2.63, SD = 2.08) and music (M = 2.43, SD = 2.08), t (58) = −0.373, p = 0.711; nor even between contemplative VR (M = 1.93, SD = 1.34) and music (M = 2.43, SD = 2.08), t (58) = 1.108, p = 0.273.
To assess state anxiety before and after exposure to one of the four distraction conditions (see Table 3), one repeated-measures ANOVA factorial designs was calculated with measurement time (i.e., before vs after) as a within-subjects factor and distraction condition (i.e., Participatory VR vs Contemplative VR vs Music vs Control) as a between-subjects factor.
A main effect of timing was found F (1, 116) = 38.990, p < .001, η2p = 0.252. Patients’ anxiety level was lower after the experiment (M = 33.79, SD = 5.85) than before (M = 38.23, SD = 3.5). A main effect of distraction type was also found F (3, 116) = 4.978, p < .003, η2p = 0.114: anxiety level varied significantly by distraction type. Anxiety was higher in patients in the no distraction condition (M = 42.83, SD = 0.47) than in patients in distraction conditions, whether participatory VR (M = 34.51, SD = 5.25), contemplative VR (M = 32.78, SD = 3.89), or music (M = 33.9, SD = 5.25).
A significant interaction between measurement timing and distraction condition was again reported, F (3, 116) = 4.036, p < .009, η2p = 0.095. The type of distraction had an effect on the timing of the measurement. According to Student’s t-test, there was a significant difference between before and after each distraction. Patients who experienced participatory VR were less anxious after the virtual experience (M = 30.8, SD = 9.49) than before (M = 38.23, SD = 12.63), t (29) = 4.206, p < 0.001, Cohen’s d = 0.77, moderate effect size. Patients who experienced contemplative VR were less anxious after the virtual experience (M = 30.03, SD = 8.56) than before (M = 35.53, SD = 12.74), t (29) = 3.561, p = 0.001, Cohen’s d = 0.65, moderate effect size. Patients who experienced music were less anxious after listening to music (M = 31.83, SD = 10.17) than before (M = 35.97, SD = 10.66), t (29) = 3.007, p < 0.005, Cohen’s d = 0.55, moderate effect size.
In contrast, there was no difference between before and after for patients in the no distraction condition: patients who received standard chemotherapy had the same level of anxiety after (M = 43.17, SD = 14.17) as before chemotherapy (M = 42.5, SD = 15.52), t (29) = 0.816, p = 0.421. A reduction in anxiety was observed in patients regardless of the type of distraction offered.
For informational purposes, we were interested in whether trait anxiety could influence patients’ situational anxiety. The data were coded and transformed according to the guidelines of the STAI-YB standard. The French recommendations of the S.T.A.I. form Y.B. (Spielberger, 1983), consider that in women, the average on the trait anxiety scale is 45.09. Above this average, they are considered anxious. We therefore calculated a t-test to compare the average trait anxiety of breast cancer patients to the norm for adult women.
The differences between the patients’ mean trait anxiety and the norm were significant t (119) = −4.511, p < .001, Cohen’s d = - 0.412, but the effect size was small. Since t cal < 0, the patients did not exhibit an anxious nature. Patients’ trait anxiety was significantly lower (M = 40.74, SD = 10.56) than the norm for women (M = 45.09, SD = 9.92). The anxiety that these patients generally experience did not influence the anxiety associated with chemotherapy sessions.
To examine the quality of the patients’ sense of presence, we considered the average spatial presence score and the engagement score (see Table 4). We therefore performed two ANOVAs (one per variable considered) according to the immersive modality (i.e., Participatory VR vs Contemplative VR).
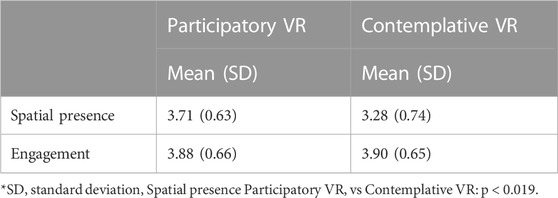
TABLE 4. Mean and standard deviation of spatial presence and engagement according to immersive modalities.
