
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
REVIEW article
Front. Virtual Real. , 30 September 2022
Sec. Virtual Reality in Medicine
Volume 3 - 2022 | https://doi.org/10.3389/frvir.2022.892905
This article is part of the Research Topic The Third Wave of Cognitive-Behavioral Therapy and Compassion-Based Interventions Delivered by VR and Other 2D to 4D Technologies View all 4 articles
The global population is aging at an unprecedented rate, increasing the necessity for effective interventions targeting the mental health needs of older adults. Technology addressing the aging process of older adults (i.e., gerontechnology) is an avenue for the efficient delivery of programs that enhance adult well-being. Virtual reality (VR) is a type of gerontechnology with the potential to improve mental health and well-being (e.g., by increasing resilience, mindfulness, compassion, connection with nature, and decreasing stress, depression, anxiety); however, evidence in this area is currently lacking and more rigorous research on the acceptability, feasibility, and effectiveness of mental health programming via VR for older adults, such as nature, mindfulness, or compassion-based interventions, is necessary. The present literature review: 1) explores, synthesizes, and critically evaluates the literature on older adult mental health, well-being and gerontechnology, with a focus on virtual reality-based nature, mindfulness, and compassion-based interventions; 2) examines research to date on the relationship between virtual reality technology and nature, mindfulness, and self-compassion; 3) identifies gaps, contradictions, and limitations of existing research; 4) identifies areas for further investigation; and 5) discusses implications for research and clinical practice.
Global population aging has been accelerating exponentially over the recent decades with the proportion of older adults predicted to surpass that of children for the first time in world history (United Nations Department of Economic and Social Affairs, 2013; World Health Organization, 2021). Critically, a substantial portion suffer from both diagnosed and sub-clinical mental health conditions (Ciechanowski et al., 2004; Gum et al., 2009; Institute of Medicine, 2012; Karel et al., 2012). Despite their need, older adults access mental health services less frequently than younger populations (Klap et al., 2003; Wang et al., 2005; Karlin et al., 2008; Bogner et al., 2009; Mental Health Foundation, 2018). New strategies to successfully target older adults’ mental health and well-being needs are therefore urgently required. Novel methods to improve the quality of life of older adults, benefitting from recent technological developments, have been applied in various settings to deliver distance interventions, encourage healthier lifestyles, and conduct non-invasive assessments (Preschl et al., 2011; Kim et al., 2017; Brimelow et al., 2020). Technology developed to meet older adults’ needs, or Gerontechnology (Bouma et al., 2009) has been increasingly integrated into daily life routines (Wootton, 2012; Calvo & Peters, 2013; Lattanzio et al., 2014; Bercovitz & Pagnini, 2016) and may have the potential to ameliorate treatment accessibility and quality (Kvedar et al., 2014). However, to maximize the effectiveness of these technology-based modalities, it is necessary to move beyond conventional telehealth methodologies and investigate fresh modalities of mental health provision for older adults, such as Virtual Reality (VR). VR may be particularly effective for older adults when incorporating natural settings, and elements of interventions focused on augmenting mindfulness and compassion. Thus, the aims of the present literature review are to: 1) explore, synthesize, and critically evaluate the literature on older adult mental health, well-being and gerontechnology, with a focus on virtual reality-based nature, mindfulness, and compassion-based interventions; 2) examine research to date on the relationship between virtual reality technology and nature, mindfulness, and self-compassion; 3) identify gaps, contradictions, and limitations of existing research; 4) identify areas for further investigation; and 5) discuss implications for research and clinical practice.
Global population trends predict a dramatic increase in the proportion of the population considered to be older adults (i.e., persons aged 60 years and older) and a general acceleration in population aging worldwide (UN DESA, 2013; WHO, 2021). Population aging can be defined as an increasing population share of older individuals, where decreases in mortality lead to decreases in fertility (UN DESA, 2013). The global share of older adults is expected to increase by more than twofold, from 841 million people in 2013 to over 2 billion in 2050, which will be approximately 21.1% of the worldwide population (UN DESA, 2013). With the current number of older adults at slightly over 1 billion, the shift in the global population’s age distribution is already being experienced (WHO, 2021). By 2047, it is predicted that the number of older adults will exceed the number of children for the first time in the history of the world (UN DESA, 2013). Additionally, the fastest growing portion of the population is the “oldest-old,” typically qualified as persons aged 85 and over. This segment of the population also has the highest healthcare needs and costs, due to medical comorbidities (UN DESA, 2019).
The process of aging consists of much diversity, defined by large inter-individual heterogeneity in general functioning, physical and mental health, coping skills, and access to socio-economic resources (Karel et al., 2012). Notably, a significant proportion of older adults suffer from mental health and cognitive conditions (Gum et al., 2009; IOM, 2012; Karel et al., 2012). For example, Karel and others (2012) found that of adults 65 years of age and older, approximately 20.4% met diagnostic criteria for a mental disorder over a period of 12 months. Additionally, mood disorders, such as depression, are becoming a growing concern for health services given their current prevalence in older adults, as well as the predicted trajectory of depression to be the main cause of disease burden by 2030 in higher income countries (Rodda et al., 2011). Of further concern, rates of depression are slightly more prevalent in the oldest old, who as mentioned previously, are the fastest growing proportion of the older adult population (Byers et al., 2010; UN DESA, 2019). These rates do not account for the significant number of older adults who experience clinically significant distress while not officially meeting the criteria for a psychiatric diagnosis or receiving a formal diagnosis (Ciechanowski et al., 2004), indicating that population rates of mental health challenges in older adults are likely underreported and that the magnitude of psychiatric difficulties could be vaster than realized. Furthermore, older adults with psychiatric symptoms are more likely to experience comorbid cognitive challenges (Gum et al., 2009), as well as poorer physical health outcomes with higher rates of hospitalization and emergency room visits (Bartels et al., 2003; IOM, 2012).
However, evidence indicates that older adults are less likely to access mental health services (Klap et al., 2003; Wang et al., 2005; Karlin et al., 2008; Bogner et al., 2009; MHF, 2018). Additionally, they are less likely to receive mental health care from specialists, compared to younger and middle-aged adults (Klap et al., 2003; Bogner et al., 2009). Common barriers to older adult mental health service provision cited in the literature include stigma, lack of information, perceived costs, mobility restraints, lack of specialized health professionals, limited mental health literacy, and beliefs that symptoms of mental health illnesses are a normal part of the aging process (Farrer et al., 2008; Bogner et al., 2009; Karel et al., 2012; Drozd et al., 2016; Titov et al., 2016; Morgan et al., 2017; Rost et al., 2017).
Given that mental health problems and cognitive impairments, such as dementia, are often under-discovered and undertreated in general medical practitioner settings (Ganguli et al., 2004; Wang et al., 2005; Unützer et al., 2006), the high rates of cognitive and psychological challenges amongst older adults (e.g., Gum et al., 2009; IOM, 2012; Karel et al., 2012), and the unprecedented aging of the population (e.g., GC, 2014; UN, 2013; WHO, 2017), there is a need for a paradigm shift encompassing innovative solutions to the approach and delivery of geriatric mental health care. Therefore, a holistic, collaborative, culturally-informed approach to care that focuses on the overall health and well-being of older adults appears to be essential to achieve positive quality of life outcomes (Karel et al., 2012; Bartels & Naslund, 2013; Pywell et al., 2020).
An approach that not only aims for normal aging, but instead “successful aging” thus seems necessary to achieve this goal (Rowe & Kahn, 1987; see also Rowe & Kahn, 1997; Rowe & Kahn, 1998). Building on the MacArthur model of successful aging (Rowe & Kahn, 1987), Rowe and Kahn’s (1997) scientific review and conceptualization of aging describes successful aging as comprising three key factors: 1) low likelihood of disease or disability related to disease, 2) strong capacity for cognitive and physical functioning, and 3) active involvement and interest in life. Rowe and Kahn (1997) postulate that while these factors on their own are important, it is their synergistic quality when combined that leads to successful aging. Therefore, it is theorized that approaches to care for older adult aging that emphasize these components are more likely to be effective at enabling positive aging experiences (Rowe & Kahn, 1997). During the past decades, this theory has been backed by an increased scientific attention to the psychological empowerment of older adults and has received continued interest in gerontological research, theory and practice (e.g., Hank, 2011; Pruchno & Carr, 2017). However, it has not been without controversy and critique, leading to an updated and revised version of the MacArthur model of successful aging (Rowe & Kahn, 2015). Main critiques of the original MacArthur model include, but are not limited to, a need for increased attention to the subjective aspects of successful aging, loosening of and expanding the successful aging criteria, defining successful aging in a way that is more inclusive and avoids discrimination or stigmatization of those who are not aging well, and Western cultural bias (Martinson & Berridge, 2015).
The term “Gerontechnology” was first coined by Graafmans and Brouwers (1989) and refers to the mixing of the scientific fields of gerontology and technological engineering. The word itself is a blend of “gerontology” (i.e., the study of aging) and “technology” (i.e., the creation and supply of technological products, services, and environments) (Fozard et al., 2000). It can be defined as the development and use of technology for the benefit of aging and older adults (Fozard et al., 2000). In Bouma and others’ (2009) review, gerontechnology is described as an essential determinant to the healthy aging and quality of life of older adults. Bouma et al. (2009) discusses how the field of gerontology often overlooks: 1) the environment of aging people, 2) proactive prevention-based solutions, instead seeking out disease countering strategies, and 3) active participation of older adults as their own agents of change in the healthy aging process. The impact and ability of technology to change the environment in which people age is highlighted as a key utility of using gerontechnology as a prevention-based intervention to promote holistic, healthy aging (Bouma et al., 2009). Fozard et al. (2000)’s seminal review highlights six key areas where gerontechnology has the potential to improve the aging process of older adults: 1) housing; 2) communication; 3) personal mobility and transportation; 4) health; 5); work; and 6) recreation and self-fulfillment. Of particular relevance, gerontechnology is posited to help with the healthy aging of older adults, for instance by preventing or postponing health problems through nonmedical interventions that help to counteract deterioration in psychological and physiological functioning, which is often linked to aging (Fozard et al., 2000). Additionally, Fozard and others (2000) points to the potential utility of computer games and visual arts-based computer programs as an under-tapped resource for self-fulfillment and well-being in older adults.
However, in order for gerontechnology to be successfully implemented, it needs to be perceived as acceptable by its primary target, namely, older adults. According to Davis’s (1989) technology acceptance model (TAM), two primary components effect an individual’s acceptance of technology: 1) perceived usefulness of the technology, and 2) perceived ease of use. That is, potential use of technology is often predicted by the extent that individuals believe it will be helpful to them. However, even if potential technology users think that a specific technology is useful, they may also think that it is too challenging to use, and that the effort involved in using the technology outweighs its benefits (Davis, 1989). Therefore, based on the TAM, effective gerontechnology should be clearly beneficial to its users, while also being developed and presented in a way that is easy for users to engage with. This hypothesis has been empirically supported through a meta-analysis conducted by Zhou and others (2020), where it was found that perceived usefulness and perceived ease of use had significant positive impacts on older adults’ attitudes and behavioral intentions related to gerontechnology.
The global impact of the aging society is further compounded by another major societal change: the technological revolution. In particular, these transformations raise questions for researchers, policymakers, and practitioners as to whether computer-based technologies will further widen the divide of age segregation, amplifying the isolation of older people, or instead break down generational barriers (Rowe & Kahn, 2015). Despite common perceptions, a growing body of research is beginning to highlight the potential acceptability of technology for older adults as evidenced by its increased integration into their daily life routines (Wootton, 2012; Calvo & Peters, 2013; Lattanzio et al., 2014; Bercovitz & Pagnini, 2016). For instance, in higher income countries, adults over 65 years of age appear to be increasingly Internet and tech-savvy (Wagner & Wagner, 2003; Crabb et al., 2012; Reardon 2012; Cangelosi and Sorrel, 2014). Estimates of older adults in the USA indicate that over 50% use email or the Internet, with around 70% of this population using them every day (Reardon, 2012). Additionally, approximately 11% of older adults own a smartphone (Reardon, 2012).
While the Internet, email, and text messaging are, at this time, the most widespread and accessible types of computer-based technology for older adults, more advanced forms of technology (e.g., patient portals, smartphone applications) that help older adults manage acute and chronic health-based conditions also appear to be acceptable, based on findings from recent scientific studies (for e.g., see Chang & Im, 2014; McMahon et al., 2014; Taha et al., 2014; Wong et al., 2014). Gerontechology is currently applied in a wide range of health-based domains such as physical activity and mobility, home care experience, and overall wellness. For example, technology has been used to assist with medication adherence in home care settings (Lapane et al., 2012; Reeder et al., 2013). Pedometer-based technology used to help with flexibility and frequency of exercise has been implemented in older adult populations through DVD-based exercise programs, tablet computers, and software applications (Bickmore et al., 2013; McAuley et al., 2013; Silveira et al., 2013). Information technology has been used to augment knowledge of and adherence to practices that improve general wellness (Cocosila et al., 2009; Thompson et al., 2011; Xie, 2011); for instance, focusing on improving mental health by reducing isolation and loneliness (McCausland & Falk, 2012). Furthermore, VR headsets have become more accessible and immersive for older adults with tools such as head-mounted display (HMD) and the cave automatic virtual environment (CAVE) that facilitate increased interaction with virtual environments, thereby improving engagement and motivation to use technological interventions (Tuena et al., 2020). The development of mobile application technology with visors and/or tracking systems (e.g., Google Cardboard) allows for further options that are accessible and provide relatively immersive virtual environments (Fang et al., 2017; Tuena et al., 2020). These VR technologies allow for the development of tailored exercises that can be meaningfully manipulated and controlled to virtual environments, enabling effective rehabilitation interventions (Winstein et al., 2016). However, the current gerontechnology research-base is heavily weighted towards biomedical and physical health interventions, often overlooking the potential for gerontechnology as a psychological intervention (Vailati-Riboni et al., 2020a). Kwon (2016)’s review of current gerontechnology applications highlights this gap in the research, noting that there is a dearth of research examining assistive technology geared towards cognitive and psychological needs, with most gerontechnology research focusing on heart disease and diabetes, as evidenced by a systematic review by Barlow and others (2007). Of the research examining gerontechnology to support psychological well-being and quality-of-life, the available technology-based interventions appear to fall into six main categories: 1) Telemedicine; 2) Smartphone applications; 3) Software; 4) Videogames; 5) Robots; and 6) VR. For a more detailed review of the psychological applications of gerontechnology, see Vailati-Riboni et al. (2020a).
As outlined above, gerontechnology can be used as a psychological intervention in a variety of ways. Encouragingly, research with varying levels of vigor has highlighted the potential benefits for mental health and well-being linked to gerontechnological interventions (for review, see Baker et al., 2018; Buyl et al., 2020; Chen & Schulz, 2016; Lampit et al., 2014; Piau et al., 2014; Vailati-Riboni et al., 2020a). While a full review of the benefits of gerontechnology is beyond the scope of this paper, a growing body of literature points to its potential benefits for social isolation (e.g., Fokkema & Knipscheer, 2007; Tsai et al., 2010; Kahlbaugh et al., 2011; Tsai & Tsai, 2011; Cotten et al., 2013; Aarts et al., 2015), cognitive performance (e.g., Ball et al., 2002; Shatil et al., 2014; Ballesteros et al., 2015; Kim et al., 2015), depression (e.g., Spek et al., 2007; Tsai & Tsai, 2011; Preschl et al., 2012; Dear et al., 2015a; Jøranson et al., 2015; Titov et al., 2015; Firth et al., 2017a), anxiety (e.g., Zou et al., 2012; Mewton et al., 2013; Dear et al., 2015a; Dear et al., 2015b; Firth et al., 2017b), quality of life (Moyle et al., 2013; Broadbent et al., 2014; Vailati-Riboni, 2018; Vailati-Riboni et al., 2020b), and well-being (Cocosila et al., 2009; Thompson et al., 2011; Xie, 2011; Silva et al., 2015). Table 1 provides an overview of findings from a selection of existing reviews evaluating the efficacy of gerontechnology for well-being and mental health.
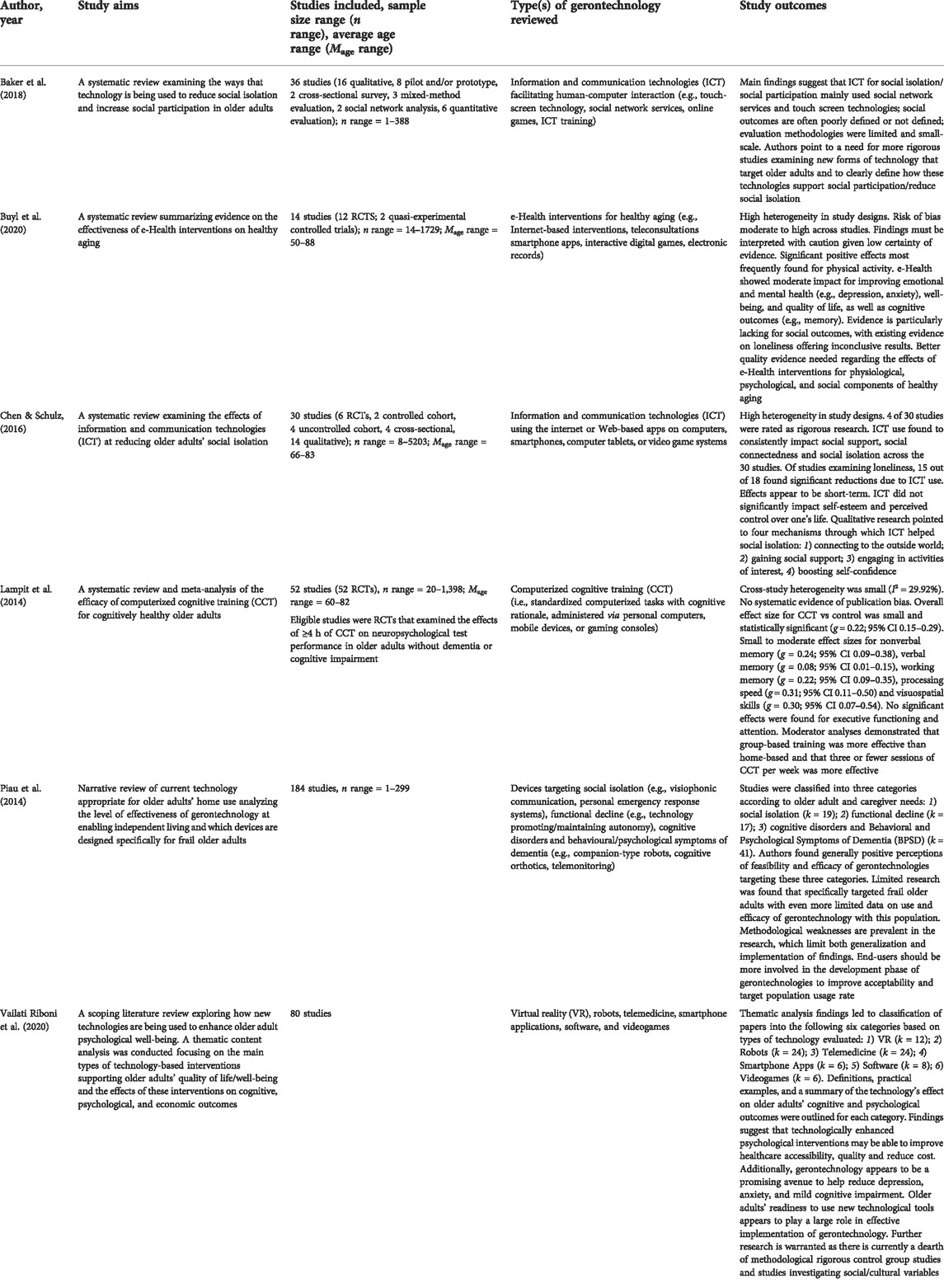
TABLE 1. Examples of recent reviews and meta-analyses evaluating gerontechnology aimed at improving mental health and well-being outcomes.