Analysis of variance reports an effect of immersive modality on spatial presence, F (1,58) = 5.841, p < .019, η2p = 0.091, cohen’s d = 0.62, with a moderate effect size. Patients’ spatial presence under participatory immersion was significantly higher (M = 3.71, SD = 0.63) than under contemplative immersion (M = 3.28, SD = 0.74). Similar to our first study (Buche et al., 2021), participatory immersion in a natural environment induced a more intense sense of presence in patients, while patient engagement in the virtual environment was identical during both immersions F (1,58) = 0.025, p = 0.876, η2p = 0.0. Thus, patients interacting with the natural elements of the environment did not feel more engaged in the virtual environment (M = 3.88, SD = 0.66) than those who navigated the environment by observing nature alone (M = 3.9, SD = 0.65).
To measure the negative effects that may have been generated by the device (see Figure 2), we calculated three ANOVAs (one per considered variable, i.e., oculomotor, nausea, total) according to the immersive modality (i.e., Participatory VR vs Contemplative VR).
The analysis of variance did not identify a main effect of distraction type on the intensity of total cybernetics F (1, 58) = 1.396, p = 0.242, η2p = 0.023. In this study, participatory VR (M = 2.73, SD = 3.96) appears to result in a lower mean cybersickness score than contemplative VR (M = 4.3, SD = 6.09), but the observed difference between these two conditions is not significant. The same is true for the oculomotor subfactor, F (1, 58) = 0.923, p = 0.341, η2p = 0.016 and the nausea subfactor F (1, 58) = 1.558, p = 0.217, η2p = 0.026 (see Figure 2). With mean scores below five in both immersive modalities, it appears that the negative symptoms generated by the VR device are negligible.
The Immersion Propensity Questionnaire examines whether participants feel they have left their physical environment and are “present” in the virtual environment. For the sake of precision, we wanted to determine to what extent our sample of patients would be predisposed to immerse themselves in a virtual environment. To do so, we calculated four Student's t-tests, to compare the means of the immersion propensity subscales (focus, involvement, emotion, play and the total mean) to the norms provided by the Cyberpsychology Laboratory at UQO (2002) (see Table 5).
The patients’ ability to focus and ignore external distractions was not significantly different from the norm t (59) = −0.370, p = 713. Patients had no difficulty or ease in focusing on VR stimuli.
The difference between the mean score for patient engagement and the norm are significant t (59) = 4.429, p < .001, Cohen’s d = 0.57, the effect size is moderate. Since t cal > 0, patients tended to feel easily involved in virtual reality. The result obtained is consistent with the high levels of involvement observed with the ITC-SOPI.
The difference between the patients’ mean emotion score and the norm are significant t (59) = 2.319, p < .024, Cohen’s d = 0.30, the effect size is small. Since t cal > 0, patients were predisposed to experience the emotions induced by the virtual environment. This result is consistent with the data processed with valence SAM.
The frequency with which participants engaged in video games was not significantly different from the norm t (59) = 0.183, p = 0.855. Patients were not particularly interested in video games.
The difference between the mean score for patients’ overall propensity to immerse themselves in an activity and the norm are significant t (59) = 3.071, p < .003, Cohen’s d 0.40, effect size is small. Since t cal > 0, patients were predisposed to immerse themselves within virtual environments, and, consequently, felt transported into the relaxing space offered by virtual nature.
The emergence of VR in oncology has shown promise during treatment, with major advantages in promoting patients’ emotional wellbeing. Most studies have highlighted the benefits of its distracting power, allowing attention to be diverted from the stressful medical context to focus on the pleasant stimuli of the virtual experience (Chirico et al., 2019). As a follow-up to a previous study (Buche et al., 2021), this research was designed to 1) examine the benefits of VR distraction as a tool to aid emotional regulation in breast cancer patients during a critical phase of management (i.e., chemotherapy), 2) compare two immersive VR modalities (i.e., Participatory VR vs Contemplative VR) to a more traditional distraction condition (i.e., Music).
In order to best appreciate the optimal conditions for VR use, a quasi-experimental protocol was set up in an oncology department. During a chemotherapy session, patients were exposed to only one of four distraction conditions: participatory VR, contemplative VR, listening to classical music or no distraction. Patients’ sense of presence in the virtual environment (ITC-SCOPI) and emotional state (STAI; SAM) were examined. Adverse effects generated by VR (CQ) were monitored in patients receiving this distraction condition. Finally, the patients’ propensity to immerse themselves in the relaxing Universe (QPI) was monitored for the entire sample.
Our results concerning the emotional wellbeing of patients surveyed via questionnaires (SAM; STAI) underscore the relevance of using VR during chemotherapy. On the one hand, these results are consistent with the theory of Frederickson, (2001) according to which the promotion of positive emotions allows individuals to better adapt to difficult situations and promotes resilience. Consistent with our initial study (Buche et al., 2021), the main strength of VR is the support of emotional regulation by eliciting pleasant emotions, thereby calming the state of emotional tension. Recent research (O'Gara et al., 2022) reports similar results in an oncological setting and shows a progressive improvement in patients’ feelings throughout the VR sessions. In the present study, the multimodal and interactive nature offered by VR was found to be more effective than musical relaxation in regulating emotions during chemotherapy (SAM Arousal; SAM Valencia), eliciting a much more positive emotion when the immersion was interactive (SAM Valencia). This feeling could be related to the sense of more intense spatial presence when patients are immersed in a natural interactive environment (Bouvier, 2009; Chirico et al., 2019; Buche et al., 2021). The possibility to create one’s own atmosphere within a virtual natural environment is an asset to be taken into account to improve the wellbeing of patients during chemotherapy. This result is reminiscent of the benefit of offering immersion in a relaxing natural environment (Riecke & von der Heyde, 2003).
On the other hand, our results report a significant decrease in anxiety in patients regardless of the type of distraction offered (i.e., Participatory VR, Contemplative VR and Music). This result, similar to the study conducted by Chirico et al. (2019) highlights the need to offer distractive accompaniments during chemotherapy sessions. Contrary to our expectations, the lack of significant difference between the three types of distractions proposed (i.e., Participatory VR, Contemplative VR, and Music) does not support the hypothesis that moving in a natural virtual environment would be more effective than observing the same environment (and/or listening to music) in relieving patients’ anxiety during chemotherapy. The use of distractions as tools for emotional regulation is therefore to be preferred, especially when the practitioner is not available during the acute phase of cancer care. In the future, it would be interesting to precisely measure the number but also the typology of actions carried out in the participatory condition, to highlight the level of patient’s interaction with the virtual environment.
Concerning the immersive qualities, our results confirm the importance of interactivity to increase the intensity of the sense of presence in the virtual Universe. Similar to our first study (Buche et al., 2021), the sense of spatial presence is more intense in a relaxing natural environment that requires repeated motor actions (i.e., participatory immersion). In line with our hypotheses, shaping one’s virtual environment reinforces the illusion of being physically present in the virtual Universe. Furthermore, the high level of engagement in both immersive modalities reveals that the patients were fully involved in their virtual experience. The propensity to immerse is one of the inherent factors of the sens of presence (Servotte et al., 2020). The IPQ results support the effectiveness of VR as a distractor and emotional regulation tool during chemotherapy. As expected, patients were predisposed to immerse themselves in the virtual environment and to feel the emotions conveyed by the natural environment. In other words, they could easily be distracted by the pleasant stimuli generated in 3D.
Overall, it appears that the VR tool was well tolerated during chemotherapy regardless of the immersive modality: the low CQ scores in both immersive modalities indicate that cybersickness did not alter the sense of presence (Servotte et al., 2020) or the onset of positive effects of VR during chemotherapy. These results are consistent with our initial study conducted in physical therapy (Buche et al., 2021). According to Witmer Singer (1998), cybersickness patients focus attention on physical and physiological symptoms. The apparent lack of physiological difficulties indicates that the patients were able to fully engage in the immersion and tasks associated with the virtual experience. It is possible that the high-tech device used is more effective than its predecessors in improving emotional comfort, without inducing significant side effects (Chirico et al., 2019). Furthermore, the minor adverse effects of VR reported by patients in this study underline the importance of using short-term immersion during chemotherapy. Again (see Buche et al., 2021), this duration enables to maximize patients’ comfort and interest while reducing the risk of cybersickness. Finally, the QC questionnaire should be presented before and after treatment to each group of patients to provide further evidence of the benefits of VR in distinguishing chemotherapy-related symptoms. It would be interesting to be able to distinguish the origin of nausea (i.e., VR vs chemotherapy) or at least the way patients attribute the cause of their nausea.