Gerontechnology is predicted to improve the aging process for older adults; however, its implementation is not without concerns and drawbacks (Kim et al., 2017). Of key importance, despite its potential for improving various aspects of older adults’ lives (e.g., social engagement, cognitive engagement, functional independence), this age group continues to show reluctance to engage with technology (Millward, 2003). Older adults’ lack of technology uptake is even more pronounced when compared with younger populations, a phenomenon referred to as the “grey digital divide” (Millward, 2003; Nielsen, 2014). Several barriers to gerontechnology use have been identified in the literature. For example, in a study by the Pew Research Center, it was found that skeptical attitudes regarding the benefits of technology use, difficulties learning to use technologies, and physical challenges were among some of the most frequently cited barriers (Smith, 2014). In a review by Kang and others (2010), obstacles to technology uptake included the tendency for many older adults to feel uncomfortable with new technology, stigma (for e.g., viewing technology as a confession of dependence) and financial concerns. In a focus group study by Vaportzis and others (2017) examining the acceptability of technology and computer tablet use, older adults expressed concerns related to three main categories: 1) barriers, such as lack of instructions, low confidence, health-related drawbacks, and cost; 2) disadvantages, such as technology that is too complex or too prolific, feelings of inadequacy, comparison with younger generations, or lack of in-person social interaction, and 3) skepticism about technology use, in general. Importantly, in a recent review on effective implementation of digital mental health interventions for older adults by Seifert and others (2019), five risks for barriers to gerontechnology use were identified: 1) lack of experience, social support, and access to digital technology increasing the risk that older adults perceive technology to be exclusionary; 2) lower use of digital technologies amongst older adults; 3) retired older adults are not required to use new technologies for their work, potentially reducing their motivation to try new technologies; 4) lower levels of socialization to technology; and 5) aging-related increases in cognitive, physical, social, and financial vulnerability leading to greater effort needed to learn to use new technologies. Given the commonly expressed challenges and barriers to gerontechnology use found in the research, effective technologies should be designed to be easily usable by older adults, provide avenues for increased social contact, be easy to fit into the user’s daily routine, and provide opportunities for rapid and/or frequent interactions with health providers (Jimison et al., 2008; Kang et al., 2010; Seifert et al., 2019). Finally, and of crucial importance, gerontechnology should be perceived as beneficial by users (Jimison et al., 2008).
Accordingly, in order to maximize the effectiveness of gerontechnology, it may be useful for research to move beyond conventional telehealth methodologies and examine fresh modalities of mental health provision for older adults, such as VR. VR technology provides computer-generated simulations of three-dimensional environments that the user is able to navigate and interact with in real time (Pratt et al., 1995). VR can be referred to as “immersive” when a user’s sensory attention is captured in such a way that they perceive a sense of truly being present in the virtual environment (Slater et al., 1994). VR devices are typically in the form of head-mounted display systems, desktop visual display systems, smartphones, tablets, or other handheld devices (Cherniack, 2011; Lee et al., 2019). For an optimal VR experience, headsets with head-mounted displays using high-end computer processors are needed to facilitate positional tracking, in addition to controlling the immersive virtual environment desktop (Lee et al., 2019). The advent of high-quality standalone headsets, such as the Quest 2 and HTC Vive Focus Plus, now makes it possible to provide quality immersive experiences without the need to connect to a separate powerful computer (Kugler, 2021). VR utilizing 360-degree videos has the ability to virtually transport users, facilitating active exploration and experience of the video from any angle and a perception of immersion in the virtual environment (Riva & Wiederhold, 2020).
In a study by Li and others (2017) where 94 undergraduate students viewed 73 different immersive VR videoclips, VR 360-degree videos were found to induce specific emotions at varying levels of arousal and valence. Additionally, in a series of experiments where participants studied 360° panoramic scenes, either through a sliding window panoramic display or using a VR headset, it was found the 360° VR videos have the potential to create a dynamic interplay between perception and memory that can be used to update and improve the specific features of these cognitive process (Robertson et al., 2016). Furthermore, VR may be able to enhance older adults’ motivation to engage in cognitive and/or physically demanding tasks given its capacity to provide fun and enjoyable experiences (Molina et al., 2014; Lee et al., 2019). These findings demonstrate particular promise for addressing mental health issues as they highlight the pathways through which immersive VR may enable lasting psychological and behavioral change.
VR appears to have strong therapeutic potential for use as an intervention for older adults and offers substantial advantages when compared to conventional treatments with respect to accessibility (e.g., to a wider number of clinical stimuli), functionality (i.e., by improving capacity to provide interactions with and tests of “real-life” skills), patient interaction with therapeutic stimuli, standardization of experimental treatments, possibilities for treatment-related virtual environment manipulation, and safety conditions for patients (Cherniack, 2011). Additionally, systematic review evidence suggests that VR may be as effective as traditional treatment methods but may achieve results in shorter periods of time (Mohr et al., 2013; Montana et al., 2020). Notably, preliminary research indicates that VR applications in mental health practice show increased acceptability by older adult patients, as measured via the Technology Acceptance Model (Davis, 1989; Benham et al., 2019).
The field of older adult VR is still relatively nascent. However, to-date, scientific research examining the effectiveness of VR interventions for older adults points to various potential benefits for physical, psychological, and social well-being (Hasan and Linger, 2016; Baez et al., 2017; Lee et al., 2019; Montana et al., 2020; Vailati-Riboni et al., 2020). Physical benefits include decreased pain (Benham et al., 2019; Dermody et al., 2020), increased functional strength (Dermody et al., 2020), improved balanced/decreased risk of falls (Bisson et al., 2007; Rendon et al., 2012; Dermody et al., 2020), improved posture (Dermody et al., 2020), and increased physical activity (Miller et al., 2014). Psychological effects include improved cognitive functioning (Optale et al., 2010; Cherniack, 2011; Dermody et al., 2020; Yen & Chiu, 2021), better emotion regulation (Hasan and Linger, 2016; Bornioli et al., 2019; Montana et al., 2020), decreased depression and anxiety (Robert et al., 2016; Yen & Chiu, 2021), creation of positive emotions and enjoyment (Lee et al., 2019), as well as an increased sense of control through environmental mastery and improved capacity to live independently (Lee et al., 2019). While there is less research examining the impact of VR on social outcomes in older adults, it has been hypothesized that VR may have the capability to increase social interaction in this population (Dudley, 2018; Miller et al., 2019). Additionally, VR used as a well-being intervention for older adults appears to have the distinct benefit of meeting more than one health-related need at once, given that VR programs often simultaneously address the physical, psychological, and social needs of the user (Hughes et al., 2017; Dudley, 2018).
Despite the numerous proposed benefits of VR for older adults, the strength of the research base is currently mixed, at best. Meta-analytic and systematic review findings indicate that many study designs are methodologically weak, with high risk for bias (Molina et al., 2014; Lee et al., 2019; Miller et al., 2013; Dermody et al., 2020; Montana et al., 2020; Thach et al., 2020; Skurla et al., 2021; Yen & Chiu, 2021). For example, in a systematic review by Dermody and others (2020) of VR interventions in community dwelling older adults, it was found that all seven of the included studies had small sample sizes (n ≤ 39), affecting the generalizability of the results. Additionally, none of the papers reviewed received a “high” quality rating (Dermody et al., 2020), based on the grading of recommendations, assessment, development, and evaluation (GRADE) approach to assess overall quality of findings (Higgins & Green, 2011). Similar methodological weaknesses were highlighted in the systematic review of 13 randomized controlled trials (RCTs) by Molina et al. (2014), where small and selective samples were a consistent issue for generalizability of results. Furthermore, none of the studies analyzed reported follow-up analyses, limiting the ability to decipher whether gains made during the intervention period would lead to lasting benefits (Molina et al., 2014). In a systematic review of 14 studies by Miller and others (2013) on the feasibility and effectiveness of VR interventions to enable physical activity in older adults, it was found that the evidence was not strong enough to conclude definitively whether interventions were effective, due to weak study quality and high risk of bias. Additionally, feasibility was reported inconsistently (Miller et al., 2014). A review by Montana and others (2020) pointed to the need for more rigorous RCTs in order to achieve an enhanced understanding of VR versus non-VR intervention efficacy. Finally, in the combined meta-analysis and systematic review of RCTs by Yen and Chiu (2021), all 18 studies were found to have moderate risk of bias based on the Cochrane Risk of Bias Rating (Higgins et al., 2011), once again highlighting a need for more rigorous research methodology in the field of VR research.
In addition to methodological limitations, important gaps in study design were identified. Older adults undergo visual and auditory changes as part of the aging process; however, many studies did not consider these age-related changes in their assessments (Dermody et al., 2020). For example, Dermody et al. (2020)’s review of community-based VR interventions for older adult health found that very few studies assessed visual acuity, (Parijat et al., 2014; Parijat et al., 2015) and often excluded participants if they had self-reported or serious visual or sensory impairment (Optale et al., 2010; Parijat et al., 2015; Parijat et al., 2015; Levy et al., 2016). Additionally, none of the studies in their review assessed hearing ability and only three studies measured for cybersickness (Parijat et al., 2015; Parijat et al., 2015; Benham et al., 2019). Furthermore, only one study included a survey question about participants’ perceived acceptability of the VR experience (Benham et al., 2019). Without attention paid to auditory and vision-based capabilities, as well as dexterity, older adults may be less likely to accept VR as an intervention. Therefore, further research examining the impact of developmental capacity on VR engagement, as well as design features in VR programs accounting for audio, visual, and physical challenges, is warranted. Notably, none of the studies reviewed by Dermody et al. (2020) integrated gaming technology in the VR system, which could be a potential way to support user engagement and enhance participant enjoyment (Molina et al., 2014). Finally, most studies reviewed examining VR programs for older adults focused on physical health-related interventions, with far fewer VR interventions incorporating an explicit focus on content related to improving psychological well-being (Molina et al., 2014; Parijat et al., 2015; Lee et al., 2019; Dermody et al., 2020; Yen & Chiu, 2021).
Several practical factors and challenges must be considered in order to implement VR as a gerontechnology that meets the standard of care for the aged care health sector. Given the mobility and strength issues that many older adults face, they may have trouble setting up VR devices and feel uncomfortable wearing headset devices for maintained lengths of time (Lee et al., 2019). However, with the rise of lightweight headsets such as the HTC Vive Flow the issue of headset weight is becoming less important (Peterson et al., 2021). Unsurprisingly, the majority of research to-date investigates the use of VR for healthy older adults (Dermody et al., 2020). The study of VR interventions for frail or unwell older adults is imperative, particularly due to the potential benefits related to cognitive decline (Optale et al., 2010; Cherniack, 2011; Yen & Chiu, 2021) and fall risk (Bisson et al., 2007; Rendon et al., 2012) that preliminary research in healthy older adults has identified. Additionally, natural age-related developments, such as visual and auditory changes, should be considered when designing VR apps for older adults, as reduced auditory and visual capacity could make VR engagement more difficult for certain older adults (Garrett et al., 2018). Financial barriers must also be considered when implementing VR interventions in aging populations, as VR technology can often be expensive. The economic cost of VR devices may be prohibitive for some older adults; however, due to technological developments, high-quality VR equipment is already becoming less expensive, often costing less than a laptop computer (Segal et al., 2011; Robert et al., 2016). Additionally, private insurance providers are beginning to include coverage for VR in healthcare treatment, further reducing financial barriers to access. For example, Bupa, Australia’s largest health insurer, is now covering XRHealth, a company providing VR and augmented reality-based therapeutic applications to the medical industry (XRHealth, 2020). Finally, common barriers to gerontechnology use such as discomfort with technology, lack of training, and skepticism should be addressed when using VR interventions with older adults in order to empower users and improve acceptability and adherence (Vailati-Riboni, 2020).
Keeping in mind the potential barriers to VR usage in older adult populations, one potential avenue for improved mental health and well-being is to design VR programs that incorporate scenes of nature. Exposure to natural settings, as well as perceived connection with nature, have both been shown to be associated with numerous improved psychological health outcomes (for review, see Aerts et al., 2018; Capaldi et al., 2014; Hartig et al., 2014, McMahan & Estes, 2015). The notion that natural settings are imperative for human thriving has been explored in the literature for decades (Orians, 1980). For instance, the Biophilia Hypothesis (Wilson, 1984), which is a seminal theory in environmental psychology, posits that human health and well-being is related to connection with our natural environment. Wilson (1984) theorizes that human affiliation with life forms and life-like processes is due to millennia of human evolution in natural surroundings, and the necessity for humans to be in contact with life-like processes in order to survive. Attention Restoration Theory (ART; Kaplan & Kaplan, 1989; Kaplan 1995) provides a theoretical framework to clarify the underlying mechanisms through which nature connection may improve mental health. ART hypothesizes that directed attention is a finite resource that can be restored through exposure and appreciation towards nature via “soft fascination”; that is, the attention directed towards interesting stimuli requiring minimal cognitive exertion (Kaplan, 1995). Furthermore, gerontechnology has been theoretically and empirically connected to the impact of the natural environment on healthy aging. For example, through developing appropriate technological interventions that consider the influence of the natural physical environment on well-being as one ages (Fozard, 2012). These hypotheses have been corroborated by a variety of studies (for e.g., Mayer et al., 2009; Nisbet et al., 2011; Roe & Aspinall, 2011; Sadowski et al., 2020; van den Berg et al., 2003; Zelenski & Nisbet, 2014) and reviews (Thompson Coon et al., 2011; Capaldi et al., 2014; Hartig et al., 2014; McMahan & Estes, 2015; Aerts et al., 2018) investigating the relationship between connection with nature and well-being.
One way proposed to utilize VR 360-degree video technology most effectively is through the incorporation of natural settings in the VR experience (Depledge et al., 2011; Smith, 2015; Browning et al., 2020). Despite the numerous benefits offered from exposure to in vivo nature, many people do not feel comfortable going into natural or “wild” environments, even if they have convenient access to them (Bixler & Floyd, 1999; Browning et al., 2017). It is important to develop and examine technologies, such as VR, that enable frequent, realistic interactions with nature, particularly in the context of older adult health promotion, given that nature may not always be accessible due to mobility restrictions and care needs related to aging, (Depledge et al., 2011; Van Houwelingen-Snippe et al., 2021). VR programs using 360-degree videos of nature are both a convenient and inexpensive way to provide access to nature (Depledge et al., 2011; Smith, 2015). This is particularly important given findings that many of the benefits of nature exposure can be achieved through VR headsets providing visual and auditory sensory information (Browning et al., 2020). Preliminary research comparing interaction with real-life nature to VR-based nature shows evidence that VR nature may provide similar benefits, although there is a lack of clarity to the extent that this comparison holds true, with some studies showing that the impacts of VR-based nature may be less beneficial for mood (Kjellgren & Buhrkall, 2010; Annerstedt et al., 2013; Calogiuri et al., 2018; Browning et al., 2020).
While the research field examining the impacts of VR-based natural environments is still relatively new, a growing body of literature points to the therapeutic efficacy of 360-degree nature videos (Valtchanov, 2010; Maples-Keller et al., 2017; Jerdan et al., 2018; White et al., 2018). For example, nature-based VR videos have been evidenced to rapidly improve mood in experimental studies of healthy, community-based young and middle-aged adults (Anderson et al., 2017) and university students (Valtchanov, 2010; Schutte et al., 2017; Yu et al., 2018). Anderson and others’ (2017) study of 18 young to middle-aged adults found that VR nature scenes 15-min in length improved both objective (electrodermal activity and heart-rate variability) and subjective (Positive and Negative Affect Schedule; Watson et al., 1988) affect. Yu et al. (2018) corroborated these findings in their study of psychological responses to 9-min VR nature videos in 30 healthy young adults, but did not find significant effects for physiological responses. Both Schutte et al. (2017) and Valtchanov (2010) reported that university student responses to short immersive VR-based nature videos indicated benefits for subjective psychological mood levels. Valtchanov (2010) also found objective improvements to relaxation via skin-conductance and heart rate.
The benefits to well-being conferred from 360-nature videos appear to extend to improvements in cognitive functioning (Gerber et al., 2017; Chung et al., 2018) and reductions in physiological levels of stress (Gerber et al., 2017; Hedblom et al., 2019). In Chung and others (2018) study of 40 healthy young adults, preliminary support was provided for the capability of 360-degree nature videos to restore attention, through subjective (Perceived Restorativeness Scale; Hartig et al., 1997) and objective measures (via event-related potential). Hedblom and others (2019) experimental study compared the effects of 360-degree virtual visual stimuli of urban environments, forests, and parks, with congruent olfactory stimuli (i.e., city and nature odors) and auditory stimuli (i.e., noise and bird songs) on physiological stress levels in 154 healthy young adults. Their findings indicated that the virtual park and forest provided significant stress reductions, but not the urban area (Hedblom et al., 2019). In addition to community settings, 360-degree VR nature videos show potential for improving attentional capacity and reducing physiological measures of stress in intensive care unit (ICU) settings, based on findings from 37 healthy younger and older adults with ages ranging from 20 to 85 (Gerber et al., 2017).
Despite preliminary support for VR-based nature videos on psychological well-being, several methodological and design limitations in the current scientific literature should be mentioned. The vast majority of reviewed studies examined healthy, younger or middle-aged adults with fairly small sample sizes. This significantly impacts the ability to generalize the results of these studies and it remains unclear whether the effects found would be the same in exclusively older adult or clinical populations. Many studies investigated both physiological and psychological outcomes, which was a methodological strength. However, most studies did not assess longitudinal outcomes of nature-based VR inductions and interventions, instead relying on single-time point evidence. Further studies are needed to clarify the durability of affective, cognitive and stress level improvements associated with 360-degree VR nature videos.
To-date, empirical research on nature-based VR interventions for older-adult well-being is extremely limited with only ten published articles found when conducting the literature search for this review. However, of these 10, only eight specifically focus on nature-based VR experiences for older adults (Banos et al., 2012; Bruun-Pedersen et al., 2014; Bruun-Pedersen et al., 2016; Bornioli et al., 2018; Moyle et al., 2018; Reynolds et al., 2018; Bornioli et al., 2019; Ludden et al., 2019), with the remaining two including older adults in their samples, but not exclusively studying this age group (Bornioli et al., 2018; Bornioli et al., 2019). Most studies focus on healthy, non-clinical samples (Banos et al., 2012; Bruun-Pedersen et al., 2014; Bruun-Pedersen et al., 2016; Bornioli et al., 2018; Bornioli et al., 2019), but three focused on older adults with symptoms of cognitive decline or dementia (Moyle et al., 2018; Reynolds et al., 2018; Ludden et al., 2019). Study findings are presented in Table 2 according to reference, sample, VR technology, VR environment, aims, design, measures, and results.