While there are many strengths to our study, there are some limitations to be mentioned. First, the development of increasingly sophisticated devices now requires that a phase of familiarization with the VR tool be integrated into the research protocol so that learning to use the virtual tool does not interfere with the soothing distractive experience (Buche et al., 2021). In the present research study, only six patients out of 120 had already experienced an immersive VR system outside of a medical context. This data underlines the importance of a discovery period prior to the actual experience during chemotherapy. Implementing a familiarization phase would reduce the surprise effect of VR (Buche et al., 2021) and moderate any novelty effect. On the other hand, repeated exposure to immersion could create a phenomenon of habituation deleterious to the effectiveness of VR (Buche et al., 2021). The use of regularly updated virtual environments that can be modulated in terms of cognitive stimulation could maintain interest and wonder in this tool (Garrett et al., 2020; Buche et al., 2021).
Second, experiments conducted in non-laboratory settings do not easily allow for physiological measures to assess the level of anxiety. Our study did not include objective measures such as electrodermal or heart rate recording to compare with subjective responses obtained in chemotherapy. In addition, the clinical setting did not allow for the addition of a variable actively engaging patients in a musical task using classical instruments (i.e., participatory music) to compare its effects to other types of distraction (i.e., Participatory VR, Contemplative VR, Music). Further research comparing VR to other forms of distraction such as music therapy, meditation, cardiac coherence or mindfulness should also be considered in order to highlight the true contribution of VR distraction during patient management.
Third, our study focuses on the ability of VR to reduce anxiety symptoms and induce a positive emotional state during treatment. However, it would be appropriate to broaden the scope of possibilities, including the effects of VR on quality of life as suggested by a recent study conducted in oncology (Reynolds et al., 2022). The contributions of VR could thus be sought at a secondary level during treatment, in particular by considering compliance and satisfaction with care. These effects should be further explored in order to promote the use of this tool in oncology and to arouse the interest of health professionals (Tennant et al., 2020).
Fourth, in order to correspond as closely as possible to patients’ preferences, their profile would benefit from being established beforehand to anticipate reactions and adaptation to distraction under VR. The evaluation of personality traits would make it possible to orient patients towards a virtual immersion which is best adapted to their personal, emotional, experiential and motivational characteristics, and finally to better predict the impact of this distractive strategy on this population (Plaisant et al., 2010). A future study should aim to measure the impact of inter-individual differences on the patients’ immersive experience and the benefits reported during several oncology treatment sessions. It would also be appropriate to ask patients whether they would recommend the use of VR as supportive care to others with cancer, and whether it should be extended to other medical procedures.
Finally, the value of utilizing VR in oncology is not only to be understood from the patient’s side, but also from the caregiver’s perspective. Depression, post-traumatic stress symptoms, non-specific anxiety disorders: in the context of Covid and post-Covid, caregivers have also payed a heavy price. The causes are well identified: deteriorated working conditions, a multiplication of new tasks, conflicts altering professional relationships, and a climate of insecurity in the hospital environment El-Hage et al., 2020; Lai et al., 2020; Morgand et al., 2022). The main psychological suffering observed among nurses placed on the front line during the pandemic involves professional exhaustion (Lai et al., 2020; Morgand et al., 2022).
In this context of a deteriorating healthcare system, given what we know about VR in chemotherapy, it would be interesting to determine the extent to which the presence of this virtual device could also be of benefit to nurses. Does VR support for patients to manage their emotions in a chemotherapy setting limit the demands on caregivers? What is the impact of these devices on nurses’ wellbeing and on their perception of being effective in their role in serving patients? These are all questions that future research would benefit from investigating.
The observed results confirm the benefits of a VR experience during chemotherapy by lowering patients’ anxiety level. This multimodal distractive strategy was found to be more effective than musical relaxation and induced more positive emotion if the immersion was interactive. This feeling could be related to the sens of spatial presence that is more intense when patients are active in a natural interactive environment. Thus, this study provides additional evidence for the use of VR to address the need for patient support during the acute phase of breast cancer care.
The raw data supporting the conclusion of this article will be made available by the authors, without undue reservation.
The studies involving humans were approved by the IRB00013686- 2023-23-CER UPVM—Université Paul Valéry—Montpellier III (France) IRB #2. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin.
All authors listed have made a substantial, direct and intellectual contribution to the work, and approved it for publication.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. The author(s) received specific funding for this study. AstraZeneca funded the virtual reality headsets required for this research. Thus, the funder was not involved in the study design, data collection, analysis, interpretation, writing of this article or the decision to submit it for publication.
The authors thank AstraZeneca for their financial support.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Ahmadpour, N., Keep, M., Janssen, A., Rouf, A. S., and Marthick, M. (2020). Design strategies for virtual reality interventions for managing pain and anxiety in children and adolescents: scoping review. JMIR serious games 8 (1), e14565. doi:10.2196/14565
Ando, M. M., Leones, L. M. B., Mendoza, M. J. L., Ting, F. I., and Sacdalan, D. B. (2022). O15-4 Use of virtual reality for management of anxiety and depression among chemotherapy-naive Filipino breast cancer patients. Ann. Oncol. 33, S478. doi:10.1016/j.annonc.2022.05.052
Baus, O., and Bouchard, S. (2014). Moving from virtual reality exposure-based therapy to augmented reality exposure-based therapy: a review. Front. Hum. Neurosci. 8, 112. doi:10.3389/fnhum.2014.00112
Birkhoff, S. D., Waddington, C., Williams, J., Verucci, L., Dominelli, M., and Caplan, R. (2021). The effects of virtual reality on anxiety and self-efficacy among patients with cancer: a pilot study. Oncol. Nurs. forum 48 (4), 431–439. doi:10.1188/21.ONF.431-439
Birnie, K. A., Kulandaivelu, Y., Jibb, L., Hroch, P., Positano, K., Robertson, S., et al. (2018). Usability testing of an interactive virtual reality distraction intervention to reduce procedural pain in children and adolescents with cancer. J. Pediatr. Oncol. Nurs. 35, 406–416. doi:10.1177/1043454218782138
Bouvier, P. (2009). La présence en réalité virtuelle, une approche centrée utilisateur Thèse de doctorat en informatique. China, Université de Paris-Est.
Bradley, M. M., and Lang, P. J. (1994). Measuring emotion: the self-assessment manikin and the semantic differential. J. Behav. Ther. Exp. Psychiatry 25, 49–59. doi:10.1016/0005-791690063-9
Buche, H., Michel, A., and Blanc, N. (2022). Use of virtual reality in oncology: from the state of the art to an integrative model. Front. Virtual Real. 3, 894162. doi:10.3389/frvir.2022.894162
Buche, H., Michel, A., Piccoli, C., and Blanc, N. (2021). Contemplating or acting? Which immersive modes should Be favored in virtual reality during physiotherapy for breast cancer rehabilitation. Front. Psychol. 12, 631186. doi:10.3389/fpsyg.2021.631186
Carline, J., and Carline, R. (2017). Greener games. Available at: http://greenergames.net/.
Chirico, A., Lucidi, F., De Laurentiis, M., Milanese, C., Napoli, A., and Giordano, A. (2016). Virtual reality in health system: beyond entertainment. A mini-review on the efficacy of VR during cancer treatment. J. Cell. Physiol. 231, 275–287. doi:10.1002/jcp.25117
Chirico, A., Maiorano, P., Indovina, P., et al. (2019). Virtual reality and music therapy as distraction interventions to alleviate anxiety and improve mood states in breast cancer patients during chemotherapy. J. Cell. Physiol. 1. 10. doi:10.1002/jcp.29422
Coppée, E. (2021). L’humanisme au cœur de la pratique quotidienne des soignants: « Quelles sont les stratégies mises en place par le personnel infirmier afin de maintenir des soins humanisants au patient malgré un système de soins contraint ? ». Faculté de santé publique. Université catholique de Louvain. Available at: http://hdl.handle.net/2078.1/thesis:30919.
Cyberpsychology Laboratory of UQO (2002). Cyberpsychologie. Available at: http://w3.uqo.ca/cyberpsy/index.php/labs-team/.