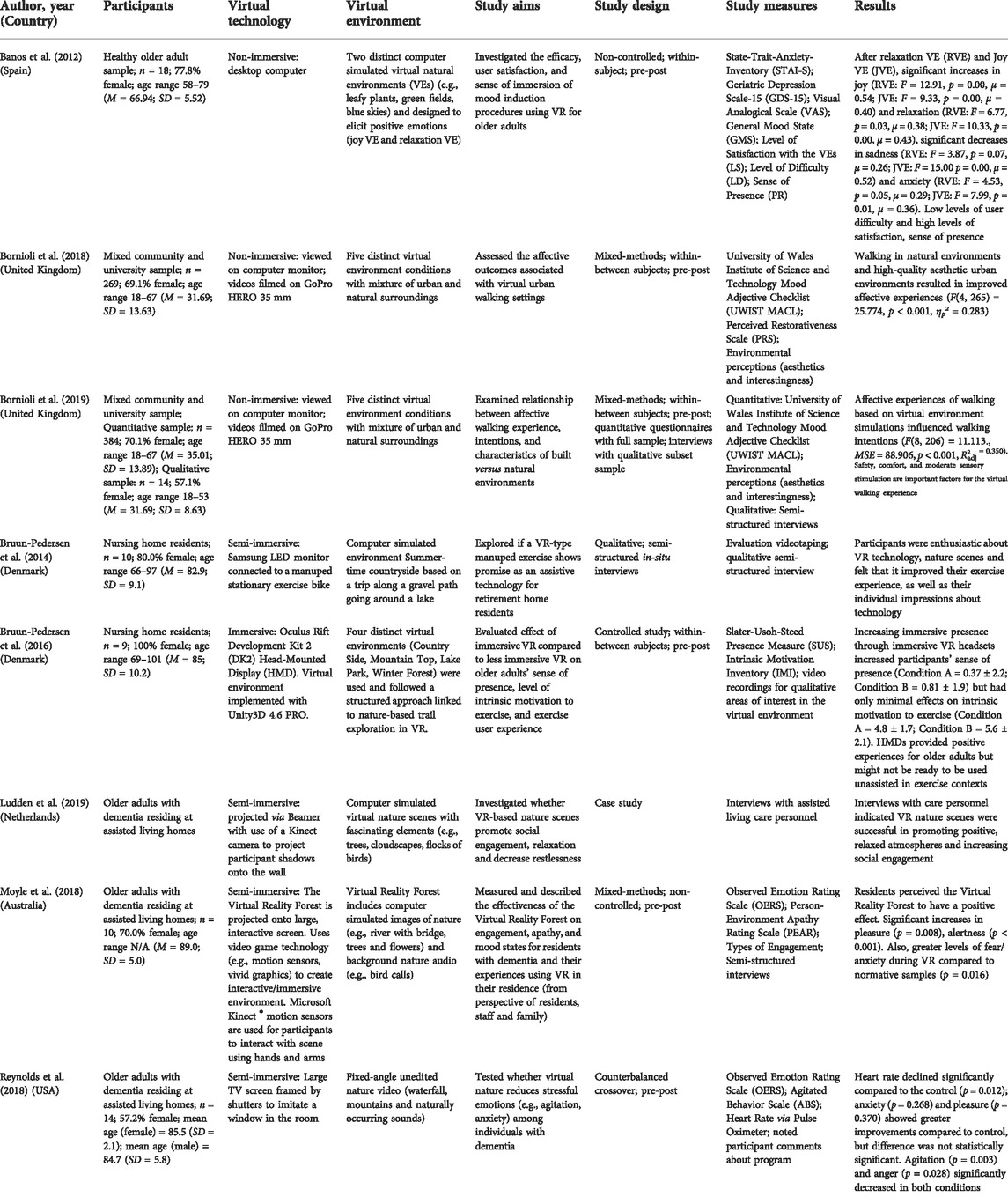
TABLE 2. Examples of empirical studies of nature-based VR interventions for older-adult mental health and well-being.
For example, in a study by Banos et al. (2012) the ability of VR-based nature walks to enhance feelings of positive mood and relaxation in 18 healthy older adults was explored. It was found that the virtual environments provided significant increases in joy and relaxation, and significant decreases in sadness and anxiety (Banos et al., 2012). Additionally, participants reported low difficulty of use along with high levels of satisfaction and sense of presence (Banos et al., 2012). However, this study used a small sample size with a non-clinical population, limiting generalizability of findings. Furthermore, the study examined only two sessions with the VR environment. In order to draw more robust conclusions, studies examining multiple nature-based VR sessions should be conducted, as it is likely that this will improve older adults’ comfortability with the VR interface, further clarifying the impact of the intervention itself on mood (Banos et al., 2012).
The impact of interactive screens with virtual nature scenes attached to exercise bicycles has been examined for potential benefits for enjoyment and self-efficacy in healthy older adults living in retirement homes (Bruun-Pedersen et al., 2014; Bruun-Pedersen et al., 2016). Results indicated that participants exercised for longer, experienced more excitement and felt an increased sense of control regarding their ability to engage in exercise (Bruun-Pedersen et al., 2014). However, these studies had small sample sizes (n ≤ 15), were conducted with healthy older adults, and did not use control groups, making findings challenging to generalize (Bruun-Pedersen et al., 2014; Bruun-Pedersen et al., 2016).
In an example of a study examining the potential use of VR-based nature videos for older adults with dementia, Ludden et al. (2019) conducted a series of case studies based at a residential care home in Sweden. Preliminary feedback from study participants and care home staff indicated acceptability and beneficial effects for mood and relaxation. However, due to the study design, the findings are once again challenging to replicate or generalize due to small sample size and lack of experimental design.
Taken together, there is clearly much work to be done to build the quality of evidence examining the impacts of VR-based nature environments for older adult well-being. While the quality of the empirical evidence is currently weak, qualitative findings indicate strong potential for clinical and practical benefits of VR-based nature interventions for the successful aging of older adults. This is particularly promising given the challenges that older adults may be faced with when trying to access nature in real life. Further research with longitudinal RCTs in both clinical and non-clinical populations is warranted to elucidate the feasibility, level of efficacy and mechanisms through which these interventions operate.
There are numerous definitions and frameworks for understanding mindfulness (for in-depth reviews of prevailing conceptualizations, see: Bodhi, 2011; Dunne, 2015; Gethin, 2011; Hart et al., 2013; Khoury et al., 2017). As a construct, the origins of mindfulness are derived from Buddhist tradition, where mindfulness is described as both the ability to remember past experiences in order to facilitate a deeper sense of purpose and awareness (Anālayo, 2003; Bodhi, 2011) and the capability to comprehend what is occurring the present moment (Brown et al., 2007; Bodhi, 2011). In recent years, mindfulness has been increasingly researched within the context of Western science, as is evidenced by growth in the number of mindfulness-related publications during the past four decades (Google Scholar, 2021). Perhaps the most prevalent westernized understanding of mindfulness is Kabat-Zinn’s (1994) conceptualization, where mindfulness is described as a non-judgmental, intentional awareness of the present moment. Mindfulness has also been theorized to be a socio-cognitive ability that allows individuals to notice and draw novel distinctions between objects, people, feelings, thoughts, or experiences and is described as the opposite of “mindlessness” (Langer, 1989; Langer and Moldoveaunu, 2000). Mindlessness is conceptualized as the state of being stuck in previously developed cognitive categories which prevents us from fully engaging with the experience at hand (Langer, 1989). Langer’s mindfulness paradigm is particularly interesting in the context of gerontechnology given the many barriers that older adults may face when attempting to use or integrate technology into their daily routines. A final important western conceptualization of mindfulness, which has been developed in more recent years as a way to reconcile different conceptual approaches, is that of embodied mindfulness (Khoury et al., 2017). Embodied mindfulness is embedded in both Buddhist philosophy and neurobiology and considers mindful consciousness as an interaction between the mind, body, and outside world (Khoury et al., 2017). The notion of embodied mindfulness becomes increasingly relevant in the context of immersive VR given the overlap between effectiveness of VR technology due to the concept of presence (i.e., the feeling of “being there” in one’s body) and the notion of embodied mindfulness as a skill or ability that includes elements of attention, awareness, and acceptance of the mind, body, and mind-body connections (Slater et al., 1994; Khoury et al., 2017). The concepts of embodied mindfulness and presence also connect to general design considerations in gerontechnology, because technologies that incorporate understanding of older adult users’ intentions and perceptions (e.g., understandability of a game or training structure, graphic realism, engaging storytelling) are generally experienced as more acceptable and easier to integrate into daily life (Triberti and Riva, 2016; Tuena et al., 2020). It is likely that the sense of mindful presence that these design elements facilitate allows for more potent gerontechnology interventions, such as VR (Tuena et al., 2020).
It has been theorized that some of the effectiveness of VR interventions is due to enhancing perceptions of mindfulness. For instance, through immersive VR’s capacity to capture participants’ attention and provide users the illusion of “being there” in the 3D computer generated environment, VR interventions may be particularly effective at incorporating mindfulness-based activities (Slater et al., 1994). By providing users with an interesting and engaging setting to practice mindfulness (e.g., simulated natural settings), limiting distractions from the real world, and increasing a sense of presence, VR may facilitate mindfulness practice (Navarro-Haro et al., 2017). As previously described, in the context of VR, “immersion” refers to the capability of a technical system to deliver an encompassing and convincing environment that a user is able to interact with, whereas the concept of “presence” refers to the experience of feeling and behaving as if one is actually in the virtual environment (Sanchez-Vives & Slater, 2005). Both of these sensations appear to have considerable overlap with elements of mindfulness in that they require the user to be present in the here and now and pay some level of attention to both their bodily sensations and environmental perceptions. Research demonstrates that the more immersive a VR intervention is, the more likely that users will endorse acceptability of the VR experience and report benefits (Riva et al., 2016). Additionally, if the VR experience is immersive enough, the VR user may have the perception that they are present in the virtual world or virtual body due to the alternation of cognitive factors that regulate the experience of body and physical space via perceptual information. In the context of VR this perception can also be referred to as “embodiment” (for a more detailed review of this theory, see Riva et al., 2015). Thus, it appears that mindfulness and immersive VR have the potential to operate in a bi-directional pathway, with increased mindfulness leading to augmented awareness and attention to the VR experience, and enhanced immersion in VR experiences leading to increased levels of mindfulness. Given the potential for mindfulness to enable older adults to approach technology with curiosity and openness to explore the unknown, improve engagement (Bercovitz & Pagnini, 2016), and the potential for VR to activate mindful experiences, VR applications that incorporate elements of mindfulness might be particularly useful in the context of gerontechnology interventions to support older-adult mental health and well-being.
Mindfulness-based interventions (MBIs) are behavioral interventions that teach mindfulness, following a mind-body medicine view of health by integrating physical, cognitive-affective, behavioral, and social components (Kabat-Zinn, 2013; Khoury et al., 2017; Khoury, 2018). MBIs have demonstrated efficacy for improving psychological well-being and reducing stress in non-clinical populations, as well as for a large range of psychological and physical disorders in clinical populations (for more in-depth review, see Carletto et al., 2020; Carrière et al., 2018; Goldberg et al., 2018; Hofmann et al., 2010; Howarth et al., 2019; Khoury et al., 2013; Khoury et al., 2015; Poissant et al., 2019).
A growing body of evidence suggests that MBIs have beneficial effects for older adults’ well-being at the psychological, cognitive, and physical levels. Regarding older adults’ psychological well-being, findings from exploratory studies and RCTs show decreased levels of stress, anxiety, worry, depression, negative self-focus, as well as increased effective coping strategies and resilience following MBIs when compared to control conditions (Young & Baime, 2010; Foulk et al., 2014; Lenze et al., 2014; Labbé et al., 2016; Perez-Blasco et al., 2016; Franco et al., 2017; Wetherell et al., 2017; Torres-Platas et al., 2019; Dikaois et al., 2020). With respect to cognitive well-being, cross-sectional studies have demonstrated associations between executive function and trait mindfulness, with reductions in stress mediating this relationship (Fiocco & Mallya, 2015). Furthermore, evidence from RCTs suggests significant improvements in older adults’ executive functioning following participation in MBIs (Moynihan et al., 2013). Concerning empirical support for the effects of MBIs on physiological well-being, participation in MBIs has been linked to benefits for immune response functionality, suggesting improved cellular level health post MBI participation (Gallegos et al., 2013; Ng et al., 2020). These findings are especially notable given that many older adults experience dysregulation of the immune system, which is associated with numerous adverse outcomes such as augmented vulnerability to infectious, autoimmune, cardiovascular, metabolic, and neurodegenerative diseases, and is worsened by chronic stress (Gouin et al., 2008; Müller et al., 2019). Findings from systematic reviews and meta-analyses further corroborate this evidence, with support found for MBIs’ ability to enhance positive mood, decrease symptoms of anxiety and depression, improve sleep quality and decrease chronic insomnia (Hazlett-Stevens et al., 2019). Additionally, meta-analytic and review findings indicate substantial support for the beneficial effects of MBIs on memory, and executive functioning, in particular, processing speed, sustained attention accuracy, and subjective attentional control (Chan et al., 2019; Hazlett-Stevens et al., 2019; Zainal & Newman, 2020).
However, these findings are not without limitations. Research investigating the efficacy of MBIs in exclusively older adult clinical populations is still minimal, with only seven RCT investigations identified to-date (Hazlett-Stevens et al., 2019). Hazlett-Stevens and others (2019) suggest that further research in specifically older adult clinical samples is needed in order to verify whether findings from research in mixed samples are actually generalizable to older adults. Additionally, findings from Hazlett-Stevens et al. (2019) point to a dearth of research examining the impacts of MBIs on comorbid conditions in older adults. Methodologically rigorous research examining the common psychiatric and medical comorbidities found in older adult patients is warranted. Additional gaps in the evidence-base include lack of measurement of quality of life and coping related to health conditions, as well as overwhelmingly westernized, educated, industrialized, rich and democratic (WEIRD) samples, which is a systemic problem biasing the psychology research field, in general (Henrich et al., 2010; Nielsen et al., 2017). Furthermore, despite the potential advantages of practicing mindfulness-based activities, many older adults who stand to benefit do not practice due to the demanding nature of developing mindfulness skills (e.g., traditional mindfulness practices may lead to states of dormancy in novice trainees which can be aversive and counter to the aims of mindful presence and attention). Unsurprisingly, this can lead to high rates of attrition during MBIs (Geiger et al., 2016).
Given the challenges for some older adults to maintain alertness when beginning mindfulness practices, and the related high levels of attrition in MBIs for older adults, facilitating mindfulness training through a VR platform could be an optimal way to help engage novice trainees, due to its ability to facilitate a sense of alertness, engagement, and presence (Slater et al., 1994; Navarro-Haro et al., 2017). Furthermore, VR programs that incorporate scenes of nature may be particularly effective at boosting user engagement with MBIs given that untrained meditators are more able to access soft fascination in restorative environments, such as nature (Kaplan, 2001; Schutte & Malouff, 2018). Preliminary findings highlight that VR is a promising technology to support MBIs, with evidence pointing to increases in well-being, self-compassion, and adherence among participants (Tong et al., 2015; Navarro-Haro et al., 2016; Navarro-Haro et al., 2017; Navarro-Haro et al., 2019; Seabrook et al., 2020; Modrego-Alarcón et al., 2021). Additionally, VR-based MBIs appear to lead to increased state (i.e., in-the-moment) mindfulness in both new and experienced meditators (Navarro-Haro et al., 2017; Chandrasiri et al., 2020), with RCT evidence suggesting that VR MBIs are as effective as in-person MBIs at cultivating state mindfulness (Chandrasiri et al., 2020). Furthermore, empirical findings indicate that VR-based MBIs incorporating scenes of nature may be effective at reducing pain (Tong et al., 2015) and improving cognitive functioning and satisfaction with life (Cikajlo et al., 2016) in clinical and non-clinical populations. The research field examining the effects of MBIs based in VR is still in its relative infancy; therefore, significant gaps in the literature exist. There are very few studies investigating the efficacy of MBIs delivered via VR, and with the exception of Cikajlo et al. (2016), who investigated a VR-based MBI 8-week in length, and Modrego-Alarcón et al. (2021) who investigated a mindfulness-compassion VR intervention 6-week in length, the existing VR-based MBI studies were either very short (e.g., one to two brief mindfulness sessions), or part of therapeutic interventions that did not focus exclusively on mindfulness, for example using Dialectical Behavior Therapy ® (Linehan, 1993; Navarro-Haro et al., 2016; Navarro-Haro et al., 2017; Navarro-Haro et al., 2019). Finally, to-date, no study has investigated MBIs delivered via VR exclusively for older adults. Current literature in related disciplines suggest benefits for this population; however, there is a need for empirical evidence to verify this claim. Examples of findings from studies of VR-based MBIs are presented in Table 3 according to reference, sample, VR technology, VR environment, aims, design, measures, and results.
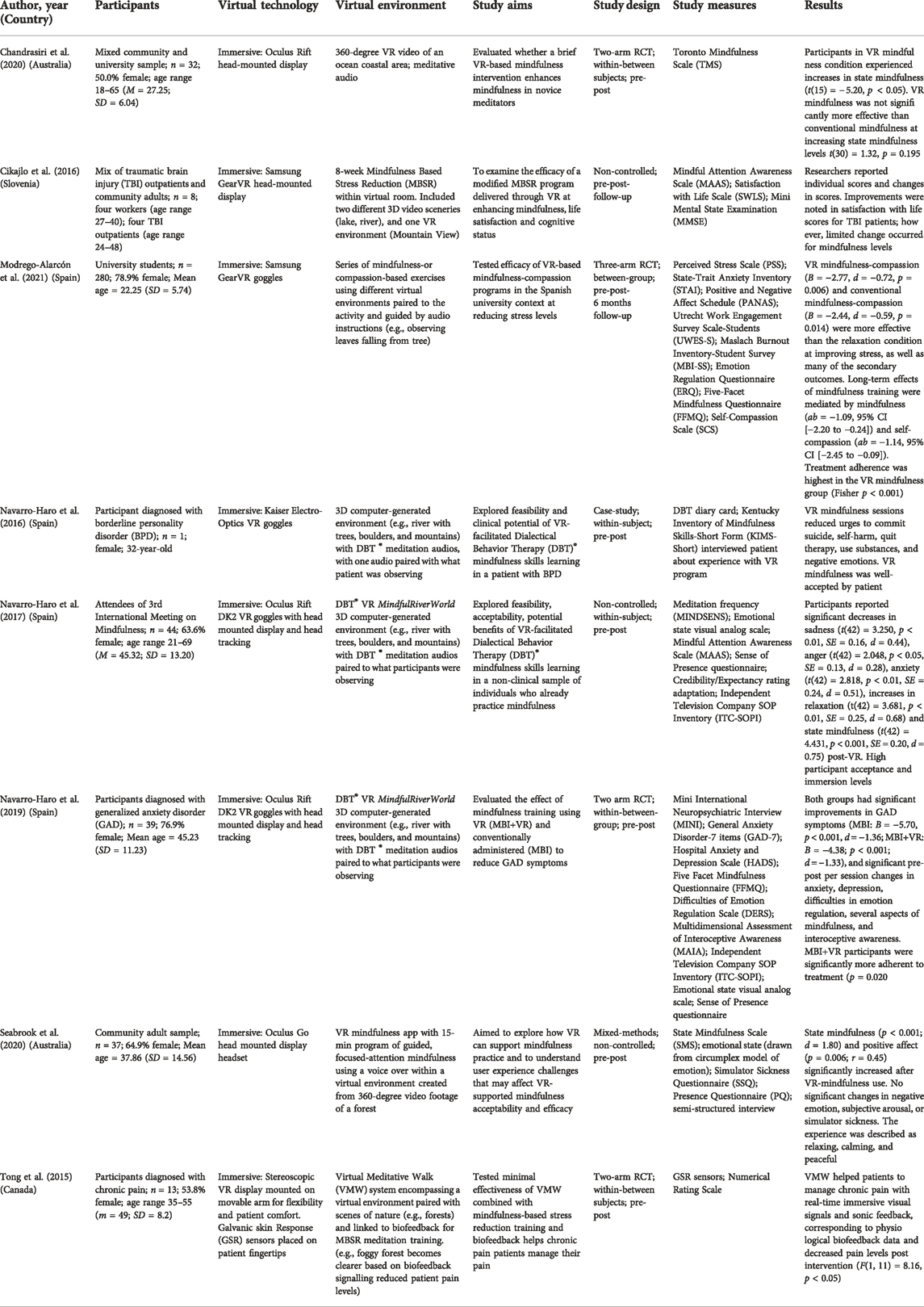
TABLE 3. Examples of empirical studies of mindfulness-based VR interventions for mental health and well-being.