El-Hage, W., Hingray, C., Lemogne, C., Yrondi, A., Brunault, P., Bienvenu, T., et al. (2020). Les professionnels de santé face à la pandémie de la maladie à coronavirus (COVID-19): quels risques pour leur santé mentale? L'encephale 46 (3), S73–S80. doi:10.1016/j.encep.2020.04.008
Fredrickson, B. (2001). The role of positive emotions in positive psychology. The broaden-and-build theory of positive emotions. Am. Psychol. 56, 218–226. doi:10.1037/0003-066x.56.3.218
Gamble, K. R., Howard, J. H., and Howard, D. V. (2014). Not just scenery: viewing nature pictures improves executive attention in older adults. Exp. Aging Res. 40 (5), 513–530. doi:10.1080/0361073X.2014.956618
Garrett, B. M., Tao, G., Taverner, T., Cordingley, E., and Sun, C. (2020). Patients perceptions of virtual reality therapy in the management of chronic cancer pain. Heliyon 6, e03916. doi:10.1016/j.heliyon.2020.e03916
Hjeij, D., Bilodeau, K., Ogez, D., Tremblay, M., Lavigne, G., Rainville, P., et al. (2022). La perception des infirmières quant à l’intégration d’une intervention novatrice inspirée de l’hypnose clinique aux traitements de chimiothérapie à la clinique externe d’oncologie. Can. Oncol. Nurs. J. 32 (3), 387–393. doi:10.5737/23688076323387
Independent Television Commission (2000). Sens of presence inventory administration and scoring instructions. London: Goldsmiths University.
Indovina, P., Barone, D., Gallo, L., Chirico, A., De Pietro, G., and Giordano, A. (2018). Virtual reality as a distraction intervention to relieve pain and distress during medical procedures. Clin. J. Pain 34, 858–877. doi:10.1097/AJP.0000000000000599
Janssen, A., Fletcher, J., Keep, M., Ahmadpour, N., Rouf, A., Marthick, M., et al. (2022). Experiences of patients undergoing chemotherapy with virtual reality: mixed methods feasibility study. JMIR serious games 10 (1), e29579. doi:10.2196/29579
Kennedy, R. S., Lane, N. E., Berbaum, K. S., and Lilienthal, M. G. (1993). Simulator Sickness Questionnaire: an enhanced method for quantifying simulator sickness. Int. J. Aviat. Psychol. 3 (3), 203–220. doi:10.1207/s15327108ijap0303_3
Krumhansl, C. C. (1997). An exploratory study of musical emotions and psychophysiology. J. Exp. Psychol. 51, 336–353. doi:10.1037/1196-1961.51.4.336
Lai, J., Ma, S., Wang, Y., Cai, Z., Hu, J., Wei, N., et al. (2020). Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw. open 3 (3), e203976. doi:10.1001/jamanetworkopen.2020.3976
Lerebours, F., Saltel, P., Béthune-Volters, A., Nallet, G., Bourdat, P., Vesin-Etterlen, F., et al. (2015). Satisfaction of Breast Cancer patients treated by chemotherapy outpatient clinics: results of the TemporELLES survey. Bull. Cancer 102 (4), 316–323. doi:10.1016/j.bulcan.2015.01.011
Macey, A. L., Macey, J., and Hamari, J. (2022). “Virtual reality in emotion regulation: a scoping review,” in International GamiFIN Conference, April 2-5, 2024, Ruka, IEEE 64–74.
Maneuvrier, A. (2020). Le sentiment de présence en réalité virtuelle: rôle modérateur des facteurs humains sur la performance (Doctoral dissertation, Normandie Université; Université de Montréal). Available at: https://www.theses.fr/2020NORMC035.