Comparable to mindfulness, there are many differing conceptualizations of self-compassion from both eastern and western perspectives (Khoury, 2019). As a practice, self-compassion originates from Buddhist traditions (Shonin et al., 2014) and was introduced to western psychology and research by clinical psychologist Paul Gilbert and research psychologist Kristin Neff (Neff, 2003; Neff, 2004; Gilbert, 2006). There is much debate regarding the definition and measurement of self-compassion (Muris et al., 2016; Cleare et al., 2018; Coroiu et al., 2018) and issues regarding a lack of a conceptualization that includes both the eastern Buddhist origins and western definitions (Davidson et al., 2002; Muris et al., 2016; Strauss et al., 2016; Zeng et al., 2016). While a full review of self-compassion and its Buddhist and westernized conceptualizations is beyond this paper, it is important to be aware of the influence that Buddhist concepts have had on the interpretation of self-compassion in western psychological science. Following a westernized conceptualization, self-compassion can be described as relating to oneself with a kind and forgiving attitude (Neff & Vonk, 2009) and involves noticing distress, as well as building understanding that one’s suffering is part of the human condition (Neff, 2003).
As previously described, embodiment in the context of VR refers to the illusion that an individual’s real body is the life-sized virtual body that is observable to them in the virtual environment (Slater et al., 2010; Petkova et al., 2011). Embodiment appears to alter physiological and psychological perspectives. For example, shifting an individual’s perception of the size of their body (e.g., adults believing their body is the size of a simulated child’s body) as well as modifying racial attitudes when perceiving embodiment in a simulated body with a different skin color than the VR user’s actual body (Banakou et al., 2013; Peck et al., 2013; Martini et al., 2014; Maister et al., 2015). It is theorized that virtual embodiment may enhance self-compassion in individuals with elevated levels of self-criticism (Falconer et al., 2014) and research is beginning to investigate the effects of embodying virtual adult and child bodies, and interacting compassionately with those bodies, on decreasing self-criticism and depressive symptoms (Baghaei et al., 2019; Falconer et al., 2016; Falconer et al., 2014). Cebolla and others (2019) highlights the importance of imagery skills in self-compassion, as many techniques for increasing compassion in therapeutic settings require mental imagery abilities that induce and train positive mental states (Pearson et al., 2013; Cebolla et al., 2019). If individuals struggle to maintain imagery during meditative compassion-practice this can lead to challenges reaching feelings of compassion and can discourage participants from continuing with the necessary training needed to foster compassion-based skills and positive qualities (Cebolla et al., 2019). To overcome attrition related to lack of ability to sustain mental imagery, VR can be very useful as it enables the construction, maintenance, inspection, and transformation of mental images and can be considered an advanced imagery system that is as effective as reality at inducing emotional, cognitive, and behavioral responses (Day et al., 2004). Self-compassion training via VR programs could be especially useful for aging populations (Tavares et al., 2020). In particular, given research indicating that older adults may respond to gradual deterioration in physical and cognitive resources with self-criticism by blaming themselves for these natural age-related changes, and experiencing elevated levels of regret, rumination, and negative affect (Baltes & Smith, 2003; Laidlaw et al., 2003; Casey, 2012). Conscientious development of gerontechnology interventions is once again crucial here. If done well, technological interventions targeting and developed in partnership with older adults may increase both general levels of compassionate service delivery, as well as users’ self-compassion levels (Fozard, 2012; Schmitter-Edgecombe et al., 2013). Teaching self-compassion in a setting that facilitates easier practice, such as VR, could be beneficial for the adoption of attitudes of kindness towards oneself and the effects of aging.
Self-compassion interventions, or compassion-based interventions (CBIs), can be described as interventions that focus on cultivating compassion towards self and others through psycho-education, training and promotion of practices that enhance compassion (Kirby, 2017). CBIs have been linked to a variety of improvements in psychological health outcomes. Research has found CBIs to be effective at decreasing stress, anxiety, and depression (Kirby et al., 2017), and increasing compassion and empathy (Brito et al., 2018). A meta-analysis by Kirby and others (2017) investigated 21 RCT studies of CBIs and found significant short-term moderate effect sizes for life satisfaction, happiness, and decreased anxiety and depression. Additionally, small-to-moderate effects were found for psychological distress. However, a need for increased rigor in study design, as well as reporting, was identified for future studies of CBIs. Ferrari et al. (2019) conducted a more recent meta-analysis of 27 RCTs regarding the effects of CBIs on psychosocial outcomes and found large effects for rumination and eating behavior, and moderate effects for depression, anxiety, stress, self-criticism, mindfulness and self-compassion. Despite these promising findings, study inclusion criteria were based on a specifically western-lens following Neff’s (2003) model of self-compassion. Future research assessing the efficacy of CBIs based on different models of self-compassion is needed given the debates over its conceptualization and operationalization (Khoury, 2019).
Furthermore, large-scale meta-analyses have linked the construct of self-compassion to enhanced well-being and reduced psychopathology in adults and adolescents (MacBeth & Gumley, 2012; Zessin et al., 2015; Marsh et al., 2018). Additionally, self-compassion shows potential for promoting resilience in the face of significant life stressors such as chronic health issues (e.g., Brion et al., 2014), divorce (e.g., Sbarra et al., 2012), parenting a child with a developmental disorder (e.g., Wong et al., 2016), and combat (e.g., Hiraoka et al., 2015). Notably, in two cross-sectional studies by Allen and others (2012) of adults aged 67–90 years old, self-compassion was found to positively moderate the relationship between physical health and psychological well-being. This moderating effect was particularly strong for older adults in poorer health, indicating that self-compassion may be especially useful for improved quality of life in aging populations with health challenges and could be a crucial component of successful aging (Rowe & Kahn, 1987; Allen et al., 2012; Rowe & Kahn, 2015). In a systematic review and meta-analysis of 11 studies by Brown and others (2019) of the effects of self-compassion on the older adult aging process, it was found that self-compassion was associated with decreased symptoms of depression and anxiety and increased psychological well-being. Meta-analytic findings indicated that self-compassion moderated the relationship between health problems and well-being (Brown et al., 2019), corroborating the findings of Allen et al. (2012). Overall, Brown et al. (2019) concluded that self-compassion is a promising resilience promoter for older adults. However, their search did not include qualitative studies, conference abstracts, or materials that were not published in English, limiting the breadth and depth of their findings, as well as the generalizability. Tavares and others (2020) conducted a scoping review of the self-compassion research base as it relates to psychological well-being of the older adult population. There were no restrictions on study design, or setting, so long as research was conducted with adults aged 60 or older, or with a mean age of 65 or older, and measured self-compassion and psychological adjustment (e.g., life satisfaction, depression or anxiety symptoms). Their review resulted in 12 studies, 1 qualitative and 11 mixed-methods design and found that self-compassion appears to be a valuable resource for older adult psychological adjustment and may promote resilience connected to age related challenges. All studies analyzed were cross-sectional therefore limiting the ability to draw meaningful conclusions from their findings. Another notable weakness of this review was the authors choice to exclude studies with compassion towards others as an outcome. This could limit the validity of the review’s findings, given the considerable theoretical overlap between compassion directed to the self (self-compassion) and compassion directed towards others (compassion).
Despite the findings from exploratory data and reviews linking the construct of self-compassion to improved well-being in older adults, there appear to be very few published studies examining the effects of CBIs on an exclusively older adult population. To this end, only one study was found when performing the literature search for this review. Perez-Blasco et al. (2016) examines the effects of a mixed mindfulness and compassion intervention for stress management in 45 healthy, community-based older adults aged 60 or older. Participants were randomly assigned to either the mindfulness-compassion intervention group or to a treatment as usual (TAU) control group. Each intervention session was 120 min long and there were 10 sessions in total. Findings suggest the synergistic benefits of combining mindfulness with self-compassion in interventions for older adults as compared to TAU. Study limitations include the small sample size and lack of follow-up data collection, restricting the ability to verify whether these are lasting improvements. As well, all participants were healthy, non-clinical older adults; therefore, it is unclear whether these findings would hold in older adults with health challenges such as cognitive decline. Further research in this area is clearly warranted given the potentially significant benefits for the aging process of older adults.
The research base of studies investigating VR-based CBIs is currently at a rudimentary stage. Findings from this review revealed six completed studies using VR to train self-compassion (Falconer et al., 2014; Holden, 2015; Falconer et al., 2016; Cebolla et al., 2019; Brown et al., 2020; Modrego-Alarcón et al., 2021) with an additional three protocol studies in existence (Baghaei et al., 2019; Baghaei et al., 2020; Baghaei et al., 2021). Perhaps the most influential study examining VR-based compassion training was conducted by Falconer et al., 2016. Designed based on the concept of virtual embodiment, this experimental study investigated an 8-min scenario where 15 participants with diagnosed depression practiced delivering compassion in one virtual body and then receiving it from themselves in a different virtual body (Falconer et al., 2016). The authors reported significant improvements in self-compassion and significant decreases in depression and self-criticism as a result of the experiment. Study limitations include the small number of participants, lack of control condition, repetition of one immersive VR scenario and a predominantly white, westernized sample. This study has led to further experimental studies investigating similar design paradigms to that of Falconer et al., 2016. In a recently published RCT by Modrego-Alarcón et al. (2021), the effects of a combined mindfulness and compassion intervention using VR were investigated in 280 university students. Students were assigned to one of three groups: “Mindfulness-based Programme” (MBP); “MBP + VR”; or “Relaxation.” The MBP focused on two central components: mindfulness and self-compassion. Sessions were 90-min in length and were held in groups at a frequency of once per week for 6 weeks. It was found that both MBP and MBP+VR were superior to Relaxation for reducing stress, with medium-to-large effects found at post and follow-up. Notably, treatment adherence (i.e., retention rates and class session attendance) was significantly higher in the MBP+VR group, building support for the hypothesis that VR could be particularly effective at reducing attrition in MBIs and interventions in general (Slater et al., 1994; Navarro-Haro et al., 2017). Similar to Perez-Blasco et al., 2016, this study highlights the additive potential of combining MBIs and CBIs for improving well-being outcomes. Some limitations in this study include that previous familiarity with mindfulness and compassion was not assessed, nor was frequency of home practice during the intervention. Additionally, some analyses were underpowered. Finally, this study used an exclusively university student sample, making its findings difficult to generalize. Despite methodological weaknesses, findings for CBIs using VR appear to be promising; however, consistent with the level of existing research for in vivo CBIs for older adults, no studies investigating the effects of VR-based compassion training for older adults appear to have been published, to-date. Findings from VR-based CBI studies are summarized in Table 4 according to reference, sample, VR technology, VR environment, aims, design, measures, and results.
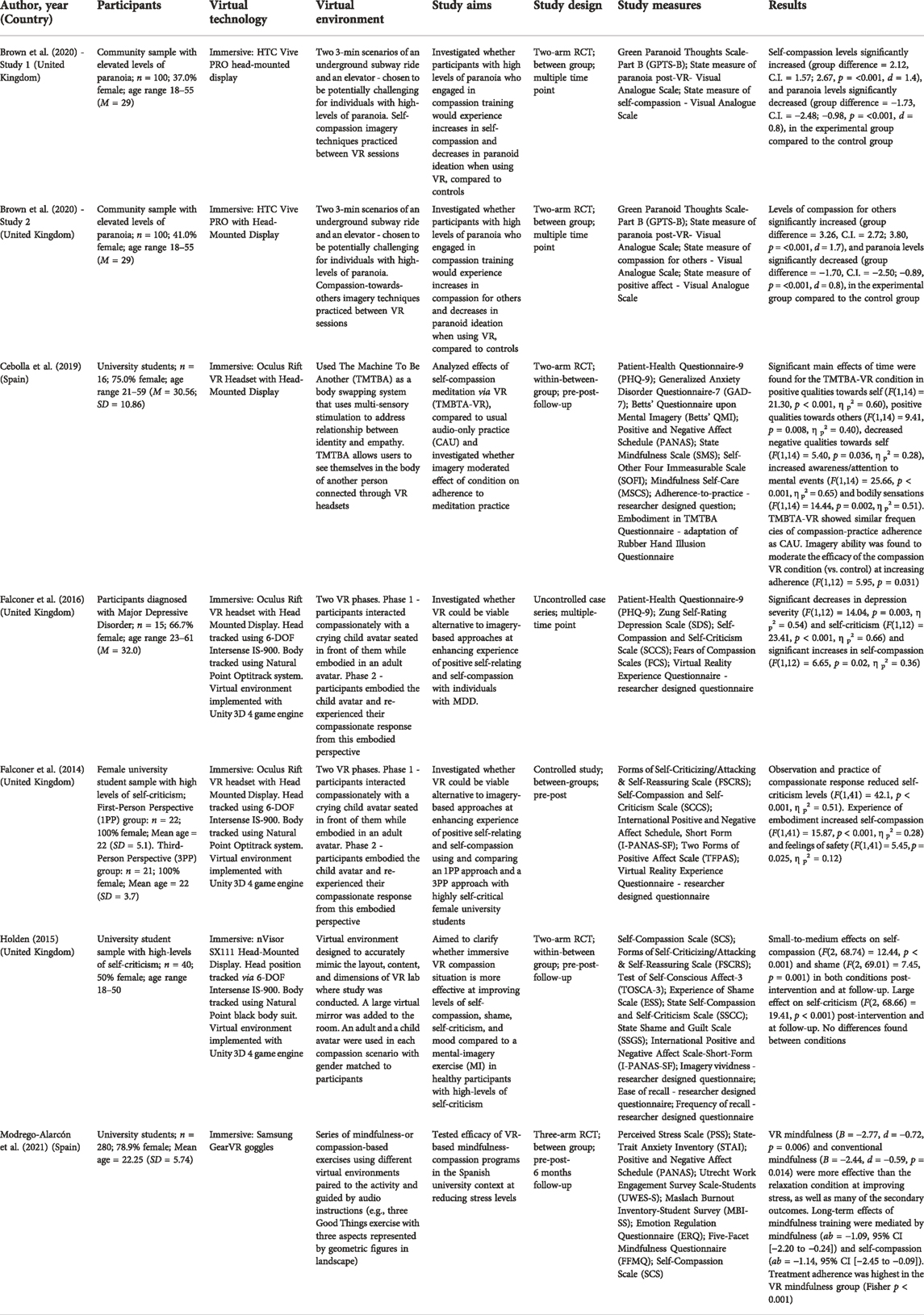
TABLE 4. Examples of empirical studies of compassion-based VR interventions for mental health and well-being.
Given the rapid aging of the global population, there is an increased need for effective and preventative health interventions in an age group that already has the highest rate of healthcare requirements and costs (GC, 2014; UN DESA, 2014; WHO, 2017). It is especially important to increase support for the significant portion of older adults experiencing mental and cognitive health conditions (Karel et al., 2012), due to their higher rates of comorbid physical and mental health conditions (Bartels et al., 2003; Gum et al., 2009; IOM, 2012) and the lower rate of mental health service access found among geriatric populations (Klap et al., 2003; Wang et al., 2005; Karlin et al., 2008; Bogner et al., 2009; MHF, 2018). To enhance the likelihood of successful aging, interventions should focus on pathways to increasing cognitive, physical, and psychological functioning, and decreasing disease-related disability through emphasizing active involvement and interest in life (Rowe & Kahn, 1997), while also accounting for cultural differences, chronic health issues, and socio-economic status barriers that may decrease the efficacy of certain interventions designed for WEIRD populations (Martinson & Berridge, 2015; Rowe & Kahn, 2015).
Growing evidence supports the importance of gerontechnology as an essential determinant to healthy aging and quality of life of older adults (Bouma et al., 2009). Gerontechnology has the potential to facilitate older adults’ active participation in the healthy aging process and may benefit communication, health, mobility, work, housing, recreation, and self-fulfillment (Fozard et al., 2000). However, for its effective uptake, older adults need to perceive gerontechnology to be useful, as well as easy to use (Davis, 1989; Zhou et al., 2020). Therefore, technological solutions need to bridge the generational gap of technology use, instead of widening it. Additionally, further emphasis is needed on the research and development of gerontechnology for mental health, given the bias toward physical health-related technological support. Effective technological interventions for older adults should account for challenges and barriers commonly expressed by older adults and should be designed for easy use, increased social contact, fit with daily routines, and include access to straightforward, regular interactions with health providers, if needed (Jimison et al., 2008; Kang et al., 2010; Seifert et al., 2019). Despite its relatively recent introduction to the mainstream market, VR has the potential to be readily accepted by older adults due to its benefits compared to conventional treatments, such as accessibility, functionality, patient interaction with therapeutic stimuli, quicker positive health impacts, and safety conditions (Cherniack, 2011; Mohr et al., 2013; Robert et al., 2016; Benham et al., 2019; Montana et al., 2020). VR shows promise as a gerontechnology intervention; however, high quality empirical literature is currently limited and further research of its applications, feasibility and efficacy is needed. Additionally, component analyses of the mechanisms through which VR may improve well-being, as well as specific design elements that facilitate better outcomes, are important for clarification of the evidence-base and for the creation of optimally effective interventions.