Michel, A., Vidal, J., Brigaud, E., Sokratous, K., and Blanc, N. (2019). Dessine-moi une réalité plus belle: la réalité virtuelle vue par les patientes atteintes d’un cancer du sein. Psychooncology 13, 69–78. doi:10.3166/pson-2019-0087
Morgand, C., Cabarrot, P., Coniel, M., Prunet, C., Gloanec, M., Morin, S., et al. (2022). Impact de la pandémie Covid-19 sur les évènements indésirables associés aux soins. Sante Publique Prépublication, 1t–12t. doi:10.3917/spub.pr1.0020
Navarro-Haro, M. V., López-del-Hoyo, Y., Campos, D., Linehan, M. M., Hoffman, H. G., García-Palacios, A., et al. (2017). Meditation experts try virtual reality mindfulness: a pilot study evaluation of the feasibility and acceptability of virtual reality to facilitate mindfulness practice in people attending a mindfulness conference. PLoS One 12 (11), e0187777. doi:10.1371/journal.pone.0187777
O'Gara, G., Murray, L., Georgopoulou, S., Anstiss, T., Macquarrie, A., Wheatstone, P., et al. (2022). SafeSpace: what is the feasibility and acceptability of a codesigned virtual reality intervention, incorporating compassionate mind training, to support people undergoing cancer treatment in a clinical setting? BMJ open 12 (2), e047626. doi:10.1136/bmjopen-2020-047626
Oyama, H., Kaneda, M., Katsumata, Akechi, T., and Ohsuga, M. (2000). Using the bedside wellness system during chemotherapy decreases fatigue and emesis in cancer patients. J. Med. Syst. 24, 173–182. doi:10.1023/a:1005591626518
Plaisant, O., Courtois, R., Réveillère, C., Mendelsohn, G. A., and John, O. P. (2010). Validation par analyse factorielle du Big Five Inventory français (BFI-Fr). Analyse convergente avec le NEO-PI-R. Annales Médico-Psychologiques. Rev. Psychiatr. 168 (2), 97–106. doi:10.1016/j.amp.2009.09.003
Prip, A., Møller, K. A., Nielsen, D. L., Jarden, M., Olsen, M. H., and Danielsen, A. K. (2018). The patient-healthcare professional relationship and communication in the oncology outpatient setting: a systematic review. Cancer Nurs. 41 (5), E11–E22. doi:10.1097/NCC.0000000000000533
Reynolds, L. M., Cavadino, A., Chin, S., Little, Z., Akroyd, A., Tennant, G., et al. (2022). The benefits and acceptability of virtual reality interventions for women with metastatic breast cancer in their homes; a pilot randomised trial. BMC cancer 22 (1), 360–413. doi:10.1186/s12885-021-09081-z
Riecke, B. E., and von der Heyde, M. (2003). “Qualitative modeling of spatial orientation processes using a logical network of necessary and sufficient conditions,” in 11th annual workshop on object perception, attention, and memory China, (OPAM 2003), 8.
Riva, G., Mantovani, F., Capideville, C. S., Preziosa, A., Morganti, F., Villani, D., et al. (2007). Affective interactions using virtual reality: the link between presence and emotions. CyberPsychology Behav. 10, 45–56. doi:10.1089/cpb.2006.9993
Rutkowski, S., Czech, O., Wrzeciono, A., Kiper, P., Szczepańska-Gieracha, J., and Malicka, I. (2021). Virtual reality as a chemotherapy support in treatment of anxiety and fatigue in patients with cancer: a systematic review and meta-analysis and future research directions. Complementary Ther. Med. 61, 102767. doi:10.1016/j.ctim.2021.102767
Sakhri, S., and Boulhart, H. (2021). Article cancer and virtual reality vr, the great challenge of the century. Archives Med. Case Rep. Case Study 5. doi:10.31579/2692-9392/101
Schneider, S. M., Kisby, C. K., and Flint, E. P. (2011). Effect of virtual reality on time perception in patients receiving chemotherapy. Support. Care Cancer 19, 555–564. doi:10.1007/s00520-010-0852-7
Schneider, S. M., and Workman, M. L. (1999). Effects of virtual reality on symptom distress in children receiving chemotherapy. Cyberpsychololgy Behav. 2, 125–134. doi:10.1089/cpb.1999.2.125
Servotte, J.-C., Goosse, M., Campbell, S. H., Hetzell, S., Dardenne, N., Simoneau, I. L., et al. (2020). Virtual reality experience: immersion, sense of presence, and cybersickness. Clin. Simul. Nurs. 38, 35–43. doi:10.1016/j.ecns.2019.09.006
Sharifpour, S., Manshaee, G., and Sajjadian, I. (2020). Effects of virtual reality therapy on perceived pain intensity, anxiety, catastrophising and self-efficacy among adolescents with cancer. Couns. Psychotherapy Res. 00, 218–226. doi:10.1002/capr.12311
Spielberger, D., Gorsuch, L., and Lushene, E. (1983). Manual for the state trait anxiety Inventory (From Y). ePalo Alto, CA: Consulting Psychologists Press.
Street, R. L., Makoul, G., Arora, N. K., and Epstein, R. M. (2009). How does communication heal? Pathways linking clinician–patient communication to health outcomes. Patient Educ. Couns. 74 (3), 295–301. doi:10.1016/j.pec.2008.11.015
Tennant, M., Youssef, G. J., McGillivray, J. A., Clark, T.-J., McMillan, L., and McCarthy, M. C. (2020). Exploring the use of immersive virtual reality to enhance psychological wellbeing in pediatric oncology: a pilot randomized controlled trial. Eur. J. Oncol. Nurs. 48, 101804. doi:10.1016/j.ejon.2020.101804
Tsaras, K., Papathanasiou, I. V., Mitsi, D., Veneti, A., Kelesi, M., Zyga, S., et al. (2018). Assessment of depression and anxiety in breast cancer patients: prevalence and associated factors. Asian Pac. J. cancer Prev. 19, 1661–1669. doi:10.22034/APJCP.2018.19.6.1661
Ulrich, R. S., Simons, R. F., Losito, B. D., Fiorito, E., Miles, M. A., and Zelson, M. (1991). Stress recovery during exposure to natural and urban environments. J. Environ. Psychol. 11, 201–230. doi:10.1016/s0272-4944(05)80184-7
Valtchanov, D., and Ellard, C. G. (2015). Cognitive and affective responses to natural scenes: effects of low level visual properties on preference, cognitive load and eye-movements. J. Environ. Psychol. 43, 184–195. doi:10.1016/j.jenvp.2015.07.001
Vincent, C., Eberts, M., Naik, T., Gulick, V., and O’Hayer, C. V. (2021). Provider experiences of virtual reality in clinical treatment. PLoS ONE 16 (10), e0259364. doi:10.1371/journal.pone.0259364
Whitehead-Pleaux, A. M., Zebrowski, N., Baryza, M. J., and Sheridan, R. L. (2007). Exploring the effects of music therapy on pediatric pain: phase 1. J. music Ther. 44 (3), 217–241. doi:10.1093/jmt/44.3.217
Wilson, K., and Scorsone, G. (2021). The use of virtual reality technologies to reduce anxiety and improve experience in chemotherapy patients during treatment. Front. Virtual Real. 2, 88. doi:10.3389/frvir.2021.695449
Witmer, B. G., and Singer, M. J. (1998). Measuring presence in virtual environments: a presence questionnaire. Presence 7 (3), 225–240. doi:10.1162/105474698565686
Wong, C. L., Li, C. K., Choi, K. C., So, W. K. W., Kwok, J. Y. Y., Cheung, Y. T., et al. (2021). Effects of immersive virtual reality for preventing and managing anxiety, nausea and vomiting among paediatric cancer patients receiving their first chemotherapy: a study protocol for an exploratory trial. PloS one 16 (10), e0258514. doi:10.1371/journal.pone.0258514
Keywords: virtual reality, breast cancer, emotional management, anxiety, chemotherapy
Citation: Buche H, Michel A and Blanc N (2023) When virtual reality supports patients’ emotional management in chemotherapy. Front. Virtual Real. 4:1294482. doi: 10.3389/frvir.2023.1294482
Received: 16 September 2023; Accepted: 31 October 2023;
Published: 14 November 2023.
Edited by:
Clint Bowers, University of Central Florida, United StatesReviewed by:
Giuseppe Caggianese, National Research Council (CNR), ItalyCopyright © 2023 Buche, Michel and Blanc. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hélène Buche, aGVsZW5lLmJ1Y2hlQHVuaXYtbW9udHAzLmZy; Aude Michel, YXVkZS5taWNoZWxAdW5pdi1tb250cDMuZnI=
†ORCID: Aude Michel, orcid.org/0009-0008-1263-1922; Nathalie Blanc, orcid.org/0000-0003-1327-0280
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.