Taken together, the research base is extremely sparse and sometimes non-existent with respect to VR-based nature interventions, MBIs, or CBIs for older adults, and is even more narrow in the area of older adult mental health and well-being. For instance, based on findings from this review, no study to-date has investigated MBIs or CBIs using VR for older adults and the studies examining nature-based VRs are very few and often methodologically weak. Of the research available, VR for older adults demonstrates potential as an intervention to enhance well-being, but there are significant methodological flaws that must be addressed in order to clarify the evidence base and create effective interventions (e.g., Dermody et al., 2020; Yen & Chiu, 2021). In general populations, nature-based, mindfulness and compassion VR interventions show promise for effectiveness at improving mental health and well-being outcomes (e.g., Falconer et al., 2016; Jerdan et al., 2018; Chandrasiri et al., 2020; Modrego-Alarcón et al., 2021). Currently, no study has investigated a VR-based combined mindfulness-compassion intervention incorporating natural settings for older adults. Given the pathways through which nature, mindfulness, and compassion interventions operate, it is likely that combining these interventions using VR could lead to improved resilience and well-being outcomes, such as mood and quality-of-life, and decreased symptoms of psychopathology. Additionally, a combined nature-mindfulness-compassion program based in VR could further enhance adherence and acceptability of mental health interventions for older adults, given preliminary findings indicating that VR: 1) appears to be an effective method for improving mindfulness, compassion, and nature-based intervention adherence, and 2) shows acceptability for older adults when administered under the right conditions (Zhou et al., 2020). Therefore, there is a need for studies with robust designs explicitly investigating nature interventions, MBIs, and CBIs for older adults, as well as interventions combining these three approaches, in addition to interventions integrating these approaches using VR technology, given their potential to improve quality-of-life and quality-of-care in soon to be the largest proportion of the population. Due to the prospective benefits, further clarification is warranted regarding the mechanisms contributing to the efficacy of VR-based nature interventions, MBIs and CBIs. Additionally, large-scale studies employing rigorous longitudinal RCT designs in cross-cultural and clinical populations are needed to better understand the effectiveness of VR interventions compared to non-VR interventions for mental health and well-being.
Despite the evidence base for older adults still requiring further development, nature, mindfulness, compassion, and VR-based interventions all have support for general population mental health and well-being, in both clinical and non-clinical populations. Key implications for practice with geriatric populations include facilitating access to effective and engaging mental health interventions by clarifying the efficacy of VR-based psychological interventions for older adults, as robust research will be instrumental for effective preventative mental health care for a population in need of this type of programming. Additionally, collecting information on the feasibility, acceptability, and effectiveness of VR for older adults will deliver vital information regarding users’ needs in the burgeoning field of digital therapeutics. Current evidence suggests that both nature-based interventions and MBIs improve emotional well-being and physical health among nonclinical community-dwelling samples of older adults. There is currently not enough research examining the efficacy of CBIs for older adults, but research examining positive associations between self-compassion as a construct and mental health outcomes suggests potential utility for CBIs in geriatric populations. Clearly, further empirical intervention studies are needed in this area. Additionally, mental health support programs that combine nature, mindfulness and compassion show promise given the connections between these constructs and their additive effects on psychological well-being in various older adult populations. Furthermore, despite the early stages of the research base, VR-based interventions appear to be a feasible and effective type of gerontechnology for both physical and psychological outcomes. Limitations to VR access should not be forgotten, there are currently technological, physical, and financial barriers, and a dearth of research examining these specific barriers in VR design and studies. Additionally, given the research focus on WEIRD populations, it is unclear to what extent VR intervention efficacy could be globally generalized. Continuing to find ways to incorporate gerontechnology that promote acceptability amongst older adults is key in order for these interventions to have ecological validity. Whenever possible, gerontechnology interventions should be developed with the input of older adults and specifically targeted to their needs.
In summary, this review has evaluated the strengths, limitations, and potential of VR as a gerontechnology that enhances mental health and well-being. Research examining VR-based interventions that incorporate elements of nature, mindfulness, and compassion has major scholarly, technological and health implications. In particular, clinical interventions in this area have the potential to provide older adults with alternative, accessible, engaging, and safe care options. However, the current state of the field highlights the need for rigorously designed, applied studies that investigate the use of VR-based mindfulness, compassion and nature programs for older adult mental health and well-being. This is especially important given the increasing necessity for attention to the mental health needs of the older adult population, who will soon make up the majority of the global population.
All authors listed have made direct, substantial, and intellectual contribution to the work, and approved it for publication.
IS is supported in part by funding from the Social Sciences and Humanities Research Council of Canada [Canada Graduate Scholarships—Doctoral] and Mitacs Accelerate [grant number IT24016].
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Aarts, S., Peek, S. T. M., and Wouters, E. J. M. (2015). The relation between social network site usage and loneliness and mental health in community‐dwelling older adults. Int. J. Geriatr. Psychiatry 30 (9), 942–949. doi:10.1002/gps.4241
Aerts, R., Honnay, O., and Van Nieuwenhuyse, A. (2018). Biodiversity and human health: Mechanisms and evidence of the positive health effects of diversity in nature and green spaces. Br. Med. Bull. 127 (1), 5–22. doi:10.1093/bmb/ldy021
Allen, A. B., Goldwasser, E. R., and Leary, M. R. (2012). Self-compassion and well-being among older adults. Self Identity 11 (4), 428–453. doi:10.1080/15298868.2011.595082
Anderson, A. P., Mayer, M. D., Fellows, A. M., Cowan, D. R., Hegel, M. T., and Buckey, J. C. (2017). Relaxation with immersive natural scenes presented using virtual reality. Aerosp. Med. Hum. Perform. 88 (6), 520–526. doi:10.3357/amhp.4747.2017
Annerstedt, M., Jönsson, P., Wallergård, M., Johansson, G., Karlson, B., Grahn, P., et al. (2013). Inducing physiological stress recovery with sounds of nature in a virtual reality forest—Results from a pilot study. Physiol. Behav. 118, 240–250. doi:10.1016/j.physbeh.2013.05.023
Baez, M., Far, I. K., Ibarra, F., Ferron, M., Didino, D., and Casati, F. (2017). Effects of online group exercises for older adults on physical, psychological and social wellbeing: A randomized pilot trial. PeerJ 5, e3150. doi:10.7717/peerj.3150
Baghaei, N., Hach, S., Khaliq, I., Stemmet, L., Krishnan, J., Naslund, J., et al. (20192019). IEEE international symposium on mixed and augmented reality adjunct (ISMAR-Adjunct). IEEE, 404–407.Increasing self-compassion inyoung people through virtual Real.
Baghaei, N., Stemmet, L., Hlasnik, A., Emanov, K., Hach, S., Naslund, J. A., et al. (2020). “Time to get personal: Indivi,” in Extended Abstracts of the 2020 CHI conference on human factors in computing systems, 1–9.dualised Virtual Real. Ment. Health
Baghaei, N., Stemmet, L., Khaliq, I., Ahmadi, A., Halim, I., Liang, H. N., et al. (2021). “Designing individualised vi,” in Companion of the 2021 ACM SIGCHI symposium on engineering interactive computing systems, 6–11.rtual Real. Appl. Supporting Depress. A Feasibility Study
Baker, S., Warburton, J., Waycott, J., Batchelor, F., Hoang, T., Dow, B., et al. (2018). Combatting social isolation and increasing social participation of older adults through the use of technology: A systematic review of existing evidence. Australas. J. Ageing 37 (3), 184–193. doi:10.1111/ajag.12572
Ball, K., Berch, D. B., Helmers, K. F., Jobe, J. B., Leveck, M. D., Marsiske, M., et al. ACTIVE Study Group (2002). Effects of cognitive training interventions with older adults: A randomized controlled trial. JAMA 288 (18), 2271–2281. doi:10.1001/jama.288.18.2271
Ballesteros, S., Mayas, J., Prieto, A., Toril, P., Pita, C., Laura, P. D. L., et al. (2015). A randomized controlled trial of brain training with non-action video games in older adults: Results of the 3-month follow-up. Front. Aging Neurosci. 7, 45. doi:10.3389/fnagi.2015.00045
Baltes, P. B., and Smith, J. (2003). New frontiers in the future of aging: From successful aging of the young old to the dilemmas of the fourth age. Gerontology 49 (2), 123–135. doi:10.1159/000067946
Banakou, D., Groten, R., and Slater, M. (2013). Illusory ownership of a virtual child body causes overestimation of object sizes and implicit attitude changes. Proc. Natl. Acad. Sci. U. S. A. 110 (31), 12846–12851. doi:10.1073/pnas.1306779110
Baños, R. M., Etchemendy, E., Castilla, D., García-Palacios, A., Quero, S., and Botella, C. (2012). Positive mood induction procedures for virtual environments designed for elderly people. Interact. Comput. 24 (3), 131–138. doi:10.1016/j.intcom.2012.04.002
Barlow, J., Singh, D., Bayer, S., and Curry, R. (2007). A systematic review of the benefits of home telecare for frail elderly people and those with long-term conditions. J. Telemed. Telecare 13 (4), 172–179. doi:10.1258/135763307780908058
Bartels, S. J., Clark, R. E., Peacock, W. J., Dums, A. R., and Pratt, S. I. (2003). Medicare and medicaid costs for schizophrenia patients by age cohort compared with costs for depression, dementia, and medically ill patients. Am. J. Geriatr. Psychiatry 11, 648–657. doi:10.1097/00019442-200311000-00009
Bartels, S. J., and Naslund, J. A. (2013). The underside of the silver tsunami—Older adults and mental health care. N. Engl. J. Med. Overseas. Ed. 368 (6), 493–496. doi:10.1056/nejmp1211456
Benham, S., Kang, M., and Grampurohit, N. (2019). Immersive virtual reality for the management of pain in community-dwelling older adults. OTJR Occup. participation health 39 (2), 90–96. doi:10.1177/1539449218817291
Benoit, M., Guerchouche, R., Petit, P. D., Chapoulie, E., Manera, V., Chaurasia, G., et al. (2015). Is it possible to use highly realistic virtual reality in the elderly? A feasibility study with image-based rendering. Neuropsychiatr. Dis. Treat. 11, 557–563. doi:10.2147/ndt.s73179
Bercovitz, K., and Pagnini, F. (2016). “Mindfulness as an opportunity to narrow the grey digital divide,” in Integrating technology in positive psychology practice. Editors D. Villani, P. Cipresso, A. Gaggioli, and G. Riva, 214–228. IGI Global Available at: http://doi.org/10.4018/978-1-4666-9986-1.ch009.
Bickmore, T. W., Silliman, R. A., Nelson, K., Cheng, D. M., Winter, M., Henault, L., et al. (2013). A randomized controlled trial of an automated exercise coach for older adults. J. Am. Geriatr. Soc. 61, 1676–1683. doi:10.1111/jgs.12449
Bisson, E., Contant, B., Sveistrup, H., and Lajoie, Y. (2007). Functional balance and dual-task reaction times in older adults are improved by virtual reality and biofeedback training. Cyberpsychology Behav. 10 (1), 16–23. doi:10.1089/cpb.2006.9997
Bixler, R. D., and Floyd, M. (1999). Hands on or hands off? Disgust sensitivity and preference for environmental education activities. J. Environ. Educ. 30 (3), 4–11. doi:10.1080/00958969909601871
Bodhi, B. (2011). What does mindfulness really mean? A canonical perspective. Contemp. Buddhism 12 (1), 19–39. doi:10.1080/14639947.2011.564813
Bogner, H. R., de Vries, H. F., Maulik, P. K., and Unu ̈tzer, J. (2009). Mental health services use: Baltimore epidemiologic catchment area follow- up. Am. J. Geriatric Psychiatry 17, 706–715. doi:10.1097/JGP.0b013e3181aad5c5
Bornioli, A., Parkhurst, G., and Morgan, P. L. (2019). Affective experiences of built environments and the promotion of urban walking. Transp. Res. Part A Policy Pract. 123, 200–215. doi:10.1016/j.tra.2018.12.006
Bornioli, A., Parkhurst, G., and Morgan, P. L. (2018). Psychological wellbeing benefits of simulated exposure to five urban settings: An experimental study from the pedestrian’s perspective. J. Transp. Health 123, 105–116. doi:10.1016/j.jth.2018.02.003
Bouma, H., Fozard, J. L., and Bronswijk, J. E. M. H. Van. (2009). Gerontechnology as a field of endeavour. Gerontechnology 8 (2), 68–75. doi:10.4017/gt.2009.08.02.004.00
Brimelow, R. E., Dawe, B., and Dissanayaka, N. (2020). Preliminary research: Virtual reality in residential aged care to reduce apathy and improve mood. Cyberpsychology, Behav. Soc. Netw. 23 (3), 165–170. doi:10.1089/cyber.2019.0286
Brion, J. M., Leary, M. R., and Drabkin, A. S. (2014). Self-compassion and reactions to serious illness: The case of HIV. J. Health Psychol. 19 (2), 218–229. doi:10.1177/1359105312467391
Brito, G., Campos, D., and Cebolla, A. (2018). Implicit or explicit compassion? Efficacy of a compassion-based intervention and comparison with mindfulness- based stress reduction intervention on empathy and compassion. Mindfulness 9, 1494–1508. doi:10.1007/s12671-018-0898-z
Broadbent, E., Peri, K., Kerse, N., Jayawardena, C., Kuo, I., Datta, C., et al. (2014). “Robots in older people's homes to improve medication adherence and quality of life: A randomised cross-over trial,” in Social robotics: International conference on social robotics; presented at: Social robotics 6th international conference (Sydney, Australia, 64–73.
Brown, K. W., Ryan, R. M., and Creswell, J. D. (2007). Mindfulness: Theoretical foundations and evidence for its salutary effects. Psychol. Inq. 18 (4), 211–237. doi:10.1080/10478400701598298
Brown, L., Huffman, J. C., and Bryant, C. (2019). Self-compassionate aging: A systematic review. Gerontologist 59 (4), e311–e324. doi:10.1093/geront/gny108
Brown, P., Waite, F., Rovira, A., Nickless, A., and Freeman, D. (2020). Virtual reality clinical-experimental tests of compassion treatment techniques to reduce paranoia. Sci. Rep. 10 (1), 8547–8549. doi:10.1038/s41598-020-64957-7
Browning, M. H., Mimnaugh, K. J., van Riper, C. J., Laurent, H. K., and LaValle, S. M. (2020). Can simulated nature support mental health? Comparing short, single-doses of 360-degree nature videos in virtual reality with the outdoors. Front. Psychol. 10, 2667. doi:10.3389/fpsyg.2019.02667
Browning, M., Stern, M., Ardoin, N. M., Heimlich, J. E., Petty, R., and Charles, C. (2017). Investigating the sets of values that community members hold toward local nature centers. Environ. Educ. Res. 23, 1291–1306. doi:10.1080/13504622.2016.1177713
Bruun-Pedersen, J. R., Pedersen, K. S., Serafin, S., and Kofoed, L. B. (2014). 2nd workshop on virtual and augmented assistive technology. New York, NY: VAAT, 23–27. doi:10.1109/VAAT.2014.6799464Augmented exercise biking with virtual environments for elderly users: A preliminary study for retirement home physical therapy
Bruun-Pedersen, J. R., Serafin, S., and Kofoed, L. B. (2016). “Going outside while staying inside-exercise motivation with immersive vs. non-immersive recreational virtual environment augmentation for older adult nursing home residents,” in Proceedings - 2016 IEEE international conference on healthcare informatics (New York, NY: ICHI), 216–226. doi:10.1109/ICHI.2016.31
Buyl, R., Beogo, I., Fobelets, M., Deletroz, C., Van Landuyt, P., Dequanter, S., and Gagnon, M. P. (2020). e-Health interventions for healthy aging: a systematic review. Syst. Rev. 9 (128), 1–15. doi:10.1186/s13643-020-01385-8
Byers, A. L., Yaffe, K., Covinsky, K. E., Friedman, M. B., and Bruce, M. L. (2010). High occurrence of mood and anxiety disorders among older adults. Arch. Gen. Psychiatry 67, 489–496. doi:10.1001/archgenpsychiatry.2010.35
Calogiuri, G., Litleskare, S., Fagerheim, K. A., Rydgren, T. L., Brambilla, E., and Thurston, M. (2018). Experiencing nature through immersive virtual environments: Environmental perceptions, physical engagement, and affective responses during a simulated nature walk. Front. Psychol. 8, 2321. doi:10.3389/fpsyg.2017.02321
Calvo, R. A., and Peters, D. (2013). Promoting psychological wellbeing: Loftier goals for new technologies [opinion]. IEEE Technol. Soc. Mag. 32 (4), 19–21. doi:10.1109/MTS.2013.2286429
Cangelosi, P. R., and Sorrell, J. M. (2014). Use of technology to enhance mental health for older adults. J. Psychosoc. Nurs. Ment. Health Serv. 52 (9), 17–20. doi:10.3928/02793695-20140721-01
Capaldi, C. A., Dopko, R. L., and Zelenski, J. M. (2014). The relationship between nature connectedness and happiness: A meta-analysis. Front. Psychol. 5, 976. doi:10.3389/fpsyg.2014.00976
Carletto, S., Cavalera, C., Sadowski, I., Rovaris, M., Borghi, M., Khoury, B., et al. (2020). Mindfulness-based interventions for the improvement of well-being in people with multiple sclerosis: A systematic review and meta-analysis. Psychosom. Med. 82 (6), 600–613. doi:10.1097/psy.0000000000000819
Carrière, K., Khoury, B., Günak, M., and Knäuper, B. (2018). Mindfulness-based interventions for weight loss: A systematic review and meta-analysis. Obes. Rev. 19 (2), 164–177. doi:10.1111/obr.12623
Casey, D. A. (2012). Depression in the elderly: A review and update. Asia-Pacific Psychiatry 4 (3), 160–167. doi:10.1111/j.1758-5872.2012.00191.x
Cebolla, A., Herrero, R., Ventura, S., Miragall, M., Bellosta-Batalla, M., Llorens, R., et al. (2019). Putting oneself in the body of others: A pilot study on the efficacy of an embodied virtual reality system to generate self-compassion. Front. Psychol. 10, 1521. doi:10.3389/fpsyg.2019.01521
Chan, J. S., Deng, K., Wu, J., and Yan, J. H. (2019). Effects of meditation and mind–body exercises on older adults’ cognitive performance: A meta-analysis. Gerontologist 59 (6), e782–e790. doi:10.1093/geront/gnz022
Chandrasiri, A., Collett, J., Fassbender, E., and De Foe, A. (2020). A virtual reality approach to mindfulness skills training. Virtual Real. 24 (1), 143–149. doi:10.1007/s10055-019-00380-2
Chang, S. J., and Im, E. O. (2014). A path analysis of Internet health information seeking behaviors among older adults. Geriatr. Nurs. 35, 137–141. doi:10.1016/j.gerinurse.2013.11.005
Chen, Y. R. R., and Schulz, P. J. (2016). The effect of information communication technology interventions on reducing social isolation in the elderly: A systematic review. J. Med. Internet Res. 18 (1), e18. doi:10.2196/jmir.4596
Cherniack, E. P. (2011). Not just fun and games: Applications of virtual reality in the identification and rehabilitation of cognitive disorders of the elderly. Disabil. rehabilitation Assistive Technol. 6 (4), 283–289. Available at: http://www.tandfonline.com/doi/full/10.3109/17483107.2 010.542570.
Chung, K., Lee, D., and Park, J. Y. (2018). Involuntary attention restoration during exposure to mobile-based 360 virtual nature in healthy adults with different levels of restorative experience: Event-related potential study. J. Med. Internet Res. 20 (11), e11152. doi:10.2196/11152
Ciechanowski, P., Wagner, E., Schmaling, K., Schwartz, S., Williams, B., Diehr, P., et al. (2004). Community-integrated home-based depression treatment in older adults: A randomized controlled trial. JAMA 291 (13), 1569–1577. doi:10.1001/jama.291.13.1569
Cikajlo, I., Čižman-Štaba, U., Vrhovac, S., Larkin, F., and Roddy, M. (2016). “Recovr: Realising collaborativ,” in Proceedings of the 3rd IASTED international conference telehealth assistive technology TAT, 11–17.e virtual Real. wellbeing self-healing
Cleare, S., Gumley, A., Cleare, C. J., and O’Connor, R. C. (2018). An investigation of the factor structure of the Self-Compassion Scale. Mindfulness 9 (2), 618–628. doi:10.1007/s12671-017-0803-1
Cocosila, M., Archer, N., Haynes, R. B., and Yuan, Y. (2009). Can wireless text messaging improve adherence to preventive activities? Results of a randomised controlled trial. Int. J. Med. Inf. 78, 230–238. doi:10.1016/j.ijmedinf.2008.07.011
Coroiu, A., Kwakkenbos, L., Moran, C., Thombs, B., Albani, C., Bourkas, S., et al. (2018). Structural validation of the Self-Compassion Scale with a German general population sample. PLoS One 13 (2), e0190771. doi:10.1371/journal.pone.0190771
Cotten, S. R., Anderson, W. A., and McCullough, B. M. (2013). Impact of internet use on loneliness and contact with others among older adults: Cross-sectional analysis. J. Med. Internet Res. 15 (2), e39. doi:10.2196/jmir.2306
Crabb, R. M., Rafie, S., and Weingardt, K. R. (2012). Health-related Internet use in older primary care patients. Gerontology 58, 164–170. doi:10.1159/000329340
Davidson, R. J., James, W., and Harrington, A. (2002). Visions of compassion: Western scientists and Tibetan Buddhists examine human nature. New York, NY: Oxford University Press.
Davis, F. D. (1989). Perceived usefulness, perceived ease of use, and user acceptance of information technology. MIS Q. 13, 319–340. doi:10.2307/249008
Day, S. J., Holmes, E. A., and Hackmann, A. (2004). Occurrence of imagery and its link with early memories in agoraphobia. Memory 12, 416–427. doi:10.1080/09658210444000034
Dear, B. F., Zou, J. B., Ali, S., Lorian, C. N., Johnston, L., Sheehan, J., et al. (2015b). Clinical and cost-effectiveness of therapist-guided internet-delivered cognitive behavior therapy for older adults with symptoms of anxiety: A randomized controlled trial. Behav. Ther. 46 (2), 206–217. doi:10.1016/j.beth.2014.09.007
Dear, B. F., Zou, J. B., Ali, S., Lorian, C. N., Johnston, L., Terides, M. D., et al. (2015a). Examining self-guided internet-delivered cognitive behavior therapy for older adults with symptoms of anxiety and depression: Two feasibility open trials. Internet Interv. 2 (1), 17–23. doi:10.1016/j.invent.2014.11.002
Depledge, M. H., Stone, R. J., and Murphy, A. (2011). Can natural and virtual environments be used to promote improved human health and wellbeing? Environ. Sci. Technol. 45, 4660–4665. doi:10.1021/es103907m
Dermody, G., Whitehead, L., Wilson, G., and Glass, C. (2020). The role of virtual reality in improving health outcomes for community-dwelling older adults: Systematic review. J. Med. Internet Res. 22 (6), e17331. doi:10.2196/17331
Dikaios, E., Escobar, S., Nassim, M., Su, C. L., Torres‐Platas, S. G., and Rej, S. (2020). Continuation sessions of mindfulness‐based cognitive therapy (mbct‐C) vs. Treatment as usual in late‐life depression and anxiety: An open‐label extension study. Int. J. Geriatr. Psychiatry 35 (10), 1228–1232. doi:10.1002/gps.5360
Drozd, F., Vaskinn, L., Bergsund, H. B., Haga, S. M., Slinning, K., and Bjørkli, C. A. (2016). The implementation of internet interventions for depression: A scoping review. J. Med. Internet Res. 18 (9), e236. doi:10.2196/jmir.5670
Dudley, D. (2018). Virtual reality used to combat isolation and improve health. Washington, DC: AARP Magazine. Available at: https://www.aarp.org/home-family/personal-technology/info-2018/vr-explained.html.
Dunne, J. D. (2015). “Buddhist styles of mindfulness: A heuristic approach,” in Handbook of mindfulness and self-regulation. Editors B. D. Ostafin, M. D. Robinson, and B. P. Meier (New York: Springer).
Falconer, C. J., Rovira, A., King, J. A., Gilbert, P., Antley, A., Fearon, P., et al. (2016). Embodying self-compassion within virtual reality and its effects on patients with depression. BJPsych Open 2 (1), 74–80. doi:10.1192/bjpo.bp.115.002147
Falconer, C. J., Slater, M., Rovira, A., King, J. A., Gilbert, P., Antley, A., et al. (2014). Embodying compassion: A virtual reality paradigm for overcoming excessive self-criticism. PloS One 9 (11), e111933. doi:10.1371/journal.pone.0111933
Fang, W., Zheng, L., Deng, H., and Zhang, H. (2017). Real-time motion tracking for mobile augmented/virtual reality using adaptive visual-inertial fusion. Sensors 17, 1037. doi:10.3390/s17051037
Farrer, L., Leach, L., Griffiths, K. M., Christensen, H., and Jorm, A. F. (2008). Age differences in mental health literacy. BMC Public Health 8 (1), 125–128. doi:10.1186/1471-2458-8-125
Ferrari, M., Hunt, C., Harrysunker, A., Abbott, M. J., Beath, A. P., and Einstein, D. A. (2019). Self-compassion interventions and psychosocial outcomes: A meta-analysis of RCTs. Mindfulness 10 (8), 1455–1473. doi:10.1007/s12671-019-01134-6
Fiocco, A. J., and Mallya, S. (2015). The importance of cultivating mindfulness for cognitive and emotional well-being in late life. J. Evid. Based. Complement. Altern. Med. 20 (1), 35–40. doi:10.1177/2156587214553940
Firth, J., Torous, J., Nicholas, J., Carney, R., Pratap, A., Rosenbaum, S., et al. (2017a). The efficacy of smartphone‐based mental health interventions for depressive symptoms: A meta‐analysis of randomized controlled trials. World Psychiatry 16 (3), 287–298. doi:10.1002/wps.20472
Firth, J., Torous, J., Nicholas, J., Carney, R., Rosenbaum, S., and Sarris, J. (2017b). Can smartphone mental health interventions reduce symptoms of anxiety? A meta-analysis of randomized controlled trials. J. Affect. Disord. 218, 15–22. doi:10.1016/j.jad.2017.04.046
Fokkema, T., and Knipscheer, K. (2007). Escape loneliness by going digital: A quantitative and qualitative evaluation of a Dutch experiment in using ect to overcome loneliness among older adults. Aging Ment. Health 11 (5), 496–504. doi:10.1080/13607860701366129
Foulk, M. A., Ingersoll-Dayton, B., Kavanagh, J., Robinson, E., and Kales, H. C. (2014). Mindfulness-based cognitive therapy with older adults: An exploratory study. J. Gerontological Soc. Work 57 (5), 498–520. doi:10.1080/01634372.2013.869787
Fozard, J. L. (2012). “Gerontechnology: Optimising relationships between ageing people and changing technology,” in Contemporary issues in gerontology (New York, NY: Routledge), 241–268.
Fozard, L., Rietsema, J., Bouma, H., and Graafmans, J. A. M. (2000). Gerontechnology: Creating enabling environments for the challenges and opportunities of aging. Educ. Gerontol. 26 (4), 331–344. doi:10.1080/036012700407820
Franco, C., Amutio, A., Mañas, I., Gázquez, J. J., and del Carmen Pérez-Fuentes, M. Ş. (2017). Reducing anxiety, geriatric depression and worry in a sample of older adults through a mindfulness training program. Ter. Psicol. 35 (1), 71–79. doi:10.4067/s0718-48082017000100007
Gallegos, A. M., Hoerger, M., Talbot, N. L., Krasner, M. S., Knight, J. M., Moynihan, J. A., et al. (2013). Toward identifying the effects of the specific components of mindfulness-based stress reduction on biologic and emotional outcomes among older adults. J. Altern. Complementary Med. 19 (10), 787–792. doi:10.1089/acm.2012.0028
Ganguli, M., Rodriguez, E., Mulsant, B., Richards, S., Pandav, R., Vander Bilt, J., et al. (2004). Detection and management of cognitive impairment in primary care: The Steel Valley Seniors Survey. J. Am. Geriatr. Soc. 52, 1668–1675. doi:10.1111/j.1532-5415.2004.52459.x
Garrett, B., Taverner, T., Gromala, D., Tao, G., Cordingley, E., and Sun, C. (2018). Virtual reality clinical research: Promises and challenges. JMIR serious games 6 (4), e10839. doi:10.2196/10839
Geiger, P. J., Boggero, I. A., Brake, C. A., Caldera, C. A., Combs, H. L., Peters, J. R., et al. (2016). Mindfulness-based interventions for older adults: A review of the effects on physical and emotional well-being. Mindfulness 7 (2), 296–307. doi:10.1007/s12671-015-0444-1
Gerber, S. M., Jeitziner, M. M., Wyss, P., Chesham, A., Urwyler, P., Müri, R. M., and Nef, T. (2017). Visuo-acoustic stimulation that helps you to relax: A virtual reality setup for patients in the intensive care unit. Sci. Rep. 7 (13228), 1–15. doi:10.1038/s41598-017-13153-1
Gethin, R. (2011). On some definitions of mindfulness. Contemp. Buddhism 12 (1), 263–279. doi:10.1080/14639947.2011.564843
Gilbert, P. (2006). Compassion: Conceptualizations, research and use in psychotherapy. New York: Routledge.
Goldberg, S. B., Tucker, R. P., Greene, P. A., Davidson, R. J., Wampold, B. E., Kearney, D. J., et al. (2018). Mindfulness-based interventions for psychiatric disorders: A systematic review and meta-analysis. Clin. Psychol. Rev. 59, 52–60. doi:10.1016/j.cpr.2017.10.011
Google Scholar (2021). Google scholar. Retrieved July 20, 2021 from Available at: https://scholar.google.com.
Gouin, J. P., Hantsoo, L., and Kiecolt-Glaser, J. K. (2008). Immune dysregulation and chronic stress among older adults: A review. Neuroimmunomodulation 15 (4-6), 251–259. doi:10.1159/000156468
Graafmans, J. A. M., and Brouwers, A. (1989). “The modeling of normal aging,” in Proceedings of the 33rd annual meeting of the human factors society (Santa Monica, CA: The Human Factors and Ergonomics Society), 187–190.
Gum, A. M., King-Kallimanis, B., and Kohn, R. (2009). Prevalence of mood, anxiety, and substance-abuse disorders for older Americans in the national comorbidity survey-replication. Am. J. Geriatric Psychiatry 17 (9), 769–781. doi:10.1097/jgp.0b013e3181ad4f5a
Hank, K. (2011). How “successful” do older Europeans age? Findings from SHARE. Journals Gerontology Ser. B Psychol. Sci. Soc. Sci. 66 (2), 230–236. doi:10.1093/geronb/gbq089
Hart, R., Ivtzan, I., and Hart, D. (2013). Mind the gap in mindfulness research: A comparative account of the leading schools of thought. Rev. General Psychol. 17 (4), 453–466. doi:10.1037/a0035212
Hartig, T., Kaiser, F., and Bowler, P. (1997). Further development of a measure of perceived environmental restorativeness. Rotterdam, Netherlands: Institute for Housing Research. Available at: http://www.diva-portal.org/smash/get/diva2:130237/FULLTEXT01.pdf.
Hartig, T., Mitchell, R., De Vries, S., and Frumkin, H. (2014). Nature and health. Annu. Rev. Public Health 35, 207–228. doi:10.1146/annurev-publhealth-032013-182443
Hasan, H., and Linger, H. (2016). Enhancing the wellbeing of the elderly: Social use of digital technologies in aged care. Educ. Gerontol. 42 (11), 749–757. doi:10.1080/03601277.2016.1205425
Hazlett-Stevens, H., Singer, J., and Chong, A. (2019). Mindfulness-based stress reduction and mindfulness-based cognitive therapy with older adults: A qualitative review of randomized controlled outcome research. Clin. Gerontol. 42 (4), 347–358. doi:10.1080/07317115.2018.1518282
Hedblom, M., Gunnarsson, B., Iravani, B., Knez, I., Schaefer, M., Thorsson, P., and Lundström, J. N. (2019). Reduction of physiological stress by urban green space in a multisensory virtual experiment. Sci. Rep. 9 (10113), 1–11. doi:10.1038/s41598-019-46099-7
Henrich, J., Heine, S. J., and Norenzayan, A. (2010). Most people are not WEIRD. Nature 466 (7302), 29. doi:10.1038/466029a
Higgins, J. P., Altman, D. G., Gøtzsche, P. C., Jüni, P., Moher, D., Oxman, A. D., et al. (2011). The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ Br. Med. J. 343, d5928. doi:10.1136/bmj.d5928
Higgins, P., and Green, S. (2011). Cochrane handbook for systematic reviews of interventions. London, England: The Cochrane Collaboration. Available at: https://handbook-5-1.cochrane.org/.
Hiraoka, R., Meyer, E. C., Kimbrel, N. A. B., DeBeer, B. B., Gulliver, S. B., and Morissette, S. B. (2015). Self-compassion as a prospective predictor of PTSD symptom severity among trauma-exposed U.S. Iraq and Afghanistan war veterans. J. Trauma. Stress 28, 127–133. doi:10.1002/jts.21995
Hofmann, S. G., Sawyer, A. T., Witt, A. A., and Oh, D. (2010). The effect of mindfulness-based therapy on anxiety and depression: A meta-analytic review. J. Consult. Clin. Psychol. 78 (2), 169–183. doi:10.1037/a0018555
Holden, A. L. (2015). A comparison of virtual reality and mental imagery scenarios to promote self-compassion and reduce shame and self-criticism [unpublished doctoral dissertation]. London, England: University College London.
Howarth, A., Smith, J. G., Perkins-Porras, L., and Ussher, M. (2019). Effects of brief mindfulness-based interventions on health-related outcomes: A systematic review. Mindfulness 10 (10), 1957–1968. doi:10.1007/s12671-019-01163-1
Hughes, S., Warren-Norton, K., Spadafora, P., and Tsotsos, L. E. (2017). Supporting optimal aging through the innovative use of virtual reality technology. Multimodal Technol. Interact. 1 (4), 23. doi:10.3390/mti1040023
Institute of Medicine (2012). The mental health and substance use workforce for older adults: In whose hands? Washington, DC: National Academies Press. Retrieved from: Available at: http://www.nap.edu/catalog.php?record_id=13400.
Jerdan, S. W., Grindle, M., van Woerden, H. C., and Boulos, M. N. K. (2018). Head-mounted virtual reality and mental health: Critical review of current research. JMIR Serious Games 6 (3), e14. doi:10.2196/games.9226
Jimison, H. B., Gorman, P., Woods, S., Nygren, P., Walker, M., Norris, S., et al. (2008). Barriers and drivers of health information technology use for the elderly, chronically ill, and underserved. (Ser. Evidence report/technology assessment, no. 175). Washington, DC: U.S. Department of Health and Human Services, Agency for Healthcare Research and Quality.
Jøranson, N., Pedersen, I., Rokstad, A. M. M., and Ihlebaek, C. (2015). Effects on symptoms of agitation and depression in persons with dementia participating in robot-assisted activity: A cluster-randomized controlled trial. J. Am. Med. Dir. Assoc. 16 (10), 867–873. doi:10.1016/j.jamda.2015.05.002
Kabat-Zinn, J. (2013). Full catastrophe living : Using the wisdom of your body and mind to face stress, pain, and illness (revised and updated). New York, NY: Bantam. doi:10.1002/shi.88
Kabat-Zinn, J. (1994). Wherever you go, there you are: Mindfulness meditation in everyday lifeNew York, NY: Hyperion, 688–695.
Kahlbaugh, P. E., Sperandio, A. J., Carlson, A. L., and Hauselt, J. (2011). Effects of playing Wii on well-being in the elderly: Physical activity, loneliness, and mood. Activities, Adapt. Aging 35 (4), 331–344. doi:10.1080/01924788.2011.625218
Kang, H. G., Mahoney, D. F., Hoenig, H., Hirth, V. A., Bonato, P., Hajjar, I., et al. (2010). center for integration of medicine and innovative technology working group on advanced approaches to physiologic monitoring for the agedin situ monitoring of health in older adults: Technologies and issues. J. Am. Geriatr. Soc. 58 (8), 1579–1586. doi:10.1111/j.1532-5415.2010.02959.x
Kaplan, R., and Kaplan, S. (1989). The experience of nature: A psychological perspective. Cambridge, United Kingdom: Cambridge University Press. doi:10.1111/j.1523-1739.2008.01010.x
Kaplan, S. (2001). Meditation, restoration, and the management of mental fatigue. Environ. Behav. 33 (4), 480–506. doi:10.1177/00139160121973106
Kaplan, S. (1995). The restorative benefits of nature: Toward an integrative framework. J. Environ. Psychol. 15 (3), 169–182. doi:10.1016/0272-4944(95)90001-2
Karel, M. J., Gatz, M., and Smyer, M. A. (2012). Aging and mental health in the decade ahead: What psychologists need to know. Am. Psychol. 67 (3), 184–198. doi:10.1037/a0025393
Karlin, B. E., Duffy, M., and Gleavs, D. H. (2008). Patterns and predictors of mental health service use and mental illness among older and younger adults in the United States. Psychol. Serv. 5, 275–294. doi:10.1037/1541-1559.5.3.275
Khoury, B. (2019). Compassion: Embodied and embedded. Mindfulness 10 (11), 2363–2374. doi:10.1007/s12671-019-01211-w
Khoury, B., Knäuper, B., Pagnini, F., Trent, N., Chiesa, A., and Carrière, K. (2017). Embodied mindfulness. Mindfulness 8 (5), 1160–1171. doi:10.1007/s12671-017-0700-7
Khoury, B., Lecomte, T., Fortin, G., Masse, M., Therien, P., Bouchard, V., et al. (2013). Mindfulness-based therapy: A comprehensive meta-analysis. Clin. Psychol. Rev. 33 (6), 763–771. doi:10.1016/j.cpr.2013.05.005
Khoury, B. (2018). Mindfulness: Embodied and embedded. Mindfulness 9 (4), 1037–1042. doi:10.1007/s12671-017-0858-z
Khoury, B., Sharma, M., Rush, S. E., and Fournier, C. (2015). Mindfulness-based stress reduction for healthy individuals: A meta-analysis. J. psychosomatic Res. 78 (6), 519–528. doi:10.1016/j.jpsychores.2015.03.009
Kim, G. H., Jeon, S., Im, K., Kwon, H., Lee, B. H., Kim, G. Y., et al. (2015). Structural brain changes after traditional and robot-assisted multi-domain cognitive training in community-dwelling healthy elderly. PloS One 10 (4), e0123251. doi:10.1371/journal.pone.0123251
Kim, K. I., Gollamudi, S. S., and Steinhubl, S. (2017). Digital technology to enable aging in place. Exp. Gerontol. 88, 25–31. doi:10.1016/j.exger.2016.11.013
Kirby, J. N. (2017). Compassion interventions: The programmes, the evidence, and implications for research and practice. Psychol. Psychother. Theory Res. Pract. 90 (3), 432–455. doi:10.1111/papt.12104
Kirby, J. N., Tellegen, C. L., and Steindl, S. R. (2017). A meta-analysis of compassion-based interventions: Current state of knowledge and future directions. Behav. Ther. 48 (6), 778–792. doi:10.1016/j.beth.2017.06.003
Kjellgren, A., and Buhrkall, H. (2010). A comparison of the restorative effect of a natural environment with that of a simulated natural environment. J. Environ. Psychol. 30 (4), 464–472. doi:10.1016/j.jenvp.2010.01.011
Klap, R., Unroe, K. T., and Unu ̈tzer, J. (2003). Caring for mental illness in the United States: A focus on older adults. Am. J. Geriatric Psychiatry 11, 517–524. doi:10.1097/00019442-200309000-00006
Kugler, L. (2021). The state of virtual reality hardware. Commun. ACM 64 (2), 15–16. doi:10.1145/3441290
Kvedar, J., Coye, M. J., and Everett, W. (2014). Connected health: A review of technologies and strategies to improve patient care with telemedicine and telehealth. Health Aff. 33 (2), 194–199. doi:10.1377/hlthaff.2013.0992
S. Kwon (Editor) (2016). Gerontechnology: Research, practice, and principles in the field of technology and aging (Springer Publishing Company).
Labbé, M., Nikolitch, K., Penheiro, R., Segal, M., Looper, K. J., Herrmann, N., et al. (2016). Mindfulness-based cognitive therapy in the treatment of late-life anxiety and depression—A pilot study. Can. Geriatr. J. 19 (3), 127–128. doi:10.5770/cgj.19.215
Laidlaw, K., Thompson, L. W., Dick-Siskin, L., and Gallagher-Thompson, D. (2003). Cognitive behaviour Therapy with older people. West Sussex, England: John Wiley & Sons.
Lampit, A., Hallock, H., and Valenzuela, M. (2014). Computerized cognitive training in cognitively healthy older adults: A systematic review and meta-analysis of effect modifiers. PLoS Med. 11 (11), e1001756. doi:10.1371/journal.pmed.1001756
Langer, E., and Moldoveanu, M. (2000). The construct of mindfulness. J. Soc. Issues 56 (1), 1–9. doi:10.1111/0022-4537.00148
Lapane, K. L., Goldman, R. E., Quilliam, B. J., Hume, A. L., and Eaton, C. B. (2012). Tailored DVDs: A novel strategy for educating racially and ethnically diverse older adults about their medicines. Int. J. Med. Inf. 81, 852–860. doi:10.1016/j.ijmedinf.2012.09.007
Lattanzio, F., Abbatecola, A. M., Bevilacqua, R., Chiatti, C., Corsonello, A., Rossi, L., et al. (2014). Advanced technology care innovation for older people in Italy: Necessity and opportunity to promote health and wellbeing. J. Am. Med. Dir. Assoc. 15 (7), 457–466. doi:10.1016/J.JAMDA.2014.04.003
Lee, L. N., Kim, M. J., and Hwang, W. J. (2019). Potential of augmented reality and virtual reality technologies to promote wellbeing in older adults. Appl. Sci. 9 (17), 3556. doi:10.3390/app9173556
Lenze, E. J., Hickman, S., Hershey, T., Wendleton, L., Ly, K., Dixon, D., et al. (2014). Mindfulness‐based stress reduction for older adults with worry symptoms and co‐occurring cognitive dysfunction. Int. J. Geriatr. Psychiatry 29 (10), 991–1000. doi:10.1002/gps.4086
Levy, F., Leboucher, P., Rautureau, G., Komano, O., Millet, B., and Jouvent, R. (2016). Fear of falling: Efficacy of virtual reality associated with serious games in elderly people. Neuropsychiatr. Dis. Treat. 12, 877–881. doi:10.2147/ndt.s97809
Li, B. J., Bailenson, J. N., Pines, A., Greenleaf, W. J., and Williams, L. M. (2017). A public database of immersive VR videos with corresponding ratings of arousal, valence, and correlations between head movements and self report measures. Front. Psychol. 8, 2116. doi:10.3389/fpsyg.2017.02116
Ludden, G. D., van Rompay, T. J., Niedderer, K., and Tournier, I. (2019). Environmental design for dementia care-towards more meaningful experiences through design. Maturitas 128, 10–16. doi:10.1016/j.maturitas.2019.06.011
MacBeth, A., and Gumley, A. (2012). Exploring compassion: A meta-analysis of the association between self-compassion and psychopathology. Clin. Psychol. Rev. 32 (6), 545–552. doi:10.1016/j.cpr.2012.06.003
Maister, L., Slater, M., Sanchez-Vives, M. V., and Tsakiris, M. (2015). Changing bodies changes minds: Owning another body affects social cognition. Trends cognitive Sci. 19 (1), 6–12. doi:10.1016/j.tics.2014.11.001
Maples-Keller, J. L., Bunnell, B. E., Kim, S. J., and Rothbaum, B. O. (2017). The use of virtual reality technology in the treatment of anxiety and other psychiatric disorders. Harv. Rev. Psychiatry 25 (3), 103–113. doi:10.1097/HRP.0000000000000138
Marsh, I. C., Chan, S. W., and MacBeth, A. (2018). Self-compassion and psychological distress in adolescents—A meta-analysis. Mindfulness 9 (4), 1011–1027. doi:10.1007/s12671-017-0850-7
Martini, M., Perez‐Marcos, D., and Sanchez‐Vives, M. V. (2014). Modulation of pain threshold by virtual body ownership. Eur. J. Pain 18 (7), 1040–1048. doi:10.1002/j.1532-2149.2014.00451.x
Martinson, M., and Berridge, C. (2015). Successful aging and its discontents: A systematic review of the social gerontology literature. Gerontologist 55 (1), 58–69. doi:10.1093/geront/gnu037
Mayer, F. S., Frantz, C. M., Bruehlman-Senecal, E., and Dolliver, K. (2009). Why is nature beneficial? The role of connectedness to nature. Environ. Behav. 41 (5), 607–643. doi:10.1177/0013916508319745
McAuley, E., Wojcicki, T. T., Gothe, N. P., Mailey, E. L., Szabo, A. N., Fanning, J., et al. (2013). Effects of a DVD-delivered exercise intervention on physical function in older adults. Journals Gerontology Ser. A Biol. Sci. Med. Sci. 68, 1076–1082. doi:10.1093/gerona/glt014
McCausland, L., and Falk, N. L. (2012). From dinner table to digital tablet: Technology’s potential for reducing loneliness in older adults. J. Psychosoc. Nurs. Ment. Health Serv. 50 (5), 22–26. doi:10.3928/02793695-20120410-01
McMahan, E. A., and Estes, D. (2015). The effect of contact with natural environments on positive and negative affect: A meta-analysis. J. Posit. Psychol. 10 (6), 507–519. doi:10.1080/17439760.2014.994224
McMahon, S., Vankipuram, M., Hekler, E. B., and Fleury, J. (2014). Design and evaluation of theory-informed technology to augment a wellness motivation intervention. Transl. Behav. Med. 1, 95–107. doi:10.1007/s13142-013-0221-4
Mental Health Foundation (2018). Mental health statistics: Older people. Available at: https://www.mentalhealth.org.uk/statistics/mental-health-statistics-older-people.
Mewton, L., Sachdev, P. S., and Andrews, G. (2013). A naturalistic study of the acceptability and effectiveness of Internet-delivered cognitive behavioural therapy for psychiatric disorders in older Australians. PLoS One 8, e71825. doi:10.1371/journal.pone.0071825
Miller, K. J., Adair, B. S., Pearce, A. J., Said, C. M., Ozanne, E., and Morris, M. M. (2014). Effectiveness and feasibility of virtual reality and gaming system use at home by older adults for enabling physical activity to improve health-related domains: A systematic review. Age ageing 43 (2), 188–195. doi:10.1093/ageing/aft194
Miller, M. R., Jun, H., Herrera, F., Yu Villa, J., Welch, G., and Bailenson, J. N. (2019). Social interaction in augmented reality. PloS One 14 (5), e0216290. doi:10.1371/journal.pone.0216290
Millward, P. (2003). The 'grey digital divide': Perception, exclusion and barriers of access to the Internet for older people. First Monday 8 (7). doi:10.5210/fm.v8i7.1066
Modrego-Alarcón, M., López-del-Hoyo, Y., García-Campayo, J., Pérez-Aranda, A., Navarro-Gil, M., Beltrán-Ruiz, M., et al. (2021). Efficacy of a mindfulness-based programme with and without virtual reality support to reduce stress in University students: A randomized controlled trial. Behav. Res. Ther. 142, 103866. doi:10.1016/j.brat.2021.103866
Mohr, D. C., Cheung, K., Schueller, S. M., Brown, C. H., and Duan, N. (2013). Continuous evaluation of evolving behavioral intervention technologies. Am. J. Prev. Med. 45 (4), 517–523. doi:10.1016/j.amepre.2013.06.006
Molina, K. I., Ricci, N. A., de Moraes, S. A., and Perracini, M. R. (2014). Virtual reality using games for improving physical functioning in older adults: A systematic review. J. neuroengineering rehabilitation 11 (156), 1–220. doi:10.1186/1743-0003-11-156
Montana, J. I., Matamala-Gomez, M., Maisto, M., Mavrodiev, P. A., Cavalera, C. M., Diana, B., et al. (2020). The benefits of emotion regulation interventions in virtual reality for the improvement of wellbeing in adults and older adults: A systematic review. J. Clin. Med. 9 (2), 500. doi:10.3390/jcm9020500
Morgan, C., Mason, E., Newby, J. M., Mahoney, A. E., Hobbs, M. J., McAloon, J., et al. (2017). The effectiveness of unguided internet cognitive behavioural therapy for mixed anxiety and depression. Internet Interv. 10, 47–53. doi:10.1016/j.invent.2017.10.003
Moyle, W., Cooke, M., Beattie, E., Jones, C., Klein, B., Cook, G., et al. (2013). Exploring the effect of companion robots on emotional expression in older adults with dementia: A pilot randomized controlled trial. J. Gerontol. Nurs. 39 (5), 46–53. doi:10.3928/00989134-20130313-03
Moyle, W., Jones, C., Dwan, T., and Petrovich, T. (2018). Effectiveness of a virtual reality forest on people with dementia: A mixed methods pilot study. Gerontologist 58, 478–487. doi:10.1093/geront/gnw270
Moynihan, J. A., Chapman, B. P., Klorman, R., Krasner, M. S., Duberstein, P. R., Brown, K. W., et al. (2013). Mindfulness-based stress reduction for older adults: Effects on executive function, frontal alpha asymmetry and immune function. Neuropsychobiology 68 (1), 34–43. doi:10.1159/000350949
Müller, L., Di Benedetto, S., and Pawelec, G. (2019). The immune system and its dysregulation with aging. Subcell. Biochem. 91, 21–43. doi:10.1007/978-981-13-3681-2_2
Muris, P., Otgaar, H., and Petrocchi, N. (2016). Protection as the mirror image of psychopathology: Further critical notes on the self-compassion scale. Mindfulness 7 (3), 787–790. doi:10.1007/s12671-016-0509-9
Navarro-Haro, M. V., Hoffman, H. G., Garcia-Palacios, A., Sampaio, M., Alhalabi, W., Hall, K., et al. (2016). The use of virtual reality to facilitate mindfulness skills training in dialectical behavioral therapy for borderline personality disorder: A case study. Front. Psychol. 7, 1573. doi:10.3389/fpsyg.2016.01573
Navarro-Haro, M. V., López-del-Hoyo, Y., Campos, D., Linehan, M. M., Hoffman, H. G., García-Palacios, A., et al. (2017). Meditation experts try virtual reality mindfulness: A pilot study evaluation of the feasibility and acceptability of virtual reality to facilitate mindfulness practice in people attending a mindfulness conference. PloS One 12 (11), e0187777. doi:10.1371/journal.pone.0187777
Navarro-Haro, M. V., Modrego-Alarcón, M., Hoffman, H. G., López-Montoyo, A., Navarro-Gil, M., Montero-Marin, J., et al. (2019). Evaluation of a mindfulness-based intervention with and without virtual reality dialectical behavior Therapy® mindfulness skills training for the treatment of generalized anxiety disorder in primary care: A pilot study. Front. Psychol. 10, 55. doi:10.3389/fpsyg.2019.00055
Neff, K. (2004). Self-compassion and psychological well-being. Constr. Hum. Sci. 9 (2), 27. doi:10.1037/e633942013-240
Neff, K. (2003). Self-Compassion: An alternative conceptualization of a healthy attitude toward oneself. Self Identity 2 (2), 85–101. doi:10.1080/15298860309032
Neff, K., and Vonk, R. (2009). Self-compassion versus global self-esteem: Two different ways of relating to oneself. J. Personality 77 (1), 23–50. doi:10.1111/j.1467-6494.2008.00537.x
Ng, T. K. S., Fam, J., Feng, L., Cheah, I. K. M., Tan, C. T. Y., Nur, F., et al. (2020). Mindfulness improves inflammatory biomarker levels in older adults with mild cognitive impairment: A randomized controlled trial. Transl. Psychiatry 10 (1), 21–14. doi:10.1038/s41398-020-0696-y
Nielsen, A. (2014). Mobile millennials: Over 85% of generation Y owns smartphones. Available at: http://www.nielsen.com/us/en/insights/news/2014/mobile-millennials-over-85-percent-of-generation-y-ownssmartphones.html.
Nielsen, M., Haun, D., Kärtner, J., and Legare, C. H. (2017). The persistent sampling bias in developmental psychology: A call to action. J. Exp. Child Psychol. 162, 31–38. doi:10.1016/j.jecp.2017.04.017
Nisbet, E. K., Zelenski, J. M., and Murphy, S. A. (2011). Happiness is in our nature: Exploring nature relatedness as a contributor to subjective well-being. J. Happiness Stud. 12 (2), 303–322. doi:10.1007/s10902-010-9197-7
Optale, G., Urgesi, C., Busato, V., Marin, S., Piron, L., Priftis, K., et al. (2010). Controlling memory impairment in elderly adults using virtual reality memory training: A randomized controlled pilot study. Neurorehabil. Neural Repair 24 (4), 348–357. doi:10.1177/1545968309353328
Orians, G. H. (1980). Habitat selection: General theory and applications to human behavior. Evol. Hum. Soc. Behav.
Parijat, P., Lockhart, T. E., and Liu, J. (2015). Effects of perturbation-based slip training using a virtual reality environment on slip-induced falls. Ann. Biomed. Eng. 43 (4), 958–967. doi:10.1007/s10439-014-1128-z
Parijat, P., Lockhart, T. E., and Liu, J. (2014). EMG and kinematic responses to unexpected slips after slip training in virtual reality. IEEE Trans. Biomed. Eng. 62 (2), 593–599. doi:10.1109/tbme.2014.2361324
Pearson, D. G., Deeprose, C., Wallace-Hadrill, S. M. A., Burnett Heyes, S., and Holmes, E. A. (2013). Assessing mental imagery in clinical psychology: A review of imagery measures and a guiding framework. Clin. Psychol. Rev. 33, 1–23. doi:10.1016/j.cpr.2012.09.001
Peck, T. C., Seinfeld, S., Aglioti, S. M., and Slater, M. (2013). Putting yourself in the skin of a black avatar reduces implicit racial bias. Conscious. cognition 22 (3), 779–787. doi:10.1016/j.concog.2013.04.016
Perez-Blasco, J., Sales, A., Meléndez, J. C., and Mayordomo, T. (2016). The effects of mindfulness and self-compassion on improving the capacity to adapt to stress situations in elderly people living in the community. Clin. Gerontol. 39 (2), 90–103. doi:10.1080/07317115.2015.1120253
Peterson, B., Hitching, R., Howard, L., Zhu, K., Fontenot, M. R., Alhalabi, W., et al. (2021). Immersive virtual reality: A safe, scalable, non-opioid analgesic for military and veteran patients. Front. Virtual Real. 145. doi:10.3389/frvir.2021.742290
Petkova, V. I., Khoshnevis, M., and Ehrsson, H. H. (2011). The perspective matters! Multisensory integration in ego-centric reference frames determines full-body ownership. Front. Psychol. 2, 35. doi:10.3389/fpsyg.2011.00035
Piau, A., Campo, E., Rumeau, P., Vellas, B., and Nourhashemi, F. (2014). Aging society and gerontechnology: A solution for an independent living? J. Nutr. Health Aging 18 (1), 97–112. doi:10.1007/s12603-013-0356-5
Poissant, H., Mendrek, A., Talbot, N., Khoury, B., and Nolan, J. (2019). Behavioral and cognitive impacts of mindfulness-based interventions on adults with attention-deficit hyperactivity disorder: A systematic review. Behav. Neurol. 16, 1. doi:10.1155/2019/5682050
Pratt, D. R., Zyda, M., and Kelleher, K. (1995). Virtual reality: In the mind of the beholder. Computer (7), 17–19.
Preschl, B., Maercker, A., Wagner, B., Forstmeier, S., Baños, R. M., Alcañiz, M., et al. (2012). Life-review therapy with computer supplements for depression in the elderly: A randomized controlled trial. Aging & Ment. Health 16 (8), 964–974. doi:10.1080/13607863.2012.702726
Preschl, B., Wagner, B., Forstmeier, S., and Maercker, A. (2011). E-Health interventions for depression, anxiety disorder, dementia, and other disorders in older adults: A review. J. CyberTherapy Rehabilitation 4 (3), 371–386. doi:10.1080/13607863.2012.702726
Pruchno, R., and Carr, D. (2017). Successful aging 2.0: Resilience and beyond. Journals Gerontology Ser. B 72 (2), 201–203. doi:10.1093/geronb/gbw214
Pywell, J., Vijaykumar, S., Dodd, A., and Coventry, L. (2020). Barriers to older adults’ uptake of mobile-based mental health interventions. Digit. health 6, 205520762090542. doi:10.1177/2055207620905422
Reardon, C. (2012). Tech-savvy older adults: Staying connected, challenging stereotypes. Soc. Work Today 12 (6), 10.
Reeder, B., Demiris, G., and Marek, K. D. (2013). Older adults' satisfaction with a medication dispensing device in home care. Inf. Health Soc. Care 38 (3), 211–222. doi:10.3109/17538157.2012.741084
Rendon, A. A., Lohman, E. B., Thorpe, D., Johnson, E. G., Medina, E., and Bradley, B. (2012). The effect of virtual reality gaming on dynamic balance in older adults. Age Ageing 41 (4), 549–552. Retrieved from:. doi:10.1093/ageing/afs053
Reynolds, L., Rodiek, S., Lininger, M., and McCulley, M. A. (2018). Can a virtual nature experience reduce anxiety and agitation in people with dementia? J. Hous. Elder. 32, 176–193. doi:10.1080/02763893.2018.1431583
Riva, G., Baños, R. M., Botella, C., Mantovani, F., and Gaggioli, A. (2016). Transforming experience: The potential of augmented reality and virtual reality for enhancing personal and clinical change. Front. Psychiatry 7, 164. doi:10.3389/fpsyt.2016.00164
Riva, G., Dakanalis, A., and Mantovani, F. (2015). The handbook of the psychology of communication technology. Chichester, UK: John Wiley & Sons, 528–547.Leveraging psychology of the virtual body for health and wellness
Riva, G. (2005). Virtual reality in psychotherapy: Review. Cyberpsychology Behav. 8 (3), 220–230. doi:10.1089/cpb.2005.8.220
Riva, G., and Wiederhold, B. K. (2020). How cyberpsychology and virtual reality can help us to overcome the psychological burden of coronavirus. Cyberpsychology, Behav. Soc. Netw. 23 (5), 277–279. doi:10.1089/cyber.2020.29183.gri
Robertson, C. E., Hermann, K. L., Mynick, A., Kravitz, D. J., and Kanwisher, N. (2016). Neural representations integrate the current field of view with the remembered 360 panorama in scene-selective cortex. Curr. Biol. 26 (18), 2463–2468. doi:10.1016/j.cub.2016.07.002
Rodda, J., Walker, Z., and Carter, J. (2011). Depression in older adults. BMJ Br. Med. J. 343 (5219), d5219–d5687. doi:10.1136/bmj.d5219
Roe, J., and Aspinall, P. (2011). The restorative benefits of walking in urban and rural settings in adults with good and poor mental health. Health & Place 17 (1), 103–113. doi:10.1016/j.healthplace.2010.09.003
Rost, T., Stein, J., Löbner, M., Kersting, A., Luck-Sikorski, C., and Riedel-Heller, S. G. (2017). User acceptance of computerized cognitive behavioral therapy for depression: Systematic review. J. Med. Internet Res. 19 (9), e309. doi:10.2196/jmir.7662
Rowe, J. W., and Kahn, R. L. (1987). Human aging: Usual and successful. Science 237, 143–149. doi:10.1126/science.3299702
Rowe, J. W., and Kahn, R. L. (1997). Successful aging. Gerontologist 37 (4), 433–440. doi:10.1093/geront/37.4.433
Rowe, J. W., and Kahn, R. L. (2015). Successful aging 2.0: Conceptual expansions for the 21st century. Journals Gerontology Ser. B 70 (4), 593–596. doi:10.1093/geronb/gbv025
Sadowski, I., Böke, N., Mettler, J., Heath, N., and Khoury, B. (2020). Naturally mindful? The role of mindfulness facets in the relationship between nature relatedness and subjective well-being. Curr. Psychol. 41, 5358–5373. doi:10.1007/s12144-020-01056-w
Sanchez-Vives, M. V., and Slater, M. (2005). From presence to consciousness through virtual reality. Nat. Rev. Neurosci. 6 (4), 332–339. doi:10.1038/nrn1651
Sbarra, D. A., Smith, H. L., and Mehl, M. R. (2012). When leaving your Ex, love yourself: Observational ratings of self-compassion predict the course of emotional recovery following marital separation. Psychol. Sci. 23 (3), 261–269. doi:10.1177/0956797611429466
Schmitter-Edgecombe, M., Seelye, A., and Cook, D. J. (2013). “Technologies for health assessment, promotion, and assistance: Focus on gerontechnology,” in Positive neuropsychology (New York, NY: Springer), 143–160.
Schutte, N. S., Bhullar, N., Stilinović, E. J., and Richardson, K. (2017). The impact of virtual environments on restorativeness and affect. Ecopsychology 9 (1), 1–7. doi:10.1089/eco.2016.0042
Schutte, N. S., and Malouff, J. M. (2018). Mindfulness and connectedness to nature: A meta-analytic investigation. Personality Individ. Differ. 127, 10–14. doi:10.1016/j.paid.2018.01.034
Seabrook, E., Kelly, R., Foley, F., Theiler, S., Thomas, N., Wadley, G., et al. (2020). Understanding how virtual reality can support mindfulness practice: Mixed methods study. J. Med. Internet Res. 22 (3), e16106. doi:10.2196/16106
Segal, R., Bhatia, M., and Drapeau, M. (2011). Therapists' perception of benefits and costs of using virtual reality treatments. Cyberpsychology, Behav. Soc. Netw. 14 (1-2), 29–34. doi:10.1089/cyber.2009.0398
Seifert, A., Reinwand, D. A., and Schlomann, A. (2019). Designing and using digital mental health interventions for older adults: Being aware of digital inequality. Front. Psychiatry 10, 568. doi:10.3389/fpsyt.2019.00568
Shatil, E., Mikulecka, J., Bellotti, F., and Bures, V. (2014). Novel television-based cognitive training improves working memory and executive function. PLoS One 9, e101472. doi:10.1371/journal.pone.0101472
Shonin, E., Van Gordon, W., and Griffiths, M. D. (2014). The emerging role of buddhism in clinical psychology: Toward effective integration. Psychol. Relig. Spiritual. 6 (2), 123–137. doi:10.1037/a0035859
Silva, P. A., Holden, K., and Jordan, P. (2015). “Towards a list of heuristics to evaluate smartphone apps targeted at older adults: A study with apps that aim at promoting health and well-being,” in 2015 48th Hawaii international conference on system sciences (IEEE), 3237–3246.
Silveira, P., van de Langenberg, R., van Het Reve, E., Daniel, F., Casati, F., and de Bruin, E. D. (2013). Tablet-based strength-balance training to motivate and improve adherence to exercise in independently living older people: A phase II preclinical exploratory trial. J. Med. Internet Res. 15 (8), e159. doi:10.2196/jmir.2579
Skurla, M. D., Rahman, A. T., Salcone, S., Mathias, L., Shah, B., Forester, B. P., et al. (2021). Virtual reality and mental health in older adults: A systematic review. Int. Psychogeriatr. 34, 143–155. doi:10.1017/s104161022100017x
Slater, M., Spanlang, B., Sanchez-Vives, M. V., and Blanke, O. (2010). First person experience of body transfer in virtual reality. PloS One 5 (5), e10564. doi:10.1371/journal.pone.0010564
Slater, M., Usoh, M., and Steed, A. (1994). Depth of presence in virtual environments. Presence. (Camb). 3 (2), 130–144. doi:10.1162/pres.1994.3.2.130
Smith, A. (2014). Older adults and technology use. Available at: http://www.pewinternet.org/2014/04/03/older-adults-and-technology-use/.
Smith, J. W. (2015). Immersive virtual environment technology to supplement environmental perception, preference and behavior research: A review with applications. Int. J. Environ. Res. Public Health 12, 11486–11505. doi:10.3390/ijerph120911486
Spek, V., Nyklíček, I., Smits, N., Cuijpers, P. I. M., Riper, H., Keyzer, J., et al. (2007). Internet-based cognitive behavioural therapy for subthreshold depression in people over 50 years old: A randomized controlled clinical trial. Psychol. Med. 37 (12), 1797–1806. doi:10.1017/s0033291707000542
Strauss, C., Lever Taylor, B., Gu, J., Kuyken, W., Baer, R., Jones, F., et al. (2016). What is compassion and how can we measure it? A review of definitions and measures. Clin. Psychol. Rev. 47, 15–27. doi:10.1016/j.cpr.2016.05.004
Taha, J., Sharit, J., and Czaja, S. J. (2014). The impact of numeracy ability and technology skills on older adults’ performance of health management tasks using a patient portal. J. Appl. Gerontol. 33, 416–436. doi:10.1177/0733464812447283
Tavares, L. R., Vagos, P., and Xavier, A. (2020). The role of self-compassion in the psychological (mal) adjustment of older adults: A scoping review. Int. Psychogeriatr., 1–14. doi:10.1017/s1041610220001222
Thach, K. S., Lederman, R., and Waycott, J. (2020). “How older adults respond to the use of virtual reality for enrichment: A systematic review,” in 32nd Australian conference on human-computer interaction, 303–313.
Thompson Coon, J., Boddy, K., Stein, K., Whear, R., Barton, J., and Depledge, M. H. (2011). Does participating in physical activity in outdoor natural environments have a greater effect on physical and mental wellbeing than physical activity indoors? A systematic review. Environ. Sci. Technol. 45 (5), 1761–1772. doi:10.1021/es102947t
Thompson, H. J., Demiris, G., Rue, T., Shatil, E., Wilamowska, K., Zaslavsky, O., et al. (2011). A holistic approach to assess older adults’ wellness using e-health technologies. Telemedicine e-Health 17, 794–800. doi:10.1089/tmj.2011.0059
Titov, N., Dear, B. F., Ali, S., Zou, J. B., Lorian, C. N., Johnston, L., et al. (2015). Clinical and cost-effectiveness of therapist-guided internet-delivered cognitive behavior therapy for older adults with symptoms of depression: A randomized controlled trial. Behav. Ther. 46 (2), 193–205. doi:10.1016/j.beth.2014.09.008
Titov, N., Fogliati, V. J., Staples, L. G., Gandy, M., Johnston, L., Wootton, B., et al. (2016). Treating anxiety and depression in older adults: Randomised controlled trial comparing guided v. self-guided internet-delivered cognitive–behavioural therapy. BJPsych Open 2 (1), 50–58. doi:10.1192/bjpo.bp.115.002139
Tong, X., Gromala, D., Choo, A., Amin, A., and Shaw, C. (2015). “The virtual meditative walk: An immersive virtual environment for pain self-modulation through mindfulness-based stress reduction meditation,” in International conference on virtual, Augmented and mixed reality (Cham: Springer), 388–397.
Torres-Platas, S. G., Escobar, S., Belliveau, C., Wu, J., Sasi, N., Fotso, J., et al. (2019). Mindfulness-based cognitive therapy intervention for the treatment of late-life depression and anxiety symptoms in primary care: A randomized controlled trial. Psychother. Psychosom. 88 (4), 254–256. doi:10.1159/000501214
Triberti, S., and Riva, G. (2016). Being present in action: A theoretical model about the “interlocking” between intentions and environmental affordances. Front. Psychol. 6, 2052. doi:10.3389/fpsyg.2015.02052
Tsai, H. H., and Tsai, Y. F. (2011). Changes in depressive symptoms, social support, and loneliness over 1 year after a minimum 3-month videoconference program for older nursing home residents. J. Med. Internet Res. 13 (4), e93. doi:10.2196/jmir.1678
Tsai, H. H., Tsai, Y. F., Wang, H. H., Chang, Y. C., and Chu, H. H. (2010). Videoconference program enhances social support, loneliness, and depressive status of elderly nursing home residents. Aging Ment. Health 14 (8), 947–954. doi:10.1080/13607863.2010.501057
Tuena, C., Pedroli, E., Trimarchi, P. D., Gallucci, A., Chiappini, M., Goulene, K., et al. (2020). Usability issues of clinical and research applications of virtual reality in older people: A systematic review. Front. Hum. Neurosci. 14, 93. doi:10.3389/fnhum.2020.00093
United Nations Department of Economic and Social Affairs (2019). World population prospects 2019. Highlights (ST/ESA/SER.A/423). Available at: http://esa.un.org/unpd/wpp/index.htm.
United Nations Department of Economic and Social Affairs, Population Division (2013). World population ageing 2013. Available at: https://www.un.org/en/development/desa/population/publications/ageing/WorldPopulationAgeing2013.asp.
Unützer, J., Schoenbaum, M., Druss, B. G., and Katon, W. J. (2006). Transforming mental health care at the interface with general medicine: Report for the president’s commission. Psychiatr. Serv. 57, 37–47. doi:10.1176/appi.ps.57.1.37
Vailati Riboni, F., Comazzi, B., Castelnuovo, G., Molinari, E., and Pagnini, F. (2018)., 253. Lecture Notes of the Institute forSpringer Verlag, 115–118. doi:10.1007/978-3-030-01093-5_15Mindful age and technology: Promoting quality of life in older adults with a tablet/smartphone appComput. Sci. Social-Informatics Telecommun. Eng. LNICST
Vailati Riboni, F., Sadowski, I., Comazzi, B., and Pagnini, F. (2020b). Mindful age and technology: A qualitative analysis of a tablet/smartphone app intervention designed for older adults. Integr. Psychol. Behav. Sci. 56, 739–754. doi:10.1007/s12124-020-09580-x
Vailati-Riboni, F., Comazzi, B., Bercovitz, K., Castelnuovo, G., Molinari, E., and Pagnini, F. (2020a). Technologically-enhanced psychological interventions for older adults: A scoping review. BMC Geriatr. 20 (1), 191. doi:10.1186/s12877-020-01594-9
Valtchanov, D. (2010). Physiological and affective responses to immersion in virtual reality: Effects of nature and urban settings [Unpublished Master’s Thesis]. Waterloo, Ontario, Canada: University of Waterloo.
Van den Berg, A. E., Koole, S. L., and van der Wulp, N. Y. (2003). Environmental preference and restoration: (How) are they related? J. Environ. Psychol. 23 (2), 135–146. doi:10.1016/s0272-4944(02)00111-1
Van Houwelingen-Snippe, J., Allouch, S. B., and Van Rompay, T. J. (2021). Virtual reality representations of nature to improve well-being amongst older adults: A rapid review. J. Technol. Behav. Sci. 6, 464–485. doi:10.1007/s41347-021-00195-6
Vaportzis, E., Giatsi Clausen, M., and Gow, A. J. (2017). Older adults perceptions of technology and barriers to interacting with tablet computers: A focus group study. Front. Psychol. 8, 1687. doi:10.3389/fpsyg.2017.01687
Wagner, L. S., and Wagner, T. H. (2003). The effect of age on the use of health and self-care information: Confronting the stereotype. Gerontologist 43, 318–324. doi:10.1093/geront/43.3.318
Wang, P. S., Lane, M., Olfson, M., Pincus, H. A., Wells, K. B., and Kessler, R. C. (2005). Twelve-month use of mental health services in the United States: Results from the national comorbidity survey replication. Arch. Gen. Psychiatry 62, 629–640. doi:10.1001/arch-psyc.62.6.629
Wetherell, J. L., Hershey, T., Hickman, S., Tate, S. R., Dixon, D., Bower, E. S., et al. (2017). Mindfulness-based stress reduction for older adults with stress disorders and neurocognitive difficulties: A randomized controlled trial. J. Clin. Psychiatry 78, e734–e743. doi:10.4088/JCP.16m10947
White, M. P., Yeo, N. L., Vassiljev, P., Lundstedt, R., Wallergård, M., Albin, M., et al. (2018). A prescription for “nature” – the potential of using virtual nature in therapeutics. Neuropsychiatr. Dis. Treat. Vol. 14, 3001–3013. doi:10.2147/ndt.s179038
Winstein, C. J., Stein, J., Arena, R., Bates, B., Cherney, L. R., Cramer, S. C., et al. (2016). Guidelines for adult stroke rehabilitation and recovery: A guideline for healthcare professionals from the American heart association/American stroke association. Stroke 47, e98–e169. doi:10.1161/STR.0000000000000098
Wong, C. C., Mak, W. W., and Liao, K. Y.-H. (2016). Self-compassion: A potential buffer against affiliate stigma experienced by parents of children with autism spectrum disorders. Mindfulness 7 (6), 1385–1395. doi:10.1007/s12671-016-0580-2
Wong, C. K., Yeung, D. Y., Ho, H. C., Tse, K. P., and Lam, C. Y. (2014). Chinese older adults’ Internet use for health information. J. Appl. Gerontol. 33, 316–335. doi:10.1177/0733464812463430
Wootton, R. (2012). Twenty years of telemedicine in chronic disease management-an evidence synthesis. J. Telemed. Telecare 18 (4), 211–220. doi:10.1258/jtt.2012.120219
World Health Organization (2017). Depression and other common mental health disorders: Global health estimates. Geneva, Switzerland. Available at: http://apps.who.int/iris/bitstream/handle/10665/254610/WHO-MSD-MER-2017.2-eng.pdf.
Xie, B. (2011). Effects of an e-health literacy intervention for older adults. J. Med. Internet Res. 13 (4), e90. doi:10.2196/jmir.1880
Xrhealth, (2020). Australia’s health provider Bupa offers XRHealth to customers for physiotherapy needs. Available at: https://www.prnewswire.com/news-releases/australias-health-provider-bupa-offers-xrhealth-to-customers-for-physiotherapy-needs-301123602.html.September 3)
Yen, H. Y., and Chiu, H. L. (2021). Virtual reality exergames for improving older adults’ cognition and depression: A systematic review and meta-analysis of randomized control trials. J. Am. Med. Dir. Assoc. 22, 995–1002. doi:10.1016/j.jamda.2021.03.009
Young, L. A., and Baime, M. J. (2010). Mindfulness-based stress reduction: Effect on emotional distress in older adults. Complement. health Pract. Rev. 15 (2), 59–64. doi:10.1177/1533210110387687
Yu, C. P., Lee, H. Y., and Luo, X. Y. (2018). The effect of virtual reality forest and urban environments on physiological and psychological responses. Urban For. urban Green. 35, 106–114. doi:10.1016/j.ufug.2018.08.013
Zainal, N. H., and Newman, M. G. (2020). Mindfulness enhances cognitive functioning: A meta-analysis of 95 randomized controlled trials. PsyArXiv 4. doi:10.31234/osf.io/vzxw7
Zelenski, J. M., and Nisbet, E. K. (2014). Happiness and feeling connected: The distinct role of nature relatedness. Environ. Behav. 46 (1), 3–23. doi:10.1177/0013916512451901
Zeng, X., Wei, J., Oei, T. P., and Liu, X. (2016). The self-compassion scale is not validated in a Buddhist sample. J. Relig. Health 55 (6), 1996–2009. doi:10.1007/s10943-016-0205-z
Zessin, U., Dickhäuser, O., and Garbade, S. (2015). The relationship between self-compassion and well-being: A meta-analysis. Appl. Psychol. Health Well-Being 7 (3), 340–364. doi:10.1111/aphw.12051
Zhou, J., Zhang, B., Tan, R., Tseng, M. L., and Zhang, Y. (2020). Exploring the systematic attributes influencing gerontechnology adoption for elderly users using a meta-analysis. Sustainability 12 (7), 2864. doi:10.3390/su12072864
Keywords: compassion, mindfulness, nature, virtual reality, gerontechnology, well-being, mental health, older adults
Citation: Sadowski I and Khoury B (2022) Nature-based mindfulness-compassion programs using virtual reality for older adults: A narrative literature review. Front. Virtual Real. 3:892905. doi: 10.3389/frvir.2022.892905
Received: 09 March 2022; Accepted: 12 September 2022;
Published: 30 September 2022.
Edited by:
Pedro Gamito, Universidade Lusófona, PortugalReviewed by:
Ali Fardinpour, Wise Realities Institute for Healthcare Emerging Technologies Research, AustraliaCopyright © 2022 Sadowski and Khoury. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Isabel Sadowski, aXNhYmVsLnNhZG93c2tpQG1haWwubWNnaWxsLmNh
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.